Abstract
Objective:
NK cells play crucial roles in the immune defense mechanisms against viral infections and transformed cells. However, the developmental progression, transcriptomic landscape, and functional subtypes of liver NK cells are not well defined. Hepatocellular carcinoma (HCC) accounts for approximately 80% of primary liver cancer worldwide, yet the biological characteristics of NK cells in the HCC environment are unclear. Therefore, we aimed to determine these cells’ roles in tumorigenesis and prognosis.
Methods:
We compared the single-cell RNA sequencing profiles of NK cells purified from blood (n = 1), healthy liver tissues (n = 3), HCC tumor tissues (n = 4), and peritumor liver tissues (n = 1) to identify NK cell subsets. Furthermore, we performed bioinformatics analysis by using The Cancer Genome Atlas (TCGA) data to identify prognostic biomarkers simultaneously overexpressed in the blood and tumor tissues of patients with HCC.
Results:
Transcriptomic analysis revealed 5 NK cell subsets (L1-NK-CD56bright, L2-NK-CD56dim, L3-NK-HLA, L4-LrNK-FCGR3A, and L5-LrNK-XCL1) in the healthy liver tissues. However, the transitional L3 subset and the CXCR6+CD16+ L4 subset with strong anti-tumor activity were absent in the HCC and peritumor liver tissues. Furthermore, 4 common prognosis-associated genes (RHOB, TALDO1, HLA-DPA1, and TKT) were significantly overexpressed in the paired tumor tissue and blood.
Conclusions:
Our study revealed 5 specific subsets of NK cells in healthy human liver tissues. However, only 3 of the 5 NK cell subsets were present in HCC and peritumor tissues. The cytotoxic NK cell subsets were absent in HCC tissues. Furthermore, we identified 4 potential non-invasive prognostic biomarkers in patients with HCC.
Keywords: Hepatocellular carcinoma, natural killer cell, single-cell RNA sequencing, heterogeneity, prognosis
Introduction
Natural killer (NK) cells and type 1 innate lymphoid cells (ILC1s) are different subsets of innate lymphoid cells (ILCs), according to the International Union of Immunological Societies, and these cells show significant differences in their development trajectories1. NK cells play major roles in the immune defense mechanisms against viral infections2 and cancer cells through cytolytic activity and the production of inflammatory cytokines3. They directly kill tumor cells that lack MHC class I molecules and enhance the functions of cytotoxic T lymphocytes4. Furthermore, NK cell-based immunotherapy has shown immense potential in the treatment of hematological cancers and solid tumors5–8.
In the peripheral blood, NK cells constitute nearly 10%–15% of all lymphocytes9. The venous blood is a common source of human NK cells for research studies. Human peripheral blood NK cells are classified into 2 subsets according to the surface expression of CD56 and CD16: the CD56dimCD16+ subset, which is highly cytotoxic, and the CD56brightCD16- subset, which secretes specific cytokines10. A large NK cell population is present in the liver11, and it accounts for nearly 30%–50% of the hepatic lymphocytes12. In the liver, NK cells play important roles in liver tolerance and immunity13. The human liver hosts diverse liver-resident and conventional NK (cNK) cell populations. Although the murine liver-resident NK (LrNK) cells (CD49a+DX5−) have been described previously14, the phenotype of human LrNK cells remains obscure. Currently, human LrNK cells are identified according to the expression levels of the transcription factors Eomes, T-bet, and Hobit (EomeshiT-betloHobit+)15–17; the expression of cell surface markers such as CXCR6, CD69, and TIGIT; and the absence of CD49e expression on their cell surfaces18,19. However, the developmental progression, transcriptomic landscape, and heterogeneity of human liver NK cells is not well defined. Therefore, in-depth characterization of the liver NK cells is critical for understanding liver immunology under normal and cancerous conditions, and may aid in determining treatment strategies for patients with liver cancer.
Single-cell RNA sequencing (scRNA-seq) technology is a powerful tool to explore rare and heterogeneous cell populations20–22. A previous study has described a “transitional NK” subset from the scRNA-seq analysis of peripheral blood and bone marrow samples that represents an intermediate stage between CD56bright and CD56dim NK cells, according to the transcriptional profiles of the signature genes defining these 2 NK cell subsets23. Another scRNA-seq study on healthy human blood has demonstrated 3 new subsets of NK cells: type I interferon–responding CD56neg NK cells, cytokine-induced memory-like NK cells, and NK cells with low ribosomal expression24. Furthermore, high-dimensional scRNA-seq analysis has demonstrated the conserved organ-specific features of the splenic NK cells in both humans and mice25.
Hepatocellular carcinoma (HCC) accounts for approximately 80% of all primary liver cancer cases worldwide26 and is the fourth most common cause of cancer-associated deaths globally27,28. The roles of different NK cell subsets may be critical for the development and progression of HCC. However, a previous scRNA-seq analysis of healthy human liver cells has identified NK cells in only 2 of 5 donors, because a mixture of parenchymal and non-parenchymal cells was present29. Furthermore, scRNA-seq analysis of liver-resident immune cells has not clearly identified distinct immunological characteristics of NK cell populations30. The comprehensive analysis of immune cell profiles provides a panoramic overall view but not extensive details regarding immune cell types. Furthermore, most scRNA-seq studies on immune cells derived from HCC tissues have focused on the characteristics of T cells, whereas the characteristics of NK cells have not been defined31,32. Hence, an urgent need exists to perform scRNA-sequencing analysis on NK cells derived from healthy liver and HCC tissues to discover new NK cell subsets that may be beneficial for immunotherapy. Therefore, in this study, we performed single cell transcriptome analysis of the NK cells from the liver, spleen, and peripheral blood of healthy control participants and patients with HCC to determine different subsets of liver-resident NK cells in healthy liver tissues and HCC tissues. We also analyzed potential prognostic genes in the NK cells isolated from paired peripheral blood and HCC tissues from a single patient with HCC.
Materials and methods
Human sample collection and ethics statement
The Ethics Committee of University of Science and Technology of China (2019 KY Ethics No. 116) and the Ethics Committee of the First Affiliated Hospital of University of Science and Technology of China [2019-N(H)-121] approved this study. All patients in this study provided written informed consent to sample collection and data analysis. The tumor tissues and peripheral blood were obtained from patients diagnosed with HCC on the basis of histopathology. Healthy liver tissues were obtained from participants without liver tumors. The clinicopathological characteristics of patients enrolled in cohort 1 are listed in Supplementary Table S1. Further details regarding the patients in cohort 1 are listed in Supplementary Table S2.
Preparation of human lymphocytes
Fresh liver tissues (HCC or healthy liver) were minced into pieces. The tissue homogenates were treated with 1 mg/ml collagenase IV (Sigma) and 150 U/ml DNase I (Sigma) for 1 h. The digested tissue homogenates were then filtered through a 70-μm filter. Tumor infiltrating lymphocytes were then isolated through Percoll-Paque density centrifugation, and RBCs were removed through RBC lysis. Peripheral blood mononuclear cells were isolated with Ficoll-Paque density centrifugation. The lymphocytes were cryopreserved in 10% DMSO in FBS for further experiments.
Cell sorting and flow cytometry
Briefly, individual human lymphocyte samples were thawed, washed, and incubated for 30 min at 4 °C in 1× PBS with 10% normal mouse serum (Beijing Yaanda Biotechnology). The cells were then stained with antibodies for 30 min at 4 °C in the dark. Then the cells were washed with MACS buffer and incubated with the dead cell marker 7-AAD. A FACSAria cell sorter (BD) was used to purify ILCs[Lin- (CD34-CD3-CD14-CD1α-CD19-FcεRIα-) CD45+]. And a FACSCelesta instrument (BD) was used to detect NK cells. The details regarding the antibodies are shown in the Supplementary materials and methods (Doc S1).
Single-cell RNA sequencing
The FACS-sorted ILCs were prepared for 10x Genomics scRNA-seq with the recommended sample preparation protocol, kept on ice, and counted. The intratumor and peritumor liver and blood samples were prepared according to the 10x Genomics Single Cell Reagent Kit user guide. RNA sequencing was performed by Genergy (Shanghai, China) on a Novaseq 6000 machine with a sequencing depth of at least 25,000 reads per cell. The data analysis methods used in this study are listed in the Supplementary materials and methods (Doc S1).
The Cancer Genome Atlas (TCGA) data analysis
HCC patient (cohort 2 and cohort 3) data from TCGA database were used to evaluate the correlation between the selected genes and the survival of patients with HCC. The gene expression data and clinical data for patients with HCC were downloaded from cBioportal (https://www.cbioportal.org/).
Statistical analysis
Statistical analysis was performed in GraphPad PRISM 6 software (GraphPad 6 Software). A P value < 0.05 was considered statistically significant (*P < 0.05, ** P < 0.01, ****P < 0.0001; ns, not significant). Bioinformatics data were statistically analyzed with R language. The bioinformatics analysis software and algorithms used in this study are listed in the Supplementary materials and methods (Doc S1).
Results
Transcriptome profiles of human NK cells significantly differ among the liver, spleen, and peripheral blood
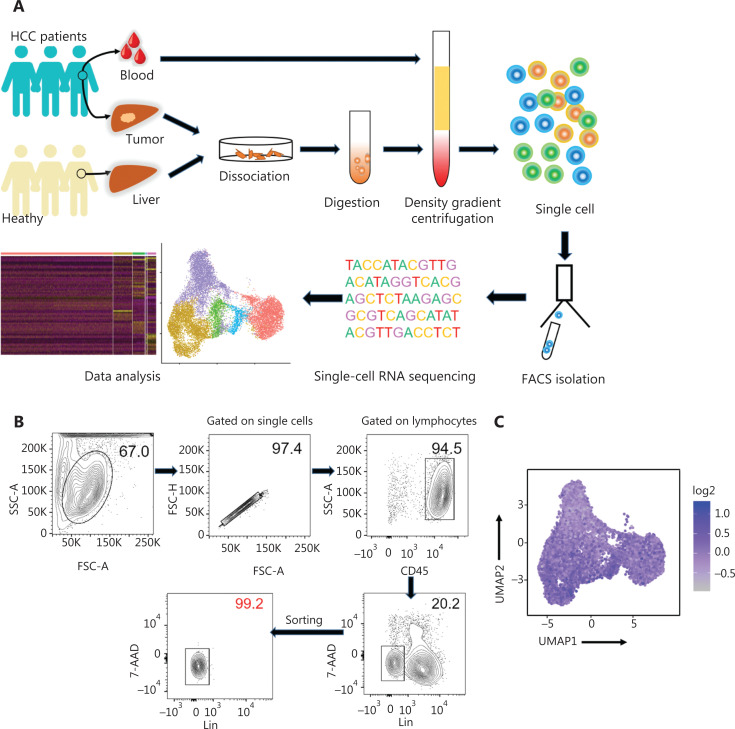
High-throughput scRNA-seq was performed to investigate the biological roles of NK cells in the human liver. The human liver ILCs were sorted by flow cytometry from untreated patients with HCC (n = 4) and healthy control donors (HC, n = 3). Furthermore, fresh lymphocytes were isolated from paired intratumor (IT) tissues, peritumor (PT) tissues, and peripheral blood from a single patient with HCC (patient number 101) to compare the differences between local and peripheral sources in 1 person (Figure 1A). The purity of FACS-sorted Lin- (CD34-CD3-CD14-CD1α-CD19-FcεRIα-) CD45+ ILCs exceeded 99% (Figure 1B). ILCs derived from the livers of HC donors (n = 3; HC1: 14,847 cells; HC2: 17,880 cells; and HC3: 16, 978 cells), peripheral blood (n = 1; 5,452 cells), HCC tumor tissues (n = 4; HCC1: 18,140 cells; HCC2: 10,264 cells; HCC3: 16,030 cells; IT: 10,771 cells), and peritumor liver tissues (n = 1; 10,135 cells) from treatment-naive patients with HCC were subjected to scRNA-sec with 10x Genomic technology. The 10x Genomics Cell Ranger software was used to process the sequences of 120,497 single cells with 29,385 mean reads per cell and 1,151 median genes per cell (Supplementary Table S3). The downstream data analysis was performed with the Seurat R package33,34, and the cells with low quality (number of genes less than 500 or more than 2,500) and a high (more than 5%) mitochondrial genome transcript ratio were removed. Furthermore, ILC1 (IL7R and CXCR3), ILC2 [IL7R and PTGDR2 (CRTH2)], and ILC3 [IL7R and KIT (CD117)] cells were removed from the analysis on the basis of their maker genes, and only NK cells were selected for the final analysis, according to high expression of NKG7 and the absence of IL7R35,36. The final analysis included 46,726 NK cell transcriptomes, including those from the blood (n = 1; 4,756 cells) and liver tissues from HC donors (n = 3; HC1: 6,234 cells; HC2: 2,124 cells; and HC3: 5,846 cells), as well as peritumor liver tissues (n = 1; 8,280 cells) and HCC specimens (n = 4; HCC1: 3,902 cells; HCC2: 4,799 cells; HCC3: 3,809 cells; IT: 6,976 cells). NK cell identity was confirmed according to the transcriptional status of CD160, CD244, CHST12, CST7, GNLY, IL18RAP, IL2RB, KLRC1, KLRC3, CD94 (KLRD1), NKp80 (KLRF1), PRF1, and XCL225 (Figure 1C).
Figure 1.
Study design and basic information for single cell RNA-seq analysis of human innate lymphoid cells. (A) Scheme of the overall study design. We performed 10x Genomics scRNA-seq on innate lymphoid cells derived from the livers (n = 3) of healthy control donors, as well as blood (n = 1), tumor (n = 4), and tumor-adjacent liver tissue (n = 1) from treatment-naive patients with HCC. The output data were integrated and combined for downstream analysis. (B) Flow cytometry plot of a representative human liver sample, illustrating the gating strategy used to sort innate lymphoid cells. Human innate lymphoid cells were defined as living single-cell Lin- (CD34- CD3- CD14- CD1α- CD19- FcεRIα-) CD45+ 7-AAD- lymphocytes. SSC, side scatter; FSC, forward scatter. (C) UMAP plot showing NK cell feature scores. Feature genes, defined according to Crinier et al.25, included CD160, CD244, CHST12, CST7, GNLY, IL18RAP, IL2RB, KLRC1, KLRC3, KLRD1, KLRF1, PRF1, and XCL2.
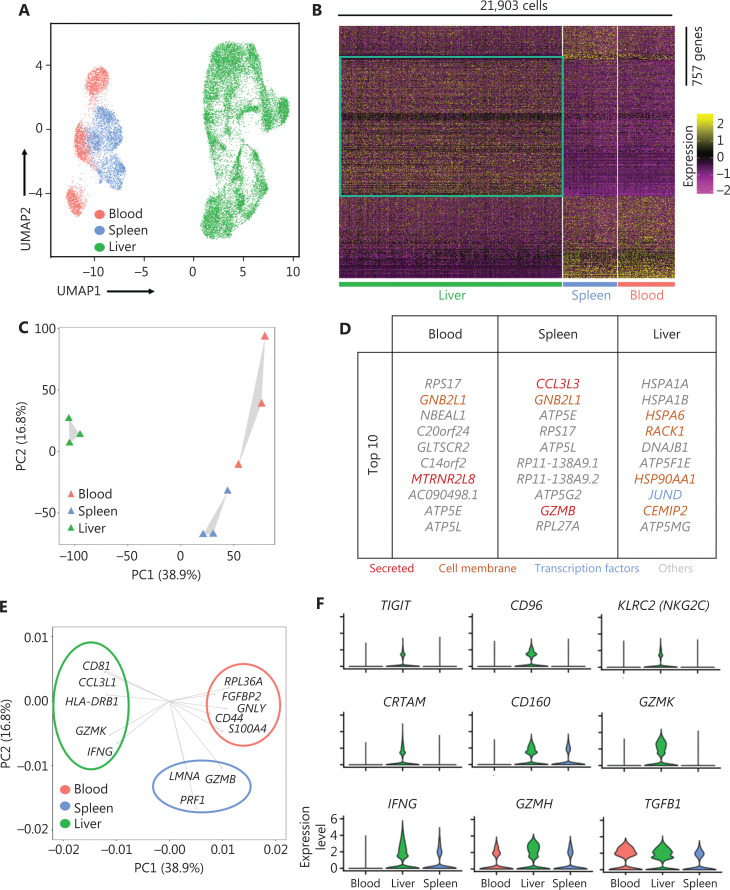
We investigated the heterogeneity of the human liver NK cells by comparing 3 liver, spleen25, and blood25 samples from healthy donors in the GEO database (GSE119562). The transcriptomic profiles of the NK cells were visualized with Uniform Manifold Approximation and Projection (UMAP) plots, in which each dot represented a single cell37. UMAP analysis of the blood (3,763), spleen (3,543), and liver (14,597) NK cells showed distinct differences in transcriptome characteristics (Figure 2A). We identified 757 genes (355 liver-specific, 189 spleen-specific, and 213 blood-specific) with significant differences in expression levels among NK cells derived from the liver, spleen, and blood (Figure 2B). The heatmap of gene expression showed a clear separation between liver NK cells and spleen and blood NK cells, according to the expression levels of these 757 genes (Figure 2B). Principal component analysis (PCA) also segregated the NK cells from the liver, spleen, and blood. PC2 separated the NK cells from those in the blood and the spleen; moreover, both PC1 and PC2 separated the liver NK cells from the blood and spleen NK cells (Figure 2C). These results suggested that liver NK cells had significantly different transcriptome characteristics from blood and spleen NK cells. Furthermore, these results suggested that the blood and spleen NK cells were more closely associated with each other than liver NK cells. The top 10 genes differentially expressed among the NK cells from the liver, blood, and spleen are shown in Figure 2D. We then confirmed the driver genes by mapping the genes in different subsets. GZMB and PRF1 (targeted cell death-associated genes) were driver genes for splenic NK cells; GNLY (a cytotoxicity-associated gene) and CD44 (a cell–cell adhesion and migration associated gene) were driver genes for blood NK cells; and HLA-DRB1 (antigen presentation gene) and IFNG (soluble cytokine gene) were driver genes for liver NK cells (Figure 2E). Violin plot analysis indicated higher gene expression of inhibitory receptors such as TIGIT and CD96; activating receptors such as KLRC2, CRTAM, and CD160; cytolytic proteins such as GZMK and GZMH; and cytokines such as IFNG and TGFB1 in NK cells from the liver than from the blood and spleen (Figure 2F). Together, these results demonstrated significant differences in the transcriptome profiles between the human liver NK cells and the NK cells from the spleen and peripheral blood.
Figure 2.
Liver NK cells are highly distinct from spleen and peripheral blood NK cells. (A) UMAP plot of healthy donor NK cells from human blood (red, 3,763 cells), spleen (blue, 3,543 cells), and liver (green, 14,597 cells) samples. (B) Heatmap of 757 informative genes for distinguishing human blood (213 genes), spleen (189 genes), and liver (355 genes) NK cells. Cells are plotted in columns by organ source, and genes are shown in rows, ranked by adjusted P value < 0.05 (Wilcoxon rank sum test). Gene expression is color coded with a scale based on z-score distribution, from −2 (purple) to 2 (yellow). (C) PCA for the 3 human organ NK cell subsets from each sample, according to the mean expression of the genes. Each triangle represents 1 sample, colored by organ. (D) Top 10 genes significantly differentially expressed among the 3 human organ NK cell subsets. Genes are ranked by log2 fold-change. (E) Genes driving human blood, spleen, or liver NK cell identity (according to the loading value), colored by cell origin. (F) Expression distribution (violin plots) in each population (horizontal axes), for known NK cell genes.
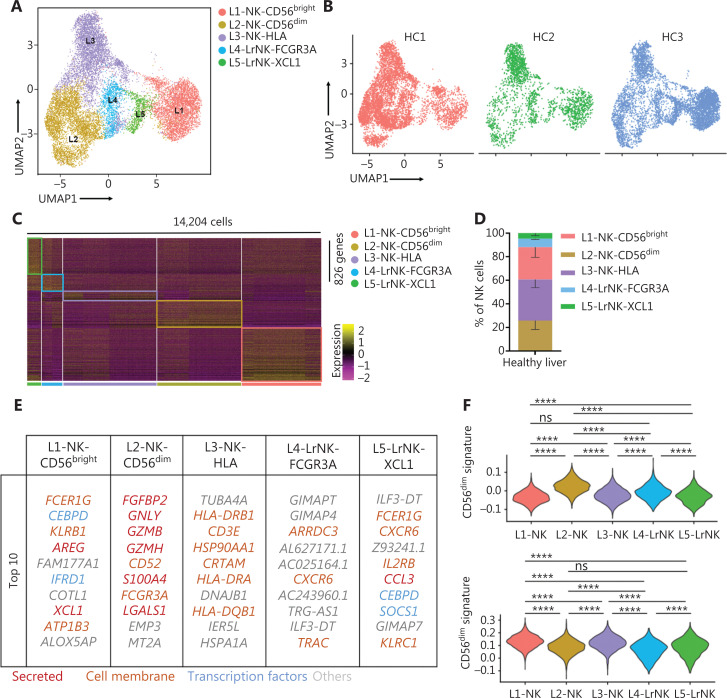
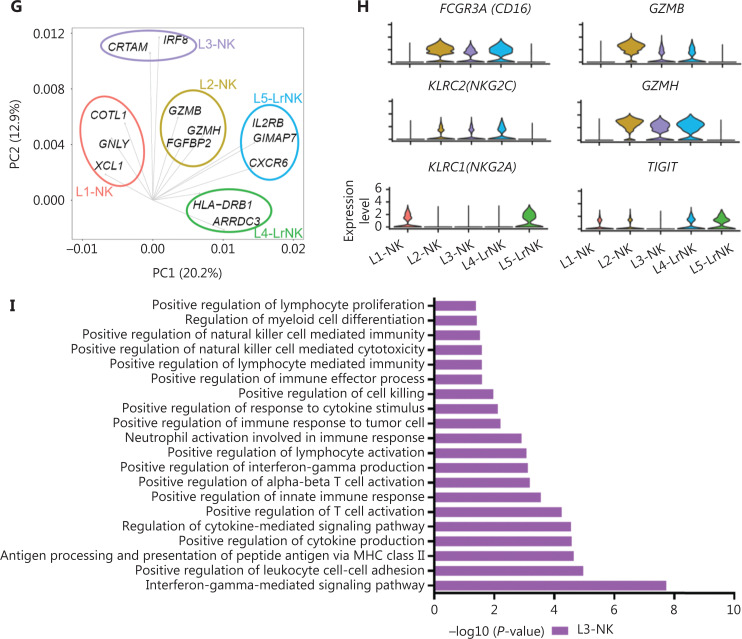
Unsupervised clustering of NK cells from the liver tissues of healthy controls reveals 5 distinct subsets
Next, we integrated the scRNA-seq datasets of 3 HC donors by using the Harmony algorithm38 to identify the functional subtypes of NK cells in the human liver. The results revealed 5 different subsets (L1–L5) in the combined dataset (Figure 3A). Each subset consisted of cells from each donor, thereby indicating a well-integrated dataset (Figure 3B). The subset-specific transcriptomic signatures of each subset are represented by the heatmap in Figure 3C. The percentages of typical CD56bright NK and CD56dim NK subsets were similar, whereas the L3 subset represented the largest proportion of NK cells among the NK cell subsets in the healthy liver (Figure 3D). The top 10 differentially expressed genes among the 5 NK cell subsets are shown in Figure 3E. The L1, L2, and L3 subsets were identified as cNK cells according to their gene transcription signatures, whereas the L4 and L5 subsets were identified as LrNK cells on the basis of the expression of CXCR6 and EOMES (Supplementary Figure S1A and S1B). The L1 subset (CD56bright NK cells) displayed high expression of genes encoding soluble factors, such as amphiregulin (ARGE), XCL1, and XCL2, which have previously been used to identify the human CD56bright NK cluster23,39. The L2 subset represented the CD56dim NK cell cluster and showed significantly high expression of cytotoxicity-associated genes, such as GNLY, GZMB, and GZMH, in addition to overexpression of FCGR3A (encoding CD16), a typical feature of CD56dim NK cells (Figure 3E). The L3-NK-HLA cluster showed moderate expression of XCL1 and FCGR3A (Supplementary Figure S1A and S1B), and represented an intermediate phenotype between those of CD56bright and CD56dim NK cells, in agreement with findings from previous reports10,40. The L3-NK-HLA cells were characterized by high expression of CRTAM (activating receptor) and the human leukocyte antigens HLA-DRB1 and HLA-DRA, which are associated with degranulation, proliferation, and IFN-γ secretion41,42. The L4-LrNK-FCGR3A and L5-LrNK-XCL1 cells showed high expression of CXCR6 and EOMES (transcription factor) (Figure 3E and Supplementary Figure S1A).
Figure 3.
High-throughput scRNA-seq identifies 5 NK cell subsets in the healthy human liver. (A) UMAP projection of NK cells from an integrated analysis of NK cells from 3 healthy control donors, showing the formation of 5 main subsets identified according to the gene expression characteristics of each subset. (B) UMAP plot of human liver NK cells from healthy livers, colored by donor (HC1: 6,234 cells; HC2: 2,124 cells; and HC3: 5,846 cells). (C) Heatmap of the 826 genes assessed with a Wilcoxon rank sum test separating the 14,204 NK cells into 5 main subsets, shown in different colors. Squares identify specific transcriptomic signatures of the distinct cell subsets. (D) The proportions for the 5 subsets defined among NK cells from the 3 healthy control donors across all liver NK cells. (E) Top 10 genes significantly differentially expressed (Wilcoxon rank sum test) among the 5 liver NK cell subsets. Genes are ranked by log2 fold-change. (F) Module scores of CD56dim and CD56bright gene expression programs defined by Hanna et al.43. Violin plots representing the distribution of module scores for CD56dim (top) CD56bright (bottom) for each liver NK cell subset (Kruskal-Wallis ANOVA followed by Dunn’s multiple comparisons test). Nonsignificant (ns) P > 0.05; ****P < 0.0001. (G) PCA for the 5 liver NK cell subsets’ driving genes. (H) Violin plots comparing the expression of selected NK cell markers in this scRNA-seq dataset. The violin represents the probability density at each value. (I) Selected Gene Ontology terms using genes upregulated (log2 fold-change > 0.25) within the L3 subset with an adjusted P < 0.05.
We then compared the gene expression profiles of the 5 human liver NK subsets with those of CD56bright and CD56dim NK cells43 to validate the classification of NK cells. The analysis of module scores calculated at the single-cell level25 Indicated that the CD56bright score of L4-LrNK-XCL1 cells was similar to those of the L1-NK-CD56bright cells, and the CD56dim score of L5-LrNK-FCGR3A cells was similar to that of L2-NK-CD56dim cells (Figure 3F). These results suggested the existence of 2 distinct LrNK subtypes of NK cells in the healthy human liver. The violin plots of module scores demonstrated that the L3-NK-HLA cells represented an intermediate subset between CD56bright and CD56dim NK cells (Figure 3F). Furthermore, PC1 separated the L1-NK, L2-NK, and L5-LrNK subsets, whereas PC2 separated the L3-NK and L4-LrNK subsets from the other NK cell subsets (Figure 3G). PCA results revealed that COTL1 (encoding a specific actin-binding protein), GNLY, and XCL1 were drivers for the L1-NK cells; cytotoxicity-associated GZMB, GZMH, and FGFBP2 (fibroblast growth factor family member) genes were drivers for L2-NK cells; CRTAM and IRF8 were drivers for the L3-NK-HLA cluster; HLA−DRB1 and ARRDC3 were drivers for the L4-LrNK-FCGR3A cluster; and IL2RB, GIMAP7, and CXCR6 were drivers for the L5-LrNK-XCL1 cluster (Figure 3G).
The transcriptional signature of the L3-NK-HLA cells showed enrichment in genes encoding the activating receptors (FCGR3A and KLRC2) and cytotoxic cytokines (GZMB and GZMH), as well as significantly low expression of inhibitory receptors (KLRC1 and TIGIT) (Figure 3H). In agreement with the gene expression data, Gene Ontology-based biological process enrichment analysis strongly suggested that the identified cell subsets are likely to have distinct physiological functions (Supplementary Figure S1C). The L3-NK-HLA cells were enriched in genes involved in positive regulation of cytokine production, leukocyte cell–cell adhesion, lymphocyte activation, and cell killing (Figure 3I).
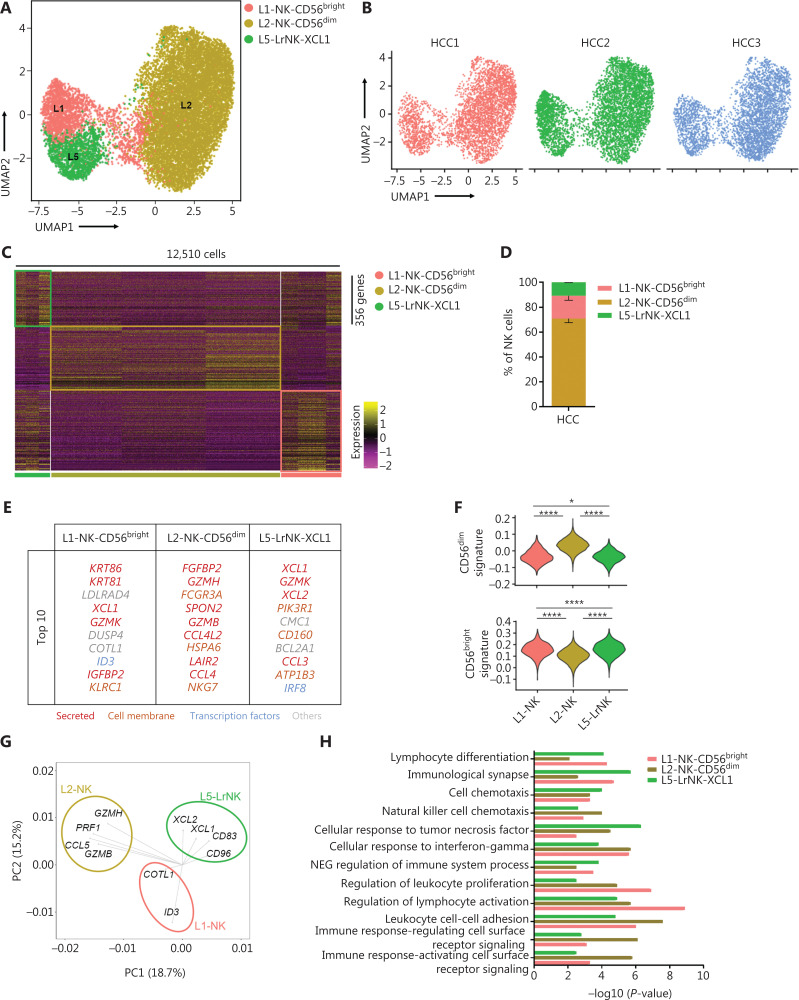
Unsupervised clustering of NK cells from patients with HCC demonstrates the absence of 2 cytotoxic NK cell subsets
We then performed scRNA-seq analysis to determine the characteristics of NK cells in the tumor microenvironment, by using samples from 3 treatment-naive patients with HCC. We identified 3 NK cell subsets in the liver IT tissues, according to differences in the transcriptional profiles (Figure 4A–4C). The L3-NK-HLA and L4-LrNK-FCGR3A subsets associated with cytotoxicity in the healthy human liver were absent in the IT tissues (Figure 4A). At the protein level, the average percentage of L4-LrNK-FCGR3A (CXCR6+CD16+) cells was 8.53% in the healthy liver, but their proportion in the liver cancer tissues (2.7%) was significantly lower than that in healthy liver tissues, as demonstrated by FACS (Supplementary Figure S2A–S2C). Furthermore, as shown by previous studies44, the proportion of L5-LrNK-XCL1 cells was significantly higher in the HCC tissues than the healthy liver tissues (Figure 4D). The top 10 differentially expressed genes in the 3 cell subsets are displayed in Figure 4E. The L1-NK-CD56bright cells overexpressed XCL1 and were comparable to the human CD56bright NK cells. The L2-NK-CD56dim cluster showed high expression of FCGR3A and was comparable to the human CD56dim NK cells. The L5-LrNK-XCL1 cells showed high expression levels of CD160, CD69, ICAM1, and TIGIT, and were comparable to the LrNK cells. The module scores showed significant enrichment in the signature genes of CD56dim NK cells for the L2-NK-CD56dim cells (Figure 4F, top) and the signature genes of CD56bright NK cells for the L1-NK-CD56bright cells and L5-LrNK-XCL1 cells (Figure 4F, bottom). We also investigated the driver genes of the 3 NK cell subsets, according to PCA plots. L1-NK cells showed high expression of COTL1 and ID3 (inhibitor of DNA binding 3); L2-NK cells showed high expression of GZMB, GZMH, PRF1, and CCL5; and L5-NK cells showed high expression of XCL1, XCL2, CD83, and CD96 as driver genes (Figure 4G). Gene Ontology biological process analysis confirmed the specific pathway enrichment of these subsets (Figure 4H). L1-NK-CD56bright cells were associated with the regulation of lymphocyte activity. The L2-NK-CD56dim cluster was associated with regulation of the immune response and activated cell surface receptor signaling. L5-LrNK-XCL1 cells were associated with the cellular response to tumor necrosis factor and the immunological synapse. In summary, the composition of the NK cell subsets was significantly altered in the HCC microenvironment, and the cytotoxic NK cell subsets were absent in HCC tissues.
Figure 4.
High-throughput scRNA-seq identifies 3 NK cell subsets in liver cancer. (A) UMAP projection of NK cells from 3 patients with HCC, showing 3 main subsets (in different colors). The putative functional description for each subset is based on the characteristic gene expression profiles of each subset. (B) UMAP plot of human liver NK cells from tumor infiltrating cells, colored by patient (HCC1: 3,902 cells; HCC2: 4,799 cells; and HCC3: 3,809 cells). (C) Heatmap of the 356 genes tested with a Wilcoxon rank sum test separating the 12,510 HCC-infiltrating NK cells into 3 main subsets shown in different colors. Squares identify specific transcriptomic signatures of different cell subsets. (D) The fractions of 3 subsets defined among NK cells in 3 patients with HCC across all liver NK cells. (E) Top 10 genes significantly differentially expressed among the 3 liver NK subsets. Genes are ranked by log2 fold-change. (F) Module scores of CD56dim and CD56bright gene expression programs defined by Hanna et al.43. Violin plots representing the distribution of module scores for CD56dim (top) CD56bright (bottom) for each liver NK cell subset (Kruskal-Wallis ANOVA followed by Dunn’s multiple comparisons test). *P < 0.05; ****P < 0.0001. (G) PCA for the driving genes of 3 liver NK cell subsets from HCC. (H) Selected Gene Ontology terms using genes upregulated (log2 fold-change > 0.25) within each subset with an adjusted P < 0.05.
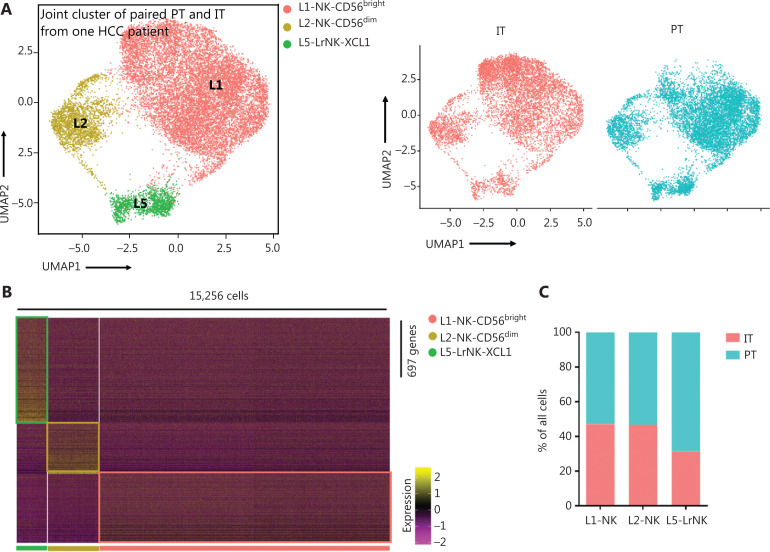
Peri-tumoral NK cells show greater anti-tumor activity than intra-tumoral NK cells
We then performed unsupervised hierarchical clustering analysis of the IT and PT NK cells from patient #101 with HCC to assess the heterogeneity between the NK cells in the whole liver. The clustering of paired PT and IT data revealed 3 subsets whose overall distribution was similar in the PT and IT tissues (Figure 5A). These findings suggested that the microenvironment of the peritumoral tissue differed from that in the healthy liver tissues. The heatmap indicated 3 distinct subsets of NK cells clearly separated on the basis of differences in gene expression patterns (Figure 5B). The general distribution patterns of cNK cells (L1-NK and L2-NK) were similar between the PT and IT tissues, but the proportion of LrNK NK cells (L5-LrNK) was higher in the PT tissues than the IT tissues (Figure 5C). This result suggested that the LrNK cells played a key role in tumor immunology. The violin plots of the module scores indicated clear enrichment in the gene signature of CD56bright NK cells43 for the L1-NK-CD56bright and L5-LrNK-XCL1 NK cells, and the enrichment in the gene signature of CD56dim NK cells43 for the L2-NK-CD56dim NK cells (Figure 5D). We therefore analyzed up-regulated genes among the 3 NK subsets in PT tissues compared with IT tissues to determine changes in gene expression in the tumor microenvironment (Figure 5E). The PT tissues showed higher expression levels of HSPA1A, which encodes a protein that stabilizes existing proteins and prevents protein aggregation, and HSPD1, which encodes a mitochondrial signaling protein that functions in the innate immune system (Figure 5E). Furthermore, violin plots of the NK cell clusters suggested that PT NK cells were more active than IT NK cells. For example, PT NK cells expressed higher levels of genes encoding functional molecules, such as TLE1 (encoding a transcriptional corepressor), IFITM1 (encoding interferon-induced transmembrane protein 1), and S1PR5 (encoding sphingosine 1-phosphate receptor), and lower levels of the inhibitory receptor gene TIGIT (Figure 5F). Gene Ontology biological process analysis of the significantly up-regulated genes showed that the PT NK cells exhibited higher immune activity, such as responses to IFN-γ, regulation of lymphocyte activation, and leukocyte cell-cell adhesion, than the IT NK cells (Figure 5G). Overall, these results suggested that the PT microenvironment distinctly differed from the healthy liver microenvironment. We additionally identified 3 subsets of NK cells in both PT and IT tissues. Moreover, the NK cells from the PT tissues were more active than the NK cells from the IT tissues.
Figure 5.
Comparison of NK cells in the IT and PT of the same patient with HCC. (A) UMAP projection of NK cells from 1 patient with HCC (ID 101; 15,256 cells), depicting 3 main subsets (shown in different colors). The functional description for each subset was determined according to gene expression profiles. UMAP plot of human liver NK cells from IT (6,976 cells) and PT (8,280 cells) of a patient with HCC. (B) Heatmap of the 697 genes tested with a Wilcoxon rank sum test separating the 15, 256 paired IT and PT NK cells into 3 main subsets (shown in different colors). Squares identify specific transcriptomic signatures for the distinct cell subsets. (C) The proportions of the 3 subsets from the IT and PT of a patient with HCC. (D) Module scores of CD56dim and CD56bright gene expression programs defined by Hanna et al.43. Violin plots representing the distribution of module scores for CD56dim (top) CD56bright (bottom) for each liver NK subset (Kruskal-Wallis ANOVA followed by Dunn’s multiple comparisons test). ****P < 0.0001. (E) Top 10 genes significantly overexpressed in PT compared with IT in 3 liver NK subsets. Genes are ranked by log2 fold-change. (F) Violin plots showing expression comparison of selected genes in NK cells. (G) Selected Gene Ontology terms using genes upregulated (log2 fold-change > 0.25) within each origin with an adjusted P < 0.05.
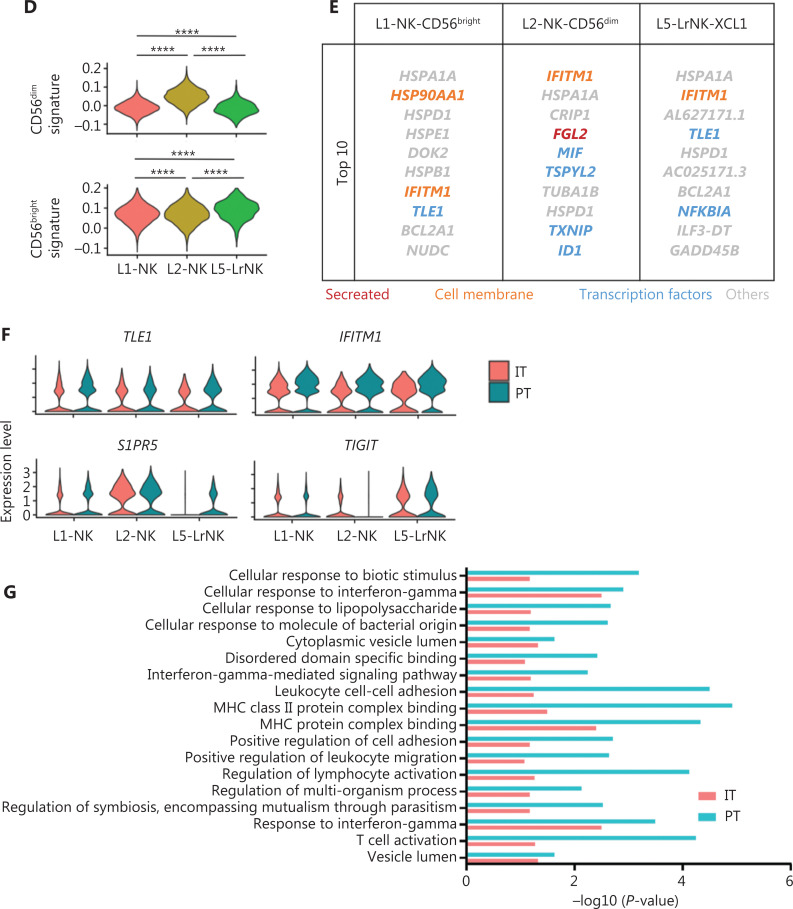
Four prognosis-associated genes are highly expressed in paired tumor and peripheral blood samples from a patient with HCC
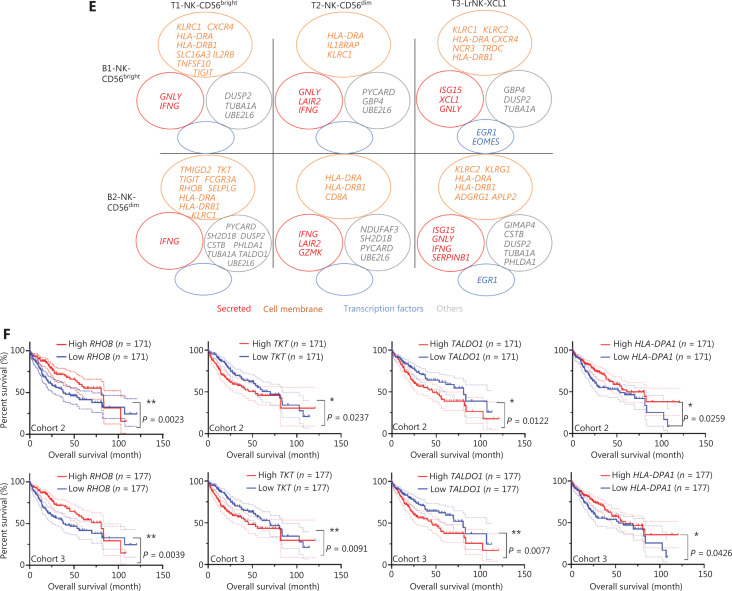
Detecting blood markers is more convenient and easier than performing histology tests in patients with cancer. Therefore, we investigated the expression levels of prognosis-associated genes in both the peripheral blood and tumor tissues to determine their clinical utility. The scRNA-seq analysis of paired blood and tumor samples from 1 patient with HCC demonstrated an absence of LrNK cells in the peripheral blood (Figure 6A). We then performed integrated analysis of the NK cells in blood samples from a healthy donor and a patient with HCC to identify highly expressed genes in the blood of patients with HCC (Supplementary Figure S3A). Venn diagram analysis demonstrated elevated expression of 71 common genes in the blood and IT tissues of patients with HCC (Figure 6B), including genes encoding secretory effector proteins (LAIR2, IFNG, and SERPINB1), membrane proteins (TIGIT, TKT, HLA-DRA, RHOB, HLA-DRB1, ADGRG1, HLA-DPA1, SELPLG, and FCGR3A), and other products (Figure 6C). Pairwise comparisons among NK cell subsets revealed 25 highly expressed common genes across the 5 NK cell subsets in the blood and tumor tissues of patients with HCC (Figure 6D), including genes encoding secretory effector proteins (LAIR2, GNLY, IFNG, GZMK, and XCL1), transcriptional regulators (EGR1 and EOMES), membrane proteins (TIGIT, TKT, HLA-DRA, RHOB, HLA-DRB1, ADGRG1, KLRC1, KLRG1, NCR3, FCGR3A, and CXCR4), and other products (Figure 6E).
Figure 6.
Comparison of NK cells in the tumor and peripheral blood of the same patient with HCC. (A) UMAP plot of human liver NK cells from 1 patient with HCC tumor (6,820 cells) and peripheral blood (4,756 cells), colored by cell origin (left) and subset (right). (B) Venn diagram showing common genes elevated in NK cells from tumor tissue (relative to peritumor tissue, log2 fold-change > 0) and those from HCC blood (relative to healthy blood, log2 fold-change > 0). (C) Common transcriptomic signature between genes elevated in all NK cell subsets from tumor tissue (relative to peritumor tissue, log2 fold-change > 0) and those from HCC blood (relative to healthy blood, log2 fold-change > 0). (D) Venn diagram showing common genes among NK cell subsets from HCC blood and tumor tissue (log2 fold-change > 0). (E) Common subset-specific immune-associated transcriptomic signatures between NK cell subsets from HCC blood and tumor tissue (log2 fold-change > 0). (F) Kaplan–Meier survival curves for the duration of OS in months, according to the gene expression levels of RHOB, TALDO1, HLA-DPA1, and TKT in IT from patients with HCC from cohort 2 and cohort 3 (high densities, red line; low densities, blue line) (log-rank test). *P < 0.05; **P < 0.01.
To explore the relationship between gene expression and patient survival, we then evaluated the potential prognostic value of these 25 highly expressed genes in the NK cells from the blood and tumor tissues of patients with HCC by analyzing TCGA data. Patients with HCC from cohort 2 (n = 372) and cohort 3 (n = 442) were divided into 2 groups on the basis of the median value of the expression of each gene. Four of 25 genes, RHOB, TALDO1, HLA-DPA1, and TKT, were associated with the prognosis of patients with HCC from both cohorts (Figure 6F). Higher expression of RHOB and HLA-DPA1 and lower expression of TALDO1 and TKT in tumors correlated with significantly longer overall survival (OS) in patients with HCC (Figure 6F). Prognostic value of CCDC167, TUBA1A, SH2D1B, and S100A11 was found in only cohort 3 and not in cohort 2 (Supplementary Figure S3B). Furthermore, we observed overexpression of RHOB and HLA-DPA1 and significant downregulation of TKT and S100A11 in the L3-NK and L4-LrNK subsets, which were identified only in healthy liver tissues but were absent in the HCC tissues (Supplementary Figure S3C). We further analyzed the correlation between the expression levels of TKT, RHOB, TALDO1, and HLA-DPA1 genes and the survival of patients with HCC, on the basis of NK cell infiltration into the tumor tissues (Supplementary Figure S4), as previously described45. The patients with HCC in TCGA database were classified according to the expression levels of CD56 and related genes (higher or lower than median expression value in all patients). Then the survival of patients with high or low expression of CD56 and the corresponding genes such as TKT, RHOB, TALDO1, and HLA-DPA1 were evaluated. Low TKT mRNA levels were associated with significantly higher OS in patients with HCC and a higher degree of NK cell infiltration in tumors, according to CD56 expression. Low TALDO1 mRNA levels were associated with longer OS in patients with HCC and a lower degree of NK cell infiltration in tumors. RHOB mRNA levels were associated with survival outcomes of patients with HCC regardless of the degree of NK cell infiltration in the tumors. However, HLA-DPA1 mRNA levels were not associated with the survival outcomes of patients with HCC after the patients were classified according to CD56 expression (Supplementary Figure S4). In summary, our data demonstrated that the expression of these 4 genes in the peripheral blood of patients with HCC can be used in clinical settings to predict HCC prognosis, because the results are consistent with the expression in tumor tissues.
Discussion
Single-cell RNA sequencing is used to investigate cellular heterogeneity in the human tissue microenvironment46,47. In humans, scRNA studies have reported whole liver cell diversity29,48, heterogeneity of liver-resident immune cells30, the landscape and dynamics of the immune cells in HCC tissues32, and the liver microenvironment in early relapsing HCC31. However, these studies have focused on the global immune system in the liver but have not characterized the heterogeneity of NK cells. For example, an scRNA-seq study on healthy human liver cells by Aizarani et al.48 has identified only 1 NK cell subset. Another scRNA-seq study on healthy liver-resident CD45+ immune cells by Zhao et al.30 has classified NK cells into cNK and LrNK cells. An scRNA-seq study of liver transplantation samples by Wang et al.49 has subdivided the liver NK cell population into 4 subsets according to the top 5 highly expressed genes but has not described their functional characteristics. In this study, we analyzed 46,726 liver-resident NK cells from 9 samples, including NK cells from healthy livers (n = 3), HCC tumors (n = 4), HCC tumor-adjacent liver tissues (n = 1), and blood samples (n = 1), to define the heterogeneity of NK cells in the human liver. Our results demonstrated distinct characteristics between liver NK cells and NK cells from the spleen and peripheral blood. The unbiased clustering of single cell sequencing results or the liver NK cell samples identified 5 distinct clusters in the healthy liver (L1, L2, L3, L4, and L5) and 3 clusters in the peritumoral and intratumoral (L1, L2, and L5) liver tissues from patients with HCC. Moreover, the L2 and L5 subsets were significantly elevated in the liver cancer tissues. In previous studies, we have demonstrated that high expression levels of NKG2A50 and CD9651 proteins in the NK cells of HCC tissues are associated with NK cell exhaustion as well as poor prognosis. A recent study has shown that high expression of the TIGIT and TIM3 proteins in the NK cells of patients with liver cancer correlates with NK cell exhaustion and disease progression52. Therefore, we analyzed these markers associated with NK cell exhaustion. Our results showed high expression of the inhibitory receptor genes NKG2A, TIGIT, TIM3, and CD96 in the L1-NK-CD56bright subset; high expression of the inhibitory receptor genes TIM3 and CD96 in the L2-NK-CD56dim subset; and high expression of the inhibitory receptor genes KLRC1 and TIGIT in the L5-LrNK-XCL1 subset (data not shown). In addition, NK cells were more active in the peritumor tissues than the intratumor tissues of patients with HCC. Moreover, we identified 4 commonly overexpressed genes in the peripheral blood and tumor tissues of patients with HCC that correlated with prognosis.
The cell surface markers of human LrNK cells have not been clearly described, in contrast to murine LrNK cells (CD49a+DX5−)14. Several studies have identified CD16neg NK cells as human LrNK cells15–17,53. However, in this study, we identified a subset of CD16pos LrNK cells (L4-LrNK-FCGR3A) in the healthy adult liver that showed high expression of cytotoxicity-associated genes, such as GNLY, FCGR3A, GZMB, GZMH, and the tissue residency-associated gene CXCR6. The L5-LrNK-XCL1 subset showed low expression of KLRC2 (activating receptor gene) and high expression of KLRC1 and TIGIT (inhibitory receptor genes). These results suggested that the L4-LrNK-FCGR3A subset was associated with strong cytotoxic functions, whereas the L5-LrNK-XCL1 subset was associated with non-cytotoxic functions. Furthermore, our findings suggested that the L5-LrNK-XCL1 subset played a major role in regulating the proliferation and differentiation of lymphocytes. The L4 and L5 liver-resident NK cell subsets were present in healthy liver tissues, but the L4 subset was absent in HCC tissues. These results suggested that in liver cancer tissues, the absence of the L4 subset of NK cells affects the immunosurveillance and cytotoxicity of HCC cells.
A transitional NK cluster with intermediate expression levels of the signature genes in CD56bright or CD56dimCD57+ NK cells has been observed in human bone marrow and blood23. In this study, we identified the intermediate subtype of NK cells (L3-NK-HLA) with a phenotype between those of the CD56bright and CD56dim NK cell populations in healthy liver samples. In comparison with the CD56bright NK cells and CD56dim NK cells, the L3-NK-HLA cells exhibited intermediate transcriptional characteristics, according to the module score. This cluster showed high expression of HLA-DR, which was associated with NK cell activity. Gene Ontology biological process analysis suggested a cytotoxic role of the L3-NK-HLA cells. The L4-LrNK-FCGR3A and L3-NK-HLA clusters were found in only healthy liver tissues and were absent in the HCC tissues. This result suggested that the L4 and L3 NK cell subsets were relatively more active and represented cytotoxic NK cells, but were absent in the tumor tissues.
We also observed that the 4 prognosis-associated genes RHOB, TALDO1, HLA-DPA1, and TKT were simultaneously elevated in the tumor and peripheral blood in patients with HCC. HLA-DPA1 is highly associated with persistent HBV infections and related HCC tissues, according to a transcriptome-wide association study54. Moreover, higher HLA-DPA1 expression in the HBV-associated HCC tissues has been found to correlate with longer OS55. The analysis of these 4 prognostic genes in patient blood samples may provide a more precise prognosis for patients with HCC from an immunological perspective. A combination of tumor biomarkers and immunological biomarkers can improve prognostic prediction for patients with HCC. Further comprehensive analysis is required to evaluate the clinical utility of these 4 genes. Thus, transcriptome data coupled with clinical information may provide a deeper understanding of liver-infiltrating NK cells. In conclusion, our comprehensive single cell study revealed detailed characteristics of NK cells from healthy liver and HCC tissues, including the different subtypes and unique gene signatures, and their potential roles in immunity against HCC. Our study improves understanding of NK cell heterogeneity in the liver tissues of HC donors and patients with HCC, and provides new avenues for the development of more effective immunotherapies for HCC.
Conclusions
Our study provided a panoramic description of NK cell subsets through transcriptomic comparison of NK cells from blood, healthy liver, HCC tumor tissue, and tumor-adjacent tissue through scRNA-seq. We found that the cytotoxic NK cell subsets L3-NK-HLA and L4-LrNK-FCGR3A were absent in patients with HCC. Furthermore, we identified 4 potential non-invasive prognostic biomarkers (RHOB, TALDO1, HLA-DPA1, and TKT) for patients with HCC. The findings improve the understanding of liver NK heterogeneity and may contribute to the development of immunotherapy.
Supporting Information
Acknowledgements
The authors thank the personnel of the hospital that participated in this study, and particularly thank all volunteers involved.
Grant support
This work was supported by the National Key R&D Program of China (Grant Nos. 2021YFC2300601 and 2019YFA0508502/3), National Natural Science Foundation of China (Grant Nos. 81972679 and 8202290021), Anhui Provincial Natural Science Foundation (Grant Nos. 2008085J35 and 2008085MH252), and USTC Research Funds of the Double First-Class Initiative (Grant No. YD3520002002).
Conflict of interest statement
No potential conflicts of interest are disclosed.
Author contributions
Conceived and designed the analysis: Rui Sun, Cheng Sun.
Collected the data: Qiang Huang, Lianxin Liu, Björn Nashan.
Contributed data or analysis tools: Huan Liu, Rongrong Qin, Ronghua Zhao.
Performed the analysis: Huan Liu, Ronghua Zhao.
Wrote the paper: Huan Liu, Zhigang Tian, Haoyu Sun.
Data availability statement
The accession number for the raw and processed RNA-seq data reported in this paper is GEO GSE162616. Publicly available software used in this study is listed in the Supplementary Information.
References
- 1.Vivier E, Artis D, Colonna M, Diefenbach A, Di Santo JP, Eberl G, et al. Innate Lymphoid Cells: 10 Years On. Cell. 2018;174:1054–66. doi: 10.1016/j.cell.2018.07.017. [DOI] [PubMed] [Google Scholar]
- 2.Mace EM, Orange JS. Emerging insights into human health and NK cell biology from the study of NK cell deficiencies. Immunol Rev. 2019;287:202–25. doi: 10.1111/imr.12725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sun JC, Lanier LL. NK cell development, homeostasis and function: parallels with CD8(+) T cells. Nat Rev Immunol. 2011;11:645–57. doi: 10.1038/nri3044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang Q, Bi J, Zheng X, Chen Y, Wang H, Wu W, et al. Blockade of the checkpoint receptor TIGIT prevents NK cell exhaustion and elicits potent anti-tumor immunity. Nat Immunol. 2018;19:723–32. doi: 10.1038/s41590-018-0132-0. [DOI] [PubMed] [Google Scholar]
- 5.Zhang C, Hu Y, Xiao W, Tian Z. Chimeric antigen receptor- and natural killer cell receptor-engineered innate killer cells in cancer immunotherapy. Cell Mol Immunol. 2021;18:2083–100. doi: 10.1038/s41423-021-00732-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xue W, Zhang M. Updating targets for natural killer/T-cell lymphoma immunotherapy. Cancer Biol Med. 2021;18:52–62. doi: 10.20892/j.issn.2095-3941.2020.0400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu Z, Huang X. Cellular immunotherapy for hematological malignancy: recent progress and future perspectives. Cancer Biol Med. 2021;18:966–80. doi: 10.20892/j.issn.2095-3941.2020.0801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruf B, Heinrich B, Greten TF. Immunobiology and immunotherapy of HCC: spotlight on innate and innate-like immune cells. Cell Mol Immunol. 2021;18:112–27. doi: 10.1038/s41423-020-00572-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fang F, Xie S, Chen M, Li Y, Yue J, Ma J, et al. Advances in NK cell production. Cell Mol Immunol. 2022;19:460–81. doi: 10.1038/s41423-021-00808-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freud AG, Mundy-Bosse BL, Yu J, Caligiuri MA. The Broad Spectrum of Human Natural Killer Cell Diversity. Immunity. 2017;47:820–33. doi: 10.1016/j.immuni.2017.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Doherty DG, Norris S, Madrigal-Estebas L, McEntee G, Traynor O, Hegarty JE. The human liver contains multiple populations of NK cells, T cells, and CD3+CD56+ natural T cells with distinct cytotoxic activities and T1, T2, and T0 cytokine secretion patterns. J Immunol. 1999;163:2314–21. [PubMed] [Google Scholar]
- 12.Doherty DG, O’Farrelly C. Innate and adaptive lymphoid cells in the human liver. Immunol Rev. 2000;174:5–20. doi: 10.1034/j.1600-0528.2002.017416.x. [DOI] [PubMed] [Google Scholar]
- 13.Ahmed O, Robinson MW, O’Farrelly C. Inflammatory processes in the liver: divergent roles in homeostasis and pathology. Cell Mol Immunol. 2021;18:1375–86. doi: 10.1038/s41423-021-00639-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peng H, Jiang X, Chen Y, Sojka DK, Wei H, Gao X, et al. Liver-resident NK cells confer adaptive immunity in skin-contact inflammation. J Clin Invest. 2013;123:1444–56. doi: 10.1172/JCI66381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lunemann S, Martrus G, Goebels H, Kautz T, Langeneckert A, Salzberger W, et al. Hobit expression by a subset of human liver-resident CD56(bright) Natural Killer cells. Sci Rep. 2017;7:6676. doi: 10.1038/s41598-017-06011-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stegmann KA, Robertson F, Hansi N, Gill U, Pallant C, Christophides T, et al. CXCR6 marks a novel subset of T-bet(lo)Eomes(hi) natural killer cells residing in human liver. Sci Rep. 2016;6:26157. doi: 10.1038/srep26157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harmon C, Robinson MW, Fahey R, Whelan S, Houlihan DD, Geoghegan J, et al. Tissue-resident Eomes(hi) T-bet(lo) CD56(bright) NK cells with reduced proinflammatory potential are enriched in the adult human liver. Eur J Immunol. 2016;46:2111–20. doi: 10.1002/eji.201646559. [DOI] [PubMed] [Google Scholar]
- 18.Aw Yeang HX, Piersma SJ, Lin Y, Yang L, Malkova ON, Miner C, et al. Cutting Edge: Human CD49e- NK Cells Are Tissue Resident in the Liver. J Immunol. 2017;198:1417–22. doi: 10.4049/jimmunol.1601818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hudspeth K, Donadon M, Cimino M, Pontarini E, Tentorio P, Preti M, et al. Human liver-resident CD56(bright)/CD16(neg) NK cells are retained within hepatic sinusoids via the engagement of CCR5 and CXCR6 pathways. J Autoimmun. 2016;66:40–50. doi: 10.1016/j.jaut.2015.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sun Y, Zhou J, Fan J, Yang X. Single-cell RNA sequencing reveals spatial heterogeneity and immune evasion of circulating tumor cells. Cancer Biology & Medicine. 2021;18:934–6. doi: 10.20892/j.issn.2095-3941.2021.0466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang L, Mo S, Li X, He Y, Yang J. Single-cell RNA-seq reveals the immune escape and drug resistance mechanisms of mantle cell lymphoma. Cancer Biol Med. 2020;17:726–39. doi: 10.20892/j.issn.2095-3941.2020.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Papalexi E, Satija R. Single-cell RNA sequencing to explore immune cell heterogeneity. Nat Rev Immunol. 2018;18:35–45. doi: 10.1038/nri.2017.76. [DOI] [PubMed] [Google Scholar]
- 23.Yang C, Siebert JR, Burns R, Gerbec ZJ, Bonacci B, Rymaszewski A, et al. Heterogeneity of human bone marrow and blood natural killer cells defined by single-cell transcriptome. Nat Commun. 2019;10:3931. doi: 10.1038/s41467-019-11947-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith SL, Kennedy PR, Stacey KB, Worboys JD, Yarwood A, Seo S, et al. Diversity of peripheral blood human NK cells identified by single-cell RNA sequencing. Blood Adv. 2020;4:1388–406. doi: 10.1182/bloodadvances.2019000699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crinier A, Milpied P, Escaliere B, Piperoglou C, Galluso J, Balsamo A, et al. High-Dimensional Single-Cell Analysis Identifies Organ-Specific Signatures and Conserved NK Cell Subsets in Humans and Mice. Immunity. 2018;49:971–86 e5. doi: 10.1016/j.immuni.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 27.Sun D, Li H, Cao M, He S, Lei L, Peng J, et al. Cancer burden in China: trends, risk factors and prevention. Cancer Biol Med. 2020;17:879–95. doi: 10.20892/j.issn.2095-3941.2020.0387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Villanueva A. Hepatocellular Carcinoma. N Engl J Med. 2019;380:1450–62. doi: 10.1056/NEJMra1713263. [DOI] [PubMed] [Google Scholar]
- 29.MacParland SA, Liu JC, Ma XZ, Innes BT, Bartczak AM, Gage BK, et al. Single cell RNA sequencing of human liver reveals distinct intrahepatic macrophage populations. Nat Commun. 2018;9:4383. doi: 10.1038/s41467-018-06318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhao J, Zhang S, Liu Y, He X, Qu M, Xu G, et al. Single-cell RNA sequencing reveals the heterogeneity of liver-resident immune cells in human. Cell Discovery. 2020;6:22. doi: 10.1038/s41421-020-0157-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sun Y, Wu L, Zhong Y, Zhou K, Hou Y, Wang Z, et al. Single-cell landscape of the ecosystem in early-relapse hepatocellular carcinoma. Cell. 2021;184:404–21 e16. doi: 10.1016/j.cell.2020.11.041. [DOI] [PubMed] [Google Scholar]
- 32.Zhang Q, He Y, Luo N, Patel SJ, Han Y, Gao R, et al. Landscape and Dynamics of Single Immune Cells in Hepatocellular Carcinoma. Cell. 2019;179:829–45 e20. doi: 10.1016/j.cell.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 33.Stuart T, Butler A, Hoffman P, Hafemeister C, Papalexi E, Mauck WM, 3rd, et al. Comprehensive Integration of Single-Cell Data. Cell. 2019;177:1888–902 e21. doi: 10.1016/j.cell.2019.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Butler A, Hoffman P, Smibert P, Papalexi E, Satija R. Integrating single-cell transcriptomic data across different conditions, technologies, and species. Nat Biotechnol. 2018;36:411–20. doi: 10.1038/nbt.4096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mazzurana L, Czarnewski P, Jonsson V, Wigge L, Ringner M, Williams TC, et al. Tissue-specific transcriptional imprinting and heterogeneity in human innate lymphoid cells revealed by full-length single-cell RNA-sequencing. Cell Res. 2021;31:554–68. doi: 10.1038/s41422-020-00445-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bjorklund AK, Forkel M, Picelli S, Konya V, Theorell J, Friberg D, et al. The heterogeneity of human CD127(+) innate lymphoid cells revealed by single-cell RNA sequencing. Nat Immunol. 2016;17:451–60. doi: 10.1038/ni.3368. [DOI] [PubMed] [Google Scholar]
- 37.Traag VA, Waltman L, van Eck NJ. From Louvain to Leiden: guaranteeing well-connected communities. Sci Rep. 2019;9:5233. doi: 10.1038/s41598-019-41695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haghverdi L, Lun ATL, Morgan MD, Marioni JC. Batch effects in single-cell RNA-sequencing data are corrected by matching mutual nearest neighbors. Nat Biotechnol. 2018;36:421–7. doi: 10.1038/nbt.4091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Scheiter M, Lau U, van Ham M, Bulitta B, Grobe L, Garritsen H, et al. Proteome analysis of distinct developmental stages of human natural killer (NK) cells. Mol Cell Proteomics. 2013;12:1099–114. doi: 10.1074/mcp.M112.024596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yu J, Mao HC, Wei M, Hughes T, Zhang J, Park IK, et al. CD94 surface density identifies a functional intermediary between the CD56bright and CD56dim human NK-cell subsets. Blood. 2010;115:274–81. doi: 10.1182/blood-2009-04-215491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Erokhina SA, Streltsova MA, Kanevskiy LM, Grechikhina MV, Sapozhnikov AM, Kovalenko EI. HLA-DR-expressing NK cells: Effective killers suspected for antigen presentation. J Leukoc Biol. 2021;109:327–37. doi: 10.1002/JLB.3RU0420-668RR. [DOI] [PubMed] [Google Scholar]
- 42.Erokhina SA, Streltsova MA, Kanevskiy LM, Telford WG, Sapozhnikov AM, Kovalenko EI. HLA-DR(+) NK cells are mostly characterized by less mature phenotype and high functional activity. Immunol Cell Biol. 2018;96:212–28. doi: 10.1111/imcb.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hanna J, Bechtel P, Zhai Y, Youssef F, McLachlan K, Mandelboim O. Novel insights on human NK cells’ immunological modalities revealed by gene expression profiling. J Immunol. 2004;173:6547–63. doi: 10.4049/jimmunol.173.11.6547. [DOI] [PubMed] [Google Scholar]
- 44.Sun H, Liu L, Huang Q, Liu H, Huang M, Wang J, et al. Accumulation of Tumor-Infiltrating CD49a(+) NK Cells Correlates with Poor Prognosis for Human Hepatocellular Carcinoma. Cancer Immunol Res. 2019;7:1535–46. doi: 10.1158/2326-6066.CIR-18-0757. [DOI] [PubMed] [Google Scholar]
- 45.Pan D, Kobayashi A, Jiang P, Ferrari de Andrade L, Tay RE, Luoma AM, et al. A major chromatin regulator determines resistance of tumor cells to T cell-mediated killing. Science. 2018;359:770–5. doi: 10.1126/science.aao1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paijens ST, Vledder A, de Bruyn M, Nijman HW. Tumor-infiltrating lymphocytes in the immunotherapy era. Cell Mol Immunol. 2021;18:842–59. doi: 10.1038/s41423-020-00565-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang Y, Zhang Z. The history and advances in cancer immunotherapy: understanding the characteristics of tumor-infiltrating immune cells and their therapeutic implications. Cell Mol Immunol. 2020;17:807–21. doi: 10.1038/s41423-020-0488-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aizarani N, Saviano A, Sagar X, Mailly L, Durand S, Herman JS, et al. A human liver cell atlas reveals heterogeneity and epithelial progenitors. Nature. 2019;572:199–204. doi: 10.1038/s41586-019-1373-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang L, Li J, He S, Liu Y, Chen H, He S, et al. Resolving the graft ischemia-reperfusion injury during liver transplantation at the single cell resolution. Cell Death Dis. 2021;12:589. doi: 10.1038/s41419-021-03878-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sun C, Xu J, Huang Q, Huang M, Wen H, Zhang C, et al. High NKG2A expression contributes to NK cell exhaustion and predicts a poor prognosis of patients with liver cancer. Oncoimmunology. 2017;6:e1264562. doi: 10.1080/2162402X.2016.1264562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sun H, Huang Q, Huang M, Wen H, Lin R, Zheng M, et al. Human CD96 Correlates to Natural Killer Cell Exhaustion and Predicts the Prognosis of Human Hepatocellular Carcinoma. Hepatology. 2019;70:168–83. doi: 10.1002/hep.30347. [DOI] [PubMed] [Google Scholar]
- 52.Yu L, Liu X, Wang X, Yan F, Wang P, Jiang Y, et al. TIGIT(+) TIM-3(+) NK cells are correlated with NK cell exhaustion and disease progression in patients with hepatitis B virusrelated hepatocellular carcinoma. Oncoimmunology. 2021;10:1942673. doi: 10.1080/2162402X.2021.1942673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jameson G, Robinson MW. Insights Into Human Intrahepatic NK Cell Function From Single Cell RNA Sequencing Datasets. Front Immunol. 2021;12:649311. doi: 10.3389/fimmu.2021.649311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Han J, Chen C, Wang C, Qin N, Huang M, Ma Z, et al. Transcriptome-wide association study for persistent hepatitis B virus infection and related hepatocellular carcinoma. Liver Int. 2020;40:2117–27. doi: 10.1111/liv.14577. [DOI] [PubMed] [Google Scholar]
- 55.Wang XK, Liao XW, Yang CK, Yu TD, Liu ZQ, Gong YZ, et al. Diagnostic and prognostic biomarkers of Human Leukocyte Antigen complex for hepatitis B virus-related hepatocellular carcinoma. J Cancer. 2019;10:5173–90. doi: 10.7150/jca.29655. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The accession number for the raw and processed RNA-seq data reported in this paper is GEO GSE162616. Publicly available software used in this study is listed in the Supplementary Information.