Abstract
Background
To evaluate the clinical, functional, radiographic, and survival outcomes in patients undergoing reverse total shoulder arthroplasty (RSA) with uncemented stem fixation for proximal humerus fractures.
Materials and Methods
This is a retrospective cohort study that evaluated a consecutive series of patients with proximal humerus fractures undergoing RSA. Clinical data, radiographs, and re-operation rates were reviewed in patients selected for uncemented stem fixation. The same parameters were compared to the remainder of the cohort undergoing cemented stem fixation.
Results
The uncemented group (n = 16, median total follow-up = 108 weeks) and cemented group (n = 12, median total follow-up = 223 weeks, p = 0.110) did not differ statistically in pre-operative demographic, post-operative outcomes or incidence of complications. Two patients (12.5%) in the uncemented group required a reoperation (Week 52 and 180) versus none in the cemented group.
Conclusion
Uncemented stem fixation in RSA for proximal humerus fractures does not yield worse results than cemented stem fixation in properly selected patients. Prospective non-inferiority trials comparing outcomes are recommended.
Keywords: proximal humerus fracture, shoulder arthroplasty, reverse arthroplasty for fracture, uncemented stem fixation, cemented stem fixation, humerus
Introduction
Proximal humerus fractures account for approximately 5% of fractures in the adult population and continue to rise as a leading fragility fracture.1,2 Displaced three and four part fractures often present an especially challenging situation in the setting of osteoporotic bone. Recently there has been a trend toward treating these fractures with reverse total shoulder arthroplasty (RSA), rather than hemiarthroplasty or open reduction and internal fixation (ORIF). 3 While the topic remains controversial, there is sufficient evidence to support acceptable outcomes with RSA. 4
Various techniques are available for RSA in the setting of fracture.4,5 Most agree that one of the challenges in comparison to RSA for arthritis is tuberosity management and fixation. Successful tuberosity reduction and healing is felt to result in better functional outcomes. 6 However, tuberosity failure in RSA typically will still result in a functional shoulder, unlike that seen with hemiarthroplasty. Most published literature available on RSA for fracture describes various techniques utilizing a cemented stem.7–10 While uncemented press fit stems have gained popularity for use in degenerative conditions, there is less evidence for their use in a fracture scenario. 11
To evaluate the success of uncemented stem fixation in properly selected patients undergoing RSA for proximal humerus fractures, we analyzed a retrospective cohort of patients of a single surgeon's experience using either cemented and uncemented stems for 3- and 4-part proximal humerus fractures. We hypothesize that there will not be any significant differences in post-surgical clinical, functional or radiological outcomes or incidence of complications in properly selected patients undergoing RSA with uncemented stem fixation for proximal humerus fractures compared to patients selected for cemented stem fixation.
Materials and Methods
This study was approved by the University at Buffalo Institutional Review Board and an exempt of consent was obtained(Approval ID MODCR00004866). Procedural and diagnostic codes were used to identify all patients treated with RSA for proximal humerus fractures by a single shoulder and elbow fellowship trained surgeon at a Level 1 trauma center from 2010–2018.
Study Population
Male and female adults (aged ≥ 18 years) undergoing RSA for acute three and four part fractures, fracture-dislocations and head split patterns were included. Patients sustaining pathologic fractures, sustaining a second contralateral proximal humerus fracture within one year, undergoing delayed treatment for proximal humerus fracture (greater than one month from injury), or with less than one year of clinical follow up were excluded. All of the patients reviewed and those ultimately included in the study were treated with the same implant system. The senior author initially performed cemented stem fixation for all RSA performed for fracture for the first three years of his career (2010-2013) and later shifted to uncemented stem fixation for indicated cases (2013-2018). The indication for uncemented stem fixation is described in the surgical technique section. From 2013–2018, 5 out of 20 patients were treated with cemented stems.
Measures and Study Definitions
Demographic information, injury details, surgical details, and clinical follow up information were reviewed for all patients. Demographic details collected included age at time of injury, body mass index (BMI), hand dominance, dominant sided fracture, and American Society of Anesthesiologist Physical Status (ASA) score. Preoperative radiographs were reviewed for all patients and fractures were classified according to the Neer and Orthopaedic Trauma Association (OTA) classifications.12,13 The presence of tuberosity comminution (defined as 2 or more fragments of either the lesser or greater tuberosity of > 1 cm on any radiograph) were documented. Post-operative clinical follow up notes were reviewed to record range of motion (ROM) at the most recent follow-up. Post-operative patient reported outcomes such as the Quick Dash functional score, American Shoulder and Elbow Society (ASES) score and Visual Analogue Scale (VAS) were obtained. Post-operative radiographs were reviewed to evaluate tuberosity healing. Tuberosity healing was documented as one of three categories based on routine sets of AP, true AP, Y lateral and axillary radiographs: healed, nonunion or resorption. Tuberosities were considered healed if they were present and healed in a position unchanged from initial post-operative radiographs. Representative radiographs for tuberosity healing are shown in Figure 1. Nonunion was defined as a tuberosity that migrated from initial position. Resorption was defined as no remaining tuberosity. Any evidence of obvious stem loosening such as change in stem position or subsidence was documented. Reoperations for any reason were recorded.
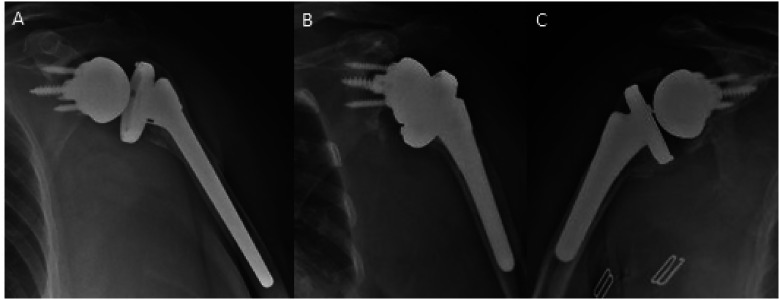
Figure 1.
Tuberosity healing radiographs.
Three classifications of tuberosity healing shown in figure 1 show a healed tuberosity in anatomic position (A), a completely resorbed tuberosity (B), and a tuberosity nonunion (C).
Surgical Technique
A standard deltopectoral approach is used to expose the proximal humerus. The tuberosity fragments are secured with non-absorbable sutures. The humeral articular surface is then excised and the extent of the calcar attached to the articular surface is measured to help determine the appropriate height of the humeral stem. The humerus is mobilized. The remaining bone in the humeral shaft is then evaluated to determine if there is sufficient bone stock for press-fit fixation of the humeral component. Typically, this requires at least 50% of the calcar height remaining attached to the humeral shaft and the lateral aspect of the fracture cannot extend into the diaphysis. Figure 2 demonstrates a case unsuitable for an uncemented prosthesis with distal fracture extension. The humeral canal is then reamed until there is cortical contact in the diaphysis. Prior to broaching, a cerclage is placed around the proximal humerus at the junction between the metaphysis and the diaphysis, with two non-absorbable #5 sutures using a racking stitch. The humeral canal is broached using 1 mm increments until a broach is seated at the appropriate height based on the remaining proximal humeral calcar. Stability of the broach is tested using axial traction and rotation of the broach handle. If the broach is stable to axial and rotational forces then an uncemented press-fit stem is suitable for the case. If axial and rotational stability of the broach are not able to be obtained at an appropriate height then cementation of the stem is performed utilizing the previously described black and tan technique. 14 The final decision for uncemented or cemented stem fixation is made intra-operatively, therefore, appropriate instruments and implants for each technique are always available at the time of surgery. After completion of the preliminary preparation of the humerus and decision for cemented or uncemented stem fixation, attention is directed to the glenoid preparation.
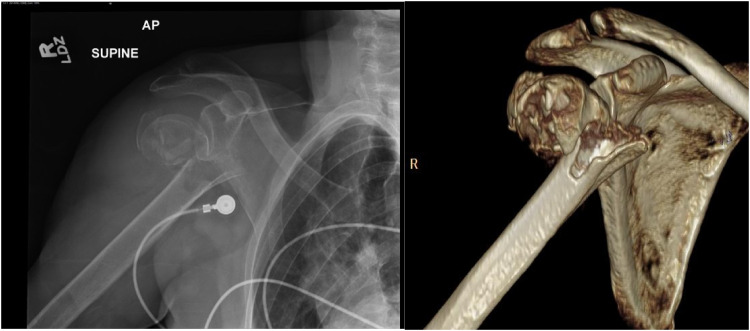
Figure 2.
Unsuitable case for uncemented fixation.
An AP radiograph and 3D CT reconstruction are shown in figure 2 which demonstrate a fracture with distal extension making an unsuitable case for uncemented fixation.
The glenoid is exposed. It is important to be careful while reaming to try to retain the subchondral plate and avoid entering the cancellous bone of the glenoid. Baseplate fixation is obtained with screws. Glenosphere size and offset are selected based on the patient's anatomy to allow for 2–3 mm of overhang around the inferior, anterior and posterior aspects of the glenoid to prevent impingement.
Following completion of the glenoid, implantation of the humeral broach is again evaluated to ensure stability to axial and rotational forces. The trial humeral bearing surface is placed on the broach and the shoulder is reduced. The shoulder is tested for ROM and stability. The tuberosity fragments are reduced anatomically to the humeral shaft. It is important to ensure contact between the humeral shaft and the tuberosity fragments to allow for healing. If stable, the broach is removed and the appropriate sized final humeral implant is impacted into the humeral canal at 30 degrees of retroversion. The stem used is a metaphyseal press-fit stem that typically gets fixation at the metaphyseal-diaphyseal junction. Diaphyseal fixation was avoided to reduce the risk of proximal stress shielding. The humeral bearing surface is trialed with the final stem in place.
Tuberosity repair is performed in three steps: reduction, bone grafting and fixation. Reduction requires contact between the tuberosity fragments and the humeral shaft and to each other. Bone graft from the humeral head is used to augment the tuberosity repair. The tuberosities are fixed using three steps: fixation to the stem, horizontal compression and vertical compression. After completion of tuberosity fixation there should be no movement between the humeral shaft and the tuberosity fragments with ROM. Representative images for a cemented and uncemented prosthesis are shown in Figure 3. The deltopectoral interval and skin are closed in standard fashion.
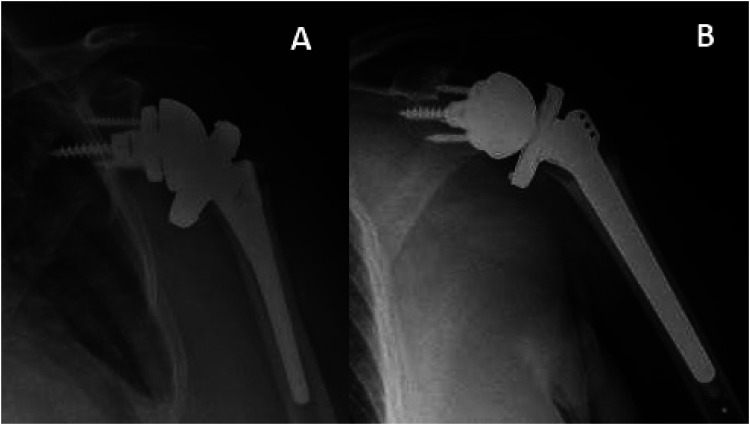
Figure 3.
Reverse total shoulder arthroplasty with cemented and uncemented stem.
Figure 2 shows a reverse total shoulder arthroplasty with uncemented stem fixation (A) and with cemented stem fixation (B).
Patients are placed in a sling and swath immobilizer for six weeks after surgery. During this time the patients are allowed to remove their arm from the immobilizer for hygiene activities and when sedentary but are discouraged from using the arm for activities. Patients are instructed on a home exercise program consisting of elbow, wrist and hand ROM exercises and shoulder pendulums and begin these as pain allows. A formal physical therapy program is initiated at two weeks for passive and active assisted ROM. Radiographs are evaluated at 6 weeks and patients are allowed to begin full active ROM and light activities if there are signs of early healing of the tuberosities such as bridging bone at the interface between the tuberosity and humeral shaft. At 3 months patients begin strengthening and progress activity as tolerated.
Statistical Analysis
Patients were categorized in the following groups based on surgery type: Cemented and Uncemented RSA. Groupwise comparisons were performed, normally distributed continuous variables were compared using an independent samples t-test, non-normally distributed continuous variables were compared using a non-parametric t-test, and categorical variables were compared using χ2 test (Fisher's Exact for group n <5). Groups were compared on initial presentation characteristics and post-surgical outcomes. Since duration of follow-up varied between patients, correlation between duration of follow-up and post-surgical outcomes was calculated. A Kaplan Meier life table stratified by surgery type was made for post-surgical complications and patients were censored on their last follow-up visit. A Log-rank test was performed to compare the equity of survival functions. A p-value of 0.05 was considered significant and statistical analysis was performed using SPSS Version 25.
Results
Thirty-nine patients underwent total RSA for humerus fractures between 2010 to 2018. However, 8 patients had follow-up for less than one year, 2 patients had delayed treatment (greater than one month since fracture) and 1 sustained a second contralateral proximal humerus fracture within one year and were excluded. Hence, 28 patients are included in the analysis. In the included sample, 16 patients were treated with uncemented RSA stems and 12 were treated with cemented RSA stems. Group wise patient demographic and pre-surgery clinical characteristics are presented in Table 1, and fracture characteristics in Table 2. No significant differences in age, sex or medical history were observed. The uncemented group had a higher incidence of current smokers and patients with history of cerebral vascular disease (CVD), but they did not reach statistical significance.
Table 1.
Groupwise demographic and Pre-surgery clinical characteristics.
| Uncemented
rTSA n = 16 |
Cemented
rTSA n = 12 |
p-value | |
|---|---|---|---|
| Age in years | 73.94 ± 8.5 | 74.92 ± 8.6 | 0.768 |
| Sex | 15 female, 1 male | 10 female, 2 male | 0.560 |
| Dominant Side | 15 right, 1 left | 12 right | >0.999 |
| Height in m | 1.58 ± 0.070 | 1.63 ± 0.084 | 0.105 |
| Weight in kg | 77.47 ± 11.9 | 76.33 ± 17.7 | 0.840 |
| Tobacco use | 5 current smokers, 5 previous smokers | 0 current smokers, 8 previous smokers | 0.060 |
| CVD | 9/16 | 2/12 | 0.054 |
| PVD | 2/16 | 1/12 | >0.999 |
| Diabetes Mellitus | 2/16 | 2/12 | >0.999 |
| Surgical Side | 7 right, 9 left | 4 right, 8 left | 0.705 |
| Tuberosity Bone Graft | 7/16 yes | 6/12 yes | 0.743 |
| Antibiotic Cement Type | - | 9 Vancomycin, 3 Gentamycin | - |
| ASA Classification | 0.569 | ||
| 2 | 5 | 5 | |
| 3 | 11 | 7 | |
Table 2.
Groupwise fracture classification.
| Uncemented RSA n = 16 |
Cemented RSA n = 12 |
p-value* | |
|---|---|---|---|
| Neer Fracture Classification | 12 4-Part, 4 3-Part | 10 4-Part, 2 3-Part | 0.673 |
| OTA Classification | 12 11-C3, 4 11-B1 | 10 11-C3, 2 11-B1 | 0.673 |
| Head-Split Pattern | 12 Yes, 4 No | 2 Yes, 10 No | >0.999 |
| Fracture-Dislocation | 7 Yes, 9 No | 2 Yes, 10 No | 0.233 |
| Tuberosity Comminution | 7 Yes, 9 No | 7 Yes, 5 No |
*Fisher's Exact Test, 2-sided
Group wise post-surgical outcomes are presented in Table 3. The uncemented group had a median follow-up duration of 108 weeks and the cemented group had a median duration of 223 weeks which was not statistically different. There were also no statistically significant differences between the two groups in QuickDASH, ASES, VAS pain, or greater tuberosity healing at final follow-up. Additionally, duration of follow-up did not correlate with QuickDASH (r = −0.147, p = 0.484), ASES (r = 0.079, p = 0.734) or greater tuberosity healing (r = 0.258, p = 0.185). There was a clinically relevant difference in favor of the cemented group in the Quick Dash (30.8 ± 18.6 vs 41.24 ± 25; p = 0.259) and ASES scores (74.26 ± 20.4 vs 58.44 ± 26.4; p = 0.144), however, they did not reach statistical significance. Patients in the uncemented group had a difference in median forward elevation (160 vs 140 degrees, p = 0.507). Patients in the cemented group did tend to have a clinically, but not statistically significant difference in ability to internally rotate beyond the lumbosacral junction. Radiographic review at final follow-up did not demonstrate a difference in tuberosity healing or resorption between the cemented and uncemented groups. There was no evidence of humeral component loosening or failure of fixation of the humeral component in either group.
Table 3.
Groupwise Post-operative outcomes.
| Uncemented RSA n = 16 |
Cemented RSA n = 12 |
p-value | |
|---|---|---|---|
| Maximum length of follow-up, median (IQR), range | 108 weeks (59.75, 184.5) (Range 53-274 weeks) |
223 weeks (103.5, 282) (Range 54-371 weeks) |
0.110 |
| Complications | 1 infection of prosthetic device (Week 180) and 1 Revision of Tuberosity Nonunion (Week 52) | None | 0.492 |
| QuickDASH | 41.24 ± 25 | 30.8 ± 18.6 | 0.259 |
| ASES | 58.44 ± 26.4 | 74.26 ± 20.4 | 0.144 |
| Visual Analog Score (VAS) | 0.5 (0, 3.75) | 0 (0, 4) | 0.525 |
| Tuberosity Comminution | 7/16 yes | 7/12 yes | 0.445 |
| Greater Tuberosity Healing | 0.283 | ||
| Healed Anatomic | 10 | 4 | |
| Nonunion | 2 | 2 | |
| Resorption | 4 | 6 | |
| Forward Elevation (degrees) | 160 (120, 160) | 140 (112.5, 157.5) | 0.507 |
| External Rotation (degrees) | 40 (30, 50) | 37.5 (25, 43.75) | 0.347 |
| Post-op Internal Rotation | 15 between T4-LS junction, 1 below LS junction | 7 between T4-LS junction, 5 below LS junction | 0.057 |
Follow-up (in weeks), VAS and ROM presented as median (inter-quartile range) and compared using non-parametric t-test.
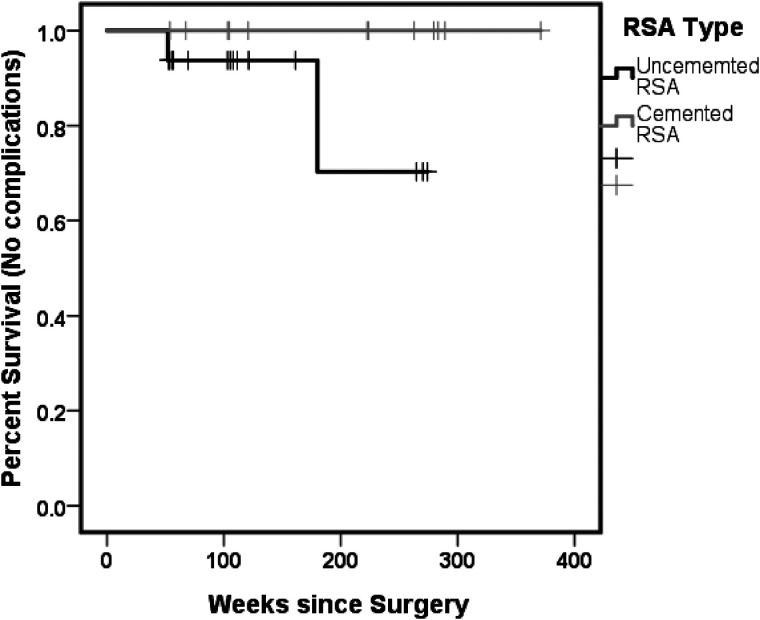
A Kaplan Meier graph comparing incidence of complications since surgery stratified by surgery type is presented in Figure 4. There was no significant difference in the equity of survival between groups on a Log-rank test (p = 0.123). There were two reoperations in the uncemented group: one for infection and one for tuberosity nonunion with contracture. There were no reoperations in the cemented group.
Figure 4.
Kaplan Meier survival graph between groups log rank test is not significantly different between groups (χ2 = 2.381, p = 0.123).
Discussion
This study presents a single surgeon's experience in using both cemented and uncemented stem fixation in RSA for proximal humerus fractures. In this study, no statistically significant difference in survival or patient reported outcome measures was found between the two groups at final follow up. Two patients in the uncemented group did undergo a reoperation. One patient was a 65-year-old male that sustained a posterior fracture dislocation from a seizure that underwent an uncemented RSA. He developed a deep infection 3.5 years following the index surgery, which was treated with implant removal and placement of an articulating antibiotic cement spacer. The patient was lost to follow up after six months, and to our knowledge has retained his spacer for two years with no recurrence of infection or reimplantation surgery. The other patient was a 71-year-old female that sustained a head splitting proximal humerus fracture that underwent uncemented RSA. She continued with post-operative pain and limited ROM. Radiographs and CT scan imaging suggested nonunion of her tuberosities in unfavorable position contributing to limited ROM from impingement. At 1-year post-op, she underwent a contracture release with excision of tuberosity fragments. One year following her revision surgery her pain was minimal, though she continued with decreased ROM.
Like other reports in the literature, we did not find a difference in major complications between patients undergoing cemented versus uncemented stem fixation in RSA for proximal humerus fractures. Phadnis et al performed a meta-analysis comparing cemented versus uncemented stems in RSA for any reason. 15 They compared 1455 patients in a cemented group with 329 in the uncemented group from 41 studies for similar clinical and radiographic outcomes. The study did have some limitations, most notably variable rates of outcomes reported among the different studies. Wiater et al performed a retrospective cohort study evaluating the use of cemented and uncemented stem fixation for RSA specifically performed for rotator cuff tear arthropathy or severe cuff deficiency. At two to five year follow up, they found no evidence of stem loosening in either group, and no difference in other outcomes between groups. 16 Wright et al reported on a case series of 30 patients that underwent RSA for proximal humerus fractures using only uncemented stem fixation by two surgeons. They reported major complications in 2/30 patients including an intraoperative periprosthetic fracture that later persisted with a loose stem and an acromial fracture at 4.5 years post op. 17 Seung-Min Youn et al reported a case series of 33 patients that underwent uncemented stem fixation RSA for proximal humerus fractures performed by three surgeons and found no major complications including stem loosening. They reported favorable functional and radiographic outcome measures. 18 Similarly our study did not demonstrate any failure of fixation following RSA for fracture with an uncemented humeral component.
Though not statistically significant, there was a trend toward better functional outcomes in the cemented group. Patients with a cemented stem did have improved Dash and ASES scores (Dash 41.24 ± 25 vs 30.8 ± 18.6; p = 0.259 and ASES scores 58.44 ± 26.4 vs 74.26 ± 20.4; p = 0.144). However, patients in the uncemented group trended toward better forward elevation. The lack of statistical difference may be due to the small sample size.
Our study presents comparable results for uncemented and cemented stem fixation in RSA performed for proximal humerus fractures in the elderly population in terms of complications or failures. Though not statistically significant, there was a trend toward better functional outcomes in the cemented group. Patients with a cemented stem did have improved QuickDash and ASES scores (QuickDash 30.8 ± 18.6 vs 41.24 ± 25; p = 0.259) and ASES scores (74.26 ± 20.4 vs 58.44 ± 26.4; p = 0.144). However, patients in the uncemented group trended toward better forward elevation.
In this series, patients received a RSA with either cemented or uncemented stems using the same technique and implant system by the same surgeon. Our results provide valuable data to the existing literature regarding favorable survival of uncemented stem fixation in RSA at mid-term follow up in properly selected patients.
This study does have several limitations. Most data was collected retrospectively. The uncemented group is made of patients in a later part of the senior author's career and may be influenced by a more experienced surgeon at this time point. It is important to note that the main objective of the study was to evaluate the success of uncemented stem fixation in patients selected for an uncemented stem. The study was not designed to compare cemented versus uncemented stems in all proximal humerus fractures, as some patients are selected for cemented stem fixation based on the criteria described in the surgical technique section. The study population is small and the differences observed in outcomes that did not reach statistical significance may be due to the lack of power in this study. Functional outcome scores were not available for all patients included in the study. However, the number of patients and mean follow up for our cohort is well within the range of recently published series. Unfortunately, long term follow up (>5years) may prove difficult to obtain in this population of elderly patients. The study period was before there was a fracture stem available in the United States, and therefore may not be reproducible. Additionally, there are multiple press fit stems available which obtain fit in different regions of the humerus.
Conclusion
Despite these limitations, our study would suggest relative safety in using uncemented stem fixation in RSA for indicated proximal humerus fractures in the elderly population performed by an experienced surgeon. This data adds to the growing support in the literature for uncemented stem use. Long term data and randomized trials would be beneficial to further evaluate this technique.
Footnotes
Author Contributions: All authors contributed to the study conception and design. Material preparation, data collection and analysis was performed by all authors. The first draft of the manuscript was written by Elias Joseph MD and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethical Standard Statement: The study was approved by an institution review board. A waiver of consent was obtained.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Elias G. Joseph https://orcid.org/0000-0001-5253-2381
References
- 1.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. DOI: 10.1016/j.injury.2006.04.130 [DOI] [PubMed] [Google Scholar]
- 2.Kim SH, Szabo RM, Marder RA. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res (Hoboken). 2012;64:407–414. DOI: 10.1002/acr.21563 [DOI] [PubMed] [Google Scholar]
- 3.Gomberawalla MM, Miller BS, Coale RM, et al. Meta-analysis of joint preservation versus arthroplasty for the treatment of displaced 3- and 4-part fractures of the proximal humerus. Injury. 2013;44:1532–1539. DOI: 10.1016/j.injury.2013.03.030 [DOI] [PubMed] [Google Scholar]
- 4.Yahuaca BI, Simon P, Christmas KN, et al. Acute surgical management of proximal humerus fractures: ORIF vs. hemiarthroplasty vs. reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2020;29:S32–s40. DOI: 10.1016/j.jse.2019.10.012 [DOI] [PubMed] [Google Scholar]
- 5.Holton J, Yousri T, Arealis G, et al. The role of reverse shoulder arthroplasty in management of proximal humerus fractures with fracture sequelae: a systematic review of the literature. Orthop Rev (Pavia). 2017;9:6977. DOI: 10.4081/or.2017.6977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ohl X, Bonnevialle N, Gallinet D, et al. How the greater tuberosity affects clinical outcomes after reverse shoulder arthroplasty for proximal humeral fractures. J Shoulder Elbow Surg. 2018;27:2139–2144. DOI: 10.1016/j.jse.2018.05.030 [DOI] [PubMed] [Google Scholar]
- 7.Werthel JD, Sirveaux F, Block D. Reverse shoulder arthroplasty in recent proximal humerus fractures. Orthop Traumatol Surg Res. 2018;104:779–785. DOI: 10.1016/j.otsr.2018.07.003 [DOI] [PubMed] [Google Scholar]
- 8.Imiolczyk JP, Moroder P, Scheibel M. Fracture-Specific and Conventional Stem Designs in Reverse Shoulder Arthroplasty for Acute Proximal Humerus Fractures-A Retrospective, Observational Study. J Clin Med. 2021;10:175. 10.3390/jcm10020175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cagle PJ, Jr., Reizner W, Parsons BO. A technique for humeral prosthesis placement in reverse total shoulder arthroplasty for fracture. Shoulder Elbow. 2019;11:459–464. DOI: 10.1177/1758573218793904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeong JJ, Kong CG, Park SE, et al. Non-fracture stem vs fracture stem of reverse total shoulder arthroplasty in complex proximal humeral fracture of Asian elderly. Arch Orthop Trauma Surg. 2019;139:1649–1657. DOI: 10.1007/s00402-019-03190-y [DOI] [PubMed] [Google Scholar]
- 11.King JJ, Farmer KW, Struk AM, et al. Uncemented versus cemented humeral stem fixation in reverse shoulder arthroplasty. Int Orthop. 2015;39:291–298. DOI: 10.1007/s00264-014-2593-6 [DOI] [PubMed] [Google Scholar]
- 12.Neer CS, 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 13.Meinberg EG, Agel J, Roberts CS, et al. Fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018;32(Suppl 1):S1–S170. DOI: 10.1097/BOT.0000000000001063 [DOI] [PubMed] [Google Scholar]
- 14.Formaini NT, Everding NG, Levy JC, et al. Tuberosity healing after reverse shoulder arthroplasty for acute proximal humerus fractures: the “black and tan” technique. J Shoulder Elbow Surg. 2015;24:e299–e306. DOI: 10.1016/j.jse.2015.04.014 [DOI] [PubMed] [Google Scholar]
- 15.Phadnis J, Huang T, Watts A, et al. Cemented or cementless humeral fixation in reverse total shoulder arthroplasty? A systematic review. Bone Joint J. 2016;98–b:65–74. DOI: 10.1302/0301-620x.98b1.36336 [DOI] [PubMed] [Google Scholar]
- 16.Wiater JM, Moravek JE, Jr., Budge MD, et al. Clinical and radiographic results of cementless reverse total shoulder arthroplasty: a comparative study with 2 to 5 years of follow-up. J Shoulder Elbow Surg 2014; 23: 1208–1214. DOI: 10.1016/j.jse.2013.11.032. [DOI] [PubMed] [Google Scholar]
- 17.Wright JO, Ho A, Kalma J, et al. Uncemented reverse total shoulder arthroplasty as initial treatment for comminuted proximal humerus fractures. J Orthop Trauma. 2019;33:e263–e269. DOI: 10.1097/BOT.0000000000001465 [DOI] [PubMed] [Google Scholar]
- 18.Youn SM, Deo S, Poon PC. Functional and radiologic outcomes of uncemented reverse shoulder arthroplasty in proximal humeral fractures: cementing the humeral component is not necessary. J Shoulder Elbow Surg. 2016;25:e83–e89. DOI: 10.1016/j.jse.2015.09.007 [DOI] [PubMed] [Google Scholar]