Abstract
Objectives
This systematic review and meta-analysis evaluates the safety and efficacy of dual antiplatelet therapy (DAPT) in elderly patients with acute coronary syndrome (ACS).
Background
The safety and efficacy of DAPT in elderly patients with ACS is not well characterized.
Methods
We performed a systematic literature review to identify clinical studies that reported safety and efficacy outcomes after DAPT for ACS in elderly patients. The primary outcomes of primary efficacy endpoint rates and bleeding event rates were reported as random effects risk ratio (RR) with 95% confidence interval. No prior ethical approval was required since all data are public.
Results
Our search yielded 660 potential studies. We included 8 studies reporting on 29,217 patients. There was a higher risk of bleeding event rates in elderly patients treated with prasugrel or ticagrelor when compared to clopidogrel with a risk ratio of 1.17 (95% CI 1.08 to 1.27, p < 0.05). There was no difference in primary efficacy endpoint rates between elderly patients treated with prasugrel or ticagrelor when compared to clopidogrel with a risk ratio of 0.85 (95% CI 0.68 to 1.07, p=0.17).
Conclusions
This systematic review and meta-analysis suggests that DAPT with prasugrel or ticagrelor compared to clopidogrel is associated with a higher risk of bleeding events in elderly patients with ACS. There was no difference in the primary efficacy endpoints between the two treatment groups.
1. Introduction
Dual oral antiplatelet therapy (DAPT) with aspirin and P2Y12 receptor inhibitors has had a key role in the management of patients with acute coronary syndrome (ACS) and remains the treatment of choice to prevent in-stent thrombosis [1]. In patients with ACS undergoing percutaneous coronary intervention (PCI), a loading dose of DAPT (either aspirin + clopidogrel or aspirin + ticagrelor) is recommended as early as possible by the latest ESC guidelines [2]. Although current guidelines recommend the new and more predictable P2Y12 receptor inhibitors ticagrelor and prasugrel in ACS patients given their superiority to clopidogrel in preventing major adverse cardiovascular events (MACE), they have been associated with higher risk of bleeding especially in elderly patients [3].
Elderly patients contribute to a large proportion of patients with ACS and have often been underrepresented in the randomized trials that provided evidence for guidelines [4]. For example, in the TRITON TIMI 38 (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel-Thrombolysis in Myocardial Infarction 38) and PLATO (Platelet Inhibition and Patient Outcomes) trials, elderly patients (age >75 years) accounted for only 13% and 15% of the study populations, respectively [5, 6]. Elderly patients are more susceptible to the adverse effects of DAPT with bleeding being one of the most common complications associated with prolonged hospitalization and increased mortality. However, investigations about the safety and efficacy of DAPT in this group are scarce [7].
In this meta-analysis and systematic review, we evaluate the impact of DAPT on clinical and bleeding outcomes in elderly patients with ACS.
2. Methods
The main objective of this review was to assess the safety and efficacy of ticagrelor or prasugrel compared to clopidogrel in elderly patients with ACS. We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement extension for network meta-analysis. The PRISMA flow diagram was used to depict the four phases of the review including identification, screening, eligibility, and inclusion. The PRISMA statement contains a checklist of items required of systematic reviews and meta-analyses. The review was not registered a priori. No ethical approval was required since this meta-analysis uses only public published data.
2.1. Search Strategy
We performed a systematic literature review to identify randomized and non-randomized clinical studies that reported the use of DAPT in elderly patients with ACS. Searches were limited to peer-reviewed primary research articles published in English up to December 1st, 2021. This research involved human subjects and described the clinical impact of DAPT in elderly patients with ACS. We developed the search strategy according to available guidance from the Cochrane Collaboration.
The search strategy in PubMed explored Medical Subject Heading (MeSH) terms related to elderly patients with ACS treated with DAPT. The articles found to be relevant during the search were stored in EndNote. Selected articles underwent full evaluation to assess their potential inclusion in the systematic review.
2.2. Study Selection
Articles were selected for inclusion based on predefined criteria, which included age, sex, DAPT, bleeding, MACE events, and the primary or secondary outcomes being mortality, bleeding, and efficacy outcomes. Exclusion criteria were patients with elective PCI without ACS. We excluded case reports and studies with fewer than 10 subjects.
Two authors (GS and SL) independently read the trials and screened the abstracts to choose potentially relevant articles. Selected articles underwent full evaluation to assess their potential inclusion in the systematic review.
2.3. Definition of Elderly Patients
Each study defined elderly patients based on an arbitrary age. An age greater than 75 years old was defined as elderly in 5 of the included studies. Ages greater than 65, 70, and 80 were each used as cutoffs by 3 of the included studies.
2.4. Definition of Outcomes
Primary efficacy outcomes were defined separately by each included study. Most studies used a composite of death, myocardial infarction, or stroke during the follow-up period.
Bleeding events were defined separately by each included study. Most studies used TIMI major or minor bleeding or PLATO major or minor bleeding, as previously defined [8, 9].
2.5. Risk of Bias
The risk of bias was assessed using the Cochrane tool for assessing the risk of bias in randomized controlled trials (RCTs) [10]. The risk of bias was assessed by two independent reviewers (GS and SL).
2.6. Statistical Analysis
Data were analyzed using Review Manager Software 5.4. We used fixed effects to assess the combined risk estimates according to I2 statistics. Analysis to determine sensitivity and publication bias was detected by funnel plots. p < 0.05 was considered statistically significant.
3. Results
3.1. Literature Search
Our search yielded 660 potential studies. We excluded 626 studies at the abstract level and selected 34 full-text articles for detailed assessment; 8 studies were ultimately included in our systematic review and meta-analysis. Figure 1 describes the flowchart of included studies.
Figure 1.
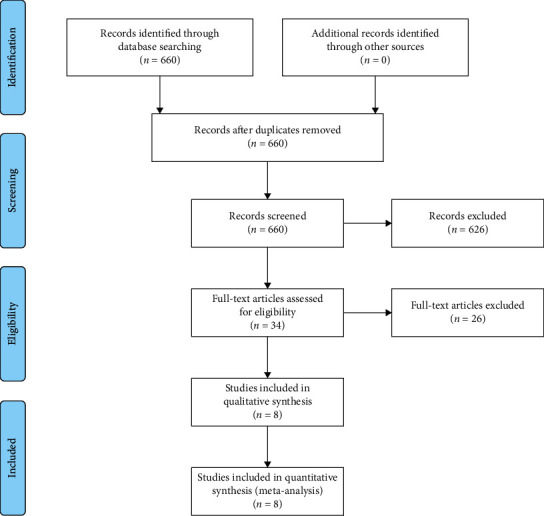
Flowchart of the included studies.
3.2. Baseline Characteristics of the Studies
Table 1 shows the baseline characteristics of the included studies. All studies were published between 2007 and 2020. The 8 studies reported on 29,217 patients. Several of the included studies did not provide demographic data stratified by age, so the comparison of baseline characteristics in our target population of elderly patients is limited.
Table 1.
Baseline characteristics of the included studies.
| Study Author Year | Trial | Sample size | Group | Gropu size | Mean/Median,Age,Years | Female | White race% | BMI,Kg/m2 | Diabetesmellitus,% | Hypertension | Currentsmoker | PriorPCI,% | PriorCABG,% | Type ofACs,STEMI,% | Type of ACs, NSTEMI,% |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wiviott et al, 2007 | TRITON-TIMI 38 | 13,608 | Prasugrel | 6813 | 61 (53–69) | 25 | 92 | 28 (25–31) | 23.0 | 64.0 | NR | NR | 8.0 | 26.0 | 74.0 |
| clopidogrel | 6795 | 61 (53–70) | 27 | 93 | 28 (25–31) | 23.0 | 64.0 | NR | NR | 7.0 | 26.0 | 74.0 | |||
|
| |||||||||||||||
| Wallentin et al.,2009 | PLATO | 18,624 | Ticagrelor | 9333 | 62.0 | 28.4 | 91.8 | 27 (13–62) | 24.9 | 65.8 | 36.0 | 13.6 | 5.7 | 35.7 | 42.9 |
| clopidogrel | 9292 | 62.0 | 28.3 | 91.1 | 27 (13–70) | 25.1 | 65.1 | 35.7 | 13.1 | 6.2 | 35.8 | 42.5 | |||
|
| |||||||||||||||
| Roe et al.,2013 | TRILOGY ACS | 9,326 | Prasugrel (Age > 75) | 1043 | 80.0 (77.0–83.0) | 49.9 | NR | NR | 34.9 | 87.5 | 7.4 | 20.7 | 17.3 | NR | 79.5 |
| Clopidogrel (Age > 75) | 1040 | 79.0 (77.0–83.0) | 51.1 | NR | NR | 35.1 | 87.4 | 8.2 | 18.4 | 15.4 | NR | 77.3 | |||
|
| |||||||||||||||
| Wang et al, 2016 | 200 | Ticagrelor | 100 | 79 (76–85) | 31 | NR | NR | 42 | 79 | 37 | 3 | 0 | 37 | 44 | |
| clopidogrel | 100 | 80 (74–86) | 34 | NR | NR | 39 | 82 | 41 | 65 | 0 | 32 | 47 | |||
|
| |||||||||||||||
| Savonitto et al.,2018 | ELDERLY ACS II | 1443 | Prasugrel | 713 | 80 (77–84) | 41.0 | NR | 26 (24–28) | 30.0 | 78.0 | 9.0 | 20.0 | 8.0 | 42.0 | 48.0 |
| clopidogrel | 730 | 80 (77–84) | 39.0 | NR | 26 (24–28) | 28.0 | 78.0 | 9.0 | 16.0 | 10.0 | 41.0 | 47.0 | |||
|
| |||||||||||||||
| Schmucker et al.,2019 | BREMEN-STEMI | 1087 | Ticagrelor | 535 | 80.9 ± 4.7 | 49.9 | NR | 26.1 ± 4.1 | 20.6 | NR | 9.6 | 11.7 | 3.2 | 67.5 | NR |
| clopidogrel | 552 | 80.9 ± 4.6 | 51.1 | NR | 25.9 ± 4.7 | 24.1 | NR | 14.3 | 10.2 | 2.9 | 60.2 | NR | |||
|
| |||||||||||||||
| Szummer et al.,2020 | SWEDEHEART | 14,005 | Ticagrelor (After IPTW) | 5,607 | 85.0 ± 3.9 | 51.8 | NR | NR | 22.2 | 69.1 | 5.6 | 13.3 | 9.0 | 30.9 | NR |
| Clopidogrel (After IPTW) | 8,421 | 84.0 ± 3.9 | 51.6 | NR | NR | 22.4 | 68.6 | 5.6 | 13.3 | 9.0 | 31.4 | NR | |||
|
| |||||||||||||||
| Gimbel et al.,2020 | POPular AGE | 1002 | Ticagrelor or prasugrel | 502 | 77 (73–82) | 35 | NR | 26.9 ± 4.2 | 30 | 73 | 13 | 24 | 17 | NR | 86 |
| clopidogrel | 500 | 77 (73–81) | 37 | NR | 26.7 ± 4.0 | 29 | 73 | 14 | 20 | 17 | NR | 86 | |||
Data are median (IQR), mean ± standard deviation, or percentages as indicated. BMI = body mass index, PCI = percutaneous coronary intervention, CABG = coronary artery bypass graft, ACS = acute coronary syndrome, STEMI = ST elevation myocardial infarction, NSTEMI = non-ST elevation myocardial infarction, and IPTW = Inverse Probability Treatment Weighting.
3.3. Risk of Bias
The risk of bias revealed adequate randomization, allocation concealment, and blinding in the 6 RCTs included in this study. The 2 non-RCTs included in this study were registry analyses that had appropriate selection and ascertainment approaches, while confounding adjustments were limited due to the observational design. Overall, the risk of bias for clinical outcomes was low in the RCTs and high in the non-RCTs.
3.4. Primary Efficacy Outcomes and Bleeding Events in Elderly Patients with CAD
Meta-analysis of the included studies revealed a higher risk of bleeding event rates in elderly patients treated with prasugrel or ticagrelor when compared to clopidogrel with a risk ratio of 1.17 (95% CI 1.08 to 1.27, p < 0.05). The forest plot for this comparison is shown in Figure 2. There was no difference in primary efficacy endpoint rates between elderly patients treated with prasugrel or ticagrelor when compared to clopidogrel with a risk ratio of 0.85 (95% CI 0.68 to 1.07, p=0.17). The forest plot for this comparison is shown in Figure 3. Meta-analysis with the non-RCT excluded revealed similar results as shown in Figures 4 and 5. The statistical heterogeneity for bleeding events was low with an I2 value of 0%. The statistical heterogeneity for primary efficacy endpoints was high with an I2 value of 94%.
Figure 2.
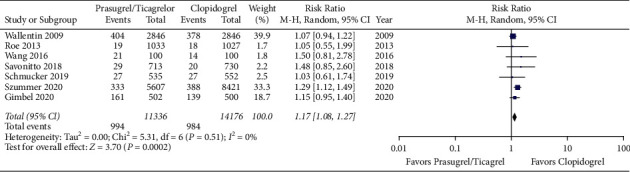
Forest plot of bleeding event rates for prasugrel or ticagrelor versus clopidogrel in elderly patients with acute coronary syndrome (CI = confidence interval).
Figure 3.
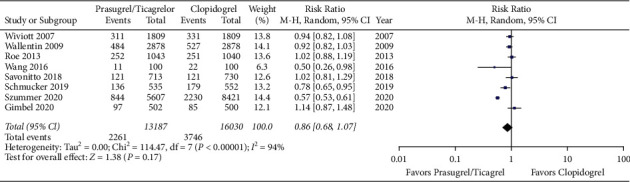
Forest plot of primary efficacy endpoint rates for prasugrel or ticagrelor versus clopidogrel in elderly patients with acute coronary syndrome (CI = confidence interval).
Figure 4.
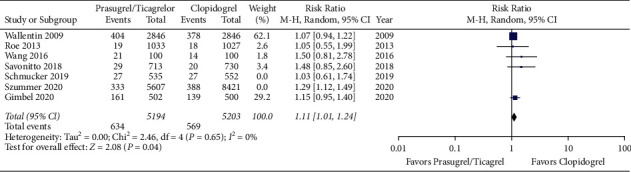
Forest plot of bleeding event rates for prasugrel or ticagrelor versus clopidogrel in elderly patients with acute coronary syndrome. The 2 non-randomized clinical trials by Schmucker et al. and Szummer et al. are excluded (CI = confidence interval).
Figure 5.
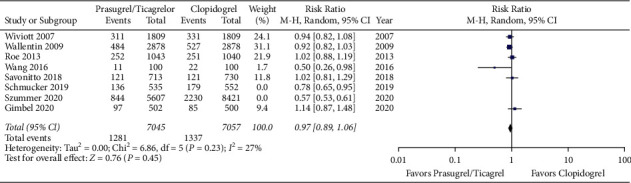
Forest plot of bleeding event rates for prasugrel or ticagrelor versus clopidogrel in elderly patients with acute coronary syndrome. The 2 non-randomized clinical trials by Schmucker et al. and Szummer et al. are excluded (CI = confidence interval).
4. Discussion
This systematic review and meta-analysis suggests that DAPT with prasugrel or ticagrelor compared to clopidogrel is associated with a higher risk of bleeding events in elderly patients with ACS. Our findings are derived from 8 studies reporting clinical outcomes in 29,217 patients [5, 9, 11–16]. There was no difference in the primary efficacy endpoints in DAPT with prasugrel or ticagrelor compared to clopidogrel in this patient population.
These findings provide a better understanding of the overall safety of DAPT in elderly patients assessed in various clinical trials. The CURE (Clopidogrel in Unstable Angina to Prevent Recurrent Events) trial demonstrated that clopidogrel was more effective than placebo in patients with ACS at the cost of increased risk of major bleeding regardless of age [17]. The benefit of prasugrel therapy compared to the risk of bleeding in elderly patients with ACS was shown to have a neutral net clinical benefit in the TRITON-TIMI 38 (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel-Thrombolysis in Myocardial Infarction 38) trial [5]. Low-dose prasugrel and clopidogrel were shown to have similar efficacy and bleeding outcomes in elderly patients in the TRILOGY ACS (Targeted Platelet Inhibition to Clarify the Optimal Strategy to Medically Manage Acute Coronary Syndromes) study [11]. In the ELDERLY ACS II (Elderly Acute Coronary Syndrome 2) trial, low-dose prasugrel and clopidogrel showed similar primary endpoints in elderly patients with ACS [13]. In a substudy of elderly patients in the PLATO (Platelet Inhibition and Patient Outcomes) trial, there was no significant difference in major bleeding events between patients treated with ticagrelor versus clopidogrel [6]. In a more recent analysis, clopidogrel was shown to have decreased bleeding events with similar efficacy rates when compared to ticagrelor in elderly patients with ACS in the POPular AGE (Ticagrelor or Prasugrel Versus Clopidogrel in Elderly Patients With an Acute Coronary Syndrome and a High Bleeding Risk: Optimization of Antiplatelet Treatment in High-Risk Elderly) trial [16]. Ticagrelor was shown to decrease major ischemic events without increasing bleeding events in elderly patient with STEMI in the Bremen STEMI registry [14]. However, in the SWEDEHEART (Swedish Web System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies) trial, ticagrelor was associated with a higher risk of bleeding and death when compared to clopidogrel in elderly patients with MI [15].
Additional studies have evaluated DAPT in elderly patients for extended periods of time over 1 year after the index event. DAPT extended for 30 months versus aspirin only was associated with decreased ischemic events and stent thrombosis at the expense of increased bleeding events in the DAPT (Dual Antiplatelet Therapy) trial. However, the benefit of prolonged DAPT was decreased and the bleeding event rates increased when stratified by age [18]. In the PEGASUS-TIMI 54 (Prevention of Cardiovascular Events in Patients With Prior Heart Attack Using Ticagrelor Compared to Placebo on a Background of Aspirin-Thrombolysis In Myocardial Infarction 54) trial, ticagrelor and aspirin were shown to have a benefit on the 3-year primary ischemic outcome at the expense of a 150% increase in bleeding events in elderly patients 1 to 3 years after a prior MI [19]. The use of ticagrelor and aspirin in patients with diabetes mellitus and stable CAD was shown to have a modest benefit on the primary ischemic outcome at the expense of increased bleeding rates in the THEMIS (The Effect of Ticagrelor on Health Outcomes in Diabetes Mellitus Patients Intervention Study) trial. This benefit was not significant when stratified by elderly patients over 75 years of age [20]. An analysis of the RENAMI (REgistry of New Antiplatelets in patients with Myocardial Infarction) registry showed reduced fatal and non-fatal ischemic events by extending DAPT with prasugrel or ticagrelor beyond 12 months. However, this benefit was reduced in patients older than 75 years due to an increased risk of bleeding [21].
This systematic review and meta-analysis provides important insights on DAPT for elderly patients with ACS that may inform decisions in clinical practice. Elderly patients with ACS have an increased risk for bleeding events that can offset the ischemic benefit of DAPT. A risk assessment should be completed before initiating DAPT and new guideline recommendations indicate that bleeding risk should be the priority for informing decision making [22]. Individual risk assessments that account for quantitative and qualitative metrics are required since the causes of bleeding are variable and multifactorial within the elderly population [23]. The PRECISE-DAPT and PARIS risk scores have shown modest accuracy in predicting bleeding risk in elderly patients [24]. As drug-eluting stents continue to improve, the use of a shorter duration of DAPT offers a potential bleeding risk mitigation strategy for elderly patients [25, 26]. P2Y12 monotherapy versus DAPT is another potential strategy to reduce bleeding events in elderly patients with CAD currently being investigated [27, 28]. Genotype-guided P2Y12 inhibitor selection is another area of research that may provide clinical benefits to elderly patients [29].
The limitations of this systematic review and meta-analysis are influenced by the limitations of the included studies. All of the included studies are likely influenced by between-center variability and the lack of centralized independent assessment of procedural results and outcomes. Antiplatelet therapy regimens and follow-up time also differ in each study and limit the generalizability of the aggregate data. The statistical heterogeneity of the meta-analysis varied by outcome likely due to clinical and methodological diversity between studies.
5. Conclusion
This systematic review and meta-analysis suggests that DAPT with prasugrel or ticagrelor compared to clopidogrel is associated with a higher risk of bleeding events in elderly patients with acute coronary syndrome. There was no difference in the primary efficacy endpoints between the two treatment groups.
Data Availability
The data used are included within the article.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Levine G. N., Bates E. R., Bittl J. A., et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American college of cardiology/American Heart association task force on clinical practice guidelines: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention, 2011 ACCF/AHA guideline for coronary artery bypass graft surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic Heart disease, 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction, 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes, and 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery. Circulation . 2016;134(10):e123–55. doi: 10.1161/CIR.0000000000000404. [DOI] [PubMed] [Google Scholar]
- 2.Ibanez B., James S., Agewall S., et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) European Heart Journal . 2018;39(2):119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 3.Vranckx P., Valgimigli M., Jüni P., et al. Ticagrelor plus aspirin for 1 month, followed by ticagrelor monotherapy for 23 months vs. aspirin plus clopidogrel or ticagrelor for 12 months, followed by aspirin monotherapy for 12 months after implantation of a drug-eluting stent: a multicentre, open-label, randomised superiority trial. The Lancet . 2018;392(10151):940–949. doi: 10.1016/s0140-6736(18)31858-0. [DOI] [PubMed] [Google Scholar]
- 4.Urban P., Mehran R., Colleran R., et al. Defining high bleeding risk in patients undergoing percutaneous coronary intervention: a consensus document from the Academic Research Consortium for High Bleeding Risk. European Heart Journal . 2019;40(31):2632–2653. doi: 10.1093/eurheartj/ehz372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wiviott S. D., Braunwald E., McCabe C. H., et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. New England Journal of Medicine . 2007;357(20):2001–2015. doi: 10.1056/nejmoa0706482. [DOI] [PubMed] [Google Scholar]
- 6.Husted S., James S., Becker R. C., et al. Ticagrelor versus clopidogrel in elderly patients with acute coronary syndromes: a substudy from the prospective randomized PLATelet inhibition and patient Outcomes (PLATO) trial. Circulation: Cardiovascular Quality and Outcomes . 2012;5:680–688. doi: 10.1161/circoutcomes.111.964395. [DOI] [PubMed] [Google Scholar]
- 7.Alexander K. P., Newby L. K., Armstrong P. W., et al. Acute coronary care in the elderly, part II: ST-segment-elevation myocardial infarction: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation . 2007;115(19):2570–2589. doi: 10.1161/circulationaha.107.182616. [DOI] [PubMed] [Google Scholar]
- 8.Wiviott S. D., Antman E. M., Gibson C. M., et al. Evaluation of prasugrel compared with clopidogrel in patients with acute coronary syndromes: design and rationale for the TRial to assess Improvement in Therapeutic Outcomes by optimizing platelet InhibitioN with prasugrel Thrombolysis in Myocardial Infarction 38 (TRITON-TIMI 38) American Heart Journal . 2006;152(4):627–635. doi: 10.1016/j.ahj.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 9.Wallentin L., Becker R. C., Budaj A., et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. New England Journal of Medicine . 2009;361(11):1045–1057. doi: 10.1056/nejmoa0904327. [DOI] [PubMed] [Google Scholar]
- 10.Higgins J. P. T., Altman D. G., Gøtzsche P. C., et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ . 2011;343 doi: 10.1136/bmj.d5928.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roe M. T., Goodman S. G., Ohman E. M., et al. Elderly patients with acute coronary syndromes managed without revascularization: insights into the safety of long-term dual antiplatelet therapy with reduced-dose prasugrel versus standard-dose clopidogrel. Circulation . 2013;128(8):823–833. doi: 10.1161/circulationaha.113.002303. [DOI] [PubMed] [Google Scholar]
- 12.Wang H., Wang X. Efficacy and safety outcomes of ticagrelor compared with clopidogrel in Chinese elderly patients with acute coronary syndrome. Therapeutics and Clinical Risk Management . 2016;12:1101–1105. doi: 10.2147/tcrm.s108965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Savonitto S., Ferri L. A., Piatti L., et al. Comparison of reduced-dose prasugrel and standard-dose clopidogrel in elderly patients with acute coronary syndromes undergoing early percutaneous revascularization. Circulation . 2018;137(23):2435–2445. doi: 10.1161/circulationaha.117.032180. [DOI] [PubMed] [Google Scholar]
- 14.Schmucker J., Fach A., Mata Marin L. A., et al. Efficacy and safety of ticagrelor in comparison to clopidogrel in elderly patients with ST-segment-elevation myocardial infarctions. Journal of American Heart Association . 2019;8(18) doi: 10.1161/jaha.119.012530.e012530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Szummer K., Montez-Rath M. E., Alfredsson J., et al. Comparison between ticagrelor and clopidogrel in elderly patients with an acute coronary syndrome: insights from the SWEDEHEART registry. Circulation . 2020;142(18):1700–1708. doi: 10.1161/circulationaha.120.050645. [DOI] [PubMed] [Google Scholar]
- 16.Gimbel M., Qaderdan K., Willemsen L., et al. Clopidogrel versus ticagrelor or prasugrel in patients aged 70 years or older with non-ST-elevation acute coronary syndrome (POPular AGE): the randomised, open-label, non-inferiority trial. The Lancet . 2020;395(10233):1374–1381. doi: 10.1016/s0140-6736(20)30325-1. [DOI] [PubMed] [Google Scholar]
- 17.Yusuf S., Zhao F., Mehta S. R., et al. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. New England Journal of Medicine . 2001;345(7):494–502. doi: 10.1056/NEJMoa010746. [DOI] [PubMed] [Google Scholar]
- 18.Mauri L., Kereiakes D. J., Yeh R. W., et al. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. New England Journal of Medicine . 2014;371(23):2155–2166. doi: 10.1056/nejmoa1409312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonaca M. P., Bhatt D. L., Cohen M., et al. Long-term use of ticagrelor in patients with prior myocardial infarction. New England Journal of Medicine . 2015;372(19):1791–1800. doi: 10.1056/nejmoa1500857. [DOI] [PubMed] [Google Scholar]
- 20.Steg P. G., Bhatt D. L., Simon T., et al. Ticagrelor in patients with stable coronary disease and diabetes. New England Journal of Medicine . 2019;381(14):1309–1320. doi: 10.1056/nejmoa1908077. [DOI] [PubMed] [Google Scholar]
- 21.D’Ascenzo F., Bertaina M., Fioravanti F., et al. Long versus short dual antiplatelet therapy in acute coronary syndrome patients treated with prasugrel or ticagrelor and coronary revascularization: insights from the RENAMI registry. European journal of preventive cardiology . 2020;27(7):696–705. doi: 10.1177/2047487319836327. [DOI] [PubMed] [Google Scholar]
- 22.Collet J. P., Thiele H., Barbato E., et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. European Heart Journal . 2021;42(14):1289–1367. doi: 10.1093/eurheartj/ehaa575. [DOI] [PubMed] [Google Scholar]
- 23.Capranzano P., Angiolillo D. J. Tailoring P2Y(12) inhibiting therapy in elderly patients with myocardial infarction undergoing primary percutaneous coronary intervention. Journal of American Heart Association . 2019;8(18) doi: 10.1161/jaha.119.014000.e014000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Montalto C., Crimi G., Morici N., et al. Bleeding risk prediction in elderly patients managed invasively for acute coronary syndromes: external validation of the PRECISE-DAPT and PARIS scores. International Journal of Cardiology . 2021;328:22–28. doi: 10.1016/j.ijcard.2020.11.065. [DOI] [PubMed] [Google Scholar]
- 25.Varenne O., Cook S., Sideris G., et al. Drug-eluting stents in elderly patients with coronary artery disease (SENIOR): a randomised single-blind trial. The Lancet . 2018;391(10115):41–50. doi: 10.1016/s0140-6736(17)32713-7. [DOI] [PubMed] [Google Scholar]
- 26.Frigoli E., Smits P., Vranckx P., et al. Design and rationale of the management of high bleeding risk patients post bioresorbable polymer coated stent implantation with an abbreviated versus standard DAPT regimen (MASTER DAPT) study. American Heart Journal . 2019;209:97–105. doi: 10.1016/j.ahj.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 27.Franzone A., McFadden E., Leonardi S., et al. Ticagrelor alone versus dual antiplatelet therapy from 1 Month after drug-eluting coronary stenting. Journal of the American College of Cardiology . 2019;74(18):2223–2234. doi: 10.1016/j.jacc.2019.08.1038. [DOI] [PubMed] [Google Scholar]
- 28.Li Y., Jing Q., Wang B., et al. Extended antiplatelet therapy with clopidogrel alone versus clopidogrel plus aspirin after completion of 9- to 12-month dual antiplatelet therapy for acute coronary syndrome patients with both high bleeding and ischemic risk. Rationale and design of the OPT-BIRISK double-blinded, placebo-controlled randomized trial. American Heart Journal . 2020;228:1–7. doi: 10.1016/j.ahj.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wood B., Lee C. R., Mulrenin I. R., et al. Effects of aging on clinical outcomes in patients receiving genotype-guided P2Y12 inhibitor selection after percutaneous coronary intervention. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy . 2021;41(12):970–977. doi: 10.1002/phar.2611. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used are included within the article.


