Abstract
Uterine fibroids are associated with heavy menstrual bleeding, abdominal discomfort, subfertility and a reduced quality of life. The present study reported a case series of life-threatening anemia with hemoglobin levels <2.0 g/dl caused by uterine fibroids and genital bleeding. Case 1 was of a 34-year-old woman who was transported to the emergency department of the Department of Obstetrics and Gynecology, Faculty of Medicine, Oita University because of a decline in consciousness level. She had been experiencing excessive and prolonged menstruation for many years but had not sought medical help. A 5-cm uterine submucosal leiomyoma was detected and the patient underwent hysteroscopic myomectomy. Case 2 was of a 36-year-old woman with a history of blood transfusions owing to severe anemia who was presented with progressive dyspnea. Although it was repeatedly explained her that her condition was life threatening, she refused to be hospitalized. Her hemoglobin level was 1.7 g/dl. Multiple uterine fibroids and adenomyosis were detected and total hysterectomy was performed. Case 3 was of a 49-year-old woman who was transported to the emergency department of the Department of Obstetrics and Gynecology, Faculty of Medicine, Oita University due to abdominal pain and severe anemia. Blood testing revealed a hemoglobin level of 1.9 g/dl. Multiple uterine fibroids with a maximum diameter of 8.5 cm were detected. However, the patient insisted on discharge because of lack of disease awareness. Total hysterectomy was performed. The present study is the largest case series showing a detailed clinical course of patients with life-threatening anemia with hemoglobin levels <2.0 g/dl. Additionally, Case 1 of the present series exhibited the lowest hemoglobin level (1.1 g/dl) reported to date. The present cases and a review of the literature suggested that the most important risk factors of life-threatening anemia are the patient's mental, social and personal factors, rather than the organic and functional abnormalities of the uterus.
Keywords: uterine myoma, anemia, case series, hysterectomy, leiomyoma, fibroids
Introduction
Uterine fibroids are the most common neoplasms affecting women and it has been postulated that they occur in >70% of women by the onset of menopause (1). It has been recognized that uterine fibroids are associated with heavy menstrual bleeding, abdominal discomfort, subfertility and a reduced quality of life (2). Management of uterine fibroids includes observation, hormonal therapy, surgery (hysterectomy, myomectomy and trans-cervical resection), uterine artery embolization and high-frequency magnetic resonance-guided focused ultrasound surgery, with appropriate management varying from case to case (2-5). These neoplasms can also lead to life-threatening anemia and death. According to the Institute for Health Metrics and Evaluation, the prevalence, incidence and mortality of uterine fibroids worldwide in 2019 were 29, 0.24 and 0.002%, respectively (6). Notably, Suthar et al (7) estimate that the COVID-19 mortality rate in the vaccinated population is two (0.002%) deaths per 100,000 people. During the COVID-19 pandemic, which is a global problem, more attention should be paid to women's health issues associated with uterine fibroids. Uterine fibroids can also be life threatening via pulmonary metastasis or intravascular extension, despite being benign tumors (8). Among women with uterine fibroids, it is necessary to identify who are at particularly high risk and propose the most appropriate treatment. Cases of severe iron deficiency anemia complicated with uterine fibroids are not rare. However, only one case of severe anemia due to uterine fibroids with hemoglobin levels <2.0 g/dl has been reported to date (9). The present study reported three cases of life-threatening anemia with hemoglobin levels <2.0 g/dl caused by uterine fibroids and genital bleeding.
Case report
Summary
Table I presents the background, clinical course, laboratory findings, clinical images, interventions and prognosis of the three patients. At first, the three women kept refusing further medical care despite being aware of having excessive and prolonged menstruation. Their symptoms were mild compared to the degree of anemia, suggesting that the patients had chronic anemia for a long period. All three patients had poor insight and understanding of their condition and underwent blood transfusion and surgery. Since then, their clinical course has been uneventful and without relapse.
Table I.
Clinical characteristics of the three presented cases.
| Characteristic | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Age (years) | 34 | 36 | 49 |
| Gravida | 0 | 0 | 0 |
| Underlying disease | None | None | None |
| Symptoms | Low consciousness | Dyspnea | Epigastric discomfort |
| BMI | 21.2 | 20.5 | 32.3 |
| On admission | |||
| Heart rate (/min) | 98 | 85 | 111 |
| Blood pressure (mmHg) | 107/74 | 123/65 | 127/68 |
| SpO2 (%) | 99 (room air) | 97 (room air) | 100 (room air) |
| WBC (/µl) | 5,520 | 4,120 | 6,560 |
| RBC (M/µl) | 0.89 | 1.19 | 1.41 |
| Hb (g/dl) | 1.1 | 1.9 | 1.7 |
| Hct (%) | 4.5 | 6.9 | 7.8 |
| MCV (fl) | 50.6 | 58 | 55.3 |
| Platelet (/µl) | 493,000 | 180,000 | 339,000 |
| AST (U/l) | 123 | 22.6 | 7.7 |
| ALT (U/l) | 89.9 | 27 | 8.1 |
| BUN | 8.4 | 6.7 | 4.3 |
| Cre | 0.61 | 0.4 | 0.44 |
| Na+ (mmol/l) | 127.9 | 136.5 | 139.2 |
| K+ (mmol/l) | 3.34 | 3.04 | 3.16 |
| Cl- (mmCl/l) | 93.8 | 103.6 | 111.4 |
| Myoma dimensions | 5x5 cm | Maximum 5 cm | Maximum 8.5 cm |
| Complications | Electrolyte imbalance, liver failure | Edema | Heart failure |
| Diagnosis | Submucosal fibroid | Adenomyosis, multiple uterine fibroids | Multiple uterine fibroids |
| Treatment | TCR | TAH | TAH |
| Tumor weight | 15 g | 210 g | 1350 g |
BMI, body mass index; SpO2, blood oxygen saturation; WBC, white blood cells; RBC, red blood cells; Hb, hemoglobin; Hct, hematocrit; MCV, mean corpuscular volume; AST, aspartate aminotransferase; ALT, alanine aminotransferase; BUN, blood urea nitrogen; Cre, creatinine; TCR, transcervical resection; TAH, total abdominal hysterectomy.
Case 1
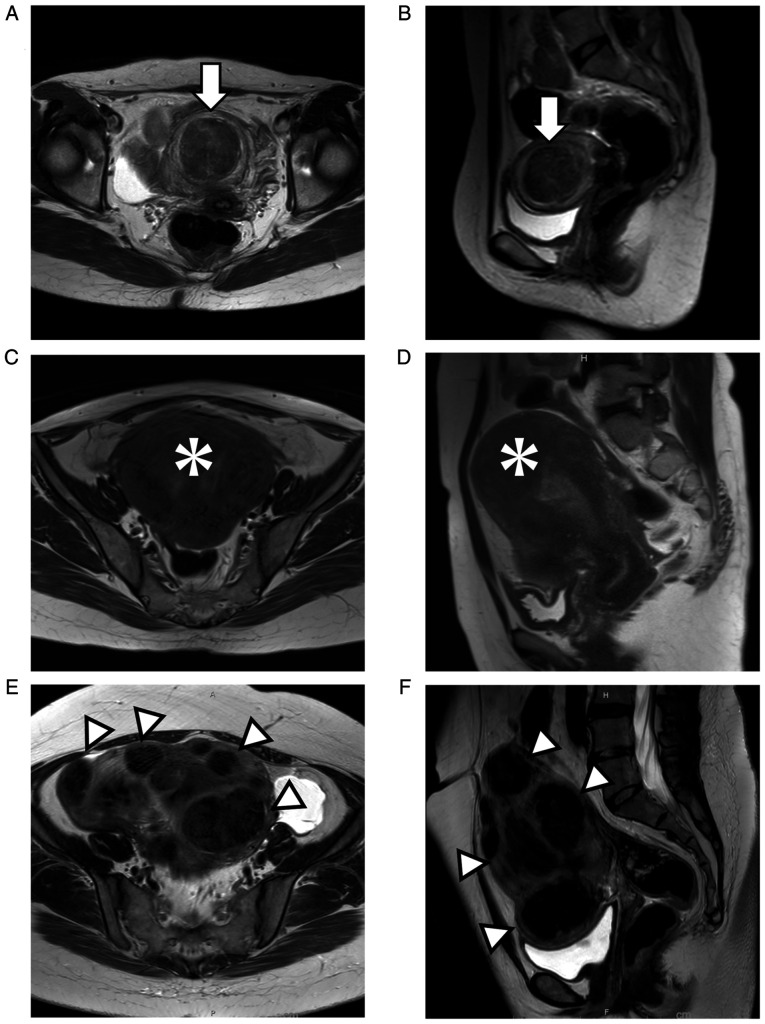
A 34-year-old woman was transported by ambulance to the emergency department of the Department of Obstetrics and Gynecology, Faculty of Medicine, Oita University owing to a decline in consciousness level. She was unemployed, solitary and stayed at home all day. She had been experiencing excessive and prolonged menstruation for many years but had not sought medical care. Her last menstruation began 3 weeks before presentation and continued at the time of her arrival. Her Glasgow Coma Scale score (10) was E3V5M6. Blood testing showed a hemoglobin level of 1.1 g/dl. A 5-cm uterine submucosal leiomyoma was detected by pelvic magnetic resonance imaging (MRI; Fig. 1A and B). During her hospitalization, she was transfused 10 units of packed red blood cells. On day 13 of admission, she was discharged home. Her hemoglobin level on discharge was 8.7 g/dl. Even though anemia improved, her reactions were slow and hazy. Her mother reported that these symptoms persisted even before admission. Cranial computed tomography (CT) scans showed cerebral atrophy. It was speculated that the patient had some underlying diseases, but the patient was not willing for detailed examination. The patient underwent hysteroscopic myomectomy (Fig. 2A). At 1 month postoperatively, her hemoglobin level was 11.6 g/dl and there had been no relapse.
Figure 1.
Clinical imaging findings: (A) axial and (B) sagittal T2-weighted MRI revealed a 5-cm uterine submucosal leiomyoma (arrows). (C) axial and (D) sagittal T2-weighted MRI confirmed multiple uterine myomas and adenomyosis (asterisks). (E) axial and (F) sagittal T2-weighted MRI revealed multiple uterine myomas (arrow heads) with a maximum diameter of 8.5 cm. MRI, magnetic resonance imaging.
Figure 2.
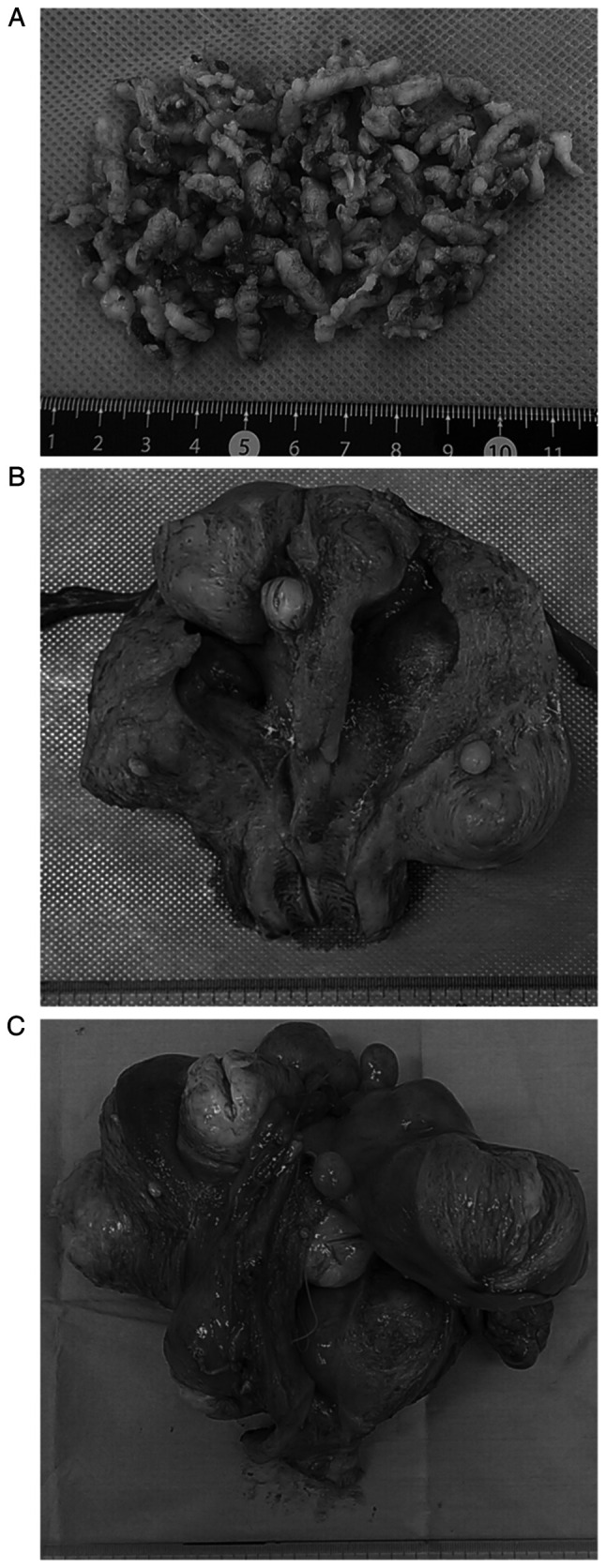
Macroscopic findings of surgically resected specimens. (A) Submucosal fibroids were fragmented and resected by TCR. (B) Myomas and adenomyosis are observed in the excised uterus. (C) Multiple fibroids are observed in the excised uterus. TCR, transcervical resectio.
Case 2
A 36-year-old woman presented with progressive dyspnea. She had a history of blood transfusions in our hospital for anemia during her last visit 5 years ago. Blood testing revealed a hemoglobin level of 1.7 g/dl. Pelvic MRI showed multiple uterine fibroids and adenomyosis (Fig. 1C and D). It was repeatedly explained to her that her condition was life threatening, but she refused to be hospitalized. We called her family to convince her and she ultimately agreed to be hospitalized. During her hospitalization, she was transfused 12 units of packed red blood cells. On admission day 6, she was discharged home. Her hemoglobin level at discharge was 12.2 g/dl. She and her husband had no desire for childbearing. Total hysterectomy was performed (Fig. 2B); at 1 month postoperatively, the hemoglobin level was 11.9 g/dl and there had been no relapse.
Case 3
A 49-year-old woman with a history of heart failure was transported by ambulance to the emergency department of the Department of Obstetrics and Gynecology, Faculty of Medicine, Oita University due to abdominal pain and severe anemia. Blood testing revealed a hemoglobin level of 1.9 g/dl. Pelvic MRI showed multiple uterine fibroids with a maximum diameter of 8.5 cm (Fig. 1E and F). During her hospitalization, she was transfused 8 units of packed red blood cells and underwent treatment for heart failure. On admission day 5, she still needed oxygen and diuretics, although her hemoglobin level had improved to 5.9 g/dl. Nevertheless, the patient insisted on discharge owing to the lack of disease awareness, which might have been the cause for not seeking medical care previously. On admission day 9, she was discharged home. Her hemoglobin level at discharge was 9.2 g/dl. Total hysterectomy was performed (Fig. 2C); at 1 month postoperatively, the hemoglobin level was 11.2 g/dl and there had been no relapse.
Discussion
The present report is the largest case series showing a detailed clinical course of patients with life-threatening anemia (hemoglobin levels <2.0 g/dl) caused by uterine fibroids. To date, only three cases of severe anemia with hemoglobin levels <2.0 g/dl have been reported (9,11,12). The present study summarized these and its own three cases in Table II. The patients' age ranged from 21 to 49 years, with an average of 35.2 years. All six patients were women. The hemoglobin levels ranged from 1.1 to 1.9 g/dl, with an average of 1.58 g/dl. Case 1 of the present study had the lowest hemoglobin level (1.1 g/dl) reported to date. Patients with anemia are in a state of high cardiac output because of decreased afterload and increased preload caused by decreased peripheral vascular resistance and viscosity (13). The compensatory mechanism of cardiac dynamics fails when hemoglobin falls below 2-3 g/dl, resulting in cardiac failure, further disruption of the systemic oxygen demand balance, organ congestion, generation of free radicals at the cellular level and imbalance of the coagulation-fibrinolytic system and the complement system. This can lead to free radical generation at the cellular level, imbalance in the coagulation-fibrinolytic and complement systems, disseminated intravascular coagulation and multiorgan failure (13). It is important to note that, despite the compensatory mechanisms, the complications of chronic anemia left untreated are not minor and can adversely affect cardiovascular function, worsen chronic conditions and ultimately lead to the development of multiple organ failure and even mortality (14). Therefore, it is necessary to appropriately identify and treat high-risk patients with severe anemia.
Table II.
Summary of all published cases of severe anemia with hemoglobin levels <2.0 g/dl.
| Characteristic | Present case 1 | Present case 2 | Present case 3 | Chai et al (2021) (9) | Can et al (2013) (11) | Jost et al (2005) (12) |
|---|---|---|---|---|---|---|
| Age (years) | 34 | 36 | 49 | 42 | 21 | 29 |
| Sex | Female | Female | Female | Female | Female | Female |
| Gravida | 0 | 0 | 0 | 0 | NA | NA |
| Para | 0 | 0 | 0 | 0 | NA | NA |
| Underlying disease/characteristics | Cerebral atrophy | Refusal of hospitalization | Lack of disease awareness | Low health literacy and lack of disease awareness | Mental retardation | Celiac disease and bulimia nervosa |
| Symptoms | Low consciousness | Dyspnea | Epigastric discomfort | Fatigue, dizziness | Fatigue, palpitations, dyspnea on exertion, dizziness | Exhaustion, fatigue and abdominal pain |
| Hb (g/dl) | 1.1 | 1.7 | 1.9 | 1.4 | 1.7 | 1.7 |
| BMI | 21.2 | 20.5 | 32.3 | 22.0 | 21.5 | 14.0 |
| Heart rate (/min) | 98 | 85 | 111 | 87 | 125 | NA |
| Blood pressure (mmHg) | 107/74 | 123/65 | 127/68 | 107/47 | 100/60 | NA |
| SpO2 (% on room air) | 99 | 97 | 100 | 100 | 96 | NA |
| Fibroids | 5x5 cm | Maximum 5 cm | Maximum 8.5 cm | 3.5 cm | NA | NA |
| Diagnosis | Submucosal fibroid | Adenomyosis, Multiple uterine fibroids | Multiple uterine fibroids | Submucosal fibroid | NA | NA |
| Transfusion volume (units) | 10 | 12 | 8 | 5 | 5 | NA |
Hb, hemoglobin; BMI, body mass index; SpO2, blood oxygen saturation.
All three patients in the present study had a background of not seeking appropriate medical attention, which is in agreement with the existing literature (9,11,12). The cases of a socially vulnerable 42-year-old woman with a hemoglobin level of 1.4 g/dl (9), of a 21-year-old woman with mental retardation and a hemoglobin level of 1.7 g/dl (11) and of a 29-year-old woman with celiac disease and anorexia nervosa showing a hemoglobin level of 1.7 g/dl (12) were reported in 2021, 2013 and 2005, respectively. These findings suggested that the most important risk factors of a life-threatening anemia are the patient's mental, social and personal problems, rather than the organic and functional abnormalities of the uterus. Similar trends have been found in other serious diseases, such as malignant tumors. Patients with mental disorders and intellectual disabilities show a lower rate of early cancer detection owing to a lack of cancer screening participation, awareness and understanding of the disease (15-17). Especially, in cases of socially vulnerable patients, patients with mental retardation and patients with marked lack of disease awareness, it is necessary to perform follow-up examinations and early surgery in a preventive perspective. Many patients suffer from hypermenorrhea and prolonged menstruation; starting aggressive treatment at the right time is important for a woman's lifelong health, not just for menstrual and fertility problems. Patients who are not aware of their condition need to be approached by a physician.
All three presented cases were resolved by surgical treatment rather than embolization or hormonal therapy. It has been reported that embolization is better in short-term prognosis (3), but total hysterectomy is associated with better long-term satisfaction (4). The patients in the present study have not presented symptom recurrence since surgery. In addition, all three cases had one thing in common: The patients had never given birth. The factor with the greatest protective effect was parity; giving birth has been associated with a five-fold reduction in the risk of uterine fibroids requiring surgical treatment compared to nulliparity in a single-center study (1,18). In summary, women who have severe menorrhagia but lack disease awareness due to mental, social and personal problems are at high risk of life-threatening anemia. Early surgical intervention and blood transfusions may improve long-term prognosis, particularly in nulliparous women.
Uterine fibroids and uterine adenomyosis are both common diseases, but they are a hormone-dependent diseases, which means that they progress slowly with each menstruation and do not progress during periods of amenorrhea. Once a woman becomes pregnant, gives birth and breastfeeds, she will be amenorrheic for ~2 years; therefore, if she gives birth to five children, she will not experience menstruation for ~10 years in total. However, currently, women are giving birth at an older age and the trend is toward fewer births. In the days of repeated pregnancies, childbirth and lactation starting from the teenage years, the number of menstrual periods during a woman's lifetime was approximately 40, but today, when women have one or two children, the number exceeds 400(19). Thus, the prevalence of hormone-dependent conditions is expected to increase.
There were two limitations to the present study. First, there was a lack of anemia etiology and iron-related tests. The three cases presented here were considered to be of iron deficiency anemia owing to low MCV and persistent genital bleeding. Blood transfusion was prioritized over iron replacement therapy considering the urgency and severity. Second, the postoperative follow-up period was short.
In conclusion, the present study is the largest case series showing detailed clinical courses of patients with life-threatening anemia, with hemoglobin level <2.0 g/dl, caused by uterine fibroids. Additionally, Case 1 of the present series is the lowest hemoglobin level (1.1 g/dl) reported to date. The present cases and a review of the literature suggested that the most important risk factors of a life-threatening anemia were the patient's mental, social and personal factors, rather than the organic and functional abnormalities of the uterus. Patients who are not aware of the severity of their condition due to life-threatening anemia need to be approached by a physician.
Acknowledgements
Not applicable.
Funding Statement
Funding: The present study was supported by The Imai Foundation.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
MK took part in the study conception and design and acquisition, analysis, interpretation of data and drafting of the manuscript. MO took part in the conception and design of the manuscript and provided important intellectual content. MY took part in the conception, design and critical revision of the manuscript, provided important intellectual content and supervised the study. YK took part in the critical revision of the manuscript, acquisition of data and supervised the study. MK, MO, and MY confirm the authenticity of all the raw data.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Written informed consent for publication was obtained from all patients.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Stewart EA, Cookson CL, Gandolfo RA, Schulze-Rath R. Epidemiology of uterine fibroids: A systematic review. BJOG. 2017;124:1501–1512. doi: 10.1111/1471-0528.14640. [DOI] [PubMed] [Google Scholar]
- 2.Manyonda I, Belli AM, Lumsden MA, Moss J, McKinnon W, Middleton LJ, Cheed V, Wu O, Sirkeci F, Daniels JP, et al. Uterine-artery embolization or myomectomy for uterine fibroids. N Engl J Med. 2020;383:440–451. doi: 10.1056/NEJMoa1914735. [DOI] [PubMed] [Google Scholar]
- 3.Edwards RD, Moss JG, Lumsden MA, Wu O, Murray LS, Twaddle S, Murray GD. Uterine-artery embolization versus surgery for symptomatic uterine fibroids. N Engl J Med. 2007;356:360–370. doi: 10.1056/NEJMoa062003. Committee of the Randomized Trial of Embolization versus Surgical Treatment for Fibroids. [DOI] [PubMed] [Google Scholar]
- 4.Hehenkamp WJ, Volkers NA, Birnie E, Reekers JA, Ankum WM. Symptomatic uterine fibroids: Treatment with uterine artery embolization or hysterectomy-results from the randomized clinical Embolisation versus hysterectomy (EMMY) Trial. Radiology. 2008;246:823–832. doi: 10.1148/radiol.2463070260. [DOI] [PubMed] [Google Scholar]
- 5.Donnez J, Dolmans MM. Uterine fibroid management: From the present to the future. Hum Reprod Update. 2016;6:665–686. doi: 10.1093/humupd/dmw023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Institute for Health Metrics and Evaluation. Uterine Fibroids - Level 4 Cause. https://www.healthdata.org/results/gbd_summaries/2019/uterine-fibroids-level-4-cause. Accessed July 10, 2022. [Google Scholar]
- 7.Suthar AB, Wang J, Seffren V, Wiegand RE, Griffing S, Zell E. Public health impact of covid-19 vaccines in the US: Observational study. BMJ. 2022;377(e069317) doi: 10.1136/bmj-2021-069317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yano M, Katoh T, Nakajima Y, Iwanaga S, Kin R, Kozawa E, Yasuda M. Uterine intravenous leiomyomatosis with an isolated large metastasis to the right atrium: A case report. Diagn Pathol. 2020;15(4) doi: 10.1186/s13000-019-0913-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chai AL, Huang OY, Rakočević R, Chung P. Critical iron deficiency anemia with record low hemoglobin: A case report. J Med Case Rep. 2021;15(472) doi: 10.1186/s13256-021-03024-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 11.Can Ç, Gulacti U, Kurtoglu E. An extremely low hemoglobin level due to menorrhagia and iron deficiency anemia in a patient with mental retardation. Int Med J. 2013;20:735–736. [Google Scholar]
- 12.Jost PJ, Stengel SM, Huber W, Sarbia M, Peschel C, Duyster J. Very severe iron-deficiency anemia in a patient with celiac disease and bulimia nervosa: A case report. Int J Hematol. 2005;82:310–311. doi: 10.1532/IJH97.E0505. [DOI] [PubMed] [Google Scholar]
- 13.Klutstein MW, Tzivoni D. Anaemia and heart failure: Aetiology and treatment. Nephrol Dial Transplant. 2005;20 (Suppl 7):vii7–vii10. doi: 10.1093/ndt/gfh1100. [DOI] [PubMed] [Google Scholar]
- 14.Tobian AA, Ness PM, Noveck H, Carson JL. Time course and etiology of death in patients with severe anemia. Transfusion. 2009;49:1395–1399. doi: 10.1111/j.1537-2995.2009.02134.x. [DOI] [PubMed] [Google Scholar]
- 15.Shin DW, Lee JW, Jung JH, Han K, Kim SY, Choi KS, Park JH, Park JH. Disparities in cervical cancer screening among women with disabilities: A national database study in South Korea. J Clin Oncol. 2018;36:2778–2786. doi: 10.1200/JCO.2018.77.7912. [DOI] [PubMed] [Google Scholar]
- 16.Shinden Y, Kijima Y, Hirata M, Nakajo A, Tanoue K, Arigami T, Kurahara H, Maemura K, Natsugoe S. Clinical characteristics of breast cancer patients with mental disorders. Breast. 2017;36:39–43. doi: 10.1016/j.breast.2017.08.010. [DOI] [PubMed] [Google Scholar]
- 17.Willis D, Samalin E, Satgé D. Colorectal cancer in people with intellectual disabilities. Oncology. 2018;95:323–336. doi: 10.1159/000492077. [DOI] [PubMed] [Google Scholar]
- 18.Sato F, Mori M, Nishi M, Kudo R, Miyake H. Familial aggregation of uterine myomas in Japanese women. J Epidemiol. 2002;12:249–253. doi: 10.2188/jea.12.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Critchley HOD, Babayev E, Bulun SE, Clark S, Garcia-Grau I, Gregersen PK, Kilcoyne A, Kim JJ, Lavender M, Marsh EE, et al. Menstruation: Science and society. Am J Obstet Gynecol. 2020;223:624–664. doi: 10.1016/j.ajog.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.