Key Points
Question
What is the estimated prevalence of substance use disorders in the US?
Findings
In this cross-sectional study, using the benchmark multiplier method and Medicaid administrative data in combination with data from the National Survey on Drug Use and Health for 2018 and 2019, the 12-month prevalence estimates of alcohol use disorder, cannabis use disorder, opioid use disorder, and stimulant use disorder were higher than estimates from the National Survey on Drug Use and Health.
Meaning
The findings suggest that the prevalence of substance use disorders may be considerably higher than National Survey on Drug Use and Health estimates indicate.
This cross-sectional study estimates the prevalence of substance use disorders among adolescents and adults in the US.
Abstract
Importance
Prevalence estimates of substance use disorders in the US rely on general population surveys. However, major population groups, such as homeless individuals and institutionalized individuals, are not captured by these surveys, and participants may underreport substance use.
Objective
To estimate the prevalence of substance use disorders in the US.
Design, Setting, and Participants
The benchmark multiplier method was used to estimate the prevalence of alcohol, cannabis, opioid, and stimulant use disorders based on data from the Transformed Medicaid Statistical Information System (T-MSIS) (the benchmark) and the National Survey on Drug Use and Health (NSDUH) (the multiplier) for 2018 and 2019. T-MSIS collects administrative data on Medicaid beneficiaries 12 years and older with full or comprehensive benefits. NSDUH is a nationally representative annual cross-sectional survey of people 12 years and older. Data were analyzed from February to June 2022.
Main Outcomes and Measures
Prevalence of substance use disorders was estimated using the benchmark multiplier method based on T-MSIS and NSDUH data. Confidence intervals for the multiplier method estimates were computed using Monte Carlo simulations. Sensitivity of prevalence estimates to variations in multiplier values was assessed.
Results
This study included Medicaid beneficiaries 12 years and older accessing treatment services in the past year with diagnoses of alcohol (n = 1 017 308 in 2018; n = 1 041 357 in 2019), cannabis (n = 643 737; n = 644 780), opioid (n = 1 406 455; n = 1 575 219), and stimulant (n = 610 858; n = 657 305) use disorders and NSDUH participants with 12-month DSM-IV alcohol (n = 3390 in 2018; n = 3363 in 2019), cannabis (n = 1426; n = 1604), opioid (n = 448; n = 369), and stimulant (n = 545; n = 559) use disorders. The benchmark multiplier prevalence estimates were higher than NSDUH estimates for every type of substance use disorder in both years and in the combined 2018 to 2019 sample: 20.27% (95% CI, 17.04-24.71) vs 5.34% (95% CI, 5.10-5.58), respectively, for alcohol; 7.57% (95% CI, 5.96-9.93) vs 1.68% (95% CI, 1.59-1.79) for cannabis; 3.46% (95% CI, 2.97-4.12) vs 0.68% (0.60-0.78) for opioid; and 1.91% (95% CI, 1.63-2.30) vs 0.85% (95% CI, 0.75-0.96) for stimulant use disorders. In sensitivity analyses, the differences between the benchmark multiplier method and NSDUH estimates persisted over a wide range of potential multiplier values.
Conclusions and Relevance
The findings in this study reflect a higher national prevalence of substance use disorders than that represented by NSDUH estimates, suggesting a greater burden of these conditions in the US.
Introduction
Access to accurate estimates of the prevalence of substance use disorders (SUDs) in a country is essential for resource allocation and service planning. In many industrialized countries, these estimates typically rely on general population surveys.1,2,3,4 In the US, the annual National Survey on Drug Use and Health (NSDUH), previously known as the National Household Survey on Drug Abuse (NHSDA), has been the main source of information on the prevalence of SUDs for decades.4,5,6,7 However, there are concerns that NSDUH and other general population surveys may not capture all persons with SUDs in the population because they do not cover homeless and institutionalized persons, including those in the criminal justice system, and these population groups often have a higher prevalence of SUDs.8,9,10 Furthermore, individuals with SUDs may be difficult to recruit in survey research.11,12 Even among those who do participate in surveys, many may not fully disclose the extent of their substance use due to the stigma associated with substance use disorders.6,7,8,13,14 Such partial disclosure would result in underestimation of SUD prevalence.15,16
The extent to which population surveys may underestimate the prevalence of SUDs was highlighted in a 1993 study6,7 of cocaine use. The study found that actual lifetime cocaine use based on multiple data sources was 2 to 3 times higher than estimates from the NHSDA. A more recent study17 in which investigators from Massachusetts linked multiple data sources and used the capture-recapture method to estimate the prevalence of opioid use disorder in the state similarly found that the 2015 prevalence of opioid use disorder in the state was nearly 4 times the NSDUH estimate (4.6% vs 1.4%).
Underestimation is not limited to harder drugs, such as cocaine and opioids. Hasin and Grant18 presented data from the Veterans Health Administration, national emergency department visits, and mortality data indicating a 50% to 115% increase in cannabis use disorder in the first decade of the 21st century. Yet the NSDUH did not record meaningful change in cannabis use disorder in this period.19
These studies highlight the benefit of using more than 1 source of data to provide a more accurate estimate of the prevalence of SUDs.20 There are calls for such data combination strategies both in the US21 and the European Union.22 Combining survey data with administrative data is one such strategy.10,23,24 As an example, Compton and colleagues10 adjusted NSDUH prevalence estimates based on data from prison and jail inmates. The estimated national prevalence of drug use disorder increased from 2% to 2.5% after this adjustment—a 25% increase.
In this report, the prevalence of SUDs in the US was estimated by combining NSDUH and Medicaid administrative data using the benchmark multiplier method that is commonly used for estimating the prevalence of stigmatized behaviors and health conditions in marginalized population groups not fully captured in general population surveys.25,26,27,28,29 This method has been used to estimate the prevalence of SUDs in a number of other settings22,25,26,28,30 and, more recently, to estimate the prevalence of asymptomatic COVID-19 infection.27 More specifically, I estimate the prevalence of alcohol, cannabis, opioid, and stimulant use disorders in the US in 2018 and 2019 by combining administrative Medicaid data on SUD treatment service use and data from NSDUH for these years.
Methods
NSDUH researchers obtained informed consent from all participants and from parents or guardians of adolescents aged 12 to 17 years. The NSDUH data collection protocol was approved by the institutional review board at Research Triangle Institute International. The present study used publicly available deidentified data deemed exempt from review by the institutional review board of the Johns Hopkins Bloomberg School of Public Health.
Samples
Medicaid data were drawn from the Transformed Medicaid Statistical Information System (T-MSIS) Substance Use Disorder Data Books for 2018 and 2019.31,32 The T-MSIS sample comprised 55 887 507 Medicaid beneficiaries with full benefits in 2018 and 55 606 179 in 2019. Medicaid-Expansion Children’s Health Insurance Program (CHIP) and separate CHIP beneficiaries who were enrolled only in these programs throughout the year were excluded. The T-MSIS data books include separate counts of beneficiaries who received services for alcohol, cannabis, opioid, and stimulant use disorders. These counts were used as benchmark data for computing the benchmark multiplier estimates in this study. Data from the T-MSIS Data Books are presented as aggregates and do not include any individual identifiers. Outpatient care was the most common SUD treatment setting for Medicaid beneficiaries and counselling the most common form of treatment (eTable 1 in the Supplement).
The NSDUH sampling methods have been described in detail elsewhere.33 In short, NSDUH uses a multistage area probability sampling design to survey the noninstitutionalized civilian population 12 years and older residing in the US with response rates of 66.6% in 2018 and 64.9% in 2019 according to the American Association for Public Opinion Research standard definitions of Response Rate 2.34 The public access data files used in this study included 56 313 participants in 2018 and 56 136 in 2019. The survey covers household residents, civilians living in housing on military bases, and individuals in noninstitutional group quarters (eg, shelters, rooming or boarding houses, college dormitories, migratory workers’ camps, and halfway houses). Homeless individuals, active-duty military personnel, and institutionalized individuals (eg, those in correctional facilities, nursing homes, mental institutions, and long-term care hospitals) are excluded.33
Assessments
SUDs in NSDUH are ascertained based on the DSM-IV definitions of 12-month substance abuse or dependence, implemented in a structured interview administered through computer-assisted self-interviewing. Using computer-assisted self-interviewing to ask questions about sensitive behaviors, such as substance use, has been shown to reduce reporting bias.33 The analyses focused on 4 groups of SUDs that could be identified in both NSDUH and Medicaid data: alcohol, cannabis (marijuana and hashish), opioid (heroin and prescription opioids), and stimulant (cocaine, methamphetamine, prescription stimulants) use disorders. Across the 2 survey years, 6753 participants (3390 in 2018 and 3363 in 2019) met criteria for alcohol use disorder, 3030 (1426 in 2018 and 1604 in 2019) for cannabis use disorder, 817 (448 in 2018 and 369 in 2019) for opioid use disorder, and 1104 (545 in 2018 and 559 in 2019) for stimulant use disorder.
In addition, in each SUD group, the proportion of participants who had Medicaid coverage and used SUD treatments were computed. These proportions were used as multipliers for computing the benchmark multiplier estimates.
The type of health insurance was ascertained using questions about each type of coverage. For participants younger than 18 years, type of health insurance was ascertained by asking the parent or guardian. Self-reports on public insurance have been shown to be accurate, with 91.4% to 92.7% of self-reports matching enrollment records.35
Treatments assessed in NSDUH included SUD treatment in a hospital, inpatient rehabilitation center, outpatient rehabilitation center, mental health center, physician’s office, or emergency department. Treatments received only in a self-help group or in a prison or jail setting were not counted for computing the multiplier because these treatments are typically not charged to insurance and would not be reflected in the Medicaid claims data (the benchmark). To assess the impact of this exclusion, in sensitivity analysis, benchmark multiplier estimates were computed based on all forms of SUD treatment, irrespective of insurance coverage.
Estimation
The benchmark multiplier method is based on estimating the size of a population using data from 2 samples from that population: a well-characterized sample of the population with known size (the benchmark) and a representative sample, typically based on a representative survey of the general population in which some individuals are also in the benchmark sample and the proportion of this latter group in the population of interest can be calculated (the multiplier). Given a benchmark of size N̂x and the probability π̂ for members of the representative sample to be in the benchmark, the size of the population (N̂y) can be estimated as N̂y =N̂x/π̂.
In this study, the population size to be estimated (N̂y) was the population of individuals with each SUD type in the US. For each SUD type, the N̂x was based on the count of Medicaid enrollees with that SUD and π̂ was the proportion of NSDUH participants with that SUD who had Medicaid and who used SUD treatment services. The benchmark and multiplier values for each type of SUD for each year and for the combined 2018 to 2019 period are presented in eTable 2 in the Supplement.
Bollaerts and colleagues26 note that even if N̂x and π̂ are unbiased, N̂y can be a biased estimator of N̂y because of its nonlinearity with respect to π̂. The authors proposed a bias-corrected version of N̂y computed as:
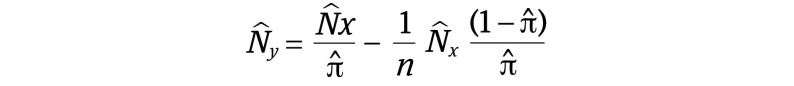 , ,
|
where n is the size of the representative sample used to estimate π̂. Furthermore, following Bollarets et al,26 π̂ was assumed to follow a β distribution, π̂ ~ β(x + 1, n − x + 1), where x is the number of individuals in the representative sample who are part of the benchmark (NSDUH participants within each SUD group who are covered by Medicaid and use SUD treatment services).
The N̂y =N̂x/π̂ for each SUD type was estimated using a separate Monte Carlo simulation model run 1000 times, and 95% CIs were estimated based on the percentiles of the 1000 simulated estimates. For comparison, the prevalence of SUDs was also estimated using the NSDUH data. Because both the benchmark and the multiplier were consistent across 2018 and 2019 (eTable 2 in the Supplement), they were combined for the main analyses to improve precision.
Producing unbiased estimates using the multiplier method is based on several assumptions. Importantly, it is assumed that the multiplier value based on the survey data are nationally representative—that is, in this case, the proportion of individuals with each type of SUD and Medicaid in the country who used SUD treatment services is the same as the proportion in NSDUH. However, it is plausible that survey participants had less severe forms of SUD and did not use SUD services as commonly as those who did not participate. It is also possible that individuals with SUDs who received SUD treatment would be more likely to endorse SUD criteria. Unfortunately, these possibilities could not be explored using available data. However, it is possible to explore the potential impact of these scenarios in sensitivity analyses. To this end, multipliers were computed for a range of SUD severity, including separately for cases meeting criteria for substance abuse (the less severe form of DSM-IV SUDs), assuming that NSDUH grossly oversamples individuals with severe SUDs who are also more likely to use SUD services, and for cases meeting substance dependence criteria (the more severe form of SUDs), assuming that NSDUH grossly oversamples individuals with less severe SUDs. These extreme scenarios were used to derive plausible ranges for prevalence estimates.
Survey weights and other survey elements were taken into account in calculation of NSDUH estimates. Furthermore, prevalence estimates from both the NSDUH and the benchmark multiplier method were multiplied by the US population 12 years and older to estimate the number of people with each SUD based on either method. Stata version 17.0 (StataCorp) was used for all analyses.
Results
This study included Medicaid beneficiaries 12 years and older accessing treatment services in the past year with diagnoses of alcohol (n = 1 017 308 in 2018; n = 1 041 357 in 2019), cannabis (n = 643 737; n = 644 780), opioid (n = 1 406 455; n = 1 575 219), and stimulant (n = 610 858; n = 657 305) use disorders and NSDUH participants with 12-month DSM-IV alcohol (n = 3390 in 2018; n = 3363 in 2019), cannabis (n = 1426; n = 1604), opioid (n = 448; n = 369), and stimulant (n = 545; n = 559) use disorders. The prevalence of alcohol, cannabis, opioid, and stimulant use disorders according to the multiplier method and NSDUH are presented in Table 1. For every SUD type, the benchmark multiplier method estimate was considerably larger than the NSDUH estimate in each year and in the combined 2018 to 2019 period: 2.2 times the NSDUH estimate for stimulant use disorder, 3.8 times for alcohol use disorder, 4.5 times for cannabis use disorder, and 5.1 times for opioid use disorder.
Table 1. Prevalence of Alcohol, Cannabis, Opioid, and Stimulant Use Disorders in the US Based on the Benchmark Multiplier Methoda and National Survey on Drug Use and Health (NSDUH) 2018-2019.
| Substance use disorder | % (95% CI) | |||||
|---|---|---|---|---|---|---|
| Combined 2018-2019 | 2018 | 2019 | ||||
| Multiplier method | NSDUH | Multiplier method | NSDUH | Multiplier method | NSDUH | |
| Alcohol use disorder | 20.27 (17.04-24.71) | 5.34 (5.10-5.58) | 18.99 (14.94-25.02) | 5.38 (5.11-5.66) | 21.84 (16.89-29.40) | 5.29 (4.98-5.63) |
| Cannabis use disorderb | 7.57 (5.96-9.98) | 1.68 (1.59-1.79) | 8.10 (5.70-12.29) | 1.62 (1.48-1.76) | 7.17 (5.21-10.40) | 1.75 (1.62-1.90) |
| Opioid use disorderc | 3.46 (2.97-4.12) | 0.68 (0.60-0.78) | 3.13 (2.56-3.96) | 0.75 (0.63-0.89) | 3.84 (3.04-5.04) | 0.62 (0.53-0.72) |
| Stimulants use disorderd | 1.91 (1.63-2.30) | 0.85 (0.75-0.96) | 2.13 (1.67-2.83) | 0.85 (0.74-0.98) | 1.74 (1.41-2.22) | 0.85 (0.72-1.00) |
The multiplier for the benchmark multiplier method was computed as the proportion of participants with substance use disorders in NSDUH who used treatments generally covered by insurance and were covered by Medicaid.
Includes marijuana and hashish.
Includes heroin and prescription opioids.
Includes cocaine, methamphetamine, and prescription stimulants.
The differences between the NSDUH and the benchmark multiplier method estimates translate into millions of individuals for each type of SUD (Table 2). For example, while the NSDUH estimate of the number of individuals with 12-month opioid use disorder in the US in 2018 to 2019 was less than 2 million, the benchmark multiplier method estimate was more than 9 million.
Table 2. Individuals With Alcohol, Cannabis, Opioid, and Stimulant Use Disorders in the US Based on the Benchmark Multiplier Methoda and National Survey on Drug Use and Health (NSDUH) 2018-2019b.
| Substance use disorder | No. in 1000s (95% CI) | |||||
|---|---|---|---|---|---|---|
| 2018-2019 | 2018 | 2019 | ||||
| Benchmark multiplier method | NSDUH | Benchmark multiplier method | NSDUH | Benchmark multiplier method | NSDUH | |
| Alcohol use disorder | 44 991 (38 502-53 611) | 14 906 (14 241-15 601) | 42 521 (34 376-54 286) | 14 978 (14 235-15 758) | 47 818 (38 176-62 005) | 14 834 (13 946-15 776) |
| Cannabis use disorderc | 17 494 (14 104-22 401) | 4705 (4429-4998) | 17 909 (13 080-25 830) | 4503 (4127-4912) | 17 209 (12 808-24 307) | 4908 (4533-5313) |
| Opioid use disorderd | 9450 (8141-11 241) | 1906 (1668-2178) | 8640 (7067-10 903) | 2080 (1747-2475) | 10 391 (8260-13 555) | 1732 (1478-2029) |
| Stimulant use disordere | 4773 (4110-5669) | 2376 (2103-2682) | 5663 (4463-7471) | 2379 (2070-2733) | 4168 (3435-5209) | 2372 (2016-2791) |
The multiplier for the benchmark multiplier method was computed as the proportion of participants with substance use disorders in NSDUH who used treatments generally covered by insurance and were covered by Medicaid.
Estimated counts were computed by multiplying the prevalence estimates from the benchmark multiplier method and NSDUH by the US population 12 years and older in 2018, 2019, and the mean of the 2018 and 2019 population.
Includes marijuana and hashish.
Includes heroin and prescription opioids.
Includes cocaine, methamphetamine, and prescription stimulants.
The differences between NSDUH prevalence estimates and benchmark multiplier method estimates persisted across a broad range of multiplier values for all SUDs (Figure). The plausible range for multipliers in these analyses was based on separate estimates of the multiplier value from cases meeting DSM-IV abuse and dependence criteria (eTable 3 in the Supplement). The upper limit of the plausible ranges of prevalence for alcohol and opioid use disorders were markedly higher than the benchmark multiplier estimates. This is because, compared with participants meeting dependence criteria with these substances, those meeting abuse criteria were much less likely to use SUD services.
Figure. 12-Month Prevalence Estimates for Substance Use Disorders in the US.
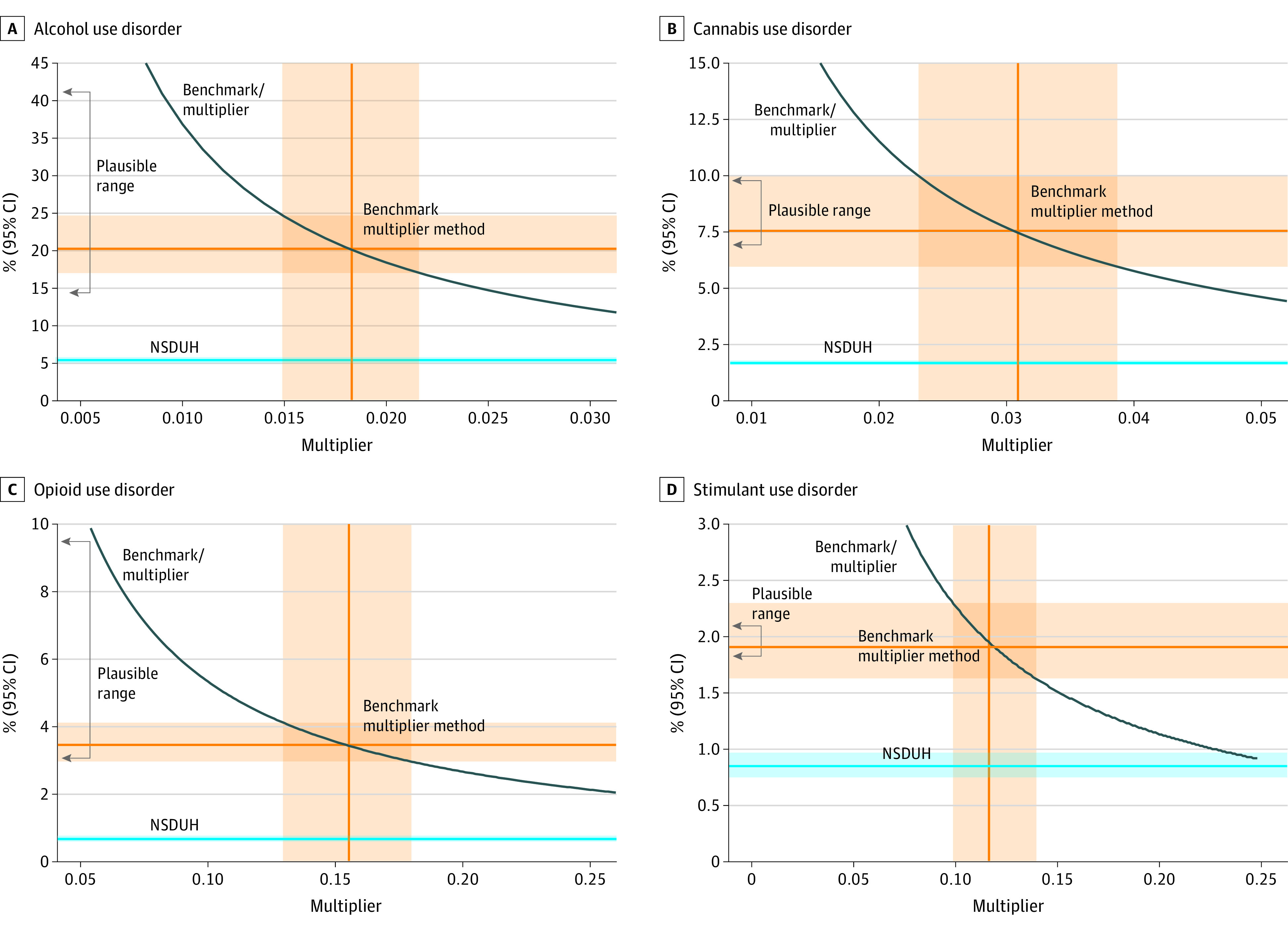
Plausible ranges for the benchmark multiplier method estimates were computed based on multiplier values for participants meeting DSM-IV substance dependence criteria (lower values) and for those meeting substance abuse criteria (upper values) for each SUD. NSDUH indicates National Survey on Drug Use and Health 2018-2019.
In sensitivity analyses in which SUD treatment service use was not limited to those typically covered by insurance, the benchmark multiplier estimates were expectedly somewhat lower due to the higher value of multipliers. Yet even in these analyses, the benchmark multiplier prevalence estimates remained markedly larger than the NSDUH estimates (eTables 4, 5, and 6 in the Supplement).
Discussion
Data based on the benchmark multiplier method used in this cross-sectional study suggest that SUDs were more common than previous estimates based on the NSDUH surveys suggested. The discrepancy between the benchmark multiplier method estimates and NSDUH was especially pronounced for opioid and cannabis use disorders. This study does not provide any information regarding the reasons for these variations in discrepancy between NSDUH and benchmark multiplier method estimates across SUD types. Opioid use disorders are especially common among marginalized population groups that are not adequately captured in general population surveys.8 Furthermore, opioid use disorder is highly stigmatized, which may lead to lower probability of endorsing opioid use disorder symptoms.8,36,37 In contrast, public attitudes have generally become more positive toward cannabis use over the years, in line with the decriminalization of cannabis.38
Over the years, a number of studies have provided evidence that NSDUH severely underestimates the prevalence of SUDs,6,10,18 though there are few recent national data to compare with the benchmark multiplier method estimates presented here. A study from Massachusetts17 using the capture-recapture method and multiple administrative data sources estimated the prevalence of opioid use disorders as 4.6% in 2015, almost 4 times larger than the NSDUH estimate for the state.
A number of factors likely contribute to the underestimation of SUDs in general population surveys, such as NSDUH, including selective nonresponse and reluctance to report stigmatized behaviors, such as drug use.16 Furthermore, general population surveys typically do not cover homeless and institutionalized individuals, who tend to have a higher prevalence of SUDs.8,39
The use of benchmark multiplier method partly addresses these limitations by capitalizing on service utilization data covered by Medicaid rather than participation in surveys. Medicaid is the major payer for SUD services in the US, especially among marginalized populations.40,41,42,43 The benchmark multiplier method is especially useful for capturing these population groups that are not well represented in surveys.25,27,28,44,45 Similar to the present study, many of the previous studies using the benchmark multiplier method capitalized on service use registries as benchmarks to estimate prevalence.46
While highlighting the limitations of NSDUH in adequately capturing SUDs in the population, this study underscores the utility of representative survey data when combined with other data sources. In conjunction with administrative data, representative population survey data are critical elements for building triangulated evidence regarding the national and local prevalence of SUDs.18,20
Limitations
In interpreting the results of this study, several limitations should be considered. Whereas the accuracy of SUD prevalence estimates based on general population surveys depends on the validity of self-reports of substance use in these surveys and adequate coverage of the population, the accuracy of estimates based on the benchmark multiplier method relies on representativeness of the multiplier values. A number of measures were taken to produce plausible values for the multipliers in this study. First, both the multiplier estimate and the benchmark were based on national data for the same years. Second, the multipliers were computed using the Monte Carlo method, thus accounting for uncertainly in these estimates given the limited sample sizes on which they were based. Third, sensitivity of prevalence estimates to variations in multiplier values obtained from SUD groups with different levels of severity were examined. Lastly, in addition to the combined estimates, separate estimates were computed for each year using benchmark and multiplier data for those years to examine consistency across the years. Nevertheless, the benchmark multiplier-derived prevalence estimates are sensitive to variations in multiplier values and future research with several multipliers would provide more confidence in the estimates.30
A further limitation is that the prevalence estimates could not be produced for different population subgroups. SUDs are not uniformly distributed across age, sex, racial, and ethnic groups and accurate prevalence estimates among different population groups are important for the design of prevention policies and planning of services. Similarly, benchmark multiplier prevalence estimates could not be computed for specific types of substances (eg, separately for individual stimulants) or for less commonly used substances (eg, inhalants and hallucinogens) because of lack of benchmark data for these drugs and smaller sample sizes for estimating the multiplier values for them.
Additionally, NSDUH 2018 to 2019 SUD diagnoses are based on DSM-IV criteria. US clinicians also typically base their diagnoses on DSM criteria. However, these diagnoses are coded using ICD-10 clinical codes. The effect of this discrepancy among the coded diagnoses and DSM-IV criteria could not be examined in this study. There is some indication that DSM-5 criteria that allow for mild disorders may be more sensitive to changes in prevalence of cannabis use disorder over time.19 Furthermore, upgrading the diagnoses from DSM-IV to DSM-5 diagnoses in NSDUH 2020 was associated with increased prevalence estimates for some SUDs compared to previous years.47 For example, the prevalence of cannabis use increased from 5.3% in NSDUH 2019 to 10.2% in NSDUH 2020 and the prevalence of alcohol use disorder increased from 4.3% to 10%.4,47 Changes for other SUDs were smaller. These numbers are closer to the benchmark multiplier estimates, but still fall short.
Conclusions
In the context of the limitations, these data provide an overview of the prevalence of SUDs in the US based on the benchmark multiplier method. The findings suggest a much larger burden of SUDs in the country than that estimated by NSDUH. The updated prevalence estimates of SUDs support greater investment in SUD prevention and treatment services and further efforts to make them more widely available.
eTable 1. SUD treatment setting and type among Medicaid-enrollees who received treatment for SUDs in 2018 and 2019 based on the Transformed Medicaid Statistical Information System (T-MSIS)
eTable 2. The benchmarks and multipliers for computing annual prevalence of alcohol, cannabis, opioid, and stimulant use disorders in the United States using the benchmark multiplier method. The multipliers were computed as the proportion of participants with substance use disorders in NSDUH 2018-2019 who used treatments typically covered by health insurance and who were covered by Medicaid
eTable 3. Multiplier estimates (+/- 95% confidence interval) among those with less severe (abuse) and more severe (dependence) SUDs in NSDUH 2018-2019 used to estimate a plausible range of prevalence estimates based on the benchmark multiplier method
eTable 4. The benchmarks and multipliers for computing annual prevalence of alcohol, cannabis, opioid, and stimulant use disorders in the United States using the benchmark multiplier method. The multipliers were computed as the proportion of participants with substance use disorders in NSDUH who used any treatments and were covered by Medicaid
eTable 5. Prevalence of alcohol, cannabis, opioid, and stimulant use disorders in the United States estimated based on the benchmark multiplier method and based on the NSDUH 2018-2019 survey. The multiplier for the benchmark multiplier method was computed as the proportion of participants with substance use disorders in NSDUH who used any treatments and were covered by Medicaid
eTable 6. Numbers (in 1,000s) of individuals with alcohol, cannabis, opioid, and stimulant use disorders in the United States estimated based on the benchmark multiplier method and based on the NSDUH 2018-2019 survey. The multiplier for the benchmark multiplier method was computed as the proportion of participants with substance use disorders in NSDUH who used any treatments and were covered by Medicaid
References
- 1.Lowry DE, Corsi DJ. Trends and correlates of cannabis use in Canada: a repeated cross-sectional analysis of national surveys from 2004 to 2017. CMAJ Open. 2020;8(3):E487-E495. doi: 10.9778/cmajo.20190229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Charles H, Heron J, Hickman M, Brown J, Hines L. Testing the validity of national drug surveys: comparison between a general population cohort and household surveys. Addiction. 2021;116(8):2076-2083. doi: 10.1111/add.15371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garnett C, Kastaun S, Brown J, Kotz D. Alcohol consumption and associations with sociodemographic and health-related characteristics in Germany: A population survey. Addict Behav. 2022;125:107159. doi: 10.1016/j.addbeh.2021.107159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Substance Abuse and Mental Health Services Administration . Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health. Accessed April 10, 2022. https://www.samhsa.gov/data/sites/default/files/reports/rpt29393/2019NSDUHFFRPDFWHTML/2019NSDUHFFR1PDFW090120.pdf
- 5.Substance Abuse and Mental Health Services Administration . Behavioral health barometer: United States, volume 6: indicators as measured through the 2019 National Survey on Drug Use and Health. Accessed April 10, 2022. https://www.samhsa.gov/data/sites/default/files/reports/rpt32815/National-BH-Barometer_Volume6.pdf [PubMed]
- 6.Homer JB. A system dynamic model of national cocaine prevalence. Syst Dyn Rev. 1993;9:49-78. doi: 10.1002/sdr.4260090104 [DOI] [Google Scholar]
- 7.Homer JB. Structure, data, and compelling conclusions: Notes from the field. Syst Dyn Rev. 1997;13:293-309. doi: [DOI] [Google Scholar]
- 8.Reuter P, Caulkins JP, Midgette G. Heroin use cannot be measured adequately with a general population survey. Addiction. 2021;116(10):2600-2609. doi: 10.1111/add.15458 [DOI] [PubMed] [Google Scholar]
- 9.Reardon ML, Burns AB, Preist R, Sachs-Ericsson N, Lang AR. Alcohol use and other psychiatric disorders in the formerly homeless and never homeless: prevalence, age of onset, comorbidity, temporal sequencing, and service utilization. Subst Use Misuse. 2003;38(3-6):601-644. doi: 10.1081/JA-120017387 [DOI] [PubMed] [Google Scholar]
- 10.Compton WM, Dawson D, Duffy SQ, Grant BF. The effect of inmate populations on estimates of DSM-IV alcohol and drug use disorders in the United States. Am J Psychiatry. 2010;167(4):473-474. doi: 10.1176/appi.ajp.2009.09081087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cottler LB, Zipp JF, Robins LN, Spitznagel EL. Difficult-to-recruit respondents and their effect on prevalence estimates in an epidemiologic survey. Am J Epidemiol. 1987;125(2):329-339. doi: 10.1093/oxfordjournals.aje.a114534 [DOI] [PubMed] [Google Scholar]
- 12.Weisner C, Schmidt L, Tam T. Assessing bias in community-based prevalence estimates: towards an unduplicated count of problem drinkers and drug users. Addiction. 1995;90(3):391-405. doi: 10.1111/j.1360-0443.1995.tb03786.x [DOI] [PubMed] [Google Scholar]
- 13.Midgette G, Caulkins JP, Reuter P. Pathways to drug prevalence estimation: synthesizing three comments on triangulation. Addiction. 2021;116(10):2615-2616. doi: 10.1111/add.15607 [DOI] [PubMed] [Google Scholar]
- 14.Ondersma SJ, Chang G, Blake-Lamb T, et al. Accuracy of five self-report screening instruments for substance use in pregnancy. Addiction. 2019;114(9):1683-1693. doi: 10.1111/add.14651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Psychiatric Association . American Psychiatric Association. DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. American Psychiatric Association; 2013. [Google Scholar]
- 16.Johnson TP. Sources of error in substance use prevalence surveys. Int Sch Res Notices. 2014;2014:923290. doi: 10.1155/2014/923290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barocas JA, White LF, Wang J, et al. Estimated prevalence of opioid use disorder in Massachusetts, 2011-2015: a capture-recapture analysis. Am J Public Health. 2018;108(12):1675-1681. doi: 10.2105/AJPH.2018.304673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hasin DS, Grant B. NESARC findings on increased prevalence of marijuana use disorders-consistent with other sources of information. JAMA Psychiatry. 2016;73(5):532. doi: 10.1001/jamapsychiatry.2015.3158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Compton WM, Han B, Jones CM, Blanco C. Cannabis use disorders among adults in the United States during a time of increasing use of cannabis. Drug Alcohol Depend. 2019;204:107468. doi: 10.1016/j.drugalcdep.2019.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Hasselt M. Data triangulation for substance abuse research. Addiction. 2021;116(10):2613-2615. doi: 10.1111/add.15596 [DOI] [PubMed] [Google Scholar]
- 21.Panel on Improving Federal Statistics for Policy and Social Science Research Using Multiple Data Sources and State-of-the-Art Estimation Methods NAoSEaMUS . Innovations in Federal Statistics: Combining Data Sources while Protecting Privacy. National Academies Press; 2017. [PubMed] [Google Scholar]
- 22.European Monitoring Centre for Drugs and Drug Addiction . Key epidemiological indicator: prevalence of problem drug use. Accessed April 10, 2022. https://www.emcdda.europa.eu/system/files/publications/321/Guidelines_Prevalence_Revision_280704_b-1_124620.pdf
- 23.Lohr SL, Raghunathan TE. Combining survey data with other data sources. Stat Sci. 2017;32(2):293-312. doi: 10.1214/16-STS584 [DOI] [Google Scholar]
- 24.McNeely J, Gourevitch MN, Paone D, Shah S, Wright S, Heller D. Estimating the prevalence of illicit opioid use in New York City using multiple data sources. BMC Public Health. 2012;12:443. doi: 10.1186/1471-2458-12-443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barrio Anta G, Oliva J, Bravo MJ, De Mateo S, Domingo-Salvany A, Itinere Working G. Estimating the prevalence of drug injection using a multiplier method based on a register of new HIV diagnoses. Eur J Public Health. 2011;21(5):646-648. doi: 10.1093/eurpub/ckq076 [DOI] [PubMed] [Google Scholar]
- 26.Bollaerts K, Aerts M, Sasse A. Improved benchmark-multiplier method to estimate the prevalence of ever-injecting drug use in Belgium, 2000-10. Arch Public Health. 2013;71(1):10. doi: 10.1186/0778-7367-71-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Comiskey CM, Snel A, Banka PS. First back-calculation and infection fatality multiplier estimate of the hidden prevalence of COVID-19 in Ireland. Eur J Public Health. 2021;31(4):908-912. doi: 10.1093/eurpub/ckab126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hiebert L, Azzeri A, Dahlui M, et al. Estimating the population size of people who inject drugs in Malaysia for 2014 and 2017 using the benchmark-multiplier method. Subst Use Misuse. 2020;55(6):871-877. doi: 10.1080/10826084.2019.1708943 [DOI] [PubMed] [Google Scholar]
- 29.Mojtabai R. Estimating the prevalence of schizophrenia in the United States using the multiplier method. Schizophr Res. 2021;230:48-49. doi: 10.1016/j.schres.2021.02.010 [DOI] [PubMed] [Google Scholar]
- 30.Mallow PJ, Sathe N, Topmiller M, Chubinski J, Carr D, Christopher R. Estimating the prevalence of opioid use disorder in the Cincinnati region using probabilistic multiplier methods and model averaging. J Health Econ Outcomes Res. 2019;6(2):61-69. doi: 10.36469/9729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.U.S. Department of Health and Human Services . Report to congress: T-MSIS substance use disorder (SUD) data book-treatment of SUD in Medicaid, 2018. Accessed February 21, 2022. https://www.medicaid.gov/medicaid/data-systems/downloads/2018-sud-data-book.pdf
- 32.U.S. Department of Health and Human Services . Report to congress: T-MSIS substance use disorder (SUD) data book-treatment of SUD in Medicaid, 2019. Accessed February 21, 2022. https://www.medicaid.gov/medicaid/data-systems/downloads/2019-sud-data-book.pdf
- 33.Center for Behavioral Health Statistics and Quality . 2019 National Survey on Drug Use and Health: methodological summary and definitions. Accessed April 5, 2022. https://www.samhsa.gov/data/report/2019-methodological-summary-and-definitions
- 34.The American Association for Public Opinion Research . Standard definitions: final dispositions of case codes and outcome rates for surveys. Accessed February 21, 2022. https://www.aapor.org/aapor_main/media/publications/standard-definitions20169theditionfinal.pdf
- 35.Pascale J, Call K, Fertig A, Ollerich D. Validating self-reported health insurance coverage: preliminary results on CPS and ACS. Accessed June 4, 2022. https://www.census.gov/newsroom/blogs/research-matters/2016/05/validating-self-reported-health-insurance-coverage-preliminary-results-on-cps-and-acs.html
- 36.Kaynak O, Whipple CR, Bonnevie E, et al. The opioid epidemic and the state of stigma: a Pennsylvania statewide survey. Subst Use Misuse. 2022;57(7):1120-1130. doi: 10.1080/10826084.2022.2064506 [DOI] [PubMed] [Google Scholar]
- 37.McCradden MD, Vasileva D, Orchanian-Cheff A, Buchman DZ. Ambiguous identities of drugs and people: a scoping review of opioid-related stigma. Int J Drug Policy. 2019;74:205-215. doi: 10.1016/j.drugpo.2019.10.005 [DOI] [PubMed] [Google Scholar]
- 38.Felson J, Adamczyk A, Thomas C. How and why have attitudes about cannabis legalization changed so much? Soc Sci Res. 2019;78:12-27. doi: 10.1016/j.ssresearch.2018.12.011 [DOI] [PubMed] [Google Scholar]
- 39.Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225. doi: 10.1371/journal.pmed.0050225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zur J, Mojtabai R. Medicaid expansion initiative in Massachusetts: enrollment among substance-abusing homeless adults. Am J Public Health. 2013;103(11):2007-2013. doi: 10.2105/AJPH.2013.301283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Parker RD, Cima MJ, Brown Z, Regier M. Expanded Medicaid provides access to substance use, mental health, and physician visits to homeless and precariously housed persons. J Community Health. 2018;43(2):207-211. doi: 10.1007/s10900-017-0405-9 [DOI] [PubMed] [Google Scholar]
- 42.Olfson M, Wall M, Barry CL, Mauro C, Feng T, Mojtabai R. Medicaid expansion and low-income adults with substance use disorders. J Behav Health Serv Res. 2021;48(3):477-486. doi: 10.1007/s11414-020-09738-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Olfson M, Wall MM, Barry CL, Mauro C, Feng T, Mojtabai R. A national survey of trends in health insurance coverage of low-income adults following Medicaid expansion. J Gen Intern Med. 2020;35(6):1911-1913. doi: 10.1007/s11606-019-05409-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jing L, Cui Y, Lu Q, Yu H. Multiplier method estimates of the population of men who have sex with men: the effect of privacy protection. J Public Health (Oxf). 2020;42(2):429-434. doi: 10.1093/pubmed/fdz019 [DOI] [PubMed] [Google Scholar]
- 45.Jing LW, Cui YH, Yu HM. Use of the multiplier method to estimate the size of populations most at risk of human immunodeficiency virus infection in China: a systematic review. Public Health. 2020;185:254-260. doi: 10.1016/j.puhe.2020.05.067 [DOI] [PubMed] [Google Scholar]
- 46.Johnston LG, Prybylski D, Raymond HF, Mirzazadeh A, Manopaiboon C, McFarland W. Incorporating the service multiplier method in respondent-driven sampling surveys to estimate the size of hidden and hard-to-reach populations: case studies from around the world. Sex Transm Dis. 2013;40(4):304-310. doi: 10.1097/OLQ.0b013e31827fd650 [DOI] [PubMed] [Google Scholar]
- 47.Substance Abuse and Mental Health Services Administration . Key substance use and mental health indicators in the United States: results from the 2020 National Survey on Drug Use and Health. Accessed February 21, 2022. https://www.samhsa.gov/data/sites/default/files/reports/rpt35325/NSDUHFFRPDFWHTMLFiles2020/2020NSDUHFFR1PDFW102121.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. SUD treatment setting and type among Medicaid-enrollees who received treatment for SUDs in 2018 and 2019 based on the Transformed Medicaid Statistical Information System (T-MSIS)
eTable 2. The benchmarks and multipliers for computing annual prevalence of alcohol, cannabis, opioid, and stimulant use disorders in the United States using the benchmark multiplier method. The multipliers were computed as the proportion of participants with substance use disorders in NSDUH 2018-2019 who used treatments typically covered by health insurance and who were covered by Medicaid
eTable 3. Multiplier estimates (+/- 95% confidence interval) among those with less severe (abuse) and more severe (dependence) SUDs in NSDUH 2018-2019 used to estimate a plausible range of prevalence estimates based on the benchmark multiplier method
eTable 4. The benchmarks and multipliers for computing annual prevalence of alcohol, cannabis, opioid, and stimulant use disorders in the United States using the benchmark multiplier method. The multipliers were computed as the proportion of participants with substance use disorders in NSDUH who used any treatments and were covered by Medicaid
eTable 5. Prevalence of alcohol, cannabis, opioid, and stimulant use disorders in the United States estimated based on the benchmark multiplier method and based on the NSDUH 2018-2019 survey. The multiplier for the benchmark multiplier method was computed as the proportion of participants with substance use disorders in NSDUH who used any treatments and were covered by Medicaid
eTable 6. Numbers (in 1,000s) of individuals with alcohol, cannabis, opioid, and stimulant use disorders in the United States estimated based on the benchmark multiplier method and based on the NSDUH 2018-2019 survey. The multiplier for the benchmark multiplier method was computed as the proportion of participants with substance use disorders in NSDUH who used any treatments and were covered by Medicaid


