Abstract
The purpose of this study was to compare the reconstructive outcomes of soft‐tissue defects around the foot and ankle with anterolateral thigh (ALT) flap or lateral supramalleolar (LSM) flap and attempt to provide an optimal strategy for elderly patients. A retrospective review of all continuous patients with foot and ankle reconstruction using different flaps from October of 2010 and October of 2020 was performed. Based on the flap types, the patients were divided into two groups: ALT flap group (n = 50) and LSM flap group (n = 46). Outcomes were assessed according to the flap survival rate, early complications, general complications, late complications, cosmetic appearance, functional outcomes and Vancouver Scar Scale (VSS). We found that there was no difference in average age, gender, aetiology, size of the defect, debridement times between the two groups; however, a significant difference in operation time, hospitalisation time and cost were noted between them. What's more, the early flap complications between them were not significantly different. The LSM flap group showed less general complications, less flap bulky and lower cosmetic appearance. Moreover, the functional evaluation and VSS seem similar (P > .05). Thus, The ALT flap and LSM flap are both flaps available for foot and ankle reconstruction in elderly patients. However, the LSM flap offers short operation time, short hospitalisation time, and less cost with a lower frequency of postoperative complications. Thus, we advocate the LSM flap for the reconstruction of moderate‐size defects of the foot and ankle region in elderly patients.
Keywords: anterolateral thigh flap, foot and ankle, lateral supramalleolar flap, soft‐tissue defects
1. INTRODUCTION
In recent years, with the significantly increased number of car and motorcycle accidents, tissue losses from the foot and ankle region are becoming increasingly frequent. Its reconstruction poses unique challenges due to its requirements for durable soft tissue that can withstand the load‐bearing function of the plantar surface while providing a thin, pliable contour for resurfacing the dorsal foot and ankle. 1 , 2 With the rapid development of microsurgical techniques and reliable flap survival in flap transfers, the use of free flap such as the anterolateral thigh (ALT) flap has been gaining more popularity in the reconstruction of such patients. 3 , 4 However, free flaps represent the highest rung on the reconstructive ladder, requiring technically demanding, costly, and time‐consuming operations, with significant complication rates, donor‐site morbidity, failure rates, and risk at the anastomosis. 5 , 6 The elderly patients, who do not need high aesthetic requirements, sometimes cannot tolerate the prolonged free flap surgery.
The lateral supramalleolar (LSM) flap was first described in 1988 by Masquelet et al. 7 It is a fasciocutaneous flap raised from the lateral aspect of the lower leg and used as a distally based pedicled flap. This flap is supplied by the perforating branch of the peroneal artery. The flap is widely used to cover the wound of the foot and ankle with a large range of rotation, presented acceptable aesthetic damage in the donor area without functional damage and are therefore a good choice for covering the foot and ankle injuries. 8 , 9 Figure 1 is a schematic diagram of LSM flap surgery. May for young patients, the free flap group presented better overall aesthetic outcomes in comparison with the local flap group in terms of colour and contour match. 10 However, data from available literature regarding flap selection for elderly patients are still controversial in the reconstruction of these areas.
FIGURE 1.
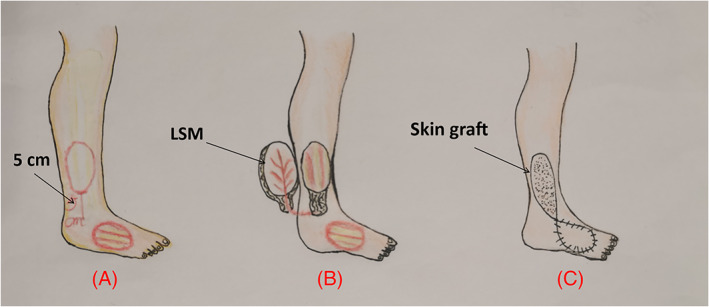
Schematic diagram of LSM flap. (A) The design of the LSM flap is 5 cm above the lateral malleolus. (B) Harvest the LSM flap according to the size of the wound on the back of the foot. (C) LSM flap covers the wound of the foot and the donor site undergoes skin grafting. ALT, anterolateral thigh; LSM, lateral supramalleolar
The aim of the current study is to compare the results obtained from using the LSM flap, and the ALT flap in reconstructing soft‐tissue defects of the ankle and foot in elderly patients.
2. PATIENTS AND METHODS
2.1. Patient materials
A retrospective review was undertaken of all patients who presented with foot and ankle soft‐tissue defects treated with ALT flap or LSM flap between October of 2010 and October of 2020. The inclusion criteria were patients who had a unilateral foot or ankle injury with soft‐tissue defects and who had undergone flap transfers with a follow‐up of no less than 1 year. A total of 10 patients (3 patients in group A and 7 patients in group B) were lost to follow‐up because of various reasons. As a result, 50 patients (ALT flap group) had free ALT perforator flaps; 46 patients (LSM flap group) underwent an LSM flap reconstruction. All procedures were performed in a single institution by the same team. All experimental procedures were approved by the Ethics Committee of our hospital and were in accordance with the Helsinki Declaration. The pictures and information of the patients involved in this article have been approved by patients in writing to publish these cases.
2.2. Surgical procedure
For every patient, the whole of the defect area must be thoroughly inspected and aggressively debrided. Surgical debridement was carried out in all instances, in addition to removal of devitalised tissues; the bony or tendon surface was abraded lightly in instances without periosteal coverage. If it is a fracture case, we will choose the appropriate fixation method. The suitability of this implant needs to be evaluated and possibly revised. If simply the bones or tendons are exposed, external fixation (cast or brace) after surgery is sufficient. Preoperatively, we detected and marked the perforators with the help of a handheld Doppler, further radiological investigation, that is, CT angiography, was only performed when needed.
In the ALT flap group, the patients were reconstructed using a free ALT flap, which was carried out by the descending branch of the lateral circumflex femoral artery and cutaneous branch femoral nerve. The donor site was closed primarily with cosmetic sutures. A below‐the‐knee protective cast in a neutral position was performed for 3 weeks after the operation. Patients were required to have absolute bed rest for 10 days postoperatively.
In the LSM flap group, all patients had reconstructions using LSM flap. A point was marked in the depression of the lower part of the local tibiofibular space, where the perforating branch of the fibular artery penetrates the interosseous membrane, around 5 cm from the tip of the lateral malleolus. The flap can be peninsular or pedunculate, in an island with a distal base, depending on the area of coverage. In all these patients, a full‐thickness skin graft is taken from the anteromedial thigh area to close the supramalleolar cutaneous defect and to repair the lateral leg skin. The same cast fixation was performed for 1 week after the operation. Absolute bed rest was not needed.
2.3. Evaluation of outcomes
In both groups, we recorded patients' characteristics, that is, age, gender, aetiology, size of the defect, debridement times, operation time, hospitalisation time, and the cost. The observation time points of early complications from postoperative to discharge included the incidence of flap necrosis, infection and haematoma in the reconstructed site, as well as infection and haematoma in the donor site. General postoperative complications of the elderly patients, such as pneumonia, pressure ulcer, and venous thrombosis of the lower limbs, were also our observation items. Partial flap necrosis was defined as those being healed by dressing change after flap necrosis; we do not need to perform the second operation. Total flap necrosis was defined as flap compromise requiring complete debridement and need to re‐surgery after skin flap necrosis.
Late complications, including the incidence of flap bulky 11 and flap ulcer, were evaluated at the follow‐up period of 6 months after the operation. We subjectively evaluated the cosmetic appearance of the recipient sites and donor sites on a scale from 1 (close to normal) to 4 (unsatisfactory). 12 , 13 We also assessed functional outcomes by Kofoed ankle scores 14 ranging from 0 to 100 with subscores for pain, function, and mobility (Kofoed score 85‐100 as excellent, 75‐85 as good, 70‐74 as moderate, and <70 as poor). One year after surgery, the scars that had formed at both the reconstructed and donor sites were evaluated according to the VSS 15 in terms of their pigmentation, vascularity, pliability, and height.
2.4. Statistical analysis
The data are presented as the mean ± standard error of the mean. Data were analysed using Student's t unpaired test and the chi‐squared test. P < .05 was considered statistically significant. Statistical analyses were performed using SPSS version 18.0 software.
3. RESULTS
The average age for patients in the ALT flap group was 66.89 ± 8.6 years and in the LSM flap group was 66.09 ± 9.2 years. There were 40 males and 10 females in the ALT flap group and 39 males and 7 females in the LSM flap group. The most common cause of injury was car accidents in both groups (35/50 vs 33/46). The size of the defect of the ALT flap group was 44.2 ± 6.8 cm2 and it was 44.7 ± 5.7 cm2 in the LSM flap group. In the ALT flap group, the debridement times were 2.04 ± 0.61. In the LSM flap group, the debridement times were 1.93 ± 0.57. However, the demographic characteristics such as age, gender, aetiology, size of the defect, and debridement times were similar between the two groups (P > .05; Table 1).
TABLE 1.
Demographic date
| ALT flap group | LSM flap group | t or X2 | P | |
|---|---|---|---|---|
| N | 50 | 46 | ||
| Age (y) | 66.89 ± 8.6 | 66.09 ± 9.2 | t = 0.437 | .663 |
| Gender | X2 = 0.376 | .540 | ||
| Male | 40 | 39 | ||
| Female | 10 | 7 | ||
| Aetiology | X2 = 0.056 | .972 | ||
| Car accident | 35 | 33 | ||
| Crush injury | 10 | 9 | ||
| Other | 5 | 4 | ||
| Size of the defect (cm2) | 44.2 ± 6.8 | 44.7 ± 5.7 | t = 0.365 | .716 |
| Debridement times | 2.04 ± 0.61 | 1.93 ± 0.57 | t = 0.873 | .385 |
Abbreviations: ALT, anterolateral thigh; LSM, lateral supramalleolar.
The results from the perioperative period were shown in Table 2. The operation time in the LSM flap printing group was 2.2 ± 0.40 hours, which was significantly shorter than the conventional group (3.9 ± 0.63 hours, P < .001). There was statistical significance in the hospitalisation time between the ALT flap group (20.4 ± 1.5 days) and the LSM flap group (15.1 ± 1.3 days, P < .001). In addition, the ALT flap group had significantly cost (47.2 ± 4.3 × 103 ¥) than the LSM flap group (37.1 ± 4.7 × 103 ¥, P < .001).
TABLE 2.
The results from the operative condition
| ALT flap group | LSM flap group | t or X2 | P | |
|---|---|---|---|---|
| N | 50 | 46 | ||
| Operation time (h) | 3.9 ± 0.63 | 2.2 ± 0.40 | t = 16.45 | .001* |
| Hospitalisation time (d) | 20.4 ± 1.5 | 15.1 ± 1.3 | t = 18.75 | .001* |
| Cost (×103 ¥) | 47.2 ± 4.3 | 37.1 ± 4.7 | t = 10.9 | .001* |
Abbreviations: ALT, anterolateral thigh; LSM, lateral supramalleolar.
* p < 0.05.
The complications are summarised in Table 3. For the early flap complications, partial necrosis occurred in one case in the ALT flap group and in four cases in the LSM flap group. Total necrosis occurred in one case of the ALT flap group, and none occurred in the LSM flap group. There were two cases of infection and one case of haematoma in the ALT flap group and LSM flap group, respectively. Totally, there are four cases in the ALT flap group and seven cases in the LSM flap group. There was no difference between the two groups for the early complications. About the general complications, there are five pneumonia cases, two pressure ulcer cases, and two venous thrombosis cases in the ALT flap group. One pneumonia case, 0 pressure ulcer cases, and one venous thrombosis case are observed in the LSM flap group. There was no significant difference between the two groups in each term (P > .05). However, the total cases in the ALT flap group (9/50) is more than it in the ALT flap group (2/46, P = .036). To evaluate the late complications of the reconstructed area, we used a numerical statement that was in terms of the bulky flap and flap ulcer. A bulky flap occurred in 20 cases in the ALT flap group and in five cases in the LSM flap group. The flap ulcer occurred in one case of the LSM flap group and no one occurred in the ALT flap group. The results showed that the late complications in the LSM flap group were significantly lower than that in the ALT flap group (P < .05).
TABLE 3.
The results from the complications
| ALT flap group | LSM flap group | X2 | P | |
|---|---|---|---|---|
| N | 50 | 46 | ||
| Early flap complications | ||||
| Partial flap necrosis | 1 | 4 | X2 = 2.176 | .191 |
| Total flap necrosis | 1 | 0 | X2 = 0.93 | .335 |
| Infection | 2 | 2 | X2 = 0.007 | .932 |
| Hematoma | 1 | 1 | X2 = 0.002 | .964 |
| Total | 4 | 7 | X2 = 1.065 | .302 |
| General complications | ||||
| Pneumonia | 5 | 1 | X2 = 2.504 | .114 |
| Pressure ulcer | 2 | 0 | X2 = 1.879 | .170 |
| Venous thrombosis | 2 | 1 | X2 = 0.264 | .607 |
| Total | 9 | 2 | X2 = 4.401 | .036* |
| Late flap complications | ||||
| Flap bulky | 20 | 5 | X2 = 10.56 | .001* |
| Flap ulcer | 0 | 1 | X2 = 1.098 | .295 |
| Cosmetic evaluation | X2 = 23.94 | .001* | ||
| Very good | 23 | 10 | ||
| Good | 22 | 10 | ||
| Satisfactory | 5 | 24 | ||
| Unsatisfactory | 0 | 2 | ||
| Functional evaluation | X2 = 0.234 | .972 | ||
| Excellent | 30 | 26 | ||
| Good | 10 | 11 | ||
| Moderate | 8 | 7 | ||
| Poor | 2 | 2 |
Abbreviations: ALT, anterolateral thigh; LSM, lateral supramalleolar.
* p < 0.05.
In term of cosmetic evaluations (Table 3), the subjective scoring showed that 46% (23/50) of the ALT flap patients rated their appearance as very good, 44% (22/50) as good, 10% (5/50) as satisfactory, and no one unsatisfactory. In the LSM flap group, 21.7% (10/46) of patients rated their appearance as very good, 21.7% (10/46) as good, 52.2% (24/46) as satisfactory, and 4.3% (2/46) as unsatisfactory. The results showed that postoperative satisfaction of guardians of the patients in the ALT flap group was significantly better than that in the LSM flap group (P < .05). In VSS (Table 4), there were no significant differences in the means standards scores between ALT flap and LSM flap groups. In the reconstructed site, the score was 4.05 ± 0.37 vs 4.0 ± 0.37; in the donor site, the score was 3.99 ± 0.37 vs 4.06 ± 0.37, respectively.
TABLE 4.
Vancouver scale of the two groups
| ALT flap group | LSM flap group | t | P | |
|---|---|---|---|---|
| N | 50 | 46 | ||
| Reconstructed site | 4.05 ± 0.37 | 4.0 ± 0.37 | 0.633 | 0.529 |
| Donor site | 3.99 ± 0.37 | 4.06 ± 0.37 | 1.044 | 0.299 |
Abbreviations: ALT, anterolateral thigh; LSM, lateral supramalleolar.
The function of the foot and ankle assessment showed that there was no significant difference between the two groups (Table 3. P > .05). In the ALT flap group, 60% (30/50) took their functional outcomes as excellent, 20% (10/50) as good, 16% (8/50) as moderate, and 4% (2/50) as poor. In the LSM flap group, 56.5% (26/46) took their functional outcomes as excellent, 23.9% (11/46) as good, 15.2% (7/46) as moderate, and 4.3% (2/46) as poor.
3.1. Case report
3.1.1. Case 1 ALT flap
A 67‐year‐old female suffered a skin defect of the left foot with exposed tendons because of a car accident (Figure 2). After thorough debridement, we considered the ALT flap of the right leg. The free skin flap was used to repair the left foot skin defect (Figure 2). The flap was completely alive after the operation, and there was no obvious sign of infection in the wound. Six months after the operation, despite it being a bulky flap, there was a satisfactory functional and cosmetic outcome (Figure 3).
FIGURE 2.

(A‐C) A 67‐year‐old female suffered a skin defect of the left foot with exposed tendons. (D) The wound was repaired with a free flap. (E‐G) Harvest the free flap and suture of the donor site
FIGURE 3.
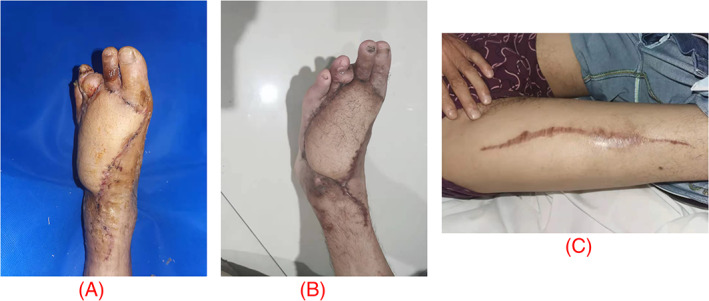
(A) 3 weeks after; (B) 6 months after the operation, a bulky flap. (C) Scars of the donor site
3.1.2. Case 2 LSM flap
A 61‐year old‐female patient sustained a skin defect of the left foot because of trauma. After complete debridement of the affected limb, the left external skin defect was repaired with the LSM flap (Figure 4) and the defect in the donor area is covered with a thick thigh blade (thin skin). One week later, the skin and muscles were vital and free from necrosis and pus (Figure 4 ). One year after the operation (Figure 5), the function is acceptable, the scar on the thigh and calf makes the appearance also satisfactory.
FIGURE 4.
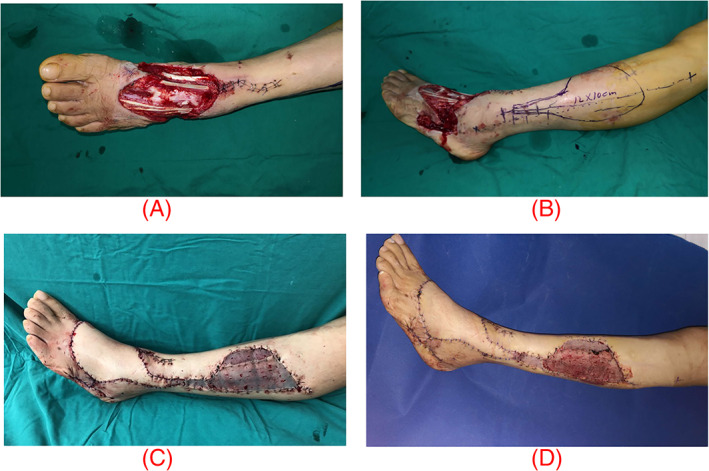
(A) a 61‐year old‐female patient sustained a skin defect of the left foot. (B) Schematic diagram of LSM flap. (C) The wound was repaired with an LSM flap and skin graft. (D) One week later, the skin and muscles were vital and free from necrosis and pus
FIGURE 5.
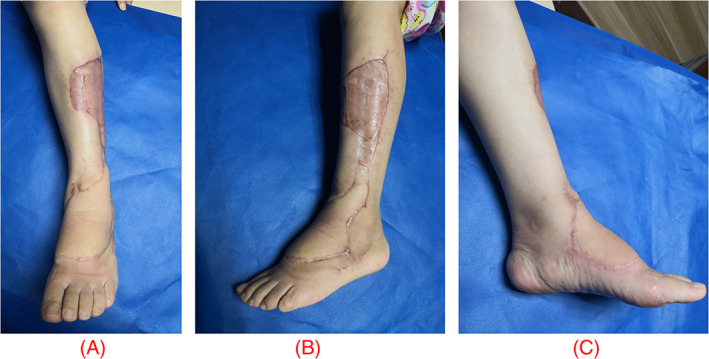
One year after the operation, the scar on the thigh and calf makes the appearance satisfactory. (A) AP view of the calf sacr. (B) lateral view of the calf sacr. (C) medial view of the calf sacr
4. DISCUSSION
At present, reconstructing complex soft‐tissue defects of the foot and ankle in elderly patients poses a major challenge for surgeons because of the limited local soft tissue availability and weight‐bear requirement. 16 A variety of techniques have evolved for reconstructing defects. 17 Sommerlad and McGrouther 18 reviewed a number of these and found that no one particular technique was superior or ideal. Especially for the elderly, as they often suffer from basic diseases and have poor surgical tolerance. Although there are many treatment methods for skin defects of the foot, each method has its own advantages and disadvantages. It is inevitable that skin necrosis, defects, and deep‐tissue exposure will inevitably occur after the operation.
Early years, it was popular of removing the tendon, multiple debridements, negative pressure sealing drainage combined with skin grafting to close the wound, 19 as the trauma was small. However, the number of operations is more, the hospital stay is long, and the skin graft is often not wear‐resistant, easy to rupture and infection. As Song et al 20 first described the use of free flaps such as ALT flap in 1984, free flaps have been widely applied in clinical settings. 21 The free ALT flap receives blood supply by the descending branch of the lateral femoral circumflex artery mostly, partly from the transverse branch. However, the operation is very risky with the highly technical demanding of small vessel anastomosis. The flaps are bloated, which often affects the appearance, and it is even inconvenient to walk in shoes. 10 What's more, many elderly people cannot tolerate is prolonged operation time. The LSM flap is a fasciocutaneous flap raised on the distal perforating branch of the peroneal artery as its vascular pedicle. Masquelet et al showed that the perforating branch of the posterior peroneal artery consistently emerges from a groove between the tibia and the fibula, just proximal to the distal tibiofibular ligament and can be found 5 cm above the lateral malleolus. The main advantages of the LSM flap include its simplicity and ease of elevation, an area up to 9 cm can be included and, importantly, it does not require the sacrifice of a major vessel or muscle function. 3 The LSM flap is similar in texture to the back of the foot, and the location is close. With the right surgical indications, it is a good choice for repairing the defect of the skin and soft tissue of the back of the foot in elderly patients.
In the present study, we found that the operation time, hospitalisation time, and cost in the ALT flap group were higher than those in the LSM free flap group. As the operation of the LSM flap is relatively simple and does not require anastomosis of blood vessels, the operation time is relatively short. In addition, it is no need to wait a long time to observe the survival of the skin flap after surgery in the hospital. Thus, the hospitalisation time and cost were less than that of the ALT flap group. This is consistent with the findings of Yuan. 10 However, they reported higher surgical costs than that of this study, which may be related to their more debridement times.
The incidence of total general complications of the ALT flap group is higher than that of the LSM flap group. It may be due to the cast fixation and absolute bed rest for a long time postoperatively. Especially for elderly patients, long‐term bed rest can cause pneumonia, pressure ulcer, and deep vein thrombosis of the lower extremities. 22
The flap bulky was more in the ALT free flap group because the subcutaneous fat of the thigh is much thicker than the ankle and lower leg, the flaps are obviously more bulky postoperatively compared with the local flaps of the lower leg. Therefore, revision surgery is needed for most patients in the second stage. 23 The advantage of the LSM flap is that it has less subcutaneous fat, skin colour, and texture close to the ankle with no need for secondary flap thinning.
In the study, patients in the ALT flap group have a better aesthetic appearance. The cosmetic evaluation shows better in the ALT flap group. For the LSM flap, the choice is the soft tissue of the calf as the regular donor area for flap transplantation, which affects the appearance of the healthy calf. The calf at some time is an important part of human beings (especially women), as it contributes to our overall beauty. However, for the elderly patients, ALT flap is not the best choice, which need longer hospital time and more medical expenses. Because most of them will not have much pursuit of beauty. What's, more, in terms of ankle function recovery, there was no significant statistical difference between the two groups of patients in the long‐term follow‐up.
For elderly patients with skin defects on the back of the foot, the most critical factors are the definite survival of the flap and the safety of the operation. Therefore, we recommend LSM flap based on the following advantages: (a) the flap is easy to design and harvest with a short operation time. In this study, the operation time of the LSM flap group was significantly shorter than that of the ALT flap group. (b) the perforator blood vessels of the flap are constant, with little variation, while the blood supply of the flap is more reliable than the free flap. (c) the LSM flap comes from a non‐weight‐bearing area, and its texture is similar to that of the back of the foot. The operation can be completed in a single time without the need for a two‐stage revision of its bulky. (d) anastomosis of blood vessels is not required of operation, which is conducive to postoperative care and rehabilitation. Similarly, LSM flaps also have some disadvantages: (a) the distal perforating branch of the peroneal artery is the pedicle of the LSM flap. Due to the limitation of the length of the vascular pedicle, it is difficult to repair the Achilles zone and the distal areas of the foot, especially the medial wound. (b) the donor site is poorly concealed, and the postoperative scar sometimes affects the appearance. For those with a larger flap area, the donor site needs skin grafting, which is prone to pigmentation.
To ensure success and obtain good clinical results, we need to pay attention to the following issues during the perioperative period: (a) although preoperative Doppler‐ultrasound marking of perforating vessels has a high accuracy rate, 24 , 25 we still believe that when the intraoperative skin flap is harvested, one side of the skin flap is first cut to make sure that the pedicle of the flap is a reliable perforator, and the flap is appropriately adjusted according to the specific position of the perforator. (b) during the operation, the severely crushed and contaminated skin should be completely removed. The skin without severe crushing, but with heavier avulsion and poor activity, should also be removed as much as possible. (c) the quality of peripheral blood vessels in the elderly is relatively poor, and the operation should be completed under a magnifying glass as much as possible, especially when the pedicle is dissected, it should be more delicate and gentle to prevent vasospasm, which will affect the blood supply of the skin flap. (d) definite haemostasis of the wound, adequate drainage under the flap, and tension‐free suture of the flap are the keys to the success of the operation. Early postoperative rehabilitation exercises are the guarantee for reducing complications and restoring functions.
A limit of our study is the small sample size; although a statistical comparison of complication rates and healing time was performed, the results need to be confirmed on a larger series to achieve higher statistical power. In addition, our research has certain limitations with the experience of only one medical centre. Prospective multiple‐centre investigations are advisable in future to compare the two flaps. Randomised controlled trials comparing the flaps are desirable to better assess advantages, disadvantages, and indications for the use of local flap and free flap in lower limb reconstruction.
5. CONCLUSION
In conclusion, the ALT flap and LSM flap are both flaps available for foot and ankle reconstruction in elderly patients. However, the LSM flap offers short operation time, short hospitalisation time, and less cost with a lower frequency of postoperative complications. Thus, we advocate the LSM flap for the reconstruction of moderate‐size defects of the foot and ankle region in elderly patients.
Li P, Zhang H, Zhu J, et al. Foot and ankle reconstruction using the lateral supramalleolar flap versus the anterolateral thigh flap in the elderly: A comparative study. Int Wound J. 2022;19(6):1518-1527. doi: 10.1111/iwj.13751
Jian Wang and Shenghu Du contributed equally to this work and should be considered co‐corresponding authors.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Tsuihiji K, Daniel BW, Kageyama T, et al. Free tensor fascia lata true‐perforator flap transfer for reconstruction of the calcaneal soft tissue defect complicated with osteomyelitis in a patient with alcohol‐induced Charcot foot: a case report and literature review. Microsurgery. 2021;41(5):473‐479. [DOI] [PubMed] [Google Scholar]
- 2. Noaman HH, Soroor YO. Foot salvage using microsurgical free muscle flaps in severely crushed foot with soft tissue defects. Injury. 2019;50(Suppl 5):S17‐S20. [DOI] [PubMed] [Google Scholar]
- 3. Lee Z‐H, Abdou SA, Daar DA, et al. Comparing outcomes for Fasciocutaneous versus muscle flaps in foot and ankle free flap reconstruction. J Reconstr Microsurg. 2019;35(9):646‐651. [DOI] [PubMed] [Google Scholar]
- 4. Kiranantawat K, Yeo MS‐W, Imaizumi A, et al. The scrotal free flap: first successful clinical application of a free Super‐Thin External Pudendal Artery (STEPA) flap for reconstruction of a foot defect. J Plast Reconstr Aesthet Surg. 2018;71(2):262‐264. [DOI] [PubMed] [Google Scholar]
- 5. Suominen S, Asko‐Seljavaara S. Free flap failures. Microsurgery. 1995;16(6):396‐399. [DOI] [PubMed] [Google Scholar]
- 6. Maffi TR, Tran NV. Free‐tissue transfer experience at a county hospital. J Reconstr Microsurg. 2001;17(6):431‐433. [DOI] [PubMed] [Google Scholar]
- 7. Masquelet AC, Beveridge J, Romana C, Gerber C. The lateral supramalleolar flap. Plast Reconstr Surg. 1988;81(1):74‐81. [DOI] [PubMed] [Google Scholar]
- 8. Quirino AC, Viegas KC. Fasciocutaneous flaps for covering foot and ankle injuries. Rev Bras Ortop. 2014;49(2):183‐188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sham E, Choi W‐T, Flood SJ. Lateral supramalleolar flap in reconstruction of pressure ulcers in patients with spinal cord injury. ANZ J Surg. 2008. Mar;78(3):167‐171. [DOI] [PubMed] [Google Scholar]
- 10. Yuan K, Zhang F, Lineaweaver WC, Chen X, Li Z, Yan H. The coverage of soft‐tissue defects around the foot and ankle using free or local flaps: a comparative cohort study. Ann Plast Surg. 2021;86(6):668‐673. [DOI] [PubMed] [Google Scholar]
- 11. Zhou Z‐B, Pan D, Pan‐Feng W, et al. Utilization of microdissected thin perforator flap technique in the treatment of bulky and deformed skin flaps. Ann Plast Surg. 2018;80(6):634‐638. [DOI] [PubMed] [Google Scholar]
- 12. Hamdi M, Larsen M, Craggs B, Vanmierlo B, Zeltzer A. Harvesting free abdominal perforator flaps in the presence of previous upper abdominal scars. J Plast Reconstr Aesthet Surg. 2014;67(2):219‐225. [DOI] [PubMed] [Google Scholar]
- 13. Thompson CM, Sood RF, Honari S, Carrougher GJ, Gibran NS. What score on the Vancouver Scar Scale constitutes a hypertrophic scar? Results from a survey of North American burn‐care providers. Burns: J Int Soc Burn Injuries. 2015. Nov;41(7):1442‐1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kofoed H, Sørensen TS. Ankle arthroplasty for rheumatoid arthritis and osteoarthritis: prospective long‐term study of cemented replacements. J Bone Joint Surg Br. 1998;80(2):328‐332. [DOI] [PubMed] [Google Scholar]
- 15. Sullivan T, Smith J, Kermode J, McIver E, Courtemanche DJ. Rating the burn scar. J Burn Care Rehabil. 1990;11(3):256‐260. [DOI] [PubMed] [Google Scholar]
- 16. Wang Y, Liu J, Xie J, Yu G, Luo Q. The effects of platelet‐rich plasma combined with a skin flap transplant on open foot fractures with soft tissue defects. Am J Transl Res. 2021;13(6):6662‐6669. [PMC free article] [PubMed] [Google Scholar]
- 17. Lorenzetti F, Lazzeri D, Bonini L, et al. Distally based peroneus brevis muscle flap in reconstructive surgery of the lower leg: postoperative ankle function and stability evaluation. J Plast Reconstr Aesthet Surg. 2010;63(9):1523‐1533. [DOI] [PubMed] [Google Scholar]
- 18. Sommerlad BC, McGrouther DA. Resurfacing the sole: long‐term follow‐up and comparison of techniques. Br J Plast Surg. 1978;31(2):107‐116. [DOI] [PubMed] [Google Scholar]
- 19. Lv Z, Wang Q, Jia R, Ding W, Shen Y. Pelnac® artificial dermis assisted by VSD for treatment of complex wound with bone/tendon exposed at the foot and ankle, a prospective study. J Invest Surg: Off J Acad Surg Res. 2020;33(7):636‐641. [DOI] [PubMed] [Google Scholar]
- 20. Song YG, Chen GZ, Song YL. The free thigh flap: a new free flap concept based on the septocutaneous artery. Br J Plast Surg. 1984. Apr;37(2):149‐159. [DOI] [PubMed] [Google Scholar]
- 21. Rinker B, Valerio IL, Stewart DH, Pu LLQ, Vasconez HC. Microvascular free flap reconstruction in pediatric lower extremity trauma: a 10‐year review. Plast Reconstr Surg. 2005;115(6):1618‐1624. [DOI] [PubMed] [Google Scholar]
- 22. Chen J, Wang X, Qian H, Ye J, Qian J, Hua J. Correlation between common postoperative complications of prolonged bed rest and quality of life in hospitalized elderly hip fracture patients. Ann Palliat Med. 2020;9(3):1125‐1133. [DOI] [PubMed] [Google Scholar]
- 23. Lai H‐T, Kuo P‐J, Chang C‐H, Lai C‐S, Lin S‐D, Kuo Y‐R. Combined use of liposuction and arthroscopic shaving for delayed debulking of free flaps in head and neck reconstruction. Ann Plast Surg. 2018;80(2S Suppl 1):S36‐S39. [DOI] [PubMed] [Google Scholar]
- 24. Voche P, Merle M, Stussi J‐D. The lateral supramalleolar flap: experience with 41 flaps. Ann Plast Surg. 2005;54(1):49‐54. [DOI] [PubMed] [Google Scholar]
- 25. Burton Wood C, Seim NB, Yancey KL, Netterville JL, Mannion K. Color Doppler ultrasonography for monitoring a free flap anastomosis during a head and neck surgical camp. Ear Nose Throat J. 2021;100(3):160‐161. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


