Abstract
Background
The aim of this study was to investigate the relationship between keratoconus disease and the antioxidant activities of catalase (CAT), reduced glutathione (GSH) and superoxide dismutase (SOD) and the level of the oxidative stress marker malondialdehyde (MDA) in serum.
Methods
The study included 50 patients diagnosed with keratoconus and 53 healthy age- and sex-matched control subjects. The keratoconus patients were grouped according to the four keratoconus stages based on the modified Krumeich keratoconus classification system. The CAT, GSH and SOD activities and MDA levels in the serum samples collected from the patient and control groups were compared.
Results
The mean serum CAT, GSH, SOD and MDA levels in the keratoconus group were determined to be 0.075 (0.074–0.078)U/L, 0.002 (0.001–0.006) mmol/ml, 1.56 (1.51–1.62)U/L and 1.69 (1.65–1.99) mmol/L, respectively, and those in the control group were determined to be 0.024 (0.013–0.037)U/L, 0.029 (0.018–0.049) mmol/ml, 4.13 (4.01–4.17) U/L and 0.74 (0.65–0.82) mmol/L. The serum GSH levels and SOD activity were significantly lower in the keratoconus group (p < 0.001 for both) than in the control group while the CAT activity and MDA levels were significantly higher (p < 0.001 for both).
Conclusion
The low serum GSH levels and SOD activity and the high CAT activity and MDA levels observed in this study suggest the presence of oxidative stress and inadequate antioxidant defence mechanisms in keratoconus patients. The studied parameters may offer auxiliary markers for use in the diagnosis and treatment of the keratoconus disease and in its potential therapeutic targets in the future.
Subject terms: Predictive markers, Corneal diseases, Predictive markers
Introduction
Keratoconus is a degenerative corneal disorder that causes progressive myopia and irregular astigmatism due to the characteristic thinning of the corneal stroma.
The cornea is the largest ocular structure exposed to ultraviolet (UV) light, a major environmental stress factor that creates cytotoxic free oxygen radicals. The cornea absorbs much of the UV light that reaches the eye [1, 2]. This leads to oxidative stress in the cornea, causing an increase in the amount of harmful reactive oxygen species (ROS) therein, such as superoxide radicals, hydrogen peroxide (H2O2) and hydroxyl radicals. ROS can damage cells by reacting with the protein, DNA and membrane phospholipids found in cellular structures. A healthy cornea has antioxidant enzymes and nonenzymatic molecules that eliminate ROS generated by oxidative stress before they damage the corneal cells. These include enzymes such as superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase and glutathione reductase, in addition to nonenzymatic molecules such as reduced glutathione (GSH) [3–6].
In corneal cells, ROS generated after UV exposure stimulate lipid peroxidation, which in turn results in the production of reactive aldehydes such as malondialdehyde (MDA) and 4-hydroxy-2-nonenal (HNE). In a healthy cornea, aldehyde dehydrogenase eliminates the reactive aldehyde forms and directly absorbs UV radiation, thereby protecting the corneal cells from reactive aldehydes such as MDA and HNE. Approximately 20–40% of the proteins in a healthy cornea are isoenzymes of aldehyde dehydrogenase enzymes. In corneas with keratoconus, MDA and HNE can damage the cellular biomolecules. This affects cells such as the keratocytes in the cornea, leading to the weakening of the corneal tissue. These aldehydes can also cause changes in the membranes of lysosomes, which in turn release proteolytic enzymes that can damage the corneal tissue, leading to corneal thinning and protrusion [2, 3].
In keratoconic corneas, there are abnormalities in the antioxidant defence mechanisms that eliminate ROS. There have been some studies that measured the oxidative stress and antioxidant enzyme levels in the corneas of keratoconus patients ex vivo [3, 7], but no previous studies have evaluated the serum CAT activity and GSH level in this patient group. The aim of the present study was to investigate the relationship between keratoconus and the antioxidant activities of CAT and SOD as well as the levels of the antioxidant molecule GSH and the oxidant stress marker MDA in serum.
Materials and methods
This study included 50 patients diagnosed with keratoconus and followed up in the ophthalmology department of Van Yüzüncü Yıl University and 53 sex- and age-matched healthy control subjects who presented themselves to the outpatient clinic. The study adhered to the principles of the Declaration of Helsinki and was approved by the Van Yüzüncü Yıl University Clinical Research Ethics Committee. All the participants were informed of everything that they needed to know about the study, and written informed consent forms were obtained from them before the study commencement.
The patients in the keratoconus group were selected through random sampling among those being followed up in the ophthalmology department of Van Yüzüncü Yıl University. Individuals who had no ocular disease other than refractive errors and who were of similar age and sex to those in the patient group were recruited in the control group.
The best-corrected visual acuity of all the participants in the patient and control groups was measured using the Snellen chart. A complete ophthalmic examination, including slit-lamp anterior chamber examination, intraocular pressure measurement, fundus examination and corneal topography (Orbscan Hz; Technolas, München, Germany), was performed.
The criteria for inclusion in the keratoconus group were age ≥18 years, diagnosis of keratoconus based on the Collaborative Longitudinal Evaluation of Keratoconus study [8] and corneal topography showing a pattern consistent with keratoconus and inferior-superior steepening >1.5 diopters (D). The criteria for inclusion in the control group, on the other hand, were age ≥18 years and absence of ocular pathology other than less than ±1.5 D spherical and/or cylindrical refractive error.
In addition to the foregoing criteria, the exclusion criteria for both groups were active smoking; the presence of osteoarthritis and other rheumatic diseases, chronic diseases such as bronchial asthma and diabetes and malignancy; regular exercise; use of chemotherapeutic, steroid, anti-inflammatory, diuretic or antioxidant medication or vitamin supplements and findings of uveitis, glaucoma or any other corneal pathology on ophthalmic examination or history of ocular surgery. The subjects in the control group who had keratoconus or suspected keratoconus based on clinical examination and corneal topography were excluded from the study.
Keratoconus was classified into four stages based on the modified Krumeich keratoconus classification system [9]. In the patients with bilateral keratoconus, keratoconus was staged according to the eye with more advanced disease.
Blood sample collection
A 3 ml venous blood sample was collected from each of the patients and control subjects and was centrifuged for 10 min at 5000 rpm. The serum was separated and stored at −80 °C until analysis.
Analysis methods
CAT activity assay
The serum CAT activity was determined using the method described by Aebi et al. [10]. First, 2.8 ml 30 mM H2O2 was placed in a blind tube, and 0.2 ml phosphate buffer was added to it. Then 2.8 ml 30 mM H2O2 was added to the sample tube. To both of these tubes, 0.2 ml enzyme was added, and the tubes were mixed through vortexing. The absorbances at 240 nm were read twice at 30 s intervals to determine the activity.
GSH assay
The GSH level was determined using the method described by Beutler et al. [11]. First, 200 µl serum was diluted in 800 µl phosphate buffer, and the first absorbance (OD1) was measured at 412 nm. Then 100 µl Ellman’s reagent was added to the same tube, and the second absorbance value (OD2) was recorded. The GSH concentration was calculated using the formula C/1000 = (OD2 − OD1)/13,600 × E1 × 5/2 × [(C: mmol/glutathione (mg/dl)].
SOD activity assay
The serum SOD activity was determined using the method recommended by Sun et al. [12]. This method is based on reading the optical density (at 560 nm) of blue formazan dye formed in the reaction of nitro blue tetrazolium with the superoxide radicals generated using xanthine and xanthine oxidase. The SOD found in the sample eliminates the superoxide radicals from the medium, inhibiting the formazan reaction. One unit of SOD inhibits the nitro blue tetrazolium reduction rate by 50% under assay conditions.
MDA level assay
MDA, one of the peroxidation products formed by the reaction of fatty acids with free radicals, was measured as the formation of its coloured form with thiobarbituric acid [10]. For each patient, 200 µl serum was transferred to a tube, and 800 µl phosphate buffer, 25 µl butyl-hydroxytoluene solution and 500 µl 30% trichloroacetic acid were added. The tubes were mixed and incubated on ice for 2 h. They were then centrifuged at 2000 rpm for 15 min, and 1 ml of each supernatant was transferred to a new tube, after which 75 µl ethylenediamine tetraacetic acid and 25 µl thiobarbituric acid were added. The tubes were mixed and incubated in a hot water bath for 15 min. They were then brought to room temperature, and the absorbance at 532 nm was read on a UV/Vis spectrophotometer.
Statistical analysis
The obtained data were analysed using the SPSS version 23.0 software (IBM Corp., Armonk, NY). Descriptive statistics were used to determine the mean and standard deviations (SDs) of age, sex and the serum biomarker levels in the patient and control groups. The Kolmogorov–Smirnov test was used to determine if the data were normally distributed. The serum SOD and CAT activities and the GSH and MDA levels of the keratoconus and control groups were compared using the Mann–Whitney U test, and those of the keratoconus stages, using the Kruskal–Wallis test. The relationships between the keratoconus stages and the CAT, GSH, SOD and MDA levels were evaluated through multinominal logistic regression analysis. A p-value below 0.05 was regarded as statistically significant.
Results
Of the 50 keratoconus patients in this study, 30 were female (60%) and 20 were male (40%), and the mean age was 22.1 years (SD 4.6, range 18–35 years). Of the 53 healthy control subjects, 32 were female (60.4%) and 21 were male (39.6%), and their mean age was 22.9 years (SD 2.8, range 18–29 years). There was no statistically significant difference between the two groups in terms of sex or age (p = 0.81 and 0.31, respectively). Keratoconus was classified as stage 1 in 17 patients, stage 2 in 24 patients, stage 3 in seven patients and stage 4 in two patients.
The serum CAT, GSH, SOD and MDA levels differed significantly between the keratoconus and control groups. The keratoconus group showed significantly lower serum SOD activity and GSH levels (p < 0.001 for both) and significantly higher CAT activity and MDA levels (p < 0.001 for both) compared to the control group. The mean SOD, CAT, GSH and MDA levels of the patient and control groups are summarised in Table 1.
Table 1.
Mean (min-max) serum CAT, GSH, SOD and MDA levels in the keratoconus and control groups.
| Keratoconus (n = 50) | Control (n = 53) | P value | CI 95% min–max | |
|---|---|---|---|---|
| CAT (U/L) | 0.075 (0.074–0.078) | 0.024 (0.013–0.037) | <0.001 | 0.049 to 0.053 |
| GSH (mmol/ml) | 0.002 (0.001–0.006) | 0.029 (0.018–0.049) | <0.001 | −0.024 to −0.028 |
| SOD (U/L) | 1.56 (1.51–1.62) | 4.13 (4.01–4.17) | <0.001 | −2.58 to −2.55 |
| MDA (mmol/L) | 1.69 (1.65–1.99) | 0.74 (0.65–0.82) | <0.001 | 0.92 to 0.96 |
CAT Catalase, GSH Reduced glutathione, SOD Superoxide dismutase, MDA Malondialdehyde.
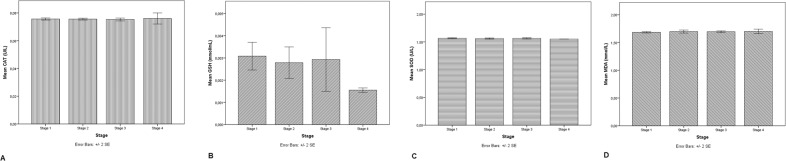
When the CAT, GSH, SOD and MDA values were compared by stage in the keratoconus group, no statistically significant differences were found among them (Table 2). There was thus no statistically significant relationship between keratoconus stage and serum CAT, GSH, SOD or MDA level (p = 0.94, 0.63, 0.71 and 0.85, respectively; Fig. 1A, B, C and D).
Table 2.
Comparison of CAT, GSH, SOD and MDA values in keratoconus stages.
| CAT (U/L) | GSH (mmol/ml) | SOD (U/L) | MDA (mmol/L) | |
|---|---|---|---|---|
| Stage 1 | 0.076 ± 0.001 | 0.003 ± 0.001 | 1.565 ± 0.016 | 1.683 ± 0.026 |
| Stage 2 | 0.076 ± 0.001 | 0.002 ± 0.001 | 1.561 ± 0.024 | 1.697 ± 0.066 |
| Stage 3 | 0.075 ± 0.001 | 0.002 ± 0.001 | 1.564 ± 0.013 | 1.694 ± 0.019 |
| Stage 4 | 0.076 ± 0.002 | 0.001 ± 0.000 | 1.550 ± 0.000 | 1.700 ± 0.049 |
| P Value | 0.96 | 0.23 | 0.46 | 0.44 |
CAT Catalase, GSH Reduced glutathione, SOD Superoxide dismutase, MDA Malondialdehyde.
Fig. 1. The relationship between keratoconus stages and serum CAT, GSH, SOD and MDA levels.
A The relationship between keratoconus stages and serum CAT activity levels. B The relationship between keratoconus stages and serum GSH levels. C The relationship between keratoconus stages and serum SOD activity levels. D The relationship between keratoconus stages and serum MDA levels.
Discussion
In this study, the serum activity levels of the antioxidant enzymes CAT and SOD and the levels of the antioxidant molecule GSH and the oxidative stress marker MDA in the keratoconus patients and healthy controls were compared. The serum SOD activity and GSH levels were found to be lower in the keratoconus group while the serum CAT activity and MDA levels were found to be higher.
Keratoconus is a multifactorial disease whose etiopathogenesis is not yet fully understood, but it is believed to have both genetic and environmental components. In recent years, it has been proposed that the disease occurs as the result of corneal cell damage caused by a disrupted balance between oxidative stress and antioxidants [4, 13]. This view is supported by the fact that higher levels of ROS, which are products of oxidative stress, are found in the corneas of keratoconus patients compared to normal corneas [3, 7, 14].
Antioxidant enzymes eliminate ROS and minimise the cell damage that they cause [6]. When ROS are not eliminated, they lead to irreversible corneal cell damage [15–17]. CAT is an enzyme that degrades H2O2, an ROS, into water and oxygen, thus rendering it harmless [18]. After oxidative stress, the H2O2 that forms in the cornea stimulates an increase in CAT level. Although there have been studies that investigated the total serum antioxidant levels in keratoconus patients [18], no study has specifically investigated the CAT level. Therefore, the present study seems the first to have examined the relationship between systemic CAT level and keratoconus. Toprak et al. [19] compared serum total oxidant status (TOS) and total antioxidant status (TAS) in 25 keratoconus patients and 25 healthy individuals and observed that TOS was significantly higher in the keratoconus group while TAS did not differ significantly between the two groups. Kenney et al. [6] evaluated the CAT mRNA and enzyme activity in 32 keratoconic corneas and 20 normal corneas and found that both the CAT enzyme activity and mRNA level were significantly higher in the keratoconic corneas. In the present study, the serum CAT levels were found to be significantly higher in the keratoconus group than in the control group.
GSH is the most important antioxidant molecule in the intracellular environment. Produced in a reaction catalysed by glutathione peroxidase, GSH is the reduced form of glutathione and reacts with H2O2 or lipid peroxides to neutralise these molecules [20]. It is found in tissues both in its reduced state (GSH) and in an oxidised state (GSSG). A decrease in GSH or an increase in GSSG in tissues is considered an indicator of oxidative stress [21]. Arnal et al. [3] reported that the level of GSH in the keratoconic corneas in their study was significantly lower than that in the normal corneas. Karamichos et al. [22] measured the oxidative stress levels in the corneal keratocytes, fibroblasts and keratoconic corneal cells and determined that the GSH/GSSG levels were significantly lower in the keratoconic corneal cells than in the other cells. A literature search yielded no previous studies that investigated the serum GSH levels in keratoconus patients. In the present study, the serum GSH levels were significantly lower in the keratoconus group than in the control group.
SOD converts superoxide radicals into oxygen and H2O2. As such, it plays an important role in the antioxidant defence mechanism. SOD deficiency results in the accumulation of ROS in tissues. Atilano et al. [7] compared SOD gene expression in the corneas of keratoconus patients and control subjects and detected decreases in the SOD1 and SOD3 genes and an increase in the SOD2 gene in the keratoconic corneas. In a similar study, Behndig et al. [23] compared the amount of SOD in corneas from keratoconus patients and controls and found that the keratoconus corneas had only half the amount of SOD in the control corneas. Balmus et al. [24] investigated the amount of SOD in the tears of keratoconus patients and found that it was significantly lower than in the tears of the healthy controls. In the literature review, few publications were found on the serum antioxidant levels in keratoconus patients. Cantemir et al. [25] evaluated the serum SOD levels in 20 keratoconus patients and 20 control subjects and reported significantly lower serum SOD in the keratoconus patients. Kılıç et al. [26] also compared the serum SOD levels of the keratoconus patients and controls but did not detect a significant difference between the two groups. In this study, similar to the previous studies, the serum SOD levels were found to be significantly lower in the keratoconus group than in the control group.
H2O2 is transformed into the water by glutathione peroxidase and into water and oxygen via CAT through two different pathways in tissues, making it harmless to the body. Reduced GSH catalyses the glutathione peroxidase enzyme. The GSH levels were found to be low in this study. In addition, although the amount of H2O2 decreased in this study due to the decrease in SOD enzyme activity, the low GSH levels at the same time caused a decrease in glutathione peroxidase activity, thus reducing the conversion of H2O2 to water by glutathione peroxidase. Thus, the amount of H2O2 increased relatively. In this case, H2O2 can be removed only through another pathway, the catalase pathway. This could have been the cause of the increased CAT activity in this study.
ROS that form due to oxidative stress induce lipid peroxidation. MDA is a free aldehyde, a toxic by-product of lipid peroxidation. For this reason, the MDA level is an indicator of lipid peroxidation and therefore also of oxidative stress [4, 27]. Buddi et al. [4] compared the MDA levels in 26 keratoconus corneas and 11 normal corneas and found them to be significantly higher in the keratoconic corneas. In a study that investigated the MDA levels in the tears of keratoconus patients, the MDA levels were found to be significantly higher than those in the tears of the control group [24]. In the study by Kılıç et al. [26], the MDA levels were significantly higher in the keratoconus group than in the control group, consistent with this study. The serum MDA levels in the present study were also found to be significantly higher in the keratoconus group than in the control group.
In conclusion, this study was the first to have investigated the CAT activity and the GSH level in the serum of keratoconus patients. The low serum GSH levels and SOD activity and the high CAT activity and MDA levels observed in this study suggest the presence of oxidative stress and inadequate antioxidant defence mechanisms in keratoconus patients. There may be a general systemic difference in oxidant–antioxidant balance in keratoconus patients. The determination of the serum CAT, GSH, SOD, and MDA levels may be considered an auxiliary method for the diagnosis and treatment of keratoconus if the findings of the present study will be supported by those of future studies with larger groups. The development of systemic and local antioxidant therapies may be a new and promising goal in keratoconus treatment.
Summary
What was known before:
Oxidative stress and reactive oxygen species (ROS) play a role in the aetiology of keratoconus (KC)
There are some biomarkers that show oxidative stress, such as superoxide dismutase (SOD), glutathione peroxidase (GPx)
What this study adds:
This study is the first to investigate the activity of antioxidants such as catalase (CAT) and reduced glutathione (GSH) in the serum of keratoconus patients.
Acknowledgements
The authors thank Professor Halit DEMİR, MD PhD and his colleagues in the biochemistry laboratory for their contributions to this study.
Author contributions
ST conceived and designed the presented study. ST and ES performed the data collection. ST performed the analysis and wrote the manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nita M, Grzybowski A. The role of the reactive oxygen species and oxidative stress in the pathomechanism of the age-related ocular diseases and other pathologies of the anterior. Oxid Med Cell Longev. 2016;2016:3164734. doi: 10.1155/2016/3164734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vallabh N, Romano V, Willoughby C. Mitochondrial dysfunction and oxidative stress in corneal disease. Mitochondrion. 2017;36:103–13. doi: 10.1016/j.mito.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 3.Arnal E, Peris-Martínez C, Menezo J. Oxidative stress in keratoconus? Invest Ophthalmol Vis Sci. 2011;52:8592–7. doi: 10.1167/iovs.11-7732. [DOI] [PubMed] [Google Scholar]
- 4.Buddi R, Lin B, Atilano SR, Zorapapel NC, Kenney MC, Brown DJ. Evidence of oxidative stress in human corneal diseases. J Histochem Cytochem. 2002;50:341–51. doi: 10.1177/002215540205000306. [DOI] [PubMed] [Google Scholar]
- 5.Squadrito G, Pryor W. Oxidative chemistry of nitric oxide: the roles of superoxide, peroxynitrite, and carbon dioxide. Free Radic Biol Med. 1998;25:392–403. doi: 10.1016/S0891-5849(98)00095-1. [DOI] [PubMed] [Google Scholar]
- 6.Kenney M, Chwa M, Atilano S, Tran A, Carballo M, Saghizadeh M, et al. Increased levels of catalase and cathepsin V/L2 but decreased TIMP-1 in keratoconus corneas: evidence that oxidative stress plays a role in this disorder. Invest Ophthalmol Vis Sci. 2005;46:823–32. doi: 10.1167/iovs.04-0549. [DOI] [PubMed] [Google Scholar]
- 7.Atilano S, Lee D, Fukuhara P, Chwa M, Nesburn A, Udar N, et al. Corneal oxidative damage in keratoconus cells due to decreased oxidant elimination from modified expression levels of SOD enzymes, PRDX6, SCARA3. J Ophthalmic Vis Res. 2019;14:62. doi: 10.4103/jovr.jovr_80_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wagner H, Barr J, Zadnik K. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study: methods and findings to date. Cont Lens Anterior Eye. 2007;30:223–32. doi: 10.1016/j.clae.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krumeich J, Kezirian G. Circular keratotomy to reduce astigmatism and improve vision in stage I and II keratoconus. j Refract Surg. 2009;25:357–65. doi: 10.3928/1081597X-20090401-07. [DOI] [PubMed] [Google Scholar]
- 10.Aebi H. Catalase in vitro. Methods Enzymol. 1984;105:121–6. doi: 10.1016/S0076-6879(84)05016-3. [DOI] [PubMed] [Google Scholar]
- 11.Beutler E. Improved method for the determination of blood glutathione. J Lab Clin Med. 1963;61:882–8. [PubMed] [Google Scholar]
- 12.Sun Y, Oberley L, Li Y. A simple method for clinical assay of superoxide dismutase. Clin Chem. 1988;34:497–500. doi: 10.1093/clinchem/34.3.497. [DOI] [PubMed] [Google Scholar]
- 13.Atilano S, Coskun P, Chwa M, Jordan N, Reddy V, Le K, et al. Accumulation of mitochondrial DNA damage in keratoconus corneas. Invest Ophthalmol Vis Sci. 2005;46:1256–63. doi: 10.1167/iovs.04-1395. [DOI] [PubMed] [Google Scholar]
- 14.Chwa M, Atilano S, Reddy V, Jordan N, Kim D, Kenney M. Increased stress-induced generation of reactive oxygen species and apoptosis in human keratoconus fibroblasts. Invest Ophthalmol Vis Sci. 2006;47:1902–10. doi: 10.1167/iovs.05-0828. [DOI] [PubMed] [Google Scholar]
- 15.Dudakova L, Liskova P, Jirsova K. Is copper imbalance an environmental factor influencing keratoconus development? Med Hypotheses. 2015;84:518–24. doi: 10.1016/j.mehy.2015.02.017. [DOI] [PubMed] [Google Scholar]
- 16.Zhou L, Sawaguchi S, Twining S, Sugar J, Feder R, Yue B. Expression of degradative enzymes and protease inhibitors in corneas with keratoconus. Invest Ophthalmol Vis Sci. 1998;39:1117–24. [PubMed] [Google Scholar]
- 17.Balasubramanian S, Mohan S, Pye D, Willcox MD. Proteases, proteolysis and inflammatory molecules in the tears of people with keratoconus. Acta Ophthalmol. 2012;90(Jun):45. doi: 10.1111/j.1755-3768.2011.02369.x. [DOI] [PubMed] [Google Scholar]
- 18.Atalla L, Fernandez MA, Rao NA. Immunohistochemical localization of catalase in ocular tissue. Curr Eye Res. 1987;6:1181–7. doi: 10.3109/02713688709025227. [DOI] [PubMed] [Google Scholar]
- 19.Toprak I, Kucukatay V, Yildirim C, Kilic-Toprak E, Erkek O. Increased systemic oxidative stress in patients with keratoconus. Eye. 2014;28:285. doi: 10.1038/eye.2013.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pompella A, Corti A. The changing faces of glutathione, a cellular protagonist. Front Pharmacol. 2015;6:98. doi: 10.3389/fphar.2015.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zitka O, Skalickova S, Gumulec J, Masarik M, Adam V, Hubalek J, et al. Redox status expressed as GSH:GSSG ratio as a marker for oxidative stress in paediatric tumour patients. Oncol Lett. 2012;4(Dec):1247–53. doi: 10.3892/ol.2012.931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karamichos D, Hutcheon A, Rich C, Trinkaus-randall V, Asara J, Zieske J. In vitro model suggests oxidative stress involved in keratoconus disease. Sci Rep. 2014;4:4608. doi: 10.1038/srep04608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Behndig A, Karlsson K, Johansson B, Brannstrom T, Marklund S. Superoxide dismutase isoenzymes in the normal and diseased human cornea. Invest Ophthalmol Vis Sci. 2001;42:2293–6. [PubMed] [Google Scholar]
- 24.Balmus I, Alexa A, Ciuntu R, Danielescu C, Stoica B, Cojocaru S, et al. Oxidative stress markers dynamics in keratoconus patients’ tears before and after corneal collagen crosslinking procedure. Exp Eye Res. 2020;190:107897. doi: 10.1016/j.exer.2019.107897. [DOI] [PubMed] [Google Scholar]
- 25.Cantemir A, Iuliana Alexa A, Ciobica A, Miruna Balmus I, Antioch I, Stoica B, et al. Evaluation of antioxidant enzymes in keratoconus. Rev Chim. 2016;67:1538–41. [Google Scholar]
- 26.Kılıç R, Bayraktar A, Bayraktar S, Kurt A, Kavutçu M. Evaluation of serum superoxide dismutase activity, malondialdehyde, and zinc and copper levels in patients with keratoconus. Cornea. 2016;35:1512–5. doi: 10.1097/ICO.0000000000001018. [DOI] [PubMed] [Google Scholar]
- 27.Esterbauer H, Schaur R, Zollner H. Chemistry and biochemistry of 4-hydroxynonenal, malonaldehyde and related aldehydes. Free Radic Biol Med. 1991;11:81–128. doi: 10.1016/0891-5849(91)90192-6. [DOI] [PubMed] [Google Scholar]