Abstract
Background
Religiosity/spirituality is a major coping mechanism for African Americans, but no prior studies have analyzed its association with the American Heart Association Life's Simple 7 (LS7) indicators in this group.
Methods and Results
This cross‐sectional study using Jackson Heart Study (JHS) data examined relationships between religiosity (religious attendance, private prayer, religious coping) and spirituality (theistic, nontheistic, total) with LS7 individual components (eg, physical activity, diet, smoking, blood pressure) and composite score among African Americans. Multivariable logistic regression assessed the odds of achieving intermediate/ideal (versus poor) LS7 levels adjusted for sociodemographic, behavioral, and biomedical factors. Among the 2967 participants (mean [SD] age=54.0 [12.3] years; 65.7% women), higher religious attendance was associated with increased likelihood (reported as odds ratio [95% CI]) of achieving intermediate/ideal levels of physical activity (1.16 [1.06–1.26]), diet (1.10 [1.01–1.20]), smoking (1.50 [1.34–1.68]), blood pressure (1.12 [1.01–1.24]), and LS7 composite score (1.15 [1.06–1.26]). Private prayer was associated with increased odds of achieving intermediate/ideal levels for diet (1.12 [1.03–1.22]) and smoking (1.24 [1.12–1.39]). Religious coping was associated with increased odds of achieving intermediate/ideal levels of physical activity (1.18 [1.08–1.28]), diet (1.10 [1.01–1.20]), smoking (1.32 [1.18–1.48]), and LS7 composite score (1.14 [1.04–1.24]). Total spirituality was associated with increased odds of achieving intermediate/ideal levels of physical activity (1.11 [1.02–1.21]) and smoking (1.36 [1.21–1.53]).
Conclusions
Higher levels of religiosity/spirituality were associated with intermediate/ideal cardiovascular health across multiple LS7 indicators. Reinforcement of religiosity/spirituality in lifestyle interventions may decrease overall cardiovascular disease risk among African Americans.
Keywords: African Americans, health behavior, lifestyle, religiosity, risk factors, spirituality
Subject Categories: Primary Prevention, Cardiovascular Disease
Nonstandard Abbreviations and Acronyms
- AA
African American
- AHA
American Heart Association
- CVH
cardiovascular health
- DSES
Daily Spiritual Experience Scale
- JHS
Jackson Heart Study
- LS7
Life's Simple 7
- PA
physical activity
- SES
socioeconomic status
Clinical Perspective.
What Is New?
In this large cohort of community‐dwelling African American adults from the Jackson Heart Study (JHS), higher levels of religiosity (eg, religious attendance, private prayer, religious coping) and spirituality (eg, theistic, nontheistic) were associated with intermediate/ideal cardiovascular health across multiple indicators of the American Heart Association Life's Simple 7.
Our study provides the first high quality evidence substantiating that religiosity and spirituality can potentially have beneficial effects on select indicators of the Life's Simple 7 in African American men and women.
What Are the Clinical Implications?
Recognition by health professionals and researchers of the centrality and influence of religiosity and spirituality in the lives of African American adults may serve as a means to address cardiovascular health disparities through sociocultural understanding and the strategic development of culturally relevant lifestyle interventions.
Cardiovascular disease (CVD) affects nearly half of all African American (AA) adults, who are 30% more likely to die of CVD (ie, coronary heart disease, heart failure, stroke, and peripheral artery disease) than the overall US population. 1 Prevention and management of major CVD risk factors are key for addressing these persistent CVD disparities for promotion of cardiovascular health (CVH). Compared with non‐Hispanic White people, AAs have 82% lower odds of achieving ≥5 ideal levels of the CVH components that make up the American Heart Association (AHA) Life's Simple 7 (LS7). 2 Developed as a primordial prevention strategy against CVD, the LS7 is an evidence‐based metric of 7 health‐promoting behaviors and biological risk factors: physical activity (PA), diet, smoking, body mass index (BMI), blood pressure (BP), cholesterol, and glucose. 3 AAs have significantly worse health status than White people in every LS7 component except for total cholesterol. 1 Among AAs in the JHS, there was a strong graded association between number of LS7 components in the ideal range and lower risk of incident CVD. 4 In addition, a stepwise decrement in lifetime risk of coronary heart disease, 5 heart failure, 6 stroke, 7 and peripheral artery disease 8 with higher LS7 scores or better CVH has been demonstrated among AAs in several observational, population‐based cohorts. Despite the substantial epidemiologic evidence for the benefits of ideal CVH among AAs, there are few data on the role of key psychosocial influences in the lives of AAs, such as their religious and spiritual beliefs, in fostering achievement of ideal LS7 indicators. A recent meta‐analysis provided evidence supporting the benefits of positive psychosocial factors such as religiosity/spirituality for CVH outcomes; however, the majority of included studies lacked focus on racial/ethnic minority groups, particularly AAs. 9 Elucidation of a link between religiosity/spirituality and CVH could also inform the design of effective, culturally tailored, and faith‐oriented interventions to improve CVH disparities by race/ethnicity, as recently endorsed in the AHA 2030 Impact Goal Presidential Advisory. 10
Research suggests that religiosity/spirituality may have an important role in CVD among AAs. The 2014 Pew Research Center's US Religious Landscape Survey found that 75% of AAs report the primary importance of religion in their lives, and 83% believe in God. 11 Furthermore, the weekly religious service attendance and spiritual practices of AAs exceed those of all other racial groups, especially among women. 12 , 13 A plethora of studies highlight the connection between religion and health, 14 several of which have shown a protective relationship between religious participation and chronic disease–related death, including that caused by CVD. 15 Greater religiosity/spirituality has been linked to better health behaviors such as lower caloric intake, alcohol use, and smoking among AAs, but findings are inconclusive regarding the effects of religiosity/spirituality on cardiometabolic profiles and CVD events. 13 , 16 Nonetheless, no community‐based cohort study has examined the effect of religiosity/spirituality on CVH behaviors and biological factors as defined by the AHA LS7. This supports the scientific premise and purpose of the current study to fill this gap by assessing the cross‐sectional relationship between religiosity/spirituality and CVH in a cohort of AAs. We hypothesized that greater levels of religiosity/spirituality are positively associated with achieving intermediate or ideal levels of LS7 components and LS7 composite score among AAs. We also posited that socioeconomic status (SES), chronic stress, and social network would modify the association of religiosity/spirituality with CVH.
Methods
Sample Population and Procedures
The data that support the findings of this study are available from the corresponding author upon reasonable request. The JHS is a community‐based, prospective cohort study examining CVD risk in 5306 AA adults (by self‐identification: 1935 men; 3371 women), aged 21 to 84 years residing in the tricounty area (Hinds, Madison, and Rankin counties) of Jackson, Mississippi. Details of the study design, recruitment approach, and measures have been previously published. 17 , 18 , 19 Participants completed in‐depth interviews (face‐to‐face and telephone) and surveys administered by trained study staff to assess an array of sociocultural factors (including stress, social network, etc) via instruments validated from previous studies including AAs. 18 The religiosity/spirituality questionnaires were completed by participants as part of a larger, self‐administered survey. 20 Although religiosity/spirituality measures were a part of this comprehensive assessment of sociocultural influences on CVD risk, there is a low likelihood of participant response bias for religiosity/spirituality, as the JHS overall objective and purpose was not solely focused on ascertainment of religiosity/spirituality. Participants underwent baseline assessments between 2000 and 2004 that included data collection of sociodemographics, medical history, physical examination, laboratory studies, medications, and health behaviors. The current study included all JHS participants with complete data on each LS7 component (or CVH metric) and religiosity/spirituality data at baseline (2000–2004). Exclusion criteria were reported CVD (eg, coronary heart disease, heart failure, stroke, and peripheral artery disease) and missing data at baseline for all main variables of interest (religiosity/spirituality and ≥1 CVH metric). The study was approved by the institutional review boards of University of Mississippi Medical Center, Jackson State University, and Tougaloo College. All participants provided written informed consent. The current study was deemed exempt by the Mayo Clinic Institutional Review Board.
Primary Independent Variables
Religiosity
The domains of religiosity assessed were religious attendance, private prayer, and religious coping. Religious attendance, defined as frequency of organized religious activities such as church attendance, service viewing on television, and participation in bible study group meetings, consisted of 1 item with 6 response options (“not at all”=1 to “nearly everyday”=6). Private prayer was assessed as frequency of prayer or meditation outside of formal religious activity to which participants responded using an 8‐point Likert scale ranging from 1 (“never”) to 8 (“more than once a day”). Religious coping, the use of religious beliefs or practices in adapting to difficult life situations and stressful events, was assessed by 1 item, “To what extent is your religion or spiritual tradition involved in understanding or dealing with stressful situations in any way?” to which participants responded using a 4‐point Likert‐type scale ranging from 1 (“not involved at all”) to 4 (“very involved”). Items were selected and adapted from the Fetzer Multidimensional Measurement of Religiousness/Spirituality (religious attendance, private prayer) and Religious Coping Scale (religious coping) instruments. 20 , 21 , 22 All 3 measures of religiosity have been previously validated in the JHS. 20 , 23 Limited psychometric properties are available for these discrete items (Cronbach α >0.80 for religious coping), but they have been extensively examined in previous studies with similar populations. 20 , 23
Spirituality
Spirituality was measured with the short version of the Daily Spiritual Experience Scale (DSES). 24 The DSES was designed to assess ordinary daily experiences according to theistic and nontheistic experiences of spirituality in 6 domains. The 6 DSES items are each rated using a 6‐point Likert scale as 1, “never,” to 6, “many times a day” (total score range, 6–36, with higher scores indicating higher spirituality). The theistic spirituality DSES subscale score (range, 3–18) was calculated by summing 3 of the items (feel God's presence, desire closer union with God, feel God's love) (Cronbach α=0.73). Likewise, the nontheistic spirituality DSES subscale score (range, 3–18) was calculated by summing 3 items (feel strength in my religion, feel deep inner peace and harmony, feel spiritually touched by creation; Cronbach α=0.76). Total spirituality DSES score was tabulated as the summation of the theistic and nontheistic subscale scores (Cronbach α=0.85). Higher scores on the total, theistic, and nontheistic DSES represent more reported daily spiritual experiences. Prior studies have demonstrated its favorable psychometric properties in the JHS. 20 , 23
Outcomes of Interest
The primary outcome of interest was CVH as measured by the AHA LS7 individual components and LS7 composite score. JHS participants completed assessments of the LS7 components at the baseline visit consisting of 7 health behaviors and biological factors: PA, diet, cigarette smoking, BMI, resting BP, total serum cholesterol level, and fasting plasma glucose level. Details on the standardized protocols and methods for measurement of the LS7 components at the assessments have been previously described. 25 The LS7 component metrics according to AHA criteria are shown in Table 1. 25 , 26 The LS7 composite score was ascertained with the assignment of 0 points for poor, 1 point for intermediate, and 2 points for ideal for each LS7 component, with a cumulative sum of all components (range, 0–14, poor to ideal). LS7 composite score as a continuous measure was further classified into 3 groups, as previously conducted in the JHS: poor CVH (0–6), intermediate CVH, 7 , 8 and ideal CVH. 9 , 10 , 11 , 12 , 13 , 14 , 25
Table 1.
Definition of Poor, Intermediate, and Ideal Life's Simple 7 Component Metrics
| Component metrics | Poor (0 points) | Intermediate (1 point) | Ideal (2 points) |
|---|---|---|---|
| Cigarette smoking | Current | Former <1 y | Never or former >1 y |
| Healthy diet* | 0–1 | 2–3 | 4–5 |
| Physical activity† | None |
1–149 min/wk moderate intensity or 1–74 min/wk vigorous intensity or 1–149 min/wk moderate+vigorous intensity |
≥150 min/wk moderate intensity or ≥75 min/wk vigorous intensity or ≥150 min/wk moderate+vigorous intensity |
| Body mass index | ≥30.0 | 25.0–29.9 | <25.0 |
| Blood pressure, mm Hg |
SBP ≥140 or DBP ≥90 |
SBP 120–139 or DBP 80–89 or Treated to goal |
<120/<80 untreated |
| Total cholesterol, mg/dL | ≥240 |
200–239 or Treated to goal |
<200 untreated |
| Fasting plasma glucose, mg/dL | ≥126 |
100–125 or Treated to goal |
<100 untreated |
Data from Lloyd‐Jones et al 3 . DBP indicates diastolic blood pressure; and SBP, systolic blood pressure.
Healthy diet score (0–5 components) included the following: fruits and vegetables, ≥4.5 cups/d; fish, ≥2 3.5‐oz servings/wk; fiber‐rich whole grains ≥1.1 g fiber/10 g carbohydrate, ≥3 1‐oz‐equivalent servings/d; sodium, ≤1500 mg/d; sugar‐sweetened beverages, ≤450 kcal/wk. Dietary recommendations are scaled according to a 2000‐kcal/d diet.
Minutes of vigorous activity are equal to 2 times the minutes of moderate activity when moderate and vigorous activities are combined.
Covariates
Covariates included baseline age (continuous), sex (men/women), educational attainment (less than high school to vocational/trade school or college graduate), income status (poor to affluent), and insurance status (insured/uninsured). For income status, 4 income categories (poor, lower‐middle, upper‐middle, and affluent) were assigned on the basis of family size, US Census poverty levels, and year of baseline clinic visit (2000–2004). 27 Corresponding income ranges for the categories were poor, less than poverty level; lower‐middle, 1 to 1.5 times the poverty level; upper‐middle, >1.5 but <3.5 times the poverty level; and affluent, ≥3.5 times the poverty level. On the basis of our prior work, 25 chronic stress was assessed at baseline using the Global Perceived Stress Scale, an adapted standardized stress scale for use in the JHS. 18 The 8‐item questionnaire measures global perceptions of ongoing stress over the prior 12‐month period in several life domains (eg, racism/discrimination, employment, and legal challenges). 25 Scores range from 0 to 24, with higher scores indicating greater levels of stress. Another key covariate, social network, was assessed with an adapted version of the Berkman Social Network Index. 28 The 5‐item instrument assesses current marital status, group membership, close friends, close relatives, and frequency of social contact. A total social network score was calculated ranging from 0 to 5, with higher scores indicating larger social network.
Statistical Analysis
Participant baseline characteristics were described overall and stratified by sex and religiosity/spirituality measures. Religious attendance, private prayer, and religious coping were categorized similar to prior work, 20 , 23 while theistic and nontheistic subscales were grouped using quartiles. The rationale for presenting the data in this manner is directly related to previously documented differences in religious participation and spiritual practices between AA men and women. 11 , 12 , 13 Characteristics were compared between groups by sex using ANOVA and χ2 tests, as appropriate, for continuous and categorical variables, respectively. By using absolute standardized differences, characteristics of participants included in the analysis were compared with those excluded; a difference <0.2 was considered to be a small effect, as outlined by Cohen. 29 The prevalence of CVH metrics (poor, intermediate, and ideal) was assessed for individual LS7 components for all participants and by sex based on the aforementioned rationale of existing sex‐related differences in religiosity/spirituality. Similar to our prior study, 25 to investigate the associations of each religiosity/spirituality measure with LS7 components and LS7 composite score, multivariable logistic regression was used to compute odds ratios (ORs) with accompanying 95% CIs to compare intermediate/ideal CVH with poor CVH (reference). This comparison was chosen to maximize power for comparisons. For each LS7 component, models were adjusted in a sequential manner including each religiosity/spirituality measure (main predictors) in separate models to minimize multicollinearity. Model 1 included adjustment for age, sex, and SES (education, income, and insurance status); model 2 added chronic stress; and model 3 added social network. Additional post hoc analyses assessed for effect modification of each religiosity/spirituality measure with age, sex, SES, chronic stress, and social network on each LS7 component (and LS7 composite score category) by inclusion of a series of interaction effects within the logistic regression framework. Tests for multiplicative interactions between religiosity/spirituality measures (ie, religious attendance*private prayer) and collectively across all religiosity/spirituality variables were conducted using the adjusted models. In all logistic regression analyses including interaction analyses, age, religiosity/spirituality measures, chronic stress, and social network scores were modeled as continuous variables. Distribution of LS7 composite scores were examined across categories of religiosity/spirituality measures to ensure that the association of these measures were approximately linear. Analyses were performed using SAS, version 9.4 (SAS Institute Inc, Cary, NC). Statistical significance was defined by 2‐sided P values with an α=0.05.
Results
Among the 5306 initial participants in the JHS, 2339 were excluded because of CVD (n=572) or missing data on religiosity/spirituality (n=1142) or CVH metrics (n=1247) (people could be excluded for more than 1 reason), resulting in a final analytic sample of 2967 participants. Compared with participants not included in this analysis (n=2339), included participants were younger, of lower education level and income status, and had better CVH (higher LS7 score) (Table S1). Table 2 summarizes the sample characteristics stratified by participant sex. Of the 2967 participants in the sample, 1949 (65.7%) were women, and the mean (SD) age was 54.0 (12.3) years. Mean (SD) reported values were high for religiosity (religious attendance, 5.0 [0.9], scale, 1–6; private prayer, 7.2 [1.3], scale, 1–8; religious coping, 3.6 [0.6], scale, 1–4), and spirituality (DSES score, 29.2 [4.7]; scale, 6–36). Compared with women, men reported higher income status (P<0.001). Women reported higher religiosity (religious attendance, private prayer, religious coping) and spirituality than men (all P<0.001). Higher chronic stress was reported among women than men (P<0.001), whereas men had a larger social network (P<0.001). The mean (SD) LS7 composite score was 7.3 (2.1), with no differences observed by sex.
Table 2.
Baseline Characteristics of Jackson Heart Study Participants by Sex*
| Characteristic | Total (N=2967) | Women (n=1949) | Men (n=1018) | P value |
|---|---|---|---|---|
| Age, y | 54.0 (12.3) | 54.3 (12.3) | 53.5 (12.2) | 0.09 |
| Education | (n=2963) | (n=1947) | (n=1016) | 0.16 |
| Less than high school | 436 (14.7) | 273 (14.0) | 163 (16.0) | |
| High school graduate/GED | 527 (17.8) | 361 (18.5) | 166 (16.3) | |
| Vocational/trade school or college graduate | 2000 (67.5) | 1313 (67.4) | 687 (67.6) | |
| Income status | (n=2550) | (n=1672) | (n=878) | <0.001 |
| Poor | 296 (11.6) | 233 (13.9) | 63 (7.2) | |
| Lower‐middle | 574 (22.5) | 413 (24.7) | 161 (18.3) | |
| Upper‐middle | 818 (32.1) | 551 (33.0) | 267 (30.4) | |
| Affluent | 862 (33.8) | 475 (28.4) | 387 (44.1) | |
| Health insured | 2583/2960 (87.3) | 1692/1944 (87.0) | 891/1016 (87.7) | 0.61 |
| Married | 1689/2961 (57.0) | 934/1945 (48.0) | 755/1016 (74.3) | <0.001 |
| Cardiovascular risk factors | ||||
| Hypertension | 1554 (52.4) | 1069 (54.8) | 485 (47.6) | <0.001 |
| Diabetes | 512 (17.3) | 347 (17.8) | 165 (16.2) | 0.27 |
| Hyperlipidemia | 342/2964 (11.5) | 231/1947 (11.9) | 111/1017 (10.9) | 0.44 |
| Current smoker | 310 (10.4) | 163 (8.4) | 147 (14.4) | <0.001 |
| LS7 composite score | 7.3 (2.1) | 7.2 (2.0) | 7.3 (2.1) | 0.28 |
| Religiosity measures | ||||
| Religious attendance | 5.0 (0.9) | 5.1 (0.8) | 4.8 (1.1) | <0.001 |
| Private prayer | 7.2 (1.3) | 7.4 (1.1) | 6.9 (1.5) | <0.001 |
| Religious coping | 3.6 (0.6) (n=2914) | 3.6 (0.6) (n=1913) | 3.5 (0.7) (n=1001) | <0.001 |
| Spirituality measures | ||||
| Theistic subscale score | 14.9 (2.5) | 15.2 (2.2) | 14.3 (2.8) | <0.001 |
| Nontheistic subscale score | 14.3 (2.6) | 14.5 (2.5) | 13.8 (2.8) | <0.001 |
| DSES total score | 29.2 (4.7) | 29.7 (4.3) | 28.2 (5.3) | <0.001 |
| Chronic stress score | 4.0 (2.0, 8.0) (n=2947) | 5.0 (2.0, 8.0) (n=1932) | 3.0 (1.0, 7.0) (n=1015) | <0.001 |
| Social network score | 4.2 (0.8) (n=2936) | 4.2 (0.8) (n=1931) | 4.3 (0.9) (n=1005) | <0.001 |
DSES indicates Daily Spiritual Experience Scale; GED, General Educational Development; and LS7, Life's Simple 7.
Data are presented as mean (SD), n (%), or median (Q1, Q3).
Participants had statistically significant differences in demographics when stratified by religiosity/spirituality measures (Tables S2A through S2E). A few notable differences observed were that participants reporting more religiosity (religious attendance, private prayer, and religious coping) tended to be older, women, more educated, and more socially connected (all P≤0.05). Similar trends were seen among the spirituality scores (theistic, nontheistic) and several demographic factors (age, sex, education, social network) with the addition of stress (all P<0.05). Hypertension and current smoking were consistently more prevalent with higher levels of religiosity/spirituality measures (P<0.05 except for religious coping). LS7 scores increased with higher religiosity/spirituality, although only religious coping was statistically significant (P=0.002). As expected, all religiosity/spirituality measures correlated well with stratification by each religiosity/spirituality measure (all P<0.001).
Prevalence of LS7 Components
The prevalence rates of all LS7 metrics by LS7 component are reported separately by sex in Figure 1. Women had higher prevalence of poor LS7 metrics for PA (46.8% versus 43.3%) and BMI (59.5% versus 41.5%) than men (both P<0.01). Compared with men, women had a higher prevalence of ideal LS7 metrics for smoking (90.5% versus 84.4%), BP (22.9% versus 20.4%), and glucose value (48.9% versus 45.1%) (all P<0.05).
Figure 1.
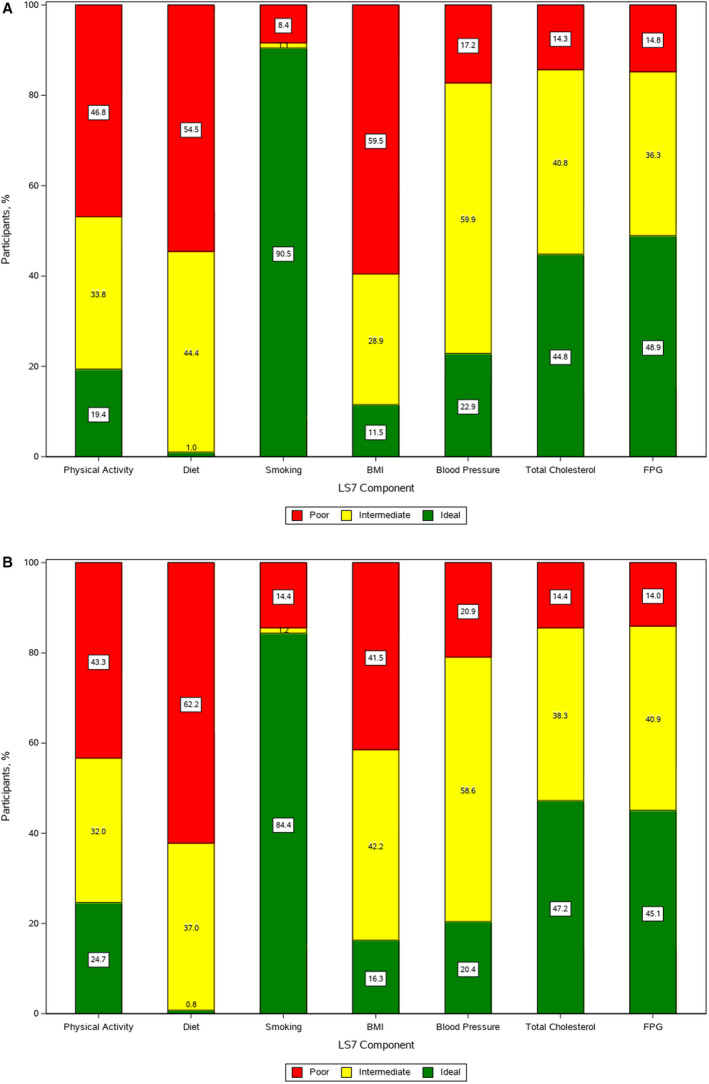
Prevalence of cardiovascular health metrics among Jackson Heart Study participants.
Percentage of poor, intermediate, and ideal cardiovascular health behaviors for each component of Life's Simple 7 (LS7) are shown. A, Women. B, Men. BMI indicates body mass index; and FPG, fasting plasma glucose.
Religiosity/Spirituality Measures and LS7
The ORs (comparing intermediate/ideal CVH with poor CVH [reference]) for each LS7 component and LS7 composite score by religiosity/spirituality measures (per each 1‐SD unit increase in each measure) for the minimally adjusted model (model 1) are shown in Figure 2.
Figure 2.
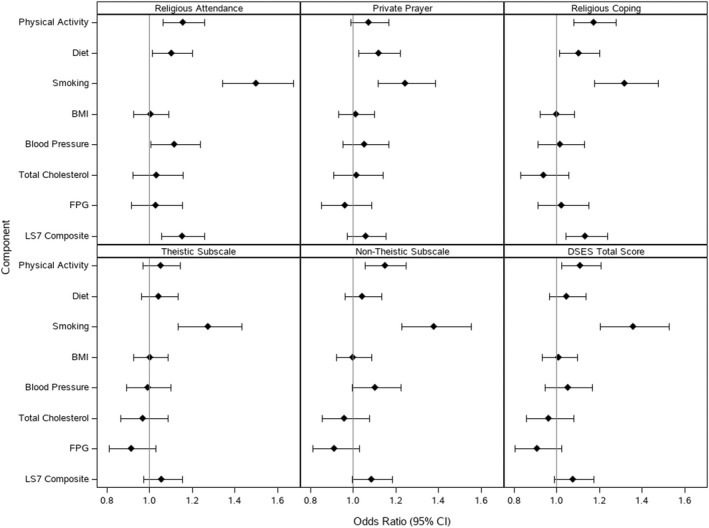
Odds ratios for the association between Life's Simple 7 (LS7) components and religiosity and spirituality measures.
Data are shown for model 1: adjusted for age, sex, education, income, and insurance status. Odds ratios of achieving intermediate/ideal levels versus poor levels (reference) of LS7 are displayed. Odds ratios are per 1‐SD unit increase in religiosity and spirituality measures. BMI indicates body mass index; DSES, Daily Spiritual Experience Scale; and FPG, fasting plasma glucose.
Religiosity
After multivariable adjustment (model 1), higher religious attendance was associated with increased odds (OR [95% CI]) of achieving intermediate/ideal levels for PA (1.16 [1.06–1.26]), diet (1.10 [1.01–1.20]), smoking (1.50 [1.34–1.68]), BP (1.12 [1.01–1.24]), and LS7 composite score (1.15 [1.06–1.26]) (Table S3). Private prayer was associated with increased odds of achieving intermediate/ideal levels for diet (1.12 [1.03–1.22]) and smoking (1.24 [1.12–1.39]). Religious coping was associated with increased odds of achieving intermediate/ideal levels for PA (1.18 [1.08–1.28]), diet (1.10 [1.01–1.20]), smoking (1.32 [1.18–1.48]), and LS7 composite score (1.14 [1.04–1.24]). The statistically significant associations of each religiosity measure with each LS7 component or LS7 composite score remained significant after adjustment for chronic stress (model 2) and social network (model 3) (Tables S4 and S5). There were no statistically significant associations between any of the religiosity measures and BMI, cholesterol, or glucose.
Spirituality
Theistic spirituality was associated with increased odds (OR [95% CI]) of achieving intermediate/ideal levels for smoking (1.27 [1.13–1.43]) (model 1, Table S6). Nontheistic spirituality was associated with increased odds of achieving intermediate/ideal levels for PA (1.15 [1.06–1.25]) and smoking (1.38 [1.23–1.55]). Total spirituality (DSES score) was associated with increased odds of achieving intermediate/ideal levels for PA (1.11 [1.02–1.21]) and smoking (1.36 [1.21–1.53]). These associations remained statistically significant after adjustment for chronic stress (model 2) and social network (model 3) (Tables S7 and S8). Although the association between nontheistic spirituality and BP was nonsignificant in model 1 (1.10 [0.99–1.22]), it became significant in model 2 (1.13 [1.01–1.25]) and model 3 (1.12 [1.01–1.25]).
Effect Modification
Post hoc analyses demonstrated effect modification of the associations of specific religiosity/spirituality measures with sex and age (model 1; data not shown). The effect of religiosity/spirituality measures and LS7 components/composite score were modified by sex (religious attendance and LS7 composite score, P=0.01; private prayer and LS7 composite score, P=0.006; theistic spirituality and BMI, P=0.03). In sex‐stratified models of religious attendance and LS7 composite score, the OR (95% CI) for achieving intermediate/ideal LS7 composite score was increased among men (1.28 [1.13–1.44]; P<0.001) but not among women (1.05 [0.93–1.19]; P=0.43). Similarly, for private prayer, the odds of achieving intermediate/ideal LS7 composite score were greater among men (1.18 [1.05–1.32]; P=0.005) but not among women (0.93 [0.82–1.07]; P=0.30). A significant interaction was also observed between theistic spirituality and BMI. When sex‐specific subgroups were examined, however, neither sex showed a significant association between theistic spirituality and BMI.
The effect of spirituality measures and LS7 components were also modified by age (theistic and PA, P=0.02; theistic and BP, P=0.04; nontheistic and diet, P=0.04; total spirituality and BP, P=0.04). For nontheistic spirituality, the odds (OR [95% CI]) of achieving intermediate/ideal diet were greater among those aged <55 years (1.17 [1.04–1.31]; P=0.009) but not among those aged ≥55 years (0.94 [0.83–1.06]; P=0.30). For total spirituality, the odds of achieving intermediate/ideal diet were greater among younger people (<55 years) (1.16 [1.03–1.31]; P=0.01) but not among older people (≥55 years) (0.95 [0.84–1.07]; P=0.40).
The interaction terms between each religiosity/spirituality measure and SES, chronic stress, and social network for each LS7 component and LS7 composite score were not statistically significant (data not shown).
Discussion
In this community cohort of AAs, higher levels of religiosity/spirituality were associated with greater likelihood of achieving intermediate/ideal (versus poor) CVH across multiple LS7 indicators. Our findings underscore that religiosity/spirituality is an integral part of the AA experience given the reported high levels of religiosity/spirituality in multiple domains that were associated with CVH behaviors (PA, diet, and smoking), biological factors (BP), and LS7 composite score in our sample. Thus, religiosity/spirituality should be acknowledged as prominent sociocultural influences on CVH in the lives of this population, rather than as heuristic constructs in need of improvement.
The association between religiosity/spirituality and CVH we report confirms and extends prior research linking religiosity/spirituality and cardiovascular risk factors among AAs. Debnam and colleagues 30 identified the role of religious social support in health behaviors such as fruit and vegetable consumption and moderate PA in AAs (N=2370). In the Multi‐Ethnic Study of Atherosclerosis cohort (N=5474, 30% AA), there was no consistent association between greater religiosity/spirituality and overall better cardiovascular risk factors. 13 Although those findings were similar to our study, AA women in that cohort were more likely to report higher levels of religiosity/spirituality, and there was a negative association between religiosity/spirituality and smoking. 13 In our study, higher religiosity/spirituality was associated with a higher likelihood of achieving intermediate or ideal smoking status (either quitting or never smoking) across all domains of religiosity/spirituality. This observation may indicate that religiosity/spirituality, as practices or habits of thought, has stronger links or parallels to modifiable CVH behaviors (eg, tobacco use) than to CVH biological factors (eg, cholesterol, glucose). This finding may also reflect underreporting by participants of sinful or morally objectionable health behaviors under religiosity/spirituality doctrine. 23 , 31 In concordance with a previous study of JHS participants, religiosity/spirituality was not cross‐sectionally related to weight or obesity indicators (ie, BMI) within our analyses. 23 A ceiling effect of high religiosity/spirituality on weight/BMI may exist across the sample as seen in other similar populations of AAs. 32 The lack of association between higher religiosity/spirituality and intermediate/ideal BMI may represent an underlying lack of motivation or confidence in ability to lose weight by some individuals or a sequela of traditional culture and environment of some AA churches (ie, high‐calorie or high‐portion‐sized meals at church‐based events leading to higher BMI). Given the link between obesity (higher BMI) and related risk factors (dyslipidemia, diabetes), 33 our comparable results for cholesterol and glucose are not of surprise.
Studies have shown inconsistent relationships between religiosity/spirituality and metabolic risk factors such as lipid and glucose levels for AAs specifically. 13 , 34 We speculate that the lack of association between religiosity/spirituality and serum markers such as cholesterol and glucose could indicate that more nuanced examinations of further religiosity constructs are necessary beyond those examined in this study. Religious health fatalism or the “belief that health outcomes are inevitable and/or determined by God” may have a deleterious impact on CVH. 35 A subscale of this religiosity measurement, helpless inevitability, has been associated with self‐reported elevated cholesterol in churchgoing AAs. 36 Although challenging to determine directionality, individuals with higher helpless inevitability may have difficulty with health‐promoting behaviors to promote cholesterol management. Therefore, it is unclear whether fatalistic beliefs cause certain health outcomes or if fatalistic beliefs occur as a result of poor health, for example. Similar to our study, measures of religious involvement (eg, prayer) lacked significant associations with elevated cholesterol. Glover et al 37 demonstrated that religious practices were not associated with prevalent type 2 diabetes among AAs enrolled in the JHS, also suggesting that further inquiry of specific religiosity/spirituality domains is warranted. We caution about overinterpretation of findings related to religiosity/spirituality and indicators of cardiometabolic risk as these are also influenced by the presence of other comorbidities (eg, autoimmune and rheumatologic disorders, etc) and potentially medical treatment (or lack thereof) of hyperlipidemia and type 2 diabetes. 38 , 39 However, there is a large proportion of individuals diagnosed with a chronic illness who may also be working diligently toward improving their overall CVH (incorporating fruits/vegetables into their diet and maintaining regular PA), which is supported by our findings.
To our knowledge, this is the first study to investigate the association of a comprehensive set of CVH behaviors and biological factors with religiosity/spirituality among AAs. An intriguing finding in the current study is the relationship between higher levels of religiosity/spirituality and discrete LS7 components traditionally found at suboptimal levels in AAs—PA, diet, and BP. 40 These results demonstrate that there remains a great deal to learn about the contribution of religiosity/spirituality on CVH in this population. Nonetheless, our study fills a gap in the literature by providing additional evidence that religiosity/spirituality exerts independent, beneficial effects on CVH.
There were noteworthy findings of effect modification of religiosity/spirituality measures by sex and age. The postulated pathway of the demonstrated magnified positive effect of dimensions of religiosity on overall CVH within men could suggest that men disproportionately express their religiosity through action compared with women. 41 Thus, men possibly translated these forms of “religiousness” to overall CVH health‐promoting behaviors and factors. The significant effect modification of spirituality measures with diet by age group in this study is a novel finding, as no literature to date has examined this relationship in detail among AAs. This could represent differing manners that younger (versus older) generations reconcile their faith through spirituality (connection to the divine) as identity formation, sense of purpose, and a way of life, which in turn influences their health behaviors. 42 , 43 , 44 , 45 , 46 , 47
Our hypothesis was supported by our findings, and there are various explanatory mechanisms by which stronger religiosity/spirituality practices may account for better CVH. One is that religious service attendance may increase people's exposure to messaging such as sermons and bible studies that integrate health and wellness topics, which in turn influences their health behaviors. 48 Another proposed mechanism is that intrinsic social support, optimistic orientation, and social services provided by religious institutions may encourage positive health behaviors. 30 , 49 , 50 , 51 In addition, higher religiosity/spirituality may encourage health care use for preventive health services both within and outside the church setting, which could lead to better cardiovascular risk factor management. 52 , 53 Furthermore, religiosity/spirituality may promote positive self‐care practices by enhancing one's ability to refrain from unhealthy behaviors in accordance with religious doctrine. 49 , 54
Our results convey important implications for CVH promotion among AAs. The high prevalence of religiosity/spirituality among AAs in our study is consistent with prior investigations. 55 This presents an opportunity to incorporate religiosity/spirituality components into culturally tailored behavioral interventions that are both age and sex appropriate to bolster their effectiveness. Future faith‐based lifestyle interventions may consider the adaptation or integration of specific religiosity/spirituality measures (eg, religious attendance, religious coping, and nontheistic spirituality) that appear to exert the most significant effects on several LS7 components (Figure 3). Church pastors can play a major role as allies for intervention implementation within AA churches to promote religious and spiritually infused messages of prevention. Our findings also support the substantial role of AA churches in CVH promotion initiatives toward a goal of CVD prevention in an extremely high‐risk group. 56 , 57 AA churches have been the cornerstone of health‐promotion programming through community‐based interventions. 56 , 58 , 59 , 60 , 61 , 62 Our previous research demonstrating improvements in CVH by targeting multiple cardiovascular risk factors through the AHA LS7 framework and AA church‐based social networks supports integration of more culturally relevant religiosity/spirituality elements to promote ideal CVH in this population. 59 , 63 Also, religiosity/spirituality may impart benefits of social and emotional stability, stress buffering, and optimism during times of crises such as the current global coronavirus disease 2019 pandemic and resurgence of racial turmoil and social unrest, which could foster and facilitate maintenance of CVH. 50 , 64 , 65 Given clear clinical gaps in access to quality health care and health information among socioeconomically disadvantaged populations, particularly AAs, culturally tailored health promotion interventions in partnership with faith‐based organizations may serve to assist in fulfilling these unmet needs. 66
Figure 3.
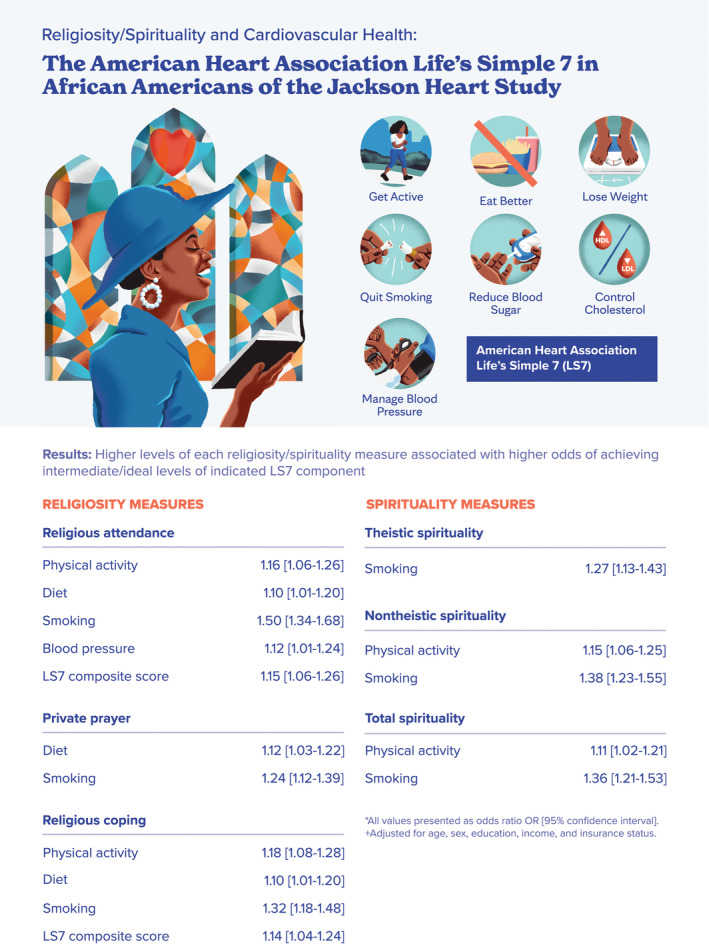
Religiosity and spirituality measures and the American Heart Association Life's Simple 7 (LS7) components.
Furthermore, our findings lend support to the recognition of the influence of religiosity/spirituality on CVH by health professionals as a means to attenuate CVH disparities through sociocultural understanding and enhancement of the patient‐physician relationship. Health care providers have expressed ethical concerns about coercion or projecting beliefs onto patients and associated time constraints with religiosity/spirituality inquiry. 67 , 68 However, there is evidence supporting patients' preference that respectful conversations surrounding religiosity/spirituality spur from comprehensive psychosocial history taking, particularly in routine medical care or screening, rather than solely during end‐of‐life care discussions. 67 Understandably, clinicians have limited time in clinical encounters, however studies have demonstrated that assessing religiosity/spirituality as a part of the psychosocial history does not necessarily lead to longer visits. 69 , 70 , 71 In fact, the Joint Commission on Accreditation of Healthcare Organizations endorses brief, culturally sensitive spiritual assessments under its behavioral health care standards, which is of particular importance in AAs. 72 , 73 Referrals to trained chaplains serve as excellent resources when religiosity/spirituality topics go beyond the competence or comfort level of the clinician. 67 , 68 Incorporation of this patient‐centered approach maintains patient autonomy to engage in discussions surrounding their religiosity/spirituality beliefs and demonstrates acknowledgement by the health care team of the patient's faith‐based practices while upholding the highest standard of ethical medical care. 68 In addition, our study findings may inform the future development of more culturally relevant tools to better categorize religiosity/spirituality status on public and population health levels to improve CVH outcomes in diverse populations.
Strengths and Limitations
This study has several strengths. The JHS is the largest study of CVD risk factors among AAs. CVH was adjudicated by rigorous methods including standardized data collection protocols by trained personnel and validated questionnaires. Furthermore, our robust assessment of multiple religiosity/spirituality domains allowed us to examine the extent to which unique religiosity/spirituality domains influence CVH. The study also has some limitations. Our cross‐sectional design allowed for evaluation of CVH metrics only at baseline; thus, longitudinal changes in LS7 metrics and causal inferences could not be determined. Participants included in this analysis tended to have better CVH than those excluded, which could potentially lead to an underestimation of associations between religiosity/spirituality and CVH metrics. 74 , 75 In addition, people with existing CVD were not included, which could provide insights into the influence of religiosity/spirituality on clinical outcomes in this population. Such analysis was beyond the scope of the current investigation because the AHA LS7 framework was principally developed for the prevention of CVD. Finally, because the study was limited to 1 metropolitan area, our findings lack generalizability to AAs in other regions of the United States. Nonetheless, our study enhances our understanding of religiosity/spirituality as a psychosocial asset that influences CVH in a population that experiences substantial disparities in social determinants and health outcomes.
Conclusions
In this large sample of community‐dwelling AAs, those with higher religiosity/spirituality were found to have intermediate/ideal CVH across multiple indicators of the AHA LS7, which persisted after multivariable adjustment for sociodemographic factors, chronic stress, and social network. Recognition and reinforcement of religiosity/spirituality in health care, along with culturally relevant lifestyle interventions (for people or groups finding such approaches acceptable), may decrease the overall cardiometabolic risk of CVD among AAs, thus mitigating CVH disparities.
Sources of Funding
This publication was supported by the Clinical and Translational Science Awards (Grant No. UL1 TR000135) from the National Center for Advancing Translational Sciences to Mayo Clinic and the Mayo Clinic Center for Health Equity and Community Engagement in Research, the American Heart Association‐Amos Medical Faculty Development Program (Grant No. 19AMFDP35040005), National Center for Advancing Translational Sciences (Clinical and Translational Science Awards Grant No. KL2 TR002379), the National Institutes of Health/National Institute on Minority Health and Health Disparities (Grant No. 1 R21 MD013490‐01), and the Centers for Disease Control and Prevention (Grant No. CDC‐DP18‐1817) during the implementation of this work.
The Jackson Heart Study is supported and conducted in collaboration with Jackson State University (HHSN268201800013I), Tougaloo College (HHSN268201800014I), the Mississippi State Department of Health (HHSN268201800015I), and the University of Mississippi Medical Center (HHSN268201800010I, HHSN268201800011I, and HHSN268201800012I) contracts from the National Institutes of Health/National Heart, Lung, and Blood Institute, and the National Institutes of Health/National Institute on Minority Health and Health Disparities. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of National Center for Advancing Translational Sciences, National Institutes of Health, US Department of Health and Human Services, or the Centers for Disease Control and Prevention.
Disclosures
None.
Supporting information
Tables S1–S8
Acknowledgments
We thank the staff and participants of the Jackson Heart Study. The authors also thank Nic Breutzman for assistance with graphic design.
For Sources of Funding and Disclosures, see page 12.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.121.024974
References
- 1. Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA Jr, Willis M, et al. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136:e393–e423. doi: 10.1161/CIR.0000000000000534 [DOI] [PubMed] [Google Scholar]
- 2. Bambs C, Kip KE, Dinga A, Mulukutla SR, Aiyer AN, Reis SE. Low prevalence of "ideal cardiovascular health" in a community‐based population: the heart strategies concentrating on risk evaluation (heart SCORE) study. Circulation. 2011;123:850–857. doi: 10.1161/CIRCULATIONAHA.110.980151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lloyd‐Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 4. Ommerborn MJ, Blackshear CT, Hickson DA, Griswold ME, Kwatra J, Djousse L, Clark CR. Ideal cardiovascular health and incident cardiovascular events: the Jackson heart study. Am J Prev Med. 2016;51:502–506. doi: 10.1016/j.amepre.2016.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD, Investigators AS . Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696. doi: 10.1016/j.jacc.2010.11.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Spahillari A, Talegawkar S, Correa A, Carr JJ, Terry JG, Lima J, Freedman JE, Das S, Kociol R, de Ferranti S, et al. Ideal cardiovascular health, cardiovascular remodeling, and heart failure in blacks: the Jackson heart study. Circ Heart Fail. 2017;10. doi: 10.1161/CIRCHEARTFAILURE.116.003682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kulshreshtha A, Vaccarino V, Judd SE, Howard VJ, McClellan WM, Muntner P, Hong Y, Safford MM, Goyal A, Cushman M. Life's simple 7 and risk of incident stroke: the reasons for geographic and racial differences in stroke study. Stroke. 2013;44:1909–1914. doi: 10.1161/STROKEAHA.111.000352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Unkart JT, Allison MA, Criqui MH, McDermott MM, Wood AC, Folsom AR, Lloyd‐Jones D, Rasmussen‐Torvik LJ, Allen N, Burke G, et al. Life's simple 7 and peripheral artery disease: the multi‐ethnic study of atherosclerosis. Am J Prev Med. 2019;56:262–270. doi: 10.1016/j.amepre.2018.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shattuck EC, Muehlenbein MP. Religiosity/spirituality and physiological markers of health. J Relig Health. 2020;59:1035–1054. doi: 10.1007/s10943-018-0663-6 [DOI] [PubMed] [Google Scholar]
- 10. Angell SY, McConnell MV, Anderson CAM, Bibbins‐Domingo K, Boyle DS, Capewell S, Ezzati M, de Ferranti S, Gaskin DJ, Goetzel RZ, et al. The American Heart Association 2030 impact goal: a presidential advisory from the American Heart Association. Circulation. 2020;141:e120–e138. doi: 10.1161/CIR.0000000000000758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pew Research Center . Religious landscape study: racial and ethnic composition. 2014. Available at: https://www.pewforum.org/religious‐landscape‐study/racial‐and‐ethnic‐composition/. Accessed March 9, 2022.
- 12. Pew Research Center . A religious portrait of African‐Americans. 2009. Available at: https://www.pewforum.org/2009/01/30/a‐religious‐portrait‐of‐african‐americans/. Accessed March 9, 2022.
- 13. Feinstein M, Liu K, Ning H, Fitchett G, Lloyd‐Jones DM. Burden of cardiovascular risk factors, subclinical atherosclerosis, and incident cardiovascular events across dimensions of religiosity: the multi‐ethnic study of atherosclerosis. Circulation. 2010;121:659–666. doi: 10.1161/CIRCULATIONAHA.109.879973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lucchetti G, Lucchetti AL. Spirituality, religion, and health: over the last 15 years of field research (1999‐2013). Int J Psychiatry Med. 2014;48:199–215. doi: 10.2190/PM.48.3.e [DOI] [PubMed] [Google Scholar]
- 15. Li S, Stampfer MJ, Williams DR, VanderWeele TJ. Association of religious service attendance with mortality among women. JAMA Intern Med. 2016;176:777–785. doi: 10.1001/jamainternmed.2016.1615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bentley‐Edwards KL, Blackman Carr LT, Robbins PA, Conde E, Zaw K, Darity WA Jr. Investigating denominational and church attendance differences in obesity and diabetes in Black Christian men and women. J Relig Health. 2020;59:3055–3070. doi: 10.1007/s10943-019-00888-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Taylor HA Jr, Wilson JG, Jones DW, Sarpong DF, Srinivasan A, Garrison RJ, Nelson C, Wyatt SB. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson heart study. Ethn Dis. 2005;15:S6–S17. [PubMed] [Google Scholar]
- 18. Payne TJ, Wyatt SB, Mosley TH, Dubbert PM, Guiterrez‐Mohammed ML, Calvin RL, Taylor HA Jr, Williams DR. Sociocultural methods in the Jackson heart study: conceptual and descriptive overview. Ethn Dis. 2005;15:S6–S38. [PubMed] [Google Scholar]
- 19. Fuqua SR, Wyatt SB, Andrew ME, Sarpong DF, Henderson FR, Cunningham MF, Taylor HA Jr. Recruiting African‐American research participation in the Jackson heart study: methods, response rates, and sample description. Ethn Dis. 2005;15:S6–S18. [PubMed] [Google Scholar]
- 20. Loustalot F, Wyatt SB, Sims M, Ellison CG, Taylor HA, Underwood L. Psychometric testing of the daily spiritual experiences scale among African Americans in the Jackson heart study. J Relig Health. 2011;50:675–685. doi: 10.1007/s10943-009-9278-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fetzer Institute, National Institute on Aging . Multidimensional Measurement of Religiousness/Spirituality for Use in Health Research. Kalamazoo, MI: Fetzer Institute; 1999. [Google Scholar]
- 22. Pargament KI, Koenig HG, Perez LM. The many methods of religious coping: development and initial validation of the RCOPE. J Clin Psychol. 2000;56:519–543. doi: [DOI] [PubMed] [Google Scholar]
- 23. Reeves RR, Adams CE, Dubbert PM, Hickson DA, Wyatt SB. Are religiosity and spirituality associated with obesity among African Americans in the southeastern United States (the Jackson heart study)? J Relig Health. 2012;51:32–48. doi: 10.1007/s10943-011-9552-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Underwood LG, Teresi JA. The daily spiritual experience scale: development, theoretical description, reliability, exploratory factor analysis, and preliminary construct validity using health‐related data. Ann Behav Med. 2002;24:22–33. doi: 10.1207/S15324796ABM2401_04 [DOI] [PubMed] [Google Scholar]
- 25. Brewer LC, Redmond N, Slusser JP, Scott CG, Chamberlain AM, Djousse L, Patten CA, Roger VL, Sims M. Stress and achievement of cardiovascular health metrics: the American Heart Association Life's simple 7 in blacks of the Jackson heart study. J Am Heart Assoc. 2018;7. doi: 10.1161/JAHA.118.008855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shay CM, Ning H, Allen NB, Carnethon MR, Chiuve SE, Greenlund KJ, Daviglus ML, Lloyd‐Jones DM. Status of cardiovascular health in US adults: prevalence estimates from the National Health and nutrition examination surveys (NHANES) 2003‐2008. Circulation. 2012;125:45–56. doi: 10.1161/CIRCULATIONAHA.111.035733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sims M, Diez‐Roux AV, Dudley A, Gebreab S, Wyatt SB, Bruce MA, James SA, Robinson JC, Williams DR, Taylor HA. Perceived discrimination and hypertension among African Americans in the Jackson heart study. Am J Public Health. 2012;102(Suppl 2):S258–S265. doi: 10.2105/AJPH.2011.300523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Berkman LF, Vaccarino V, Seeman T. Gender differences in cardiovascular morbidity and mortality: the contribution of social networks and support. Ann Behav Med. 1993;15:112–118. [Google Scholar]
- 29. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: L. Erlbaum Associates; 1988. [Google Scholar]
- 30. Debnam K, Holt CL, Clark EM, Roth DL, Southward P. Relationship between religious social support and general social support with health behaviors in a national sample of African Americans. J Behav Med. 2012;35:179–189. doi: 10.1007/s10865-011-9338-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Clark EM, Williams BR, Huang J, Roth DL, Holt CL. A longitudinal study of religiosity, spiritual health locus of control, and health behaviors in a National Sample of African Americans. J Relig Health. 2018;57:2258–2278. doi: 10.1007/s10943-017-0548-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bauer AG, Berkley‐Patton J, Bowe‐Thompson C, Ruhland‐Petty T, Berman M, Lister S, Christensen K. Do Black Women's religious beliefs about body image influence their confidence in their ability to lose weight? Prev Chronic Dis. 2017;14:E98. doi: 10.5888/pcd14.170153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Powell‐Wiley TM, Banks‐Richard K, Williams‐King E, Tong L, Ayers CR, de Lemos JA, Gimpel N, Lee JJ, DeHaven MJ. Churches as targets for cardiovascular disease prevention: comparison of genes, nutrition, exercise, wellness and spiritual growth (GoodNEWS) and Dallas County populations. J Public Health. 2013;35:99–106. doi: 10.1093/pubmed/fds060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Obisesan T, Livingston I, Trulear HD, Gillum F. Frequency of attendance at religious services, cardiovascular disease, metabolic risk factors and dietary intake in Americans: an age‐stratified exploratory analysis. Int J Psychiatry Med. 2006;36:435–448. doi: 10.2190/9W22-00H1-362K-0279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Franklin MD, Schlundt DG, McClellan LH, Kinebrew T, Sheats J, Belue R, Brown A, Smikes D, Patel K, Hargreaves M. Religious fatalism and its association with health behaviors and outcomes. Am J Health Behav. 2007;31:563–572. doi: 10.5555/ajhb.2007.31.6.563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. de Dios MA, Childress SD, Cano M, McNeill LH, Reitzel LR, Vaughan E. Elevated cholesterol among African American adults: the role of fatalistic attitudes about health. Ethn Health. 2020;25:835–842. doi: 10.1080/13557858.2018.1469734 [DOI] [PubMed] [Google Scholar]
- 37. Glover LM, Bertoni AG, Golden SH, Baltrus P, Min YI, Carnethon MR, Taylor H, Sims M. Sex differences in the association of psychosocial resources with prevalent type 2 diabetes among African Americans: the Jackson heart study. J Diabetes Complications. 2019;33:113–117. doi: 10.1016/j.jdiacomp.2018.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Appel SJ, Oster RA, Floyd NA, Ovalle F. Cardiometabolic risk among African American women: a pilot study. J Cardiovasc Nurs. 2009;24:140–150. doi: 10.1097/JCN.0b013e318197aa3a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Alfaddagh A, Martin SS, Leucker TM, Michos ED, Blaha MJ, Lowenstein CJ, Jones SR, Toth PP. Inflammation and cardiovascular disease: from mechanisms to therapeutics. Am J Prev Cardiol. 2020;4:100130. doi: 10.1016/j.ajpc.2020.100130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Djousse L, Petrone AB, Blackshear C, Griswold M, Harman JL, Clark CR, Talegawkar S, Hickson DA, Gaziano JM, Dubbert PM, et al. Prevalence and changes over time of ideal cardiovascular health metrics among African‐Americans: the Jackson heart study. Prev Med. 2015;74:111–116. doi: 10.1016/j.ypmed.2015.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Paul Sullins D. Gender and religion: deconstructing universality, constructing complexity. Am J Sociol. 2006;112:838–880. doi: 10.1086/507852 [DOI] [Google Scholar]
- 42. Wright AM. Spiritual Lives of Young African Americans. New York, NY: Oxford University Press; 2017. [Google Scholar]
- 43. Reed TD, Neville HA. The influence of religiosity and spirituality on psychological well‐being among Black women. J Black Psychol. 2014;40:384–401. doi: 10.1177/0095798413490956 [DOI] [Google Scholar]
- 44. Pew Research Center . Faith among Black Americans, 2021. Available at: https://www.pewforum.org/2021/02/16/faith‐among‐black‐americans/. Accessed March 9, 2022.
- 45. The Washington Post . Creating a space for black millennials to discuss their spirituality, 2018. Available at: https://www.washingtonpost.com/local/social‐issues/creating‐a‐space‐for‐black‐millennials‐to‐talk‐spirituality/2018/08/24/e8f6a01a‐a71a‐11e8‐8fac‐12e98c13528d_story.html. Accessed March 9, 2022.
- 46. WCNC Charlotte. More Black Millennials are Turning Away from Traditional Religion to Find Their Spirituality, 2020. Retrieved from: https://www.washingtonpost.com/local/social‐issues/creating‐a‐space‐for‐black‐millennials‐to‐talk‐spirituality/2018/08/24/e8f6a01a‐a71a‐11e8‐8fac‐12e98c13528d_story.html. Accessed March 9, 2022. [Google Scholar]
- 47. Vox Media . How Some Black Americans are Finding Solace in African Spirituality, 2020. Available at: https://www.vox.com/2020/7/31/21346686/orisha‐yoruba‐african‐spirituality‐covid. Accessed March 9, 2022. [Google Scholar]
- 48. Dessio W, Wade C, Chao M, Kronenberg F, Cushman LE, Kalmuss D. Religion, spirituality, and healthcare choices of African‐American women: results of a national survey. Ethn Dis. 2004;14:189–197. [PubMed] [Google Scholar]
- 49. Holt CL, Roth DL, Huang J, Clark EM. Role of religious social support in longitudinal relationships between religiosity and health‐related outcomes in African Americans. J Behav Med. 2018;41:62–73. doi: 10.1007/s10865-017-9877-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Modell SM, Kardia SLR. Religion as a health promoter during the 2019/2020 COVID outbreak: view from Detroit. J Relig Health. 2020;59:2243–2255. doi: 10.1007/s10943-020-01052-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sims M, Glover LM, Norwood AF, Jordan C, Min YI, Brewer LC, Kubzansky LD. Optimism and cardiovascular health among African Americans in the Jackson heart study. Prev Med. 2019;129:105826. doi: 10.1016/j.ypmed.2019.105826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Benjamins MR, Ellison CG, Krause NM, Marcum JP. Religion and preventive service use: do congregational support and religious beliefs explain the relationship between attendance and utilization? J Behav Med. 2011;34:462–476. doi: 10.1007/s10865-011-9318-8 [DOI] [PubMed] [Google Scholar]
- 53. Pullins CT, Seele PC, White RO, Willis FB, Poole K, Albertie ML, Chamie C, Allen AM, Kelly M, Penheiter S, et al. Health behaviors and preventive healthcare utilization among African‐American attendees at a faith‐based public health conference: healthy churches 2020. J Relig Health. 2018;57:2538–2551. doi: 10.1007/s10943-018-0667-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Abu HO, Ulbricht C, Ding E, Allison JJ, Salmoirago‐Blotcher E, Goldberg RJ, Kiefe CI. Association of religiosity and spirituality with quality of life in patients with cardiovascular disease: a systematic review. Qual Life Res. 2018;27:2777–2797. doi: 10.1007/s11136-018-1906-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Taylor RJ, Chatters LM, Levin J. Religion in the Lives of African Americans: Social, Psychological, and Health Perspectives. Thousand Oaks, CA: SAGE Publications; 2004. doi: 10.4135/9781452229782 [DOI] [Google Scholar]
- 56. Brewer LC, Williams DR. We've come this far by faith: the role of the Black Church in Public Health. Am J Public Health. 2019;109:385–386. doi: 10.2105/AJPH.2018.304939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Diaz CL, Shah NS, Lloyd‐Jones DM, Khan SS. State of the Nation's cardiovascular health and targeting health equity in the United States: a narrative review. JAMA Cardiol. 2021;6:963–970. doi: 10.1001/jamacardio.2021.1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Elgazzar R, Nolan TS, Joseph JJ, Aboagye‐Mensah EB, Azap RA, Gray DM 2nd. Community‐engaged and community‐based participatory research to promote American Heart Association Life's simple 7 among African American adults: a systematic review. PLoS One. 2020;15:e0238374. doi: 10.1371/journal.pone.0238374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Brewer LC, Hayes SN, Jenkins SM, Lackore KA, Breitkopf CR, Cooper LA, Patten CA. Improving cardiovascular health among African‐Americans through Mobile health: the FAITH! App pilot study. J Gen Intern Med. 2019;34:1376–1378. doi: 10.1007/s11606-019-04936-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Schoenthaler AM, Lancaster KJ, Chaplin W, Butler M, Forsyth J, Ogedegbe G. Cluster randomized clinical trial of FAITH (FAITH‐based approaches in the treatment of hypertension) in blacks. Circ Cardiovasc Qual Outcomes. 2018;11:e004691. doi: 10.1161/CIRCOUTCOMES.118.004691 [DOI] [PubMed] [Google Scholar]
- 61. Bauer AG, Berkley‐Patton J, Bennett K, Catley D, Bowe‐Thompson C, Lister S, Christensen K. Dietary intake among church‐affiliated African Americans: the role of intentions and beliefs. J Black Psychol. 2020;46:29–54. doi: 10.1177/0095798419887629 [DOI] [Google Scholar]
- 62. Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church‐based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213–234. doi: 10.1146/annurev.publhealth.28.021406.144016 [DOI] [PubMed] [Google Scholar]
- 63. Brewer LC, Balls‐Berry JE, Dean P, Lackore K, Jenkins S, Hayes SN. Fostering African‐American improvement in Total health (FAITH!): an application of the American Heart Association's Life's simple 7 among midwestern African‐Americans. J Racial Ethn Health Disparities. 2017;4:269–281. doi: 10.1007/s40615-016-0226-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Koenig HG. Maintaining health and well‐being by putting faith into action during the COVID‐19 pandemic. J Relig Health. 2020;59:2205–2214. doi: 10.1007/s10943-020-01035-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. DeSouza F, Parker CB, Spearman‐McCarthy EV, Duncan GN, Black RMM. Coping with racism: a perspective of COVID‐19 church closures on the mental health of African Americans. J Racial Ethn Health Disparities. 2021;8:7–11. doi: 10.1007/s40615-020-00887-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. May I, George N. Faith Community nursing: faith element enhances cardiovascular risk reduction program outcomes. J Christ Nurs. 2021;38:38–46. doi: 10.1097/cnj.0000000000000788 [DOI] [PubMed] [Google Scholar]
- 67. Hebert RS, Jenckes MW, Ford DE, O'Connor DR, Cooper LA. Patient perspectives on spirituality and the patient‐physician relationship. J Gen Intern Med. 2001;16:685–692. doi: 10.1111/j.1525-1497.2001.01034.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Levin J, Chatters LM, Taylor RJ. Religion, health and medicine in African Americans: implications for physicians. J Natl Med Assoc. 2005;97:237–249. [PMC free article] [PubMed] [Google Scholar]
- 69. Levinson W, Roter D. Physicians' psychosocial beliefs correlate with their patient communication skills. J Gen Intern Med. 1995;10:375–379. doi: 10.1007/bf02599834 [DOI] [PubMed] [Google Scholar]
- 70. Roter DL, Hall JA, Kern DE, Barker LR, Cole KA, Roca RP. Improving physicians' interviewing skills and reducing patients' emotional distress. A randomized clinical trial. Arch Intern Med. 1995;155:1877–1884. doi: 10.1001/archinte.1995.00430170071009 [DOI] [PubMed] [Google Scholar]
- 71. Behforouz HL, Drain PK, Rhatigan JJ. Rethinking the social history. N Engl J Med. 2014;371:1277–1279. doi: 10.1056/NEJMp1404846 [DOI] [PubMed] [Google Scholar]
- 72. Hodge DR. A template for spiritual assessment: a review of the JCAHO requirements and guidelines for implementation. Soc Work. 2006;51:317–326. doi: 10.1093/sw/51.4.317 [DOI] [PubMed] [Google Scholar]
- 73. Joint Commission: The Source . Body, mind, spirit, Part 2 hospital chaplains contribute to patient satisfaction and well‐being Part 2. February 2018, Volume 16, Issue 2. Available at: https://www.nacc.org/wp‐content/uploads/2018/01/Part‐2.‐Body‐Mind‐Spirit‐JC‐The‐Source‐Feb.2018‐Vol.16.2.pdf. Accessed March 9, 2022.
- 74. Samieri C, Perier MC, Gaye B, Proust‐Lima C, Helmer C, Dartigues JF, Berr C, Tzourio C, Empana JP. Association of Cardiovascular Health Level in older age with cognitive decline and incident dementia. JAMA. 2018;320:657–664. doi: 10.1001/jama.2018.11499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Liang Y, Ngandu T, Laatikainen T, Soininen H, Tuomilehto J, Kivipelto M, Qiu C. Cardiovascular health metrics from mid‐ to late‐life and risk of dementia: a population‐based cohort study in Finland. PLoS Med. 2020;17:e1003474. doi: 10.1371/journal.pmed.1003474 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S8


