Abstract
Intrauterine devices (IUDs) are very common as a method of birth control. By adding progesterone (levonorgestrel), a decrease in the risk of complications has been documented, including the risk of perforation. Even though only a few complications have been described, adjacent organs may be involved in the case of migration—a life-threatening situation. A 45-year-old G4P2 woman was seen in our clinic for LNg-IUD removal, according to the medical instructions. Her main complaints were abdominal discomfort, low back pain, and recurrent menorrhagia. A “lost” IUD was initially suspected; the patient confirmed the detection and removal of the control strings, and a subsequent discussion related to delayed transmural migration of the IUD being followed. The ultrasonography revealed the migration of the IUD to the uterine cervix and size-decreased uterine fibroids, confirming the effectiveness of the LNg-IUD. The MRI and ultrasonography being useless, a subsequent X-ray and CT scan were requested, both confirming a myometrium-positioned IUD, adjacent to the serosa and lumbosacral plexus. Even though the IUD is considered a safe device with reversible effect, it can be associated with severe morbidity, with an ultrasound follow-up being required. For more precise detection of the IUD, we strongly recommend an X-ray or CT scan examination, followed by safe removal.
Keywords: intrauterine contraceptive device, transmural migration, embedment, perforation, CT, MRI, ultrasonography
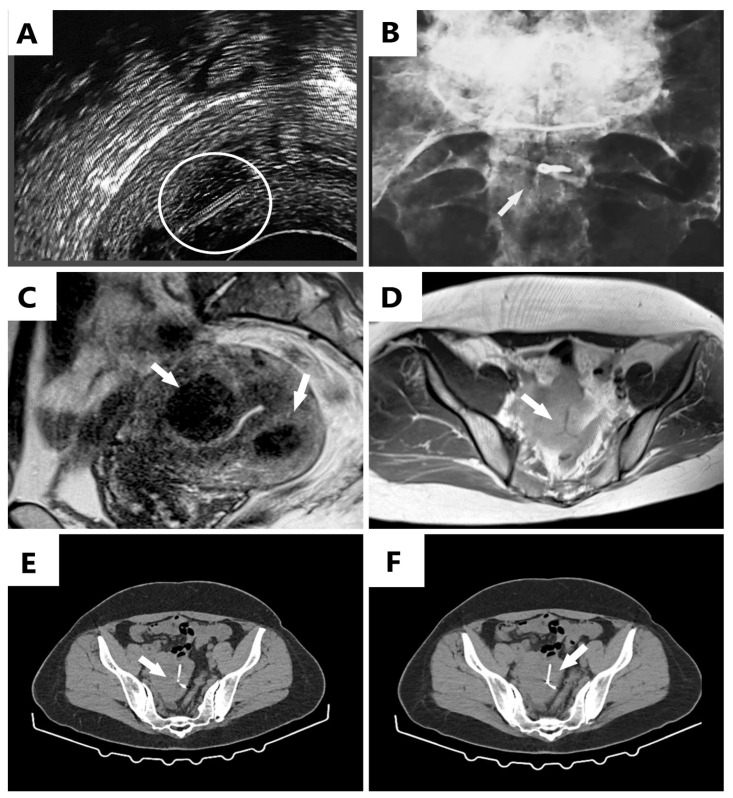
Figure 1.
(A) Ultrasound examination revealing the control strings of the IUD, initially mistaken for a migrated device marked inside the white circle; (B) plain pelvic X-ray revealing the round area of the IUD where the control strings were normally attached (white arrow); (C,D) magnetic resonance imaging (MRI) scans revealing the uterus with two fibroids (white arrows) and no identified IUD (C), and the intramural IUD with a vicious position (upside-down), identified near the serosa (white arrow) (D); (E,F) computed tomography (CT) scan revealing the IUD adjacent to the serosa and lumbosacral plexus (white arrows). A 45-year-old G4P2 woman was seen in our clinic for levonorgestrel (LNg) intrauterine device (IUD) removal according to the medical instructions, having been used for menstrual management. After the insertion of the intrauterine device (IUD), the patient was subsequently followed up with by the gynecology service. Her past medical history included a lumbar discopathy surgery and multiple uterine fibroids, larger than 5 cm in diameter. At the time of admission, the main complaints were about abdominal discomfort, low back pain corresponding to the lumbosacral region of the spine, and recurrent menorrhagia. The ultrasonography revealed what we thought to be the migration of the IUD to the uterine cervix and size-decreased uterine fibroids to 3.5 cm in diameter. The effectiveness of the LNg-IUD was confirmed; not only did it reduce the menorrhagia, but it also reduced the size of the fibroids. An attempt to remove the IUD by extraction failed, obtaining only the control strings of the intrauterine device. Another unsuccessful attempt by hysteroscopy followed, with no evidence of the IUD in the uterine cavity. In the first instance, a “lost” IUD was suspected; however, the patient confirmed the detection and removal of the control strings, a fact that determined a subsequent discussion related to delayed transmural migration of the IUD. Since a subsequent perforation was expected, radiography was requested. Even if the IUD was identified in the myometrium, its vicious position prevented a correct diagnosis: only the part where the strings were attached was visible (Figure 1A), and the device was seen as midline-placed, adjacent to the lumbosacral plex (Figure 1B). Since our patient had in her past medical history a lumbar discopathy surgery, it was considered an explanation for her lumbosacral pains, with no direct causality with the IUD being suspected. A magnetic resonance imaging (MRI) scan by the doctor who performed the hysteroscopy and a computed tomography (CT) scan by the doctor who attempted to remove the IUD were indicated. The MRI scan was declared not very effective at highlighting the device (Figure 1C,D). The CT scan (Figure 1E,F) revealed the myometrium-positioned IUD, adjacent to the serosa and lumbosacral plexus, a fact that explained the patient’s lumbar pain. Furthermore, subsequent removal by laparoscopic hysterectomy with an eventual conversion to laparotomy in the case of failure was proposed. This maneuver was successfully performed, and the patient easily recovered without difficulties, the back pain has subsided. To our knowledge, complications occur rarely, of 1/1000 insertions [1], but these can be severe and life-threatening, such as intramural IUD migration, with one of two manifestations: embedment, in which case it does not exceed the serosa, remaining at the level of myometrium, or perforation, in which case it can migrate to the organs inside the peritoneal cavity, a situation encountered in 85% of cases [1]. Another complication described was related to an intrauterine device identified within an ovarian tumor, in a 63-year-old patient, without a clear explanation as to whether the tumor was a consequence of the migration of the IUD inside the ovary or its development was concomitant [1]. The mechanism of migration remains unknown [1], but uterine contractions are thought to play a role [2,3,4]. According to Chai et al., two devices encountered in the same patient were described as migrating devices, the second one being inserted during a cesarean section procedure, both exceeding the uterine serosa and discovered on CT scan, the second one being inserted after considering the first one, erroneously, “lost” [5]; this incident draws attention to the importance of an accurate diagnosis before making a decision to mount another intrauterine device. As in our patient’s case, migration of the IUD can occur over time as a distant migration, a result of gradual erosion of the myometrium [2,3], or it can occur immediately after insertion, this phenomenon being encountered in the immediate postpartum period. According to World Health Organization (WHO) recommendations, the indicated treatment is extraction of the IUD, as soon as possible; if we are not able to retrieve the device, a laparoscopy should be considered [6,7,8,9,10]. Laparotomy should remain the optimal option for most of the complicated cases [3]. In case of migration in areas such as the rectosigmoid, the colon, or the urinary bladder, other minimally invasive methods should be considered, such as colonoscopy and cystoscopy, as more appropriate [11,12,13,14,15]. The strong point of our case report is represented by the levonorgestrel-releasing IUD detected as migrated before perforating the serosa and bringing about serious consequences for the patient. As levonorgestrel-releasing IUDs are considered useful for the management of menometrorrhagia, these patients require careful follow-up, performing an ultrasound examination of the IUD in the uterine cavity. We strongly recommend that when the IUD cannot be visualized by ultrasound and the control string cannot be seen, it should not be considered as having been expelled. We suggest a subsequent radiographic examination or a CT scan for adequate detection of its localization, followed by safe removal.
Acknowledgments
Many thanks to the patient for her cooperation.
Author Contributions
Conceptualization, M.-I.M.; methodology, M.-I.M., D.M.C. and O.S.C.; software, D.M.C., M.C.M., A.C.T., A.-H.S., M.C.P. and I.-G.C.; validation, M.-I.M., C.M. and M.L.C.; formal analysis, T.I.; investigation, M.-I.M. and D.M.C.; resources, I.P. (Izabella Petre), I.P. (Ion Petre) and E.S.B.; writing—original draft preparation, M.-I.M. and D.M.C.; writing—review and editing, M.-I.M. and D.M.C.; visualization, M.-I.M., R.M., T.I., E.S.B., I.P. (Izabella Petre), and O.S.C.; supervision, M.-I.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to the retrospective case report, which did not impact the management of the patient.
Informed Consent Statement
Written informed consent was obtained from the patient to publish this paper.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tabatabaei F., Masoumzadeh M. Dislocated intrauterine devices: Clinical presentations, diagnosis and management. Eur. J. Contracept. Reprod. Health Care. 2021;26:160–166. doi: 10.1080/13625187.2021.1874337. [DOI] [PubMed] [Google Scholar]
- 2.Akpinar F., Ozgur E.N., Yilmaz S., Ustaoglu O. Sigmoid colon migration of an intrauterine device. Case Rep. Obstet. Gynecol. 2014;2014:207659. doi: 10.1155/2014/207659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ayodele A., Oloruntobi R. Perforation of the appendix and the sigmoid colon by an ectopic IUD. Int. J. Reprod. Contracept. Obstet. Gynecol. 2017;4:1618–1621. doi: 10.18203/2320-1770.ijrcog20150762. [DOI] [Google Scholar]
- 4.Cheung M.L., Rezai S., Jackman J.M., Patel N.D., Bernaba B.Z., Hakimian O., Nuritdinova D., Turley C.L., Mercado R., Takeshige T., et al. Retained Intrauterine Device (IUD): Triple Case Report and Review of the Literature. Case Rep. Obstet. Gynecol. 2018;2018:9362962. doi: 10.1155/2018/9362962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldstuck N.D., Wildemeersch D. Role of uterine forces in intrauterine device embedment, perforation, and expulsion. Int. J. Womens Health. 2014;6:735–744. doi: 10.2147/IJWH.S63167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weerasekera A., Wijesinghe P., Nugaduwa N. Sigmoid colocolic fistula caused by intrauterine device migration: A case report. J. Med. Case Rep. 2014;8:81. doi: 10.1186/1752-1947-8-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mederos R., Humaran L., Minervini D. Surgical removal of an intrauterine device perforating the sigmoid colon: A case report. Int. J. Surg. 2008;6:e60–e62. doi: 10.1016/j.ijsu.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Dimitropoulos K., Skriapas K., Karvounis G., Tzortzis V. Intrauterine device migration to the urinary bladder causing sexual dysfunction: A case report. Hippokratia. 2016;20:70–72. [PMC free article] [PubMed] [Google Scholar]
- 9.Lauridsen A.H., Olesen P.G. Intrauterine Device Migration. Ugeskr. Laeger. 2012;174:3098. [PubMed] [Google Scholar]
- 10.Rowlands S., Oloto E., Horwell D.H. Intrauterine devices and risk of uterine perforation: Current perspectives. Open Access J. Contracept. 2016;7:19–32. doi: 10.2147/OAJC.S85546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shin D.G., Kim T.N., Lee W. Intrauterine device embedded into the bladder wall with stone formation: Laparoscopic removal is a minimally invasive alternative to open surgery. Int. Urogynecol. J. 2012;23:1129–1131. doi: 10.1007/s00192-011-1632-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Subramanian V., Athanasias P., Datta S., Anjum A., Croucher C. Surgical options for the retrieval of a migrated intrauterine contraceptive device. J. Surg. Case Rep. 2013;2013:rjt072. doi: 10.1093/jscr/rjt072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferguson C.A., Costescu D., Jamieson M.A., Jong L. Transmural migration and perforation of a levonorgestrel intrauterine system: A case report and review of the literature. Contraception. 2016;93:81–86. doi: 10.1016/j.contraception.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 14.Aliukonis V., Lasinskas M., Pilvelis A., Gradauskas A. Intrauterine device migration into the lumen of large bowel: A case report. Int. J. Surg. Case Rep. 2020;72:306–308. doi: 10.1016/j.ijscr.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Golightly E., Gebbie A.E. Low-lying or malpositioned intrauterine devices and systems. J. Fam. Plann. Reprod. Health Care. 2014;40:108–112. doi: 10.1136/jfprhc-2013-100684. [DOI] [PubMed] [Google Scholar]