Abstract
Background:
The increasing awareness and diagnosis of dementia in Africa necessitate documentation of caregiving practices to understand local patterns and improve the quality of care. Caregiving in African communities is rooted in informal-communal social organization. This scoping review analyses caregiver characteristics and experiences, and practices of caregiving for persons living with dementia in Africa.
Methods:
A total of 152 references were retrieved, with 64 references obtained from PubMed, 85 from AJOL, and three from Scopus. Based on the relevance of titles, 83 references were further retained from PubMed (64), AJOL (16), and Scopus (3). A rapid review of abstracts was done in Distiller SR, and finally, six relevant articles were content-analyzed using Atlas ti 8.4 qualitative analysis software.
Results:
All six included studies were published between 2003 and 2018. Four themes were identified: article characteristics, caregiver characteristics, caregiver in context, and caregiver potentialities (challenges and opportunities). Studies reported findings from research conducted in four African countries: three from Nigeria, and one each from South Africa, Egypt, and Tanzania. Caregivers of persons living with dementia typically had eight years or less of formal education, were unpaid, and spent a daily average of 13 hours in caregiving. Cultural thresholds and individual caregiver differences underlie the interpretation of stressors across cultures. Caregivers lack the right training and information as well as support systems to improve their role performance and reduce accumulated stress.
Conclusion:
In African countries, informational and educational platforms are essential for improved individual dementia caregiving, vis-à-vis strengthened roles of governments, and religious/traditional leaders and organizations.
Keywords: dementia, Africa, caregivers, caregiving, older persons, geriatric
Introduction
As an incrementally degenerative neurological condition, dementia can cause the loss of cognitive function across the spectrum of mild to severe stages. Dementia accounts for an increasing decline in the mental capacity for recognition and awareness, affecting social interaction and other functional areas. Alzheimer’s disease is the most common dementia type (Korczyn, 2002). Although younger-onset dementia has emerged as an area of interest in recent studies (Livingston et al., 2020), dementia is predominant among the “elderly.” The cut-off age for “elderly” status is an area of conceptual and practical debate. This debate is essentially a reflection of social, legal, and cultural demarcations of chronological and biological aging. In most studies from low-and-middle-income countries (LMICs), 60 years is a socially acceptable cut-off point for classifying older persons (de Freitas et al., 2010)—although this term is also culturally controversial from a social roles and expectations perspective (Fayehun & Salami, 2014; Omobowale, 2014). As the global population of older persons rises to about two billion in 2050, the African numbers are projected to increase to 213 million (Brown, 2016). By 2050, the estimated prevalence of dementia would have increased to 131.5 million cases, rising from an initial 46.8 million in 2015 (Prince et al., 2015). At least 68% of the world’s dementia population will be from LMICs in 2050, and African people will account for about 14% of dementia cases in LMICs (Prince et al., 2015), increasing from 2.6% in 2015 (Klimova et al., 2016). Dementia is known to be one of the strong correlates of aging (Livingston et al., 2020; Irwin et al., 2018; LoGiudice & Watson, 2014), and the demographic transition in Africa will potentially contribute to the increased prevalence of dementia (Musyimi et al., 2021; World Health Organization, 2011).
The changing health needs and demographics of older persons will expectedly initiate a transition in financing, organization, and health systems administration. However, aging in Africa often occurs within weak or non-existent health policy climates. Especially in these settings, an increasing population of older persons will account for vulnerable populations in poor health (World Health Organization, 2011). Mental health and, specifically, dementia is of particular concern in this context. Dementia diagnoses are bound to increase due to higher life expectancy among older persons. This holds true in high-income countries like Canada and the United States (Manuel et al., 2016; Zissimopoulos et al., 2018). Population dynamics have a direct implication for caregiving needs. With the anticipated increase in dementia burden, especially in African countries, and the potential need for more caregivers, there is a need to better understand the requirements and current care practices for persons living with dementia.
Informal caregiving is the predominant approach to providing general care for older persons in Africa. In the case of dementia, the family’s role is vital to improving early reportage and care of dementia (Uwakwe & Prince, 2004). First, the informal caregiving approach is a culturally-rooted practice; second, orthodox mental healthcare costs are high (Klimova et al., 2016); third, there is stigma associated with dementia (Ineichen, 2000). The need for informal dementia care is also driven by mental health workforce shortages, especially in LMICs (Baiyewu et al., 2003; Gureje et al., 2015). Thus, older people in these countries seldom seek hospital-based dementia care. A Tanzanian study asserted that health facilities’ elderly care is not for treating dementia but other comorbidities (Mushi et al., 2014). Traditional African societies have a kinship, family, and household network (horizontal and vertical), which meets older persons’ care needs. Nearly 80% of caregivers for people living with dementia are their children, and females predominantly occupy a caregiving role in dementia care (Osundina et al., 2016; Uwakwe et al., 2009). A gendered slant in this role has immense health and social implications for women.
The cognitive and behavioral manifestations of dementia impose significant physical, social, and psychological stress on caregivers. In the typical situation, informal caregivers do not possess sufficient training to effectively recognize and provide home-management for the cognitive and behavioral manifestations of dementia (Mushi et al., 2014). Hence, they are ill-prepared to address these challenges. Although numeric scales measure dementia caregiver burden (Langman, 2016; Peipert et al., 2018), the underlying dynamics and socio-cultural dimensions are mostly underinvestigated. Caregivers of persons living with dementia often require professional counseling (Lopez-Hartmann et al., 2012), support groups (Clarke et al., 2013), and supporting infrastructure like daycare centers to improve their caregiver roles and quality of life outcomes. Emerging ethnographic evidence (Tanyi et al., 2018) demonstrates that in most parts of Africa, the family as social protection and source of informal caregiving for older persons is declining. Migration from rural to urban areas, particularly among girls and young women, has reduced the availability of traditional support systems (Uwakwe et al., 2009).
Among African countries, there is a paucity of literature regarding the pattern and practice of dementia caregiving, and individuals involved. In this scoping review, we aim to (1) Describe sociodemographic characteristics of dementia caregivers in Africa, (2) Document the contexts and patterns of dementia caregiving in Africa by focusing on the experiences, practices, and challenges associated with dementia caregiving roles, and (3) Explore opportunities for improving the experiences and practices of dementia caregiving in Africa.
Methods
We conducted a scoping review of studies reporting on dementia caregiving practices in African countries, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) (Munn et al., 2018).
Search strategy
We searched PubMed (1950—to week 4 of January 2020); Scopus (the 1990s—week 1 of February 2020); African Journals Online (AJOL)—(the 1990s—week 4 of January 2020). We used operators and took cognizance of MeSH (Medical subject heading) terms and their associated approaches. There were variations across the broad terms—dementia OR dementia care OR dementia care mapping OR dementia/family caregiver AND Alzheimer’s and caregiver OR Alzheimer’s care OR Alzheimer’s caregiver education AND Africa OR Nigeria.
Study selection
Studies were selected based on the following inclusion criteria: (1) Title reflects a focus on Africa (2) Written in English Language, (3) focused on any of the dementias, (4) conducted in Africa and among Africans in Africa, (5) designed based on a systematic process of methods—qualitative or quantitative traditions of inquiry, and (6) specific references made to the roles of “caregivers” or “carers” in dementia caregiving. This was to ensure that the personal/social characteristics of caregivers, challenges/gaps, and opportunities for dementia caregiving in the African context were highlighted.
A total of 152 references were retrieved: 64 from PubMed, 85 from AJOL, and three from Scopus (Figure 1) As a first exclusion criteria, titles that did not refer to Africa or an Africa country were removed from the list. This reduced the number to 83 references (PubMed—64, AJOL-16, and three from Scopus) and these were imported into Endnote, (a reference manager which has an interface for extracting abstracts and full-text articles). From Endnote, abstracts corresponding to the imported references were extracted, and these were exported to Distiller SR. which is a literature review software platform that standardizes the data collection, triage and assessment process, thus facilitating transparency and reproducibility of reviews. Using Distiller SR, an independent rapid review of abstracts was done; exclusion criteria ensured that abstracts focused specifically on one or more African countries. These exclusions rendered 67 more abstracts ineligible. The full texts of 16 articles were downloaded and exported to Atlas Ti 8.4 software, a qualitative data analysis tool used for content-analysis of textual data through a system of inductive and/or deductive codes to depict contexts and social processes. Here, exclusion criteria were to ensure that each article provided relevant contextual analysis of the experiences and practices of dementia caregiving in a specific African country. Ten articles were excluded because they did not make sufficiently specific reference to dementia caregiving in a given African country/countries. Ultimately, only six articles were assessed for the final stage of the scoping review.
Figure 1.
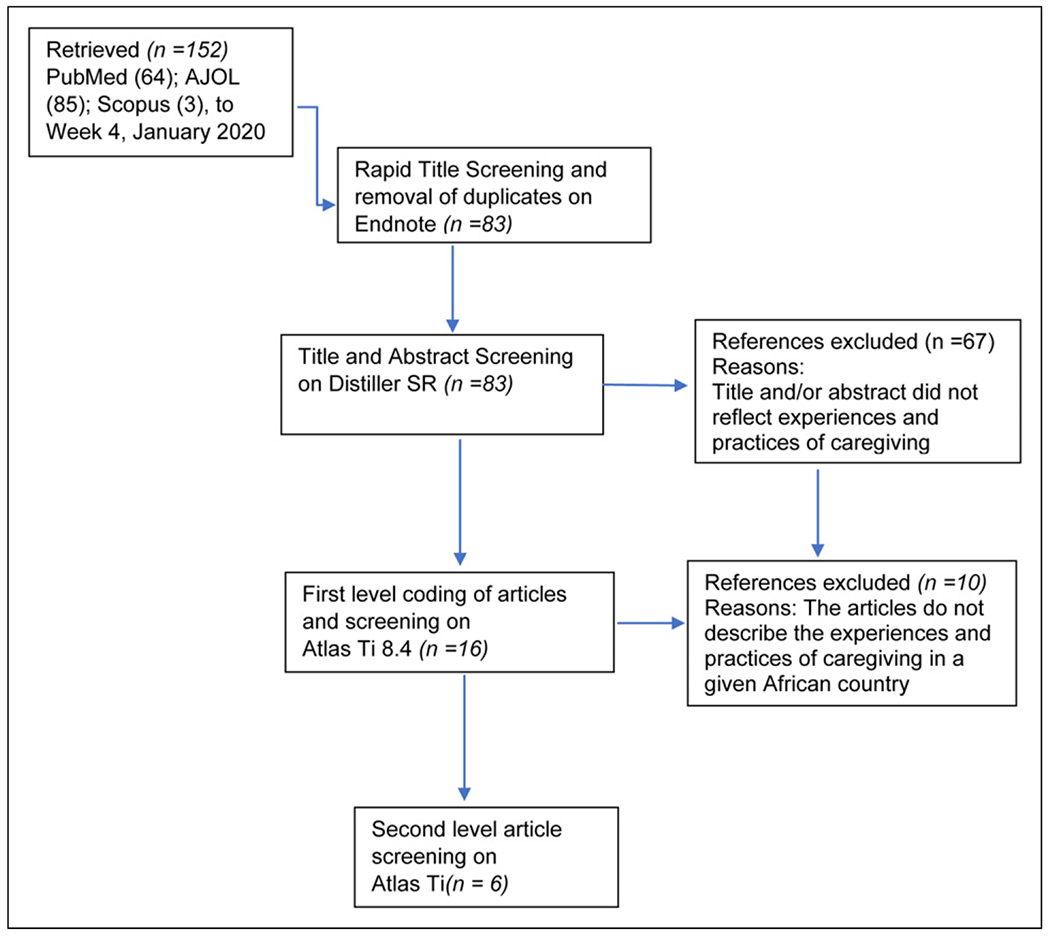
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension flow diagram for scoping literature review of experiences and practices of dementia caregiving for older persons in Africa.
Data extraction and analysis
This scoping review aimed not to pool data as in a quantitative review, but to provide a narrative of prevailing caregiving practices and identify patterns. We turned to the epistemological and ontological bases of reflexivity in qualitative analysis (Evans et al., 2018; Mills et al., 2010). Reflexivity addresses the researchers’ bias in qualitative data analysis. Therefore, using Atlas Ti, we adopted two iterative steps of content analysis. In the first stage, codes were created a posteriori—this process allowed for deductive engagement with the articles. In the first step of content analysis, a total of 35 codes were assigned to 164 quotations across 16 documents. In the second iterative step of content analysis, through inductive logic, the existing codes were restructured, such that four main themes emerged, consisting of 21 parent cross-cutting codes and five sub-codes across six documents (Table 1).
Table 1.
Data extraction and analysis description–first and second stages of textual analysis.
| S/N | First level codes | Themes | Major codes | Sub-codes | ||
|---|---|---|---|---|---|---|
| 1 | Alzheimer’s disease profile | 1 | Study characteristics | 1 | Research design | i.) Research tradition |
| 2 | Age of caregiver | |||||
| 3 | Areas of needs for caregiving/ | ii.) Research instrument | ||||
| 4 | caregivers | |||||
| 5 | Behavioral issues | iii.) Unit of analysis | ||||
| 6 | Benefits of caregiving | |||||
| 7 | Data/Facts on incidence/ | 2 | Study site | i.) Area | ||
| 8 | prevalence | ii.) Setting | ||||
| 9 | Cause(s) of dementia | 2 | Caregiver characteristics | 3 | Sample size | |
| 10 | Dementia - incidence | 4 | Gender | |||
| 11 | Dimensions of dependence | 5 | Age | |||
| 12 | Education of caregiver | 6 | Employment status | |||
| 13 | Effect of dementia on | 7 | Socio-economic status | |||
| 14 | caregiver | 8 | Education of caregivers | |||
| 15 | Effect on the family | 9 | Medical training for | |||
| 16 | Employment status of | 10 | geriatric care | |||
| 17 | caregiver-Employed/ | 11 | Relationship of | |||
| 18 | Unemployed | 12 | caregiver with the | |||
| 19 | Ethical issues-regarding | 13 | patient | |||
| 20 | Do Not Resuscitate considerations | 14 | The regularity of seeing the patient | |||
| 21 | Familial caregivers/ | |||||
| 22 | caregiving | Number of hours of | ||||
| 23 | Gender of caregiver | caregiving | ||||
| 24 | Health care-pathways | Length of caregiving | ||||
| 25 | Help provided/required | years | ||||
| 26 | History | Living arrangement for caregiving | ||||
| 27 | Hours spent on caregiving | |||||
| 28 | Length of caregiving | 3 | The caregiver in context | 15 | Health care pathways | |
| 29 | Living arrangement | 16 | Source of support for | |||
| 30 | Pathways to care | 17 | caregivers | |||
| 31 | Reaction to diagnosis | 18 | Kind of support | |||
| 32 | Relationship of caregiver with | 19 | provided | |||
| 33 | patient | Recognizable | ||||
| 34 | Research design | symptoms of dementia | ||||
| 35 | Relationship/interaction | Stressors | ||||
| Role of culture | 4 | Potentialities | 20 | Challenges | ||
| Role of government | 21 | Opportunities | ||||
| Socio-economic status of the caregiver | ||||||
| Source of caregiving knowledge | ||||||
| Specific challenges identified for caregivers | ||||||
| Theoretical explanation | ||||||
| Treatment issues |
Results
The six included articles engaged fundamental issues in the dementia caregiving discourse. The engagement included living arrangements and health care pathways. Also, the articles interrogated conditions such as length of caregiving and personal characteristics of caregivers. The articles discussed and/or highlighted challenges/gaps and opportunities for dementia caregiving in African contexts.
Characteristics of selected studies
Selected studies are shown in Table 2. Three of the articles were published from Nigeria (Baiyewu et al., 2003; Ogunniyi et al., 2005; Yusuf & Baiyewu, 2012), and one from South Africa (Hendricks-Lalla & Pretorius, 2020), Egypt (Mansi, 2014), and Tanzania (Mushi et al., 2014). One study was conducted in a predominantly rural setting in Tanzania (Mushi et al., 2014). All the studies were published between 2003 and 2020. The research design of all but two (Baiyewu et al., 2003; Ogunniyi et al., 2005) were outcomes of cross-sectional studies. These two articles reported two different aspects of findings from a major longitudinal study of dementia (the Indianapolis–Ibadan Dementia study) which was conducted in Nigeria from 1992 to 2011. Only one study adopted a purely quantitative approach (Yusuf & Baiyewu, 2012); two studies adopted a sequential quantitative-qualitative approach (Baiyewu et al., 2003; Ogunniyi et al., 2005), and the remaining three studies were purely qualitative in approach (Hendricks-Lalla & Pretorius, 2020; Mansi, 2014; Mushi et al., 2014). Caregivers were purposively selected for inclusion in all the studies, and were included as “primary caregivers” who provided care to validly diagnosed care recipients.
Table 2.
Study characteristics.
| Research design |
Study site |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Author(s) | Title of article | Year | Country | Type of article | Research tradition | Research instrument | Unit of analysis | Study area | Setting | |
| 1 | Hendricks-Lalla, A., Pretorius, C | The male familial caregiver experience of caring for persons with Alzheimer’s disease from low socioeconomic status: A South African perspective | 2020 | South Africa | Empirical | Qualitative/cross-sectional | Semi-structured interviews | Male caregivers | Cape town | Urban |
| 2 | Mansi, I. A | Between two worlds | 2014 | Egypt | Empirical | Case-study | Life history | Individuals | Alexandria | Urban |
| 3 | Mushi, D., Rongai, A., Paddick, S. M., Dotchin, C., Mtuya, C., Walker, R | Social representation and practices related to dementia in Hai District of Tanzania | 2014 | Tanzania | Empirical | Qualitative/cross-sectional | Interview guides | Individuals (people Living with dementia and caregivers) | Hai district | Rural |
| 4 | Baiyewu, O., Smith-Gamble, V., Akinbiyi, A., Lane, K. A., Hall, K. S., Ogunniyi, A., Gureje, O., Hendrie, H. C | Behavioral and caregiver reaction of dementia as measured by the neuropsychiatric inventory in Nigerian community residents | 2003 | Nigeria | Empirical | Quantitative/longitudinal | Mini-mental state examination (MMSE); blessed Activities of daily Living (ADL); NPI (neuropsychiatric inventory) | Individuals | Ibadan | Urban |
| 5 | Ogunniyi, A., Hall, K.S., Baiyewu, O., Gureje, O., Unverzagt, F.W. | Caring for individuals with dementia: The Nigerian experience | 2005 | Nigeria | Report | Qualitative and quantitative | Mini-mental state examination (MMSE); blessed Activities of daily Living (ADL); NPI (neuropsychiatric inventory) | Individuals | Ibadan | Urban |
| 6 | Yusuf, A.J., Baiyewu, O | Beliefs and Attitudes towards dementia among community leaders in northern Nigeria | 2012 | Nigeria | Empirical | Quantitative/Cross-sectional | Questionnaire | Group (Community leaders) | Zaria | Urban |
Socio-demographic characteristics of caregivers
The data in Table 3 presents socio-demographic characteristics of the 267 caregivers described in the six reviewed studies. More females than males were involved in domestic caregiving of persons with dementia. The lowest age of caregivers was 19 years, mostly unemployed (Hendricks-Lalla & Pretorius, 2020; Mansi, 2014; Mushi et al., 2014); most caregivers were unpaid family members (Baiyewu et al., 2003; Hendricks-Lalla & Pretorius, 2020;Mushi et al., 2014; Ogunniyi et al., 2005), and were predominantly of low-income status (Hendricks-Lalla & Pretorius, 2020; Mansi, 2014; Ogunniyi et al., 2005). Formal education received was not higher than eight years of schooling (Hendricks-Lalla & Pretorius, 2020; Mansi, 2014; Mushi et al., 2014; Ogunniyi et al., 2005; Yusuf & Baiyewu, 2012). Some form of semi-formal training and apprenticeship for older persons’ care was documented among caregivers (Mansi, 2014; Ogunniyi et al., 2005).
Table 3.
Socio-demographic characteristics of caregivers.
| Hendricks-Lalla and Pretorius (2020) | Mansi (2014) | Mushi et al. (2014) | Baiyewu et al. (2003) | Ogunniyi et al. (2005) | Yusuf and Baiyewu (2012) | |
|---|---|---|---|---|---|---|
| Sample size | 11 respondents | 2 | 16 | 40 | 98 | 100 |
| Gender | Males | Females | Females—11; males—5 | Males—10; females—30 | Females—74; males—24 | Males-100 |
| Age | Ages 48–83 and a mean average of 62 years | Young women | Range of 19–58 years | The average age was 42 years | The average age was 42 years | 57.76 ± 11.10 |
| Employment status | Equal proportion (18%) are full-time, part-time unemployed without a grant (18%). Precisely 46% are unemployed but access some grants | 50% was employed; the other 50% were unemployed | 37.5% were employed; others unemployed | Not reported | Not reported | 100 |
| Socio-economic status of the caregiver | Low income | Low income | Not reported | Not reported | Low-income | Middle-income |
| Education of caregivers | Formal education (5.6%) | Formal education (100%) | Not reported | Formal education (60%) | About 7.4 years of schooling | Formal education (63%) |
| Medical training for geriatric care | Not reported | Some training | Not reported | Not reported | Some training | Not reported |
| Relationship of caregiver with the patient | The role of male children (55%) and husbands (45%) were almost of equal proportion | Paid caregiver | Unpaid relatives or children | Daughters—35%; sons—15%; sisters—40%; brother—10%; spouse—10%; other kins—35% | Sisters and daughters | Religious leaders and traditional leaders |
| The regularity of seeing the patient | Daily | Daily | Daily | Daily | Daily | Not reported |
| Number of hours of caregiving | Between 6 and 24 hours every day and an average of 13.4 hours every day | 24 hours | Not reported | Not reported | Not reported | Not reported |
| Length of caregiving years | Range of two (2) years to eleven (11) years. Average of 5.6 years |
More than ten (10) years; Less than three (3) years | Ten (10) years | Not reported | Not reported | Not reported |
| Living arrangement for caregiving | In-Residence | In-residence | In-residence | Up to 92% live in-residence with a multigenerational household structure | Living with spouse(s) and children, if dementia is mild/moderate. Severe cases are institutionalized. About 85% of dementia patients live in multigenerational households | Outside the home |
All caregivers had daily contact with the persons living with dementia, except where they were traditional leaders also serving their communities. A daily average of 13 hours was spent on caregiving, and the shortest duration of providing dementia care was two years (Hendricks-Lalla & Pretorius, 2020), while the most lasted for a 10-year period (Mushi et al., 2014). Most of the caregivers lived in the same house as the person with dementia (Baiyewu et al., 2003; Hendricks-Lalla & Pretorius, 2020; Mansi, 2014; Mushi et al., 2014; Ogunniyi et al., 2005). The live-in living arrangement occurred in multigenerational households (Baiyewu et al., 2003; Ogunniyi et al., 2005). As community-based religious/spiritual and traditional leaders, this subgroup of caregivers (Yusuf & Baiyewu, 2012) typically lived outside the household (Baiyewu et al., 2003; Ogunniyi et al., 2005).
Caregiver in context
Caregivers are at the core of providing home care to persons living with dementia, providing assisted-living, and overseeing hospital visits. In terms of supporting healthcare pathways for persons living with dementia caregivers supported both pluralistic care methods (Mushi et al., 2014), and facilitated attendance at the hospital (Yusuf & Baiyewu, 2012). Home management as an outcome of living arrangement encompasses all the available options for care. Caregivers provided services such as cooking, dressing, feeding, grooming, bathing, and facilitated healthcare visits and drug refills (Hendricks-Lalla & Pretorius, 2020; Mansi, 2014; Mushi et al., 2014). Baiyewu and colleagues observed that younger family members took up most household tasks, and persons living with dementia are not allowed to participate (Baiyewu et al., 2003). This attribute in the African household structure is a barrier to identifying cognitive and functional decline among older persons who may have dementia. The practice potentially slows down the early identification of dementia conditions.
Reviewed studies revealed that caregivers have first-hand information and observer experiences regarding dementia symptoms among persons living with dementia. The challenges of poor appetite, speech problems that affect communication, forgetfulness, getting lost, erratic night-time behavior, depression, apathy, irritability, auditory and visual hallucinations, and requiring assistance with eating were identified (Baiyewu et al., 2003; Hendricks-Lalla & Pretorius, 2020; Mushi et al., 2014; Yusuf & Baiyewu, 2012). Baiyewu and colleagues noted that cultural differences existed in terms of dementia symptoms as examples from Italy, China, and Japan have shown (Baiyewu et al., 2003). Stressors for caregivers varied and were partly dependent on caregivers’ “cultural threshold” and individual differences. Ogunniyi and others observed that the severity of dementia determined the care approach and the extent of tolerance (Ogunniyi et al., 2005). Stressors in dementia caregiving occurred due to conflicts between caregivers and persons living with dementia, usually due to communication problems, lack of support from (other) family members, embarrassing behavior in public, erratic night-time behaviors, disinhibition, anxiety, financial problems, patient feeding, and lack of appropriate information among caregivers (Baiyewu et al., 2003; Hendricks-Lalla & Pretorius, 2020; Mansi, 2014; Mushi et al., 2014; Ogunniyi et al., 2005). Caregiver support was also provided from community support groups (Hendricks-Lalla & Pretorius, 2020), and community projects, including medical treatment and caregiver training/education, which Ogunniyi and colleagues found to be an effective strategy for improving caregiving quality (Ogunniyi et al., 2005).
Potentialities of dementia caregiving in African settings
In African settings, the relational and emotional connectedness of caregivers to the persons living with dementia and well-defined roles offer opportunities for improving the quality of caregiving. The psycho-social dimensions of caregiving roles provide the basis for leveraging information and education platforms to support caregivers and improve their skills through small support groups, as demonstrated in Tanzania and Nigeria (Mushi et al., 2014; Ogunniyi et al., 2005). First, the efficacy of radio as a channel of communication was demonstrated in Egypt and Tanzania (Mansi, 2014; Mushi et al., 2014). Second, religious and traditional institutions provided the opportunity for improving caregiving through care services for older persons (Mansi, 2014), training and capacity building for intending caregivers (Mansi, 2014; Mushi et al., 2014) and counseling through religious leaders (Yusuf & Baiyewu, 2012). Third, interventions like drop-in services, modern daycare, and other informal care services were also found effective in South Africa (Hendricks-Lalla & Pretorius, 2020). Fourth, similar to the Tanzania example, in Nigeria, Ogunniyi and colleagues also demonstrated that small groups which provide training, knowledge-sharing and networking to caregivers can be effective for quality caregiving outcomes. By drawing on different scenarios, the data provided a four-pronged approach to improving caregiving services for people living with dementia in African contexts, as follows: the use of radio (among other accessible information channels), incorporating religious and traditional institutions, creating informal care service like drop-in services, and setting up small group to provide support and training to caregivers.
Discussion
In recent times, the household/family resource approach for caregiving is changing, due to changing demographics, culture, and migration. The family-based approach has evolved alternatives to institutionalized care by engaging paid or non-family personal caregivers (Mansi, 2014). Both the family and paid/personal caregiver approaches serve the purposes of reducing the cost of care and shielding older persons from the physical, social, and function-based adverse outcomes of aging and related morbidities.
Although caregivers may have first-hand information about dementia onset, their observations are not early enough. In LMICs, it takes about 56 weeks for the first symptoms of dementia to be reported to a specialist (Volpe et al., 2020). There are various reasons for delayed identification of dementia by caregivers of older persons in Africa. First, older persons are exempted for regular daily activities, hence, their functional deficiencies are easy to miss (Ineichen, 2000). Second, there is limited ability to recognize early signs of dementia due to personal (educational) caregiver and institutional (availability) gaps. In typical African settings, there is little to no formal training for the caregiving role, and care duties emanate from cultural interpretations of dementia (Mushi et al., 2014) and on perceptions and folk knowledge regarding mental health (Mansi, 2014). Third, there are cultural and individual differences in the observation, interpretation, and reportage of dementia signs across different ethnicities and nationalities. Baiyewu and colleagues (2003, 2012) noted that Yoruba caregivers observed dementia symptoms (appetite change, depression, and irritability) differently from Japanese, Taiwanese, and Italian accounts.
Caregiving stress is substantial and multidimensional (Uwakwe et al., 2009); however, there is little available literature describing variations by culture (Ineichen, 2000). The behavioral challenges of persons living with dementia affect caregivers in communication, which is a major stressor. Embarrassing behaviors, especially in public, was one of the stressors identified (Hendricks-Lalla & Pretorius, 2020; Ogunniyi et al., 2005). An average of 13 hours was required every day, and in extreme cases, it was a 24-hour role (Hendricks-Lalla & Pretorius, 2020; Mansi, 2014). There appears to be higher time-demands on live-in domestic caregivers (average 14 hours daily) compared to institutional caregivers (11–70 hours per week) (Klimova et al., 2016). In terms of time cost, caregivers in Nigeria cut down on up to 84% of their paid work to cater for a person living with dementia (Prince, 2004). The cost of dementia medication accounts for about one-fifth of the health care cost of older persons with dementia (Uwakwe et al., 2009). Alzheimer’s medications are often in low supply and financially out of reach for many families in a majority of African countries (Suh et al., 2009; Amoo et al., 2011. For example, a 5 mg tablet pack (30-day supply) of donepezil (a cholinesterase inhibitor), is still unaffordable in Nigeria. This is because a 30-day supply costs more than 1 days’ wage (approximately 1000 naira, about about $2.60 as in $2.60) (Ewen et al., 2017). At the time of this review, the minimum wage in Nigeria is 30,000 naira (approximately $79) a month. Stress tolerance levels are subject to different cultural interpretations, prescribed normative standards (Baiyewu et al., 2003), disease acceptance (Mushi et al., 2014), and social circumstances (Ihezue & Okpara, 1989). To improve the experiences of caregivers in their role, educational assistance from family members, who are especially medically knowledgeable has been found to improve the delivery of caregiving (Mansi, 2014). It has also been demonstrated that training is valuable for improving role performance and personal health outcomes of caregivers. (Ogunniyi et al., 2005). There is a deep sense of duty and enthusiasm among caregivers, which presents an opportunity for improving their impact in caregiving. Caregiving has helped these individuals to discover their competence in other functional roles. Monthly meetings with caregivers fostered knowledge sharing, networking, and improved compliance with care plans in Tanzania (Mushi et al., 2014), Nigeria (Ogunniyi et al., 2005), and South Africa (Hendricks-Lalla & Pretorius, 2020).
Caregivers have religious convictions regarding their roles and the need to reciprocate parental or familial care. These perceptions constitute underlying considerations for the low adoption of nursing homes among Africans (Mushi et al., 2014). The social organization of religion and traditional authority in African settings provides a basis for providing focused caregiving education and information to caregivers. These social organizations overlap, and are related in terms of their structure and functions. Religious and traditional institutions have great potential for advancing dementia caregiving in Africa (Musyimi et al., 2021; Mansi, 2014; Mushi et al., 2014; Yusuf & Baiyewu, 2012). They have functioned in the intersections of early detection, counseling, spirituality, social support, community mobilization of resources, and interpretation of the cause of dementia in African communities. Traditional and religious leaders’ roles and services should be explored as a platform to train caregivers and re-orient caregivers towards bio-medical approaches to caregiving. Religious and traditional leaders understand that mental health symptoms relating to dementia require medical attention beyond the spiritual basis for specific health conditions.
Study limitations
This scoping review is not an epidemiological investigation, and thus reviewed articles could not be assessed in line with the Alzheimer’s Disease international study selection and quality criteria (Prince et al., 2015). However, we adopted a conceptual and qualitative approach, described article types (conceptual or empirical), research tradition (qualitative or quantitative), and the research instrument adopted for data gathering, as basis for considering good fit for selection and review.
Also, due to methodological differences in the included studies, it was observed that articles adopting quantitative approaches accounted for a larger proportion of participant caregivers than those from qualitative studies. As a result, the sample sizes for the mainly qualitative studies (Hendricks-Lalla, Pretorius, 2020; Mansi, 2014; Mushi et al., 2014) were relatively small, because the studies were small-scale community studies. These studies were focused on exploring specific subjective social and cultural processes like gender, life history and social representation in dementia caregiving. Other studies were large-scale longitudinal studies which had engaged mixed-methods approaches. Thus, because more caregivers were engaged in the large studies, generalizations about the status of caregivers largely depended on quantitative evidence, while qualitative studies provided context. These methodological biases notwithstanding, do not detract from the validity of the assertions about the experiences and practices of dementia caregiving in the African countries that were examined.
It is observable that there were more studies conducted within Nigeria and one each in South Africa, Egypt, and Tanzania. This may result in some dimensions of bias regarding the contexts of caregiving. In the countries under our focus, it was observed that the veneration of older persons, management of cognitive impairment in such population, and the caregiving practices are similar. Hence, the review provides a valid description of social and cultural processes. The preceding engagements point to the fact that attention to research traditions and contexts are relevant to the caregiving discourse. Methodological approaches should be well-driven to capture the nuances and colorations of the social dimensions of caregiving of older persons living with dementia.
Conclusions and recommendations
Informal caregivers are valuable stakeholders in the care of older persons with dementia. However, they require access to guidance, information, and resources to help understand symptoms and adequately manage the health of persons living with dementia. Education and information should explain roles and expectations for caregivers, and should also include culturally relevant and culturally appropriate descriptions of dementia symptoms from onset, and as the disease progresses. It is also important to recognize caregiver burden in terms of adverse psychosocial outcomes and increased risk of conditions like anxiety and depression. The social organization of religion and traditional authority in African settings provide a basis for support, education, and dementia caregiving information.
Acknowledgements
Research reported in this publication was supported by the Fogarty International Center and the National Institute on Aging (NIA) of the National Institutes of Health under Award Number D43 TW010543. The development of this manuscript was supported by the Central and West Africa Implementation Science Alliance (CAWISA), with funding from the Fogarty International Center The content is solely the responsibility of the authors and does not necessarily represent the official views of the US National Institutes of Health.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The Fogarty International Center and the National Institute of Aging of the US National Institutes of Health.
Biographies
Isaac A Adedeji, PhD, is a lecturer in Medical Sociology/Anthropology and Bioethics at Olabisi Onabanjo University, Nigeria. He is a member of the Nigeria Implementation Science Alliance (NISA), and a Scholar of the Central and West Africa Implementation Science Alliance (CAWISA). Dr. Adedeji is a 2021-2022 Fogarty Global Health Fellow of the Harvard University, Boston University, Northwestern University, and University of New Mexico (HBNU) Global Health Fellows Consortium. He has research interest in the cultural understanding of mental health—including dementia caregiving. Dr. Adedeji is also focused on expanding the application of Social Science methodologies in implementation research conducted in African countries.
Adesola Ogunniyi, MBBS, is a clinician, neurologist and neuroepidemiologist at the College of Medicine, University of Ibadan, Nigeria. One of Prof. Ogunniyi’s major research areas is in the burden and determinants of neurological disorders from cross-cultural, community perspectives. He has been a leader in cross-cultural studies of dementia, including studies among African-Americans and Yoruba Africans aged 65 years and above.
David C Henderson, MD, currently serves as Psychiatrist-in-Chief, Division of Psychiatry, at Boston Medical Center and Professor and Chair, Department of Psychiatry, at Boston University School of Medicine. Prof. Henderson’s body of work includes mental health policy development and strategic planning, and mental health capacity building programs for both specialized and primary health professionals in multiple countries.
Nadia A Sam-Agudu, MD, CTropMed is an Associate Professor of Pediatrics at the University of Maryland School of Medicine, and a Senior Technical Advisor and Research Faculty at the Institute of Human Virology Nigeria. She is a clinician-scientist specializing in pediatric infectious diseases and implementation research. Dr. Sam-Agudu is a NISA member, and serves as the lead for CAWISA, where she and other scientists provide mentorship to early career investigator-scholars across West and Central Africa.
Footnotes
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
This is a review article based on publicly available published data, thus no ethical approval was sought, as no primary data were collected.
Contributor Information
Isaac A Adedeji, Department of Sociology, Olabisi Onabanjo University, Ago-Iwoye, Nigeria.
Adesola Ogunniyi, Department of Medicine, University College Hospital, Ibadan, Nigeria.
David C Henderson, Department of Psychiatry, Boston University School of Medicine, USA.
Nadia A Sam-Agudu, International Research Center of Excellence, Institute of Human Virology, Nigeria, Abuja, Nigeria; Department of Paediatrics and Child Health, University of Cape Coast School of Medical Sciences, Cape Coast, Ghana; Division of Epidemiology and Prevention, Institute of Human Virology, University of Maryland School of Medicine, Baltimore, USA.
References
- Amoo G, Akinyemi RO, Onofa LU, Akinyemi JO, Baiyewu O, Ogunlesi AO, & Ogunniyi A (2011). Profile of clinically-diagnosed dementias in a neuropsychiatric practice in Abeokuta, south-western Nigeria. African Journal of Psychiatry, 14(5), 377–382. 10.4314/ajpsy.v14i5.5 [DOI] [PubMed] [Google Scholar]
- Baiyewu O, Smith-Gamble V, Akinbiyi A, Lane KA, Hall KS, Ogunniyi A, & Hendrie HC (2003). Behavioral and caregiver reaction of dementia as measured by the neuropsychiatric inventory in Nigerian community residents. International Psychogeriatrics, 15(4), 399–409. 10.1017/s1041610203009645 [DOI] [PubMed] [Google Scholar]
- Brown S (2016). Global Aging. In Morgan LA & Kunkel SR (Eds.), Aging, Society, and the life course (Fifth ed., pp. 271–298). Springer Publishing Company. [Google Scholar]
- Clarke C, Keyes S, Wilkinson H, & Alexjuk J (2013). Healthbridge: The national evaluation of peer support networks and dementia advisers in implementation of the national dementia strategy for England. Department of Health. [Google Scholar]
- de Freitas MC, Queiroz TA, & de Sousa JA (2010). [The meaning of old age and the aging experience of in the elderly]. Revista da Escola de Enfermagem da USP, 44(2), 407–412. 10.1590/s0080-62342010000200024 [DOI] [PubMed] [Google Scholar]
- Evans A, Nistrup A, Henderson H, Allen-Collinson J, & Siriwardena N (2018). Reflexivity in qualitative research: Two figurational studies. https://methods.sagepub.com/case/reflexivity-in-qualitative-research-two-figurational-studies
- Ewen M, Zweekhorst M, Regeer B, & Laing R (2017). Baseline assessment of WHO’s target for both availability and affordability of essential medicines to treat non-communicable diseases. Plos One, 12(2), e0171284. 10.1371/journal.pone.0171284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fayehun OA, & Salami KK (2014). Older persons and malaria treatment in Nigeria. African Population Studies, 27(2), 424–433. 10.11564/27-2-486 [DOI] [Google Scholar]
- Gureje O, Abdulmalik J, Kola L, Musa E, Yasamy MT, & Adebayo K (2015). Integrating mental health into primary care in Nigeria: Report of a demonstration project using the mental health gap action programme intervention guide. BMC Health Services Research, 15, 242. 10.1186/s12913-015-0911-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks-Lalla A, & Pretorius C (2020). The male familial caregiver experience of caring for persons with Alzheimer’s disease from low socio-economic status: A South African perspective. Dementia, 19(3), 618–639. 10.1177/1471301218781372 [DOI] [PubMed] [Google Scholar]
- Ihezue UH, & Okpara E (1989). Psychiatric disorders of old age in enugu, Nigeria. Sociodemographic and clinical characteristics. Acta Psychiatrica Scandinavica, 79(4), 332–337. 10.1111/j.1600-0447.1989.tb10267.x. [DOI] [PubMed] [Google Scholar]
- Ineichen B (2000). The epidemiology of dementia in Africa: A review. Social Science & Medicine, 50(11), 1673–1677. 10.1016/S0277-9536(99)00392-5 [DOI] [PubMed] [Google Scholar]
- Irwin K, Sexton C, Daniel T, Lawlor B, & Naci L (2018). Healthy aging and Dementia: Two roads diverging in midlife? Frontiers in Aging Neuroscience, 10, 275. 10.3389/fnagi.2018.00275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klimova B, Maresova P, & Kuca K (2016). Non-pharmacological approaches to the prevention and treatment of Alzheimer’s disease with respect to the rising treatment costs. Current Alzheimer Research, 13(11), 1249–1258. 10.2174/1567205013666151116142302. [DOI] [PubMed] [Google Scholar]
- Korczyn AD (2002). Mixed dementia-the most common cause of dementia. Annals of the New Year Academy of Sciences, 977, 129–134. 10.1111/j.1749-6632.2002.tb04807.x [DOI] [PubMed] [Google Scholar]
- Langman N (2016). Caregivers of dementia patients mental health screening & support. Clinician Reviews, 26(6), 42–49. https://cdn.mdedge.com/files/s3fs-public/issues/articles/content_73ded0cb4dc46c62fd_042_0616CR%20CE.PDF [Google Scholar]
- Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Baneijee S, Brayne C, Burns A, Cohen-Mansfield J, Cooper C, Costafreda SG, Dias A, Fox N, Gitlin LN, Howard R, Kales HC, Kivimäki M, Larson EB, Ogunniyi A, … Mukadam N. (2020). Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet, 396(10248), 413–446. 10.1016/S0140-6736(20)30367-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LoGiudice D, & Watson R. (2014). Dementia in older people: An update. Internal Medicine Journal, 44(11), 1066–1073. 10.1111/imj.12572 [DOI] [PubMed] [Google Scholar]
- Lopez-Hartmann M, Wens J, Verhoeven V, & Remmen R (2012). The effect of caregiver support interventions for informal caregivers of community-dwelling frail elderly: A systematic review. International Journal of Integrated Care, 12, e133. 10.5334/ijic.845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansi IA (2014). Between two worlds. Patient Education and Counseling, 94(3), 442–443. 10.1016/j.pec.2013.10.011 [DOI] [PubMed] [Google Scholar]
- Manuel DG, Garner R, Finés P, Bancej C, Flanagan W, Tu K, & Bernier J (2016). Alzheimer’s and other dementias in Canada, 2011 to 2031: A microsimulation population health modeling (POHEM) study of projected prevalence, health burden, health services, and caregiving use. Population Health Metrics, 14(1), 37. 10.1186/s12963-016-0107-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills AJ, Durepos G, & Wiebe E (2010). Encyclopedia of case study research. SAGE. [Google Scholar]
- Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, & Aromataris E (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18(1), 143. 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mushi D, Rongai A, Paddick SM, Dotchin C, Mtuya C, & Walker R (2014). Social representation and practices related to dementia in Hai District of Tanzania. BMC Public Health, 14, 260. 10.1186/1471-2458-14-260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musyimi CW, Ndetei DM, Evans-Lacko S, Oliveira D, Mutunga E, & Farina N (2021). Perceptions and experiences of dementia and its care in rural Kenya. Dementia. 10.1177/14713012211014800 [DOI] [PubMed] [Google Scholar]
- Ogunniyi A, Hall KS, Baiyewu O, Gureje O, Unverzagt FW, Gao S, & Hendrie HC (2005). Caring for individuals with dementia: The Nigerian experience. West African Journal of Medicine, 24(3), 259–262. 10.4314/wajm.v24i3.28211 [DOI] [PubMed] [Google Scholar]
- Omobowale AO (2014). An ethnographic textual analysis of aging and the elders in South Western Nigeria. The Canadian Journal of Sociology/Cahiers Canadiens de Sociologie, 39(2), 211–230. [Google Scholar]
- Osundina AF, Akanni OO, Olotu SO, & Agbonile IO (2016). Patterns of psychiatric illnesses among elderly patients receiving treatment in a neuropsychiatric hospital in Nigeria. Nigerian Journal of Psychiatry, 14(1). https://www.ajol.info/index.php/njpsyc/article/view/148506 [Google Scholar]
- Peipert JD, Jennings LA, Hays RD, Wenger NS, Keeler E, & Reuben DB (2018). A Composite measure of caregiver burden in dementia: The dementia burden scale-caregiver. Journal of the American Geriatrics Society, 66(9), 1785–1789. 10.1111/jgs.15502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince MJ (2004). Care arrangements for people with dementia in developing countries. International Journal of Geriatric Psychiatry, 19(2), 170–177. 10.1002/gps.1046 [DOI] [PubMed] [Google Scholar]
- Prince MJ, Wimo A, Guerchet MM, Ali GC, Wu Y-T, & Prina M (2015). World alzheimer report 2015-the global impact of dementia. Alzheimer’s Disease International. [Google Scholar]
- Suh GH, Wimo A, Gauthier S, O’Connor D, Ikeda M, Homma A, Dominguez J, & Yang BM (2009). Mental health economics task force of the international psychogeriatric association international price comparisons of Alzheimer’s drugs: A way to close the affordability gap. International Psychogeriatrics, 21(6), 1116–1126. 10.1017/S104161020999086X. [DOI] [PubMed] [Google Scholar]
- Tanyi PL, André P, & Mbah P (2018). Care of the elderly in Nigeria: Implications for policy. Cogent Social Sciences, 4(1), 1555201. 10.1080/23311886.2018.1555201 [DOI] [Google Scholar]
- Uwakwe R, Ibeh CC, Modebe AI, Bo E, Ezeama N, Njelita I, & Prince MJ (2009). The epidemiology of dependence in older people in Nigeria: Prevalence, determinants, informal care, and health service utilization. A 10/66 dementia research group cross-sectional survey. Journal of the American Geriatrics Society, 57(9), 1620–1627. 10.1111/j.1532-5415.2009.02397.x [DOI] [PubMed] [Google Scholar]
- Uwakwe R, & Prince M (2004). Identifying dementia and depression in the elderly: The role of the family. Nigerian journal of clinical practice. Nigerian Journal of Clinical Practice, 7(2), 82–87. [Google Scholar]
- Volpe U, Amin H, Ayinde OO, Burns A, Chan WC, David R, Dejanovic SD, Djokic G, Eraslan D, Fischer GAL, Gracia-Garcéa P, Hamdani SU, Han C, Jafri H, Kallivayalil RA, Kriekaart RL, Kua EH, Lam LCW, Lecic-Tosevski D,… & Sartorius N (2020). Pathways to care for people with dementia: An international multicentre study. International Journal of Geriatrics Psychiatry, 35(2), 163–173. 10.1002/gps.5223 [DOI] [PubMed] [Google Scholar]
- World Health Organization (2011). Global health and aging. https://www.who.int/ageing/publications/globalhealth.pdf?ua.
- Yusuf AJ, & Baiyewu O (2012). Beliefs and attitudes towards dementia among community leaders in northern Nigeria. West African Journal of Medicine, 31(1), 8–13. [PubMed] [Google Scholar]
- Zissimopoulos JM, Tysinger BC, St Clair PA, & Crimmins EM (2018). The impact of changes in population health and mortality on future prevalence of Alzheimer’s disease and other dementias in the United States. Journal of Gerontology Series B: Psychological Sciences and Social Sciences, 73(suppl_1), S38–S47. 10.1093/geronb/gbx147 [DOI] [PMC free article] [PubMed] [Google Scholar]


