Abstract
Background
The use of a tourniquet has become widely accepted as standard practice during total knee arthroplasty (TKA). There are conflicting outcomes in using a tourniquet during TKA. This brings to question the role a tourniquet has in TKA. Therefore, we conducted a retrospective cohort study to examine the effects of TKA with and without the use of a tourniquet.
Methods
A total of 120 patients (n = 60 underwent TKA with tourniquet and n = 60 underwent TKA without tourniquet) were included in this study. Patient medical records were retrospectively reviewed for preoperative and postoperative data. The Gross formula, a validated formula for calculating blood loss, was used to calculate each patient’s total blood loss. Statistical analysis was performed using independent t-tests, Mann-Whitney U tests, and/or chi-square tests. Significance was determined using an alpha level of P < .05.
Results
There was no statistically significant difference (P = .49) in the amount of total blood loss between patients undergoing TKA with a tourniquet and those without (199.6 ± 92.2 mL vs 211.1 ± 88.1 mL, respectively). However, there were statistically significant differences in the operating room time (P = .005), surgery time (P = .008), and functional return of postoperative straight leg raise (P < .001) between groups.
Conclusions
This study supports existing evidence that tourniquet use during TKA does not significantly alter blood loss and presents evidence that using a tourniquet during TKA may add additional cost and increase surgical time without benefit.
Keywords: Tourniquet, Total knee arthroplasty, Blood loss, TKA
Introduction
The demand for primary total knee arthroplasty (TKA) continues to rise with recent projections estimated to be over 6 million cases performed each year by 2040 [1]. As popularity increases for this procedure, there is a growing need to improve efficiency in the operating room (OR) while maintaining the quality that leads to excellent patient outcomes. One aspect of TKA that has become widely accepted as standard practice during TKA is the use of a tourniquet. Tourniquet use has been associated with decreased intraoperative blood loss, improved surgical field visualization, and improved cement-bone interface during TKA [[2], [3], [4]]. However, tourniquet use has also been linked to a paradoxical increase in intraoperative blood loss, increased postoperative pain, neuromuscular injuries, wound complications, reperfusion injury, patellar tracking issues, and delayed rehabilitation [[2], [3], [4], [5], [6]]. These conflicting outcomes bring to question the role a tourniquet has in TKA.
The primary purpose of this study was to assess the perioperative blood loss in patients undergoing primary TKA with and without the use of a tourniquet. We hypothesized that patients who underwent TKA without a tourniquet would have more blood loss yet significant improvements in secondary outcomes than patients who underwent TKA with a tourniquet. Secondary outcomes of interest included operative time, surgical time, ability to perform a straight leg raise (SLR) postoperatively, distance walked with physical therapy postoperatively, and length of hospital stay.
Material and methods
We performed a retrospective cohort study through chart review of patients who had undergone a primary TKA from October 2017 to May 2018. Patients were excluded from the study for any revision arthroplasty procedure (including patients who had removal of hardware at the time of primary TKA) and if they had a deformity or ligamentous laxity that required a greater constraint than a cruciate-retaining TKA (posterior stabilized, constrained, or hinged knees). For our pilot study, we chose a total of 120 patients to include for analysis. We chose this sample size based on prior studies, which evaluated tourniquet use in patients with TKA [4,5]. We randomly selected 60 patients who had undergone primary TKA with the use of a tourniquet (T group) and 60 patients who had undergone primary TKA without the use of a tourniquet (NT group). Institutional review board approval was obtained from the Sparrow Hospital for this retrospective chart review.
All TKA surgeries were performed by a single fellowship-trained total joint arthroplasty orthopedic surgeon with over 10 years of experience at a single institution. The implant choice for all patients was a cemented, cruciate-retaining Stryker Triathlon Total Knee (Stryker, Kalamazoo, MI) that included patellar resurfacing. All patients received 1 g of tranexamic acid preoperatively and an additional 1 g dose after the incision was closed. For patients in the T group, the tourniquet was placed high on the operative thigh and inflated to 350 mm Hg just prior to incision and was deflated after component implantation and once the cement had hardened. Hemostasis was obtained prior to closure. A standard surgical technique was performed for routine primary TKA including a medial parapatellar approach, intramedullary femoral guide with posterior condylar referencing, and the use of an extramedullary tibial guide with the measured resection technique. A deep drain was placed in all patients and discontinued on postoperative day (POD) 1. The skin was closed in a layered fashion with suture and occlusive dressing (Prineo; Ethicon, Inc., Somerville, NJ). All patients in our study received a spinal anesthetic with a quadriceps-sparing femoral nerve block as well as an infiltration between popliteal artery and capsule of the knee block that were administered preoperatively. Patients all received sequential compression devices on their lower extremities and began chemoprophylaxis for deep vein thrombosis on POD 1. Depending on time of surgery and spinal anesthetic duration, patients began working with physical therapy on POD 0 or the morning of POD 1.
Medical records were reviewed to collect both preoperative and postoperative data. Preoperative data included age, sex, hemoglobin, hematocrit, platelets, and American Society of Anesthesiologists score. Postoperative data included POD 1 hemoglobin, hematocrit, platelets, drain output, OR time (time in room until out of room), surgical time (incision to skin closure), tourniquet time (if used), perioperative complications (including need for transfusion), and length of hospital stay. Physical therapy initial evaluation for range of motion, gait distance, and the ability to perform an SLR on POD 1 were also recorded.
The Gross formula [7], a validated formula for calculating blood loss [8], was used to calculate each patient’s total blood loss. The formula utilizes sex, height, and weight along with preoperative and postoperative hematocrit values: Vloss total = BV × (Hct preop – Hct postop), where Vloss total = total volume of red blood cell loss in ml and BV = patient’s blood volume before surgery in ml: BV = k1 ×H3+ k2 × W + k3, where H = patient’s height in meters and W = patient’s weight in kg. For males, k1 = 0.3669; k2 = 0.03219; and k3 = 0.6041. For females, k1 = 0.3561; k2 = 0.03308; and k3 = 0.1833.
Statistical analysis was performed by using a Shapiro-Wilk test to assess for data normality. For data sets that were found to be normally distributed, an independent t-test was used for analysis, and the results were recorded as mean values ± 1 standard deviation. Non-normally distributed data were analyzed with a Mann-Whitney U test and were recorded as median and range. Categorical data were analyzed using chi-square tests and reported as counts/frequencies. Statistical analysis was performed with SPSS Statistics software (Version 27.0; IBM Corp, Armonk, NY), and statistical significance was determined using an alpha level of P < .05.
Results
This study included the review of 120 patients who underwent primary TKA. There were 60 patients selected that underwent TKA with the use of a tourniquet (T group) and 60 patients who underwent TKA without the use of a tourniquet (NT group). There were no statistically significant differences (P < .05) between groups with regards to age, sex, body mass index, preoperative hemoglobin and hematocrit, and American Society of Anesthesiologists score (Table 1).
Table 1.
Preoperative characteristics of patients who underwent TKA with or without a tourniquet.
| Preoperative characteristics | With tourniquet | No tourniquet | P value |
|---|---|---|---|
| Ageb(y) | 65.6 (8.1) | 67.7 (10.0) | .2 |
| Sexa | .56 | ||
| Male | 25 | 22 | |
| Female | 35 | 38 | |
| BMIb (Kg/m2) | 33.1 (5.2) | 32.9 (5.3) | .80 |
| Hemoglobinb (G/dL) | 13.4 (1.4) | 13.6 (1.5) | .54 |
| Hematocritc (%) | 40.6 (20) | 39.6 (20.7) | .25 |
| ASAa | 1: 0 | 1: 1 | .13 |
| 2: 28 | 2: 37 | ||
| 3: 32 | 3: 22 |
ASA, American Society of Anesthesiologists; BMI, body mass index.
Data in which significance was determined with independent t-test and recorded as mean ± 1 standard deviation.
Data in which significance was determined with chi-square test.
Data in which significance was determined with Mann-Whitney U test and recorded as the median.
Postoperative data (Table 2) included calculated blood loss, tourniquet time (for the T group), hemoglobin, hematocrit, drain output, OR time, surgical time, distance walked with physical therapy on initial evaluation, ability to perform an SLR on POD 1, and length of stay in the hospital.
Table 2.
Postoperative outcomes of patients who underwent TKA with or without a tourniquet.
| Postoperative outcomes | With tourniquet | No tourniquet | P value |
|---|---|---|---|
| Calculated blood lossb (mL) | 199.6 (92.2) | 211.1 (88.1) | .49 |
| Tourniquet time (min) | 36.6 (7.2) | N/A | |
| Hemoglobinb (g/dL) | 11.5 (1.4) | 11.5 (1.4) | .95 |
| Hematocritb (%) | 34.8 (4.0) | 33.6 (3.6) | .08 |
| Drain outputb (mL) | 210.9 (153.4) | 216.5 (123.8) | .83 |
| Operating room timec (min) | 98.5 (46) | 93 (43) | .005a |
| Surgical timec (min) | 67 (71) | 62 (25) | .008a |
| Distance walked with physical therapyc (feet) | 100 (210) | 100 (598) | .54 |
| Length of stayc (d) | 1.3 (.62) | 1.1 (.54) | .26 |
| Able to perform SLRb | 46/60 (77%) | 60/60 (100%) | <.001a |
Data in which significance was determined with independent t-test and recorded as mean ± 1 standard deviation.
Data in which significance was determined with chi-square test.
Data in which significance was determined with Mann-Whitney U test and recorded as the median.
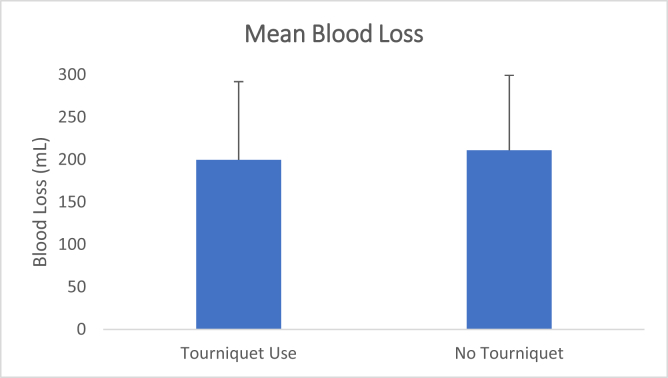
There was no statistically significant difference (P = .49) in calculated blood loss between the T group (199.6 ± 92.2 mL) and NT group (211.1 ± 88.1 mL) (Fig. 1). There were statistically significant differences between the T group and NT group in both OR time (P = .005) and surgical time (P = .008). The proportion of patients able to perform an SLR on POD 1 was larger in the NT group than that in the T group (100% vs 77%, respectively). There were no statistically significant differences in postoperative distance walked with physical therapy, length of hospital stay, hemoglobin, hematocrit, or drain output between the 2 groups.
Figure 1.
Mean blood loss (±1 standard deviation), determined by the Gross formula, for the tourniquet use group and the no tourniquet group.
There were no intraoperative or immediate postoperative complications observed in either group, and no transfusions were required during the hospital stay of any patients.
Discussion
The results of the current study demonstrate that there was no statistically significant difference (P = .49) in the calculated amount of total blood volume lost during surgery between patients who underwent TKA with a tourniquet and those without (199.6 ± 92.2 mL vs 211.1 ± 88.1 mL, respectively). It is important to amass such data as the number of TKA cases continues to rise, and surgeons must use every available advantage to produce a satisfactory outcome for their patients. Increased blood loss in TKA may lead to an increase in blood product transfusion rate, which not only amplifies the risk of complications but also increases the cost of the procedure [6]. Tourniquet use, which is suggested to decrease blood loss during TKA continues to be a highly debated topic. Meta-analyses have shown conflicting results with respect to tourniquet use in TKA; 1 meta-analysis suggests a decrease in intraoperative and calculated blood loss when using a tourniquet [9], while another suggests that using a tourniquet produces no difference in total blood loss [10]. Tai et al. [6] preformed a randomized controlled trial with and without tourniquet use and found that patients undergoing TKA without a tourniquet had higher volumes of total blood loss. This is in contrary to the study by Schnettler et al. [5] who found a paradoxical increase in total blood loss with tourniquet during TKA, which was likely secondary to hidden blood loss. Our results demonstrate no significant difference in blood loss between groups, which may be explained, in part, by the surgical technique performed by the surgeon in our study. In our protocol with tourniquet use, the tourniquet is let down prior to the start of incision closure. At this time, hemostasis can be gained, which may help in preventing any significant hidden blood loss.
Achieving a great functional outcome for every patient should be the goal of every surgeon performing primary TKA. However, functional gains are multifactorial and are influenced by factors that occur outside of the operative theater including pain management, patient’s muscle strength, and range of motion postoperatively. Several studies have shown that there may be a small advantage at the 3- to 6-month mark in the timed up and go (TUG) test and stair climb testing in patients who underwent TKA without the use of a tourniquet. Alexandersson et al. [11] found a 10% improvement (1.1 seconds) in the TUG test in patients who underwent TKA without a tourniquet. Although that improvement was statistically significant, it has been shown that the minimal clinically important difference for the TUG test is 1.3 seconds [12,13]. Similarly, Goel et al. found that patients who underwent TKA without the use of a tourniquet were able to perform a faster stair climb at 6-month follow-up (14.6 seconds) than patients who had a tourniquet applied (17.4 seconds) [14]. Again, this did not meet a minimal clinically important difference, which is 5.5 seconds for the stair climb test [15]. As our study only assessed immediate postoperative and intraoperative measures, we did not examine other functional measures (eg, TUG test or stair climb testing) in our patients. We did, however, examine the distance walked with physical therapy postoperatively and did not find a statistically significant difference between the NT group and T group (P = .54) although there was considerably more variance observed in the NT group.
Tourniquet use has been associated with a decrease in quadricep volume [1] as well as electromyography changes in the quadriceps for up to 6 months post-TKA [2]. Quadricep muscle testing postoperatively in the clinical setting is commonly assessed by having the patient perform an active SLR [16]. Conflicting literature exists regarding the relevance of the SLR test. Ishii et al. found no correlation of SLR to standing up and walking [16]; however, a more recent study found that the ability to perform an SLR on POD 1 led to decreased time to ambulation, stair climbing, and a decrease in length of stay in the hospital [17]. Our study demonstrated a statistically significant difference in the patient’s ability to perform an SLR on POD 1, with 100% of patients in the NT group able to SLR while only 77% of patients in the T group were able to SLR (P < .001). While this difference was detected, as previously noted, we did not show any difference in the length of stay or distance walked with physical therapy between the 2 groups in our current sample size.
Lastly, we found a statistically significant time difference within our 2 groups in total OR time (98.5 minutes T group vs 93 minutes NT group, P = .005) and surgical time (67 minutes T group vs 62 minutes NT group, P = .008). This difference is likely due to tourniquet application and obtaining hemostasis once the tourniquet is deflated and before the closure was started. This is an interesting finding due to the increased focus on the rising health-care costs and value of care. A study by Ronald Shippert [18] found that the average cost for 1 minute of OR time was $66, which included the cost of anesthesia. Another study by Childers and Maggard-Gibbons [19] found that an average of 1 minute of OR time costs between $36 and $37. The surgeon in our study routinely performs 250-300 primary TKAs per year at our institution, which would relate to up to 1650 minutes of OR time saved per year if tourniquets were not used. Although there is a wide range of OR cost per minute documented in literature, a rough estimate with that amount of time saved could have resulted in saving $75,000 per year.
There are limitations to our study. The study was performed by a single fellowship-trained total joint arthroplasty surgeon that operates at 3 different centers. Data were only available at 1 center limiting the number of patients we included in our study. Taken together, this limits the generalizability of our findings. While the sample size was relatively small, there have been other studies with similar samples sizes used to estimate blood loss. Our current pilot study has an insufficient sample size to draw major conclusions but does lay the foundation for further adequately powered studies to be performed. Blood loss was also not directly measured in this study although this concern can be mitigated by our use of the Gross formula to calculate total blood loss. This formula has remained accurate in calculating the measurement of total blood loss even after review as it demonstrated a maximum of 5% error after patients had retained 2 liters of fluid [5]. This study was also a result of a protocol change due to the senior surgeon discontinuing the use of a tourniquet when performing TKA. This may have resulted in selection bias in patient selection; however, there was no difference in preoperative variables between groups.
Conclusions
In conclusion, based on the result of our study, there was no statistically significant difference in the amount of total blood loss between patients undergoing TKA with a tourniquet and those without. Furthermore, there was statistically significant differences in the OR time, surgery time, and functional return of postoperative SLR ability between groups. This study supports existing evidence that tourniquet use does not alter blood loss in TKA and presents evidence that using a tourniquet during TKA may add additional cost and increase surgical time without benefit.
Conflicts of interest
The authors declare there are no conflicts of interest.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2022.08.010.
Appendix A. Supplementary Data
References
- 1.Singh J.A., Yu S., Chen L., Cleveland J.D. Rates of total joint replacement in the United States: future projections to 2020–2040 using the national inpatient sample. J Rheumatol. 2019;46:1134–1140. doi: 10.3899/jrheum.170990. [DOI] [PubMed] [Google Scholar]
- 2.Arthur J.R., Spangehl M.J. Tourniquet use in total knee arthroplasty. J Knee Surg. 2019;32:719–729. doi: 10.1055/s-0039-1681035. [DOI] [PubMed] [Google Scholar]
- 3.Jiang F., Zhong H., Hong Y., Zhao G. Use of a tourniquet in total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Orthop Sci. 2015;20:110–123. doi: 10.1007/s00776-014-0664-6. [DOI] [PubMed] [Google Scholar]
- 4.McCarthy Deering E., Hu S.Y., Abdulkarim A. Does tourniquet use in TKA increase postoperative pain? A systematic review and meta-analysis. Clin Orthop. 2019;477:547–558. doi: 10.1097/CORR.0000000000000572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schnettler T., Papillon N., Rees H. Use of a tourniquet in total knee arthroplasty causes a paradoxical increase in total blood loss. J Bone Joint Surg Am. 2017;99:1331–1336. doi: 10.2106/JBJS.16.00750. [DOI] [PubMed] [Google Scholar]
- 6.Tai T.-W., Chang C.-W., Lai K.-A., Lin C.-J., Yang C.-Y. Effects of tourniquet use on blood loss and soft-tissue damage in total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2012;94:2209–2215. doi: 10.2106/JBJS.K.00813. [DOI] [PubMed] [Google Scholar]
- 7.Gross J.B. Estimating allowable blood loss: corrected for dilution. Anesthesiology. 1983;58:277–280. doi: 10.1097/00000542-198303000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Gao F.-Q., Li Z.-J., Zhang K., Sun W., Zhang H. Four methods for calculating blood-loss after total knee arthroplasty. Chin Med J (Engl) 2015;128:2856–2860. doi: 10.4103/0366-6999.168041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cai D.F., Fan Q.H., Zhong H.H., Peng S., Song H. The effects of tourniquet use on blood loss in primary total knee arthroplasty for patients with osteoarthritis: a meta-analysis. J Orthop Surg Res. 2019;14:348. doi: 10.1186/s13018-019-1422-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu Y., Si H., Zeng Y., Li M., Xie H., Shen B. More pain and slower functional recovery when a tourniquet is used during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2020;28:1842–1860. doi: 10.1007/s00167-019-05617-w. [DOI] [PubMed] [Google Scholar]
- 11.Alexandersson M., Wang E.Y., Eriksson S. A small difference in recovery between total knee arthroplasty with and without tourniquet use the first 3 months after surgery: a randomized controlled study. Knee Surg Sports Traumatol Arthrosc. 2019;27:1035–1042. doi: 10.1007/s00167-018-5196-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gautschi O.P., Stienen M.N., Corniola M.V., Joswig H., Schaller K., Hildebrandt G., et al. Assessment of the minimum clinically important difference in the timed up and go test after surgery for lumbar degenerative disc disease. Neurosurgery. 2017;80:380–385. doi: 10.1227/NEU.0000000000001320. [DOI] [PubMed] [Google Scholar]
- 13.Wright A.A., Cook C.E., Baxter G.D., Dockerty J.D., Abbott J.H. A comparison of 3 methodological approaches to defining major clinically important improvement of 4 performance measures in patients with hip osteoarthritis. J Orthop Sports Phys Ther. 2011;41:319–327. doi: 10.2519/jospt.2011.3515. [DOI] [PubMed] [Google Scholar]
- 14.Goel R., Rondon A.J., Sydnor K., Blevins K., O'Malley M., Purtill J.J., et al. Tourniquet use does not affect functional outcomes or pain after total knee arthroplasty: a prospective, double-blinded, randomized controlled trial. J Bone Joint Surg Am. 2019;101:1821–1828. doi: 10.2106/JBJS.19.00146. [DOI] [PubMed] [Google Scholar]
- 15.Kennedy D.M., Stratford P.W., Wessel J., Gollish J.D., Penney D. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord. 2005;6:3. doi: 10.1186/1471-2474-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ishii Y., Noguchi H., Sato J., Ishii H., Yamamoto T., Sakurai T., et al. Clinical relevance of active straight leg raising, standing up, and walking after total knee arthroplasty in a cross-sectional study. Eur J Orthop Surg Traumatol. 2018;28:947–953. doi: 10.1007/s00590-017-2100-z. [DOI] [PubMed] [Google Scholar]
- 17.Suh J., Liow M.H.L., Pua Y.H., Chew E.S.X., Chia S.L., Lo N.N., et al. Early postoperative straight leg raise is associated with shorter length of stay after unilateral total knee arthroplasty. J Orthop Surg (Hong Kong) 2021;29 doi: 10.1177/23094990211002294. 230949902110022. [DOI] [PubMed] [Google Scholar]
- 18.Shippert R.D. A study of time-dependent operating room fees and how to save $100 000 by using time-saving products. Am J Cosmet Surg. 2005;22:25–34. doi: 10.1177/074880680502200104. [DOI] [Google Scholar]
- 19.Childers C.P., Maggard-Gibbons M. Understanding costs of care in the operating room. JAMA Surg. 2018;153:e176233. doi: 10.1001/jamasurg.2017.6233. [DOI] [PMC free article] [PubMed] [Google Scholar]
Further readings
- 1.Guler O., Mahirogullari M., Isyar M., Piskin A., Yalcin S., Mutlu S., et al. Comparison of quadriceps muscle volume after unilateral total knee arthroplasty with and without tourniquet use. Knee Surg Sports Traumatol Arthrosc. 2016;24:2595–2605. doi: 10.1007/s00167-015-3872-5. [DOI] [PubMed] [Google Scholar]
- 2.Liu D., Graham D., Gillies K., Gillies R.M. Effects of Tourniquet Use on Quadriceps Function and Pain in Total Knee Arthroplasty. Knee Surg Relat Res. 2014;26:207–213. doi: 10.5792/ksrr.2014.26.4.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.