Abstract
Background
Social isolation, the relative absence of or infrequency of contact with different types of social relationships, and loneliness (perceived isolation) are associated with adverse health outcomes.
Objective
To review observational and intervention research that examines the impact of social isolation and loneliness on cardiovascular and brain health and discuss proposed mechanisms for observed associations.
Methods
We conducted a systematic scoping review of available research. We searched 4 databases, PubMed, PsycInfo, Cumulative Index of Nursing and Allied Health, and Scopus.
Findings
Evidence is most consistent for a direct association between social isolation, loneliness, and coronary heart disease and stroke mortality. However, data on the association between social isolation and loneliness with heart failure, dementia, and cognitive impairment are sparse and less robust. Few studies have empirically tested mediating pathways between social isolation, loneliness, and cardiovascular and brain health outcomes using appropriate methods for explanatory analyses. Notably, the effect estimates are small, and there may be unmeasured confounders of the associations. Research in groups that may be at higher risk or more vulnerable to the effects of social isolation is limited. We did not find any intervention studies that sought to reduce the adverse impact of social isolation or loneliness on cardiovascular or brain health outcomes.
Conclusions
Social isolation and loneliness are common and appear to be independent risk factors for worse cardiovascular and brain health; however, consistency of the associations varies by outcome. There is a need to develop, implement, and test interventions to improve cardiovascular and brain health for individuals who are socially isolated or lonely.
Keywords: AHA Scientific Statements, brain health, cardiovascular health, loneliness, social isolation
Subject Categories: Statements and Guidelines
The role of social isolation, loneliness, and other social determinants in shaping cardiovascular and brain health outcomes is well established. 1 , 2 , 3 , 4 Social isolation is defined as the objective state of having few or infrequent social contacts. 5 Loneliness is perceived isolation that is distressing for the individual. Although related, they are distinct constructs 6 that operate through different pathways and have unique downstream effects on health. Individuals can lead a relatively isolated life and not feel lonely; conversely, individuals with many social contacts may still experience loneliness. Both social isolation and loneliness denote some degree of social disconnection.
Social isolation and loneliness are common, and the risk for social isolation and loneliness appears highest for the young and the old, although for different reasons. Nearly one‐quarter of community‐dwelling Americans ≥65 years of age are socially isolated. 5 Prevalence rates of loneliness are even higher. Estimates from national surveys conducted in 2018 by the Henry J. Kaiser Family Foundation, 7 Association for Advancement of Retired People, 8 and Cigna 9 noted prevalence estimates for loneliness of 22%, 35%, and 47%, respectively. A survey conducted by Cigna described Gen Z (adults 18–22 years) as the loneliest generation, whereas the Greatest Generation (adults ≥72 years of age) were the least lonely or socially isolated compared with middle‐aged adults. 9 Data suggest that social isolation and loneliness may have increased since the start of the COVID‐19 (coronavirus disease 2019) pandemic, particularly among young adults (18–25 years of age), older adults, women, and low‐income individuals. 10 , 11 , 12 It is well known that risk for social isolation increases with age because of life course factors, such as widowhood and retirement. Notable reasons for increased isolation and loneliness among younger adults are greater social media use, less engagement in meaningful in‐person activities, and less experience regulating emotions, so everything is felt more intensely. Moreover, young adulthood is naturally isolating as individuals’ identities are changing and they are learning how to relate to others and their environment. 12
More than 4 decades of research have documented robust evidence that lack of social connection, using measures of social isolation, is associated with increased risk of premature death from all causes, as well as other adverse health outcomes. 3 , 5 Much of this research is summarized in a consensus study by the National Academies of Sciences, Engineering, and Medicine published in February 2020. This study focused on the impact of social isolation and loneliness on the health and well‐being of older adults (≥50 years of age). 5 Although this study includes a brief discussion of the impact of social isolation and loneliness on cardiovascular and brain health, these topics were not the focus of the study, and the impact of social isolation and loneliness in younger populations was not addressed, limiting applicability of this literature to a broader population. It is important to examine the impact of social isolation and loneliness on cardiovascular and brain health because social isolation, which is considered a stressor, has been shown to impact both risk of incident cardiovascular disease (CVD) and cerebrovascular disease, as well as prognosis once disease manifests.
Risk and Protective Factors
Risk and protective factors for social isolation and loneliness have been well described. These include predisposing physical health conditions (eg, chronic illness, functional impairments), psychological and cognitive factors (eg, depression, anxiety), and socioenvironmental factors (eg, transportation, living arrangement, dissatisfaction with family relationships, pandemics, natural disasters). Some of these factors increase the risk for adverse health effects, whereas others lower the risk. In addition, there is a bidirectional relationship between risk factors and social isolation or loneliness. For example, depression may lead to social isolation, and social isolation may make an individual more likely to experience depression.
Certain populations are at higher risk for social isolation and CVD based on sociodemographic characteristics such as race and ethnicity, sexual orientation, gender identity, socioeconomic status, and social status (eg, immigrants, incarcerated individuals), or place of residence (eg, rural and underresourced settings). However, research on health effects of social isolation and loneliness within these special populations is sparse. 5
This statement builds on, yet extends, the National Academies of Sciences, Engineering, and Medicine consensus study and seeks to (1) critically review observational and intervention research that examines direct associations and mediating pathways between social isolation, loneliness, and cardiovascular and brain health and (2) highlight, where available, studies of the impact of social isolation and loneliness on cardiovascular and brain health in special populations.
METHODS
Literature Synthesis
This statement summarizes the available literature related to social isolation (objective and perceived) and cardiovascular and brain health and emphasizes social isolation as a contextual factor of relevance to researchers and clinicians. This statement is not intended to answer a specific research question(s) or to provide evidence to inform clinical decision making; thus, we did not conduct a systematic review or assess risk of bias within the studies. Instead, we conducted a scoping review, one designed to “assess the size and scope of the available research literature and to identify the nature and extent of research evidence” using a structured process. 13 , 14 We searched 4 databases, PubMed, PsycInfo, Cumulative Index of Nursing and Allied Health, and Scopus, for English‐language published research available up to July 2021. To narrow the scope of the review, we focused primarily on studies that examined social isolation as a composite variable, as opposed to using single‐item proxy measures such as living alone or marital status. For screening purposes, we did not limit articles based on study design. The studies presented are a synthesis of the existing literature.
RESULTS
Cardiovascular Health
Incident Coronary Heart Disease
Data on the association between social isolation, loneliness, and risk of incident coronary heart disease (CHD) are inconsistent. Valtorta et al conducted a meta‐analysis of 19 studies using 16 longitudinal data sets (11 CHD and 8 stroke studies) and found that social isolation (n=16 studies) or loneliness (n=3 studies) increased the risk of incident CHD (n=4628 events; pooled relative risk [RR], 1.29 [95% CI, 1.04–1.59]). 4 Most of these studies focused on acute myocardial infarction (MI) and/or CHD death as the measure of CHD.
A study from the United Kingdom (N=479 059; 40–69 years of age) in individuals without CVD at baseline reported that both social isolation (number of people in household, engagement with friends and in social activities) and loneliness (frequency of loneliness and of confiding in a person who is close to the individual) were associated with incident acute MI (hazard ratio [HR], 1.43 [95% CI, 1.3−1.55] and HR, 1.49 [95% CI, 1.36–1.64], respectively) in unadjusted analyses; however, adjustment for conventional biological, behavioral, socioeconomic, psychological, and health‐related risk factors explained most of the excess risk. 15
More recently, Smith et al combined the Million Women and UK Biobank studies (n=938 558) and found that social isolation, based on a composite of living alone, contact with family or friends, and group participation (most versus least), was not associated with incident CHD (RR, 1.01 [95% CI, 0.98–1.04]). 16 Similarly, prospective data from the English Longitudinal Study of Aging found that social isolation was not independently associated with incident CHD or stroke; however, loneliness was independently associated with increased risk. The risk was not mediated by traditional biological CVD risk factors and social isolation (odds ratio [OR], 1.27 [95% CI, 1.01–1.57]). 17
Naito and colleagues examined associations between social isolation and health outcomes in 119 894 community‐dwelling middle‐aged adults (35–70 years of age) from urban and rural communities in 20 high‐, middle‐, and low‐income countries. 18 They found that social isolation (assessed using Berkman‐Syme Social Network Index) was associated with greater risk of incident CVD (HR, 1.15 [95% CI, 1.05–1.25]).
Incident CHD Mortality and All‐Cause Mortality
Smith and colleagues found that a composite score of social isolation is associated with incident CHD death before reaching a hospital (RR, 1.86 [95% CI, 1.64–2.12]). 16 Another study, conducted in an all‐woman sample, found that social isolation (assessed using the simplified Berkman‐Syme Social Network Index) was associated with fatal CHD but not nonfatal MI, after adjusting for demographic factors, medical risk factors, and depressive symptoms. 19 Gronewold and colleagues found that social isolation (assessed using the Berkman‐Syme Social Network Index) was associated with increased cardiovascular events (stroke, MI, or CVD deaths) and all‐cause mortality; however, the association with cardiovascular events was not statistically significant, and the association with all‐cause mortality was explained by behavior, socioeconomic status, and depressive symptoms. 20
Kraav and colleagues found that among middle‐aged Finnish men, social isolation (HR, 1.09 [95% CI, 1.02–1.15]) and loneliness (HR, 1.06 [95% CI, 1.03–1.18]) was associated with greater all‐cause mortality after adjusting for lifestyle, diet, sleep, depression, and inflammation, socioeconomic status, and physiological variables. In this study, loneliness (HR, 1.12 [95% CI, 1.03–1.24]) was also associated with increased CVD mortality (HR, 1.12 [95% CI, 1.01–1.24]), but the association between social isolation and CVD mortality was not significant in the fully adjusted model (HR, 1.06 [95% CI, 0.97–1.16]). Naito and colleagues found that social isolation was associated with higher cardiovascular (HR, 1.30 [95% CI, 1.13–1.50]) and all‐cause (HR, 1.26 [95% CI, 1.17–1.36]) mortality. 18
Prognostic Effects on Prevalent CVD and All‐Cause Mortality
Studies examining prognostic effects of social isolation and loneliness following MI are numerous and compelling. 21 One systematic review found that, among patients with existing CHD, social isolation was associated with a 2‐ to 3‐fold increased morbidity and mortality for up to 6 years, independent of cardiac risk factors. 22 Another systematic review found that low structural support (characteristics of the network and interaction with that network, including size, frequency of contact, marital status, and community membership) was not associated with increased risk of cardiac mortality (RR, 1.56 [95% CI, 0.94–2.58]; n=5) or composite cardiac and all‐cause mortality (RR, 1.12 [95% CI, 0.98–1.29]). 23
Smaller social networks are associated with recurrent cardiovascular events and mortality among patients with significant CHD (RR, 2.43; P=0.001 for cardiac mortality; RR, 2.11; P=0.001 for all‐cause mortality), 20 and patients >65 years of age hospitalized for acute MI (OR, 2.9 [95% CI, 1.2–6.9] for 6‐month mortality). 24 , 25 Yu et al found that among men ≥65 years of age with existing CVD living in Taiwan, social isolation (based on composite of marital status, living alone, frequency of contact with family/friends, and community participation) was associated with increased risk of mortality, even after adjusting for loneliness (HR, 1.16 [95% CI, 1.07–1.27]), whereas loneliness was not associated with increased mortality. 26 Hakulinen and colleagues found that social isolation was associated with higher risk of mortality after acute MI (HR, 1.50 [95% CI, 1.25–1.79]). 15 This association was attenuated by 50% but remained statistically significant after adjusting for biological, behavioral, socioeconomic, depressive symptoms, and health‐related risk factors. 15
Heart Failure
Limited data support a causative association between social isolation and incident heart failure (HF). 27 , 28 Using longitudinal data from the Atherosclerosis Risk in Communities Study 27 and the Women’s Health Initiative study, 28 Cené and colleagues demonstrated that social isolation (assessed using adapted versions of the Berkman‐Syme Social Network Index) increased the risk of HF hospitalization in individuals free of CVD at baseline by 21% and 23%, respectively, after adjusting for traditional CVD risk factors. Conversely, Rod and colleagues found no association between structural aspects of social networks (based on living alone and regular contact with family and friends) and incident HF hospitalization. 29 This may be attributable to differences in study population (US samples versus Danish sample) and social network measurement. Notably, Naito and colleagues did not find an association between social isolation and incident HF (HR, 1.28 [95% CI, 0.98–1.50]). 18
As prognostic indicators in patients with HF, social isolation, living alone, and suboptimal social networks have been shown to increase the risk for HF‐related hospital readmissions. 30 The Waiting for a New Heart Study found that those with social isolation (<4 social contacts/month) and clinical depression (versus those with >10 social contacts/month without depression) were more likely to die or deteriorate while waiting for a heart transplant over 12 months. 31 Five‐year survival rates were 60% for patients who were socially isolated and 62% for those who were both socially isolated and clinically depressed, compared with 79% for those with more social contacts without depression. 31
SOCIAL ISOLATION, LONELINESS, AND BRAIN HEALTH
A growing body of literature supports associations between social isolation, loneliness, incident stroke, and other measures of brain health.
Incident Stroke
A meta‐analysis 4 and several large population‐based cohorts 15 , 18 , 32 have noted an increased risk of incident stroke with social isolation and loneliness. In a meta‐analysis of 8 longitudinal observational studies, social isolation and loneliness were associated with a 32% increased risk of incident stroke (RR, 1.32 [95% CI. 1.04–1.68]) after adjustment for age, sex, and socioeconomic position. 4
Among participants of the UK Biobank study (N=479 054), social isolation, assessed using a 3‐item instrument measuring living situation, frequency of visits, and types of social engagement, was associated with a significantly increased risk of incident stroke (HR, 1.39 [95% CI, 1.25–1.54]). 15 However, the association was attenuated and no longer significant after adjusting for cardiovascular risk factors, health behaviors, socioeconomic position, and depressive symptoms. Similarly, the positive association between loneliness and incident stroke (HR, 1.36 [95% CI, 1.20–1.55]) was reduced and no longer statistically significant in the adjusted models. 15
Recurrent Stroke
Although data are sparse, social isolation and loneliness are associated with an increased risk of recurrent stroke and mortality. Among participants of the Northern Manhattan Stroke Study, a multiracial and multiethnic population‐based sample, socially isolated (eg, <3 versus ≥3 social connections) adults had a 40% increased risk of recurrent stroke, MI, or mortality (HR, 1.40 [95% CI, 1.1–1.8]) when adjusted for age, race and ethnicity, atrial fibrillation, and requiring help at home. 33 Notably, stroke severity 48 hours after the event did not vary significantly by categories of social connectedness. Because of study heterogeneity, strength of the associations between social isolation and loneliness with stroke are uncertain. However, it should be noted that robust data from animal models document detrimental health effects of social isolation and support an important role of social interaction in promoting stroke recovery. 34 , 35 , 36
Dementia
We did not find any studies that examined associations between social isolation, loneliness, and vascular dementia. Although several studies have examined the association between loneliness, social isolation, and Alzheimer dementia, disparate findings have been reported for each construct. Two meta‐analyses examined the association between loneliness and dementia. 2 , 37 One reported a 26% increased risk of dementia (RR, 1.26 [95% CI, 1.11–1.39]), 37 whereas another reported a statistically nonsignificant increased risk of dementia (RR, 1.38 [95% CI, 0.98–1.94]). 2 It is important to consider that social withdrawal may precede the manifestations of dementia and could confound results.
Several studies have also reported an increased risk of incident Alzheimer dementia with loneliness, but not with social isolation. 38 , 39 , 40 For example, among participants in the China Health and Retirement Longitudinal Study (OR, 1.31 [95% CI, 1.11–1.56]) 39 and older adults in the Netherlands (OR, 1.64 [95% CI, 1.05–2.56]), 40 loneliness but not social isolation was significantly associated with risk of dementia. These data underscore the fact that social isolation and loneliness are distinct constructs with independent associations with brain health.
Cognitive Impairment
Data examining associations between loneliness or social isolation with cognitive impairment are sparse and mixed, with some studies demonstrating positive associations with either social isolation or loneliness, 37 , 41 , 42 whereas others have not observed an association. 43 Data from the ELSA (English Longitudinal Study of Ageing), a longitudinal panel study in adults ≥50 years of age, suggest a positive association between loneliness and incident dementia and cognitive decline, which may be bidirectional. 42 Similarly, Barnes et al found that social integration (less social isolation) reduces the rate of cognitive decline over an average of 5.3 years in a sample of >6000 Black Americans (61%) and White Americans ≥65 years of age. 44
MEDIATORS: BEHAVIORAL, PSYCHOLOGICAL, AND PHYSIOLOGICAL PATHWAYS
We sought to understand mediators (mechanisms or pathways) by which social isolation or loneliness influence cardiovascular and brain health. To be a mediator, or an intermediate, a variable must be a step in the pathway between exposure and outcome. In this section, we review literature examining the association between the exposures (social isolation and loneliness) and potential mediators. In 2020, the Royal Society of Medicine in the United Kingdom published a literature synthesis and conceptual framework on the mechanisms linking loneliness, social isolation, CVD, and mortality. 45 This framework proposes that social isolation and loneliness impact cardiovascular and brain health through multiple and divergent pathways, including behavioral, psychological, and physiological effects. Guided by this conceptual framework, we highlight literature examining associations between potential mediators and social isolation and loneliness (Figure).
Figure 1. Conceptual model examining associations between social isolation, loneliness, and outcomes.
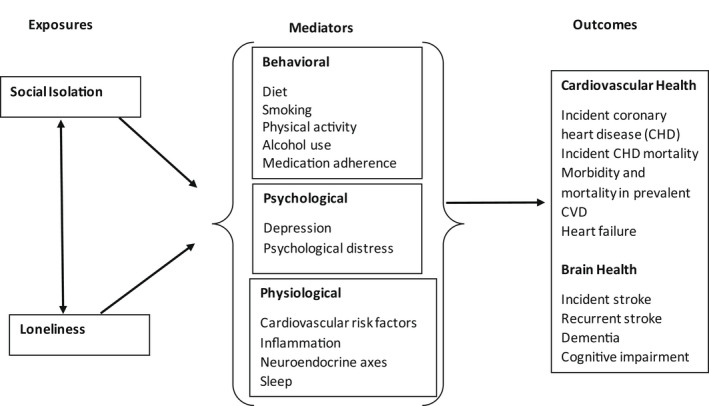
CHD indicates coronary heart disease; and CVD, cardiovascular disease. Adapted from Hodgson et al. 45 Copyright 2020 The Authors. Published on behalf of the Royal Society of Medicine by Sage Publishing. This is an open access article under the terms of the Creative Commons Attribution‐By Author License, which permits use, distribution, and reproduction in any medium, provided the original work is properly cited.
Behavioral Factors
Behavioral risk factors for CVD, such as smoking, physical inactivity or sedentary behavior, diet, and sleep have been examined for their relation with social isolation and loneliness with mixed findings. 3 , 46 Several studies, including 3 systematic reviews, 47 , 48 , 49 examined the relationship between loneliness and tobacco use. 3 In a systematic review, 13 of 25 studies documented positive associations between loneliness and smoking behaviors; the majority of studies that relied on large nationally representative populations noted significant positive associations. 47 Among participants of ELSA, greater isolation (based on a social isolation index including marital/cohabitating status, frequency of contact with family and friends, and participation in organizations/groups) was associated with lower levels of self‐reported physical activity and fruit and vegetable intake 50 and greater sedentary time, based on objectively measured physical activity; however, no association was noted for loneliness (University of California Los Angeles Loneliness Scale). 49 In a multiethnic longitudinal study of men and women (N=229), Hawkley and colleagues found that loneliness was associated with a reduced odds of physical activity over time and greater likelihood of transitioning from being physically active to inactive. 51
Associations between social isolation and loneliness and alcohol use have also been examined; however, findings are mixed, suggesting that population age and alcohol use assessment may influence associations. For example, a study among adolescents noted positive associations between loneliness and unhealthy alcohol use, 52 whereas a study among older adults noted experiencing loneliness (University of California Los Angeles Loneliness Scale 53 ) was associated with lower alcohol consumption. 54 In addition, several cross‐sectional studies have reported equivocal data on the association between social isolation, loneliness, and obesity; however, longitudinal data explicitly examining social isolation and loneliness as predictors of obesity are lacking. 55 Other behavioral factors, such as medication adherence and health care use, may also be important mediators between social isolation, loneliness, and CVD 5 ; however, further longitudinal data are needed to identify the temporal sequence and assess the magnitude of their contribution. Health‐related behaviors and psychological factors (eg, depression) can in turn influence social isolation loneliness, it is important to consider that social isolation and loneliness may be markers rather than causes. Additional analyses are needed to disentangle potential reverse causality (in which deficiencies in social relationships are the result of subclinical disease) and synergistic effects.
Psychological Factors
Psychological factors, such as depression, have also been associated with both loneliness and social isolation; however, associations with loneliness may be stronger. Data from 2 population‐based studies of adults showed that loneliness (assessed by the University of California Los Angeles Loneliness Scale and the 4‐item Seeman and Syme Loneliness Scale) was significantly associated with depressive symptoms (β, 0.33–0.44; P<0.05) in multivariable analyses adjusted for demographic factors, behavioral factors, and medical history. 56 , 57 However, in these same studies, multivariable association between social isolation and depressive symptoms was weak (β, −0.11 to −0.07; P<0.05); both studies used the Lubben Social Network Scale 58 to assess social isolation.
Cross‐sectional data from the Swiss Health Survey (N=20 007) suggest that loneliness is associated with moderate and high psychological distress, depressive symptoms, and impaired self‐perceived health. 46 In another study, depressive symptoms and physical activity largely explained the association between loneliness and all‐cause and CVD mortality. 59 Notably, social isolation and depressive symptoms tend to cluster in the prognostic literature. One study of 292 women with established CHD found that patients with social isolation (condensed version of the Interview Schedule for Social Interaction) and depressive symptoms, compared with those with neither, were more likely to have recurrent CHD (cardiovascular death, recurrent acute MI, or revascularization) independent of cardiac risk factors. 60
Physiological Factors (Response to Stress, Allostatic Load, Inflammatory)
Data on the impact of social isolation or loneliness on biomarkers of cardiovascular health are limited and may vary by individual biomarkers. A recent systematic review and meta‐analysis examined the association between loneliness, social isolation, and inflammatory biomarkers. 61 Although 14 studies on loneliness and 16 studies on social isolation were identified in this review, each varied in the biomarkers assessed, limiting the robustness of pooled estimates. Overall, loneliness demonstrated a significant positive correlation with IL‐6 (interleukin‐6) but not CRP (C‐reactive protein) or fibrinogen. In contrast, social isolation demonstrated a significant positive correlation with CRP and fibrinogen, but not IL‐6. 61 Few studies have examined the longitudinal relationship between loneliness and social isolation with biomarkers of cardiovascular risk, and results have been inconsistent. 62 , 63 Social isolation (composite of marital status, contact with friends/family, religious affiliation, and religious/community participation) has been associated with both elevated CRP levels and CHD mortality, although individual measures within the social isolation composite were not statistically significant, suggesting an additive or composite effect of indicators of social integration. 64 Several studies noted that loneliness was associated with short sleep duration and poor sleep quality among adults. 56 , 65
High‐quality evidence from multiple systematic reviews demonstrates a negative association between social connectedness and allostatic load 66 or the wear and tear on the body accumulated through repeated exposure to chronic stress. Measures of allostatic load include neuroendocrine and cardiovascular biomarkers, as well as inflammatory markers. Data from a review of multiple studies clearly demonstrate that the more socially connected individuals are, the less likely they are to experience physiological manifestation of chronic stress, known as allostatic load. Socioeconomic status and the quality of social connections are important moderators of this association. 66 Meanwhile, single studies suggest that marital status (a proxy for social isolation), specifically being widowed or single, may be independently associated with coronary artery calcium scores. 67
In summary, studies explicitly testing mediating pathways between social isolation, loneliness, and CVD are sparse and equivocal. 18 , 45 , 68 Most studies do not use path analysis or causal mediation methods that are more appropriate than standard regression techniques for examining explanatory pathways. 69 This gap is important because it is not possible to control for confounding of the exposure‐mediator association, as well as the exposure‐outcome directly using standard regression‐based mediation analyses. 70 Of the studies we reviewed, a study found, using standard regression techniques, that unhealthy behaviors and comorbidities mediate 21% of the association between social isolation and mortality. 18 In addition, some of the potential mediators, such as health‐related behaviors and depression, could also be confounders, and there may be unmeasured confounders that are associated with both the exposure and the outcome. These unmeasured confounders could result in a spurious association between social isolation or loneliness and our outcomes of interest.
SPECIAL POPULATIONS WITH INCREASED VULNERABILITY
Risks for CVD and cerebrovascular disease and social isolation and loneliness are not consistent across populations. 71 Multiple factors may place individuals at risk for social isolation (objective or perceived) and may moderate the association between social isolation, loneliness, and cardiovascular and brain health outcomes. Because of space constraints and limited empiric data on effect moderators, we limited our discussion to age, socioeconomic status, and sex. Some data have documented a higher prevalence of social isolation and loneliness among lesbian, gay, bisexual, transgender, and queer older adults, 72 , 73 but these studies did not evaluate associations with cardiovascular or brain health. Similarly, we did not identify any studies of social isolation or loneliness and cardiovascular or brain health that specifically examined the role of race and ethnicity (a proxy for structural racism 74 or culture).
Children and Youth
A few studies have examined childhood social isolation and cardiovascular risk factors during adulthood. 75 , 76 These studies have found that childhood social isolation (socially isolated versus low levels of social isolation) is associated with cardiovascular risk factors such as overweight, hypertension, hemoglobin A1c levels, and CRP. Using data from the National Child Development Study in Great Britain, Lacey and colleagues examined the association between child (7–11 years of age) social isolation, assessed using social rejection and withdrawal questions, and levels of CRP in middle age (44 years of age). 77 The study found that socially isolated youth had higher CRP levels in midlife (standardized coefficient, 0.05; P<0.001) compared with those with lower social isolation scores, an increase deemed clinically significant. These youth had more psychological distress, less educational/career attainments, and worse health behaviors (obesity, smoking) across adulthood; health behaviors and adult body mass index seemed to explain most of the variance in CRP levels. Notably, in this study, adult social isolation was defined by having <3 sources of emotional or practical support, thus conflating social isolation with social support.
Income
Socioeconomically disadvantaged groups may be especially prone to social isolation. At least 1 prospective cohort study in a sample of 4888 Irish adults ≥50 years of age examined social connectedness (Berkman‐Syme Social Network Index 78 ) and loneliness (University of California Los Angeles Loneliness Scale) as mediators of the social gradient in resting heart rate, a key risk factor for CVD mortality. 79 This study found that lower income was associated with higher loneliness and less social connectedness (eg, greater social isolation), and individuals from more socially disadvantaged backgrounds had significantly higher resting heart rates compared with socially advantaged adults. Moreover, the magnitude of the socioeconomic differential was greater for men than women. 79 In a study that examined data from low‐, middle‐, and high‐income countries, the positive association between social isolation and all‐cause mortality was greatest in younger adults and men. 18
Sex
Few studies have examined sex differences in the risk of social isolation or loneliness on CVD or brain health outcomes. In 1 study, the association between social isolation (assessed using the Berkman‐Syme Social Network Index) and all‐cause mortality was stronger in men than women. 20 Another study had similar results, showing that low social contacts (based on small social network size and not being married or cohabitating) was significantly associated with increased all‐cause and cardiovascular mortality in men but not in women. 80 However, the meta‐analysis of 19 studies by Valtorta et al did not find any subgroup differences by sex. 4
SUMMARY AND LIMITATIONS OF OBSERVATIONAL LITERATURE
Despite the breadth of literature for cardiovascular outcomes, data on the association between social isolation and loneliness and various cardiovascular and brain health outcomes are mixed but suggest that social isolation and loneliness increase risk for and worsen outcomes in cardiovascular and brain health. Even where associations were found, after adjusting for factors that are presumed to be on the causal pathway, the effect sizes are on the order of 1 to 1.5, which is comparable to recognized psychosocial factors, including depression and anxiety. 81 , 82 Observed effects may be attributable to residual confounding from incomplete measurement of potentially confounding or mediating factors. Although the effect sizes are considered small, the population health impact is still large, given the prevalence of social isolation and loneliness in the population. Moreover, the effects may be underestimated because of underrepresentation or loss to follow‐up in longitudinal studies of individuals and groups who may be at higher risk for both social isolation and CVD, such as individuals from underrepresented racial and ethnic groups; individuals with multiple chronic conditions (including physical and visual impairments); and those with lower levels of education, income, wealth, or social status (eg, immigrants, incarcerated individuals).
There are notable limitations of the observational literature in this body of research. It is unclear which (social isolation or loneliness) matters most for cardiovascular and brain health, 5 because only a few studies 4 , 17 have examined both in the same sample. One study found that loneliness was more important when assessing disease risk, 17 whereas other studies showed no significant difference between social isolation and loneliness. 4 Few studies assess social isolation and loneliness at multiple time points and examine associations in a time‐varying way. This gap is important because social isolation and loneliness can be episodic or chronic. 5 Finally, most of the studies did not present or explicate a conceptual causal model to guide their selection of variables, including proposed mediators and moderators.
INTERVENTIONS
Despite robust observational literature, we did not identify any intervention studies that sought to mitigate the adverse impact of social isolation or loneliness on cardiovascular or brain health specifically. Therefore, we focus this section on interventions that have primarily aimed to reduce social isolation and loneliness among older adults (irrespective of intervention outcome). 83 , 84 , 85 A review conducted by Cohen‐Mansfield and Perach 86 concluded that there was no solid evidence of efficacy of the interventions for older community‐dwelling adults, highlighting the preliminary state of the science and the need for rigorous studies.
A recent scoping review of 33 published reviews summarized findings from interventions to reduce social isolation (n=4), loneliness (n=11), and both loneliness and social isolation (n=13) among older adults. 85 The remaining 5 reviews focused on loneliness and other outcomes such as anxiety and depression (n=3) or social participation and social connectedness (n=2). Of interventions to reduce social isolation, physical activity interventions (eg, resistance exercise, walking, stretching) show the most promise in older adults. 84 A meta‐analysis found that interventions for loneliness that address maladaptive social cognition, negative thoughts of self‐worth, and other people’s perception of the individual rather than interventions involving strengthening social support or increasing social interactions, have been the most successful. 87
Despite suggestions that technology may be a promising strategy to mitigate social isolation and loneliness, evidence is mixed. A review of systematic reviews of internet/computer e‐interventions to reduce loneliness in older adults living in residential settings or nursing homes found insufficient support for any impact on loneliness. 88 This review confirmed the poor quality of evidence, largely driven by study designs unable to determine causation. A recent Cochrane review also found little evidence for the effectiveness of video call interventions to reduce loneliness in older adults. 89 In contrast, in another review of interventions to reduce loneliness and social isolation, 90 results were mixed, with some, but not all, reporting significant improvement in loneliness or social isolation. Interventions (eg, fitness programs, recreational activity) implemented within complex programs (eg, senior center programs), technology interventions (eg, computer use, interaction with companion robots), and incorporating various approaches appeared most successful. However, most of the studies had poor‐quality designs with significant threats to internal validity, including selection bias. 90
Gardiner and associates 91 conducted an integrative review of 39 studies using a wide range of research designs to identify the scope of interventions that target social isolation and loneliness among older adults. However, they reported that most interventions included multiple intervention components, making it unclear which mechanism reduced social isolation or loneliness. Nonetheless, 3 keys to success included interventions that (1) were adapted to the local context, (2) used a community development approach with service users involved in the design, and (3) included productive engagement of the participants. 91 Overall, characteristics of the most effective interventions include specific targeting of socially isolated individuals, a multisystemic approach, active participation of older adults, and having a sound theoretical basis. 5 There are several key limitations of extant literature, including:
Lack of conceptual clarity and standardization: Many studies fail to differentiate loneliness and social isolation or specify the hypothesized mediators or mechanisms of action (for intervention studies). O’Rourke and colleagues summarized the nature of strategies and interventions in 44 studies designed to affect loneliness/social connectedness in older adults as opposed to determining intervention efficacy. 92 They grouped interventions according to their active ingredient, not their mode of delivery. These active ingredients included development of one’s structural social network, social participation, feeling cared for, personal development, personal contact, and social support. They found inconsistency in the mechanisms by which the interventions were thought to affect loneliness/social connectedness. 92 Most interventions were complex (multicomponent) and relied on >1 mechanism for reducing social isolation and loneliness, making it unclear which component contributed to intervention effectiveness. 91 One narrative review of 40 systematic reviews, 47 nonsystematic reviews, and 3 meta‐analyses identified 62 different self‐report questionnaires that were used to measure loneliness, social isolation, and related concepts. 3 This lack of standardization and poor research designs continues to be a major limitation in this field.
Confusing categorization for interventions: Terminology used to categorize interventions were wide ranging, such as: format, 87 delivery mode, 87 , 90 , 93 goal, 94 type, 86 , 87 , 90 , 93 focus, 86 and nature, 94 and often the same terms had different meanings. Some authors used 2 or more categorization systems (eg, delivery mode and type). 86 , 87 , 90 , 93 , 94 Gardiner et al used a thematic synthesis to categorize interventions based on their purpose, mechanisms of action, and intended outcomes to determine the effective intervention components. 91 The categories of interventions included: social facilitation, psychological therapies, health and social care provision, animal interventions, befriending interventions, and leisure/skills development.
Poor study designs: Published reviews of interventions to alleviate loneliness and social isolation note the poor quality of the evidence 85 , 87 , 88 , 91 , 93 , 95 , 96 because of heterogeneous definitions and measurement of social isolation and loneliness, limited age ranges (mostly older adults) with small study samples, and limited follow‐up. Few intervention trials use a randomized design, and therefore causality cannot be assessed, biases cannot be accounted for, and only broad generalizations of effective intervention characteristics are possible.
CONCLUSIONS
Social isolation and loneliness are common, yet underrecognized determinants of cardiovascular health and brain health. Overall, findings suggest an increased risk of worse outcomes among individuals with prevalent CHD and stroke in those who are also socially isolated or lonely; however, these studies do not suggest causality, and associations may be mediated by other factors that need to be further tested in intervention trials. Data on the association of social isolation and loneliness with incident CHD, heart failure, dementia, and cognitive impairment are sparse and mixed. No published interventions have been tested to mitigate the adverse impact of social isolation and loneliness on cardiovascular and brain health, thus making it difficult to identify implications for future clinical practice. Although recommended by the Institute of Medicine 97 that data on social isolation and loneliness be included in electronic health records, this practice is still evolving and not widely adopted.
SUGGESTIONS FOR FUTURE RESEARCH
Several gaps are most relevant to primary or secondary prevention of CVD and cerebrovascular disease and form the basis of our future suggestions. Understanding the independent effects of social isolation and loneliness on cardiovascular and brain health in vulnerable populations and intervening to reduce social isolation and loneliness could help to advance health equity, an American Heart Association 2024 impact goal. 98 The Table highlights 5 key areas for future research.
Table 1.
Top 5 Suggestions for Future Research
|
CHD indicates coronary heart disease; and COVID‐19, coronavirus disease 2019.
Disclosures
Writing Group Disclosures
| Writing group member | Employment | Research grant | Other research support | Speakers’ bureau/honoraria | Expert witness | Ownership interest | Consultant/advisory board | Other |
|---|---|---|---|---|---|---|---|---|
| Crystal W. Cené | University of California San Diego Health and University of California San Diego School of Medicine | None | None | None | None | None | None | None |
| Theresa M. Beckie | University of South Florida College of Nursing/College of Medicine | None | None | None | None | None | None | None |
| Brooke Aggarwal | Columbia University, Irving Medical Center | American Heart Association (PI of a research grant)† | None | None | None | None | None | None |
| Bamba Gaye | INSERM, Paris Cardiovascular Research Center (France) | None | None | None | None | None | None | None |
| Monik C. Jiménez | Brigham and Women’s Hospital | None | None | None | None | None | None | None |
| Louise D. McCullough | The University of Texas Health Science Center at Houston | American Heart Association*; National Institutes of Health (Javits Award on Social Isolation)† | None | None | None | None | None | None |
| Nathalie Moise | Columbia University Medical Center | None | None | None | None | None | None | None |
| Mario Sims | University of Mississippi Medical Center | None | None | None | None | None | None | None |
| Shakira F. Suglia | Emory University Rollins School of Public Health | NIMHD (PI)†; NIA (PI)† | None | None | None | None | None | None |
This table represents the relationships of writing group members that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all members of the writing group are required to complete and submit. A relationship is considered to be significant if (1) the person receives $10 000 or more during any 12‐month period, or 5% or more of the person’s gross income; or (2) the person owns 5% or more of the voting stock or share of the entity, or owns $10 000 or more of the fair market value of the entity. A relationship is considered to be modest if it is less than significant under the preceding definition.
Modest.
Significant.
Reviewer Disclosures
| Reviewer | Employment | Research grant | Other research support | Speakers’ bureau/honoraria | Expert witness | Ownership interest | Consultant/advisory board | Other |
|---|---|---|---|---|---|---|---|---|
| Nada El Husseini | Duke University Medical Center | None | None | None | None | None | None | None |
| Randi Foraker | Washington University in St. Louis, School of Medicine | None | None | None | None | None | None | None |
| Bernhard Haring | Saarland University Hospital (Germany) | None | None | None | None | None | None | None |
| Deepika Laddu | University of Illinois at Chicago | None | None | None | None | None | None | None |
This table represents the relationships of reviewers that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all reviewers are required to complete and submit. A relationship is considered to be significant if (1) the person receives $10 000 or more during any 12‐month period, or 5% or more of the person’s gross income; or (2) the person owns 5% or more of the voting stock or share of the entity, or owns $10 000 or more of the fair market value of the entity. A relationship is considered to be modest if it is less than significant under the preceding definition.
The American Heart Association makes every effort to avoid any actual or potential conflicts of interest that may arise as a result of an outside relationship or a personal, professional, or business interest of a member of the writing panel. Specifically, all members of the writing group are required to complete and submit a Disclosure Questionnaire showing all such relationships that might be perceived as real or potential conflicts of interest.
This statement was approved by the American Heart Association Science Advisory and Coordinating Committee on March 8, 2022, and the American Heart Association Executive Committee on April 11, 2022. A copy of the document is available at https://professional.heart.org/statements by using either Search for Guidelines & Statements or the Browse by Topic area.
The American Heart Association requests that this document be cited as follows: Cené CW, Beckie TM, Sims M, Suglia SF, Aggarwal B, Moise N, Jiménez MC, Gaye B, McCullough LD; on behalf of the American Heart Association Social Determinants of Health Committee of the Council on Epidemiology and Prevention and Council on Quality of Care and Outcomes Research; Prevention Science Committee of the Council on Epidemiology and Prevention and Council on Cardiovascular and Stroke Nursing; Council on Arteriosclerosis, Thrombosis and Vascular Biology; and Stroke Council. Effects of objective and perceived social isolation on cardiovascular and brain health: a scientific statement from the American Heart Association. J Am Heart Assoc. 2022;11:e026493. doi: 10.1161/JAHA.122.026493
The expert peer review of American Heart Association–commissioned documents (eg, scientific statements, clinical practice guidelines, systematic reviews) is conducted by the American Heart Association Office of Science Operations. For more on American Heart Association statements and guidelines development, visit https://professional.heart.org/statements. Select the Guidelines & Statements drop‐down menu, then click Publication Development.
References
- 1. Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz‐Flores S, Davey‐Smith G, Dennison‐Himmelfarb CR, Lauer MS, Lockwood DW, et al; on behalf of the American Heart Association Council on Quality of Care and Outcomes Research, Council on Epidemiology and Prevention, Council on Cardiovascular and Stroke Nursing, Council on Lifestyle and Cardiometabolic Health, and Stroke Council. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–898. doi: 10.1161/CIR.0000000000000228 [DOI] [PubMed] [Google Scholar]
- 2. Penninkilampi R, Casey AN, Singh MF, Brodaty H. The association between social engagement, loneliness, and risk of dementia: a systematic review and meta‐analysis. J Alzheimers Dis. 2018;66:1619–1633. doi: 10.3233/JAD-180439 [DOI] [PubMed] [Google Scholar]
- 3. Leigh‐Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, Caan W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035 [DOI] [PubMed] [Google Scholar]
- 4. Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta‐analysis of longitudinal observational studies. Heart. 2016;102:1009–1016. doi: 10.1136/heartjnl-2015-308790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. National Academy of Sciences Engineering and Medicine . Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. The National Academies Press; 2020. [PubMed] [Google Scholar]
- 6. Petersen J, Kaye J, Jacobs PG, Quinones A, Dodge H, Arnold A, Thielke S. Longitudinal relationship between loneliness and social isolation in older adults: results from the Cardiovascular Health Study. J Aging Health. 2016;28:775–795. doi: 10.1177/0898264315611664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. DiJulio B, Hamel L, Muñana C, Brodie M. Loneliness and social isolation in the United States, the United Kingdom, and Japan: an international survey. The Economist & Kaiser Family Foundation. 2018. Accessed November 19, 2021. https://files.kff.org/attachment/Report‐Loneliness‐and‐Social‐Isolation‐in‐the‐United‐States‐the‐United‐Kingdom‐and‐Japan‐An‐International‐Survey
- 8. Anderson GO, Thayer CE. Loneliness and social connections: a national survey of adults 45 and older. AARP Foundation; 2018. doi: 10.26419/res.00246.001.pdf. Accessed November 19, 2021. https://www.aarp.org/content/dam/aarp/research/surveys_statistics/general/2012/loneliness‐2010 [DOI]
- 9. Nemecek D. Cigna US Loneliness Index: survey of 20,000 Americans examining behaviors driving loneliness in the United States. Cigna[Google Scholar]. 2018. Accessed November 19, 2021. https://www.multivu.com/players/English/8294451‐cigna‐us‐loneliness‐survey/docs/IndexReport_1524069371598‐173525450.pdf
- 10. Smith ML, Steinman LE, Casey E. Combatting social isolation among older adults in a time of physical distancing: the COVID‐19 social connectivity paradox. Front Public Health. 2020;8:403. doi: 10.3389/fpubh.2020.00403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. AARP . The pandemic effect: a social isolation report. October 6, 2020. Accessed November 19, 2021. https://connect2affect.org/wp‐content/uploads/2020/10/The‐Pandemic‐Effect‐A‐Social‐Isolation‐Report‐AARP‐Foundation.pdf
- 12. Weissbourd RBM, Lovison V, Torres E. Loneliness in America: how the pandemic has deepened an epidemic of loneliness and what we can do about it. 1–13. Accessed November 19, 2021. https://static1.squarespace.com/static/5b7c56e255b02c683659fe43/t/6021776bdd04957c4557c212/1612805995893/Loneliness+in+America+2021_02_08_FINAL.pdf
- 13. Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26:91–108. doi: 10.1111/j.1471-1842.2009.00848.x [DOI] [PubMed] [Google Scholar]
- 14. Munn Z, Peters MD, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:1–7. doi: 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hakulinen C, Pulkki‐Raback L, Virtanen M, Jokela M, Kivimaki M, Elovainio M. Social isolation and loneliness as risk factors for myocardial infarction, stroke and mortality: UK Biobank cohort study of 479 054 men and women. Heart. 2018;104:1536–1542. doi: 10.1136/heartjnl-2017-312663 [DOI] [PubMed] [Google Scholar]
- 16. Smith RW, Barnes I, Green J, Reeves GK, Beral V, Floud S. Social isolation and risk of heart disease and stroke: analysis of two large UK prospective studies. Lancet Public Health. 2021;6:e232–e239. doi: 10.1016/S2468-2667(20)30291-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Valtorta NK, Kanaan M, Gilbody S, Hanratty B. Loneliness, social isolation and risk of cardiovascular disease in the English Longitudinal Study of Ageing. Eur J Prev Cardiol. 2018;25:1387–1396. doi: 10.1177/2047487318792696 [DOI] [PubMed] [Google Scholar]
- 18. Naito R, Leong DP, Bangdiwala SI, McKee M, Subramanian SV, Rangarajan S, Islam S, Avezum A, Yeates KE, Lear SA, et al. Impact of social isolation on mortality and morbidity in 20 high‐income, middle‐income and low‐income countries in five continents. BMJ Glob Health. 2021;6:e004124. doi: 10.1136/bmjgh-2020-004124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chang S‐C, Glymour M, Cornelis M, Walter S, Rimm EB, Tchetgen Tchetgen E, Kawachi I, Kubzansky LD. Social integration and reduced risk of coronary heart disease in women: the role of lifestyle behaviors. Circ Res. 2017;120:1927–1937. doi: 10.1161/CIRCRESAHA.116.309443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gronewold J, Kropp R, Lehmann N, Schmidt B, Weyers S, Siegrist J, Dragano N, Jöckel K‐H, Erbel R, Hermann DM. Association of social relationships with incident cardiovascular events and all‐cause mortality. Heart. 2020;106:1317–1323. doi: 10.1136/heartjnl-2019-316250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Glozier N, Tofler GH, Colquhoun DM, Bunker SJ, Clarke DM, Hare DL, Hickie IB, Tatoulis J, Thompson DR, Wilson A, et al. Psychosocial risk factors for coronary heart disease. Med J Aust. 2013;199:179–180. doi: 10.5694/mja13.10440 [DOI] [PubMed] [Google Scholar]
- 22. Mookadam F, Arthur HM. Social support and its relationship to morbidity and mortality after acute myocardial infarction: systematic overview. Arch Intern Med. 2004;164:1514–1518. doi: 10.1001/archinte.164.14.1514 [DOI] [PubMed] [Google Scholar]
- 23. Barth J, Schneider S, von Kanel R. Lack of social support in the etiology and the prognosis of coronary heart disease: a systematic review and meta‐analysis. Psychosom Med. 2010;72:229–238. doi: 10.1097/PSY.0b013e3181d01611 [DOI] [PubMed] [Google Scholar]
- 24. Brummett BH, Barefoot JC, Siegler IC, Clapp‐Channing NE, Lytle BL, Bosworth HB, Williams RB Jr, Mark DB. Characteristics of socially isolated patients with coronary artery disease who are at elevated risk for mortality. Psychosom Med. 2001;63:267–272. doi: 10.1097/00006842-200103000-00010 [DOI] [PubMed] [Google Scholar]
- 25. Berkman LF, Leo‐Summers L, Horwitz RI. Emotional support and survival after myocardial infarction. A prospective, population‐based study of the elderly. Ann Intern Med. 1992;117:1003–1009. doi: 10.7326/0003-4819-117-12-1003 [DOI] [PubMed] [Google Scholar]
- 26. Yu B, Steptoe A, Chen L‐J, Chen Y‐H, Lin C‐H, Ku P‐W. Social isolation, loneliness, and all‐cause mortality in patients with cardiovascular disease: a 10‐year follow‐up study. Psychosom Med. 2020;82:208–214. doi: 10.1097/PSY.0000000000000777 [DOI] [PubMed] [Google Scholar]
- 27. Cene CW, Loehr L, Lin FC, Hammond WP, Foraker RE, Rose K, Mosley T, Corbie‐Smith G. Social isolation, vital exhaustion, and incident heart failure: findings from the Atherosclerosis Risk in Communities Study. Eur J Heart Fail. 2012;14:748–753. doi: 10.1093/eurjhf/hfs064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cené CW, Leng XI, Faraz K, Allison M, Breathett K, Bird C, Coday M, Corbie‐Smith G, Foraker R, Ijioma NN, et al. Social isolation and incident heart failure hospitalization in older women: Women’s Health Initiative Study Findings. J Am Heart Assoc. 2022;11:e022907. doi: 10.1161/JAHA.120.022907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rod NH, Andersen I, Prescott E. Psychosocial risk factors and heart failure hospitalization: a prospective cohort study. Am J Epidemiol. 2011;174:672–680. doi: 10.1093/aje/kwr144 [DOI] [PubMed] [Google Scholar]
- 30. Heidari Gorji MA, Fatahian A, Farsavian A. The impact of perceived and objective social isolation on hospital readmission in patients with heart failure: a systematic review and meta‐analysis of observational studies. Gen Hosp Psychiatry. 2019;60:27–36. doi: 10.1016/j.genhosppsych.2019.07.002 [DOI] [PubMed] [Google Scholar]
- 31. Spaderna H, Mendell NR, Zahn D, Wang Y, Kahn J, Smits JM, Weidner G. Social isolation and depression predict 12‐month outcomes in the "waiting for a new heart study". J Heart Lung Transplant. 2010;29:247–254. doi: 10.1016/j.healun.2009.07.018 [DOI] [PubMed] [Google Scholar]
- 32. Zhou Z, Lin C, Ma J, Towne SD, Han Y, Fang Y. The association of social isolation with the risk of stroke among middle‐aged and older adults in China. Am J Epidemiol. 2019;188:1456–1465. doi: 10.1093/aje/kwz099 [DOI] [PubMed] [Google Scholar]
- 33. Boden‐Albala B, Litwak E, Elkind MS, Rundek T, Sacco RL. Social isolation and outcomes post stroke. Neurology. 2005;64:1888–1892. doi: 10.1212/01.WNL.0000163510.79351.AF [DOI] [PubMed] [Google Scholar]
- 34. Venna VR, McCullough LD. Role of social factors on cell death, cerebral plasticity and recovery after stroke. Metab Brain Dis. 2015;30:497–506. doi: 10.1007/s11011-014-9544-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Holmes A, Xu Y, Lee J, Maniskas ME, Zhu L, McCullough LD, Venna VR. Post‐stroke social isolation reduces cell proliferation in the dentate gyrus and alters miRNA profiles in the aged female mice brain. Int J Mol Sci. 2021;22:99. doi: 10.3390/ijms22010099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Friedler B, Crapser J, McCullough L. One is the deadliest number: the detrimental effects of social isolation on cerebrovascular diseases and cognition. Acta Neuropathol. 2015;129:493–509. doi: 10.1007/s00401-014-1377-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lara E, Caballero FF, Rico‐Uribe LA, Olaya B, Haro JM, Ayuso‐Mateos JL, Miret M. Are loneliness and social isolation associated with cognitive decline? Int J Geriatr Psychiatry. 2019;34:1613–1622. doi: 10.1002/gps.5174 [DOI] [PubMed] [Google Scholar]
- 38. Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, Tang Y, Bennett DA. Loneliness and risk of Alzheimer disease. Arch Gen Psychiatry. 2007;64:234–240. doi: 10.1001/archpsyc.64.2.234 [DOI] [PubMed] [Google Scholar]
- 39. Zhou Z, Wang P, Fang Y. Loneliness and the risk of dementia among older Chinese adults: gender differences. Aging Ment Health. 2018;22:519–525. doi: 10.1080/13607863.2016.1277976 [DOI] [PubMed] [Google Scholar]
- 40. Holwerda TJ, Deeg DJ, Beekman AT, van Tilburg TG, Stek ML, Jonker C, Schoevers RA. Feelings of loneliness, but not social isolation, predict dementia onset: results from the Amsterdam Study of the Elderly (AMSTEL). J Neurol Neurosurg Psychiatry. 2014;85:135–142. doi: 10.1136/jnnp-2012-302755 [DOI] [PubMed] [Google Scholar]
- 41. Rawtaer I, Gao Q, Nyunt MS, Feng L, Chong MS, Lim WS, Lee TS, Yap P, Yap KB, Ng TP. Psychosocial risk and protective factors and incident mild cognitive impairment and dementia in community dwelling elderly: findings from the Singapore Longitudinal Ageing Study. J Alzheimers Dis. 2017;57:603–611. doi: 10.3233/JAD-160862 [DOI] [PubMed] [Google Scholar]
- 42. Yin J, Lassale C, Steptoe A, Cadar D. Exploring the bidirectional associations between loneliness and cognitive functioning over 10 years: the English Longitudinal Study of Ageing. Int J Epidemiol. 2019;48:1937–1948. doi: 10.1093/ije/dyz085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Shankar A, Hamer M, McMunn A, Steptoe A. Social isolation and loneliness: relationships with cognitive function during 4 years of follow‐up in the English Longitudinal Study of Ageing. Psychosom Med. 2013;75:161–170. doi: 10.1097/PSY.0b013e31827f09cd [DOI] [PubMed] [Google Scholar]
- 44. Barnes LL, De Leon CM, Wilson RS, Bienias JL, Evans DA. Social resources and cognitive decline in a population of older African Americans and whites. Neurology. 2004;63:2322–2326. doi: 10.1212/01.WNL.0000147473.04043.B3 [DOI] [PubMed] [Google Scholar]
- 45. Hodgson S, Watts I, Fraser S, Roderick P, Dambha‐Miller H. Loneliness, social isolation, cardiovascular disease and mortality: a synthesis of the literature and conceptual framework. J R Soc Med. 2020;113:185–192. doi: 10.1177/0141076820918236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hammig O. Health risks associated with social isolation in general and in young, middle and old age. PLoS One. 2019;14:e0219663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Dyal SR, Valente TW. A systematic review of loneliness and smoking: small effects, big implications. Subst Use Misuse. 2015;50:1697–1716. doi: 10.3109/10826084.2015.1027933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Seo DC, Huang Y. Systematic review of social network analysis in adolescent cigarette smoking behavior. J Sch Health. 2012;82:21–27. doi: 10.1111/j.1746-1561.2011.00663.x [DOI] [PubMed] [Google Scholar]
- 49. Shankar A, McMunn A, Banks J, Steptoe A. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol. 2011;30:377. doi: 10.1037/a0022826 [DOI] [PubMed] [Google Scholar]
- 50. Kobayashi LC, Steptoe A. Social isolation, loneliness, and health behaviors at older ages: longitudinal cohort study. Ann Behav Med. 2018;52:582–593. doi: 10.1093/abm/kax033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts reduced physical activity: cross‐sectional & longitudinal analyses. Health Psychol. 2009;28:354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Stickley A, Koyanagi A, Koposov R, Schwab‐Stone M, Ruchkin V. Loneliness and health risk behaviours among Russian and US adolescents: a cross‐sectional study. BMC Public Health. 2014;14:1–12. doi: 10.1186/1471-2458-14-366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2 [DOI] [PubMed] [Google Scholar]
- 54. Canham SL, Mauro PM, Kaufmann CN, Sixsmith A. Association of alcohol use and loneliness frequency among middle‐aged and older adult drinkers. J Aging Health. 2016;28:267–284. doi: 10.1177/0898264315589579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hajek A, Kretzler B, König H‐H. The association between obesity and social isolation as well as loneliness in the adult population: a systematic review. Diabetes Metab Syndr Obes. 2021;14:2765. doi: 10.2147/DMSO.S313873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Cho JH‐J, Olmstead R, Choi H, Carrillo C, Seeman TE, Irwin MR. Associations of objective versus subjective social isolation with sleep disturbance, depression, and fatigue in community‐dwelling older adults. Aging Ment Health. 2019;23:1130–1138. doi: 10.1080/13607863.2018.1481928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ge L, Yap CW, Ong R, Heng BH. Social isolation, loneliness and their relationships with depressive symptoms: a population‐based study. PLoS One. 2017;12:e0182145. doi: 10.1371/journal.pone.0182145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lubben J, Blozik E, Gillmann G, Iliffe S, von Renteln KW, Beck JC, Stuck AE. Performance of an abbreviated version of the Lubben Social Network Scale among three European community‐dwelling older adult populations. Gerontologist. 2006;46:503–513. doi: 10.1093/geront/46.4.503 [DOI] [PubMed] [Google Scholar]
- 59. Patterson AC, Veenstra G. Loneliness and risk of mortality: a longitudinal investigation in Alameda County, California. Soc Sci Med. 2010;71:181–186. doi: 10.1016/j.socscimed.2010.03.024 [DOI] [PubMed] [Google Scholar]
- 60. Horsten M, Mittleman MA, Wamala SP, Schenck‐Gustafsson K, Orth‐Gomer K. Depressive symptoms and lack of social integration in relation to prognosis of CHD in middle‐aged women. The Stockholm Female Coronary Risk Study. Eur Heart J. 2000;21:1072–1080. doi: 10.1053/euhj.1999.2012 [DOI] [PubMed] [Google Scholar]
- 61. Smith KJ, Gavey S, RIddell NE, Kontari P, Victor C. The association between loneliness, social isolation and inflammation: a systematic review and meta‐analysis. Neurosci Biobehav Rev. 2020;112:519–541. doi: 10.1016/j.neubiorev.2020.02.002 [DOI] [PubMed] [Google Scholar]
- 62. Walker E, Ploubidis G, Fancourt D. Social engagement and loneliness are differentially associated with neuro‐immune markers in older age: time‐varying associations from the English Longitudinal Study of Ageing. Brain Behav Immun. 2019;82:224–229. doi: 10.1016/j.bbi.2019.08.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Vingeliene S, Hiyoshi A, Lentjes M, Fall K, Montgomery S. Longitudinal analysis of loneliness and inflammation at older ages: English longitudinal Study of Ageing. Psychoneuroendocrinology. 2019;110:104421. doi: 10.1016/j.psyneuen.2019.104421 [DOI] [PubMed] [Google Scholar]
- 64. Heffner KL, Waring ME, Roberts MB, Eaton CB, Gramling R. Social isolation, C‐reactive protein, and coronary heart disease mortality among community‐dwelling adults. Soc Sci Med. 2011;72:1482–1488. doi: 10.1016/j.socscimed.2011.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Shankar A. Loneliness and sleep in older adults. Soc Psychiatry Psychiatr Epidemiol. 2020;55:269–272. doi: 10.1007/s00127-019-01805-8 [DOI] [PubMed] [Google Scholar]
- 66. Larrabee Sonderlund A, Thilsing T, Sondergaard J. Should social disconnectedness be included in primary‐care screening for cardiometabolic disease? A systematic review of the relationship between everyday stress, social connectedness, and allostatic load. PLoS One. 2019;14:e0226717. doi: 10.1371/journal.pone.0226717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Kop WJ, Berman DS, Gransar H, Wong ND, Miranda‐Peats R, White MD, Shin M, Bruce M, Krantz DS, Rozanski A. Social network and coronary artery calcification in asymptomatic individuals. Psychosom Med. 2005;67:343–352. doi: 10.1097/01.psy.0000161201.45643.8d [DOI] [PubMed] [Google Scholar]
- 68. Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40:218–227. doi: 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Richiardi L, Bellocco R, Zugna D. Mediation analysis in epidemiology: methods, interpretation and bias. Int J Epidemiol. 2013;42:1511–1519. doi: 10.1093/ije/dyt127 [DOI] [PubMed] [Google Scholar]
- 70. Cole SR, Hernán MA. Fallibility in estimating direct effects. Int J Epidemiol. 2002;31:163–165. doi: 10.1093/ije/31.1.163 [DOI] [PubMed] [Google Scholar]
- 71. Health Resources and Services Administration . The Loneliness Epidemic. Accessed February 1, 2020. https://www.hrsa.gov/enews/past‐issues/2019/january‐17/loneliness‐epidemic
- 72. Perone AK, Ingersoll‐Dayton B, Watkins‐Dukhie K. Social isolation loneliness among LGBT older adults: lessons learned from a pilot friendly caller program. Clin Soc Work J. 2020;48:126–139. doi: 10.1007/s10615-019-00738-8 [DOI] [Google Scholar]
- 73. Goldsen KF. Shifting social context in the lives of LGBTQ older adults. Public Policy Aging Rep. 2018;28:24–28. doi: 10.1093/ppar/pry003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Churchwell K, Elkind MSV, Benjamin RM, Carson AP, Chang EK, Lawrence W, Mills A, Odom TM, Rodriguez CJ, Rodriguez F, et al; on behalf of the American Heart Association. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation. 2020;142:e454–e468. doi: 10.1161/CIR.0000000000000936 [DOI] [PubMed] [Google Scholar]
- 75. Caspi A, Harrington H, Moffitt TE, Milne BJ, Poulton R. Socially isolated children 20 years later: risk of cardiovascular disease. Arch Pediatr Adolesc Med. 2006;160:805–811. doi: 10.1001/archpedi.160.8.805 [DOI] [PubMed] [Google Scholar]
- 76. Danese A, Moffitt TE, Harrington H, Milne BJ, Polanczyk G, Pariante CM, Poulton R, Caspi A. Adverse childhood experiences and adult risk factors for age‐related disease: depression, inflammation, and clustering of metabolic risk markers. Arch Pediatr Adolesc Med. 2009;163:1135–1143. doi: 10.1001/archpediatrics.2009.214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Lacey RE, Kumari M, Bartley M. Social isolation in childhood and adult inflammation: evidence from the National Child Development Study. Psychoneuroendocrinology. 2014;50:85–94. doi: 10.1016/j.psyneuen.2014.08.007 [DOI] [PubMed] [Google Scholar]
- 78. Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine‐year follow‐up study of Alameda County residents. Am J Epidemiol. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674 [DOI] [PubMed] [Google Scholar]
- 79. McCrory C, Finucane C, O’Hare C, Frewen J, Nolan H, Layte R, Kearney PM, Kenny RA. Social disadvantage and social isolation are associated with a higher resting heart rate: evidence from the Irish Longitudinal Study on Ageing. J Gerontol B Psychol Sci Soc Sci. 2016;71:463–473. doi: 10.1093/geronb/gbu163 [DOI] [PubMed] [Google Scholar]
- 80. Stringhini S, Berkman L, Dugravot A, Ferrie JE, Marmot M, Kivimaki M, Singh‐Manoux A. Socioeconomic status, structural and functional measures of social support, and mortality: the British Whitehall II Cohort Study, 1985–2009. Am J Epidemiol. 2012;175:1275–1283. doi: 10.1093/aje/kwr461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Roest AM, Martens EJ, de Jonge P, Denollet J. Anxiety and risk of incident coronary heart disease: a meta‐analysis. J Am Coll Cardiol. 2010;56:38–46. doi: 10.1016/j.jacc.2010.03.034 [DOI] [PubMed] [Google Scholar]
- 82. Gan Y, Gong Y, Tong X, Sun H, Cong Y, Dong X, Wang Y, Xu X, Yin X, Deng J, et al. Depression and the risk of coronary heart disease: a meta‐analysis of prospective cohort studies. BMC Psychiatry. 2014;14:1–11. doi: 10.1186/s12888-014-0371-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. National Academies of Sciences, Engineering, and Medicine . Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. Accessed June 3, 2022. http://nap.edu/25663 [PubMed] [Google Scholar]
- 84. Veazie S, Gilbert J, Winchell K, Paynter R, Guise J‐M. Addressing social isolation to improve the health of older adults: a rapid review. 2019. [PubMed]
- 85. Fakoya OA, McCorry NK, Donnelly M. Loneliness and social isolation interventions for older adults: a scoping review of reviews. BMC Public Health. 2020;20:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Cohen‐Mansfield J, Perach R. Interventions for alleviating loneliness among older persons: a critical review. Am J Health Promot. 2015;29:e109–e125. doi: 10.4278/ajhp.130418-LIT-182 [DOI] [PubMed] [Google Scholar]
- 87. Masi CM, Chen HY, Hawkley LC, Cacioppo JT. A meta‐analysis of interventions to reduce loneliness. Pers Soc Psychol Rev. 2011;15:219–266. doi: 10.1177/1088868310377394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Chipps J, Jarvis MA, Ramlall S. The effectiveness of e‐Interventions on reducing social isolation in older persons: a systematic review of systematic reviews. J Telemed Telecare. 2017;23:817–827. doi: 10.1177/1357633X17733773 [DOI] [PubMed] [Google Scholar]
- 89. Noone C, McSharry J, Smalle M, Burns A, Dwan K, Devane D, Morrissey EC. Video calls for reducing social isolation and loneliness in older people: a rapid review. Cochrane Database Syst Rev. 2020;5:CD013632. doi: 10.1002/14651858.CD013632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Poscia A, Stojanovic J, La Milia DI, Duplaga M, Grysztar M, Moscato U, Onder G, Collamati A, Ricciardi W, Magnavita N. Interventions targeting loneliness and social isolation among the older people: an update systematic review. Exp Gerontol. 2018;102:133–144. doi: 10.1016/j.exger.2017.11.017 [DOI] [PubMed] [Google Scholar]
- 91. Gardiner C, Geldenhuys G, Gott M. Interventions to reduce social isolation and loneliness among older people: an integrative review. Health Soc Care Community. 2018;26:147–157. doi: 10.1111/hsc.12367 [DOI] [PubMed] [Google Scholar]
- 92. O'Rourke HM, Collins L, Sidani S. Interventions to address social connectedness and loneliness for older adults: a scoping review. BMC Geriatr. 2018;18:214. doi: 10.1186/s12877-018-0897-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Dickens AP, Richards SH, Greaves CJ, Campbell JL. Interventions targeting social isolation in older people: a systematic review. BMC Public Health. 2011;11:647. doi: 10.1186/1471-2458-11-647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Grenade L, Boldy D. Social isolation and loneliness among older people: issues and future challenges in community and residential settings. Aust Health Rev. 2008;32:468–478. doi: 10.1071/AH080468 [DOI] [PubMed] [Google Scholar]
- 95. Akl EA, Welch V, Pottie K, Eslava‐Schmalbach J, Darzi A, Sola I, Katikireddi SV, Singh J, Murad MH, Meerpohl J, et al. GRADE equity guidelines 2: considering health equity in GRADE guideline development: equity extension of the guideline development checklist. J Clin Epidemiol. 2017;90:68–75. doi: 10.1016/j.jclinepi.2017.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Franck L, Molyneux N, Parkinson L. Systematic review of interventions addressing social isolation and depression in aged care clients. Qual Life Res. 2016;25:1395–1407. doi: 10.1007/s11136-015-1197-y [DOI] [PubMed] [Google Scholar]
- 97. Adler NE, Stead WW. Patients in context—EHR capture of social and behavioral determinants of health. Obstet Gynecol Surv. 2015;70:388–390. doi: 10.1097/01.ogx.0000465303.29687.97 [DOI] [PubMed] [Google Scholar]
- 98. American Heart Association . 2024 Health equity impact goal: championing health equity for all. Accessed June 3, 2022. https://www.heart.org/en/about‐us/2024‐health‐equity‐impact‐goal#
- 99. van Deursen AJ, van Dijk JA. The first‐level digital divide shifts from inequalities in physical access to inequalities in material access. New Media Soc. 2019;21:354–375. doi: 10.1177/1461444818797082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Bhatnagar A. Environmental determinants of cardiovascular disease. Circ Res. 2017;121:162–180. doi: 10.1161/CIRCRESAHA.117.306458 [DOI] [PMC free article] [PubMed] [Google Scholar]


