Abstract
Amiodarone is a widely prescribed antiarrhythmic drug with a relatively high incidence of adverse effects associated with its long-term oral use. Pulmonary toxicity may manifest as organizing pneumonia, which responds well to amiodarone discontinuation and corticosteroid treatment. We present a case of an organizing pneumonia secondary to amiodarone treatment, discuss the diagnostic approach and provide tips for an accurate diagnosis based on imaging findings. A brief literature review is performed.
Keywords: CT, Organizing pneumonia, Amiodarone
CT; Organizing pneumonia; Amiodarone.
1. Case description
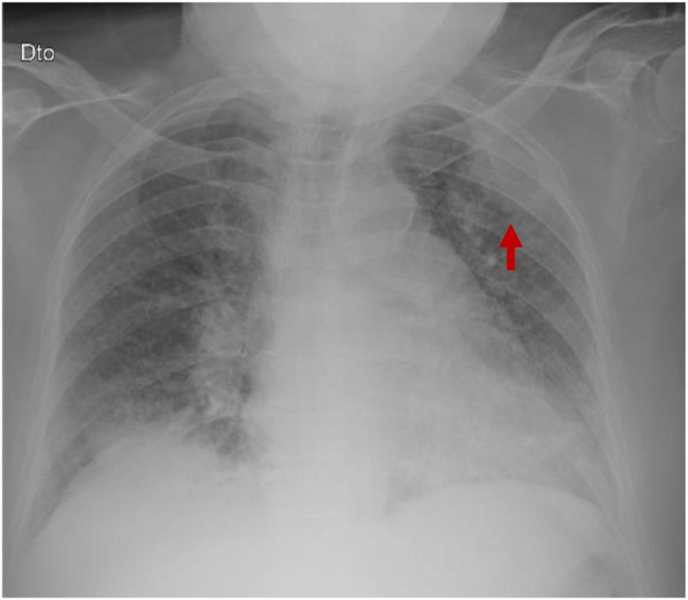
We present the case of a 64-year-old female who came to the emergency department with a 2-week history of fever, nonproductive cough, and pleuritic chest pain. She also complained of malaise and weight loss (12 kg) during the previous 3 months. Her past medical history included rheumatic valve disease and atrial fibrillation, treated with oral amiodarone for the last 4 years. Chest radiography (Figure 1) performed in the emergency department revealed an ill-defined opacity in the left upper lung field (arrow), superimposed on the left scapula. Chest CT was performed for further work-up.
Figure 1.
Chest radiography performed in the emergency department showing an ill-defined opacity in the upper left lung superimposed with the left scapula (arrow).
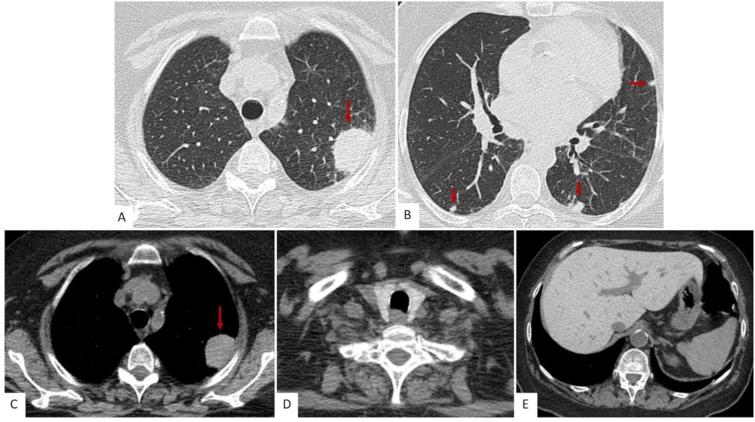
Unenhanced chest CT (Figure 2) revealed a subpleural hyperattenuating mass in the left upper lobe (arrows in A and C) and small subpleural nodules (arrows in B and C). The thyroid (D) and liver (E) parenchyma were hyperattenuating due to iodine accumulation secondary to amiodarone treatment.
Figure 2.
Unenhanced chest CT. Lung window through the upper (A) and mid (B) lung fields showing a subpleural hyperattenuating mass (arrow in A and C) and small subpleural nodules (arrows in B). The thyroid (D) and liver (E) parenchyma are also hyperattenuating due to iodine accumulation secondary to amiodarone treatment.
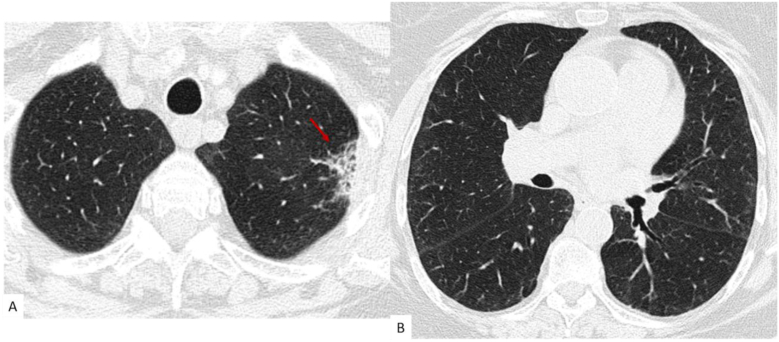
Lung cancer was suspected, and a transthoracic lung biopsy of the mass was performed. Pathology revealed the presence of foamy macrophages and features of organizing pneumonia (OP), establishing the diagnosis of OP secondary to amiodarone treatment. Amiodarone treatment was stopped and replaced with flecainide. In addition, electric cardioversion was performed three weeks after the initial CT and the patient has remained in sinus rhythm until the last follow-up. The patient’s symptoms and radiographic findings also improved. An early CT follow-up was performed two months after the emergency department visit, which showed mild improvement in the lung findings. CT performed six months after the initial episode (Figure 3) shows almost complete resolution of the lung findings, with residual fibrotic changes where the mass was previously seen (arrow in A), which persisted in the last CT follow-up performed 12 months after the acute episode. Thyroid and liver hyperdensity persisted one year after amiodarone discontinuation.
Figure 3.
Lung window unenhanced chest CT through the upper (A) and mid (B) lung fields, obtained 6 months after the diagnosis and treatment. There is resolution of the previously described anomalies, with mild residual fibrotic changes remaining where the left upper lobe mass was previously seen.
2. Case discussion
Organizing pneumonia is a rare disease manifesting clinically by a subacute illness with variable degrees of cough and dyspnea. Most patients recover completely with corticosteroid treatment. Relapses are common, and a small subset of patients may have progressive disease with lung fibrosis. OP can be secondary to several conditions, including infections, drug toxicity, radiotherapy, or inhalation of toxics. When no underlying cause is found it is called cryptogenic.
The classic form manifests radiologically by patchy areas of migratory lung consolidations, usually bilaterally and predominantly in a subpleural or peribronchial distribution [1]. The presence of perilobular opacities and reversed halo sign support the diagnosis [2]. The nodular form with nodular opacities and mass-like areas of consolidation is less common and poses a diagnostic challenge. In these cases, transthoracic lung biopsy is frequently required to establish the diagnosis and exclude lung neoplasia [3].
Histologically OP corresponds to the presence of granulation tissue filling the alveoli and alveolar ducts, with chronic inflammation of the surrounding lung parenchyma. Although most abnormalities are alveolar, OP is still classified as an interstitial pneumonia by the American Thoracic Society and European Respiratory Society [2].
Amiodarone is a widely prescribed antiarrhythmic drug, with a relatively high incidence of adverse effects associated with its long-term oral use. Lung toxicity ranges from mild subacute lung disease to acute respiratory distress syndrome (ARDS) [4]. Subacute and chronic lung toxicity may present different radiographic patterns, most frequently eosinophilic pneumonia, OP or NSIP. Patients frequently present with hyperattenuating liver, spleen and thyroid on nonenhanced CT due to iodine accumulation. These findings are specific to amiodarone treatment but may be seen in patients without toxicity. However, their association with hyperdense lung consolidations or masses is a unique feature of amiodarone lung toxicity. Treatment consists of drug discontinuation and corticosteroid treatment, with a minority of patients remaining with residual changes or developing pulmonary fibrosis [4].
Patient informed consent was obtained for the publication of this case report.
3. Teaching point
Hyperattenuating liver, spleen, and thyroid, associated with hyperattenuating lung consolidations or masses on nonenhanced CT scans is a unique finding of amiodarone lung toxicity.
Declarations
Author contribution statement
All authors listed have significantly contributed to the investigation, development and writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
No data was used for the research described in the article.
Declaration of interest’s statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Footnotes
This article is a part of the Advanced Imaging in Cardiovascular Diseases.
References
- 1.Baque-Juston M., Pellegrin A., Leroy S., Marquette C.H., Padovani B. Organizing pneumonia: what is it? A conceptual approach and pictorial review. Diagn. Interv. Imaging. 2014;95(9):771–777. doi: 10.1016/j.diii.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 2.Travis W.D., Costabel U., Hansell D.M., et al. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am. J. Respir. Crit. Care Med. 2013;188(6):733–748. doi: 10.1164/rccm.201308-1483ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MacMahon H., Naidich D.P., Goo J.M., et al. Guidelines for management of incidental pulmonary nodules detected on CT images: from the fleischner society. Radiology. 2017;284(1):228–243. doi: 10.1148/radiol.2017161659. [DOI] [PubMed] [Google Scholar]
- 4.Papiris S.A., Triantafillidou C., Kolilekas L., Markoulaki D., Manali E.D. Amiodarone: review of pulmonary effects and toxicity. Drug Saf. 2010;33(7):539–558. doi: 10.2165/11532320-000000000-00000. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data was used for the research described in the article.