Abstract
To the best of our knowledge, there are no useful screening methods for early detection of endometrial cancer in asymptomatic individuals. The present study evaluated the usefulness of genetic analysis of liquid-based cytology (LBC) specimens by assessing whether pathological genetic mutations detected in cancer tissue sections were detected in LBC specimens from the cervix and uterus. The primary endpoint was genetic analysis of cervical cytology specimens and LBC for the detection of endometrial cancer. Endometrial thickening (>11 mm) assessed using transvaginal ultrasonography was present in 60% of cases and adenocarcinoma assessed using cervical cytology was present in 50% of cases. In 70% of cases, pathogenic mutations detected in cancer tissue sections were also detected in cervical and/or endometrial LBC specimens. The pathogenic variants identified were PTEN in four cases, tumor protein P53, PI3K catalytic subunit α and fibroblast growth factor receptor 2 in two cases each and APC regulator of WNT signaling pathway, KRAS and catenin β1 in one case each. In the present study, a combination of endometrial thickening assessed by transvaginal ultrasonography, cervical cytology and genetic analysis resulted in a high sensitivity of 90% for detection of endometrial cancer. The combination of these tests is more expensive than conventional methods, but delayed detection of uterine cancer requires multidisciplinary treatment, which increases healthcare costs. Increased spending on early detection of uterine cancer is better economically and may improve patient quality of life.
Keywords: cervical cytology, liquid-based cytology, endometrial cancer, next-generation sequencing
Introduction
In 2020, 417,367 novel cases of endometrial cancer were diagnosed worldwide, with a cumulative risk of 1.6% (1). In Japan, 17,089 new cases of endometrial cancer were diagnosed in 2018 and 2,597 deaths associated with endometrial cancer were reported in 2019 (2).
Risk factors for uterine cancer include high estrogen levels (due to obesity, diabetes and high-fat diet), menarche at a young age, non-menarche, menopause at an older age, Lynch syndrome, older age (>55 years) and use of tamoxifen (3). The incidence of uterine cancer is increasing owing to increased life expectancy and obesity (3). The medical cost of uterine cancer is increasing year on year and early detection is important for the associated medical economic effects (3,4).
To the best of our knowledge, there are currently no useful screening methods for early detection of uterine cancer in asymptomatic individuals based on European Society for Medical Oncology (ESMO) and National Comprehensive Cancer Network (NCCN) guidelines (3,5). According to the Japanese guidelines, uterine cancer may be suspected in women with irregular vaginal bleeding and endometrial thickening ≥20 mm or ≥5 mm on transvaginal ultrasonography before or after menopause, respectively (6). The ESMO guidelines state that endometrial thickening >11 mm on transvaginal ultrasonography should be managed on a case-by-case basis (5).
Endometrial carcinoma is classified as either type I, which is estrogen-dependent, or type II, which is estrogen-independent. Type I is a histological type of endometrioid carcinoma with a clinical background of obesity and dyslipidemia and typically develops following emergence of precancerous lesions, such as endometrial hyperplasia. Type II adenocarcinoma is caused by mismatch repair gene abnormality and multistep carcinogenesis, characterized by mutations in KRAS and PTEN genes. Moreover, type II endometrial cancer can be of multiple unique histological types, including serous and clear cell carcinoma, and are associated with a poor prognosis. Overexpression of human epidermal growth factor receptor-2/neu and mutations in tumor protein P53 (TP53) gene are carcinogenesis-associated factors (7). In an integrated analysis of endometrial carcinoma in The Cancer Genome Atlas (TCGA) database, four novel categories were proposed as follows: i) Ultra-mutated polymerase ε (POLE); ii) hypermutated microsatellite instability; iii) low copy number (endometrioid) and iv) high copy number (serous-like) (7). Furthermore, endometrial carcinoma is divided into four molecular subtypes according to the World Health Organization (WHO) classification system as follows: i) POLE-ultra-mutated; ii) mismatch repair-deficient and iii) p53-mutant endometrioid carcinoma and iv) no specific molecular profile (8). The molecular features of WHO classification subgroups correspond to those of the TCGA genomic classification system (8).
Identification of biomarkers based on molecular genetic characteristics may contribute to elucidation of mechanisms of uterine carcinogenesis and development of methods for early diagnosis. Notably, Matsuura et al (9) reported that the diagnostic yield of uterine cancer may be improved by combining endometrial cytology with next-generation sequencing (NGS) analysis of liquefied endometrial cytology specimens: The sensitivity was reported as 88.5%, however there were numerous false-positive cases (25.2%). The diagnostic criteria and specimen standardization are insufficient for early detection of endometrial cancer (5,9). Furthermore, endometrial cytology is not currently included in ESMO or NCCN guidelines (3,4). In Japan, endometrial cytology is routinely used to test for uterine cancer (10). Moreover, it has been recognized worldwide that cervical cytology is a useful tool for the prevention and early detection of cervical cancer (11). Endometrial cytology can be painful and cannot be performed if the cervix is narrow. The detection sensitivity of cervical cytology for uterine cancer is ~45% (12). Therefore, it was hypothesized that an approach combining cervical cytology and NGS analysis of cervical liquid-based cytology (LBC) samples for detection of tumor cells migrating to the cervix may improve diagnostic rate. Therefore, the sensitivity of cervical cytology combined with NGS analysis of cervical LBC specimens for early detection of uterine cancer was evaluated.
Patients and methods
Patients and clinical information
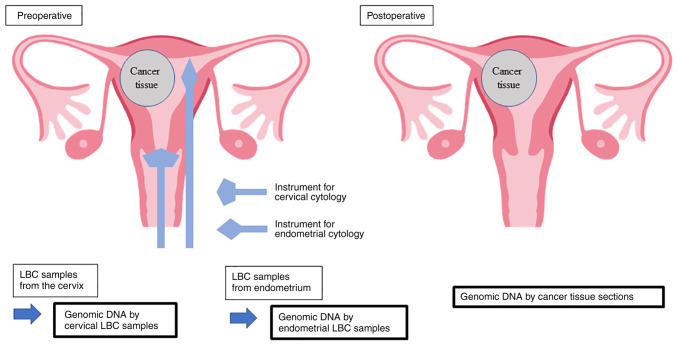
The present study was approved by the institutional review board of Mie University Hospital (approval no. H2020-075) and performed according to the ethical standards of The Declaration of Helsinki, revised in 2001. A total of 30 female patients diagnosed with endometrial cancer from October 2019 to November 2020 at the Department of Obstetrics and Gynecology, Mie University Hospital, was included. The median age of patients was 55.7 years (range, 36–74 years). Written informed consent was obtained from all patients. A schematic representation of the present study is presented in Fig. 1. LBC specimens of the uterine cervix and endometrium were collected prior to surgery. They were processed using SurePath kits (Becton-Dickinson and Company) according to manufacture's protocol, and cytologically diagnosed using light microscopy after Papanicolaou staining (Leica Autostainer XL; Leica Biosystems Nussloch GmbH). Briefly, samples underwent fixation with 100% ethanol for 10 min, 70% ethanol for 40 sec, 50% ethanol for 60 sec, rinse in tap water, Gill hematoxylin for 100 sec, rinse in tap water, 70% ethanol with 0.5% hydrochloric acid for 30 sec, rinse in tap water, 70% ethanol for 50 sec, 95% ethanol for 60 sec, OG-6 for 3 min, 95% ethanol for 60 sec twice, EA-50 for 4 min, 95% ethanol for 55 sec, 100% ethanol for 30 sec ×3 times then 60 sec, Hemo-De® (a xylene substitute for low-toxicity, Falma Inc.) for 5 min ×4 times, all processes were performed at room temperature. Surgically resected organs were fixed in 10% buffered formalin at room temperature for 24 to 48 h, the tissue specimens were formalin-fixed and paraffin-embedded by automated tissue processor (Tissue-Tek® VIP6; Sakura Finetek Japan Co., Ltd.). FFPE specimens were thin sectioned at 4 µm, stained with hematoxylin and eosin with autostainer (Leica Autostainer XL) as follows; Clear Plus (a xylene substitute for low-toxicity; Falma Inc.) for 5 min ×3 times, 100% ethanol for 3 min ×3 times, rinse in tap water, distilled water for 2 min, Mayer hematoxylin for 7 min, rinse in tap water, wash in warm tap water for 3 min, 100% ethanol for 60 sec, eosin Y for 5 min, 100% ethanol for 30 sec ×2 times, 2 min ×1, 4 min ×1, then Clear Plus for 5 min ×3 times, all processes were performed at room temperature except for warm tap water. Tissue slides were pathologically examined under light microscopy. Furthermore, endometrial thickness on transvaginal ultrasonography (6 MHz) was measured to investigate the sensitivity and specificity of primary screening.
Figure 1.
Schematic representation of the present study. In cases of endometrial cancer, LBC specimens from the cervix and endometrium were assessed to determine if pathological genetic mutations detected in cancer tissue samples could also be detected in LBC specimens. Image adapted from Free Graphic Design Software: kango-roo.com/ki/image_289/. LBC, liquid-based cytology.
The primary endpoint was genetic analysis of the cervical cytology specimens and LBC for detection of endometrial cancer. The secondary endpoints were concordance rates of gene mutations in cervical and endometrial cytology and surgically removed cancer tissue sections. The median age of patients with endometrial thickness ≥11 and <11 mm and cervical cytology test results were compared using Mood's median test. The reproducibility of endometrial thickening by transvaginal ultrasonography, cervical cytology and genetic analysis were assessed using Cohen's κ coefficient.
Statistical analysis
Student's unpaired t-test and Mood's median test were used for comparison between endometrial thickness and cervical cytology test results and age. Data are presented as the mean ± SD. All statistical tests were performed using SPSS (version 27.0; IBM Corp.). P<0.05 was considered to indicate a statistically significant difference.
DNA extraction from formalin-fixed paraffin-embedded (FFPE) samples and LBC specimens
FFPE tissue blocks were serially sectioned at 10 µm thickness. Mucosal endometrial tissue was micro-dissected and genomic DNA was extracted using the QIAmp DNA FFPE Tissue kit (Qiagen, Inc.) according to the manufacturer's protocol. Genomic DNA was extracted from LBC and paraffin-embedded surgical tissue samples using QIAmp DNA Mini kits (Qiagen, Inc.), according to the manufacturer's protocol. The quality and quantity of each DNA sample were assessed using Qubit® dsDNA (Thermo Fisher Scientific, Inc.), according to the manufacturer's protocol.
Next-generation sequencing (NGS) of 50 cancer-associated genes
NGS of genomic DNA from each sample was performed using the Ion Ampliseq™ Cancer Hotspot Panel v2 (cat. no. 4475346; Thermo Fisher Scientific, Inc.), which covers ~2,800 mutational hotspot regions from 50 cancer-associated genes, as previously described (13–15). Endometrioid carcinoma is preferentially associated with mutations in PTEN, KRAS, AT-rich interaction domain 1A (ARID1A), catenin β1 (CTNNB1) and PI3K catalytic subunit α (PIK3CA) as well as microsatellite instability, whereas serous (non-endometrioid, type II) carcinoma exhibits HER2 amplification and TP53 and PPP2R1A mutations (16), which were assessed in the present study. Briefly, 10 ng genomic DNA extracted from FFPE or LBC specimens was used to construct barcoded DNA libraries utilizing an Ion Ampliseq Library kit Plus (cat. no. A38875; Thermo Fisher Scientific, Inc.). The obtained libraries were purified using AMPure XP Reagent (Beckman Coulter, Inc.) and sequenced using an Ion Personal Genome Machine® or Ion GeneStudio™ S5 platform (Thermo Fisher Scientific, Inc.). Sequencing nucleotide is single end. Sequence kit names are Ion PGM Hi-Q View Chef Kit (A30798) and Ion 510™ & Ion 520™ & Ion 530™ Kit-Chef (A34461). The loading concentration of the library is 25 pM. The sequencing reads were aligned to the reference genome GRCh37 and converted into binary alignment and map files using Torrent Suite 5.12.3 Software (Thermo Fisher Scientific, Inc.). Sequence variants were called using Ion Reporter™ 5.12 (Thermo Fisher Scientific, Inc.), according to the manufacturer's protocols. The mean read depth of coverage in DNA sequencing was >1,500-fold.
Classification of oncogenic mutations
Somatic mutations were called based on all criteria as follows: i) Variant allele frequency of somatic mutations in tumor tissue >5%; ii) variant allele frequency of somatic mutations in LBC >0.1% and iii) registration of mutations as ‘pathogenic/likely pathogenic variants’ in the ClinVar database (https://www.ncbi.nlm.nih.gov/clinvar/).
Results
Background and clinical characteristics
Patient background and clinical characteristics are presented in Table I. The mean age of patients was 58.1±8.92 years (range, 45–74 years) and the mean body mass index (BMI) was 24.2±8.12 kg/m2 (range, 18–47 kg/m2). Obesity is a risk factor for uterine cancer; one of the ten patients was considered to be obese (BMI ≥30) (3). The mean endometrial thickness was 13.6±8.92 mm (range, 4–22 mm). A total of seven of ten patients were postmenopausal and six of ten patients presented with endometrial thickness of ≥11 mm. The age of patients with endometrial thickness ≥11 mm (56.70±8.80 years) and <11 mm (60.25±8.67 years) were not significantly different. Cervical cytology demonstrated adenocarcinoma in five of ten patients. Age of patients in adenocarcinoma and negative for intraepithelial lesion or malignancy (NILM) groups as assessed using cervical cytology was not significantly.
Table I.
Patient background and clinical characteristics.
| Case | Age, years | Number of births | BMI | Menopausal status | Endometrium thickness, mm | Cervical cytology |
|---|---|---|---|---|---|---|
| 1 | 45 | 0 | 29 | Premenopausal | 21 | NILM |
| 2 | 50 | 0 | 21 | Premenopausal | 9 | NILM |
| 3 | 59 | 3 | 20 | Postmenopausal | 6 | Adenocarcinoma |
| 4 | 51 | 2 | 47 | Premenopausal | 20 | NILM |
| 5 | 58 | 2 | 24 | Postmenopausal | 4 | NILM |
| 6 | 71 | 2 | 20 | Postmenopausal | 13 | Adenocarcinoma |
| 7 | 52 | 2 | 18 | Postmenopausal | 11 | Adenocarcinoma |
| 8 | 65 | 0 | 20 | Postmenopausal | 21 | Adenocarcinoma |
| 9 | 56 | 1 | 22 | Postmenopausal | 22 | NILM |
| 10 | 74 | 2 | 21 | Postmenopausal | 9 | Adenocarcinoma |
BMI, body mass index; NILM, negative for intraepithelial lesion or malignancy.
Cytology and genetic analysis
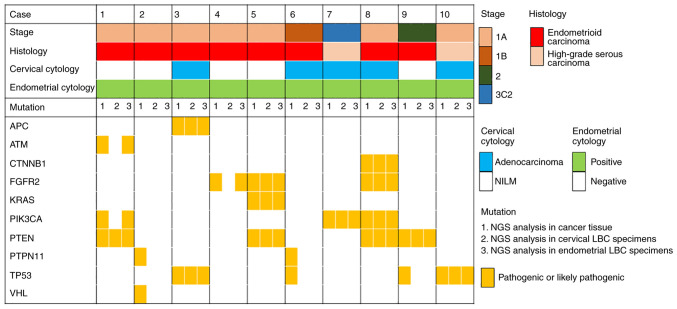
The pathogenic variants detected in cancer tissue sections and cervical and endometrial LBC specimens are presented in Fig. 2. A total of eight of the ten cases was assessed to be endometrioid and two were serous carcinoma. Histopathological examination demonstrated no double cervical cancer cases. In seven of ten cases, pathogenic variants detected in cancer tissue sections were also detected in cervical and/or endometrial LBC specimens. Variants detected in ≥2 types of sample are presented in Table II. Pathogenic variants were called in PTEN in four cases, TP53, PIK3CA and fibroblast growth factor receptor 2 (FGFR2) in two cases each and APC regulator of WNT signaling pathway (APC), KRAS and CTNNB1 in one case each.
Figure 2.
Pathogenic variants detected in cancer tissue and cervical and endometrial LBC specimens and association with World Health Organization stage classification, histology, cervical cytology and endometrial cytology. LBC, liquid-based cytology; NILM, negative for intraepithelial lesion or malignancy; NGS, next-generation sequencing; APC, APC regulator of WNT signaling pathway; ATM, ATM serine/threonine kinase; CTNNB1, catenin β1; FGFR2, fibroblast growth factor receptor 2; PIK3CA, PI3K catalytic subunit α; PTPN11, protein tyrosine phosphatase non-receptor type 11; TP53, tumor protein P53; VHL, Von Hippel-Lindau tumor suppressor.
Table II.
Variants detected in ≥2 sample types from cancer tissue sections and cervical and endometrial liquid-based cytology specimens.
| Gene | Variant | Classification | Case |
|---|---|---|---|
| PTEN | c.388C>G (p.Arg130Gly) | Pathogenic | 1 |
| c.518G>A (p.Arg173His) | Pathogenic | 5 | |
| c.697C>T (p.Arg233Ter) | Pathogenic | 5 | |
| c.388C>G (p.Arg130Gly) | Pathogenic | 8 | |
| c.209+5G>A | Pathogenic | 9 | |
| TP53 | c.818G>T (p.Arg273Leu) | Pathogenic | 3 |
| c.818G>A (p.Arg273His) | Pathogenic | 10 | |
| PIK3CA | c.1357G>A (p.Glu453Lys) | Likely pathogenic | 7 |
| c.1053T>A (p.Asn345Lys) | Likely pathogenic | 8 | |
| FGFR2 | c.758C>G (p.Pro253Arg) | Pathogenic | 5 |
| c.755C>G (p.Ser252Trp) | Pathogenic | 8 | |
| APC | c.4671delT (p.lle1557MetfsTer8) | Pathogenic | 3 |
| KRAS | c.175G>A (p.Ala59Thr) | Pathogenic | 5 |
| CTNNB1 | c.110C>T (p.Ser37Phe) | Pathogenic | 8 |
APC, APC regulator of WNT signaling pathway; CTNNB1, catenin β1; FGFR2, fibroblast growth factor receptor 2; PIK3CA, PI3K catalytic subunit α; TP53, tumor protein P53.
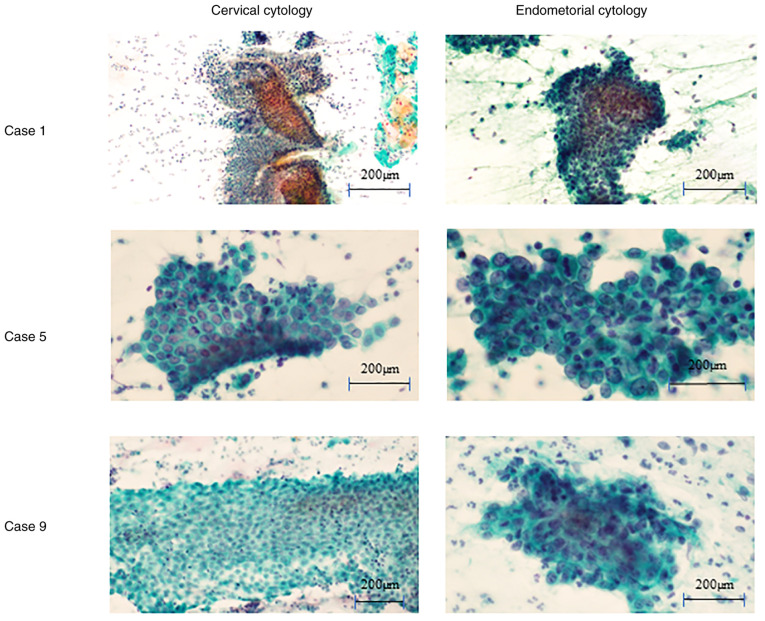
LBC specimens were obtained from the cervix and endometrium before surgery in patients with pre-operatively diagnosed endometrial cancer. A total of three of seven cases with pathogenic variants detected in ≥2 types of sample were negative for intraepithelial lesions (NILM) or malignancy using cervical cytology (cervical and endometrial cytology is presented in Fig. 3). Case 1 demonstrated no endometrial cells using cervical cytology. Cases 5 and 9 demonstrated benign endometrial cells using cervical cytology. The sheet patterns were accompanied by stromal cells and nuclear overlapping was limited to <3 layers. All ten cases demonstrated malignant endometrial cells using endometrial cytology. Notable nuclear overlapping was observed in the cluster and nuclei demonstrated enlarged and varied shapes. In eight of ten cases, pathogenic variants detected in cancer tissue sections were also detected in endometrial LBC specimens. Detected pathogenic variants were PTEN in four cases, FGFR2 in three cases, TP53 and PIK3CA in two cases each and APC, KRAS and CTNNB1 in one case each.
Figure 3.
Papanicolaou-stained cervical and endometrial cytology of cases with matching pathogenic variants exhibited negative for intraepithelial lesion or malignancy cervical cytology. Case 1 demonstrated no endometrial cells using cervical cytology. Cases 5 and 9 demonstrated benign endometrial cells using cervical cytology. Malignant endometrial cells using endometrial cytology were observed in all ten cases.
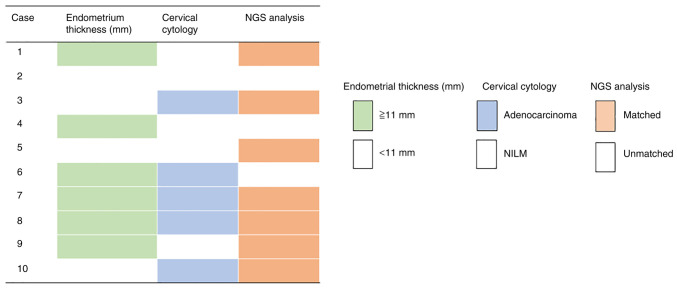
Sensitivity of the combination of tests
Endometrial thickening (>11 mm) on transvaginal ultrasonography was present in 60% of cases and adenocarcinoma on cervical cytology was present in 50% of cases. The concordance of cervical LBC specimen and genetic analysis results was 70%. Furthermore, combined cervical cytology and genetic analysis showed a sensitivity of 80%, whereas combined endometrial thickening assessed using transvaginal ultrasonography, cervical cytology and genetic analysis had a sensitivity of 90% (Fig. 4).
Figure 4.
Summarised results of endometrial thickening, cervical cytology and genetic analysis. NILM, negative for intraepithelial lesion or malignancy; NGS, next-generation sequencing.
The reproducibility of endometrial thickening assessment using transvaginal ultrasonography, cervical cytology and genetic analysis was analyzed using Cohen's κ coefficient (Table III). All tests had a reproducibility of ≤0.2, which indicated that each test may be used independently to diagnose endometrial cancer. These tests may be considered to be an effective combination.
Table III.
Cohen's κ coefficient for endometrial thickening using transvaginal ultrasonography, cervical cytology and genetic analysis.
| Test | κ coefficient | P-value |
|---|---|---|
| Transvaginal ultrasonography-cervical cytology | 0.000 | 1.000 |
| Transvaginal ultrasonography-genetic analysis | 0.097 | 0.778 |
| Cervical cytology-genetic analysis | 0.200 | 0.490 |
Discussion
NCCN guidelines recommend endometrial biopsy for the diagnosis of endometrial cancer, which has a sensitivity of 90% and a false-negative rate of 10% (3). In the present study, the combination of assessment of endometrial thickening using transvaginal ultrasonography, cervical cytology and genetic analysis demonstrated a sensitivity of 90%, which was equivalent to that of endometrial biopsy. Furthermore, comparable sensitivity to endometrial biopsy was achieved by combining these three minimally invasive tests, indicating that this method may alleviate the need for highly invasive endometrial biopsy. Methods of testing for uterine cancer include blood sampling (tumor marker), CT and MRI; however, it can be difficult to perform these tests on the same day. However, it is not difficult to perform transvaginal ultrasonography, cervical cytology and genetic analysis in the same day. Matsuura et al (9) reported the use of endometrial cytology to test for uterine cancer, however endometrial cytology is not used worldwide. By contrast, cervical cytology is used worldwide, has excellent versatility and is convenient (3). Certain pathogenic variants were not detected compared with endometrial cytology, however most pathogenic variants were identified by cervical cytology in the present study. Furthermore, if TCGA categories can be determined pre-operatively following early diagnosis using NGS analysis, prognosis could be estimated before treatment and choice of treatment strategy could be more effective, such as deciding whether a more aggressive surgical approach is necessary, whether referral to a high-volume center should be considered and how long the patient can wait until starting treatment (7).
In three cases (cases 2, 4 and 6), pathological gene mutations detected in cancer tissue sections were not be detected in LBC specimens from the cervix. In case 6, the cervical cytology was adenocarcinoma and endometrial cells with malignant findings were demonstrated using cervical cytology, however no pathological genetic mutations were detected. In case 2 and 4, the cervical cytology was NILM and endometrial cells were not demonstrated using cervical cytology.
There were certain limitations to the present study. First, the sensitivity of cervical cytology for detecting uterine cancer was only 45%. Furthermore, the present approach requires multiple tests to be combined to achieve high sensitivity. Therefore, future studies are required to increase sample size, establish early screening methods for uterine cancer and plan treatment strategies using NGS data before treatment. A further limitation of the present study was that no healthy subjects were assessed. It would have been desirable to assess the specificity and false-positive and -negative rates by including normal cases or to evaluate only Stage 1A cases. However, owing to lack of funding, it was decided to conduct a balanced analysis of advanced stages and histological types using these 10 cases to assess the usefulness of the present method. In the present study, 30 endometrial cancer cases were diagnosed; 25 cases were stage I, one was stage II and four were stage III. The histological types were endometrial carcinoma in 26 cases and serous carcinoma in 4 cases. A total of 10 cases were selected for inclusion in the present study. Furthermore, the present study was performed to detect specific somatic variants for each patient. The specificity was assessed to be high. To the best of our knowledge, however, an optimal endometroid cancer biomarker has not yet been widely reported; therefore, further studies are needed, including a broader panel and a panel that includes not only the genome but also the epigenome.
In the present study, the combination of the assessment of endometrial thickening using transvaginal ultrasonography, cervical cytology and genetic analysis resulted in a high sensitivity of 90% for the detection of endometrial cancer. The three tests reported here are more expensive than conventional diagnosis methods; however, delayed detection of uterine cancer requires multidisciplinary treatment, which increases healthcare costs. Increased spending on early detection of uterine cancer is better economically and may improve patient quality of life.
Acknowledgements
Not applicable.
Glossary
Abbreviation
- LBC
liquid-based cytology
Funding Statement
Funding: No funding was received.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the SAMD00511249-SAMD00511278 repository, ddbj.nig.ac.jp/search.
Authors' contributions
EK, RN and YO conceptualized the study. RN, EK, KY, MKK, MNi, MI, MNa, HI, YO, KN and TI performed experiments and collected data. EK, KY and HI analyzed data. MI and MNa performed NGS. KN designed the study methodology. MNi and MKK performed study administration. EK provided software. KN supervised the study. EK and KY validated the results. TI produced visualization. RN and EK wrote the first draft. EK and MI confirm the authenticity of all the raw data. All authors reviewed and edited the manuscript. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
The present study was approved by the institutional review board of Mie University Hospital (approval no. H2020-075). Written informed consent was obtained from all patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Bray F, Colombet M, Mery L, Piñeros M, Znaor A, Zanetti R, Ferlay J, editors. International Agency for Research on Cancer Lyon; 2017. 2021. Cancer incidence in five continents, Vol XI (electronic version) Available from: Accessed November 14. [Google Scholar]
- 2.National Cancer Center Japan, Cancer Statistics, endometrial cancer, corp-author. https://ganjoho.jp/reg_stat/statistics/stat/cancer/18_corpus_uteri.html. [ April 20; 2022 ]; Available from. [Google Scholar]
- 3.National Comprehensive Cancer Network [NCCN guidelines], corp-author Cervical cancer version 1.2021, 2021. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1426. [ November 14; 2021 ]; Available from. [Google Scholar]
- 4.Kosa SD, Ferguson SE, Panzarella T, Lau S, Abitbol J, Samouëlian V, Giede C, Steed H, Renkosinski B, Gien LT, Bernardini MQ. A prospective comparison of costs between robotics, laparoscopy, and laparotomy in endometrial cancer among women with class III obesity or higher. J Surg Oncol. 2022;125:747–753. doi: 10.1002/jso.26769. [DOI] [PubMed] [Google Scholar]
- 5.Colombo N, Creutzberg C, Amant F, Bosse T, González-Martín A, Ledermann J, Marth C, Nout R, Querleu D, Mirza MR, et al. ESMO-ESGO-ESTRO consensus conference on endometrial cancer: Diagnosis, treatment and follow-up. Int J Gynecol Cancer. 2016;26:2–30. doi: 10.1097/IGC.0000000000000609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kawaguchi R, Matsumoto K, Ishikawa T, Ishitani K, Okagaki R, Ogawa M, Oki T, Ozawa N, Kawasaki K, Kuwabara Y, et al. Guideline for gynecological practice in Japan: Japan society of obstetrics and gynecology and Japan association of obstetricians and gynecologists 2020 edition. J Obstet Gynaecol Res. 2021;47:5–25. doi: 10.1111/jog.14487. [DOI] [PubMed] [Google Scholar]
- 7.Cancer Genome Atlas Research Network, corp-author. Kandoth C, Schultz N, Cherniack AD, Akbani R, Liu Y, Shen H, Robertson AG, Pashtan I, Shen R, et al. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497:67–73. doi: 10.1038/nature12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO Classification of Tumors Editorial Board, corp-author. WHO classification of tumours. 5th edition. Vol 4. International Agency for Research on Cancer; 2020. Female genital tumors; pp. 252–255. [Google Scholar]
- 9.Matsuura M, Yamaguchi K, Tamate M, Satohisa S, Teramoto M, Iwasaki M, Sugita S, Hasegawa T, Koubo R, Takane K, et al. Efficacy of liquid-based genetic diagnosis of endometrial cancer. Cancer Sci. 2018;109:4025–4032. doi: 10.1111/cas.13819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fujiwara H, Takahashi Y, Takano M, Miyamoto M, Nakamura K, Kaneta Y, Hanaoka T, Ohwada M, Sakamoto T, Hirakawa T, et al. Evaluation of endometrial cytology: Cytohistological correlations in 1,441 cancer patients. Oncology. 2015;88:86–94. doi: 10.1159/000368162. [DOI] [PubMed] [Google Scholar]
- 11.Hamashima C, Aoki D, Miyagi E, Saito E, Nakayama T, Sagawa M, Saito H, Sobue T, Japanese Research Group for Development of Cervical Cancer Screening Guidelines The Japanese guideline for cervical cancer screening. Jpn J Clin Oncol. 2010;40:485–502. doi: 10.1093/jjco/hyq036. [DOI] [PubMed] [Google Scholar]
- 12.Frias-Gomez J, Benavente Y, Ponce J, Brunet J, Ibáñez R, Peremiquel-Trillas P, Baixeras N, Zanca A, Piulats JM, Aytés Á, et al. Sensitivity of cervico-vaginal cytology in endometrial carcinoma: A systematic review and meta-analysis. Cancer Cytopathol. 2020;128:792–802. doi: 10.1002/cncy.22266. [DOI] [PubMed] [Google Scholar]
- 13.Ab Mutalib NS, Syafruddin SE, Md Zain RR, Mohd Dali AZ, Mohd Yunos RI, Saidin S, Jamal R, Mokhtar NM. Molecular characterization of serous ovarian carcinoma using a multigene next generation sequencing cancer panel approach. BMC Res Notes. 2014;7:805. doi: 10.1186/1756-0500-7-805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Watanabe T, Nanamiya H, Kojima M, Nomura S, Furukawa S, Soeda S, Tanaka D, Isogai T, Imai JI, Watanabe S, Fujimori K. Clinical implication of oncogenic somatic mutations in early-stage cervical cancer with radical hysterectomy. Sci Rep. 2020;10:18734. doi: 10.1038/s41598-020-72518-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Watanabe T, Nanamiya H, Endo Y, Kojima M, Nomura S, Furukawa S, Soeda S, Tamura H, Ryufuku M, Tanaka D, et al. Identification and clinical significance of somatic oncogenic mutations in epithelial ovarian cancer. J Ovarian Res. 2021;14:129. doi: 10.1186/s13048-021-00876-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murali R, Soslow RA, Weigelt B. Classification of endometrial carcinoma: More than two types. Lancet Oncol. 2014;15:e268–e278. doi: 10.1016/S1470-2045(13)70591-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available in the SAMD00511249-SAMD00511278 repository, ddbj.nig.ac.jp/search.