Abstract
Easy and robust antimicrobial susceptibility testing (AST) methods are essential in clinical bacteriology laboratories (CBL) in low-resource settings (LRS). We evaluated the Beckman Coulter MicroScan lyophilized broth microdilution panel designed to support Médecins Sans Frontières (MSF) CBL activity in difficult settings, in particular with the Mini-Lab. We evaluated the custom-designed MSF MicroScan Gram-pos microplate (MICPOS1) for Staphylococcus and Enterococcus species, MSF MicroScan Gram-neg microplate (MICNEG1) for Gram-negative bacilli, and MSF MicroScan Fastidious microplate (MICFAST1) for Streptococci and Haemophilus species using 387 isolates from routine CBLs from LRS against the reference methods. Results showed that, for all selected antibiotics on the three panels, the proportion of the category agreement was above 90% and the proportion of major and very major errors was below 3%, as per ISO standards. The use of the Prompt inoculation system was found to increase the MIC and the major error rate for some antibiotics when testing Staphylococci. The readability of the manufacturer’s user manual was considered challenging for low-skilled staff. The inoculations and readings of the panels were estimated as easy to use. In conclusion, the three MSF MicroScan MIC panels performed well against clinical isolates from LRS and provided a convenient, robust, and standardized AST method for use in CBL in LRS.
Keywords: antibiotic susceptibility testing, low-resource settings, clinical bacteriology, MicroScan
1. Introduction
Antimicrobial resistance (AMR) is today universally recognized as a global threat, because of the rapid emergence and dissemination of resistant bacteria and genes among humans, animals, and the environment on a global scale. It represents a heavy burden for healthcare systems all over the world [1,2,3,4]; however, the situations in low- and middle-income countries (LMICs) are particularly concerning because of the limited availability of diagnostic/surveillance and clinical/control resources [5,6].
1.1. Antibiotic Susceptibility Testing in Low-Resource Settings
Developing evidence-based treatment guidelines and measuring the impacts of AMR control efforts require representative and comparable data for drug-resistant bacterial infections [7]. Yet, such data have proven extremely difficult to obtain in LMICs, despite the increasing evidence that AMR is rapidly escalating in these contexts [4,8,9,10,11,12]. Available data on AMR in LMICs lack standardized laboratory and data collection practices and are often not representative of populations outside of the main cities [13]. The limited access to adequate laboratory support, in some settings with low resources, contributes to the increase in antibiotic resistance and complicates the management of infections [14]. AMR poses a unique threat in LMICs, with the potential to reverse recent progress toward infectious disease control, to damage healthcare provision generally, and threaten the safety of essential health services, such as surgery to the most vulnerable and underserved populations [8,9,12].
In this article, we define low-resource setting(s) (LRS) as an area within a country with limited access to medication, equipment, supplies, and devices, with less-developed infrastructure (electrical power, transportation, controlled environment/buildings), fewer or less-trained laboratory personnel, basic diagnostic laboratory, no expert microbiologist, and with no (or hardly introduced) clinical bacteriology [15,16,17].
The deployment of conventional microbiology laboratories in LRS is challenging. It requires complex infrastructure, logistics, equipment, and specialized human resources, often lacking in LRS [17,18,19,20,21]. Affordable and effective point-of-care (POC) diagnostics, especially those that distinguish between viral and bacterial infections, identify pathogens, and provide antibiotic susceptibility testing (AST) are yet to materialize [12,22]. As a result, Médecins Sans Frontières (MSF) developed its own solution: the Mini-Lab. The Mini-Lab is a transportable, self-contained, quality-assured, stand-alone CBL adapted to low-resource settings. It can be operated by laboratory technicians without prior microbiology expertise except for a short, one-month training [23,24,25,26].
1.2. Development of Adapted AST Solution for LRS within the Context of Mini-Lab
AST techniques have been embarked in the Mini-Lab in order for their users to (1) improve case management of bloodstream infections, (2) support antimicrobial stewardship, and (3) capture data from decentralized rural areas for AMR surveillance [27]. First, technical specifications (target product profile) were defined, a market analysis was performed, and a call for proposal was launched. The MicroScan® (Beckman Coulter, Inc., West Sacramento, CA, USA) platform and the PROMPTTM inoculation system (Beckman Coulter, Inc., West Sacramento, CA, USA) were selected for their ready-to-use and sealed/packaged formats. Moreover, lyophilized MIC AST micro-broth dilution systems were considered less error-prone than disc diffusion methods. They provide first-rate information [28,29], such as MIC, which can be read manually or with an automatic reader, and produces high-reproducibility and standardized results thanks to its pre-prepared panels. MSF partnered with Beckman Coulter to tailor the MIC panel. The selection of antibiotics was based on (i) the list of antibiotics available as CE-IVD from Beckman Coulter, (ii) the list of antibiotics used in MSF facilities, and (iii) the WHO’s essential drug lists [30]. Those panels were tailored to the needs of the patients, the local epidemiology, and expected antibiotic resistance (ABR) patterns (Supplementary Table S1).
Special attention was given to commonly-used antibiotics, antibiotics of last resort, and proxy indicators of resistance mechanisms as per GLASS requirements [27] and AWaRe classifications [31]. Drug dilutions were chosen to match both CLSI and EUCAST breakpoints in 2019 [32,33] and were embedded by Beckman Coulter on the MicroScan panels (Figure 1 and Supplementary Table S2); antibiotics abbreviations were defined as per EUCAST recommendations [34].
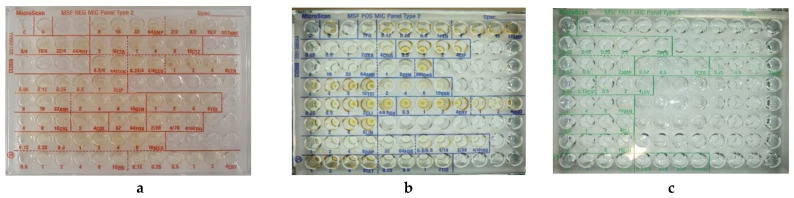
Figure 1.
Example of the three MSF MicroScan MIC panels. (a) MicroScan MSF dried overnight Gram-positive panel, (b) MicroScan MSF dried overnight Gram-negative panel, (c) MSF dried overnight fastidious panel.
Three CE-IVD AST microplates were developed: one for rapidly-growing aerobic and facultatively anaerobic gram-positive cocci (MicroScan MSF dried overnight Gram-positive panel, C32698), one for aerobic and facultatively anaerobic gram-negative bacilli (MicroScan MSF dried overnight Gram-negative panel, C32699), and one for aerobic non-enterococcal streptococci (including Streptococcus pneumoniae and Haemophilus spp.) (MicroScan MSF dried overnight fastidious panel, C32700).
During the CE-IVD certification process, most of the performance testing by manufacturers relies on isolates from high-income countries, where etiologies of sepsis are usually different from those in LMICs [27,28,29,30]. Therefore, our study aimed (i) to verify the accuracy of the three panels used with the Prompt inoculation methods and isolates either from LRS or challenging strains following ISO20776-2:2007 recommendations [35], and (ii) to verify the inter-observer variability in manually reading the panels
2. Materials and Methods
2.1. MicroScan MSF MIC Panels
We evaluated the MicroScan MSF dried overnight Gram-positive type 1 (MICPOS1), MicroScan MSF dried overnight Gram-negative type 1 (MICNEG1), and MSF dried overnight fastidious type 1 (MICFAST1) panels. In the current manuscript, we will further use the terms MICPOS1, MICNEG1, and MICFAST1 panels, respectively, to refer to each of these panels. When mentioning all types of panels, we will refer to “MSF MIC panels”. The breakpoints table of EUCAST version 9.1 (2019) [33] was used to interpret the MIC results. The lot numbers of the panels and reagents used in this experiment are listed in Supplementary Table S3.
2.2. Clinical Isolates and Reference Strains
A total of 387 anonymized clinical isolates, either fresh, recently frozen, or from stock, were tested. These included 332 isolates corresponding to the most common bloodstream pathogens or contaminants in LRS. Of the clinical isolates, 47.4% originated from sub-Saharan Africa, 28.5% from Asia, 12.2% from South America, and 11.4% from Europe (See Table 1 for details per species). On the MICPOS1, 123 Gram-positive strains were tested, of which, 60% (74) were Staphylococcus spp. isolates and 40% (49) were Enterococcus spp. isolates. On the MICNEG1, 157 Gram-negative rod isolates were tested, of which 72% (112) were Enterobacterales and 28% (45) were non-fermenting Gram-negative rods. On the MICFAST1, 107 fastidious isolates were tested, of which 82% (87) were Streptococcus spp. isolates and 18% (20) were Haemophilus influenzae isolates. Bacterial isolates were obtained from microbiological surveillance studies in LRS, from the strain collections of the Institute of Tropical Medicine (ITM), Antwerp, Belgium, of the Bicêtre University Hospital, French National Reference Laboratory for Antimicrobial Resistance (French AMR NRL), Paris, France, and of the Hôpital Universitaire Saint-Pierre, Université Libre Bruxelles (LHUB-ULB), Brussels, Belgium. As per ISO recommendations for evaluating the performance of AST [36], at least 25% of the isolates in the entire study were from fresh clinical samples.
Table 1.
Geographical origins of the isolates. Anonymized isolates were obtained from surveillance studies of several partners (ITM, French AMR NRL, LHUB-ULB).
| Species | Total Number of Isolates Tested | Africa | Asia | South America | Europe |
|---|---|---|---|---|---|
| Species Tested on the MSF Pos MIC Panel | |||||
| Staphylococcus aureus | 47 | 23 | 13 | 6 | 5 |
| Staphylococcus epidermidis | 11 | 5 | 3 | 1 | 2 |
| Staphylococcus hominis | 15 | 7 | 4 | 2 | 2 |
| Staphylococcus haemolyticus | 10 | 5 | 3 | 1 | 1 |
| Staphylococcus warneri | 1 | 1 | - | - | - |
| Enterococcus faecium | 35 | 14 | 10 | 4 | 4 |
| Enterococcus faecalis | 14 | 6 | 4 | 2 | 2 |
| Total isolates tested on the panel | 133 | 61 | 37 | 16 | 16 |
| Species Tested on the MSF Neg MIC Panel | |||||
| Escherichia coli | 25 | 12 | 7 | 3 | 3 |
| Klebsiella pneumoniae | 29 | 14 | 8 | 4 | 3 |
| Klebsiella oxytoca | 9 | 4 | 3 | 1 | 1 |
| Klebsiella ozaena | 1 | 1 | - | - | - |
| Morganella morganii | 1 | 1 | - | - | - |
| Salmonella Paratyphi A | 8 | 4 | 2 | 1 | 1 |
| Salmonella Typhimurium a | 8 | 4 | 2 | 1 | 1 |
| Salmonella Choleraesuis | 7 | 3 | 2 | 1 | 1 |
| Enterobacter cloacae | 16 | 7 | 5 | 2 | 2 |
| Enterobacter hermannii | 1 | 1 | - | - | - |
| Enterobacter kobei | 1 | 1 | - | - | - |
| Enterobacter asburiae | 1 | 1 | - | - | - |
| Citrobacter freundii complex | 5 | 2 | 1 | 1 | 1 |
| Pseudomonas aeruginosa | 15 | 7 | 4 | 2 | 2 |
| Acinetobacter baumannii complex | 14 | 6 | 4 | 2 | 2 |
| Burkholderia cepacia | 10 | 5 | 3 | 1 | 1 |
| Stenotrophomonas maltophilia | 6 | 3 | 2 | 1 | - |
| Total isolates tested on the panel | 157 | 76 | 43 | 20 | 18 |
| Species Tested on the MSF FAST MIC Panel | |||||
| Streptococcus pneumoniae | 54 | 26 | 15 | 7 | 6 |
| Streptococcus agalactiae | 37 | 17 | 12 | 4 | 4 |
| Streptococcus pyogenes | 30 | 14 | 9 | 4 | 3 |
| Streptococcus mitis | 22 | 10 | 6 | 3 | 2 |
| Streptocococcus oralis | 6 | 3 | 2 | 1 | 1 |
| Streptococcus anginosus | 10 | 5 | 3 | 1 | 1 |
| Streptococcus constellatus | 2 | 1 | 1 | - | - |
| Haemophilus influenzae | 20 | 10 | 6 | 2 | 2 |
| Total isolates tested on the panel | 181 | 86 | 54 | 22 | 19 |
aS. enterica subsp. enterica serovar Typhimurium (hereafter, S. Typhimurium).
2.3. Reference Antimicrobial Susceptibility Testing Methods
The antimicrobial susceptibility profiles of the isolates were determined in most cases by disc diffusion (Kirby Bauer) following the EUCAST standard method [37]. Exceptions were: agar gradient diffusion (Liofilchem, Roseto degli Abruzzi, Italy) for teicoplanin and vancomycin with all staphylococci (84), broth microdilution (dried panels from Sensititre, Thermo Fisher Scientific, East Grinstead, UK) for colistin with all Gram-negative bacilli (157) and daptomycin with all staphylococci (84), and agar dilution (Liofilchem, Roseto degli Abruzzi, Italy) for fosfomycin with all staphylococci (84), as per EUCAST guidelines (the complete list of reagents can be found in Supplementary Table S3). Reference testing was performed at the same time as MSF panels testing, according to the manufacturer’s instructions, and will be referred to in this article as AST reference panels or reference method.
2.4. Inoculum Preparation
Prior to testing, frozen isolates were subcultured twice and fresh isolates were subcultured once on tryptic soy agar plates containing 5% sheep blood (blood agar plate (BAP)) (or chocolate agar for H. influenzae) and incubated at 35 °C for 18 to 24 h under aerobic or CO2 atmosphere as per isolate requirement.
For the turbidity methods (MSF MIC Panels), in accordance with the manufacturer instruction for users (IFU), four to five large, or five to ten small well-isolated colonies were collected from an 18–24 h BAP or chocolate agar using a cotton swab and resuspended in 3 mL of Inoculum Water (B1015-2, Beckman Coulter, Inc., West Sacramento CA, USA) for 2–3 s using a vortex. Turbidity was measured using a turbidimeter (Den 1B, Biosan, Riga, Latvia) and adjusted as needed to reach the final turbidity of 0.5 +/− 0.02 McFarland. For the MICPOS1 and MICNEG1, 100 μL (0.1 mL) of the suspension was transferred into a 25 mL tube of Inoculum Water with Pluronic (B1015-7, Beckman Coulter, Inc., West Sacramento CA, USA) and mixed 8–10 times. For the MICFAST1, 100 μL (0.1 mL) of the suspension was transferred into a 25 mL tube of Haemophilus Test Medium (HTM) (B1015-26, Beckman Coulter, Inc., West Sacramento CA, USA) for Haemophilus spp. isolates or into a 25 mL tube of cation-adjusted Mueller–Hinton Broth with 3% Lysed Horse Blood (LHB) (B1015-25, Beckman Coulter, Inc., West Sacramento CA, USA) for Streptococcus spp. isolates and mixed 8–10 times.
2.5. Comparison between Standard Inoculum Method and Prompt Inoculation Method
All isolates inoculum-tested with MICPOS1 and MICNEG1 panels were prepared using the turbidity method and the Prompt inoculum method [38]. The Prompt Inoculation System-D (reference B1026-10D, Beckman Coulter, Inc., West Sacramento CA, USA) consists of a rod with a groove at its tip, it is designed to hold a specific number of bacteria (“wand”) and a bottle of diluent for the resuspension of bacteria. A breakaway collar is a small cylinder placed along the wand that serves as a wiping mechanism. Here, the wand was used to touch three different colonies as large as (or larger than) the tip, holding the wand perpendicular to the agar surface, and then the collar was slid down to wipe the wand before placing it into the bottle, pressing down to ensure a tight seal. The bottle was then vigorously shaken 8 to 10 times to resuspend the bacteria from the wand tip. The Prompt microbial suspension was used within 4 h, as stated by IFU.
2.6. Panel Inoculation and Incubation
Purity check plates were performed on all isolates tested using Mueller–Hinton agar or chocolate agar. MSF MIC panels were inoculated using the Renok Rehydrator/Inoculator, a manual pipettor that simultaneously rehydrates and inoculates all 96 wells of MicroScan panels. Contents of the inoculated Pluronic tube used with the turbidity method or of the Prompt bottle were poured into the Seed Tray Renok disposable D-inoculation set (B1013-4, Beckman Coulter, Inc., West Sacramento, CA, USA), an inoculator set consisting of a transfer lid (to hold and dispense the inoculum), and a seed trough (to contain the inoculum). The solution was transferred to the MSF MIC panels using MicroScan Renok (B1018-18, Beckman Coulter), which delivered 115 ± 10 µL of broth suspension to each well. Reference panels were inoculated and incubated according to EUCAST and IFU from the manufacturer. All MSF MIC panels were incubated at 35 +/− 2 °C in an offline, ambient air non-CO2 incubator.
2.7. Manual Panel Reading and Inter Observer Variability
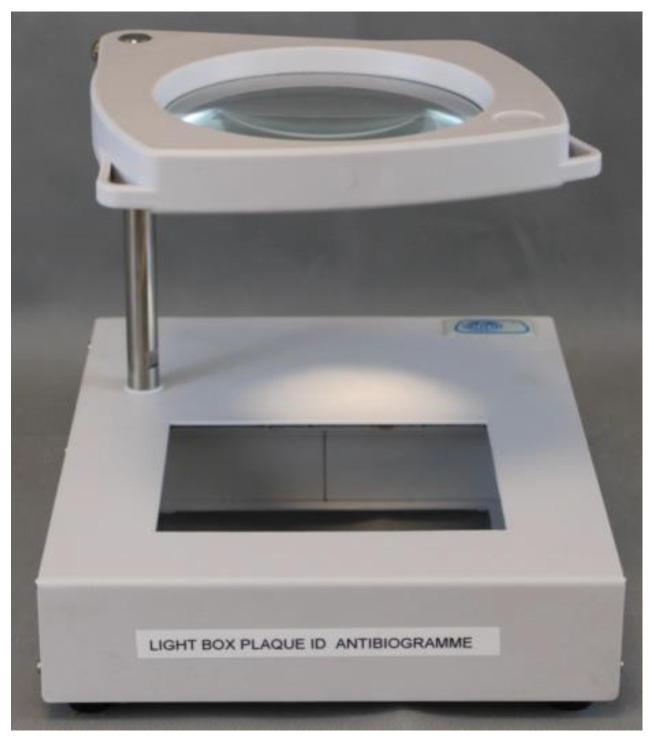
The MSF MIC panels were read 16–20 h after incubation. The panels were read manually against a black, indirectly lighted background using a viewer box prototype (Figure 2) adapted for this purpose (Ref. 9999400, JP Selecta, Barcelona, Spain) with interchangeable white or black backgrounds according to the type of panels. Growth in a well was defined as turbidity in the form of haze throughout the well, a button in the center of the well, or fine granular growth throughout the well as per EUCAST [39]. MSF MIC panels were read manually by two technicians. For inter-observer variability calculation, laboratory technicians were blinded to each other’s results. If a discrepancy in reading was found, a consensus was made among readers for the final reading results. All results were recorded onto specific bench sheets and imported into WHONET version 5.6, freely available software for the interpretation of AST using MIC or inhibition zone diameter data [40,41].
Figure 2.
Prototype of the microplate viewer box by JP Selecta, used for visual reading. The background at the bottom can be changed from black to white [26].
2.8. Ease of Use
Assessment of the ease of use was done by surveying the operators with a questionnaire for feedback on each of the components of the system. The readability level of the IFU was assessed using Flesch–Kincaid Grade levels (https://www.online-utility.org/english/readability_test_and_improve.jsp; accessed on 20 March 2021) [13].
2.9. Data Analysis
The a priori sample size calculation was not performed before the start of the study. Data were collected on worksheets and entered into Microsoft Excel 2019 (version 2110). The sample size was determined following ISO 20776:2 2007 standard [35] recommendations. Statistical analyses were performed in R (version 4.0.2) using RStudio or Microsoft Excel 2019 (version 2110). The essential agreement (EA) was not calculated as most of the reference testing consisted of disc diffusion methods giving only interpretative category results. Categorical agreement (CA), very major errors (VMEs), major errors (MEs), and minor errors (mEs) were calculated as described in the ISO 20776:2 2007 standard [35]. The CA was defined as susceptible (S), susceptible to increased exposure (I), or resistant (R), as per the EUCAST definition V9, which was the same with both methods. A VME was defined as a false susceptible result with the MSF MIC panels, whereas an ME was a false R or non-susceptible result with the MSF MIC panels; a mE was identified when one method reported an I result while the other method reported S or R results. The acceptance criteria for the study are based on ISO 20776-2:2007 and are as follows: CA ≥ 90%; ME ≤ 3%, VME ≤ 3%.
For inter-observer agreement, two indicators were calculated. First, a measure of the reliability of reading the MIC by a reader against the final reading (an agreement made by both readers if there was a discrepancy) with the calculation of Cohen’s kappa (CK) coefficient [42]. A CK > 0.8 was considered as a very good agreement; 0.6 < CK ≤ 0.8 as a good agreement; 0.4 < CK ≤ 0.6 as a moderate agreement; 0.2 < CK ≤ 0.4 as a fair agreement; and CK ≤ 0.2 as a poor agreement. Second, CA against the AST reference method was calculated by each reader to determine the impact on the result interpretations.
2.10. Quality Control
Daily QC was done on the MSF MIC panel tested according to the Beckman recommendations (E. coli ATCC1 25922, P. aeruginosa ATCC 27853, S. aureus ATCC1 29213, E. faecalis ATCC 29212, H. influenzae ATCC 49766, and S. agalactiae ATCC 13813). For out-of-control QC results, after a careful panel examination, QC testing was repeated and if the “out-of-control” occurred again, testing was stopped to identify the problem.
2.11. Resolution of Discrepancies
Isolates with a VME or ME were retested using both methods, as were selected isolates with specific drug/organism combinations resulting in ≥10% mEs. Calculations of CA, VMEs, MEs, and mEs were obtained following resolutions of discrepant results after repeated testing. If an error persisted after repeated testing, it was included in the calculations. If the error was resolved after repeated testing, it was not counted as an error, and the initial result was disregarded.
3. Results
3.1. Evaluation of the MSF MicroScan MIC Panels
3.1.1. MSF Gram-Pos Panel Results
Individual antimicrobial data are presented in Table 2 for Staphylococcus spp. and Table 3 for Enterococcus spp., CA and error rates were within acceptable limits. Of the 74 Staphylococcus spp. tested, after repeated testing, VME occurred in 2 isolates (3%) for teicoplanin and 1 isolate each (1%) for erythromycin and clindamycin. ME occurred in two isolates (3%) for ciprofloxacin, gentamicin, and tetracycline, and one isolate each (1%) for the cefoxitin screening test, amikacin, erythromycin, fosfomycin, trimethoprim/sulfamethoxazole, and tigecycline. Of the 49 Enterococcus spp. tested, after repeated testing, 1 (2%) VME was noted for ampicillin, gentamicin high level, and tigecycline. One (2%) ME occurred for ampicillin, ciprofloxacin, gentamicin high level, and tigecycline.
Table 2.
Results for Staphylococci tested with the MICPOS1 standard turbidity inoculum method and visual reading versus AST reference methods.
| No. of Isolates AST Reference a |
No. of Isolates MICPOS1 b | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Antimicrobial | Total | R | I | S | R | I | S | CA c (no. [%]) |
mE d (no. [%]) |
ME e (no. [%]) |
VME f (no. [%]) |
| Penicillin | 63 | 59 | 0 | 4 | 59 | 0 | 4 | 63 (100) | 0 (0) | 0 (0) | 0 (0) |
| Ciprofloxacin | 74 | 37 | 0 | 37 | 39 | 0 | 35 | 72 (97) | 0 (0) | 2 (3) | 0 (0) |
| Amikacin | 74 | 17 | 4 | 53 | 16 | 8 | 50 | 69 (93) | 4 (5) | 1 (1) | 0 (0) |
| Gentamicin | 74 | 28 | 0 | 46 | 30 | 0 | 44 | 72 (97) | 0 (0) | 2 (3) | 0 (0) |
| Teicoplanin | 74 | 3 | 0 | 71 | 1 | 0 | 73 | 72 (97) | 0 (0) | 0 (0) | 2 (3) |
| Vancomycin | 74 | 2 | 0 | 72 | 2 | 0 | 72 | 74 (100) | 0 (0) | 0 (0) | 0 (0) |
| Quinupristin-dalfopristin | 74 | 0 | 7 | 67 | 0 | 7 | 67 | 74 (100) | 0 (0) | 0 (0) | 0 (0) |
| Erythromycin | 74 | 30 | 0 | 44 | 30 | 1 | 43 | 71 (96) | 1 (1) | 1 (1) | 1 (1) |
| Clindamycin | 74 | 14 | 0 | 60 | 12 | 1 | 61 | 72 (97) | 1 (1) | 0 (0) | 1 (1) |
| Daptomycin | 74 | 1 | 0 | 73 | 1 | 0 | 73 | 74 (100) | 0 (0) | 0 (0) | 0 (0) |
| Fosfomycin | 74 | 29 | 0 | 45 | 30 | 0 | 44 | 73 (99) | 0 (0) | 1 (1) | 0 (0) |
| Trimethoprim/Sulfamethoxazole | 74 | 18 | 0 | 56 | 19 | 3 | 52 | 70 (95) | 3 (4) | 1 (1) | 0 (0) |
| Linezolid | 74 | 5 | 0 | 69 | 5 | 0 | 69 | 74 (100) | 0 (0) | 0 (0) | 0 (0) |
| Tetracycline | 74 | 37 | 0 | 37 | 39 | 0 | 35 | 72 (97) | 0 (0) | 2 (3) | 0 (0) |
| Tigecycline | 74 | 0 | 0 | 74 | 1 | 0 | 73 | 73 (99) | 0 (0) | 1 (1) | 0 (0) |
a Number of isolates tested with the reference method and classified as R resistant; I, susceptible, increased exposure; S, susceptible; b number of isolates tested with the evaluated method and classified as R resistant; I, susceptible, increased exposure; S, susceptible; c CA, categorical agreement; d mE, minor error; e ME, major error; f VME, very major error.
Table 3.
Results for Enterococci tested with the MICPOS1 standard turbidity inoculum method and visual reading versus AST reference methods.
| No. of Isolates AST Reference a |
No. of Isolates MICPOS1 b | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Antimicrobial | Total | R | I | S | R | I | S | CA c (no. [%]) |
mE d (no. [%]) |
ME e (no. [%]) |
VME f (no. [%]) |
| Ampicillin | 49 | 30 | 0 | 19 | 29 | 1 | 18 | 47 (96) | 0 (0) | 1 (2) | 1 (2) |
| Ciprofloxacin | 49 | 29 | 0 | 20 | 30 | 0 | 19 | 48 (98) | 0 (0) | 1 (2) | 0 (0) |
| Teicoplanin | 49 | 23 | 0 | 26 | 23 | 0 | 26 | 49 (100) | 0 (0) | 0 (0) | 0 (0) |
| Vancomycin | 49 | 23 | 0 | 26 | 23 | 0 | 26 | 49 (100) | 0 (0) | 0(0) | 0 (0) |
| Quinupristin-dalfopristin | 49 | 19 | 16 | 14 | 19 | 16 | 14 | 45 (91) | 4 (9) | 0 (0) | 0 (0) |
| Linezolid | 49 | 2 | 0 | 47 | 2 | 0 | 47 | 49 (100) | 0 (0) | 0 (0) | 0 (0) |
| Tigecycline | 49 | 4 | 0 | 45 | 4 | 0 | 45 | 47 (96) | 0 (0) | 1 (2) | 1 (2) |
a Number of isolates tested with the reference method and classified as R resistant; I, intermediate; S, susceptible; b number of isolates tested with the evaluated method and classified as R resistant; I, intermediate; S, susceptible; c CA, categorical agreement; d mE, minor error; e ME, major error; f VME, very major error.
3.1.2. MSF Gram-Neg Panel Results
Individual antimicrobial data are presented in Table 4 for Enterobacterales and Table 5 for non-fermenting Gram-negative rods. For all isolates tested, CA and error rates were within acceptable limits. Of the 112 Enterobacterales tested, VME occurred in two isolates (3%) for gentamicin and trimethoprim/sulfamethoxazole, and one isolate each (1%) for ampicillin, amoxicillin–clavulanate, amikacin, colistin, and ertapenem. Two isolates (3%) were found to have ME for amoxicillin–clavulanate, ciprofloxacin, and gentamicin, and one (1%) isolate each for ceftazidime, ceftriaxone, trimethoprim/sulfamethoxazole, colistin, and meropenem.
Table 4.
Results for Enterobacterales tested with the MICNEG1 standard turbidity inoculum method and visual reading versus AST reference methods.
| No. of Isolates AST Reference a |
No. of Isolates MICPNEG1 b | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Antimicrobial | Total | R | I | S | R | I | S | CA c (no. [%]) |
mE d (no. [%]) |
ME e (no. [%]) |
VME f (no. [%]) |
| Ampicillin | 112 | 100 | 0 | 12 | 99 | 0 | 13 | 111 (99) | 0 (0) | 0 (0) | 1 (1) |
| Amoxicillin/Clavulanic Acid | 112 | 72 | 0 | 40 | 73 | 0 | 39 | 109 (97) | 0 (0) | 2 (2) | 1 (1) |
| Ceftazidime | 112 | 47 | 2 | 63 | 49 | 0 | 64 | 108 (96) | 3 (3) | 1 (1) | 0 (0) |
| Ceftriaxone | 112 | 50 | 0 | 62 | 51 | 1 | 60 | 110 (98) | 1 (1) | 1 (1) | 0 (0) |
| Piperacillin/Tazobactam | 112 | 39 | 4 | 69 | 39 | 4 | 69 | 106 (93) | 6 (7) | 0 (0) | 0 (0) |
| Ciprofloxacin | 112 | 51 | 4 | 57 | 53 | 4 | 55 | 106 (93) | 4 (4) | 2 (2) | 0 (0) |
| Amikacin | 112 | 16 | 4 | 92 | 14 | 5 | 93 | 106 (93) | 5 (6) | 0 (0) | 1 (1) |
| Gentamicin | 112 | 40 | 5 | 67 | 40 | 4 | 68 | 104 (92) | 4 (4) | 2 (2) | 2 (2) |
| Trimethoprim/Sulfamethoxazole | 112 | 69 | 1 | 42 | 69 | 0 | 43 | 108 (96) | 1 (1) | 1 (1) | 2 (2) |
| Chloramphenicol | 112 | 47 | 0 | 65 | 47 | 0 | 65 | 112 (100) | 0 (0) | 0 (0) | 0 (0) |
| Colistin | 112 | 12 | 0 | 77 | 12 | 0 | 77 | 110 (98) | 0 (0) | 1 (1) | 1 (1) |
| Fosfomycin | 112 | 1 | 0 | 111 | 1 | 0 | 111 | 112 (100) | 0 (0) | 0 (0) | 0 (0) |
| Tigecycline | 112 | 0 | 0 | 112 | 0 | 0 | 112 | 112 (100) | 0 (0) | 0 (0) | 0 (0) |
| Meropenem | 112 | 16 | 6 | 90 | 17 | 6 | 79 | 106 (93) | 5 (6) | 1 (1) | 0 (0) |
| Imipenem | 112 | 19 | 7 | 86 | 19 | 7 | 86 | 112 (100) | 0 (0) | 0 (0) | 0 (0) |
| Ertapenem | 112 | 33 | 0 | 79 | 32 | 0 | 80 | 111 (99) | 0 (0) | 0 (0) | 1 (1) |
a Number of isolates tested with the reference method and classified as R resistant; I, susceptible, increased exposure; S, susceptible; b number of isolates tested with the evaluated method and classified as R resistant; I, susceptible, increased exposure; S, susceptible; c CA, categorical agreement; d mE, minor error; e ME, major error; f VME, very major error.
Table 5.
Results for non-fermenting Gram-neg bacilli tested with the MICNEG1 standard turbidity inoculum method and visual reading versus AST reference methods.
| No. of Isolates AST Reference a |
No. of Isolates MICPNEG1 b | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Antimicrobial | Total | R | I | S | R | I | S | CA c (no. [%]) |
mE d (no. [%]) |
ME e (no. [%]) |
VME f (no. [%]) |
| Ceftazidime | 15 | 8 | 3 | 4 | 8 | 2 | 5 | 14 (96) | 1 (4) | 0 (0) | 0 (0) |
| Piperacillin/Tazobactam | 15 | 4 | 0 | 11 | 4 | 0 | 11 | 15 (100) | 0 (0) | 0 (0) | 0 (0) |
| Ciprofloxacin | 29 | 12 | 6 | 11 | 12 | 6 | 11 | 29 (100) | 0 (0) | 0 (0) | 0 (0) |
| Amikacin | 29 | 7 | 2 | 20 | 7 | 2 | 20 | 29 (100) | 0 (0) | 0 (0) | 0 (0) |
| Gentamicin | 29 | 15 | 0 | 14 | 15 | 0 | 14 | 29 (100) | 0 (0) | 0 (0) | 0 (0) |
| Trimethoprim/Sulfamethoxazole | 29 | 10 | 0 | 20 | 9 | 1 | 20 | 28 (99) | 1 (1) | 0 (0) | 0 (0) |
| Chloramphenicol | 9 | 4 | 3 | 2 | 4 | 3 | 2 | 9 (100) | 0 (0) | 0 (0) | 0 (0) |
| Colistin | 15 | 3 | 0 | 12 | 3 | 0 | 12 | 15 (100) | 0 (0) | 0 (0) | 0 (0) |
| Meropenem | 45 | 14 | 6 | 25 | 14 | 6 | 25 | 43 (96) | 2 (4) | 0 (0) | 0 (0) |
| Imipenem | 29 | 12 | 0 | 17 | 10 | 1 | 18 | 27 (94) | 1 (3) | 0 (0) | 1 (3) |
a Number of isolates tested with the reference method and classified as R resistant; I, susceptible, increased exposure; S, susceptible; b number of isolates tested with the evaluated method and classified as R resistant; I, susceptible, increased exposure; S, susceptible; c CA, categorical agreement; d mE, minor error; e ME, major error; f VME, very major error.
3.1.3. MSF FAST Panel Results
Individual antimicrobial data are presented in Table 6 for Streptococci and Table 7 for H. influenzae. For all isolates tested, CA and error rates were within acceptable limits. Of the 87 Streptococci tested, VME was found in one isolate (1%) for vancomycin, clindamycin, trimethoprim/sulfamethoxazole, and chloramphenicol. ME was observed in one (2%) isolate of Streptococcus pneumoniae for meropenem and one isolate of Streptococcus mitis for penicillin, clindamycin, and trimethoprim/sulfamethoxazole. Of the 20 Haemophilus influenzae tested, only 1 was found to be discrepant between I and R (i.e., mE) for trimethoprim/sulfamethoxazole.
Table 6.
Results for Streptococcus spp. test tested with the MICFAST1 standard turbidity inoculum method and visual reading versus AST reference methods.
| No. of Isolates AST Reference a |
No. of Isolates MICPFAST1 b | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Antimicrobial | Total | R | I | S | R | I | S | CA c (no. [%]) |
mE d (no. [%]) |
ME e (no. [%]) |
VME f (no. [%]) |
| Penicillin | 87 | 10 | 9 | 68 | 12 | 8 | 67 | 84 (97) | 2 (2) | 1 (1) | 0 (0) |
| Meropenem g | 53 | 0 | 0 | 53 | 1 | 0 | 52 | 52 (98) | 0 (0) | 1 (2) | 0 (0) |
| Ceftriaxone f | - | - | - | - | - | - | - | - | - | - | - |
| Ampicillin g | 53 | 12 | 6 | 35 | 14 | 2 | 37 | 49 (92) | 4 (8) | 0 (0) | 0 (0) |
| Levofloxacin h | 63 | 1 | 0 | 62 | 1 | 0 | 62 | 63 (100) | 0 (0) | 0 (0) | 0 (0) |
| Vancomycin | 87 | 2 | 0 | 85 | 1 | 0 | 86 | 86 (99) | 0 (0) | 0 (0) | 1 (1) |
| Clindamycin | 87 | 16 | 0 | 71 | 16 | 0 | 71 | 85 (98) | 0 (0) | 1 (1) | 1 (1) |
| Trimethoprim/Sulfamethoxazole | 87 | 4 | 0 | 83 | 4 | 0 | 83 | 85 (98) | 0 (0) | 1 (1) | 1 (1) |
| Chloramphenicol | 87 | 3 | 0 | 84 | 2 | 0 | 85 | 86 (99) | 0 (0) | 0 (0) | 1 (1) |
| Linezolid i | 63 | 0 | 0 | 63 | 0 | 0 | 63 | 63 (100) | 0 (0) | 0 (0) | 0 (0) |
a Number of isolates tested with the reference method and classified as R resistant; I, susceptible, increased exposure; S, susceptible; b number of isolates tested with the evaluated method and classified as R resistant; I, susceptible, increased exposure; S, susceptible; c CA, categorical agreement; d mE, minor error; e ME, major error; f VME, very major error; g The susceptibility of streptococcus group A, B, C, G to cephalosporins is inferred from the benzylpenicillin susceptibility, no breakpoint available on disc diffusion; h Only interpretation for S. pneumoniae and S. viridans group; i Only interpretation for S. pneumoniae, S. viridans group, and S. anginosus group.
Table 7.
Results for the H. influenzae test with the MICFAST1 standard turbidity inoculum method and visual reading versus AST reference methods.
| No. of Isolates AST Reference a |
No. of Isolates MICPFAST1 b | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Antimicrobial | Total | R | I | S | R | I | S | CA c (no. [%]) |
mE d (no. [%]) |
ME e (no. [%]) |
VME f (no. [%]) |
| Meropenem | 20 | 0 | 0 | 20 | 0 | 0 | 20 | 20 (100) | 0 (0) | 0 (0) | 0 (0) |
| Ceftriaxone | 20 | 3 | 0 | 17 | 3 | 0 | 17 | 20 (100) | 0 (0) | 0 (0) | 0 (0) |
| Ampicillin | 20 | 2 | 0 | 18 | 2 | 0 | 18 | 20 (100) | 0 (0) | 0 (0) | 0 (0) |
| Ciprofloxacin | 20 | 3 | 0 | 17 | 3 | 0 | 17 | 20 (100) | 0 (0) | 0 (0) | 0 (0) |
| Levofloxacin | 20 | 2 | 0 | 18 | 2 | 0 | 18 | 20 (100) | 0 (0) | 0 (0) | 0 (0) |
| Trimethoprim/Sulfamethoxazole | 20 | 6 | 1 | 13 | 7 | 0 | 13 | 19 (95) | 1 (5) | 0 (0) | 0 (0) |
| Chloramphenicol | 20 | 0 | 0 | 20 | 0 | 0 | 20 | 20 (100) | 0 (0) | 0 (0) | 0 (0) |
a Number of isolates tested with the reference method and classified as R resistant; I, susceptible, increased exposure; S, susceptible; b number of isolates tested with the evaluated method and classified as R resistant; I, susceptible, increased exposure; S, susceptible; c CA, categorical agreement; d mE, minor error; e ME, major error; f VME, very major error.
Specific resistance mechanism detection data, tested with the MICPOS1 or MICNEG1 panels, are presented in Table 8.
Table 8.
Results for specific resistance tests using MICNEG1 or MICPOS1 standard turbidity inoculum methods and visual reading versus AST reference methods.
| No. of Isolates | AST Reference a | MSF Panel b | ||||||
|---|---|---|---|---|---|---|---|---|
| Multidrug Resistant Organism | Total | R | S | R | S | CA c (no. [%]) |
ME d (no. [%]) |
VME e (no. [%]) |
| Methicillin-resistant Staphylococcus aureus f | 47 | 33 | 14 | 33 | 14 | 47 (100) | 0 (0) | 0 (0) |
| Inducible clindamycin-resistant Staphylococci f | 74 | 26 | 48 | 26 | 48 | 74 (100) | 0(0) | 0 (0) |
| Vancomycin-resistant Staphylococcus aureus f | 47 | 2 | 45 | 2 | 45 | 47 (100) | 0 (0) | 0 (0) |
| High-level gentamicin resistance Staphylococci f | 49 | 25 | 24 | 25 | 24 | 47 (96) | 1 (2) | 1 (2) |
| Vancomycin-resistant Enterococci f | 49 | 23 | 26 | 23 | 26 | 49 (100) | 0(0) | 0 (0) |
| Extended-spectrum beta-lactamase-producing Enterobacterales g | 112 | 19 | 93 | 19 | 93 | 112 (100) | 0 (0) | 0 (0) |
| Carbapenem-resistant Enterobacterales g | 112 | 33 | 79 | 32 | 80 | 111 (99) | 0 (0) | 1 (1) |
| Colistin-resistant Enterobacterales g | 112 | 12 | 77 | 12 | 77 | 110 (98) | 1 (1) | 1 (1) |
| Carbapenem-resistant Pseudomonas aeruginosa g | 15 | 4 | 11 | 4 | 11 | 15 (100) | 0 (0) | 0 (0) |
| Colistin-resistant Pseudomonas aeruginosa g | 15 | 4 | 11 | 4 | 11 | 15 (100) | 0 (0) | 0 (0) |
| Carbapenem-resistant Acinetobacter baumannii g | 14 | 8 | 6 | 8 | 6 | 15 (100) | 0 (0) | 0 (0) |
a Number of isolates tested with the reference method and classified as R resistant; I, susceptible, increased exposure; S, susceptible; b number of isolates tested with the evaluated method and classified as R resistant; I, susceptible, increased exposure; S, susceptible; c CA, categorical agreement; d ME, major error; e VME, very major error; f Resistance test evaluated on the MICPOS1 panel; g Resistance test evaluated on the MICNEG1 panel.
3.2. Results of the Evaluation of the Prompt Performance
Results of the evaluation of MSF MIC panels using the Prompt inoculation method can be found in Supplementary Table S4–S7 for Staphylococci, Enterococci, Enterobacterales, and non-fermenting gram-negative rods, respectively. Specific resistance mechanism detection data are presented in Supplementary Table S8. When Staphylococci were tested with Prompt, the amikacin molecule had the largest number of discrepancies with a CA of 78%, of which 11 and 5 isolates were found to have mE and ME, respectively. Compared with the turbidity inoculum method, more ME in Staphylococci were observed for ciprofloxacin (9%), gentamicin (9%), vancomycin (4%), erythromycin (9%), trimethoprim/sulfamethoxazole (14%), and linezolid (5%), all above the 3% threshold of ISO 20776-2: 2007. For Enterococci, four (9%) isolates had mEs for quinupristin–dalfopristin and two (4%) isolates had VMEs for tigecycline.
3.3. Inter-Observer Variability
The results of the inter-observer agreement between the two independent readers who read the panels visually are presented in Table 9. Overall, the reading agreements for MICNEG1 and MICFAST1 were both classified as very good (CK 0.94 and 0.95, respectively). The reading agreement of MICPOS1 was classified as good (CK 0.82). This was mainly due to the lower agreement in reading for ampicillin (0.76), amikacin (0.78), teicoplanin (0.79), and tigecycline (0.82), and especially for daptomycin (0.37), fosfomycin (0.63), and linezolid (0.37). However, the discrepancies in MIC reading did not affect the CA between each of the two readers and the reference method, with CAs of 96% and 96% for daptomycin, 76% and 77% for fosfomycin, and 97% and 96% for linezolid.
Table 9.
Results of the inter-observer variability test using MSF MIC panels with the Prompt inoculation method versus the standard AST method.
| Staphylococci and Enterococci | Gram-negative bacilli | Fastidious organisms | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Antimicrobial | n a | Kappa Cohen | R1 CA b [%] |
R2 CA c [%] |
n a | Kappa Cohen | R1 CA b [%] |
R2 CA c [%] |
n a | Kappa Cohen | R1 CA b [%] |
R2 CA c [%] |
| Penicillin | 63 | 0.95 | 98 | 98 | 87 | 0.99 | 97 | 97 | ||||
| Ampicillin | 123 | 0.76 | 96 | 92 | 112 | 0.91 | 99 | 98 | 107 | 1.00 | 98 | 98 |
| Amoxicillin/Clavulanic Ac | 112 | 0.97 | 99 | 98 | ||||||||
| Cefoxitin screening/Oxacillin | 74 | 0.95 | 92 | 93 | ||||||||
| Ceftazidime | 127 | 0.95 | 97 | 96 | ||||||||
| Ceftriaxone | 112 | 0.89 | 97 | 98 | 20 | 1.00 | 100 | 100 | ||||
| ESBL test | 112 | 0.97 | 99 | 97 | ||||||||
| Piperacillin/Tazobactam | 127 | 0.97 | 99 | 93 | ||||||||
| Levofloxacin | 83 | 0.98 | 100 | 100 | ||||||||
| Ciprofloxacin | 49 | 0.89 | 99 | 99 | 141 | 0.95 | 94 | 96 | ||||
| Amikacin | 123 | 0.78 | 78 | 76 | 141 | 0.99 | 99 | 93 | ||||
| Gentamicin | 123 | 0.92 | 100 | 96 | 141 | 1.00 | 92 | 92 | ||||
| Gentamicin (high level) | 49 | 0.90 | 90 | 90 | ||||||||
| Teicoplanin | 123 | 0.79 | 99 | 96 | ||||||||
| Vancomycin | 123 | 1.00 | 97 | 97 | 87 | 1.00 | 98 | 98 | ||||
| Quinupristin-dalfopristin | 123 | 0.93 | 89 | 91 | ||||||||
| Erythromycin | 74 | 0.97 | 96 | 96 | ||||||||
| Clindamycin | 74 | 0.99 | 97 | 97 | 87 | 0.64 | 100 | 100 | ||||
| Inducible clindamycin resistance | 74 | 0.96 | 97 | 95 | ||||||||
| Daptomycin | 74 | 0.37 | 96 | 96 | ||||||||
| Fosfomycin | 74 | 0.63 | 76 | 77 | 112 | 0.76 | 100 | 100 | ||||
| Trimethoprim/Sulfamethoxazole | 74 | 0.62 | 95 | 95 | 142 | 0.87 | 96 | 96 | 107 | 0.92 | 98 | 93 |
| Linezolid | 123 | 0.37 | 97 | 96 | 63 | 1.00 | 100 | 100 | ||||
| Tetracycline | 74 | 0.94 | 97 | 97 | ||||||||
| Tigecycline | 123 | 0.82 | 95 | 94 | 112 | 0.97 | 100 | 100 | ||||
| Chloramphenicol | 121 | 0.90 | 99 | 99 | 107 | 1.00 | 98 | 98 | ||||
| Colistin | 127 | 0.97 | 98 | 98 | ||||||||
| Meropenem | 157 | 0.96 | 93 | 93 | 73 | 0.97 | 98 | 98 | ||||
| Imipenem | 141 | 0.96 | 100 | 100 | ||||||||
| Ertapenem | 112 | 0.97 | 99 | 99 | ||||||||
| Average all molecules | 0.82 | 94 | 93 | 0.94 | 98 | 97 | 0.95 | 99 | 98 | |||
a Total number of isolates tested by the molecule. b R1CA categorical agreement between Reader 1 and reference methods. c R2CA categorical agreement between Reader 1 and reference methods.
3.4. Ease of Use
The instructions for interpretation of growth results were considered by the laboratory technicians as understandable but, as no pictures were included to ease the comprehension, the color atlas document made by EUCAST was much appreciated [39]. The Flesch–Kincaid grade levels (FKGL) of the three MSF MIC panels IFU were nine each. FKGL refers to US grade levels (i.e., years of schooling) necessary to understand the text. The FKGL of the first part of the IFU of the Prompt method, with all instructions and limitations (Figure 3a), was 11. The FKGL dropped to six in the last part, where instructions for the Prompt are explained as bench aids with black and white figures (Figure 3b). The FKGL of the IFU of the Renok, which included bench aids as well, was rated 6.
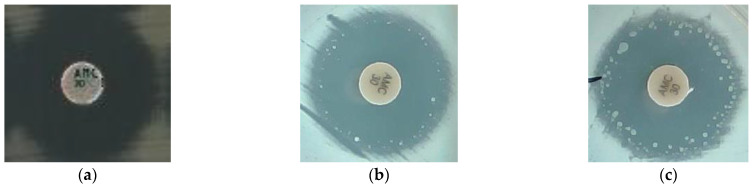
Figure 3.
Photo of the inhibition zone produced by Salmonella Typhimurium with: (a) initial reference method with Mueller–Hinton agar from Becton, Dickinson and a disc from Bio-Rad with no sign of heteroresistance; (b,c) sign of heteroresistance when using bioMérieux Mueller–Hinton Enterobacterales agar (bioMérieux Inc., Marcy l’ Étoile, France) and an AMC disc from i2a (i2a, Montpellier, France).
Both the Prompt™ and the RENOK systems were considered user-friendly and time-efficient by both users, particularly compared to other inoculation methods using 0.5 McFarland standards and single-pipette dispensers. Interpreting the panels was not considered difficult, except for trimethoprim/sulfamethoxazole because of the “trailing effect”, a typical reading of this antibiotic where the MIC should be read as: (1) approximately 80% reduction of growth, (2) a white button less than 2 mm in diameter, or (3) a white button that is semi-translucent.
The packaging of individual panels was of very good quality, providing air-sealed individual aluminum–plastic pouches with humidity indicators; they were easy to open. Other components were provided within sturdy cardboard boxes fit for difficult transport conditions in LRS. Concerning the shelf life of the MSF MIC panels, Prompt and Pluronic water were within the limits predefined by the Mini-Lab target product profile (minimally 12 months), and the storage conditions (2–25 °C) were within the acceptable Mini-Lab specifications (2–40 °C). However, the shelf life of the HTM and LHB broth needed to rehydrate MICFAST1 was 6 months at 2–8 °C.
4. Discussion
4.1. Performance Evaluation of the MSF MIC Panels
For all drug/organism combinations, our study showed that MICPOS1, MICNEG1, and MICFAST1 panels performed satisfactorily, in agreement with the previous evaluation using the MicroScan technology [43,44,45,46,47], and when testing isolates from LMICs. In addition, they performed as expected with challenging strains for confirmation of resistance mechanisms, such as extended-spectrum beta-lactamase-producing Enterobacterales, methicillin-resistant Staphylococcus aureus, induced resistance to clindamycin among Staphylococci, high-level aminoglycoside resistance among Enterococci, and screening of carbapenemase-producing Enterobacterales, Acinetobacter baumannii, and Pseudomonas aeruginosa. As mentioned by the manufacturer, a limitation of the MICFAST1 panel is its inability to detect resistance to levofloxacin in Streptococcus spp. and resistance to ciprofloxacin and meropenem in Haemophilus influenzae, due to the lack of resistant strains at the time of comparative testing.
However, before repeated testing for the resolution of discrepant results, amoxicillin–clavulanate (AMC) of the MICNEG1 was found to have a CA of 89% with 11% ME. All MEs (12/112) on the AMC were found in Salmonella species, 5 Salmonella enterica serotype Choleraesuis (from Cambodia, Ecuador), and 7 S. Typhimurium (from DRC, Burkina Faso). When these strains were removed from the analysis, the CA for AMC was 100%. We suspected that the presence of monoclonal heteroresistance was not captured by the disc diffusion methods we used as reference. This has previously been described for other organisms/drug combinations [48,49,50] and colistin, polymyxin, and carbapenems among S. Typhimurium [51]. Therefore, we re-evaluated the 12 discrepant isolates using various combinations of discs and media from different manufacturers in triplicate with the addition of another broth microdilution (BMD) panel (Sensititre, Thermo Fisher Scientific, East Grinstead, UK) and gradient diffusion strip (E-test, bioMérieux, Marcy-l’ Étoile, France). The results are presented in Supplementary Table S7 and photos of the inhibition zone produced by Salmonella Typhimurium are presented in Figure 3. Sensititre BMD and MICNEG1 gave similar MIC results for AMC. Only the combination of BioMérieux specific Mueller–Hinton agar for Enterobacterales (bioMérieux, Marcy-l’ Étoile, France) with a disc from i2a (Montpellier, France) gave similar results to the MICNEG1. To our knowledge, heteroresistance for amoxicillin–clavulanate within the Salmonella species has not been described in the literature and should be further studied using a population analysis profile and other methods, as proposed by Andersson et al. in their recent review on the impact of heteroresistance [52].
4.2. Performance Evaluation of the Prompt Inoculation Method
The manufacturer IFU stated that the Prompt System demonstrated elevated MICs with fluoroquinolones (e.g., gatifloxacin), lincosamides (e.g., clindamycin), and macrolides (e.g., erythromycin), and a potential ME with tigecycline and Staphylococci, when compared with the reference method, for reasons that were not able to be identified from the literature. Our experiment showed a similar increase in MIC when using the Prompt inoculation method with ciprofloxacin and erythromycin, which impacted the ME rates for Staphylococci coming from LRS but we did not find an increase in the ME rate with tigecycline and clindamycin. Moreover, our results suggest that the Prompt inoculation methods increased MIC and MEs on aminoglycosides, such as gentamicin, amikacin, vancomycin, trimethoprim–sulfamethoxazole, and linezolid for Staphylococci
Other studies suggest and confirm that the Prompt inoculation method has no effect on the MIC for the aerobic and facultatively anaerobic Gram-negative bacilli and Enterococci when compared to the standard inoculum method [38,53].
4.3. Inter-Observer Variability
Overall, the agreements between readers were very good, with four different readers during the entire duration of the experiment. No studies reporting agreements between visual readers using Dried overnight MicroScan panels have been published. Despite the first impression of reading difficulties and some disagreements in the reading of some antibiotic MICs, reader discrepancies had no impact on the final clinical category result interpretations.
4.4. Adaptation to LRS: Stability, Ease-of-Use
The temperature stability of the MicroScan panels, currently assured up to 25 °C, does not entirely fulfill the requirements for tropical settings because cool storage (<30 °C) is not always feasible [54]; however, when compared to disc diffusion that requires cold chain storage of the disc, it is more achievable for the MSF supply system in a district hospital to have access to storage facilities with air conditioning than shipping and storing in temperatures between 2 and 8 °C. Regarding the ease-of-use, the MicroScan inoculation system and panel reading (Renok and Prompt for Gram-negative bacilli) is positive; it does not require multiple steps to inoculate panels and the interpretation of panels is quite easy, with the exception of the trimethoprim–sulfamethoxazole (TRS) wells that require some practice. The dedicated prototype microplate viewer box greatly facilitated the reading process. The Flesch–Kincaid grade level scores of the IFU suggested that for MICPOS1, MSFNEG1, and MSFFAST1, a fair level of schooling is required to understand the IFU. Although the language used in professional documents may be at a slightly higher level, Flesch–Kincaid levels below six are desirable for IFU [55,56] as well as for the bench aid parts of the Prompt and Renok systems.
4.5. Recommendations for Use and Further Development of the MicroScan System
The current limitations of the Prompt and IFU panels explained above were tackled within the Mini-Lab project, by developing training material, such as videos, adapted laboratory procedures, bench aids, a color atlas of the different types of growth, and a microplate viewer for visual reading (see Supplementary Figure S2). This evaluation allowed us to adapt our recommendations to field workers, as, for example, to avoid the Prompt when suspecting Staphylococci. In addition, we encourage the manufacturer to mitigate (to the best possible extent) the issues described above. Bench aids could be included with the product as well as video training (available on their website) showing the different growth types from the wells. Lastly, extended shelf-life testing and stability testing in tropical environments are necessary to assure product quality in LRS.
4.6. Strengths and Limitations of the Study
To our knowledge, this is the first study that evaluated the MicroScan Dried MICs on clinical isolates with typical LRS pathogens [57,58]. Furthermore, we assessed robustness and ease of use. We have several limitations to the verification of some drug/organism combinations as we were lacking a number of resistant isolates; amikacin, teicoplanin, vancomycin, quinupristin–dalfopristin, clindamycin, daptomycin, linezolid, tigecycline for Staphylococci; fosfomycin, tigecycline for Enterobacterales; amikacin, piperacillin-tazobactam, chloramphenicol, and colistin for non-fermenting Gram-negative bacilli. Because we did not dispose of the Biosafety Level-3 (BSL-3) facilities, we could not test pathogens such as Burkholderia pseudomallei. No inter-user, intra-lot, or intra-method repetition was done. Furthermore, comparing disc diffusion to MIC values is by itself a limitation of this study, but would have not been financially possible.
5. Conclusions
Confronted with clinical isolates from LRS, MicroScan dried overnight MIC tailored for MSF had excellent performance for Gram-negative, Gram-positive, and fastidious organisms. The Prompt inoculation system together with the Renok transfer system is very convenient but cannot be used for Staphylococci. The study additionally identified potential improvements in stability, robustness, and ease of use to ensure adaptation of the MicroScan system to the constraints of LRS for use outside of the MSF Mini-Lab setting and highlight underseen heteroresistance with the disc diffusion method used to test amoxicillin–clavulanate with Salmonella species, which should be further studied.
Acknowledgments
We thank Cécile Emeraud, Delphine Girlich, Sandrine Bernabeu, Remy Bonnin, Laura Biez, and Camille Gonzalez for their advice concerning the laboratory technical section, and our surveillance study partners for providing the clinical isolates. Furthermore, we are indebted to Barbara Zimmer for her valuable feedback on the use of the panels, comments provided on the article, and intellectual support. Finally, we would like to thank all people involved in MSF, especially the Mini-Lab team, the Mini-Lab scientific committee, and the Mini-Lab Steering committee for their continued and valued scientific and practical input.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/diagnostics12092106/s1, Table S1: List of antibiotics or resistance mechanisms tests included onto the different MSF MIC panels as pers WHO AWaRe category and based on the list of essential medicine, Table S2. (a) MicroScan MSF Dried Overnight Gram-Negative panel are designed for use in determining antimicrobial agent sus-ceptibility of aerobic and facultatively anaerobic gram-negative bacilli (Enterobacteriacea and non-fermenting Gram negative bacilli), Table S2. (b) MicroScan MSF Dried Overnight Gram Positive panel are designed for the determination of antimicrobial agent sus-ceptibility of rapidly growing aerobic and facultative gram-positive cocci (Staphylococcus spp and Enterococcus spp), Table S2. (c) MicroScan MSF Dried Overnight Fastidious panel are designed for use in determining antimicrobial agent suscepti-bility of aerobic non-enterococcal streptococci (including Streptococcus pneumoniae) and Haemophilus spp. Not to be used for testing of Neisseria, Table S3: Technical information on the different panel, disc, media used for the experiment (Lot number, reference, expiry date, etc.), Table S4: Results for Staphylococci tested with MICPOS1 using Prompt inoculum method and visual reading versus AST reference panels, Table S5: Results for Enterococci tested with MICPOS1 using Prompt inoculum method and visual reading versus AST reference panels, Table S6: Results for Enterobacterales tested with MICNEG1 using Prompt inoculum method and visual reading versus AST reference panels, Table S7: Results for Non-fermenting Gram negative bacilli tested with MICNEG1 using Prompt inoculum method and visual reading versus AST reference panels, Table S8: Results for specific resistance test using MICNEG1 or MICPOS1 using Prompt inoculum method and visual reading versus AST reference methods, Figure S1: Extraction of the Prompt® Inoculation System-D Instruction For Use with Microdilution Susceptibility Tests with, (a) general instructions and (b) bench aid like part with more comprehensive instructions, Table S9: Results of the repetition done for AMC discrepant results using different AST methods and brand for disc, media, Figure S2: Extraction of Mini-Lab Bench aid user manual Version1 2022 with, (a) description of type of growth and (b) visual description of the identification of MIC and mechanism of resistance.
Author Contributions
Conceptualization, J.-B.R., S.O., C.L., T.K., A.N., O.V. and T.N.; data curation, J.-B.R.; formal analysis, J.-B.R. and A.N.; funding acquisition, J.-B.R.; methodology, J.-B.R., S.O., C.L., T.K., A.N., W.E., L.H., O.V. and T.N.; project administration, J.-B.R.; supervision, A.N., O.V. and T.N.; visualization, J.-B.R.; writing—original draft preparation, J.-B.R.; writing—review and editing, all authors. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Because the study did not involve research on human or animal subjects, data, or material, ethical clearance was waived. Bacterial isolates were obtained from microbiological surveillance studies in LRS (surveillance of antimicrobial resistance among consecutive blood culture isolates in tropical settings, Institutional Review Board number 613/08, Ethical Committee Antwerp University Hospital 8/20/96) or from anonymous strain collections of Institute of Tropical Medicine (ITM) travel clinic, Antwerp, Belgium or the Bicêtre University Hospital, French National Referral Laboratory for Antibiotic Resistance (French AMR NRL), and of the Saint Pierre Laboratoire Hospitalo-Universitaire Brussel-Université Libre Bruxelle (LHUB-ULB).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data will be available upon reasonable request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest. The manufacturer of the panels had no role in the design of the study, in the collection, analyses, or interpretation of data, in the writing of the manuscript, or in the decision to publish the results.
Funding Statement
This study was funded by Médecins Sans Frontières (Mini-Lab project) under the transformational investment committee, funding number: STATIC001.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nadimpalli M., Delarocque-Astagneau E., Love D.C., Price L.B., Huynh B.-T., Collard J.-M., Lay K.S., Borand L., Ndir A., Walsh T., et al. Combating Global Antibiotic Resistance: Emerging One Health Concerns in Lower-and Middle-Income Countries. Clin. Infect. Dis. 2018;66:963–969. doi: 10.1093/cid/cix879. [DOI] [PubMed] [Google Scholar]
- 2.Iskandar K., Molinier L., Hallit S., Sartelli M., Catena F., Coccolini F., Hardcastle T.C., Roques C., Salameh P. Drivers of antibiotic resistance transmission in low-and middle-income countries from a ‘one health’ perspective—A review. Antibiotics. 2020;9:372. doi: 10.3390/antibiotics9070372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O’Neill J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. The Review on Antimicrobial Resistance; London, UK: May, 2016. [Google Scholar]
- 4.Murray C.J., Ikuta K.S., Sharara F., Swetschinski L., Aguilar G.R., Gray A., Han C., Bisignano C., Rao P., Wool E., et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet. 2022;399:629–655. doi: 10.1016/S0140-6736(21)02724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Founou R.C., Founou L.L., Essack S.Y. Clinical and economic impact of antibiotic resistance in developing countries: A systematic review and meta-analysis. PLoS ONE. 2017;12:e0189621. doi: 10.1371/journal.pone.0189621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bebell L.M., Muiru A.N. Antibiotic use and emerging resistance: How can resource-limited countries turn the tide? Glob. Heart. 2014;9:347–358. doi: 10.1016/j.gheart.2014.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clift C. The Royal Institute of International Affairs. Forest Stewardship Council; Bonn, Germany: 2019. Review of Progress on Antimicrobial Resistance. [Google Scholar]
- 8.Gelband H., Molly Miller P., Pant S., Gandra S., Levinson J., Barter D., White A., Laxminarayan R. State of the World’s Antibiotics 2015. Wound Health S. Afr. 2015;8:30–34. [Google Scholar]
- 9.World Health Organization . Global Antimicrobial Resistance Surveillance System (GLASS) Report: Early Implementation 2016–2017. WHO; Geneva, Switzerland: 2017. [Google Scholar]
- 10.World Health Organization . Presentation WHO Report on Antibacterial Resistance. WHO; Geneva, Switzerland: 2014. [Google Scholar]
- 11.Ashley E.A., Recht J., Chua A., Dance D., Dhorda M., Thomas N., Ranganathan N., Turner P., Guerin P.J., White N.J. An Analysis of Surveillance Networks. IDDO; Oxford, UK: 2016. Antimicrobial Resistance in Low and Middle Income Countries. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Welcome Trust . The Global Response to AMR: Momentum, Success, and Critical Gaps. Wellcome Trust; London, UK: 2020. [Google Scholar]
- 13.Gandra S., Alvarez-Uria G., Turner P., Joshi J., Limmathurotsakul D., van Doorn H.R. Antimicrobial resistance surveillance in low-and middle-income countries: Progress and challenges in eight South Asian and Southeast Asian countries. Clin. Microbiol. Rev. 2020;33:e00048-19. doi: 10.1128/CMR.00048-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lewis J.M., Feasey N.A., Rylance J. Aetiology and outcomes of sepsis in adults in sub-Saharan Africa: A systematic review and meta-analysis. Crit. Care. 2019;23:212. doi: 10.1186/s13054-019-2501-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Girosi F., Olmsted S.S., Keeler E., Burgess D.C.H., Lim Y.-W., Aledort J.E., Rafael M.E., Ricci K.A., Boer R., Hilborne L., et al. Developing and interpreting models to improve diagnostics in developing countries. Nature. 2006;444:3–8. doi: 10.1038/nature05441. [DOI] [PubMed] [Google Scholar]
- 16.Jacobs J., Hardy L., Semret M., Lunguya O., Phe T., Affolabi D., Yansouni C., Vandenberg O. Diagnostic Bacteriology in District Hospitals in Sub-Saharan Africa: At the Forefront of the Containment of Antimicrobial Resistance. Front. Med. 2019;6:205. doi: 10.3389/fmed.2019.00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ombelet S., Barbé B., Affolabi D., Ronat J.-B., Lompo P., Lunguya O., Jacobs J., Hardy L. Best Practices of Blood Cultures in Low- and Middle-Income Countries. Front. Med. 2019;6:131. doi: 10.3389/fmed.2019.00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saeed D.K., Hasan R., Naim M., Zafar A., Khan E., Jabeen K., Irfan S., Ahmed I., Zeeshan M., Wajidali Z., et al. Readiness for antimicrobial resistance (AMR) surveillance in Pakistan; a model for laboratory strengthening. Antimicrob. Resist. Infect. Control. 2017;6:101. doi: 10.1186/s13756-017-0260-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hazim C., Ibrahim R.A., Westercamp M., Belete G.A., Kibret B.A., Kanter T., Yimer G., Adem T.S., Stevenson K.B., Urrego M., et al. Establishment of a Sentinel Laboratory-Based Antimicrobial Resistance Surveillance Network in Ethiopia. Health Secur. 2018;16((Suppl. S1)):S30–S36. doi: 10.1089/hs.2018.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ombelet S., Ronat J.-B., Walsh T., Yansouni C.P., Cox J., Vlieghe E., Martiny D., Semret M., Vandenberg O., Jacobs J., et al. Clinical bacteriology in low-resource settings: Today’s solutions. Lancet Infect. Dis. 2018;18:e248–e258. doi: 10.1016/S1473-3099(18)30093-8. [DOI] [PubMed] [Google Scholar]
- 21.Baron E.J. Clinical Microbiology in Underresourced Settings. Clin. Lab. Med. 2019;39:359–369. doi: 10.1016/j.cll.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 22.Okeke I.N., Feasey N., Parkhill J., Turner P., Limmathurotsakul D., Georgiou P., Holmes A., Peacock S.J. Leapfrogging laboratories: The promise tech solutions for and pitfalls of high-tech solutions for antimicrobial resistance surveillance in low-income settings. BMJ Glob. Health. 2020;5:e003622. doi: 10.1136/bmjgh-2020-003622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ronat J.-B., Natale A., Kesteman T., Andremont A., Elamin W., Hardy L., Kanapathipillai R., Michel J., Langendorf C., Vandenberg O., et al. AMR in low-resource settings: Médecins Sans Frontières bridges surveillance gaps by developing a turnkey solution, the Mini-Lab. Clin. Microbiol. Infect. 2021;27:1414–1421. doi: 10.1016/j.cmi.2021.04.015. [DOI] [PubMed] [Google Scholar]
- 24.Natale A., Ronat J.-B., Mazoyer A., Rochard A., Boillot B., Hubert J., Baillet B., Ducasse M., Mantelet F., Oueslati S., et al. The Mini-Lab: Accessible clinical bacteriology for low-resource settings. Lancet Microbe. 2020;1:e56–e58. doi: 10.1016/S2666-5247(20)30012-4. [DOI] [PubMed] [Google Scholar]
- 25.Ombelet S., Natale A., Ronat J.-B., Kesteman T., Vandenberg O., Jacobs J., Hardy L. Biphasic versus monophasic manual blood culture bottles for low-resource settings: An in-vitro study. The Lancet Microbe. 2022;3:e124–e132. doi: 10.1016/S2666-5247(21)00241-X. [DOI] [PubMed] [Google Scholar]
- 26.Ombelet S., Natale A., Ronat J.-B., Vandenberg O., Hardy L., Jacobs J. Evaluation of MicroScan Bacterial Identification Panels for Low-Resource Settings. Diagnostics. 2021;11:349. doi: 10.3390/diagnostics11020349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization . GLASS Manual for Early Implementation. WHO; Geneva, Switzerland: 2015. [Google Scholar]
- 28.Jorgensen J.H., Ferraro M.J. Antimicrobial susceptibility testing: A review of general principles and contemporary practices. Clin. Infect. Dis. 2009;49:1749–1755. doi: 10.1086/647952. [DOI] [PubMed] [Google Scholar]
- 29.The European Committee and Antimicrobial Susceptibility Testing . Testing Breakpoint Tables for Interpretation of MICs and Zone Diameters. Volume 10 EUCAST; Växjö, Sweden: 2020. [Google Scholar]
- 30.World Health Organization . Mental and Holistic Health: Some International Perspectives. Volume 21. WHO; Geneva, Switzerland: 2019. World health organization model list of essential medicines; pp. 119–134. [Google Scholar]
- 31.Sharland M., Pulcini C., Harbarth S., Zeng M., Gandra S., Mathur S., Magrini N. Classifying antibiotics in the WHO Essential Medicines List for optimal use—Be AWaRe. Lancet Infect. Dis. 2018;18:18–20. doi: 10.1016/S1473-3099(17)30724-7. [DOI] [PubMed] [Google Scholar]
- 32.Clinical and Laboratory Standards Institute (CLSI) M100 Performance Standards for Antimicrobial Susceptibility Testing M100-Ed29. CLSI; Wayne, PA, USA: 2019. [Google Scholar]
- 33.EUCAST . Breakpoint Tables for Interpretation of MICs and Zone Diameters. Volume 9 EUCAST; Växjö, Sweden: 2019. [Google Scholar]
- 34.EUCAST . EUCAST System for Antimicrobial Abbreviations. EUCAST; Växjö, Sweden: 2018. [Google Scholar]
- 35.ISO . Clinical Laboratory Testing and In Vitro Diagnostic Test Systems—Susceptibility Testing of Infectious Agents and Evaluation of Performance of Antimicrobial Susceptibility Test Devices—Part 2: Evaluation of Performance of Antimicrobial Susceptibility Test Devices Against Reference Broth Micro-Dilution. ISO; Geneva, Switzerland: 2007. [Google Scholar]
- 36.CLSI . Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard—Ninth Edition 32. CLSI; Wayne, PA, USA: 2012. [Google Scholar]
- 37.Matuschek E., Brown D.F.J., Kahlmeter G. Development of the EUCAST disk diffusion antimicrobial susceptibility testing method and its implementation in routine microbiology laboratories. Clin. Microbiol. Infect. 2014;20:O255–O266. doi: 10.1111/1469-0691.12373. [DOI] [PubMed] [Google Scholar]
- 38.Flejzor B., Bokkenheuser V.D. Performance of the prompt system in identification and antimicrobial susceptibility testing of clinical isolates. J. Clin. Microbiol. 1985;21:267–268. doi: 10.1128/jcm.21.2.267-268.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.EUCAST . European Committee on Antimicrobial Susceptibility Testing. EUCAST; Växjö, Sweden: 2020. EUCAST reading guide for broth microdilution (version 2.0) pp. 1–20. [Google Scholar]
- 40.Stelling J.M. News and Notes WHONET: An Information System for Monitoring Recommendations for Preventing the Spread of Antimicrobial resistance. Emerg. Infect. Dis. 1995;1:66–67. doi: 10.3201/eid0102.950209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hindler J., Stelling J. Analysis and presentation of cumulative antibiograms: A new consensus guideline from the Clinical and Laboratory Standards Institute. Clin. Infect. Dis. 2007;44:867–873. doi: 10.1086/511864. [DOI] [PubMed] [Google Scholar]
- 42.Cohen J. A coefficient of agreement for nominal scales. Educ. Psychol. Meas. 1960;20:37–46. doi: 10.1177/001316446002000104. [DOI] [Google Scholar]
- 43.Bankert D.A., Crist A.E., George W., Eastman J.T., Han A., Horning A. Multicenter Evaluation of Four Automated ID/AST Systems for Antimicrobial Susceptibility Testing of Commonly Isolated Enterococcus spp. and Staphylococcus spp. American Society of Microbiology; Washington, DC, USA: 2007. pp. 1–4. [Google Scholar]
- 44.Anderson K.F., Lonsway D.R., Rasheed J.K., Biddle J., Jensen B., McDougal L.K., Carey R.B., Thompson A., Stocker S., Limbago B., et al. Evaluation of methods to identify the Klebsiella pneumoniae carbapenemase in Enterobacteriaceae. J. Clin. Microbiol. 2007;45:2723–2725. doi: 10.1128/JCM.00015-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bankert D.A. ASM2. American Society of Microbiology; Washington, DC, USA: 2006. C-122 Multicenter Evaluation of Four Automated ID/AST Systems for Antimicrobial Susceptibility Testing of Enterobacteriaceae and Commonly Isolated Glucose Non-Fermenting Gram-Negative Bacilli; p. 122. [Google Scholar]
- 46.Roe D. A Multicenter Evaluation of a MicroScan Dried Overnight Panel for Screening E. coli and Klebsiella spp. for the Presence of ESBLs. American Society of Microbiology; Washington, DC, USA: 1999. pp. 1–5. [Google Scholar]
- 47.Rennie R. et al. Multicenter Evaluation of Daptomycin and Ertapenem in a MicroScan Dried Overnight Panel with Gram-Positive Bacteria. American Society of Microbiology; Washington, DC, USA: 2005. pp. 1–6. [Google Scholar]
- 48.Creely D., Zambardi G., Van Belkum A., Dunne W.M., Peyret M., Gayral J.P., Shortridge D., Shubert C. International dissemination of Escherichia coli strains with discrepant behaviour in phenotypic antimicrobial susceptibility tests. Eur. J. Clin. Microbiol. Infect. Dis. 2013;32:997–1002. doi: 10.1007/s10096-013-1837-5. [DOI] [PubMed] [Google Scholar]
- 49.Shubert C., Slaughter J., Creely D., van Belkum A., Gayral J.P., Dunne W.M., Zambardi G., Shortridge D. Population analysis of Escherichia coli isolates with discordant resistance levels by piperacillin-tazobactam broth microdilution and agar dilution testing. Antimicrob. Agents Chemother. 2014;58:1779–1781. doi: 10.1128/AAC.02181-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lo-Ten-Foe J.R., de Smet A.M.G.A., Diederen B.M.W., Kluytmans J.A.J.W., van Keulen P.H.J. Comparative evaluation of the VITEK 2, disk diffusion, etest, broth microdilution, and agar dilution susceptibility testing methods for colistin in clinical isolates, including heteroresistant Enterobacter cloacae and Acinetobacter baumannii strains. Antimicrob. Agents Chemother. 2007;51:3726–3730. doi: 10.1128/AAC.01406-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nicoloff H., Hjort K., Levin B.R., Andersson D.I. The high prevalence of antibiotic heteroresistance in pathogenic bacteria is mainly caused by gene amplification. Nat. Microbiol. 2019;4:504–514. doi: 10.1038/s41564-018-0342-0. [DOI] [PubMed] [Google Scholar]
- 52.Andersson D.I., Nicoloff H., Hjort K. Mechanisms and clinical relevance of bacterial heteroresistance. Nat. Rev. Microbiol. 2019;17:479–496. doi: 10.1038/s41579-019-0218-1. [DOI] [PubMed] [Google Scholar]
- 53.Lund M.E., Hawkinson R.W. Evaluation of the prompt inoculation system for preparation of standardized bacterial inocula. J. Clin. Microbiol. 1983;18:84–91. doi: 10.1128/jcm.18.1.84-91.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.World Health Organization . COVID-19 Target Product Profiles for Priority Diagnostics to Support Response to the COVID-19 Pandemic. Volume 0 WHO; Geneva, Switzerland: 2020. [Google Scholar]
- 55.World Health Organization Technical Guidance Series (TGS) for WHO Prequalification—Diagnostic Assessment Guidance on Test Guidance on Test Method Validation for In Vitro Diagnostic Medical Devices TGS–4; Tech. Guid. Ser. WHO Prequalification—Diagnostic Assess 2017. [(accessed on 5 May 2022)]. Available online: http://apps.who.int/iris/bitstream/10665/258971/1/WHO-EMP-RHT-PQT-TGS4-2017.04-eng.pdf?ua=1.
- 56.Gillet P., Maltha J., Hermans V., Ravinetto R., Bruggeman C., Jacobs J. Malaria rapid diagnostic kits: Quality of packaging, design and labelling of boxes and components and readability and accuracy of information inserts. Malar. J. 2011;10:39. doi: 10.1186/1475-2875-10-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.A Reddy E., Shaw A.V., A Crump J. Community-acquired bloodstream infections in Africa: A systematic review and meta-analysis. Lancet Infect. Dis. 2010;10:417–432. doi: 10.1016/S1473-3099(10)70072-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kern W.V., Rieg S. Burden of bacterial bloodstream infection—A brief update on epidemiology and significance of multidrug-resistant pathogens. Clin. Microbiol. Infect. 2019;26:151–157. doi: 10.1016/j.cmi.2019.10.031. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data will be available upon reasonable request from the corresponding author.