Abstract
Introduction
This study sought to explore individual and facility-level variation in social connectedness among long-stay nursing home residents with Alzheimer's or other dementias (ADRD).
Methods
We identified 721,074 long-stay residents with ADRD using 2016 Minimum Data Set 3.0 data. Social connectedness was defined using the social connectedness index (SCI) (high: SCI = 5, lower: 0 < SCI ≤ 4). Adjusted odds ratios (aOR) provided estimates of the associations between resident-level and facility-level characteristics, and high SCI was derived from logistic models.
Results
The SCI Cronbach's alpha was 0.69; 78.6% had high SCI scores. Men were less likely than women to have higher SCI scores (aOR = 0.97; 95% CI: 0.97–0.98). Increasing age was associated with higher SCI scores (e.g., aOR [85–94 vs. 40–64 years]: 1.07; 95% CI: 1.06–1.07). Those with moderate cognitive impairment (aOR: 0.87) and severe cognitive impairment (aOR: 0.85) had reduced odds of SCI = 5 relative to those with mild/intact cognitive function. Residents living in homes with special care dementia units and with higher percentage of residents with dementia had decreased odds of high social connectedness.
Discussion/Conclusion
Understanding resident- and nursing home-level variation in social connectedness may be important for targeting interventions that reduce isolation among residents with ADRD.
Keywords: Social connectedness, Nursing homes, Facility factors, Alzheimer's disease, Dementia
Introduction
Of people with Alzheimer's disease and other related dementias (ADRD), three quarters will spend time in nursing homes before 80 years of age (compared to 4% of the general population), they will spend on average 2 years in nursing homes and most will die there [1, 2, 3]. Positive and meaningful peer relationships contribute to thriving in nursing homes [4, 5], yet residents with ADRD are prone to social isolation because of their cognitive impairment and other factors [6]. In nursing homes, social networks are often small and sparse [7]. Half of residents report that they had never spoken to their roommate, only partly due to communication challenges [8]. Residents with dementia are often willing conversationalists, but due to cognitive challenges, their conversations may be unwelcomed [9]. Closer social bonds occur between residents with similar degrees of cognitive function [5]. Yet, the development of social relationships may be hindered by the tendency of a nursing home to group residents by similar conditions and needs [10]. While close, positive relationships are considered crucial for the delivery of high-quality care in nursing homes [11, 12], few studies have investigated social connectedness in this setting.
Research on the role of social connectedness and health dates back more than 50 years and includes the belief that a sense of social connectedness begins in adolescence and continues throughout adulthood [13]. Problems with achieving social connectedness can negatively affect day-to-day social functioning [13, 14], and among those successful at achieving social connectedness, regression to earlier ways of functioning can occur when individuals have difficulty adjusting to changes in life circumstances [13]. The loss of autonomy and control in nursing home residents with progressive cognitive impairment could result in acting out behaviors due to loss of social connections. We previously reported that social connectedness could be measured in nursing home residents with ADRD by evaluating observable behaviors such as residents' conflict with others and negative acting out behaviors [15].
Understanding social connectedness among those in nursing homes is important because of the devastating effects of the COVID-19 pandemic in this unique setting [16]. The extraordinary measures utilized to protect nursing home residents (e.g., isolation, restricted visiting, wearing of masks, shields, gloves by personnel) may have harmed residents with ADRD [17]. The role that social connectedness plays in nursing home residents can be quantified through use of a valid and reliable measure.
A recent mixed-methods systematic review demonstrated the positive impact of special care units on the social interactions of nursing home residents with ADRD [18]. This study underscored the need to better understand how social connectedness varies by type of facility. Such research is important for both validating the social connectedness index (SCI) [15] and for advancing the science in this area. The goals of the study were two-fold. First, this study was conducted to further validate the SCI in residents with ADRD by examining the internal consistency reliability of the SCI. Second, we sought to examine individual and facility-level variation in social connectedness among long-stay nursing home residents with ADRD. Our hypotheses are shown in Table 1.
Table 1.
Hypothesized association between resident characteristics and nursing home factors and social connectedness scores
| High social connectedness among residents | Low social connectedness among residents | |
|---|---|---|
| Resident Level | Women | Men |
| ≥85 years | Age <85 years | |
| Independent in ADLs | Dependent in ADLs | |
| Asian, Black, Native Hawaiian/PI, Hispanic, multiracial | Non-Hispanic White | |
| Family involvement important | American Indian/Alaska Native | |
| Mild cognitive impairment | Family involvement less important | |
| Increased length of nursing home stay | Severe cognitive impairment | |
| Nursing Home Level | Private non-profit home | Dedicated special care dementia unit |
| Part of chain | High % of short-stay skilled nursing facility residents | |
| Use of nurse practitioners and physician assistants | High % of residents with ADRD | |
| Low % of residents with ADRD | ||
| High star ratings |
Materials and Methods
The study was approved by the University of Massachusetts Chan Medical School Institutional Review Committee.
Data Sources and Study Sample
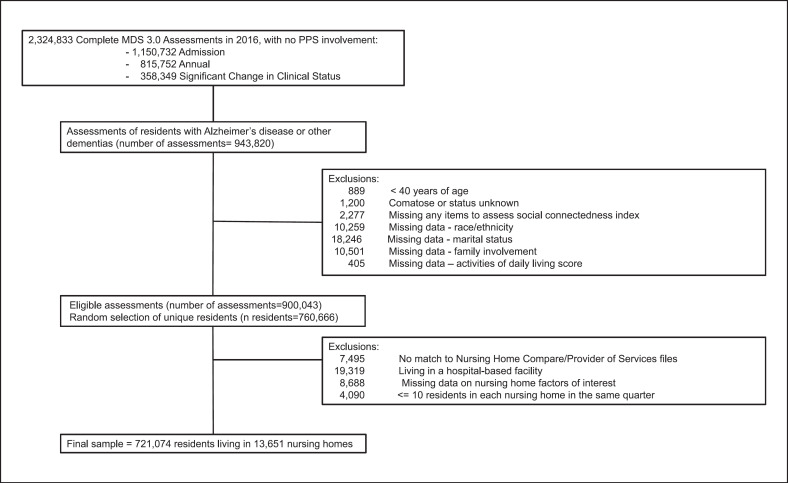
We used three data resources: (1) resident-level data from the national 2016 Minimum Data Set 3.0 (MDS) [19]; (2) 2016 nursing home-level Nursing Home Compare data [20]; and (3) 2016 Provider of Service data [21]. The MDS 3.0 is a comprehensive resident assessment mandated for all the USA0 nursing home residents in Medicare/Medicaid-certified nursing homes. Nursing home-level data were mostly based on information gathered in survey reports (occurring at intervals of ∼12–15 months), presently called Certification and Survey Provider Enhanced Reports data. Cerification and Survey provider Enhanced reports data include information regarding operating and structural characteristics and regulatory variables (e.g., deficiencies noted). Nursing Home Compare includes quality ratings. After applying our inclusion criteria, there were 900,043 eligible assessments from which we randomly selected one assessment per resident such that one unique assessment for the 760,666 residents was included. We then applied additional exclusion criteria to define our sample of long-stay nursing home residents with ADRD. The final sample included 721,074 residents living in 13,651 nursing homes (shown in Fig. 1).
Fig. 1.
Sample construction flowchart.
Social Connectedness Index
The SCI was calculated from the sum of five dichotomous indicators from MDS 3.0 [15]: absence of behavioral symptoms directed towards others, behaviors interfering with social interactions, behaviors impacting others, wandering that intrudes on others, and rejection of care. The SCI had adequate reliability (KR-20: 0.63–0.74), and good content, criterion-related, and construct validity in persons with ADRD.
Resident-Level Characteristics
We examined gender, age, race/ethnicity, length of nursing home residency, and family involvement in care. Dependence in activities of daily living [22] was categorized as independent (score 0–2), extensive assistance required (score 3–4), or dependent (score 5–6). Using the Cognitive Function Scale [23], we categorized residents as intact/mildly impaired, moderately impaired, or severely cognitive impaired.
Nursing Home-Level Characteristics
We considered a variety of organizational (ownership status, number of beds, and occupancy) and operational (process, staffing, and outcome) nursing home characteristics [24, 25] and categorized the variables guided by previous literature [26]. Process variables included % residents with skilled nursing care and % residents with ADRD. Staffing variables included presence of nurse practitioners/physician assistants, direct care staff per resident per day, and adjusted RN time per resident per day. Nursing Home Compare provided quality ratings (i.e., overall, staffing, RN staffing) and adjusted staffing levels. We took the most recent survey data available before December 31, 2016. The Provider of Services file provided information on the presence of special care dementia units, use of nurse practitioners/physician assistants, total number of beds, the profit orientation/ownership, and whether the home was part of a chain. Two nursing home-level variables were calculated by aggregating all MDS data for each home: (1) % skilled nursing facility residents; (2) % residents with ADRD (0–39%, 40–49%, 50–59%, 60–100%).
Analytic Approach
We calculated the Cronbach's alpha for the SCI and considered an SCI score of 5 to indicate “high social connectedness” and scores of 0–4 to indicate “low/moderate social connectedness.” We described resident and nursing home characteristics and estimated the prevalence of high social connectedness across characteristics of interest. We identified three variables (staffing star rating, registered nursing star rating, and registered nurse staffing <0.5 h per resident per day) causing multicollinearity based on variance inflation factors >2.5. We developed two logistic models using generalized estimating equations: (1) including all resident characteristics and (2) adding nursing home characteristics. For variables with multicollinearity concerns, we adjusted for resident factors only. Adjusted odds ratios (aOR) and corresponding 95% confidence intervals (CI) were estimated from these models.
Results
The sample included mostly women (69.1%), ≥ age 75 years (81.6%), with moderate to severe cognitive impairment (64.1%) (Table 2). The Cronbach's alpha for the SCI was 0.69 and was considered acceptable. Most lived in homes with over 100 beds, with 19% nearly at full occupancy. Twenty-three percent lived in homes offering Alzheimer's specialty care beds with 19.5% living in homes with >50% having a diagnosis of ADRD. One in five residents lived in a home that received a 5-star overall rating, 8.1% in a home that received a 5-star overall staffing rating, and 17.3% lived in a home that received a 5-star rating for registered nurse staffing.
Table 2.
Characteristics of nursing home residents with ADRD
| Total, N = 721,074, %* | |
|---|---|
| Resident characteristics | |
| Women | 69.1 |
| Men | 30.9 |
| Age group, years | |
| 40–64 | 5.7 |
| 65–74 | 12.8 |
| 75–84 | 30.2 |
| 85–94 | 41.9 |
| ≥95 | 9.5 |
| Hispanic of any race(s) | 5.9 |
| Not Hispanic and | |
| White only | 78.5 |
| Black only | 13.1 |
| American Indian/Alaska Native only | 0.3 |
| Asian only | 1.8 |
| Native Hawaiian/Pacific Islander only | 0.3 |
| Multiracial | 0.1 |
| Marital status | |
| Married | 23.2 |
| Widowed | 50.6 |
| Divorced/separated | 13.1 |
| Never married | 13.1 |
| Family involvement in care | |
| Important | 89.4 |
| Not important | 10.6 |
| Cognitive function | |
| Intact/mild impairment | 35.9 |
| Moderate impairment | 46.1 |
| Severe impairment | 17.9 |
| Activities of daily living | |
| No limitations | 14.9 |
| Modified independence | 57.7 |
| Dependent | 27.4 |
| Resident living in the home for, months | |
| 6–11 | 14.5 |
| 12–23 | 18.3 |
| ≥24 | 25.8 |
|
| |
| Nursing home factors | |
| Member of a chain | 56.5 |
| Not member of a chain | 43.5 |
| Ownership | |
| Government | 22.6 |
| For profit | 70.4 |
| Not for profit | 7.0 |
| Beds | |
| ≥200 beds | 16.0 |
| 100–199 beds | 55.5 |
| 50–100 beds | 25.4 |
| <50 beds | 3.1 |
| Occupancy | |
| ≥95% | 19.0 |
| 90 to <95% | 22.8 |
| 80% to <90% | 30.3 |
| <80% | 27.9 |
| Located in rural area | 20.7 |
| Not located in rural area | 79.4 |
|
| |
| Skilled nursing/short stay, % | |
| ≥60% | 12.3 |
| 50–59% | 15.2 |
| 40–49% | 21.6 |
| ≤39% | 50.9 |
| Alzheimer's specialty care beds | 23.0 |
| No Alzheimer's specialty care beds | 77.0 |
| Residents with Alzheimer's disease/dementia | |
| ≥60% | 7.3 |
| 50–59% | 12.2 |
| 40–49% | 22.7 |
| ≤39% | 57.7 |
|
| |
| Nursing home staffing variables | |
| Any nurse practitioners or physician assistants | 74.8 |
| No nurse practitioners or physician assistants | 25.2 |
| Adjusted direct care staff <3 per resident per day | 8.6 |
| Adjusted direct care staff ≥3 per resident per day | 91.4 |
| Adjusted registered nurse <0.5 per resident per day | 53.3 |
| Adjusted registered nurse ≥0.5 per resident per day | 46.7 |
| RN staffing star rating | |
| 1 | 9.1 |
| 2 | 18.1 |
| 3 | 28.7 |
| 4 | 26.9 |
| 5 | 17.3 |
| Overall staffing star rating | |
| 1 | 12.6 |
| 2 | 15.3 |
| 3 | 32.5 |
| 4 | 31.5 |
| 5 | 8.1 |
| Overall star rating | |
| 1 | 17.2 |
| 2 | 19.5 |
| 3 | 19.4 |
| 4 | 23.2 |
| 5 | 20.8 |
May not total 100% due to rounding.
Prevalence of Higher SCI Scores by Resident and Facility Characteristics
Overall, 78.7% had high social connectedness, with 79.9% of women and 76.2% of men with SCI = 5 (Table 3). While 74.0% of residents aged between 40 and 64 years had high social connectedness, 80.1% of those ≥85 years had SCI = 5. While 79.4% of those rating family involvement as important had high social connectedness, 72.8% of those saying family involvement is not important had an SCI = 5. The prevalence of high social connectedness was 86.0% in residents with mild/no cognitive impairment and 73.1% in those with severe cognitive impairment.
Table 3.
Prevalence of high social connectedness score (SCI = 5) by resident and facility characteristics among nursing home residents with ADRD
| Sample size, n | % | |
|---|---|---|
| Resident characteristics | ||
| Women | 498,416 | 79.9 |
| Men | 222,658 | 76.2 |
| Age group, years | ||
| 40–64 | 40,885 | 74.0 |
| 65–74 | 92,052 | 76.5 |
| 75–84 | 217,636 | 78.2 |
| 85–94 | 302,156 | 80.1 |
| ≥95 | 68,345 | 80.1 |
| Hispanic of any race(s) | 42,675 | 81.6 |
| Not Hispanic and | ||
| White only | 566,208 | 77.8 |
| Black only | 94,275 | 81.8 |
| American Indian/Alaska Native only | 2,153 | 74.3 |
| Asian only | 13,181 | 85.9 |
| Native Hawaiian/Pacific Islander only | 2,254 | 81.5 |
| Multiracial | 328 | 79.3 |
| Marital status | ||
| Married | 167,450 | 77.4 |
| Widowed | 364,869 | 80.0 |
| Divorced/separated | 94,305 | 77.1 |
| Never married | 94,450 | 77.6 |
| Family involvement in care | ||
| Important | 644,802 | 79.4 |
| Not important | 76,272 | 72.8 |
| Cognitive function scale | ||
| Intact/mild impairment | 259,073 | 86.0 |
| Moderate impairment | 332,656 | 75.2 |
| Severe impairment | 129,345 | 73.1 |
| Activities of daily living | ||
| Independent | 107,551 | 82.7 |
| Modified independence | 416,071 | 77.1 |
| Dependent | 197,452 | 79.9 |
| Living in nursing home for, months | ||
| ≤5 | 298,964 | 78.3 |
| 6–11 | 104,186 | 78.8 |
| 12–23 | 131,874 | 79.1 |
| ≥24 | 186,050 | 79.1 |
|
| ||
| Nursing home factors | ||
| Member of a chain | ||
| Yes | 407,574 | 79.6 |
| No | 313,500 | 77.5 |
| Ownership | ||
| Government | 50,484 | 75.1 |
| For profit | 507,804 | 79.7 |
| Not for profit | 162,786 | 76.7 |
| Beds | ||
| ≥200 beds | 115,592 | 78.0 |
| 100–199 beds | 400,377 | 79.6 |
| 50–100 beds | 182,875 | 77.7 |
| <50 beds | 22,230 | 74.0 |
| Occupancy, % | ||
| ≥95 | 137,235 | 77.9 |
| 90 to <95 | 164,028 | 79.2 |
| 80% to <90 | 218,485 | 79.2 |
| <80 | 201,326 | 78.4 |
|
| ||
| Location | ||
| Rural | 148,880 | 75.3 |
| Urban | 572,194 | 79.6 |
| % Skilled nursing/short stay, % | ||
| ≥60 | 88,849 | 83.5 |
| 50–59 | 109,592 | 81.1 |
| 40–49 | 155,662 | 80.2 |
| ≤39 | 366,971 | 76.2 |
| Alzheimer's specialty care beds | ||
| Any | 165,786 | 73.9 |
| None | 555,288 | 80.2 |
| Residents with Alzheimer's disease/dementia, % | ||
| ≥60 | 52,924 | 69.4 |
| 50–59 | 88,039 | 74.5 |
| 40–49 | 163,733 | 76.9 |
| ≤39 | 416,378 | 81.5 |
|
| ||
| Nursing home staffing variables | ||
| Nurse practitioners or physician assistants | ||
| Any | 539,415 | 79.1 |
| None | 181,659 | 77.6 |
| Adjusted direct care staff <3 per resident per day | ||
| Yes | 62,072 | 78.8 |
| No | 659,002 | 78.3 |
| Adjusted registered nurse <0.5 per resident per day | ||
| Yes | 384,546 | 79.2 |
| No | 336,528 | 78.1 |
| RN staffing star rating | ||
| 1 | 65,234 | 78.7 |
| 2 | 130,472 | 79.6 |
| 3 | 206,848 | 79.2 |
| 4 | 193,882 | 78.7 |
| 5 | 124,638 | 77.0 |
| Overall staffing star rating | ||
| 1 | 90,557 | 79.4 |
| 2 | 110,387 | 78.7 |
| 3 | 234,628 | 79.4 |
| 4 | 227,290 | 78.3 |
| 5 | 58,212 | 76.4 |
| Overall star rating | ||
| 1 | 123,998 | 78.1 |
| 2 | 140,385 | 78.9 |
| 3 | 139,814 | 78.4 |
| 4 | 166,901 | 78.5 |
| 5 | 149,976 | 79.6 |
Association between High SCI Scores and Resident and Facility Characteristics
Table 4 shows that after adjusting for resident characteristics, men were slightly less likely than women to have an SCI = 5 (aOR = 0.97; 95% CI: 0.97–0.98), and increasing age was associated with SCI = 5 (e.g., aOR [85–94 years vs. 40–64 years]: 1.07; 95% CI: 1.06–1.07). Further adjustment for facility factors produced estimates that were essentially the same. Nursing home and resident characteristics related to ADRD (e.g., living in a home with special care dementia or a home with greater percentages of residents with ADRD, or having more severe cognitive impairment) were associated with reduced odds of SCI = 5. Residents living in homes with greater percentages of skilled nursing facility post-acute stays had greater odds of higher social connectedness (aOR [≥60% vs. ≤39%]: 1.04; 1.03–1.04).
Table 4.
Resident and nursing home characteristics associated with highest SCI score
| Resident characteristics adjusted* odds ratios (95% CI) | Resident and nursing home characteristics adjusted* odds ratios (95% CI) | |
|---|---|---|
| Resident characteristics | ||
| Men (vs. women) | 0.97 (0.97–0.98) | 0.97 (0.97–0.98) |
| Age, years | ||
| 40–64 | 0.98 (0.98–0.99) | 0.98 (0.98–0.99) |
| 65–74 | Reference | Reference |
| 75–84 | 1.02 (1.02–1.03) | 1.02 (1.02–1.03) |
| ≥85 | 1.05 (1.04–1.05) | 1.05 (1.04–1.05) |
| Race/ethnicity | ||
| Hispanic of any race(s) | 1.02 (1.01–1.02) | |
| Not Hispanic and | ||
| White only | Reference | |
| Black only | 1.03 (1.02–1.03) | |
| American Indian/Alaska Native only | 1.01 (0.99–1.04) | |
| Asian only | 1.05 (1.04–1.06) | |
| Native Hawaiian/Pacific Islander only | 1.01 (0.99–1.04) | |
| Multiracial | 1.02 (0.98–1.07) | |
| Family involvement in care important | 1.05 (1.04–1.05) | 1.05 (1.04–1.05) |
| Cognitive impairment | ||
| Intact/mild | Reference | Reference |
| Moderate | 0.88 (0.87–0.88) | 0.88 (0.88–0.88) |
| Severe | 0.86 (0.85–0.86) | 0.86 (0.86–0.87) |
| Activities of daily living | ||
| Independent | Reference | Reference |
| Modified independence | 0.95 (0.95–0.95) | 0.95 (0.95–0.95) |
| Dependent | 0.99 (0.98–0.99) | 0.98 (0.98–0.99) |
| Length of stay, months | ||
| ≤5 | Reference | Reference |
| 6–11 | 1.02 (1.01–1.02) | 1.02 (1.01–1.02) |
| 12–23 | 1.02 (1.02–1.03) | 1.02 (1.02–1.03) |
| ≥24 | 1.03 (1.02–1.03) | 1.03 (1.02–1.03) |
|
| ||
| Nursing home characteristics | ||
| Member of a chain | 1.01 (1.01–1.02) | |
| Ownership | ||
| Government | 0.99 (0.98–1.00) | |
| For Profit | Reference | |
| Not for Profit | 1.02 (1.01–1.03) | |
| Beds | ||
| ≥200 beds | 1.01 (1.00–1.02) | |
| 100 to <200 beds | Reference | |
| 50 to <100 beds | 1.00 (0.99–1.01) | |
| <50 beds | 0.97 (0.95–0.98) | |
| Occupancy, % | ||
| ≥95 | Reference | |
| 90 to <95 | 1.00 (0.99–1.01) | |
| 80% to <90 | 1.00 (0.99–1.01) | |
| <80 | 1.00 (0.99–1.01) | |
| Location | ||
| Rural | 0.98 (0.97–0.99) | |
| % Skilled nursing/short stay, % | ||
| ≥60 | 1.04 (1.03–1.04) | |
| 50–59 | 1.03 (1.02–1.04) | |
| 40–49 | 1.03 (1.02–1.03) | |
| ≤39 | Reference | |
|
| ||
| Alzheimer's specialty care beds | 0.98 (0.98–0.99) | |
| % w/Alzheimer's disease/dementia, % | ||
| ≥60 | 0.93 (0.92–0.95) | |
| 50–59 | 0.97 (0.96–0.98) | |
| 40–49 | 0.98 (0.98–0.99) | |
| ≤39 | Reference | |
|
| ||
| Nursing home staffing variables | ||
| Nurse practitioners/physician assistants | 1.00 (1.00–1.01) | |
| Adjusted direct care staff <3 per resident/day | 0.99 (0.98–1.00) | |
| Adjusted RN <0.5 h per resident/day** | 1.00 (0.99–1.00) | |
| RN staffing star rating** | ||
| 1 | 1.00 (0.99–1.01) | |
| 2 | 1.02 (1.01–1.02) | |
| 3 | 1.02 (1.01–1.03) | |
| 4 | 1.02 (1.01–1.02) | |
| 5 | Reference | |
| Overall staffing star rating** | ||
| 1 | 1.01 (0.99–1.02) | |
| 2 | 1.01 (1.00–1.02) | |
| 3 | 1.02 (1.01–1.03) | |
| 4 | 1.01 (1.00–1.02) | |
| 5 | Reference | |
| Overall star rating | ||
| 1 | 0.99 (0.98–1.00) | |
| 2 | 0.99 (0.98–1.00) | |
| 3 | 0.99 (0.99–1.00) | |
| 4 | 0.99 (0.98–1.00) | |
| 5 | Reference | |
Adjusted for all variables in the column, marital status, and clustering of residents in nursing homes using generalized estimating equations. Race/ethnicity was not included in the resident and nursing home factor model due to issues with convergence.
Estimates for overall staffing rating, RN staffing rating, and adjusted RN <0.5 h per resident/day were adjusted only for resident-level factors owing to model convergence issues and multicol-linearity.
Discussion/Conclusion
We found that the SCI is a reliable instrument to measure social connectedness in nursing home residents with ADRD and the results herein provide additional evidence in support of its validity. In a national sample of nursing home residents with ADRD, more than three quarters had high social connectedness. We hypothesized that resident and facility factors would be associated with high social connectedness, and our study provided empirical evidence in support of most of our hypotheses.
The most striking findings from this study related to the relationship between measures germane to ADRD. As we hypothesized, resident severity of cognitive impairment, living in a nursing home with a special care dementia unit, and living in a nursing home with higher percentage of residents with ADRD were each independently associated with decreased odds of social connectedness. That severity of cognitive impairment was associated with decreased odds of high social connectedness was not surprising given that people with ADRD may be susceptible to social isolation due to their cognitive impairment [6]. There are several reasons that may explain why our findings contrast with findings from a recent systematic review focused on special care dementia units [18]. Our data did not permit us to identify who actually received care in a special care unit. Care practices from the dementia special care unit do not appear to diffuse to residents who are not in the special care dementia unit [27]. There is great variability in how nursing homes operationalize the concept of specialty care for dementia. Some evidence suggests that care is different in special care units but may not be better [28, 29].
We hypothesized that residents who had been in a nursing home longer would have greater odds of high social connectedness relative to those who recently entered the nursing home, and this hypothesis was supported by our findings. With staff, residents develop relationships as an unintentional consequence of clinical interactions, and the nature of these interactions strongly influences the degree to which residents perceive these relationships as friendly or unfriendly [30]. Relationships between residents and staff are often oriented around strategies to meet needs and avoid conflict, but dialog and active listening can result in deeper caring relationships [31]. Staff intentionality about developing relationships, such as acknowledging residents as special or providing “extras,” fostered more positive relationships with residents [32]. Relationships between staff and residents likely vary by the context of the nursing home itself. In a nursing home serving an affluent population, staff may be more aware of resident needs and may employ relationship-oriented problem-solving approaches to help better meet resident needs [33]. More work to understand the impact of nursing home context on social interactions is needed.
We found that several of our hypothesized nursing home factors were associated with high social connectedness with the exception of quality star ratings and use of nurse practitioners and physician assistants. Our findings are consistent with some (but not all [34]) literature that supports the link between characteristics of nursing homes and differences in important outcomes. For example, Connecticut nursing homes with more RNs and higher quality ratings had fewer COVID-19 cases and deaths [35]. Other studies have suggested that antipsychotic medications [36], hospitalization rates [37], functional improvement [38], and infection rates [39] were related to nursing home characteristics. It is possible that nurse practitioner and physician assistant roles vary among nursing homes [40], and in some settings may involve less direct patient care compared to other providers (e.g., nursing assistants) thus, the presence (or absence) of NP/PAs would result in minimal change in resident social connectedness. With respect to the lack of consistent associations across multiple quality measures, this may be due to poor reliability and validity of star ratings for predicting quality outcomes as the star rating system remains controversial [41, 42]. Thus, it was not surprising that the star ratings were not associated with SCI scores.
Considering our findings in light of alterative definitions of social connection is useful. Holt-Lunstad [43] posits that social connection is a continuous multifactorial risk factor with components related to structure, function, and quality with low levels of these components associated with risk and high levels associated with protection from adverse health outcomes. How this contextualization differs in the nursing home relative to community-dwelling older adults and how it may differ in light of the significant cognitive impairment residents with ADRD needs further development. Nevertheless, our findings may offer more insights with respect to this contextualization of social connection. Of the three domains (i.e., structure, function, and quality), we believe the SCI most closely aligns with the quality domain as quality relates to the sense of connection to others that is based on positive and negative qualities. The specific MDS 3.0 items included in the SCI appear to capture dimensions of quality. The development of the SCI was guided by an ecologic framework [44]. We originally considered a wide array of items consistent with the individual and relational domains specified by the ecologic framework which also could be thought to fall under the structure (connection to others via the existence of relationships and their roles) and function (sense of connection that results from actual or perceived support or inclusion) domains. However, these items did not reach the threshold for inclusion in the final SCI measure. Our study did explore the association between some factors that may be associated with quality, structure (e.g., size of network, number of social roles, whether a person lives alone or with others), and function (e.g., received or perceived availability of social support, resources, and aid). With respect to quality, we believe that the finding that residents who had been in a nursing home longer had greater odds of high social connectedness relative to those who recently entered the nursing supports this domain as this finding suggests that staff and residents develop relationships as they get to know each other through day-to-day interactions that occur as a result of care provision. With respect to structure, by definition, all nursing home residents live in a congregate setting. The MDS 3.0 provides no information about number of social roles. Our study found no association between the size of the facility and the SCI. We recognize that it is a poor proxy of size of network, but the MDS 3.0 lacks items to capture the actual network size. With respect to function, measures of hours per resident per day of care provision (as proxies for resources and aid) were not associated with SCI. However, we only evaluated the average hours per day of care rather than the exact number of hours of care each resident received because such detailed information was not available. More research to explore different conceptualizations of social connectedness in the nursing home context with residents with ADRD is needed.
Our findings must be considered with strengths and limitations in mind. Our study is national, but the most recent data available pre-dates the COVID-19 pandemic. Given the dramatic impact of COVID-19 on care in this setting, research with contemporaneous data is warranted. We developed a measure of social connectedness based on items routinely collected on the MDS 3.0. The MDS 2.0-Index of Social Engagement [45] and Revised Index of Social Engagement [46] offer different perspectives on social connectedness. Unfortunately, the MDS 2.0 items on which the social engagement scales were developed have no direct analogue in MDS 3.0. Social disconnection could be conflated with dementia-related behaviors when using the SCI to define social connection. As such, the finding of an association between SCI score and ADRD-related indicators may also suggest that this conflation is occurring. Additional work to understand the operating characteristics of the SCI in contemporaneous data resources is needed.
Conclusions
One in four residents with ADRD had low/moderate social connectedness. The longer the residents were in the nursing home, their odds of high social connectedness increased suggesting that interventions to help residents with ADRD transition to their new environment and make new social connections may be effective. Individual characteristics indicated that men, those in younger age groups and those with moderate to severe cognitive impairment had decreased odds of high social connectedness. Future work on interventions should consider targeting these groups. Further, we found that residents with ADRD who live in homes with special care dementia units and a greater proportion of residents with ADRD had decreased odds of high social connectedness. Interventions to promote social connectedness in these settings should also be prioritized.
Statement of Ethics
The University of Massachusetts Chan Medical School Institutional Review Board reviewed and approved this study protocol, approval number H00022181. The University of Massachusetts Chan Medical School Institutional Review Board granted a waiver of informed consent because the data resource was de-identified.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This work was supported by grants to Dr. Lapane from the National Institute of Nursing Research (R01NR016977) and the National Institute on Aging (R01AG071692). The funders had no role in the preparation of the data or the manuscript.
Author Contributions
Dr. Kate L. Lapane obtained funding for the study, acquired the data used in the study, participated in the design of the study, verified the coding of the study, interpreted the analysis, and drafted the manuscript. Dr. Catherine E. Dubé assisted in obtaining funding and acquiring the data, drafted parts of the manuscript, and provided critical feedback on the analyses and manuscript. Dr. Carol Bova led the development of the index used, participated in the design of the study, drafted portions of the manuscript, interpreted the data, and provided critical review of the manuscript. Dr. Bill M. Jesdale conducted the analysis, developed the tables, drafted parts of the manuscript, interpreted the analyses, and provided critical feedback on the manuscript.
Data Availability Statement
Data for these analyses were obtained by the authors through a data user agreement with the U.S. Centers for Medicare and Medicaid Services. Individual researchers can access the data by purchasing the data through Research Data Assistant Center at https://resdac.org/.
References
- 1.Zissimopoulos J, Crimmins E, St Clair P. The value of delaying Alzheimer's disease onset. Forum Health Econ Policy. 2014 Nov;18((1)):25–39. doi: 10.1515/fhep-2014-0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arrighi HM, Neumann PJ, Lieberburg IM, Townsend RJ. Lethality of Alzheimer disease and its impact on nursing home placement. Alzheimer Dis Assoc Disord. 2010 Jan–Mar;24((1)):90–5. doi: 10.1097/WAD.0b013e31819fe7d1. [DOI] [PubMed] [Google Scholar]
- 3.Taylor CA, Greenlund SF, McGuire LC, Lu H, Croft JB. Deaths from Alzheimer's disease - United States, 1999–2014. MMWR Morb Mortal Wkly Rep. 2017;66((20)):521–6. doi: 10.15585/mmwr.mm6620a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bergland A, Kirkevold M. The significance of peer relationships to thriving in nursing homes. J Clin Nurs. 2008;17((10)):1295–302. doi: 10.1111/j.1365-2702.2007.02069.x. [DOI] [PubMed] [Google Scholar]
- 5.Abbott KA, Pachucki MC. Associations between social network characteristics, cognitive function, and quality of life among residents in a dementia special care unit: a pilot study. Dementia. 2017;16((8)):1004–19. doi: 10.1177/1471301216630907. [DOI] [PubMed] [Google Scholar]
- 6.Savikko N, Routasalo P, Tilvis R, Strandberg T, Pitkälä KH. Predictors and subjective causes of loneliness in an aged population. Arch Gerontol Geriatr. 2005;41((3)):223–33. doi: 10.1016/j.archger.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 7.Casey AN, Low LF, Jeon YH, Brodaty H. Residents perceptions of friendship and positive social networks within a nursing home. Gerontologist. 2016;56((5)):855–67. doi: 10.1093/geront/gnv146. [DOI] [PubMed] [Google Scholar]
- 8.Kovach SS, Robinson JD. The roommate relationship for the elderly nursing home resident. J Soc Pers Relat. 1996;13((4)):627–34. [Google Scholar]
- 9.Mok Z, Müller N. Staging casual conversations for people with dementia. Dementia. 2014;13((6)):834–53. doi: 10.1177/1471301213488609. [DOI] [PubMed] [Google Scholar]
- 10.Bonifas RP, Simons K, Biel B, Kramer C. Aging and place in long-term care settings: influences on social relationships. J Aging Health. 2014;26((8)):1320–39. doi: 10.1177/0898264314535632. [DOI] [PubMed] [Google Scholar]
- 11.McCormack B, McCance TV. Development of a framework for person-centred nursing. J Adv Nurs. 2006;56((5)):472–9. doi: 10.1111/j.1365-2648.2006.04042.x. [DOI] [PubMed] [Google Scholar]
- 12.Koren MJ. Person-centered care for nursing home residents: The culture-change movement. Health Aff. 2010;29((2)):312–7. doi: 10.1377/hlthaff.2009.0966. [DOI] [PubMed] [Google Scholar]
- 13.Lee RM, Robbins SB. Measuring belongingness: the social connectedness and the social assurance scales. J Counsel Psychol. 1995;42((2)):232–41. [Google Scholar]
- 14.Kohut H. How does Analysis Cure? New York: International Universities Press; 1984. [Google Scholar]
- 15.Bova CA, Jesdale BM, Mbrah A, Botelho L, Lapane KL. Development and psychometric evaluation of the Social Connectedness Index in nursing home residents with Alzheimer's disease and dementia using the minimum data set 3.0. Int J Geriatr Psychiatry. 2021 Jul;36((7)):1110–9. doi: 10.1002/gps.5516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Medicare and Medicaid Services (CMS) CMS nursing home data. 2021. Available from https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data/bkwz-xpvg (accessed September 23, 2021)
- 17.LeVasseur AL. Effects of social isolation on a long-term care resident with dementia and depression during the COVID-19 pandemic. Geriatr Nurs. 2021 May-Jun;42((3)):780–1. doi: 10.1016/j.gerinurse.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adlbrecht L, Bartholomeyczik S, Hildebrandt C, Mayer H. Social interactions of persons with dementia living in special care units in long-term care: a mixed-methods systematic review. Dementia. 2021 Apr;20((3)):967–84. doi: 10.1177/1471301220919937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for medicare & medicaid services . Centers for medicare & medicaid services long-term care facility resident assessment instrument 3.0 user's manual. U.S. Department of Health & Human Services; 2015. [Google Scholar]
- 20.Centers for Medicare & Medicaid Services (CMS) Nursing home compare: 2016 annual files. Nursing home compare data archive. 2016. Available from https://data.medicare.gov/data/archives/nursing-home-compare (accessed November 16, 2021)
- 21.Centers for Medicare & Medicaid Services (CMS) Provider of Services (POS): 2016 POS File. 2016. Available from https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/Provider-of-Services/POS2016.html (accessed November 16, 2021)
- 22.Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999;54((11)):M546–53. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- 23.Thomas KS, Dosa D, Wysocki A, Mor V. The minimum data Set 3.0 cognitive function scale. Med Care. 2015;55((9)):e68–72. doi: 10.1097/MLR.0000000000000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Unruh L, Wan TT. A systems framework for evaluating nursing care quality in nursing homes. J Med Syst. 2004 Apr;28((2)):197–214. doi: 10.1023/b:joms.0000023302.80118.74. [DOI] [PubMed] [Google Scholar]
- 25.Bostick JE, Rantz MJ, Flesner MK, Riggs CJ. Systematic review of studies of staffing and quality in nursing homes. J Am Med Dir Assoc. 2006 Jul;7((6)):366–76. doi: 10.1016/j.jamda.2006.01.024. [DOI] [PubMed] [Google Scholar]
- 26.Mack DS, Baek J, Tjia J, Lapane KL. Geographic variation of statin use among US nursing home residents with life-limiting illness. Med Care. 2021 May 1;59((5)):425–36. doi: 10.1097/MLR.0000000000001505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gruneir A, Lapane KL, Miller SC, Mor V. Does the presence of a dementia special care unit improve nursing home quality? J Aging Health. 2008 Oct;20((7)):837–54. doi: 10.1177/0898264308324632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gruneir A, Lapane KL, Miller SC, Mor V. Is dementia special care really special? A new look at an old question. J Am Geriatr Soc. 2008 Feb;56((2)):199–205. doi: 10.1111/j.1532-5415.2007.01559.x. [DOI] [PubMed] [Google Scholar]
- 29.Cadigan RO, Grabowski DC, Givens JL, Mitchell SL. The quality of advanced dementia care in the nursing home: the role of special care units. Med Care. 2012 Oct;50((10)):856–62. doi: 10.1097/MLR.0b013e31825dd713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roberts T, Bowers B. How nursing home residents develop relationships with peers and staff: a grounded theory study. Int J Nurs Stud. 2015;52((1)):57–67. doi: 10.1016/j.ijnurstu.2014.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palacios-Ceña D, Losa-Iglesias ME, Gómez-Calero C, Cachón-Pérez JM, Brea-Rivero M, Fernández-de-las-Peñas C. A qualitative study of the relationships between residents and nursing home nurses. J Clin Nurs. 2014;23((3–4)):550–9. doi: 10.1111/jocn.12202. [DOI] [PubMed] [Google Scholar]
- 32.Roberts TJ. Nursing home resident relationship types: what supports close relationships with peers & staff? J Clin Nurs. 2018;27((23–24)):4361–72. doi: 10.1111/jocn.14554. [DOI] [PubMed] [Google Scholar]
- 33.Ryvicker M. Staff-resident interaction in the nursing home: an ethnographic study of socio-economic disparities and community contexts. J Aging Stud. 2011;25((3)):295–304. [Google Scholar]
- 34.Field TS, Fouayzi H, Crawford S, Kapoor A, Saphirak C, Handler SM, et al. The association of nursing home characteristics and quality with adverse events after a hospitalization. J Am Med Dir Assoc. 2021;22((10)):2196–200. doi: 10.1016/j.jamda.2021.02.027. [DOI] [PubMed] [Google Scholar]
- 35.Li Y, Temkin-Greener H, Shan G, Cai X. COVID-19 infections and deaths among connecticut nursing home residents: facility correlates. J Am Geriatr Soc. 2020;68((9)):1899–906. doi: 10.1111/jgs.16689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hughes CM, Lapane KL, Mor V. Influence of facility characteristics on use of antipsychotic medications in nursing homes. Med Care. 2000 Dec;38((12)):1164–73. doi: 10.1097/00005650-200012000-00003. [DOI] [PubMed] [Google Scholar]
- 37.Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. J Am Geriatr Soc. 2004;52((10)):1730–6. doi: 10.1111/j.1532-5415.2004.52469.x. [DOI] [PubMed] [Google Scholar]
- 38.Spector WD, Takada HA. Characteristics of nursing homes that affect resident outcomes. J Aging Health. 1991;3((4)):427–54. doi: 10.1177/089826439100300401. [DOI] [PubMed] [Google Scholar]
- 39.Zimmerman S, Gruber-Baldini AL, Hebel JR, Sloane PD, Magaziner J. Nursing home facility risk factors for infection and hospitalization: importance of registered nurse turnover, administration, and social factors. J Am Geriatr Soc. 2008;50((12)):1987–95. doi: 10.1046/j.1532-5415.2002.50610.x. [DOI] [PubMed] [Google Scholar]
- 40.Rapp MP. Opportunities for advance practice nurses in the nursing facility. J Am Med Dir Assoc. 2003 Nov–Dec;4((6)):337–43. doi: 10.1097/01.JAM.0000095253.60570.43. [DOI] [PubMed] [Google Scholar]
- 41.Center for Medicare Advocacy Nursing facilities' “quality measures” do not reflect actual quality of care provided to residents. 2018. Available from https://medicareadvocacy.org/nursing-facilities-quality-measures-do-not-reflect-actual-quality-of-care-provided-to-residents/ (accessed December 1, 2021)
- 42.Flynn M. SNF star ratings matter: nursing homes with high ratings produce better outcomes. Skilled Nursing News; 2019. Jun 18, Available from https://skillednursingnews.com/2019/06/snf-star-ratings-matter-nursing-homes-with-high-ratings-produce-better-outcomes/ (accessed December 1, 2021) [Google Scholar]
- 43.Holt-Lunstad J. The major health implications of social connection. Curr Dir Psychol Sci. 2021;30((3)):251–9. [Google Scholar]
- 44.Cottrell N, Buffel T, Phillipson C. Preventing social isolation in older people. Maturitas. 2018;113((1873–4111)):80–4. doi: 10.1016/j.maturitas.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 45.Mor V, Branco K, Fleishman J, Hawes C, Phillips C, Morris J, et al. The structure of social engagement among nursing home residents. J Gerontol B Psychol Sci Soc Sci. 1995;50:P1–8. doi: 10.1093/geronb/50b.1.p1. [DOI] [PubMed] [Google Scholar]
- 46.Gerritsen DL, Achterberg WP, Steverink N, Pot AM, Frijters DHM, Ribbe MW. The MDS challenging behavior profile for long-term care. Aging Ment Health. 2008;12:116–23. doi: 10.1080/13607860701529882. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data for these analyses were obtained by the authors through a data user agreement with the U.S. Centers for Medicare and Medicaid Services. Individual researchers can access the data by purchasing the data through Research Data Assistant Center at https://resdac.org/.