Abstract
This cohort study evaluates the incidence of dermatomyositis and its trend over time in the US Department of Veterans Affairs health care system.
The incidence of dermatomyositis (DM) has been reported as stable or increasing within several countries throughout the world.1,2 In the US, the incidence of DM has been reported as being between 0.1 and 1.8 cases per 100 000 person-years,1 but the incidence trend is largely unknown. This study evaluates the incidence of DM and its trend over time in the US Department of Veterans Affairs (VA) health care system.
Methods
We conducted a retrospective cohort study of veterans with a diagnosis of DM in the outpatient VA health care system between January 1, 2005, and December 31, 2019. Patients were included (eFigure in the Supplement) if they had 2 International Classification of Diseases, Ninth Revision (ICD-9) or International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes for DM from VA dermatology or rheumatology outpatient encounters during the study period. To capture incident cases, we excluded patients without a VA health care system encounter in the year prior to DM diagnosis. The incidence of DM was calculated as the number of new cases of DM divided by the total number of veterans seen in the outpatient setting in each of the study years. Observed rates were adjusted for age and sex using direct standardization to 2010 US Census data. Trends in incidence rates over time were evaluated using Poisson regression, performed using R, version 4.0.5 (R Group for Statistical Computing). All P values were from 2-sided tests and results were deemed statistically significant at P < .05. This study was approved by the University of Utah institutional review board, which waived consent because this study involves the collection of historical and retrospective electronic medical record data. It would not be feasible to obtain consent from the entire study population (nearly 13 million individuals). If the study team were to attempt to obtain consent and authorization from each participant, participant refusals and/or failure to establish contact with participants due to incorrect, outdated, or incomplete contact information would create large gaps in sampling and diminish representativeness of the data.
Results
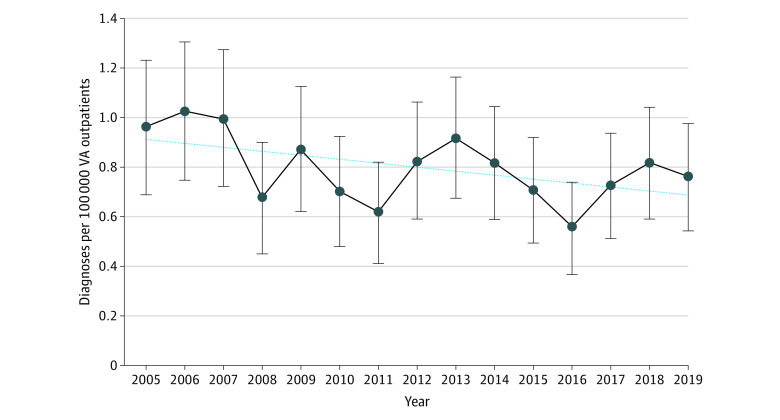
Among 12 991 999 individuals in the VA outpatient system, 1 825 082 had dermatology or rheumatology outpatient encounters during the study period (Table). We identified 679 individuals (82.2% men; median age, 60 years [IQR, 52-67 years]) with incident cases of DM during the study period. There was a higher percentage of women (17.5% vs 12.8%) and White patients (68.2% vs 63.5%) in the DM cohort compared with the general VA outpatient population. Most cases of DM were diagnosed when the patient was between 50 and 69 years of age (59.8%). The yearly incidence is shown in the Figure; the mean (SD) yearly incidence during the study was 0.8 (0.2) per 100 000 VA outpatients. The mean (SD) yearly incidence adjusted for age and sex was 1.0 (0.4) per 100 000 persons. The mean yearly incidence rate for DM among women during the study period was 1.4 (0.7) per 100 000 female VA outpatients. Poisson regression demonstrated a significant downward trend (point estimate, −0.019) in the incidence of DM during the study period (95% CI, −0.034 to −0.004; P = .01). In contrast, the incidence of DM among women showed a fractional upward trend (point estimate, 0.031) during the study period that was not statistically significant (95% CI, −0.027 to 0.089; P = .29).
Table. Demographic Characteristics for Patients With DM and All Dermatology and Rheumatology Outpatients Compared With All VA Outpatients.
| Characteristic | No. (%) | ||
|---|---|---|---|
| Patients with DM (n = 679) | VA dermatology and rheumatology outpatients (n = 1 825 082) | VA outpatients (N = 12 991 999) | |
| Sex | |||
| Male | 558 (82.2) | 1 654 561 (90.7) | 11 322 559 (87.2) |
| Female | 119 (17.5) | 170 521 (9.3) | 1 669 407 (12.8) |
| Racea | |||
| Asian | <10 | 14 096 (0.8) | 123 464 (1.0) |
| Black | 166 (24.4) | 283 477 (15.5) | 2 646 250 (20.4) |
| Hawaiian or Pacific Islander | <10 | 13 422 (0.7) | 100 675 (0.8) |
| Mixedb | <10 | 15 116 (0.8) | 90 278 (0.7) |
| Native American | <10 | 9968 (0.5) | 80 494 (0.6) |
| White | 463 (68.2) | 1 390 743 (76.2) | 8 245 382 (63.5) |
| Missing | 28 (4.1) | 98 260 (5.4) | 1 705 456 (13.1) |
| US Census region | |||
| South | 312 (45.9) | 772 072 (42.3) | 5 310 400 (40.9) |
| Midwest | 145 (21.4) | 374 139 (20.5) | 2 974 011 (22.9) |
| West | 135 (19.9) | 389 340 (21.3) | 2 770 381 (21.3) |
| Northeast | 82 (12.1) | 272 954 (15.0) | 1 808 067 (13.9) |
| Missing or outside the US | 5 (0.7) | 16 577 (0.9) | 129 140 (1.0) |
| Age, y | |||
| Median (IQR) | 60 (52-67) | 62 (53-70) | 57 (42-70) |
| 18-39 | 58 (8.5) | 190 182 (0.4) | 2 959 400 (22.8) |
| 40-49 | 87 (12.8) | 179 304 (9.8) | 1 669 324 (12.8) |
| 50-59 | 180 (26.5) | 383 239 (21.0) | 2 546 152 (19.6) |
| 60-69 | 226 (33.3) | 575 368 (31.5) | 2 565 309 (19.7) |
| 70-79 | 101 (14.9) | 314 242 (17.2) | 1 990 074 (15.3) |
| ≥80 | 27 (4.0) | 182 747 (10.) | 1 261 740 (9.7) |
| Facility type | |||
| VA medical center | 623 (91.8) | 1 636 698 (89.7) | 8 829 626 (68.0) |
| Community-based clinic | 23 (3.4) | 62 576 (3.4) | 2 917 091 (22.5) |
| Other | 33 (4.9) | 125 808 (6.9) | 1 245 282 (9.6) |
Abbreviations: DM, dermatomyositis; VA, Veterans Affairs.
Self-reported for most patients. If self-reported data were missing, then data were obtained from medical records.
Used if patient was identified as having 2 or more of the other races listed.
Figure. Incidence of Dermatomyositis in the Veterans Affairs (VA) Health Care System by Year From January 1, 2005, to December 31, 2019.
Vertical lines indicate 95% CIs.
Discussion
It is challenging to evaluate the incidence trend for a rare disease, such as DM, particularly in the US, given the lack of a unified medical record system. Of the few available studies, most demonstrate a stable incidence of DM, with the exception of a small cohort study from Olmsted County, Minnesota.3 A more recent study from Olmsted County demonstrated no change in incidence from 2009 to 2017 compared with the period from 1995 to 2007.4 There are more studies evaluating idiopathic inflammatory myopathies as a whole or evaluating polymyositis plus DM.1 All studies demonstrate an increasing incidence, but 1 study from Southern Australia showed that inclusion body myositis was associated with the apparent increase in idiopathic inflammatory myopathies.5 Our study suggests that DM incidence is not increasing among the VA population.
Our study has some limitations, including a lack of external generalizability to the US population, given that the VA health care system has an older, male-predominant population. However, when adjusted for age and sex, the mean yearly incidence for DM in our study was similar to previous reports.1 The use of ICD-9 or ICD-10 coding to identify patients with DM has its limitations. Kronzer et al4 reported a positive predictive value of 49% for 2 DM ICD-9 or ICD-10 codes when using EULAR/ACR (European Alliance of Associations for Rheumatology/American College of Rheumatology) 2017 diagnostic criteria. This suggests that ICD-9 and ICD-10 coding alone is not precise in identifying DM cases. We attempted to mitigate this issue by requiring codes from subspecialty clinics only. If the true positive predictive value of DM ICD-9 and ICD-10 codes is low, then our incidence may be falsely inflated. To our knowledge, this is the only nationwide study specifically evaluating the incidence trend of DM in the US.
eFigure. VA Incident Dermatomyositis Cohort Attrition
References
- 1.Meyer A, Meyer N, Schaeffer M, Gottenberg JE, Geny B, Sibilia J. Incidence and prevalence of inflammatory myopathies: a systematic review. Rheumatology (Oxford). 2015;54(1):50-63. doi: 10.1093/rheumatology/keu289 [DOI] [PubMed] [Google Scholar]
- 2.Cho SK, Kim H, Myung J, et al. Incidence and prevalence of idiopathic inflammatory myopathies in Korea: a nationwide population-based study. J Korean Med Sci. 2019;34(8):e55. doi: 10.3346/jkms.2019.34.e55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bendewald MJ, Wetter DA, Li X, Davis MD. Incidence of dermatomyositis and clinically amyopathic dermatomyositis: a population-based study in Olmsted County, Minnesota. Arch Dermatol. 2010;146(1):26-30. doi: 10.1001/archdermatol.2009.328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kronzer VL, Kimbrough BA, Crowson CS, Davis JM III, Holmqvist M, Ernste FC. Incidence, prevalence, and mortality of dermatomyositis: a population-based cohort study. Arthritis Care Res (Hoboken). Published online September 21, 2021. doi: 10.1002/acr.24786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tan JA, Roberts-Thomson PJ, Blumbergs P, Hakendorf P, Cox SR, Limaye V. Incidence and prevalence of idiopathic inflammatory myopathies in South Australia: a 30-year epidemiologic study of histology-proven cases. Int J Rheum Dis. 2013;16(3):331-338. doi: 10.1111/j.1756-185X.2011.01669.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. VA Incident Dermatomyositis Cohort Attrition