Abstract
Marginal zone B-cell lymphoma (MZBCL) of mucosa-associated lymphoid tissue (MALT) type, which is primary to the central nervous system (CNS), is a rare lesion, with those originating within the parenchyma even more so. We present the case of a 64-year-old male with weakness in the left hand and focal motor seizures of his arm, who was found to have a right frontal intraparenchymal lesion. Following resection, histopathological and immunohistochemical evaluations were completed, leading to a diagnosis of a primary CNS MZBCL of MALT type in the context of a negative workup of systemic disease. Neuroimaging, histopathological, and immunohistochemical findings, as well as a comprehensive literature review of similar cases, are discussed.
Keywords: surgical case report, intraparenchymal, marginal zone b cell lymphoma, cns lymphoma, cns lesions, mucosa-associated lymphoid tissue (malt), mucosa-associated lymphoid tissue (malt) lymphoma
Introduction
Primary central nervous system lymphoma (PCNSL) is an aggressive yet rare variant of extranodal non-Hodgkin lymphomas, accounting for roughly 4% of primary and malignant tumors of the CNS [1]. They mainly arise from the brain, leptomeninges, spinal cord, and vitreoretinal compartment of the eye [2]. Approximately 90% of cases reported as PCNSL are diffuse large B-cell lymphomas, leaving small B-cell lymphomas in the minority [3].
Under the category of small B-cell lymphomas, marginal zone lymphomas (MZL) represent the majority of neoplasms that are primary to the CNS [4]. Mucosa-associated lymphoid tissue (MALT) lymphoma as a subtype of MZL, originally described as low-grade lymphomas within the gastrointestinal tract, is primarily found within the stomach but is also commonly found within salivary glands, the thyroid, ocular adnexa, lungs, and breasts [5,6]. However, primary CNS MALT lymphomas are rare.
Tu et al. reported 15 primary CNS MZL cases, of which 93% were dural-based lesions mimicking meningiomas, arising from sites including the convexity of the brain, falx, tentorium, middle skull base, ventricles, and spinal dura mater [7]. Primary CNS MZL lesions that arise from the parenchyma, however, are exceptionally rare and can be misdiagnosed as gliomas in certain patients [8].
We present a case of a patient with primary CNS intraparenchymal MALT lymphoma with an immunohistochemical profile. Furthermore, a review of the literature on similar cases, including treatment options and outcomes, is discussed. To our knowledge, the present case represents the first reported instance of a patient with such a lesion to be managed solely with surgical resection.
Case presentation
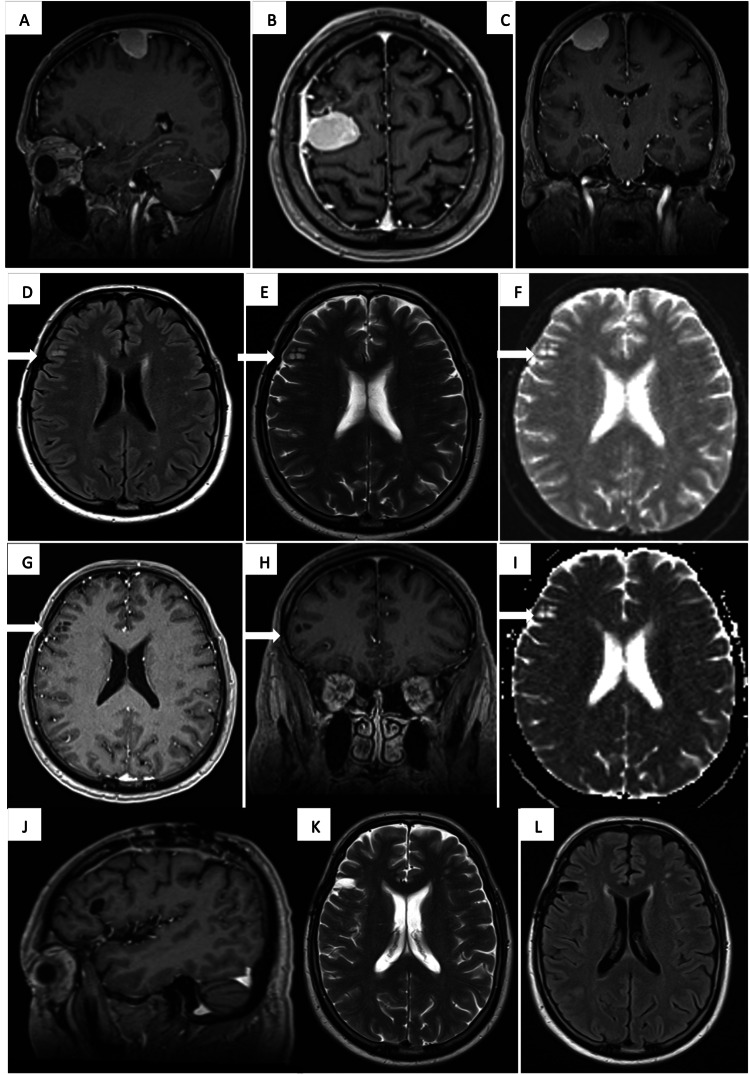
A 64-year male with a history of rheumatoid arthritis and anti-phospholipid syndrome presented with mild left-hand weakness and a focal motor seizure involving his arm. The patient was receiving hydroxychloroquine for his rheumatoid arthritis and no biologic agents were used to our knowledge. He was found to have an extra-axial mass overlying the posterior right frontal lobe at the convexity, measuring approximately 2.3 x 2.7 x 2.3 cm (anteroposterior (AP) x transverse (TR) x craniocaudal (CC)), and an intra-parenchymal lesion within the subcortical white matter of the right frontal lobe spanning approximately 0.8 x 1.1 cm with radiologic features consistent with a low-grade glial tumor (Figure 1).
Figure 1. Magnetic resonance imaging.
Panels A, B, and C demonstrate right frontal meningioma. Panels D and E represent the FLAIR and T2 sequence where the white arrows point to the lesion diagnosed as MZBCL of MALT type while panels F and I are the diffusion-weighted image and apparent diffusion coefficient. Axial and coronal T1 with gadolinium are shown in panels G and H, respectively. Panels J, K, and L show a follow-up MRI obtained nine months after surgery, which confirms there is no residual or recurrent lesion.
FLAIR: fluid-attenuated inversion recovery; MZBCL: marginal zone B-cell lymphoma; MALT: mucosa-associated lymphoid tissue
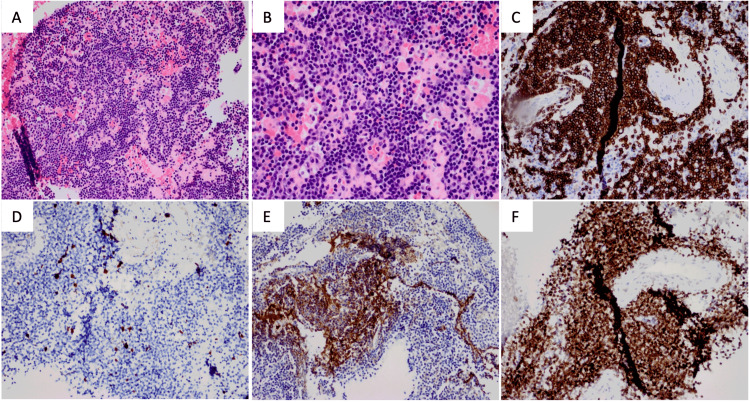
He was assessed by the hematology team and was cleared for surgery to resect these lesions. Neuropathologic assessment following surgical resection confirmed the diagnosis of meningioma for the convexity tumor. Histopathologic evaluation of the intraparenchymal lesion demonstrated diffuse lymphoplasmacytic infiltrate composed of small mature lymphocytes, plasmacytoid lymphocytes, and mature plasma cells. Immunohistochemistry showed that most cells were CD20-positive (B cells) with kappa light chain restriction. Ki-67 demonstrated a very modest proliferative index. The tumor was uniformly positive for BCL2 and negative for CD5, CD21, CD10, and cyclin-D1 (Figure 2). Finally, immunohistochemistry for synaptophysin and GFAP showed that the cellular infiltrate was non-reactive. This was diagnosed as an MZBCL of MALT type.
Figure 2. Microscopic and selected immunohistochemical stains.
Panels A and B show hematoxylin and eosin stain at medium (4x objective) and high power (20x), respectively. Immunohistochemistry for CD20 (C), ki67 (D), GFAP (E), and BCL2 (F) are also shown.
With the diagnosis of low-grade B-cell lymphoma, the patient subsequently had a bone marrow biopsy, CSF analysis, and lymph node biopsy, which did not show systemic disease. He was also found to be HIV and H. pylori-negative. To date, the patient has elected not to proceed with adjuvant therapies, and the nine-month follow-up MR and positron emission tomography imaging has confirmed no recurrent mass or adverse interval change within the parenchyma.
Discussion
Only a few cases of intracranial primary low-grade lymphomas of the MALT subtype have been reported in the literature, with the vast majority located in the dura mater. As the CNS does not contain any mucosal or MALT tissue, it has been hypothesized that the meningothelial cells in the brain are analogous to epithelial cells at other sites where MALT lymphoma typically arises [8]. However, it remains unclear how primary MZBCL can manifest in intraparenchymal tissue. Recently, an association has been found between autoimmune disease and MZBL [9]. Our patient had a history of both rheumatoid arthritis and antiphospholipid syndrome, giving rise to the possibility of a causative antigen stimulus process.
A review of the literature using the EMBASE and MEDLINE databases using the keywords of “MALT lymphoma” or “mucosa-associated lymphoid tissue lymphoma” and “brain tumors” primarily yielded previous cases of dural MALT lymphomas. In total, 13 cases were found in the literature of cases who were diagnosed with primary MZBCL of MALT type involving the brain parenchyma (Table 1) [7,8,10-16]. Five cases involved the frontal cortex, four in the parietal cortex, two involved the basal ganglia, and one the midbrain. The remaining studies reported a patient with multiple lesions involving the temporal and occipital cortex, as well as the spinal cord. With the exception of the patient diagnosed post-mortem via autopsy, all cases utilized either radiation or chemotherapy with only one patient receiving both radiation and surgery.
Table 1. Clinical summary of patients all with a final diagnosis of intraparenchymal MZBCL from the literature.
M: male; F: female; NED: no evidence of disease; AWD: alive with disease; DWD: dead with disease; NR: not reported; N/A: not applicable; MZBCL: marginal zone B-cell lymphoma
| Age/Gender | Location | Tumor Size | Presentation | Treatment | Outcome |
| 66/M [7] | Right frontal cortex | NR | Seizures | Surgery and Radiation | NED at 13 months |
| 48/M [8] | Left frontal cortex | 2.0 x 1.4 x 1.6 cm | Seizures and bilateral upper extremity weakness | Radiation | NED at 15 months |
| 18/M [10] | Left basal ganglia | 4.0 x 3.5 cm | Right-sided central facial nerve palsy, weakness, dizziness, and dysarthria | Radiation | NED at 22 months |
| 70/M [11] | Left posterior putamen, posterior subinsular region, mid-temporal region | 3.5 x 2.9 cm | Dysnomia, right arm and leg numbness, slurred speech, and blurry vision | Chemotherapy | No change in residual mass at 24 months |
| 45/M [12] | Right parietal cortex | NR | Seizures, left-sided weakness, and slurred speech | Radiation | NED at 64 months |
| 39/F [13] | Frontal lobe cortex | NR | Vision defects with nystagmus | Chemotherapy | AWD at 24 months |
| 53/M [14] | Right temporal, left occipital lobe, spinal cord | NR | Memory and gait disturbance with urinary incontinence | Chemotherapy | NED, unknown time |
| 65/F [15] | Parietal lobe | NR | Diagnosed post-mortem via autopsy | N/A | N/A |
| NR/M [15] | Parietal lobe | NR | NR | Chemotherapy | DWD at 38 months |
| NR/F [15] | Parietal lobe | NR | NR | Chemotherapy | AWD at 15 months |
| NR/F [15] | Frontal lobe | NR | NR | Radiation | DWD at 61 months |
| NR/F [15] | Frontal lobe | NR | NR | Chemotherapy | AWD at 40 months |
| 33/M [16] | Left midbrain | 1.9 x 1.8 cm | Left ptosis, right limb numbness, and weakness | Radiation | NED at 6 months |
| 64/M Present Case | Right frontal cortex | 0.8 x 1.1 cm | Left-hand weakness and focal motor seizure in arm | Surgery | NED at 9 months |
In addition to presenting a novel and interesting radiologic diagnosis, this case poses questions regarding the oncologic management of intraparenchymal MALT lymphomas. Currently, surgery, chemotherapy, radiation, or a combination of these modalities are used to treat CNS lymphomas. To our knowledge, our case represents the first reported instance of a patient with intraparenchymal MZBCL of MALT type to be managed solely with surgical resection. Our patient has remained disease-free at nine months postoperatively suggesting that adjuvant treatment may not be required in the initial management of intracranial MALT lymphoma in certain cases. Radiation and chemotherapy may cause significant neurotoxicity. Hence, cases need to be carefully evaluated on an individual basis to minimize iatrogenic sequelae from exposure to these therapies. Furthermore, given the propensity of MALT lymphomas to recur, this patient and others similarly affected, ought to be closely followed with serial MR imaging [17].
Conclusions
In conclusion, the results presented here indicate that primary MZBCL may not be isolated to the meninges and can develop in brain parenchyma. Thus, MZBCL should be considered in the differential diagnosis of intra-axial CNS masses. This case suggests that localized MZBCL may be managed with local excision without the need for early radiation or chemotherapy. However, more evidence is required to draw conclusions regarding the optimal management of this disease.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.How we treat primary central nervous system lymphoma. Calimeri T, Steffanoni S, Gagliardi F, Chiara A, Ferreri AJ. ESMO Open. 2021;6:100213. doi: 10.1016/j.esmoop.2021.100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Primary central nervous system lymphomas: a diagnostic overview of key histomorphologic, immunophenotypic, and genetic features. Lauw MI, Lucas CG, Ohgami RS, Wen KW. Diagnostics (Basel) 2020;10:1076. doi: 10.3390/diagnostics10121076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Swerdlow SH, Campo E, Pileri SA, et al. Blood. 2016;127:2375–2390. doi: 10.1182/blood-2016-01-643569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Extranodal marginal zone lymphoma of the central nervous system. Ayanambakkam A, Ibrahimi S, Bilal K, Cherry MA. Clin Lymphoma Myeloma Leuk. 2018;18:34–37. doi: 10.1016/j.clml.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 5.Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Isaacson P, Wright DH. Cancer. 1983;52:1410–1416. doi: 10.1002/1097-0142(19831015)52:8<1410::aid-cncr2820520813>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 6.Incidence of marginal zone lymphoma in the United States, 2001-2009 with a focus on primary anatomic site. Khalil MO, Morton LM, Devesa SS, Check DP, Curtis RE, Weisenburger DD, Dores GM. Br J Haematol. 2014;165:67–77. doi: 10.1111/bjh.12730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clinicopathologic and genetic profile of intracranial marginal zone lymphoma: a primary low-grade CNS lymphoma that mimics meningioma. Tu PH, Giannini C, Judkins AR, et al. J Clin Oncol. 2005;23:5718–5727. doi: 10.1200/JCO.2005.17.624. [DOI] [PubMed] [Google Scholar]
- 8.Primary CNS marginal zone lymphoma: a case report and review of the literature. Aqil B, Rouah E, Verstovsek G. Open J Pathol. 2013;3:55–59. [Google Scholar]
- 9.Salivary gland mucosa-associated lymphoid tissue lymphoma in 2 patients with Sjögren's syndrome: clinical and sonographic features with pathological correlation. Lewis K, Vandervelde C, Grace R, Ramesar K, Williams M, Howlett DC. J Clin Ultrasound. 2007;35:97–101. doi: 10.1002/jcu.20280. [DOI] [PubMed] [Google Scholar]
- 10.Primary central nervous system marginal zone B-cell lymphoma of the basal ganglia mimicking low-grade glioma: a case report and review of the literature. Park I, Huh J, Kim JH, Lee SW, Ryu MH, Kang YK. Clin Lymphoma Myeloma. 2008;8:305–308. doi: 10.3816/CLM.2008.n.043. [DOI] [PubMed] [Google Scholar]
- 11.Rare case of a primary non-dural central nervous system low grade B-cell lymphoma and literature review. Papanicolau-Sengos A, Wang-Rodriguez J, Wang HY, et al. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3267491/ Int J Clin Exp Pathol. 2012;5:89–95. [PMC free article] [PubMed] [Google Scholar]
- 12.Rare case of cerebral MALToma presenting with stroke-like symptoms and seizures. Wei D, Rich P, Bridges L, Martin AJ, Chau I, Bodi I, MacDonald BK. BMJ Case Rep. 2013;2013:0. doi: 10.1136/bcr-2012-008494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Extranodal marginal zone lymphoma of the CNS arising after a long-standing history of atypical white matter disease. Schiefer AI, Vastagh I, Molnar MJ, et al. Leuk Res. 2012;36:0–7. doi: 10.1016/j.leukres.2012.03.022. [DOI] [PubMed] [Google Scholar]
- 14.Central nervous system marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue type involving the brain and spinal cord parenchyma. Ueba T, Okawa M, Abe H, et al. Neuropathology. 2013;33:306–311. doi: 10.1111/j.1440-1789.2012.01350.x. [DOI] [PubMed] [Google Scholar]
- 15.Extranodal marginal zone lymphoma of the central nervous system includes parenchymal-based cases with characteristic features. Nomani L, Cotta CV, Hsi ED, Ferry JA, Cook JR. Am J Clin Pathol. 2020;154:124–132. doi: 10.1093/ajcp/aqaa032. [DOI] [PubMed] [Google Scholar]
- 16.Primary mucosa-associated lymphoid tissue lymphoma in the midbrain: a case report. Zhao YR, Hu RH, Wu R, Xu JK. World J Clin Cases. 2021;9:6566–6574. doi: 10.12998/wjcc.v9.i22.6566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue of the head and neck area: high rate of disease recurrence following local therapy. Wenzel C, Fiebiger W, Dieckmann K, Formanek M, Chott A, Raderer M. Cancer. 2003;97:2236–2241. doi: 10.1002/cncr.11317. [DOI] [PubMed] [Google Scholar]