Abstract
We report the case of a 34-year-old woman with hypothenar pain due to a solitary neurofibroma (NF) of the ulnar nerve, with an extrafascicular location, outside Guyon canal, with no clinical evidence of associated neurologic impairment, who was successfully treated with surgical resection. The identification of this isolated tumor led to the diagnosis of a new genetic variant of neurofibromatosis type 1 after genome sequencing. At the 1-year follow-up, the patient remains asymptomatic without recurrence or other peripheral nerve sheath tumors. A solitary NF of a deep-seated nerve is extremely rare, especially in the context of neurofibromatosis type 1. To our knowledge, there are no reports of a NF of the ulnar nerve with an extraneural location. In the presence of a solitary NF related to a deep-seated peripheral nerve, neurofibromatosis type 1 should always be excluded.
Key words: Neurofibromatosis, NF-1, Peripheral nerve sheath tumor, Hand tumor, Solitary neurofibroma, Ulnar nerve neurofibroma
Neurofibromas (NFs) are uncommon, benign peripheral nerve sheath tumors (PNSTs) that result from the abnormal proliferation of Schwann cells and fibroblasts.1, 2, 3, 4, 5 Almost 90% of the NFs occur sporadically, whilst 10% are associated with neurofibromatosis type-1 (NF-1).1,3,5,6 The incidence rates of NFs located in the hand are 0.8% in the general population and between 10% and 15% within patients with NF-1.4 The presence of a solitary NF of the ulnar nerve at the level of the hand is extremely uncommon; also, to our knowledge a solitary NF of the ulnar nerve with an extrafascicular location, outside of Guyon canal, has not been previously described in the literature. Also, to our knowledge there are no reports regarding a symptomatic, solitary NF of the ulnar nerve as an inaugural presentation of NF-1. Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Case Report
The authors report the case of a 34-year-old woman (Hospital da Luz Lisboa), right-handed, with no clinical records of previous or current illness, who was referred to the Hand Surgery outpatient clinic due to progressive left hypothenar pain, which was worse with gripping, with 6 months of evolution. No other symptoms were mentioned. A small, stiff, and painful tumor was palpable deep at the hypothenar eminence. There was no clinical evidence of the hand’s neurologic impairment. Hand and finger ranges of motion were unaffected.
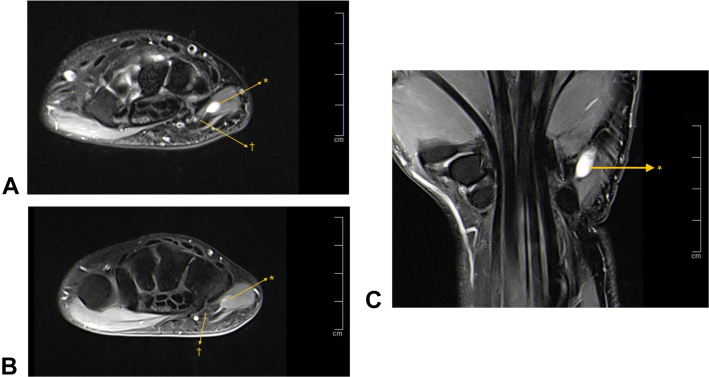
There were no abnormal findings upon plain radiographs (Fig. 1). An ultrasound was performed that showed a cystic-like, well-defined lesion within the hypothenar muscles (Fig. 2). Due to its atypical location and persistent pain, contrast-enhanced magnetic resonance imaging was undertaken. Magnetic resonance imaging revealed a 10 × 5 × 6-mm, oval-shaped, cystic-like mass (hypointense on T1 weighted image and hyperintense on T2 weighted image), with a tiny rim enhancement of its walls. There was no “target sign,” “split-fat sign,” nor denervation edema. Even though these findings were subtle, this mass was located outside the roof of Guyon canal, with a close relationship to the ulnar nerve inside the canal at this location (Fig. 3).
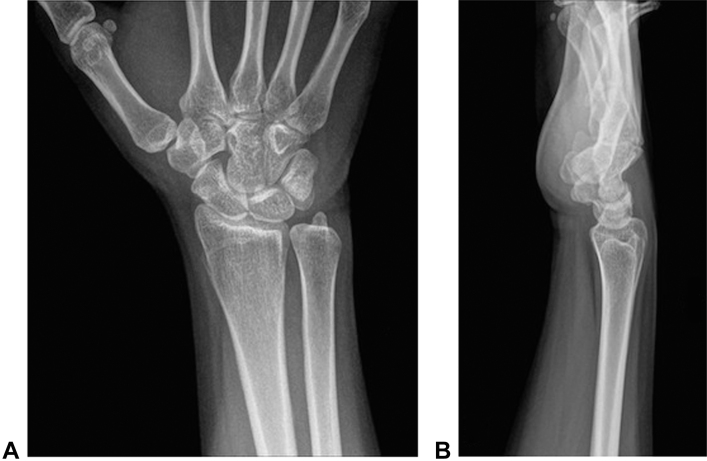
Figure 1.
Radiographs of the A anteroposterior view and B lateral view. No abnormal masses nor calcifications are seen.
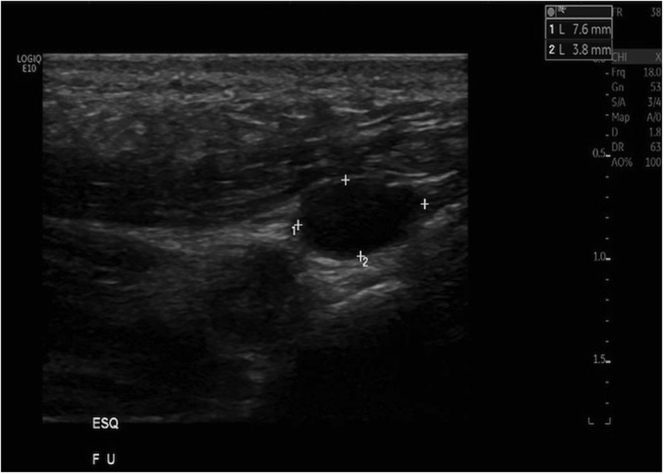
Figure 2.
Ultrasound over the ulnar side of the wrist shows a well-defined, smooth, hypoechogenic intramuscular mass with posterior enhancement but without Doppler signal, simulating a ganglion.
Figure 3.
Magnetic resonance images. A Coronal and B axial proton-density weighted images show a well-defined, ovoid-shaped lesion within the abductor muscle of the digiti minimi with a very high signal. B There is a close relation to the ulnar nerve. C A contrast-enhanced, axial, proton-density weighted image shows no central enhancement, only a mild enhancement of the walls. ∗Tumor; †ulnar nerve.
Given the clinical and imaging findings, the hypothesis of an atypical, solitary NF or a Schwannoma was raised, and the patient underwent surgical resection. The procedure was performed under locoregional anesthesia and tourniquet at the base of the limb. A longitudinal, volar approach over the hypothenar eminence was used, in the direction of the ulnar side of the ring finger and without crossing the proximal wrist flexor crest. Blunt dissection of the hypothenar muscles was undertaken, with care to avoid injury of the sensitive branch of the ulnar nerve. An oval, white, smooth, and elastic tumor, with dimensions of 12 × 7 × 5 mm, was identified over the roof of Guyon canal (volar carpal ligament) and carefully dissected (Fig. 4). A small pedicle connecting the lesion to the inside structures of Guyon canal was identified and ligated, and the tumor was resected en bloc, without opening the canal. Postoperative immediate mobilization of the wrist was encouraged. The anatomopathologic examination confirmed the diagnosis of a NF (Fig. 5).
Figure 4.
Macroscopic appearance of the tumor, which appears as an oval, white, smooth mass of an elastic consistency and dimensions of 12 × 7 × 5 mm.
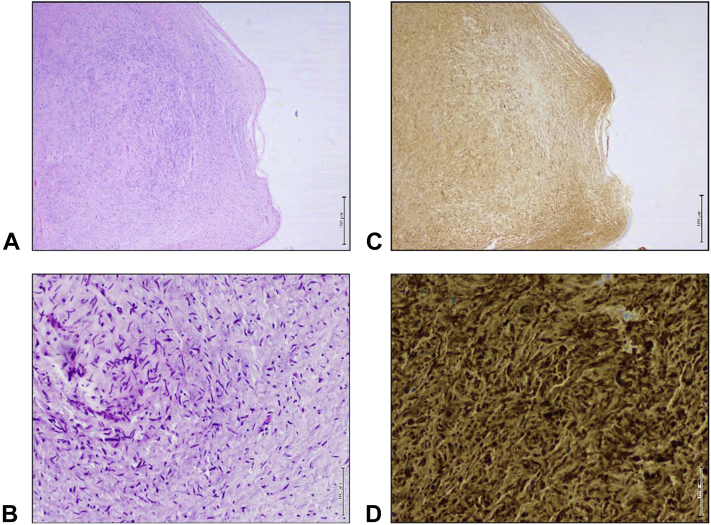
Figure 5.
Predominance of cells with thin, wavy nuclei embedded in a myxoid matrix with variable amounts of collagen arranged in a haphazard fashion. The immunophenotype is characterized by uniform S100 expression in the neoplastic cells These findings are diagnostic of NF. (Hematoxylin-eosin stain; magnification A, ×20 B, ×200 C, ×20 and D, ×200).
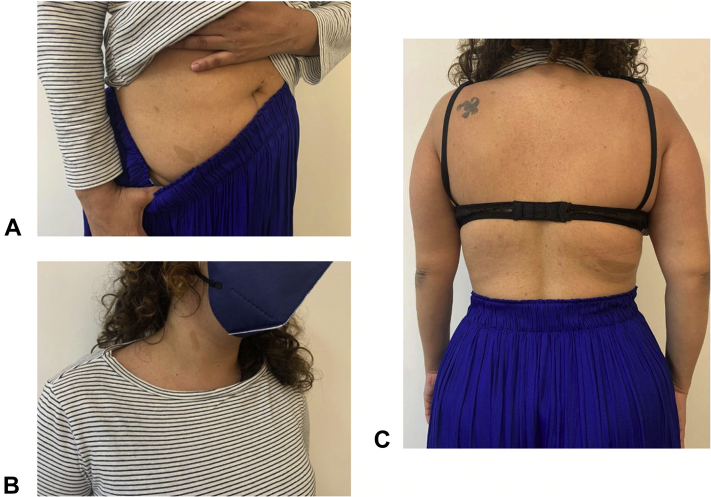
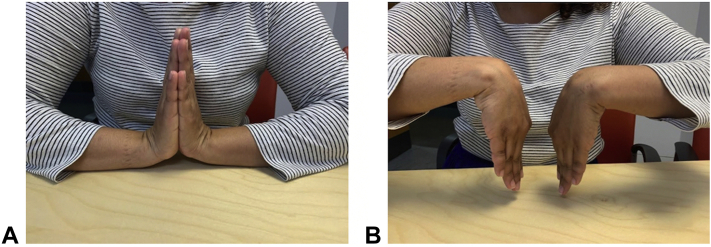
Although solitary NFs tend to occur sporadically and usually are not associated NF-1, cafe au lait spots were noticed on the patient’s back, lower portion of the abdomen, and neck upon follow-up evaluation (Fig. 6). There were no records of a familial history of NF-1. The patient was referred for a genetic evaluation for NF-1 exclusion. After genome sequencing, heterozygotic variant c.1722C>A p. (Ser574Arg) of the NF-1 gene was found, and the diagnosis of NF-1 was established. To our knowledge, this variant has never been described before and therefore cannot be found in the worldwide genome database gnomAD (PM2). The postoperative period elapsed without any complications, and the patient is asymptomatic with normal hand and wrist ranges of motion (Fig. 7). No recurrence or other PNSTs were found.
Figure 6.
Cafe au lait spots present on the A lower portion of the abdomen, B neck, and C lower portion of the back.
Figure 7.
Normal postoperative range of motion in A extension and B flexion.
Discussion
Neurofibromas represent approximately 5% of the benign soft-tissue tumors. Neurofibromas can be classified regarding to their location, morphology, and growth pattern as either solitary (also known as localized, sporadic, or nodular form), diffuse cutaneous (more common at the head and neck), plexiform (multinodular tumors associated with deep nerves or plexus), or massive soft-tissue form (often a diffuse infiltration of a distal extremity).2, 3, 4,6,7 The solitary NF is the most commonly found subtype (approximately 90%), and usually emerges from superficial cutaneous nerves as extraneural and pediculated in relation to the nerve. More rarely, a solitary NF may originate from deep-located nerves, and will typically result in fusiform expansion of the nerve trunk (intraneural subtype).2,3,6 Almost 95% of solitary NFs occur sporadically, mostly in young to middle-aged patients, and are not associated with NF-1.2,3,5,6
A wide range of PNSTs can occur in patients with NF-1, and these are mostly multiple solitary, cutaneous NFs.1,2 The massive-sized or plexiform NF subtypes are highly specific and almost always associated with NF-1.2,5,6 Additionally, larger and multiple solitary NFs, deeper in location, have been described in the setting of NF-1.3,5
The emergence of PNSTs in the extremities is rarely reported in the literature. Also, differently from the presented case, the majority of solitary NFs occurring at the hand or wrist level are cutaneous and tend to arise from the flexor crests and cutaneous nerves in adults, without the presence of NF-1.1
Solitary NFs may have a variable initial presentation, ranging from an asymptomatic, slow-growing tumor that is incidentally found to neurogenic dysfunction with progressive pain, weakness, hypoesthesia, and tingling due to the mass’ effect upon adjacent nerves.3,4,6 Neurologic symptoms are more likely when the NF originates from a deep-seated nerve, whereas superficial NFs are usually small, asymptomatic masses.6
Magnetic resonance imaging is the gold standard used to distinguish NFs from other, more common hand and wrist tumors, such as ganglion, which are the most common soft-tissue tumors at these locations.1,3,6 Radiographs of PNSTs are frequently normal, and might reveal unusual, tumor-associated calcifications or, infrequently, evidence of bone erosion or invasion. On ultrasound, these masses are often hypoechoic with posterior acoustic enhancement, and may simulate a ganglion. The presence of a Doppler signal and peripheral nerve continuity suggests the diagnosis of a PNST.6
On magnetic resonance images, a PNST typically appears as a well-defined, fusiform-shaped mass, typically of less than 5 cm in diameter and with low to intermediate signal intensity on T1 weighted images and high signal intensity on T2 weighted images. The enhancement is usually diffuse and central, unless it has a necrotic or cystic component, as seen in this case. The presence of the mass at the anatomic location of a peripheral nerve is highly suggestive of a PNST. The “string sign” represents the entering and exiting nerve that is in continuity with the nerve sheath tumor. The “target sign” is another classic presentation of PNST, characterized by a central area of hypointensity surrounded by a peripheral halo of hyperintensity on T2 weighted images.1,3,5,6 It can be encountered in all PNSTs, either benign or malignant, but is more commonly seen in NFs than in other PNSTs. Another sign related to PNSTs is the “split sign,” which corresponds to the peripheral rim of fat that is often found surrounding the margins of the PNST. Furthermore, magnetic resonance imaging can depict the neurovascular bundles well and can be used to seek denervation edema or fatty infiltration of the muscles supplied by motor branches of the nerves.3
Despite being the first-line imaging option, magnetic resonance images cannot reliably differentiate NFs from other PNSTs, such as Schwannomas, which are the second most common PNST. Some findings might be suggestive (NF is more central regarding the nerve course, while Schwannoma is more eccentric).1,2,6
The definitive diagnosis is histological, with solitary NFs presenting as generally nonencapsulated structures of fusiform cells meshed in a myxomatous matrix and with low cellularity.1, 2, 3,5 Unlike Schwannomas, NFs are immunohistochemically positive for S100 protein in 85% of cases, as can be seen in this case.1,2 Additionally, NFs incorporate a mixture of non-neoplastic peripheral nerve components, including axons, perineurial cells, fibroblasts, and variable inflammatory elements, such as mast cells, lymphocytes, and CD34+ stromal cells of unclear histogenesis.2,3,7 This contrasts with Schwannoma, which has a more homogeneous neoplastic proliferation of mature Schwann cells.2,7
Surgical treatment of solitary NFs is indicated when they become symptomatic with pain, neurologic impairment, or limited range of motion, or when the tumor has a diameter of more than 4 cm. Also, when the tumor is closely related to a large, deep-seated nerve, its excision is usually offered sooner in order to differentiate it from Schawnnoma and because of the higher risk of malignancy transformation.1,8 For this reason, solitary NFs occurring in the setting of NF-1 are also managed with surgical excision.8 As solitary NFs of deep-seated nerves tend to be intraneural and interfascicular, surgical excision is technically demanding and often associated with a certain degree of iatrogenic fascicular disruption requiring repair.9
Local recurrence is extremely rare after surgical excision.8,10 Simple observation and follow-up can be done in the vast majority of sporadic, solitary NFs not associated with NF-1, given the low recurrence rate and rare malignant transformation.8
Despite NF being described in the literature as a benign tumor, there is a 3% to 15% reported risk of malignant transformation.4,5 In fact, only the plexiform, massive-sized, and localized intraneural forms of NF have been found to be important precursors of malignant PNSTs (MPNSTs).2,4 Although only a small proportion of patients with NF-1 (about 5%) develop MPNST, up to 50% to 60% of MPNSTs occur in patients with NF-1.4,6,9 In the context of NF-1, malignant transformation tends to occur in deeply located NFs and usually is clinically silent.4 Therefore, patients with NF-1 associated with NF should undergo genetic counseling and be monitored throughout their lives for the occurrence of MPNST.4,9,10
To authors’ knowledge, the authors provide the first description of hypothenar pain due to an atypical solitary NF of the ulnar nerve, with an extraneural location, outside of Guyon canal, without neurologic impairment. The extraneural location also made the excisional biopsy easier and resulted in no complications, since there was no need to dissect the tumor from within the ulnar nerve sheath. The finding of cafe au lait spots led to further investigation that to our knowledge confirmed a new pathologic variant of the NF-1 gene c.1722C>A p. (Ser574Arg), therefore establishing the diagnosis of NF-1.
In conclusion, despite being a very rare form of NF in patients with NF-1, in the presence of a solitary NF related to a deep-seated peripheral nerve, NF-1 should always be excluded, given the higher incidence of other PNSTs and MPNSTs in this population; thus, regular monitoring through the patient’s life is warranted.
Footnotes
Declaration of interests: No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
References
- 1.Behrens J., Ho D.S.K., Frojo G., Tadisina K.K., Kraemer B.A. Neurofibromas on the hands. EPlasty. 2018;18:ic8. [PMC free article] [PubMed] [Google Scholar]
- 2.Rodriguez F.J., Folpe A.L., Giannini C., Perry A. Pathology of peripheral nerve sheath tumors: diagnostic overview and update on selected diagnostic problems. Acta Neuropathol. 2012;123(3):295–319. doi: 10.1007/s00401-012-0954-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soldatos T., Fisher S., Karri S., Ramzi A., Sharma R., Chhabra A. Advanced MR imaging of peripheral nerve sheath tumors including diffusion imaging. Semin Musculoskelet Radiol. 2015;19(2):179–190. doi: 10.1055/s-0035-1546823. [DOI] [PubMed] [Google Scholar]
- 4.Tabrizi A., Afshar A., Mohebbi I., Pourjabali M., Taleb H. Schwannoma and neurofibroma, originating from the ulnar nerve in neurofibromatosis: a case report and review of the literature. Surg J (N Y) 2020;6(3):e139–e144. doi: 10.1055/s-0040-1712536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilkinson L.M., Manson D., Smith C.R. Best cases from the AFIP: plexiform neurofibroma of the bladder. RadioGraphics. 2004;24(suppl 1):S237–S242. doi: 10.1148/rg.24si035170. [DOI] [PubMed] [Google Scholar]
- 6.Chee D.W., Peh W.C., Shek T.W. Pictorial essay: imaging of peripheral nerve sheath tumours. Can Assoc Radiol J. 2011;62(3):176–182. doi: 10.1016/j.carj.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 7.Belakhoua S.M., Rodriguez F.J. Diagnostic pathology of tumors of peripheral nerve. Neurosurgery. 2021;88(3):443–456. doi: 10.1093/neuros/nyab021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abdellatif E., Kamel D. Neurofibroma-general. https://www.pathologyoutlines.com/topic/softtissueneurofibroma.html
- 9.Ferner R.E., Huson S.M., Thomas N., et al. Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. J Med Genet. 2007;44(2):81–88. doi: 10.1136/jmg.2006.045906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Messersmith L., Krauland K. StatPearls; FL: 2021. Neurofibroma. Treasure Island. [Google Scholar]