Abstract
In the context of difficult-to-treat carbapenem-resistant Pseudomonas aeruginosa infections, we evaluated imipenem, meropenem, and doripenem combinations against eleven carbapenemase-producing P. aeruginosa isolates. According to the widespread global distribution of high-risk clones and carbapenemases, four representative isolates were selected: ST175 (OXA-2/VIM-20), ST175 (VIM-2), ST235 (GES-5), and ST111 (IMP-33), for efficacy studies using a sepsis murine model. Minimum inhibitory concentration (mg/L) ranges were 64–256 for imipenem and 16–128 for meropenem and doripenem. In vitro, imipenem plus meropenem was synergistic against 72% of isolates and doripenem plus meropenem or imipenem against 55% and 45%, respectively. All combinations were synergistic against the ST175, ST235, and ST155 clones. In vivo, meropenem diminished the spleen and blood bacterial concentrations of four and three isolates, respectively, with better efficacy than imipenem or doripenem. The combinations did not show efficacy compared with the more active monotherapies, except for imipenem plus meropenem, which reduced the ST235 bacterial spleen concentration. Mortality decreased with imipenem plus meropenem or doripenem for the ST175 isolate. Results suggest that carbapenem combinations are not an alternative for severe infections by carbapenemase-producing P. aeruginosa. Meropenem monotherapy showed in vivo efficacy despite its high MIC, probably because its dosage allowed a sufficient antimicrobial exposure at the infection sites.
Keywords: carbapenemase-producing Pseudomonas aeruginosa, doripenem, efficacy studies, imipenem, meropenem, murine sepsis model
1. Introduction
Pseudomonas aeruginosa is a common cause of community-acquired infections in patients with chronic underlying diseases and hospital-acquired infections, such as pneumonia, urinary tract infections, and bloodstream infections (BSIs) [1]. Recently, it has been described as a pathogen that co-infects patients with COVID-19 [2,3]. The 2016 report by the ECDC on infections acquired in the ICU in 18 European countries showed that, in 2014, P. aeruginosa was the most common cause of ventilator-associated pneumonia and the fifth most prevalent in ICU-acquired BSI [4]. P. aeruginosa infections are associated with elevated disease burden and mortality rates in the absence of optimal treatment [5]. A prospective study showed that patients with P. aeruginosa BSI present higher mortality rates than those with Enterobacteriaceae or other non-lactose fermenting Gram-negative bacilli (GNB) infections [6].
Carbapenem-resistant P. aeruginosa is a significant health concern listed by the WHO as a “priority pathogen”; therefore, it is urgent and necessary to search for new treatments [7]. The European Antimicrobial Resistance Surveillance Network (EARS-Net) reported that 16.9%, 18.9%, 14.5%, and 11.5% of analyzed P. aeruginosa isolates were non-susceptible to ceftazidime, fluoroquinolones, and imipenem/meropenem, and demonstrated combined resistance to three or more antimicrobial groups (including piperacillin/tazobactam, ceftazidime, carbapenems, fluoroquinolones, and aminoglycosides), respectively (2019 data from 30 European Union countries) [8]. Moreover, due to the increased use of carbapenems to treat multidrug-resistant (MDR) P. aeruginosa infections, there is also a growth in carbapenemase production among carbapenem-resistant P. aeruginosa isolates, including the Ambler class A KPC- and GES-type beta-lactamases and the Ambler class B or metallo-beta-lactamases (MBLs), mainly VIM (Verona integrin-encoded MβL), IMP (imipenemase), and NDM (New Delhi MβL) types [9]. In Spain, according to EARS-Net, resistance to carbapenems in invasive isolates of P. aeruginosa has increased up to 21.8% in 2019 [8].
A recent study in India showed that most hospital-acquired P. aeruginosa isolates were MDR [10]; moreover, carbapenem-resistant P. aeruginosa (CRPA) frequently produced carbapenemase, with 62.7% of isolates having at least one carbapenemase gene [11].
The production of MBLs, especially VIM and IMP, has increased in P. aeruginosa isolates [12,13]. Dissemination of high-risk clones, such as ST175 and ST244, producing class B carbapenemases (VIM and IMP) caused outbreaks [14,15,16]. Carbapenemase-producing P. aeruginosa is correlated with higher morbidity and mortality. Health services urgently need to focus on infection prevention and adequate infection management by developing new therapies for these infections [17].
Recent studies found that the association of two carbapenems is efficacious both in vitro and in sepsis models in mice against carbapenemase-producing Acinetobacter baumannii [18,19], multidrug-resistant Enterobacteriaceae [20], KPC-producing Klebsiella pneumoniae [21], and KPC-producing Escherichia coli [22]. In the search for new alternatives for difficult-to-treat carbapenem-resistant P. aeruginosa infections, we aimed to evaluate whether a dual carbapenem treatment could be useful in infections by carbapenemase-producing P. aeruginosa.
2. Results
2.1. In Vitro Results
2.1.1. Isolates’ Carbapenemase Production, Molecular Typing, Antimicrobial Susceptibility Testing, and FICi of Dual Carbapenem Combinations
The sequence types, carbapenemases produced, and MICs of each antibiotic for the eleven isolates are shown in Table 1. All isolates were resistant to the three carbapenems. The checkerboard assays show synergy of meropenem plus doripenem against three strains (CAT05-004 (VIM-1), ST253; MAD05-041 (VIM-2), ST111; and MUR01-018 (IMP-33), ST111); meropenem plus imipenem against MAD02-007 (VIM-2), ST175; and imipenem plus doripenem against CAT05-004 (VIM-1), ST253.
Table 1.
MICs of imipenem, meropenem, and doripenem and fractional inhibitory concentration indexes (FICi) of dual carbapenem combinations for the eleven carbapenemase-producing Pseudomonas aeruginosa clinical strains.
| P. aeruginosa | ST | Carbapenemases | MIC (mg/L) | ΣFICi (mg/L) | ||||
|---|---|---|---|---|---|---|---|---|
| IMP | MEM | DOR | IMP + MEM | IMP + DOR | MEM + DOR | |||
| ARA01-015 | 235 | VIM-2 | 128 | 16 | 64 | 1.06 | 0.56 | 1.00 |
| ARA01-045 | 973 | VIM-2 | 64 | 32 | 32 | 0.75 | 1.06 | 0.63 |
| CAT05-004 | 253 | VIM-1 | 128 | 128 | 128 | 1.00 | 0.50 | 0.50 |
| CLE02-006 | 664 | IMP-1 | 128 | 64 | 64 | 0.75 | 1.00 | 0.75 |
| CVA03-019 | 175 | OXA-2/VIM-20 | 128 | 32 | 32 | 0.75 | 0.75 | 0.75 |
| MAD02-005 | 175 | GES-5 | 64 | 128 | 64 | 0.75 | 0.75 | 0.63 |
| MAD02-007 | 175 | VIM-2 | 128 | 32 | 32 | 0.50 | 1.25 | 1.00 |
| MAD02-021 | 235 | GES-5 | 64 | 128 | 64 | 0.63 | 0.75 | 0.63 |
| MAD04-041 | 155 | IMP-8 | 128 | 16 | 16 | 0.75 | 1.50 | 0.63 |
| MAD05-041 | 111 | VIM-2 | 128 | 16 | 16 | 1.00 | 0.75 | 0.50 |
| MUR01-018 | 111 | IMP-33 | 256 | 128 | 128 | 1.06 | 1 | 0.25 |
ST: Sequence Type. According to EUCAST guidelines: IMP (imipenem) R > 4 mg/L; MEM (meropenem) R > 8 mg/L; DOR (doripenem) R > 4 mg/L. Data on STs and carbapenemases were obtained from a previous study, which includes the complete description of the resistome of the studied strains [23]. Synergistic activity is highlighted in bold. FICi ≤ 0.5 indicates synergy; FICi = 0.5–4 indicates no interaction; and FICi > 4 indicates antagonism.
2.1.2. Time-Kill Assays
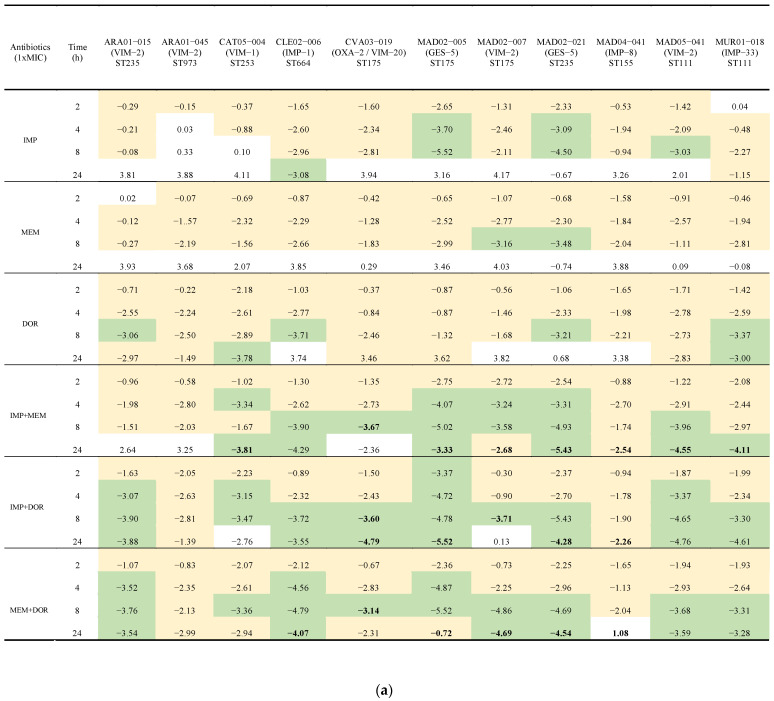
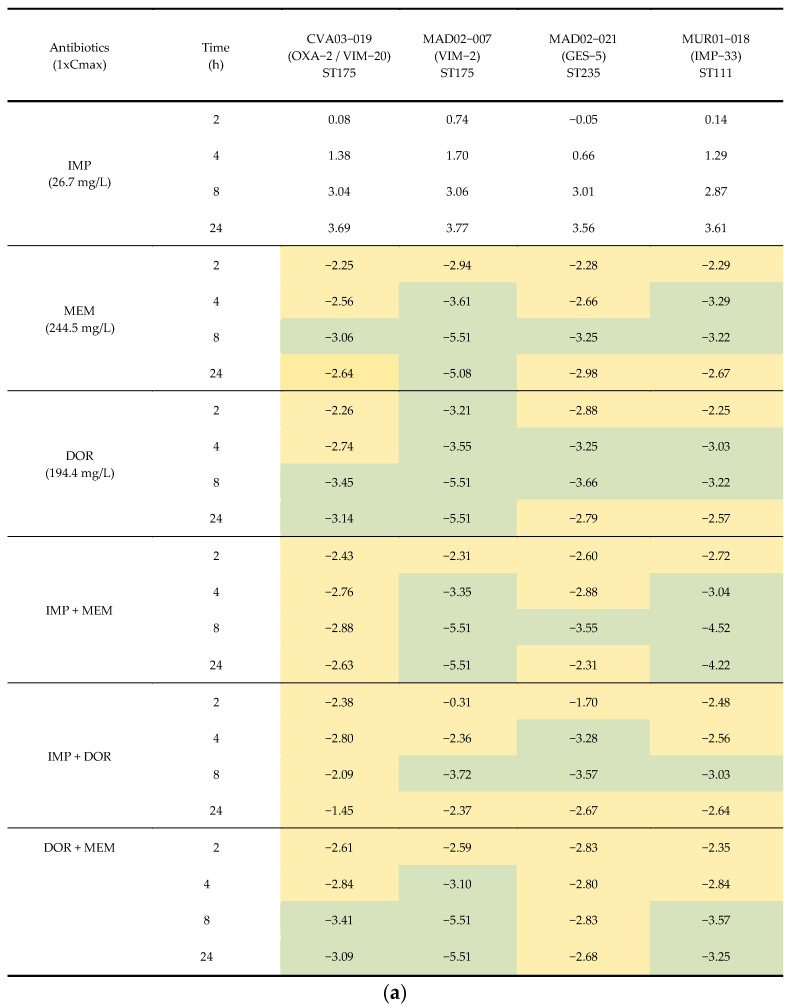
With the assays carried out at MIC concentrations, doripenem was bactericidal against 55% (6/11), imipenem against 36% (4/11), and meropenem against 9% (1/11) of the isolates. The three combinations of carbapenems increased activity compared to when they were tested alone. Bactericidal activity occurred against 9 out of the 11 isolates—the exceptions were ARA01-045 (VIM-2), ST973 and MAD04-041 (IMP-8), ST155. The combination of imipenem plus meropenem was synergistic against 72% (8/11) of isolates, followed by doripenem plus meropenem or imipenem against 55% (6/11) and 45% (5/11), respectively. All combinations were bactericidal and synergistic against the high-risk ST175 (CVA03-019 (OXA2/VIM-20), MAD02-005 (GES-5), and MAD02-007 (VIM-2)) and the ST235 (MAD02-021 (GES-5)) isolates. Finally, for the P. aeruginosa ST973 (ARA01-045 (VIM-2)) isolate, no carbapenem alone or in combination showed bactericidal activity or synergy (Figure 1a,b and Supplementary Material Figure S1).
Figure 1.
(a) Time-kill assays for imipenem, meropenem, and doripenem alone and in combination at MIC concentrations against eleven isolates of carbapenemase-producing P. aeruginosa isolates. Results are represented as differences (log10 CFU/mL) relative to the initial time point (0 h). Green indicates a >3 log10 CFU/mL decrease, yellow a <3 log10 CFU/mL decrease. Bold represents synergistic activity with respect to the most active drug alone at that time point. IMP: imipenem; MEM: meropenem; DOR: doripenem. (b) Time-kill assays for imipenem, meropenem, and doripenem alone and in combination at MIC concentrations against the four carbapenemase-producing P. aeruginosa isolates selected for in vivo studies. Solid circle: growth control; Square: imipenem (IMP); Triangle: meropenem (MEM); Inverted triangle: doripenem (DOR); Empty circle: IMP + MEM; Empty square: IMP + DOR; Empty triangle: MEM + DOR; Dotted line: bactericidal activity.
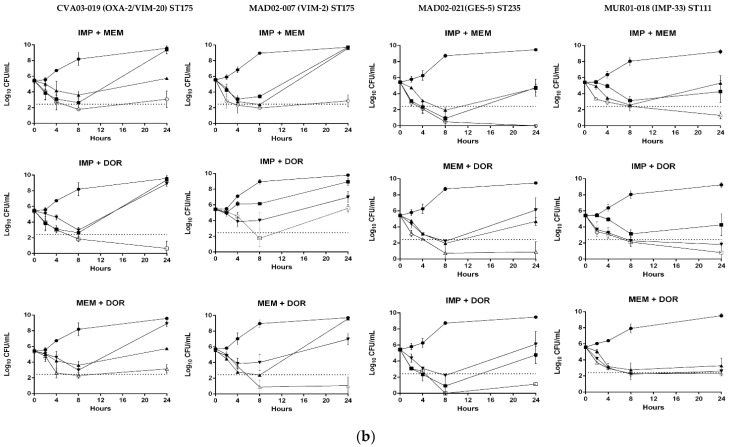
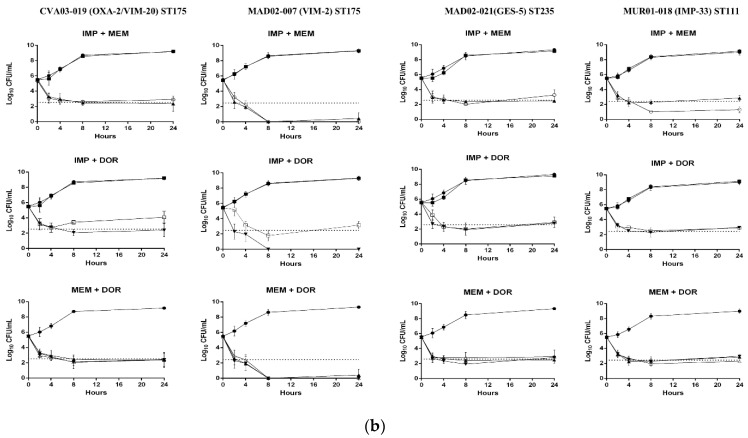
The time-kill assays at Cmax concentrations were performed against the four isolates selected for the in vivo experiments: CVA03-019 (OXA-2/VIM-20), ST175; MAD02-007 (VIM-2), ST175; MAD02-021 (GES-5), ST235; and MUR01-018 (IMP-33), ST111. Imipenem alone was not bactericidal against any of the four isolates, as expected due to the lower value of Cmax with respect to its MIC. On the contrary, meropenem and doripenem, with Cmax higher than their respective MICs, were bactericidal against the four isolates. The combinations of the carbapenems at Cmax were not synergistic (Figure 2a,b).
Figure 2.
(a) Time-kill assays for imipenem, meropenem, and doripenem alone and in combination at maximum mice plasma concentration (Cmax) against the four isolates of carbapenemase-producing P. aeruginosa selected for in vivo studies. Results are represented as differences (log10 CFU/mL) relative to the initial time point (0 h). Green indicates a >3 log10 CFU/mL decrease, yellow a < 3 log10 CFU/mL decrease. (b) Time-kill assays for imipenem, meropenem, and doripenem alone and in combination at maximum mice plasma concentration (Cmax) against the four of carbapenemase-producing P. aeruginosa isolates selected for in vivo studies. Solid circle: growth control; Square: imipenem (IMP); Triangle: meropenem (MEM); Inverted triangle: doripenem (DOR); Empty circle: IMP + MEM; Empty square: IMP + DOR; Empty triangle: MEM + DOR; Dotted line: bactericidal activity.
2.2. In Vivo Results
2.2.1. Peritoneal Sepsis Model
The MLDs obtained for the peritoneal sepsis model in mice were: 8.28, 9.55, 7.11, and 8.66 log10 CFU/mL for CVA03-019 (OXA-2/VIM-20), MAD02-007 (VIM-2), MAD02-021 (GES-5), and MUR01-018 (IMP-33), respectively. Bacterial loads in the spleen and blood and the frequency of bacteremia at initiation of treatment and at 24 h are detailed in Table 2.
Table 2.
Bacterial concentrations in spleen and blood and percentages of bacteremia in infected, untreated mice at initiation of treatment and at 24 h after infection.
| Hours after Infection | Isolates | Carbapenemases | ST | Spleen (log10 CFU/g) |
Blood (log10 CFU/mL) |
Bacteremia (%) | Mortality (%) |
|---|---|---|---|---|---|---|---|
| 2 | CVA03-019 | OXA-2/VIM-20 | 175 | 5.62 ± 0.51 | 3.35 ± 0.49 | 100 | - |
| MAD02-007 | VIM-2 | 175 | 7.38 ± 0.12 | 5.69 ± 0.55 | 100 | - | |
| MAD02-021 | GES-5 | 235 | 5.64 ± 0.49 | 3.50 ± 0.28 | 100 | - | |
| MUR01-018 | IMP-33 | 111 | 5.90 ± 0.79 | 2.67 ± 0.46 | 100 | - | |
| 24 | CVA03-019 | OXA-2/VIM-20 | 175 | 8.7 ± 0.1 | 7.2 ± 1.1 | 100 | 83 |
| MAD02-007 | VIM-2 | 175 | 8.6 ± 1.1 | 7.1 ± 1.1 | 100 | 83 | |
| MAD02-021 | GES-5 | 235 | 8.3 ± 0.5 | 7.4 ± 0.6 | 100 | 100 | |
| MUR01-018 | IMP-33 | 111 | 6.5 ± 0.4 a,b,c | 2.8 ± 1.0 a,b,c | 100 | 17 c |
-: Animals were sacrificed two hours after infection; a: p < 0.05 with respect to CVA03-019 isolate; b: p < 0.05 with respect to MAD02-007 isolate and c: p < 0.05 with respect to MAD02-021 isolate.
2.2.2. Efficacy Studies
The in vivo efficacies of imipenem, meropenem, and doripenem in monotherapy and combination against the four selected isolates are detailed in Table 3. Meropenem monotherapy diminished the spleen bacterial concentrations in control mice for all isolates between −2.0 and −4.9 log10 CFU/g; similarly, in blood, it diminished bacterial concentrations in three isolates between −3.7 and −5.9 log10 CFU/mL, the exception being the MUR01-018 (IMP-33) isolate. Meropenem monotherapy was better than imipenem in decreasing the spleen and blood bacterial concentrations in the infection with three and two isolates, respectively. Furthermore, meropenem monotherapy was better than doripenem against two and one isolates, respectively.
Table 3.
In vivo efficacy of imipenem, meropenem, and doripenem, in monotherapy and in combinations, for the experimental peritoneal sepsis model.
| Isolates; Clone (Carbapenemase) |
Therapy | n | Doses (mg/kg) |
Spleen (log10 CFU/g) |
Blood (log10 CFU/mL) |
Mortality (%) |
|---|---|---|---|---|---|---|
| IMP plus MEM | ||||||
| CVA03-019; ST175 (OXA-2/VIM-20) |
Control | 6 | - | 8.7 ± 0.1 | 7.2 ± 1.1 | 83 |
| IMP | 6 | 30 | 7.6 ± 1.2 | 4.9 ± 1.4 | 17 | |
| MEM | 6 | 300 | 4.0 ± 0.9 a,b | 1.5 ± 1.6 a | 17 | |
| IMP + MEM | 5 | 4.4 ± 0.5 a,b | 1.6 ± 1.1 a,b | 0 a | ||
| MAD02-007; ST175 (VIM-2) |
Control | 6 | - | 8.6 ± 1.1 | 7.1 ± 1.1 | 83 |
| IMP | 6 | 30 | 8.5 ± 0.4 | 6.2 ± 0.8 | 50 | |
| MEM | 6 | 300 | 6.6 ± 0.6 a, b | 3.4 ± 0.6 a,b | 33 | |
| IMP + MEM | 6 | 6.3 ± 0.9 a,b | 3.1 ± 0.8 a,b | 50 | ||
| MAD02-021; ST235 (GES-5) |
Control | 6 | - | 8.3 ± 0.5 | 7.4 ± 0.6 | 100 |
| IMP | 6 | 30 | 6.9 ± 1.4 | 4.1 ± 1.0 a | 17 a | |
| MEM | 6 | 300 | 3.4 ± 1.1 a,b | 1.5 ± 1.3 a,b | 17 a | |
| IMP + MEM | 5 | 0.5 ± 1.1 a,b,c | 0.0 ± 0.0 a,b | 0 a | ||
| MUR01-018; ST111 (IMP-33) |
Control | 6 | - | 6.5 ± 0.4 | 2.8 ± 1.0 | 17 |
| IMP | 6 | 30 | 3.6 ± 0.5 a | 0.7 ± 0.9 a | 0 | |
| MEM | 6 | 300 | 3.4 ± 0.6 a | 1.5 ± 1.4 | 0 | |
| IMP + MEM | 5 | 3.6 ± 0.3 a | 0.7 ± 1.2 | 0 | ||
| IMP plus DOR | ||||||
| CVA03-019; ST175 (OXA-2/VIM-20) |
Control | 6 | - | 8.7 ± 0.1 | 7.2 ± 1.1 | 83 |
| IMP | 6 | 30 | 7.6 ± 1.2 | 4.9 ± 1.4 | 17 | |
| DOR | 5 | 150 | 7.3 ± 1.5 | 4.8 ± 2.2 | 40 | |
| IMP + DOR | 5 | 5.9 ± 1.4 a | 2.2 ± 0.5 a | 0 a | ||
| MAD02-007; ST175 (VIM-2) |
Control | 6 | - | 8.6 ± 1.1 | 7.1 ± 1.1 | 83 |
| IMP | 6 | 30 | 8.5 ± 0.4 | 6.2 ± 0.8 | 50 | |
| DOR | 5 | 150 | 7.8 ± 0.6 | 5.6 ± 0.7 | 20 | |
| IMP + DOR | 5 | 6.2 ± 1.3 | 3.0 ± 2.2 a | 20 | ||
| MAD02-021; ST235 (GES-5) |
Control | 6 | - | 8.3 ± 0.5 | 7.4 ± 0.6 | 100 |
| IMP | 6 | 30 | 6.9 ± 1.4 | 4.1 ± 1.0 a | 17 a | |
| DOR | 5 | 150 | 4.5 ± 1.7 a | 3.0 ± 2.7 | 0 a | |
| IMP + DOR | 5 | 2.3 ± 1.3 a,b | 2.4 ± 1.8 a | 0 a | ||
| MUR01-018; ST111 (IMP-33) |
Control | 6 | - | 6.5 ± 0.4 | 2.8 ± 1.0 | 17 |
| IMP | 6 | 30 | 3.6 ± 0.5 a,d | 0.7 ± 0.9 a | 0 | |
| DOR | 6 | 150 | 4.8 ± 0.6 a | 2.2 ± 1.9 | 10 | |
| IMP + DOR | 5 | 3.0 ± 1.7 a | 0.0 ± 0.0 a | 0 | ||
| MEM plus DOR | ||||||
| CVA03-019; ST175 (OXA-2/VIM-20) |
Control | 6 | - | 8.7 ± 0.1 | 7.2 ± 1.1 | 83 |
| MEM | 6 | 300 | 4.0 ± 0.9 a,d | 1.5 ± 1.6 a | 17 | |
| DOR | 5 | 150 | 7.3 ± 1.5 | 4.8 ± 2.2 | 40 | |
| MEM + DOR | 5 | 4.8 ± 1.0 a | 2.0 ± 1.6 a | 20 | ||
| MAD02-007; ST175 (VIM-2) |
Control | 6 | - | 8.6 ± 1.1 | 7.1 ± 1.1 | 83 |
| MEM | 6 | 300 | 6.6 ± 0.6 a | 3.4 ± 0.6 a,d | 33 | |
| DOR | 5 | 150 | 7.8 ± 0.6 | 5.6 ± 0.7 | 20 | |
| MEM + DOR | 5 | 6.8 ± 1.0 | 4.0 ± 1.2 a | 20 | ||
| MAD02-021; ST235 (GES-5) |
Control | 6 | - | 8.3 ± 0.5 | 7.4 ± 0.6 | 100 |
| MEM | 6 | 300 | 3.4 ± 1.1 a | 1.5 ± 1.3 a | 17 a | |
| DOR | 5 | 150 | 4.5 ± 1.7 a | 3.0 ± 2.7 | 0 a | |
| MEM + DOR | 5 | 2.4 ± 1.4 a | 0.0 ± 0.0 a | 0 a | ||
| MUR01-018; ST111 (IMP-33) |
Control | 6 | - | 6.5 ± 0.4 | 2.8 ± 1.0 | 17 |
| MEM | 6 | 300 | 3.4 ± 0.6 a,d | 1.5 ± 1.4 | 0 | |
| DOR | 6 | 150 | 4.8 ± 0.6 a | 2.2 ± 1.9 | 10 | |
| MEM + DOR | 5 | 4.0 ± 0.5 a | 0.5 ± 0.9 | 0 | ||
IMP: imipenem; MEM: meropenem; DOR: doripenem; -: without treatment; CFU: colony-forming unit; a: p < 0.05 with respect to control group; b: p < 0.05 with respect to IMP group; c: p < 0.05 with respect to MEM group; and d: p < 0.05 with respect to DOR group.
Imipenem monotherapy diminished the spleen and blood bacterial concentrations only for the MUR01-018 (IMP-33) isolate (−2.9 log10 CFU/g) and for the MAD02-021 (GES-5) and MUR01-018 (IMP-33) (−3.3 and −2.1 log10 CFU/mL) isolates, respectively. Doripenem monotherapy diminished only the spleen bacterial concentrations for the MAD02-021 (GES-5) and MUR01-018 (IMP-33) (−3.8 and −1.7 log10 CFU/g) isolates. Regarding the mortality rate, the three carbapenems in monotherapy increased the survival for the MAD02-021 (GES-5).
The three combinations of two carbapenems were efficacious in reducing the bacterial concentrations in spleen and blood, compared with their respective controls, against the four P. aeruginosa clinical isolates producing OXA-2/VIM-20, VIM-2, GES-5, or IMP-33. The exceptions were the bacterial concentration in blood for the IMP-33 producer with imipenem plus meropenem, the bacterial spleen concentration for the VIM-2 producer with imipenem plus doripenem, and the bacterial spleen and blood concentrations for the VIM-2 and IMP-33 producers with meropenem plus doripenem. However, the combinations of two carbapenems did not show efficacy in general compared with the more active monotherapies. Only the combination of imipenem plus meropenem reduced the spleen bacterial concentration, compared with the most efficacious monotherapy, for the GES-5 producer isolate (−2.9 log10 CFU/g). Regarding mortality, it decreased with imipenem plus meropenem or doripenem for the OXA-2/VIM-20 producer isolate (83% vs. 0%) compared with the monotherapies.
3. Discussion
To the best of our knowledge, dual carbapenem combinations have never been tested in vivo against carbapenemase-producing P. aeruginosa. In this study, we found that the combination of carbapenems was not more efficacious than the most active carbapenem monotherapy in a murine sepsis model infected with P. aeruginosa clinical isolates producing OXA-2/VIM-20, VIM-2, GES-5, or IMP-33. Unexpectedly, meropenem monotherapy showed in vivo efficacy despite its high MIC against the tested isolates in reducing bacterial concentrations in the spleen and blood and was better than imipenem or doripenem. Meropenem in monotherapy was also able to reduce mortality compared to control mice against the GES-5 producer. These results with meropenem monotherapy are probably associated with its serum concentration exceeding the MIC for more than 50% of the time between doses (with the dosage used), which is equivalent to a dosage in humans of 2 g every eight hours [24]. A pharmacokinetics/pharmacodynamics (PK/PD) model using a Monte Carlo simulation [25] supports this hypothesis by showing that an optimized administration of meropenem at a dose of 2 g/8 h achieved a PD target ≥90% for P. aeruginosa isolates with an MIC of up to 128 mg/L, similar to the isolates used in our in vivo experiments, with a cumulative fraction of response ≥90%. These results with meropenem reinforce the category of “susceptible increased exposure” released by the EUCAST in 2021 [26]. The efficacy of this dosage was also observed in a recent study in a murine sepsis model by carbapenemase-producing A. baumannii [19].
Imipenem monotherapy reduced the bacterial concentration in the spleen and blood in the in vivo experiments with the IMP-33 producer isolate and in blood with the GES-5 producer. The efficacy of imipenem monotherapy may not be associated with the pharmacodynamics of the dosage used, based on the reported pharmacokinetics (PK) data [27]. In the case of the GES-5 producer isolate, the in vivo efficacy mimics the time-kill in vitro results, in which imipenem at concentrations equivalent to its MIC was bactericidal at 4 and 8 h. However, its in vivo efficacy against the IMP-33 producer may not be related to the in vitro results. In this case, the results with imipenem and doripenem may be related to the low virulence of the IMP-33 producer isolate in terms of lesser bacterial concentrations in the spleen and blood and its lower mortality compared with the other three isolates tested in vivo. The efficacy of imipenem was also observed in a murine model against OXA-58 and OXA-23 A. baumannii producer strains [19]. Similarly, doripenem monotherapy showed efficacy in reducing the spleen bacterial concentrations against the GES-5 and the IMP-33 producer isolates, respectively, thereby mimicking the bactericidal activity observed in vitro in the time-kill studies, besides the low virulence of the IMP-33 isolate. It must be mentioned that, currently, doripenem is available in very few countries.
The three combinations of two carbapenems were generally efficacious in reducing the bacterial concentrations in the spleen and blood compared with their respective controls against the four P. aeruginosa clinical isolates producing OXA-2/VIM-20, VIM-2, GES-5, or IMP-33. However, the combinations of two carbapenems were not better than the most efficacious monotherapy in reducing the spleen bacterial concentration for the GES-5 producer isolate, apart from imipenem plus meropenem. These in vivo results were not in agreement with the in vitro studies, which showed synergistic activity of the three combinations against the OXA-2/VIM-20, VIM-2, and GES-5 producer isolates, as well as the imipenem plus meropenem combination against the IMP-33 producer isolate. Besides the impact of the innate immune response and the pharmacodynamics of the in vivo experiments, the in vitro studies were performed with MIC concentrations higher than those achieved in vivo, considering the carbapenem resistance of the isolates. The good results achieved with the carbapenem combinations compared with the untreated controls were also reported against OXA-58 and OXA-23 A. baumannii producers [18,19].
The lack of proven valid therapeutic options and the rapid development of antimicrobial resistance for infections caused by carbapenemase-producing P. aeruginosa isolates justifies the use of combination therapy for infections caused by carbapenemase-producing pathogens [28]. Thus, in vitro synergism between meropenem and ertapenem has been reported against carbapenem-resistant K. pneumoniae [29]. Further combinations include meropenem plus doripenem or ertapenem against OXA-181 and VIM E. coli producers, NDM-1 K. pneumoniae producer isolates, and the combination of imipenem plus meropenem against the NDM-1 K. pneumoniae producer isolate [30]. The combination of two synergistic carbapenems, alone or combined with other families of antibiotics, has been suggested as a treatment for carbapenem-resistant, carbapenemase-producing K. pneumoniae [31] and carbapenemase-producing A. baumannii [19]. In addition to the different in vitro studies showing activity with dual carbapenem combinations [18,29,32], there have been positive clinical outcomes reported with meropenem plus ertapenem in BSI by KPC-producing E. coli [22] and by carbapenemase-producing K. pneumoniae [20], as well as reports that ertapenem plus meropenem or doripenem was efficacious in BSI and urinary tract infection by KPC-producing K. pneumoniae [21].
Although there are more experimental and clinical studies about the use of dual carbapenem therapies against infections by MDR-GNB published every day, the safety of these approaches has not been widely addressed. Nevertheless, there are some studies that have evaluated both the efficacy and safety of carbapenem combination treatments, suggesting that these treatments may be effective and safe to treat carbapenemase-producing K. pneumoniae [33] or carbapenem-resistant Enterobacteriaceae [34].
Although the exact mechanism of action is not fully understood against KPC-producing K. pneumoniae, some have postulated that the mechanisms for dual carbapenems against carbapenemase-producing organisms could be related to the binding of one of the carbapenems to the active site of the enzyme, using its action in a concentration-independent way, while the other carbapenem binds to the bacterial target [21,29]. Others have suggested that the benefit of the ertapenem plus doripenem combination could be related to the preferential affinity of the enzyme for ertapenem. In this way, the enzyme is consumed during the hydrolysis of ertapenem, leaving higher concentrations of doripenem acting against the pathogen [35].
Although our results suggest that these combinations are not an alternative for severe infections by carbapenemase-producing strains of P. aeruginosa, as in any animal model study, a limitation is the general caution to translate the preclinical studies to the clinical setting, although the antibiotics dosages have been chosen according to the pharmacodynamic targets in human beings. Moreover, the 3R rules [36] (Hubrecht and Carter, 2019) prevent us from increasing the numbers of animals to test the same hypothesis in male mice. As strengths of the study, the chosen isolates from the GEMARA/REIPI collection [23], both for the in vitro and in vivo studies, are representative of high-risk clones and widespread acquired carbapenemases [15,37,38,39].
4. Conclusions
The results suggest that dual carbapenem combinations are not a therapeutic alternative for severe infections by carbapenemase-producing strains of P. aeruginosa. Moreover, the in vitro activity of carbapenem combinations against class A and B carbapenemase producers did not match the in vivo results. Thus, the highest efficacy was observed against the ST 235, GES-5 producer isolate, despite its being the most efficient binding and catalyzing carbapenem from class A carbapenemases [40]. Unexpectedly, meropenem monotherapy showed in vivo efficacy despite its high MIC against the tested isolates, probably because its dosage allowed a sufficient antimicrobial exposure at the infection sites.
5. Materials and Methods
5.1. In Vitro Studies
5.1.1. Bacterial Isolates’ Characterization and Molecular Typing
The GEMARA/REIPI study group collected healthcare-associated non-duplicated P. aeruginosa clinical isolates from 51 participating Spanish hospitals in 2017 [23], identified by a Microflex LT-MALDI Biotyper mass spectrometer (Bruker Daltonics GmbH, Bremen, Germany). The presence of carbapenemase genes and genes coding for other beta-lactamases was confirmed by PCR and sequencing; moreover, representative XDR isolates and PFGE clonal types were fully sequenced (Miseq, Illumina, La Jolla, CA, USA) [23]. Eleven of such isolates producing diverse carbapenemases and belonging to different clonal types were selected for the in vitro studies: ARA01-015 (VIM-2), ST235; ARA01-045 (VIM-2), ST973; CAT05-004 (VIM-1), ST253; CLE02-006 (IMP-1), ST664; CVA03-019 (OXA-2/VIM-20), ST175; MAD02-005 (GES-5), ST175; MAD02-007 (VIM-2), ST175; MAD02-021 (GES-5), ST235; MAD04-041 (IMP-8), ST155; MAD05-041 (VIM-2), ST111, and MUR01-018 (IMP-33), ST111. According to the widespread global distribution of P. aeruginosa high-risk clones and their association with acquired carbapenemases [15,16], the following four strains were selected for preclinical studies in mice, CVA03-019 (OXA-2/VIM-20), ST175; MAD02-007 (VIM-2), ST175; MAD02-021 (GES-5), ST235; and MUR01-018 (IMP-33), ST111.
5.1.2. Antimicrobials
For the in vitro experiments, antibiotic drugs were used as standard laboratory powders: imipenem and doripenem from Alsachim (Alsachim, Illkirch Graffenstaden, France) and meropenem from Sigma (Sigma-Aldrich, Madrid, Spain).
For the in vivo studies, clinical formulations were used for imipenem (Fresenius Kabi, Barcelona, Spain) and meropenem (Ranbaxy, Barcelona, Spain). In the case of doripenem, as it is not used in the clinic setting in Europe, it was used as a standard powder from Alsachim (Alsachim, Illkirch Graffenstaden, France).
5.1.3. Antimicrobial Susceptibility Testing
MICs of the three carbapenems were determined by the broth microdilution method with geometric two-fold serial dilutions of the antimicrobial agents (ranging from 2 to 1024 mg/L), as recommended by the EUCAST [26]. Tests were conducted using Cation-adjusted Müller Hinton Broth II (CAMHBII, 90922 Merck Life Science S.L., Madrid, Spain) and a final inoculum of 5 × 105 CFU/mL. Quantification of the initial inoculum and bacterial growth was obtained by subculture on blood agar plates (Becton Dickinson) incubated for 18–24 h at 37 °C in air. P. aeruginosa ATCC 27853 was used as a quality control strain. MICs were evaluated after 24 h of incubation at 37 °C. The MIC was defined as the lowest concentration of antibiotic at which no growth was visible. Results were interpreted according to the EUCAST breakpoints [26].
5.1.4. Synergy Studies
Checkerboard Assays
The antibiotic concentrations studied were from 8 to 512 mg/L for imipenem and from 4 to 256 mg/L for meropenem and doripenem, respectively. A two-fold dilution of each antimicrobial agent alone or with different combinations was performed in CAMHBII in 96-wells microplates. A freshly prepared inoculum of each isolate was added to obtain a concentration of 5 × 105 CFU/mL in each well. Plates were incubated at 37 °C for 18–24 h, and the MIC was read. Growth and sterility controls were also included in each plate. The reference strain P. aeruginosa ATCC27853 was used as a control. The assay was performed in triplicates for each antibiotic.
Fractional inhibitory concentration indexes (FICi) were calculated according to the following formula, FICi = FIC of antibiotic A + FIC of antibiotic B where FIC of A or B = MIC of A or B in combination, divided by the MIC of A or B alone. Interpretation of the results was based on the following FICi values: synergy ≤ 0.5, no interaction > 0.5 to 4, and antagonism > 4 [18].
Time-Kill Assays
Imipenem, meropenem, and doripenem were tested at MIC values alone and in combination for the eleven isolates. Moreover, for the four isolates selected for the peritoneal sepsis model, time-kill assays were also performed at the peak concentrations achievable in serum. The studies were carried out in log-phase with a starting inoculum of 5 × 105 CFU/mL with the antibiotics alone or in combination. Tubes were incubated at 37 °C with shaking, and samples were taken at 0, 2, 4, 8, and 24 h, serially diluted, and seeded in 5% sheep blood plates [41]. Bactericidal activity was defined as a ≥3 log10 CFU/mL decrease from the initial inoculum. Synergistic activity was defined as a decrease of ≥2 log10 CFU/mL for the antimicrobial combination compared with the most active single agent [42].
5.2. In Vivo Studies
5.2.1. Animals
A total of 165 immunocompetent C57BL/6J female mice weighing 20 g (7–9 weeks old) were used (Production and Experimentation Animal Centre, University of Seville, Seville, Spain). Mice were housed in a ventilated cage system under specific pathogen-free conditions, with water and food ad libitum. The study was carried out following the recommendations in the Guide for the Care and Use of Laboratory Animals [43]. All efforts were made to minimize suffering. This study was approved by the Committee on the Ethics of Animal Experiments of the University Hospital Virgen del Rocío and the Ministry of Agricultura, Pesca, and Desarrollo Rural (08/03/2019/028), Spain. Mice were sacrificed using an intraperitoneal (ip) lethal dose of sodium thiopental (B. Braun Medical S.A., Barcelona, Spain).
5.2.2. Peritoneal Sepsis Model
An experimental peritoneal sepsis model was used [27] with the four selected P. aeruginosa isolates based on their ST and carbapenemase production: CVA03-019 (OXA-2/VIM-20), ST175; MAD02-007 (VIM-2), ST175; MAD02-021 (GES-5) ST235; and MUR01-018 (IMP-33), ST111. The minimum lethal doses (MLDs, concentration of inoculum killing 100% of the animals) were determined by the Reed and Munch method [44] for the four strains. Briefly, for each strain, groups of six unanesthetized mice were ip inoculated with 0.5 mL of decreasing bacterial concentrations. The inoculum ranges used were 9.28 to 7.49 log10 CFU/mL for P. aeruginosa CVA03-019; 9.55 to 7.41 log10 CFU/mL for P. aeruginosa MAD02-007; 9.02 to 7.11 log10 CFU/mL for P. aeruginosa MAD02-021; and 8.66 to 7.56 log10 CFU/mL for P. aeruginosa MUR01-018. After inoculation, animals were observed and monitored for 7 days.
5.2.3. Efficacy Studies
After the peritoneal sepsis model characterization for each isolate, we evaluated the efficacy of dual carbapenem treatment. Concisely, groups of mice (n = 5–6) were ip inoculated with 500 µL of the MLD (log10 CFU/mL) of each isolate. Treatments were initiated two hours after inoculation and lasted 24 h. Infected mice were randomly assigned to the followings groups: (i) control (untreated); (ii) imipenem 30 mg/kg/q4h administered intramuscularly (im); (iii) meropenem 300 mg/kg/q2h/ip; (iv) doripenem 150 mg/kg/q12h/ip; (v) imipenem plus meropenem; (vi) imipenem plus doripenem; and (vii) meropenem plus doripenem. Antimicrobials were used in combination with the same dosage schedule as in monotherapy, receiving the first dose of both carbapenems two hours after inoculation and the remaining doses with the specified time intervals. The antimicrobial dosages were based on the PK/PD data and their proven efficacy, alone and in combination, in experimental models of infected mice [19,24,27,45,46,47]. Samples were extracted and processed immediately after mouse death; survivor mice were sacrificed (sodium thiopental/ip) after 24 h of treatment. Aseptic thoracotomies were carried out, and through cardiac punctures, blood samples were obtained for quantitative (log10 CFU/mL) and qualitative blood cultures. Results were expressed as positive (≥1 CFU present in the plate) or negative. Spleens were aseptically extracted, weighed, and homogenized in sterile saline (Stomacher 80; Tekmar Co., Cincinnati, OH, USA) before quantitative cultures (log10 CFU/g) in Columbia agar with 5% sheep blood plates.
5.3. Statistical Analysis
Mortality and positive blood cultures were expressed as percentages. Bacterial spleen concentrations (log10 CFU/g) and bacterial blood concentrations (log10 CFU/mL) were expressed as means ± SD. Differences in bacterial concentrations were compared by analysis of variance and the Dunnet and Tukey’s post hoc tests. Mortality and blood sterility rates between groups were compared by the two-tailed Fisher’s test. A p-value < 0.05 was considered significant. SPSS v22.0 was used (SPSS Inc., Chicago, IL, USA).
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/antibiotics11091212/s1, Figure S1. Time-kill curves at 1xMIC of dual carbapenem combination against seven carbapenemase-producing P. aeruginosa.
Author Contributions
S.H.-E., E.D.B.-T., T.C.-C. and C.L.-C. performed the in vitro and in vivo experiments. R.Á.-M. obtained the funds to perform the studies and reviewed the manuscript and the experiments. J.M.C., A.O. and J.P. reviewed the manuscript and the experiments. M.E.P.-I. coordinated the experiments, reviewed the results, and wrote the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of University Hospital Virgen del Rocío and the Ministry of Agricultura, Pesca, and Desarrollo Rural (08/03/2019/028).
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding Statement
This study was supported by the Instituto de Salud Carlos III, Proyectos de Investigación en Salud (PI18-01842), Subdirección General de Redes y Centros de Investigación Cooperativa, Ministerio de Economía, Industria y Competitividad, and the Spanish Network for Research in Infectious Diseases (REIPI, RD16/0016/0004, RD16/0016/0009)—co-financed by the European Development Regional Fund, A way to achieve Europe, Operative program Intelligent Growth 2014-2020. S.H.E is supported by the by the Instituto de Salud Carlos III, Proyectos de Investigación en Salud (PI18-01842). M.E.P.I. is a researcher belonging to the program “Nicolás Monardes” (C1-0038-2019), Servicio Andaluz de Salud, Junta de Andalucía, Spain. R.A.M., J.M.C., and M.E.P.I. (CB21/13/00006) and A.O.P. (CB21/13/00099) also received support from the CIBER de Enfermedades Infecciosas (CIBERINFEC), Instituto de Salud Carlos III, Ministerio de Ciencia e Innovación, co-financed by the European Development Regional Fund. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pachori P., Gothalwal R., Gandhi P. Emergence of antibiotic resistance Pseudomonas aeruginosa in intensive care unit; a critical review. Genes Dis. 2019;6:109–119. doi: 10.1016/j.gendis.2019.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Qu J., Cai Z., Liu Y., Duan X., Han S., Liu J., Zhu Y., Jiang Z., Zhang Y., Zhuo C., et al. Persistent Bacterial Coinfection of a COVID-19 Patient Caused by a Genetically Adapted Pseudomonas aeruginosa Chronic Colonizer. Front. Cell. Infect. Microbiol. 2021;11:641920. doi: 10.3389/fcimb.2021.641920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loyola-Cruz M.Á., Durán-Manuel E.M., Cruz-Cruz C., Marquez-Valdelamar L.M., Bravata-Alcantara J.C., Cortés-Ortíz I.A., Cureño-Díaz M.A., Ibáñez-Cervantes G., Fernández-Sánchez V., Castro-Escarpulli G., et al. ESKAPE bacteria characterization reveals the presence of Acinetobacter baumannii and Pseudomonas aeruginosa outbreaks in COVID-19/VAP patients. Am. J. Infect. Control. 2022 doi: 10.1016/j.ajic.2022.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.European Centre for Disease Prevention and Control (ECDC) Healthcare-Associated Infections in Intensive Care Units (Annual Epidemiological Report for 2016) [(accessed on 4 May 2018)]. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/AER_for_2016-HAI_0.pdf.
- 5.Zilberberg M.D., Shorr A.F. Prevalence of multidrug-resistant Pseudomonas aeruginosa and carbapenem-resistant Enterobacteriaceae among specimens from hospitalized patients with pneumonia and bloodstream infections in the United States from 2000 to 2009. J. Hosp. Med. 2013;8:559–563. doi: 10.1002/jhm.2080. [DOI] [PubMed] [Google Scholar]
- 6.Thaden J.T., Park L.P., Maskarinec S.A., Ruffin F., Fowler V.G., Jr., van Duin D. Results from a 13-Year prospective cohort study show increased mortality associated with bloodstream infections caused by Pseudomonas aeruginosa compared to other bacteria. Antimicrob. Agents Chemother. 2017;61:e02671-16. doi: 10.1128/AAC.02671-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization (WHO) Global Priority List of Antibiotic-Resistant Bacteria to Guide Research, Discovery, and Development of New Antibiotics. [(accessed on 27 February 2017)]. Available online: https://www.who.int/news/item/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed.
- 8.European Centre for Disease Prevention and Control (ECDC) European Antimicrobial Resistance Surveillance Network. [(accessed on 18 November 2020)]. Available online: https://www.ecdc.europa.eu/en/publications-data/surveillance-antimicrobial-resistance-europe-2019.
- 9.Walsh T.R., Toleman M.A., Poirel L., Nordmann P. Metallo-beta-lactamases: The quiet before the storm? Clin. Microbiol. Rev. 2005;18:306–325. doi: 10.1128/CMR.18.2.306-325.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khodare A., Kale P., Pindi G., Joy L., Khillan V. Incidence, microbiological profile, and impact of preventive measures on central line-associated bloodstream infection in liver care Intensive Care Unit. Indian J. Crit. Care Med. 2020;24:17–22. doi: 10.5005/jp-journals-10071-23325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Verma N., Prahraj A.K., Mishra B., Behera B., Gupta K. Detection of carbapenemase-producing Pseudomonas aeruginosa by phenotypic and genotypic methods in a tertiary care hospital of East India. J. Lab. Phys. 2019;11:287–291. doi: 10.4103/JLP.JLP_136_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hopman J., Meijer C., Kenters N., Coolen J.P.M., Ghamati M.R., Mehtar S., van Crevel R., Morshuis W.J., Verhagen A., van den Heuvel M.M., et al. Risk Assessment after a severe hospital-acquired infection associated with carbapenemase-producing Pseudomonas aeruginosa. JAMA Netw. Open. 2019;2:e187665. doi: 10.1001/jamanetworkopen.2018.7665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hong D.J., Bae I.K., Jang I.H., Jeong S.H., Kang H.K., Lee K. Epidemiology and characteristics of metallo-β-lactamasepProducing Pseudomonas aeruginosa. Infect. Chemother. 2015;47:81–97. doi: 10.3947/ic.2015.47.2.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pérez-Vázquez M., Sola-Campoy P.J., Zurita Á.M., Ávila A., Gómez-Bertomeu F., SolÍs S., López-Urrutia L., Gónzalez-BarberÁ E.M., Cercenado E., Bautista V., et al. Carbapenemase-producing Pseudomonas aeruginosa in Spain: Interregional dissemination of the high-risk clones ST175 and ST244 carrying bla(VIM-2), bla(VIM-1), bla(IMP-8), bla(VIM-20) and bla(KPC-2) Int. J. Antimicrob. Agents. 2020;56:106026. doi: 10.1016/j.ijantimicag.2020.106026. [DOI] [PubMed] [Google Scholar]
- 15.Del Barrio-Tofiño E., López-Causapé C., Oliver A. Pseudomonas aeruginosa epidemic high-risk clones and their association with horizontally-acquired β-lactamases: 2020 update. Int. J. Antimicrob. Agents. 2020;56:106196. doi: 10.1016/j.ijantimicag.2020.106196. [DOI] [PubMed] [Google Scholar]
- 16.Oliver A., Mulet X., López-Causapé C., Juan C. The increasing threat of Pseudomonas aeruginosa high-risk clones. Drug Resist. Updat. 2015;21:41–59. doi: 10.1016/j.drup.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 17.Ramírez-Estrada S., Borgatta B., Rello J. Pseudomonas aeruginosa ventilator-associated pneumonia management. Infect. Drug Resist. 2016;9:7–18. doi: 10.2147/IDR.S50669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nordmann P., Perler J., Kieffer N., Poirel L. In-vitro evaluation of a dual carbapenem combination against carbapenemase-producing Acinetobacter baumannii. J. Infect. 2020;80:121–142. doi: 10.1016/j.jinf.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 19.Cebrero-Cangueiro T., Nordmann P., Carretero-Ledesma M., Pachón J., Pachón-Ibáñez M.E. Efficacy of dual carbapenem treatment in a murine sepsis model of infection due to carbapenemase-producing Acinetobacter baumannii. J. Antimicrob. Chemother. 2021;76:680–683. doi: 10.1093/jac/dkaa487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oliva A., D’Abramo A., D’Agostino C., Iannetta M., Mascellino M.T., Gallinelli C., Mastroianni C.M., Vullo V. Synergistic activity and effectiveness of a double-carbapenem regimen in pandrug-resistant Klebsiella pneumoniae bloodstream infections. J. Antimicrob. Chemother. 2014;69:1718–1720. doi: 10.1093/jac/dku027. [DOI] [PubMed] [Google Scholar]
- 21.Giamarellou H., Galani L., Baziaka F., Karaiskos I. Effectiveness of a double-carbapenem regimen for infections in humans due to carbapenemase-producing pandrug-resistant Klebsiella pneumoniae. Antimicrob. Agents Chemother. 2013;57:2388–2390. doi: 10.1128/AAC.02399-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oliva A., Cipolla A., Gizzi F., D’Abramo A., Favaro M., De Angelis M., Ferretti G., Russo G., Iannetta M., Mastroianni C.M., et al. Severe Bloodstream Infection due to KPC-Producer E. coli in a renal transplant recipient treated with the double-carbapenem regimen and analysis of in vitro synergy testing: A case report. Medicine. 2016;95:e2243. doi: 10.1097/MD.0000000000002243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Del Barrio-Tofiño E., Zamorano L., Cortes-Lara S., López-Causapé C., Sánchez-Diener I., Cabot G., Bou G., Martínez-Martínez L., Oliver A. Spanish nationwide survey on Pseudomonas aeruginosa antimicrobial resistance mechanisms and epidemiology. J. Antimicrob. Chemother. 2019;74:1825–1835. doi: 10.1093/jac/dkz147. [DOI] [PubMed] [Google Scholar]
- 24.Sabet M., Tarazi Z., Nolan T., Parkinson J., Rubio-Aparicio D., Lomovskaya O., Dudley M.N., Griffith D.C. Activity of meropenem-vaborbactam in mouse models of infection due to KPC-Producing carbapenem-resistant Enterobacteriaceae. Antimicrob. Agents Chemother. 2018;62:e01446-17. doi: 10.1128/AAC.01446-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Song X., Wu Y., Cao L., Yao D., Long M. Is Meropenem as a Monotherapy Truly Incompetent for Meropenem-Nonsusceptible Bacterial Strains? A Pharmacokinetic/Pharmacodynamic Modeling with Monte Carlo Simulation. Front. Microbiol. 2019;10:2777. doi: 10.3389/fmicb.2019.02777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The European Committee on Antimicrobial Susceptibility Testing (EUCAST) Breakpoint Tables for Interpretation of MICs and Zone Diameters, Version 11.0. [(accessed on 31 January 2021)]. Available online: http://www.eucast.org.
- 27.Parra Millán R., Jiménez Mejías M.E., Sánchez Encinales V., Ayerbe Algaba R., Gutiérrez Valencia A., Pachón Ibáñez M.E., Díaz C., Pérez Del Palacio J., López Cortés L.F., Pachón J., et al. Efficacy of lysophosphatidylcholine in combination with antimicrobial agents against Acinetobacter baumannii in experimental murine peritoneal sepsis and pneumonia models. Antimicrob. Agents Chemother. 2016;60:4464–4470. doi: 10.1128/AAC.02708-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vila J., Pachón J. Therapeutic options for Acinetobacter baumannii infections: An update. Expert Opin. Pharmacother. 2012;13:2319–2336. doi: 10.1517/14656566.2012.729820. [DOI] [PubMed] [Google Scholar]
- 29.Oliva A., Scorzolini L., Cipolla A., Mascellino M.T., Cancelli F., Castaldi D., D’Abramo A., D’Agostino C., Russo G., Ciardi M.R., et al. In vitro evaluation of different antimicrobial combinations against carbapenemase-producing Klebsiella pneumoniae: The activity of the double-carbapenem regimen is related to meropenem MIC value. J. Antimicrob. Chemother. 2017;72:1981–1984. doi: 10.1093/jac/dkx084. [DOI] [PubMed] [Google Scholar]
- 30.Fredborg M., Sondergaard T.E., Wang M. Synergistic activities of meropenem double and triple combinations against carbapenemase-producing Enterobacteriaceae. Diagn. Microbiol. Infect. Dis. 2017;88:355–360. doi: 10.1016/j.diagmicrobio.2017.04.015. [DOI] [PubMed] [Google Scholar]
- 31.De Pascale G., Martucci G., Montini L., Panarello G., Cutuli S.L., Di Carlo D., Di Gravio V., Di Stefano R., Capitanio G., Vallecoccia M.S., et al. Double carbapenem as a rescue strategy for the treatment of severe carbapenemase-producing Klebsiella pneumoniae infections: A two-center, matched case-control study. Crit. Care. 2017;21:173. doi: 10.1186/s13054-017-1769-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Galani I., Nafplioti K., Chatzikonstantinou M., Souli M. In vitro evaluation of double-carbapenem combinations against OXA-48-producing Klebsiella pneumoniae isolates using time-kill studies. J. Med. Microbiol. 2018;67:662–668. doi: 10.1099/jmm.0.000725. [DOI] [PubMed] [Google Scholar]
- 33.Nazer L.O., Le J. Critical review of double-Carbapenem therapy for the treatment of Carbapenemase-producing Klebsiella pneumoniae. Ann. Pharmacother. 2019;53:70–81. doi: 10.1177/1060028018790573. [DOI] [PubMed] [Google Scholar]
- 34.White B.P., Patel S., Tsui J., Chastain D.B. Adding double carbapenem therapy to the armamentarium against carbapenem-resistant Enterobacteriaceae bloodstream infections. Infect. Dis. 2019;51:161–167. doi: 10.1080/23744235.2018.1527470. [DOI] [PubMed] [Google Scholar]
- 35.Bulik C.C., Nicolau D.P. Double-carbapenem therapy for carbapenemase-producing Klebsiella pneumoniae. Antimicrob. Agents Chemother. 2011;55:3002–3004. doi: 10.1128/AAC.01420-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hubrecht R.C., Carter E. The 3Rs and Humane Experimental Technique: Implementing Change. Animals. 2019;9:754. doi: 10.3390/ani9100754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mulet X., Fernández-Esgueva M., Norte C., Zamorano L., Del Barrio-Tofiño E., Oliver A. Validation of MALDI-TOF for the early detection of the ST175 high-risk clone of Pseudomonas aeruginosa in clinical isolates belonging to a Spanish nationwide multicenter study. Enferm. Infecc. Microbiol. Clin. 2021;39:279–282. doi: 10.1016/j.eimc.2020.05.022. [DOI] [PubMed] [Google Scholar]
- 38.Bedenić B., Meštrović T. Mechanisms of resistance in gram-negative urinary pathogens: From country-specific molecular insights to global clinical relevance. Diagnostics. 2021;11:800. doi: 10.3390/diagnostics11050800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tenover F.C., Nicolau D.P., Gill C.M. Carbapenemase-producing Pseudomonas aeruginosa—An emerging challenge. Emerg. Microbes Infect. 2022;11:811–814. doi: 10.1080/22221751.2022.2048972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stewart N.K., Smith C.A., Frase H., Black D.J., Vakulenko S.B. Kinetic and structural requirements for carbapenemase activity in GES-type β-lactamases. Biochemistry. 2015;54:588–597. doi: 10.1021/bi501052t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Canut Blasco A., Collazos Blanco A., Díez Aguilar M., Morosini Reilly M.I., Rodríguez-Gascón A., Seral-García C. Métodos Microbiológicos para la Determinación In Vitro de la Actividad de Combinaciones de Antimicrobianos. Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica (SEIMC); Madrid, Spain: 2020. [Google Scholar]
- 42.Pachón-Ibáñez M.E., Labrador-Herrera G., Cebrero-Cangueiro T., Díaz C., Smani Y., Del Palacio J.P., Rodríguez-Baño J., Pascual A., Pachón J., Conejo M.C. Efficacy of colistin and its combination with rifampin in vitro and in experimental models of infection caused by carbapenemase-producing clinical isolates of Klebsiella pneumoniae. Front. Microbiol. 2018;9:912. doi: 10.3389/fmicb.2018.00912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.National Academies Press (NAP) In: Guide for the Care and Use of Laboratory Animals. Committee for the Update of the Guide for the Care and Use of Laboratory Animals; Institute for Laboratory Animal Research; Division on Earth and Life Studies; National Research Council, editor. National Academies Press (NAP); Washington, DC, USA: 2010. [Google Scholar]
- 44.O’Reilly T., Cleeland R., Squires E. Evaluation of antimicrobials in experimental animal infections. In: Lorian V., editor. Antibiotics in Laboratory Medicine. 4th ed. William & Wilkins; New York, NY, USA: 1996. pp. 604–765. [Google Scholar]
- 45.Dinc G., Demiraslan H., Elmali F., Ahmed S.S., Alp E., Doganay M. Antimicrobial efficacy of doripenem and its combinations with sulbactam, amikacin, colistin, tigecycline in experimental sepsis of carbapenem-resistant Acinetobacter baumannii. New Microbiol. 2015;38:67–73. [PubMed] [Google Scholar]
- 46.Bretonnière C., Jacqueline C., Caillon J., Guitton C., Le Mabecque V., Miégeville A.F., Villers D., Potel G., Boutoille D. Efficacy of doripenem in the treatment of Pseudomonas aeruginosa experimental pneumonia versus imipenem and meropenem. J. Antimicrob. Chemother. 2010;65:2423–2427. doi: 10.1093/jac/dkq334. [DOI] [PubMed] [Google Scholar]
- 47.Kim A., Banevicius M.A., Nicolau D.P. In vivo pharmacodynamic profiling of doripenem against Pseudomonas aeruginosa by simulating human exposures. Antimicrob. Agents Chemother. 2008;52:2497–2502. doi: 10.1128/AAC.01252-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.