Highlights
-
•
The review evaluated internal and external validity using the rE-AIM Framework.
-
•
Results indicate an overall low reporting of validity factors.
-
•
Information on adoption and maintenance was particularly low.
-
•
Future studies should improve the reporting across all rE-AIM dimensions.
-
•
Future studies should consider adaptations during the implementation phase.
Keywords: Physical activity, External validity, Socioeconomic disadvantage, RE-AIM
Abstract
The promotion of physical activity in people from lower social strata is a public health priority. Previous reviews of physical activity interventions among socioeconomically disadvantaged adults have focused on intervention effectiveness without considering their translation into practice. This review utilised the RE-AIM framework (Reach, Efficacy/Effectiveness, Adoption, Implementation, Maintenance) to (1) evaluate the extent to which experimental and non–/quasi-experimental trials of interventions to promote physical activity among socioeconomically disadvantaged adults report on issues of internal and external validity and (2) to provide recommendations for future intervention studies.
Four databases were searched through June 2021. We included studies published in English or German since 2000 that tested physical activity interventions for socioeconomically disadvantaged adults. Two researchers coded all studies using a validated RE-AIM data extraction tool with 61 indicators referring to internal and external validity. Binary coding (yes = 1/no = 0) was applied to calculate the number and percentage of studies reporting each of the indicators.
We included 39 studies of which 22 were non–/quasi-experimental trials. Indicators of reach were most frequently reported (59.2%), followed by implementation (38.9%) and efficacy/effectiveness (28.9%). Dimensions related to external validity were least frequently reported (adoption: 21.9%, maintenance: 17.8%). Few differences were found between experimental and non–/quasi-experimental trials.
Analysis showed overall poor reporting of components related to internal and external validity. We recommend that future research should increase attention on reporting indicators of internal and external validity to facilitate their translation and implementation into real world settings.
Trial registration: The review was registered with PROSPERO (CRD42021283688).
1. Introduction
1.1. Background
There is a considerable socioeconomic gradient in physical activity participation and associated health outcomes (O’Donoghue et al., 2018). Socioeconomically disadvantaged individuals are less likely to meet public health guidelines for recommended levels of physical activity and perceive higher barriers to an active lifestyle compared to those who are more affluent (Gidlow et al., 2006, Gray et al., 2016). The term socioeconomic disadvantage covers indicators such as low income, low educational attainment, low job status, or living in socioeconomically disadvantaged areas (Ball et al., 2015). Previous studies show consistent findings regarding insufficient engagement in physical activity for these common indicators at both, area- and individual-levels (Beenackers et al., 2012, Bull et al., 2020). In Germany, for example, studies showed a higher risk of physical inactivity in people with low income (Nocon et al., 2007) which is defined as income below the threshold of two thirds of the German median income (German Institute for Economic Research., 2022).
Regular and sufficient physical activity is an indispensable pillar regarding the prevention and treatment of mental and physical diseases (Warburton and Bredin, 2017). Consequently, the social gradients in physical activity appears to contribute to pronounced health inequalities. Insufficient physical activity poses a major threat to the health of socioeconomically disadvantaged individuals, and, as a consequence, has a strong impact on the health care system (Wen and Wu, 2012). Thus, the promotion of physical activity in socioeconomically disadvantaged communities is a major priority in public health (Ball et al., 2015). This has been addressed in recent years by developing and implementing various policies and interventions based on individual-, group-, and community-levels (Müller-Riemenschneider et al., 2009).
Interventions to promote physical activity for socioeconomically disadvantaged individuals have been studied primarily in terms of their effectiveness (Cleland et al., 2013, Cleland et al., 2012). Craike et al. (Craike et al., 2018) summarized earlier research across all age groups in their umbrella review. They found inconclusive evidence for the effectiveness among adults and recommended to also consider indicators that go beyond internal validity for future research. This claim is supported by research that, while effective physical activity interventions have been implemented in small-scale, controlled settings, there is little evidence that effective interventions have been successfully implemented and widely adopted beyond the research setting (Hallal et al., 2012).
One reason for the lack of implementation is that the scientific approach emphasizes high internal validity, which refers to the extent to which differences identified between groups are a result of the intervention being tested, at the expense of external validity, which refers to the extent to which study results can be applied in other individuals or settings (Estabrooks and Gyurcsik, 2003, Eldridge et al., 2008). It has been indicated that the absence of analysing external validity is associated with a lack of generalisability and transferability of research into health promotion practice or its impact on public health (Glasgow et al., 2003). As a reason, increased attention has been focused on the importance of health behaviour change interventions also demonstrating external validity (Steckler and McLeroy, 2008).
Glasgow et al. (Glasgow et al., 1999) developed the RE-AIM framework (Reach, Efficacy/Effectiveness, Adoption, Implementation, Maintenance) to provide a comprehensive evaluation tool for indicators of internal and external validity that has become a public health standard for investigating if and how interventions create public health impact (Glasgow et al., 1999). The balanced and consistent reporting of internal and external validity could lead to a better understanding of complexity, improve generalisability of efficacy trials, and speed up the translation of behavioural interventions into sustained practice (Glasgow et al., 2019).
RE-AIM is an acronym for five defined dimensions. Reach measures participation on the individual-level and refers to the proportion and representativeness of a given population in a study. The dimension efficacy/effectiveness determines the impact of an intervention, possible positive or negative consequences, and outcomes related to quality of life, such as physical activity. Adoption assesses the proportion and representativeness of staff and setting willing to initiate and adopt an intervention. The fourth dimension, Implementation, refers to the extent to which the intervention protocol was delivered as intended including time and costs of the intervention. Maintenance considers the sustainability of individual- and organizational-level components in an intervention. It further refers to the sustainability of an intervention in the setting in which it took place (Glasgow et al., 1999, Gaglio et al., 2013). The RE-AIM approach has already been used to extensively evaluate various health behaviour interventions (Cuthbert et al., 2017, Bhuiyan et al., 2019, McGoey et al., 2016). For example, previous RE-AIM reviews reported on internal and external validity factors of different types of physical activity interventions (Paez et al., 2015) and interventions targeting different populations (Bhuiyan et al., 2019, Kennedy et al., 2021, Galaviz et al., 2014). In summary, these studies draw the conclusion that inadequate reporting results in a lack of information about for whom and under what conditions physical activity programs were successful. Translating interventions into practice is challenging, especially in relation to the group of socioeconomically disadvantaged individuals who require highly context-dependent interventions. However, systematically assessing indicators of external validity enables researchers to draw conclusions about the generalisability of study results to disadvantaged and deprived populations. In order for successful implementation of evidence-based interventions in these complex target groups, as well as, scaling them up and embedding them in different settings, it is crucial to investigate the internal and external validity of interventions (Cleland et al., 2013). To our knowledge, no earlier review has specifically addressed issues related to external validity of research on physical activity interventions for socioeconomically disadvantaged adults.
1.2. Aim of the study
To fill this research gap, the purpose of the present study is (1) to apply the RE-AIM framework to comprehensively assess the extent to which experimental and non–/quasi-experimental trials of interventions that promote physical activity among socioeconomically disadvantaged adults have reported dimensions of internal and external validity and (2) to provide recommendations for future physical activity intervention studies.
2. Method
2.1. Protocol and registration
This systematic review was registered with the PROSPERO international prospective register of systematic reviews (registration number: CRD42021283688) and adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines. The PRISMA checklist is available in the Additional file A.
2.2. Eligibility criteria
We included published full-text studies that met the inclusion criteria described in Table 1. We included all intervention studies promoting physical activity among socioeconomically disadvantaged individuals. The intervention must have been developed specifically for this target group and include predominately participants with socioeconomic disadvantage. Studies were excluded if 1) promoting physical activity was not one of the study’s main objectives, 2) they did not report on physical activity outcomes or only reported on changes in physical function measures (e.g., muscles function, gait speed, grip strength) 3) they had no clear definition of socioeconomic disadvantage and 4) the study targeted participants aged < 18 years or with a specific disease or condition (e.g. diabetes, cardiovascular disease, obesity), pregnant women, athletes, or sport students. Studies on the treatment of obesity were excluded, whereas studies on the prevention of obesity with the focus on increasing physical activity were included.
Table 1.
Study inclusion criteria.
| Data type | Inclusion criteria |
|---|---|
| Population | Predominately adults aged ≥ 18 years |
| Language | English, German |
| Intervention | All interventions Targeted towards people experiencing socioeconomic disadvantage, including studies for people with low socioeconomic status, low education level, low income, low status occupations or living in an area of low socioeconomic status1. We accepted each study’s definition of socioeconomic disadvantage due to the lack of a universally accepted definition and cut-points. With the promotion of PA is one of the study’s defined main objectives. |
| Control condition | Any control group (not limited to no intervention/contact, active control, wait list control or participants as their own control i.e. pre-and post-measure) |
| Outcome | Any statistically analysed PA outcome and outcomes considered to be closely related to physical activity (e.g., cardiorespiratory fitness, exercise) measured at baseline and at least one point post-intervention with no restriction on type of PA assessment (subjective, objective). |
| Study design | Experimental, quasi-experimental, non-experimental |
“area of low socioeconomic status” is defined as an area, neighbourhood, or community whose residents are considered disadvantaged compared to the overall population.
2.3. Search strategy
We developed the search strategy in collaboration with a professional librarian. An example search string can be found in the Additional file B. Four electronic databases (PubMed, Web of Science, PsycINFO and SPORTDiscus) were searched. Due to practical reasons, the search was limited to original research studies that tested the effectiveness of physical activity interventions published in German or English language from 2000 and listed in the databases on June 10, 2021. The reference lists of similar reviews and the included full-text articles were further hand searched to identify additional articles meeting the inclusion criteria [e.g., Cleland et al., 2012; Cleland et al., 2013]. The included full-text articles were also searched for companion articles. Companion articles are those that are related to the primary study and that may include additional intervention details (e.g., study protocols, cost-effectiveness studies, qualitative studies reporting on additional RE-AIM indicators). Companion articles were not counted as included articles but were used for data extraction and are listed in the data extraction coding tool.
2.4. Study selection
The search results were managed using “Covidence” software. We downloaded the citation details for all articles (e.g., year of publication, authors, journal name, title, abstract). Duplicates of articles were deleted. Two reviewers (SL and SF) independently assessed all titles and abstracts identified in the search process for suitability. Both reviewers then independently reviewed the full texts of the remaining articles against inclusion and exclusion criteria. All disagreements were discussed in depth until consensus was reached. Reasons for exclusion were documented at the abstract and full-text screening stage. The Kappa statistic (Cohen, 1960) was calculated to evaluate inter-rater reliability. The average Kappa statistic for consistency of coding was 0.81, indicating strong inter-rater reliability.
2.5. Data extraction and rE-AIM coding protocol and scoring
Two reviewers (SL and SF) extracted the data. Key study characteristics were extracted including study design, sociodemographic characteristics, intervention details (sample size, study design, control group, duration), physical activity outcomes and measures as well as intervention effects (Table 2).
Table 2.
Individual study characteristics of the 39 studies included in the review separated into experimental and non–/quasi-experimental trials.
| Authors (year) |
Sample description (N, mean age, % female) |
Control group | Length, Intervention |
Type of PA, Measures |
Main PA results | Theoretical foundation |
|---|---|---|---|---|---|---|
| Experimental trials | ||||||
| Albright et al. (Albright et al., 2005) | Low-income, ethnic minority women (N = 72, mean age 32.1, 100 % female) |
AC (2 month weekly 1-hr classes, then mailed newsletters) | 12 month Phone + Mail Counselling: 2 months of weekly 1-hr classes, then home-based telephone counselling for PA + information & feedback via mailed newsletters |
TEE 7-Day PAR |
IG: significantly greater increases in estimated total energy expenditure compared to CG (p <.05) after 10 month. | SCT, TTM |
| Armitage et al. (2010) (Armitage and Arden, 2010) |
People with low SES (N = 68, mean age 27.5, 49 % women) |
AC (volitional help sheet, no instructions) | 4 weeks IG received a volitional help sheet with explicit instructions to linked occasions on which IG was tempted not to be physically active with appropriate behavioural responses (process of change) |
PA (MET-min/week) IPAQ |
Significant increase in PA in IG relative to CG, F(1, 66) = 7.28, p < 0.01. | Theory of implementation intentions, Processes of Change |
| Cohen et al. (Cohen et al., 2017) | Residents near high-poverty neighbourhood parks (N = 1445, mean age 43.3, 62 % female) |
CG (no intervention) | 6 month IG1 (free PA classes for adults over 6 month); IG2 (frequent user program where adults could win prizes based upon the number of park-visits); IG3 (combination of both programs) |
Park-level use, park-based PA (MET scores) SOPARC |
No statistically significant increases in overall park-level use and park-based PA, no differences across study arms. |
None |
| Colenman et al. (2012) (Coleman et al., 2012) |
Low-income, Hispanic females (N = 1093, mean age 52, 100 % female) |
CG (usual care) | 12 month Culturally tailored adaption of the WISEWOMEN program including three one-on-one counselling sessions delivered by community health workers |
MPA, VPA PAA (adapted) |
IG: significant increases in moderate (71 %, baseline; 84 %, follow-up, p <.001) and vigorous (13 % to 33 %, p <.001) PA; CG: no significant changes in moderate (p =.57) and vigorous (p =.58) PA | TTM |
| Fahren-wald et al. (2004) (Fahrenwald et al., 2004) |
MA women (N = 44, mean age 26.5, 100 % women) |
AC (counselling on self-breast examination) | 8 weeks “Moms on the Move” promotora (community health worker) -led intervention on the U.S. Mexico border |
PA (min/week); EE/day; MPA (min/week), step counts 7-day PAR, Digi-Walker SW-200 Step Counter |
IG had greater PA behavior: PA, F(1, 42) = 46.85, p <.001; daily energy expenditure, F(1, 42) = 23.01, p <.001; MPA, F(1, 42) = 32.63, p <.001. IG subgroup (n = 11) step counts increased pre–post,t(10) = 6.16,p <.001 | TTM |
| Goyder et al. (Goyder et al., 2014) | Adults in deprived areas (N = 282, mean age 54.6, 53.9 % female) |
CG (inactive) | 3 month IG1 (“full booster”: 2 face-to-face sessions of PA booster consultations in MI-style); IG2 (“mini booster”: 2 telephone-sessions of PA booster consultations in MI-style) |
TEE/day Actihead device (accelerometer) |
mean difference in TEE/day between baseline and 3 months post randomization was not significant between CG and IG1 and IG2 (p = 0.57) | TTM |
| Hovell et al. (Hovell et al., 2008) | Low-income Latinas (N = 151, mean age 31.4, 100 % female) |
AC (18 safety education sessions over 6 month) | 6 month, 12-month FU 3 sessions per week of supervised aerobic dance (exercise component + education component) |
Moderate/vigorous exercise, walking Project GRAD survey |
6-month: IG showed significantly more vigorous exercise (p <.001) and walking (p =.005) than CG. 12-month FU: vigorous exercise was higher in the IG (p =.001) | None |
| Kendzor et al. (Kendzor et al., 2017) | Homeless adults (N = 32, mean age 48.4, 25 % female) |
CG (assessment only) | 4 weeks Diet and PA intervention (tailored educational newsletters + fruit/vegetable snacks + pedometers |
MVPA (min/day) BRFSS, Actigraph GT3X |
IG: significantly greater accelerometer-measured daily MVPA (p <.001) than CG (Md = 60 daily min. vs 41 daily min.). | None |
| Keyserling et al. (Keyserling et al., 2008) | Low-income mid-life women (N = 236, mean age 53, 100 % female) |
CG (minimum intervention) | 12 month (also measure at 6-month) Enhanced WISEWOMAN intervention with components: individual counselling, group sessions, phone contacts, reinforcement mailings, community resource linkage |
MPA (min/week), LPA (min/week), VPA (min/week) Actigraph accelerometer, New Leaf PAA |
Accelerometer: no statistically difference of MPA between IG and CG (p = 0.45; multivariate model, p = 0.08); Self-report: greater MPA in IG (p = 0.01; multivariate model, p = 0.001). | Chronic Care Model (intervention conceptual framework) |
| Lowther et al. (Lowther et al., 2002) | Community population high in social and economic deprivation N = 370, mean age 40.9, 64 % female) |
AC (CG1: fitness assessment; CG2: exercise consultation) | 12 month (immediate effect at 4 weeks, 3 month; long-term effect at 6 month, 12 month) IG1 (fitness assessment) ;IG2 (exercise consultation) |
LTPA (min/week) Scot-PASQ |
LTPA increased significantly from baseline to 4 weeks for both RCTs and maintained 3 months post-test for both. Only IG2 significantly increased LTPA after 12 month. |
None |
| Marcus et al. (Marcus et al., 2013) | Predominately low-income Latinas (54 % family-income <$20,000 per year) (N = 266, mean age 40.7, 100 % female) |
CG (wellness contact control) | 6 month Culturally adapted, Spanish-language, individually tailored, computer expert system–driven PA print-based intervention including regular mailing of PA manuals, individually tailored feedback reports. |
MVPA (min/week) 7-Day PAR, accelerometer |
Increases in MVPA were significantly greater in the IG compared to CG (mean difference = 41.36, SE = 7.93, p <.01). The difference was corroborated by accelerometer (rho = 0.44, p < 0.01). |
SCT, TTM |
| Pekmezi et al. (Pekmezi et al., 2009) | Latinas with low income and ac-culturation (N = 93, mean age 40.7, 100 % female) |
CG (wellness contact control) | 6 month The “Seamos Activas” program consisted of monthly mailings of PA manuals that were matched to the current level of motivational readiness and individually tailored computer expert-system feedback reports. Pedometers and PA logs were further provided. |
MPA or greater (min/week) 7-Day PAR |
MPA (or greater): IG (Baseline: 16.56 min/week (SD = 25.76); 6 month: 147.27 (SD = 241.55)), CG (Baseline: 11.88 min/week (SD = 21.99); 6 month: 96.79 (SD = 118.49)). No between-group differences in overall PA. | SCT, TTM |
| Resnick et al. (Resnick et al., 2008) | Minority older adults from public housing develop-ments (N = 166, mean age 73, 81 % female) |
CG (attention control) | 12 weeks The “Senior Exercise Self-Efficacy Project” included exercise, aerobic and efficacy-enhancing components and nutrition education modules. |
TPA, time spent in exercise YPAS |
IG spent more time in exercise (F = 4.5, p =.04) than CG. There were no significant differences in TPA (F = 0.28, p =.63) between IG and CG. | Self-Efficacy Theory |
| Sheeran et al. (Sheeran et al., 2013) | Overweight, middle-aged low-SES men (N = 467, mean age 53.9, 0 % female) |
CG (inactive) | 1 month FU 7 month FU Mental contrasting intervention |
PA Scale developed by Godin, Jobin, and Bouillon (1986) |
1-month FU: marginally significant difference in PA favoring IG F(1, 82) = 3.77, p =.056, d = 0.43. 7-month FU: highly significant difference F(1, 82) = 15.50, p <.001, d = 0.87. No significant change in PA in CG (Mchange = 0.43), F(1, 41) = 1.08, ns, d = 0.32, significant, large increase in IG (Mchange = 1.14), F(1, 41) = 12.02, p <.001, d = 1.10. | FRT, Mental Contrasting |
| Spelt et al. (Spelt et al., 2019) | People facing low-SES disadvantages (N = 195, mean age 41.1, 68 % female) |
CG (inactive) | 19 weeks E-coaching application including an activity tracker connected to a mobile application with focus on the target of at least 30 active minutes/day. Further elements are coaching messages, summaries of behaviour on the activity tracker, monthly step-challenges. |
TPA (MET-min/week) S-IPAQ |
IG: PA levels significantly improved after 6 weeks (p < 0.001) and 19 weeks (p < 0.001) compared to baseline; significant difference between 6 and 19 weeks (p = 0.014). CG: significant improvement only after 6 weeks (p = 0.002). Increase from baseline after 19 weeks was significantly higher in IG compared to CG (p = 0.002), as well as the increase between week 6 and week 19 (p = 0.007) |
TTM, TPB, COM-B Model |
| Wexler et al. (Wexler et al., 2021) | Low-income residents (N = 167, mean age 40.4, 78 % female) |
CG (no intervention) | 24 month Informal intervention for Households receiving monthly, neighbourhood-specific newsletters about park-based PA opportunities, park program brochures, trail maps, and activity guides. |
park visits, park-based PA (min) SPLASH |
Positive yet moderate average treatment effect by respondent age. 20-year olds: treatment is associated with 0.97 (p <.05) additional park visits and 31.24 (p <.05) additional minutes of park-based PA over a 3-day recall period. 40-year old: smaller effects 0.36 (p <.05) additional visits and 4.66 (p <.05) additional minutes. |
None |
| Wilson et al. (2015) (Wilson et al., 2010) |
Three underserved, low-income AA communities* (N = 434, mean age 51, 62 % female) |
CG (walking only) | 24 month “Positive Action for Today’s Health” trial is an integration of a police-patrolled walking program with social marketing strategies directed at improving the social and physical environment |
MVPA Omnidirectional Actical Accelerometer |
no significant differences across communities over 24 months for MVPA. | Ecological Model |
| Non–/quasi-experimental trials | ||||||
| Agomo et al. (Agomo et al., 2015) | Women at or below 250 % of the federal poverty level (N = 20, mean age 52, 100 % female) |
No CG | 4 weeks ‘‘Be Wise’ intervention includes 4 modules delivered in 90-min sessions aiming to empower women to improve dietary intake, increase PA, and enhance social support. |
LPA (hours/week), MPA (hours/week), VPA (hours/week) Community Healthy Activities Model Program for Seniors questionnaire |
Significant increases in overall PA, F(2, 34) = 31.53, p <.0005, and MPA, F(2, 34) = 24.18, p <.0005. | SCT |
| Baba et al. (Baba et al., 2017) | Adults from 2 regions with highest Social Vulnerability Index of Sao Paulo (N = 195, mean age 47.8, 88 % women) |
CG (no infor-mation about PA recommendations) |
6 month, 12-month FU 5 weekly health promotion sessions (supervised PA + educational initiatives) |
TPA, LTPA (min/week), counts per minute IPAQ, Actigraph GT3X |
IG: increased levels of PA at post-intervention and 12-month FU. Differences between IG and CG were not statisticallysignificant (LTPA: p =.752, TPA: p =.712, counts per minute: p =.478) |
None |
| Backman et al. (Backman et al., 2011) | Low-income AA women (N = 327, mean age not reported, 100 % women) |
CG (no intervention) | 6 weeks Health educators delivered 6 1hr-Toolbox classes (3 nutrition classes, 2 PA classes, 1 community empowerment lesson) |
PA previous week (days/week), PA usual week (days/week) California Behavioral Risk Factor Survey |
IG: significant increase in “physically active for ≥ 5 days/week in previous week” (pre: 34.0, post: 59.0, p <.001) and “physically active for ≥ 5 days/week in usual week” (pre: 37.2, post: 60.3, p <.001). No significant changes in CG. | SCT |
| Brown et al. (2007) (Brown and Werner, 2007) |
Residents from low-income, mixed ethnicity (79 % White, 16 % Hispanic) neighbourhood (N = 51, mean age 41, 47 % female) |
No CG | 12 month Natural intervention of a new light rail stop |
Moderate PA bouts (METS) accelerometer |
Cross-sectional: Times 1 and 2, rides on light rail were significantly related to more METS. Longitudinal: light-rail rides at Time 2 predicted increased Time 2 moderate activity. Both controlled for: gender, household size, home ownership | None |
| Buscail et al. (Buscail et al., 2016) | Low-income neighbourhood (N = 416, mean age 39.4, 61 % female) |
No CG | 24 month Community-based intervention with several actions to promote PA (e.g., improving offering and accessibility to PA at community centres, communication, urban redevelopment) |
Global PA, LTPA (MET hours/week) RPAQ |
The proportion of inhabitants reaching a sufficient level of PA significantly increased from 48.1 % at baseline to 63.5 % at post-intervention (p =.001). |
None |
| Cochrane et al. (2008) (Cochrane and Davey, 2008) |
Two deprived urban communities (N = 1532, mean age not reported, 55 % female) |
CG (no intervention) | 12 month “Burngreave in Action” sought to influence low PA levelsby changing the environment and peer influences to promote health-enhancing PA within the community |
PA Attendance at activities and questionnaire. |
IG: significantly increased levels of PA compared to CG (p ≤ 0.001). Overall intervention effect size: d = 0 0.23. 30.6 % (IG) vs 18.3 % (CG) reported an increase in PA compared with one year ago, while 13.7 % (IG) vs 24.5 % (CG) reported no intention to exercise. | Social ecology model |
| Collins et al. (Collins et al., 2004) | Low-income, multi-ethnic women (75 % Latina) (N = 82, mean age 31.7, 100 % female) |
No CG |
8 weeks IMPACT Preparatory class with eight 1-hour, weekly skills-building classes to prepare women to increase PA |
Walking for exercise (min/week), EE 7-Day PAR |
Significant pre-post increase in the number of minutes reported walking for exercise (26.9 ± 8 min; t = 3.3, p <.001); no significant changes in EE. | TTM |
| D’Alonzo et al. (D’Alonzo et al., 2018) | Low-income immigrant Latinas (N = 76, mean age 29.8, 100 % women) |
No CG |
12 weeks culturally tailored, promotora-facilitated PA intervention with twice weekly classes |
PA, aerobic fitness NASA-JSC PA-R, non-exercise estimate of V02max |
significant improvements in aerobic fitness & daily PA levels (p <.001) |
Freirian Structured Dialog Model |
| Gademan et al. (Gademan et al., 2012) | Women from multi-ethnic deprived neighbourhoods (N = 514, mean age 42.5, 100 % female) |
CG (usual care) | 6 month, 12 month FU EoP with 18 sessions of supervised PA conducted once/week by trained sports instructors |
PA (total, domain-specific: commuting, household, work, leisure time, sports) SQUASH |
Total PA did not change at 6- and 12-month. LTPA increased at 6 and at 12 months and household PA increased at 12 months (pIGvsCG < 0.05). | None |
| Griffin et al. (Griffin et al., 2020) | Low-income women (N = 104, mean age 36.1, 100 % female) |
No CG | 12 weeks “MyQuest”, an mHealth intervention using text messages and weekly eNewsletters containing PA and nutrition goals |
steps Pedusa PE330 step pedometer |
Significant increase of step counts over 12-week intervention (F(1.36,51.55) = 5.07, p =.019, η2 = 0.118). |
SCT |
| Hardcastle et al. (Hardcastle et al., 2012) | Deprived community (N = 207, mean age not reported, 65 % women) |
No CG |
27 weeks behaviour change intervention (“lifestylechange facilitation service”) with one-to-one behaviour change counselling |
TPA, MPA, VPA, Walking (MET min/week) IPAQ |
Significant improvements in PA at 6-month. Significant main effect for time on TPA (F(1,199) = 42.87, p <.001), VPA (F(1,199) = 3.48, p =.06), MPA (F(1, 199) = 10.68, p <.001),walking (F(1, 199) = 34.00, p <.001). | MI, TTM |
| Jenum et al. (Jenum et al., 2009) | Residents from 2 low-SES districts (N = 2950, mean age 49, 56 % female) |
CG (no intervention) | 3 years FU Comprehensive intervention launched in an orchestrated manner to change PA behaviour in the community (e.g. leaflets, reminders, individual counselling, group-based activities) |
PA Questionnaire |
Increase in PA was 9.5 % (p = 0.008) and 8.1 % (p = 0.02), respectively | SCT, ecological models, empowerment and participatory approaches |
| Luten et al. (Luten et al., 2016) | Older adults (≥50 years) in socio-economically disadvantaged community (N = 643, mean age 66.5, 59 % female) |
CG (inactive) | 3 month FU, 9 month FU Intervention including local media campaign (e.g. posters, flyers, radio spots) and environmentalapproaches (e.g. community involvement) implemented during high intensity period (3 month) followed by a low intensity period (6 month) |
Changes of PA (total, transport-related, household-related, leisure-time) SQUASH |
No significant differences between IG and CG in changes to any outcome except for transport-related PA at 3 and 9 months FU. | Integrated Model for Change, ANGELO framework |
| Mier et al. (Mier et al., 2011) | Low-income MA women from economically-disadvantaged, poorly urbanized “colonias” areas (N = 16, mean age 32.4, 100 % female) |
No CG | 12 weeks Walking program consisted of 12 weekly sessions with community health workers. The sessions included e.g. discussions and activities related to ways to incorporate walking into the women's lifestyle; barriers to walking; injury prevention; benefits of PA and using social support. |
Walking (METs) S-IPAQ |
After exposure to the program, the participants reported a significant increase in walking (915.8 METs; p <.002) | TTM |
| Prins et al. (Prins et al., 2019) | Older adults from deprived neighbourhoods (N = 455, mean age 65.8, 46 % female) |
CG (inactive) | T1: 3 month FU, T2: 9 month FU IG1 (physical condition with designated walking route); IG2 (social condition withneighbourhood walking group); IG3 (combined physical & social condition) |
Total walking (min/week), recreational walking (min/week), utilitarian walking (min/week) IPAQ. |
Total walking increased between T0 and T1 for all conditions. The Incidence Rate Ratio for IG1 was 1.46 (95 % CI: 1.06;2.05) and for IG2 1.52 (95 %CI: 1.07;2.16). At T2, these differences remained significant for IG1, not for IG2 and IG3. |
TPB |
| Rabiee et al. (Rabiee et al., 2015) | Residents in a deprived inner city area (N = 257, mean age, 44 % female) |
No CG | 6 month A public health policy called “Gym for Free” scheme which provided residents free access to leisure centres. |
Use of leisure facilities Validated questionnaire |
Use of leisure facilities increased markedly (p <.05). | None |
| Speck et al. (Speck et al., 2007) | Low-income women (N = 104, mean age 39.6, 100 % female) |
CG (inactive) | 26 weeks (post-assessment 23 weeks after baseline) Environmental intervention with an Advanced Registered Nurse Practitioner. Approximately 6 PA opportunities/week including 4 exercise opportunities at a community centre and 2 neighbourhood walks |
Steps/day, (MET score) 7-day PAR, Yamax SW-701 pedometers |
No between-group differences for PA behavior. IG: non-significant changes (decreased steps per day (5791.3 to 5369.6); increased MET score (42.9 to 48.8) CG: decreased steps per day 5314.6 to 4094.9 (p < 0.05); non-significant increase in MET score per day 49.2 to 49.8. | Adapted Health Promotion Model |
| Stewart et al. (Stewart et al., 2006) | Lower-income, minority seniors (N = 321, mean age not reported, 86 % female) |
No CG | 6-month, 18-month FU CHAMPS III refers to a lifestyle individually tailored PA-promotion program providing e.g., information, skills training, support, regular telephone follow-up, group workshops, newsletters, activity diaries. Participants are encouraged to join existing community-based PA classes and programs. |
PA (hours/week), caloric expenditure CHAMPS |
Non-significant increased PA (0.8 h/week) in IGs, For the total sample there was a trend toward increased caloric expenditure (+213 kcal/week, p =.10). |
SCT |
| Tannis et al. (Tannis et al., 2019) | Low-income adults (N = 88, mean age 38.9, 78 % female) |
CG (inactive; from housing without AD features) | 12 month FU Affordable housing with AD features (e.g., accessible, prominent, and well-lit stairwells with locally-produced artwork; point-of-decision prompts at elevators demonstrating locations of stairs; proposed outdoor community garden areas; outdoor fitness areas) |
Recreational/work VPA (min/week), recreational/work MPA (min/week), steps/day RPAQ, GPAQ |
mean steps/day increased at 12 month in IG participants who moved from an elevator building (Δ6782, p = 0.051) and in the CG (Δ2960, p = 0.023). Aggregate moderate work-related activity was higher at 12 month in IG (746 vs 401, p = 0.031). No significant changes were found for recreational activity, time spent walking/cycling for travel, or sitting time. |
None |
| Toto et al. (Toto et al., 2012) | Community-dwelling older adults from low-income households (N = 15, mean age 78.1, 100 % female) |
No CG | 10 weeks Multicomponent, best-practice PA program including group exercise sessions and home exercise program. |
PA YPAS |
Of the 8 YPAS indices, significance for main effect was found for: total time, TEE, leisurely walking index. Post hoc analyses revealed no significant differences, except for the leisurely walking index, from pre- to post-test. | None |
| White et al. (White et al., 2006) | Low-income middle-aged women (N = 100, mean age not reported, 100 % female) |
No CG | 6 weeks, 6-month FU Weekly curriculum-based group meetings with a peer facilitator focussing on discussions of health issues and participants’ progress toward personal behaviour change goals. |
Days/week walking > 10 min continuously, min/day walking, time/day walking IPAQ |
Time/day walking: IGPanama (Pre: 81.67, post: 41.31, 6 month: 32.65), IGTrinidad&Tobago (Pre: 34.13, 6-month: 14.98). | Theory of implementation intentions, theory of social support |
| Zoellner et al. (Zoellner et al., 2010) | Low-SES vulnerable AA community (N = 83, mean age 44, 94 % female) |
No CG | 6 month “Fit for Life” Steps Community based participatory research walking intervention with trained community coaches |
Steps/day Yamax Pedometer |
Significant increase in average step/day from 6665 (SD = 3,396) during month 1 and increasing to 9232 (SD = 3670) during month 6 (F = 4.5, p <.0001). | TTM and social support frameworks |
*based on census tract level information (crime, physical activity, ethnic minorities, income).
AA: African American; AC: active control; ADLs: Activities of Daily Living; ANGELO: Analysis Grid for Elements linked to Obesity; BRFSS: Behavioral Risk Factor Surveillance System Physical Activity Questionnaire; CG: control group; CHAMPS: Community Health Activities Model Program for Seniors Physical Activity; d = Cohen’s d; EE: energy expenditure; FRT: Fantasy Realization Theory; FU: Follow-Up; GPAQ: Global Physical Activity Questionnaire; hr: hour; IG: intervention group; IPAQ: International Physical Activity Questionnaire; LTPA: Leisure-time Physical Activity; MA: Mexican American; MET: metabolic equivalent of task; MI: Motivational Interviewing; MPA: Moderate Physical Activity; MVPA: Moderate-to-Vigorous Physical Activity; NASA-JSC PA-R: National Aeronautics and Space Administration-Johnson Space Center Physical Activity Rating Scale; New LEAF PAA: New Leaf Physical Activity Assessment; PA: Physical activity; PAA: Physical Activity Assessment; RCT: randomized controlled trial; RPAQ Recent Physical Activity Questionnaire; Scot-PASQ: Scottish Physical Activity Questionnaire; SCT: Social Cognitive Theory; SD: standard deviation; SES: socioeconomic status; S-IPAQ: Short-Form of International Physical Activity Questionnaire; SOPARC: System of Observing Play and Recreation in Communities; SPLASH: Survey of Parks, Leisure-time Activity, and Self-reported Health; SQASH: Short Questionnaire to Assess Health-enhancing Physical Activity; TEE: Total energy expenditure; TPB: Theory of Planned Behavior; TTM: Transtheoretical Model; VPA: Vigorous Physical Activity; YPAS: Yale Physical Activity Survey;
We examined internal and external validity using the RE-AIM framework. We used a RE-AIM data extraction coding tool (from re-aim.org) to examine the degree to which studies reported on the five RE-AIM dimensions (reach, efficacy/effectiveness, adoption, implementation, maintenance). The dimensions reflect factors influencing internal and external validity including reach of the intervention for the target population, efficacy/effectiveness of the intervention on desired outcomes, adoption of the intervention at the level of staff and setting, implementation as intended, and related costs and maintenance of intervention effects on individual and setting level over time (Gaglio et al., 2013). This tool includes 61 RE-AIM indicators (reach: n = 13, efficacy/effectiveness: n = 10, adoption: n = 21, implementation: n = 9, maintenance: n = 8). Two reviewers (SL and SF) independently extracted and coded data for all indicators from the included studies. In case of disagreements between coders regarding the extracted data, they were discussed until consensus was reached. To report the presence or absence of indicators, binary coding (yes = 1 /no = 0) was applied for all five RE-AIM dimensions. First, we identified the number of indicators for individual RE-AIM dimension and total number of indicators for each study. We further computed the average proportion of indicators across all studies (i.e. number of indicators reported for a given dimension divided by the total number of possible indicators within the dimension). Second, we calculated the number of studies reporting each of the 61 indicators (sum, frequencies) for all studies and separately for experimental and non–/quasi-experimental trials, respectively.
Insert: Table 2. Individual study characteristics of the 39 studies included in the review separated into experimental and non–/quasi-experimental trials.
3. Results
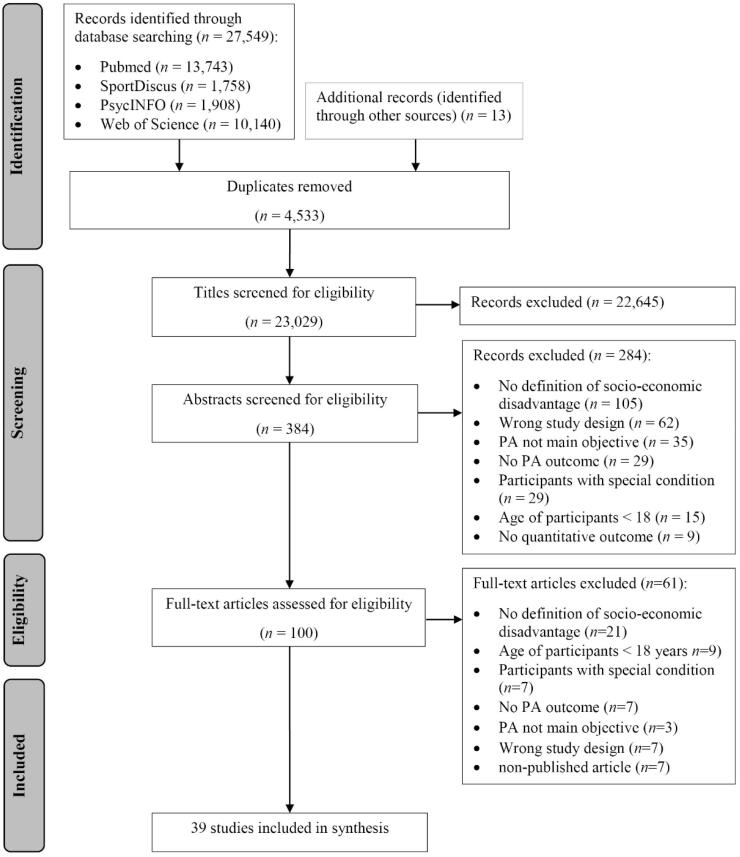
A total of 27,549 articles were found by electronic database searching, with a further 13 citations found by searching grey literature and the reference lists of key articles (Fig. 1). Our search yielded 23,029 articles after the exclusion of duplicates. Of those, 22,645 articles were excluded during title screening (main reasons: non-healthy participants, wrong study design, physical activity was no main objective) and 284 articles were excluded during abstract screening, yielding 100 articles for full-text review. An additional 61 articles were excluded after review of the full text, resulting in a total of 39 articles representing 39 studies.
Fig. 1.
Summary of articles identified, excluded and included in the RE-AIM review.
Insert: Fig. 1 Summary of articles identified, excluded and included in the RE-AIM review.
3.1. Study and participant characteristics
Table 2 summarizes the 39 reviewed studies organized by study design. Of all included studies, 17 were experimental trials (Albright et al., 2005, Armitage and Arden, 2010, Cohen et al., 2017, Coleman et al., 2012, Fahrenwald et al., 2004, Goyder et al., 2014, Hovell et al., 2008, Kendzor et al., 2017, Keyserling et al., 2008, Lowther et al., 2002, Marcus et al., 2013, Pekmezi et al., 2009, Resnick et al., 2008, Sheeran et al., 2013, Spelt et al., 2019, Wexler et al., 2021, Wilson et al., 2010) and 22 were non–/quasi-experimental trials (Agomo et al., 2015, Baba et al., 2017, Backman et al., 2011, Brown and Werner, 2007, Buscail et al., 2016, Cochrane and Davey, 2008, Collins et al., 2004, D’Alonzo et al., 2018, Gademan et al., 2012, Griffin et al., 2020, Hardcastle et al., 2012, Jenum et al., 2009, Luten et al., 2016, Mier et al., 2011, Prins et al., 2019, Rabiee et al., 2015, Speck et al., 2007, Stewart et al., 2006, Tannis et al., 2019, Toto et al., 2012, White et al., 2006, Zoellner et al., 2010). Several studies were related. The “Seamos Activas” intervention (Pekmezi et al., 2009) was a pilot study for the “Seamos Saludables” program (Marcus et al., 2013). Three studies (Coleman et al., 2012, Keyserling et al., 2008, Agomo et al., 2015) examined interventions in the “Well-Integrated Screening and Evaluation for Women Across the Nation” (WISEWOMEN) program. Collins et al. (Collins et al., 2004) examined a preparatory course related to the intervention of Albright et al. (Albright et al., 2005).
The sample size across all studies ranged from 15 (Toto et al., 2012) to 2,950 (Jenum et al., 2009) (m = 362.6, median = 195). Most of the trials were conducted in the US (n = 23), seven trials took place in the UK and four trials in the Netherlands (Spelt et al., 2019, Gademan et al., 2012, Luten et al., 2016, Prins et al., 2019). One trial each took place in Brazil (Baba et al., 2017), France (Buscail et al., 2016) and Norway (Jenum et al., 2009). Two of the studies were each implemented across two countries (Spelt et al., 2019, White et al., 2006). One intervention only included male participants (Spelt et al., 2019), 17 exclusively included women (Albright et al., 2005, Coleman et al., 2012, Fahrenwald et al., 2004, Hovell et al., 2008, Keyserling et al., 2008, Marcus et al., 2013, Pekmezi et al., 2009, Agomo et al., 2015, Brown and Werner, 2007, Mier et al., 2011, Speck et al., 2007, Toto et al., 2012, White et al., 2006, Collins et al., 2004, D’Alonzo et al., 2018, Gademan et al., 2012, Griffin et al., 2020). Five interventions were designed for older adults (Sheeran et al., 2013, Luten et al., 2016, Prins et al., 2019, Stewart et al., 2006, Toto et al., 2012). Most of the studies focused on low-income adults (n = 16), ethnic minorities (Mexican Americans, Latinas, African Americans, Hispanics) (n = 13) and deprived, low-SES areas (n = 16). Kendzor et al. (Kendzor et al., 2017) developed a shelter-based intervention for homeless adults (Kendzor et al., 2017).
Eleven trials used the Transtheoretical Model as theoretical foundation (Albright et al., 2005, Marcus et al., 2013, Pekmezi et al., 2009, Spelt et al., 2019, Collins et al., 2004, Hardcastle et al., 2012, Mier et al., 2011, Zoellner et al., 2010, Coleman et al., 2012, Fahrenwald et al., 2004, Goyder et al., 2014), eight trials used the Social Cognitive Theory (Albright et al., 2005, Marcus et al., 2013, Pekmezi et al., 2009, Agomo et al., 2015, Backman et al., 2011, Griffin et al., 2020, Jenum et al., 2009, Stewart et al., 2006). Three studies reported to use social ecological models (Wilson et al., 2010, Cochrane and Davey, 2008, Jenum et al., 2009) and two studies used the theory of implementation intentions (Armitage and Arden, 2010, White et al., 2006). Seven of the non–/quasi-experimental trials and five of the experimental trials did not report a theoretical foundation.
Most of the studies measured physical activity outcomes by self-report (n = 26). IPAQ (n = 7) and 7-Day PAR (n = 6) were the most commonly used questionnaires. Six studies used objective measures (Goyder et al., 2014, Wexler et al., 2021, Wilson et al., 2010, Brown and Werner, 2007, Griffin et al., 2020, Zoellner et al., 2010) and another six used a combination of self-report and objective measures (Fahrenwald et al., 2004, Kendzor et al., 2017, Keyserling et al., 2008, Marcus et al., 2013, Baba et al., 2017, Speck et al., 2007). The main objective measurement tools were accelerometers (n = 7) and pedometers (n = 4). Of the included studies, 26 reported significant improvements in at least one physical activity, exercise, or fitness outcome.
3.2. RE-AIM indicators
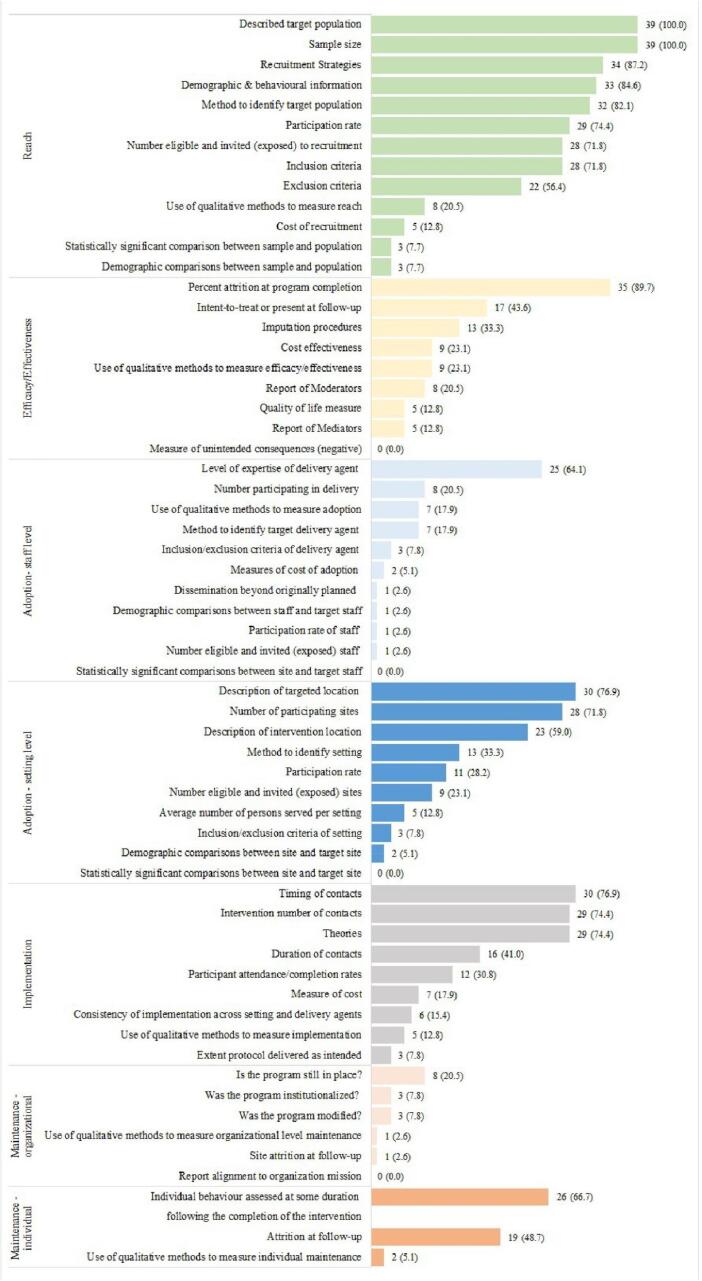
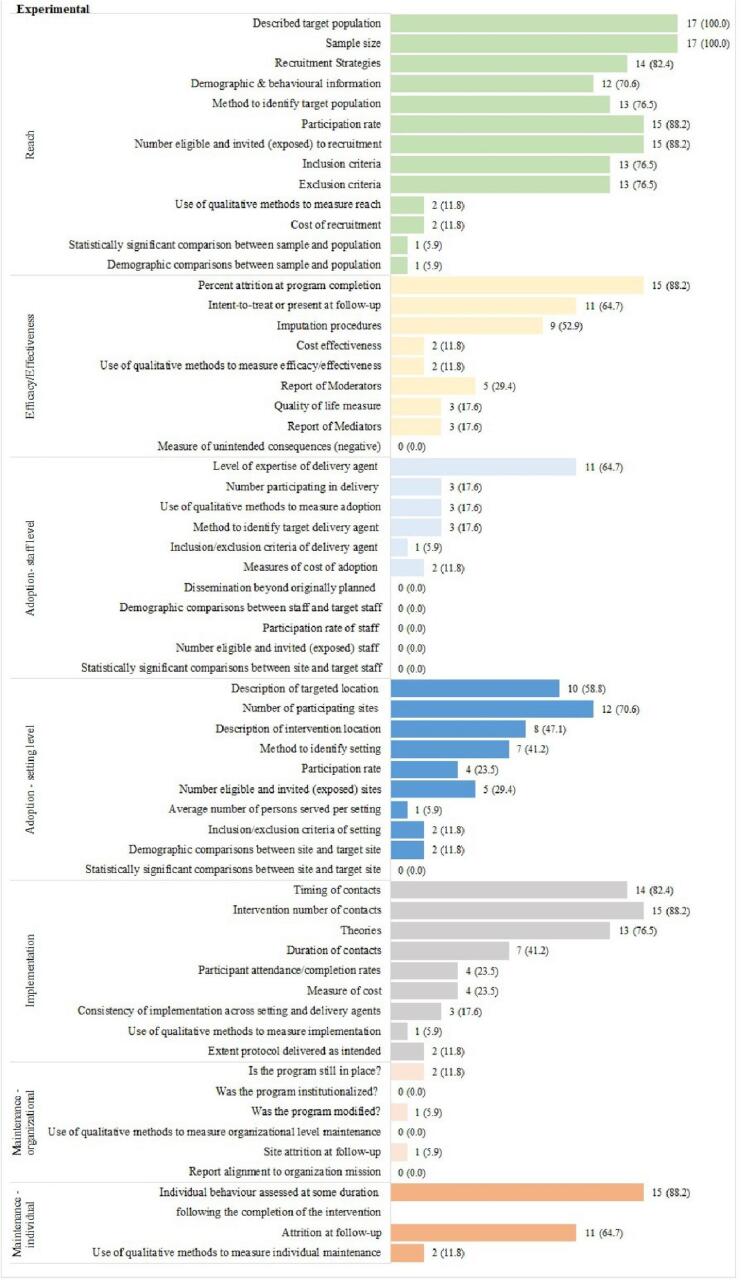
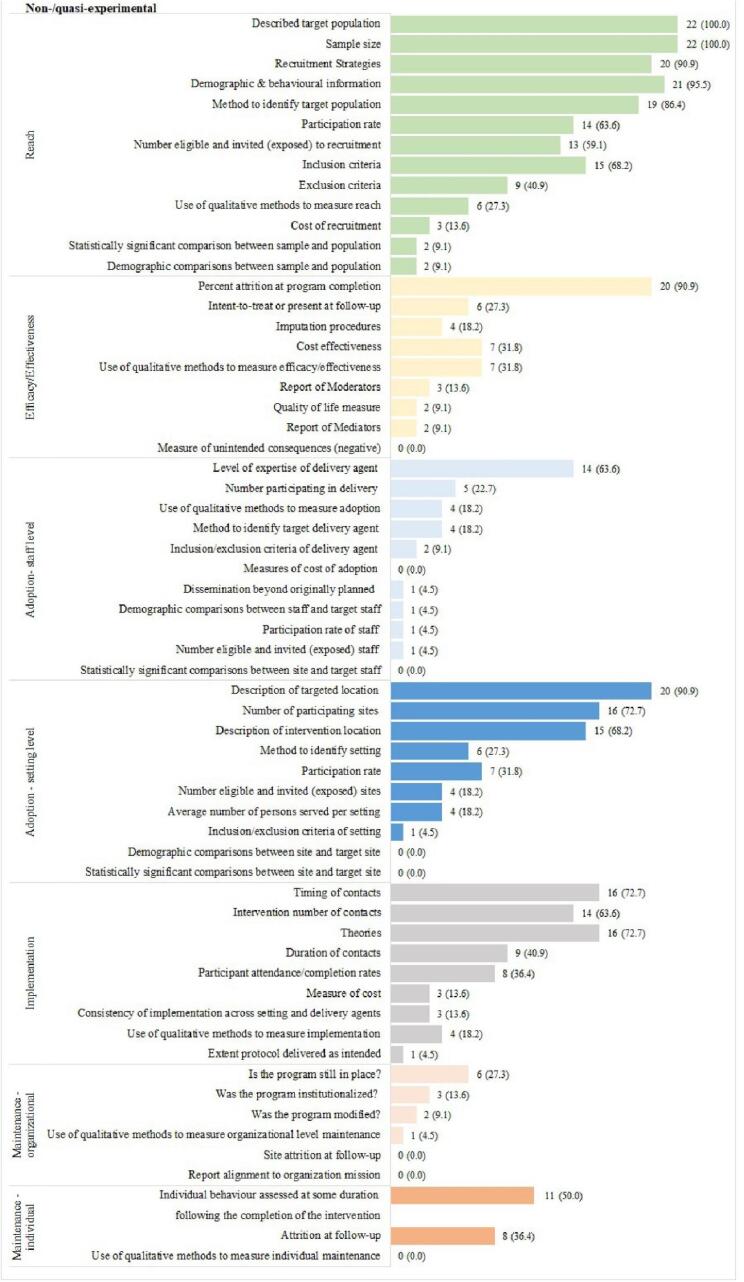
The number of reported indicators in each study is presented in Table 3. Fig. 2 presents the total number and percentage of studies reporting on each RE-AIM indicator and the explicit results for experimental and non–/quasi-experimental studies. One study (Baba et al., 2017) explicitly stated to follow the RE-AIM framework to assess their program. Overall, the studies reported 12 to 32 (m = 20.1, mdn = 19) out of a total of 61 RE-AIM indicators. On average, reach (59.2 %) was the most commonly reported dimension. Fewer studies reported indicators of implementation (38.9 %), efficacy/effectiveness (28.9 %), and adoption (21.9 %). Maintenance was reported least frequently (17.8 %).
Table 3.
Number (frequencies) of the 61 indicators of all RE-AIM dimensions across all studies.
| Author, Year |
Reach (n = 13) |
Effectiveness/Efficacy (n = 9) |
Adoption (n = 21) |
Implementation (n = 9) |
Maintenance (n = 9) |
Total (N = 61) |
|---|---|---|---|---|---|---|
| N | N | N | N | N | N (%) | |
| Experimental trials (range: n (%) of indicators) | 6–11 (46.2–84.6) |
1–8 (11.1–88.9) |
0–11 (0.0–52.4) |
1–5 (11.1–55.6) |
0–4 (0.0–44.4) |
14–32 (23.0–52.5) |
| (Albright et al., 2005) | 6 | 3 | 4 | 5 | 2 | 20 (32.8) |
| Armitage et al., 2010 | 7 | 4 | 3 | 2 | 0 | 16 (26.2) |
| (Cohen et al., 2017) | 8 | 2 | 11 | 4 | 2 | 27 (44.3) |
| (Coleman et al., 2012) | 9 | 1 | 8 | 5 | 2 | 25 (41.0) |
| (Fahrenwald et al., 2004) | 10 | 2 | 3 | 3 | 2 | 20 (32.8) |
| (Goyder et al., 2014) | 11 | 8 | 5 | 5 | 3 | 32 (52.5) |
| (Hovell et al., 2008) | 7 | 1 | 4 | 5 | 2 | 19 (31.1) |
| (Kendzor et al., 2017) | 9 | 1 | 1 | 3 | 0 | 14 (23.0) |
| (Keyserling et al., 2008) | 9 | 3 | 5 | 5 | 2 | 24 (39.3) |
| (Lowther et al., 2002) | 8 | 3 | 4 | 1 | 2 | 18 (29.5) |
| (Marcus et al., 2013) | 8 | 4 | 1 | 3 | 2 | 18 (29.5) |
| (Pekmezi et al., 2009) | 7 | 3 | 2 | 3 | 4 | 19 (31.1) |
| (Resnick et al., 2008) | 7 | 3 | 5 | 5 | 1 | 21 (33.4) |
| (Sheeran et al., 2013) | 6 | 3 | 1 | 3 | 2 | 15 (24.6) |
| (Spelt et al., 2019) | 7 | 2 | 0 | 3 | 2 | 14 (23.0) |
| (Wexler et al., 2021) | 7 | 2 | 7 | 3 | 1 | 20 (32.8) |
| Wilson et al., 2010 | 9 | 4 | 10 | 5 | 3 | 31 (50.8) |
| Non–/quasi-experimental trials(range: n (%) of indicators) |
5–11 (38.5–84.6) |
0–6 (0.0–66.7) |
1–9 (4.8–42.9) |
0–6 (0.0–66.7) |
0–5 (0.0–55.6) |
12–31 (19.7–50.8) |
| (Agomo et al., 2015) | 9 | 2 | 7 | 4 | 2 | 24 (39.3) |
| (Baba et al., 2017) | 8 | 3 | 2 | 4 | 3 | 20 (32.8) |
| (Backman et al., 2011) | 5 | 2 | 9 | 4 | 0 | 20 (32.8) |
| Brown and Werner, 2007 | 7 | 2 | 2 | 1 | 0 | 12 (19.7) |
| (Buscail et al., 2016) | 8 | 0 | 3 | 1 | 0 | 12 (19.7) |
| Cochrane and Davey, 2008 | 6 | 1 | 7 | 1 | 1 | 16 (26.2) |
| (Collins et al., 2004) | 6 | 1 | 3 | 5 | 0 | 15 (24.6) |
| (D’Alonzo et al., 2018) | 8 | 4 | 1 | 5 | 0 | 18 (29.5) |
| (Gademan et al., 2012) | 7 | 4 | 3 | 3 | 2 | 19 (31.1) |
| (Griffin et al., 2020) | 9 | 2 | 2 | 6 | 0 | 19 (31.1) |
| (Hardcastle et al., 2012) | 6 | 4 | 5 | 4 | 0 | 19 (31.1) |
| (Jenum et al., 2009) | 9 | 3 | 4 | 2 | 2 | 20 (32.8) |
| (Luten et al., 2016) | 10 | 1 | 4 | 3 | 2 | 20 (32.8) |
| (Mier et al., 2011) | 7 | 2 | 5 | 4 | 1 | 19 (31.1) |
| (Prins et al., 2019) | 11 | 6 | 8 | 4 | 2 | 31 (50.8) |
| (Rabiee et al., 2015) | 8 | 3 | 6 | 0 | 2 | 19 (31.1) |
| (Speck et al., 2007) | 6 | 1 | 6 | 5 | 1 | 19 (31.1) |
| (Stewart et al., 2006) | 6 | 2 | 9 | 4 | 5 | 25 (41.0) |
| (Tannis et al., 2019) | 9 | 1 | 3 | 0 | 2 | 15 (24.6) |
| (Toto et al., 2012) | 8 | 2 | 4 | 5 | 2 | 21 (33.4) |
| (White et al., 2006) | 5 | 2 | 6 | 5 | 2 | 20 (32.8) |
| (Zoellner et al., 2010) | 10 | 3 | 7 | 5 | 1 | 26 (42.6) |
Fig. 2.
Proportion of RE-AIM indicators across all studies (N = 39), experimental (n = 17) and non–/quasi-experimental trials (n = 22).
Insert: Table 3. Number (frequencies) of indicators of each RE-AIM dimension across all studies.
Insert: Fig. 2. Proportion of RE-AIM indicators across all studies (N = 39), experimental (n = 17), and non–/quasi-experimental trials (n = 22).
3.2.1. Reach
On average, the included studies reported 7.7 indicators for reach. None of the studies reported all 13 indicators. Differences between experimental and non–/quasi-experimental trials were small (61.1 % vs 58.8 %). All studies included a brief description of the broader target population and reported the sample size. Recruitment (n = 34, 87.2 %) was done in a variety of ways. Most studies used advertising strategies such as flyers (Cohen et al., 2017, Kendzor et al., 2017, D’Alonzo et al., 2018, Wilson et al., 2010, Agomo et al., 2015, Baba et al., 2017, Backman et al., 2011), newspaper announces (Keyserling et al., 2008, Marcus et al., 2013, Wilson et al., 2010, Prins et al., 2019, Stewart et al., 2006), or radio spots (Keyserling et al., 2008, Marcus et al., 2013). Other studies used door-to-door recruitment (Brown and Werner, 2007, Buscail et al., 2016) or drew on community contacts for recruitment, such as trained community coaches (Zoellner et al., 2010), community health workers (Mier et al., 2011), or general practitioners (Keyserling et al., 2008, Gademan et al., 2012). One of the studies engaged a recruitment agency (Spelt et al., 2019). Some aspects of costs of recruitment (n = 5, 12.8 %) were reported and ranged between 10€ gift vouchers for each participant (Prins et al., 2019) and incentives of entry into a $250 prize draw (Cochrane and Davey, 2008). Costs and representativeness (the demographic comparisons between sample and population) (n = 3, 7.7 %) were the least reported. One study compared age and gender to non-participants (Prins et al., 2019) and another study compared participants to non-participants against low education, low income, and percentage divorced (Jenum et al., 2009). Experimental trials (n = 13, 76.5 %) reported exclusion criteria more frequently than non–/quasi-experimental trials (n = 9, 40.9 %).
3.2.2. Efficacy/effectiveness
Studies reported on average 2.6 indicators of efficacy/effectiveness. The indicators were more likely to be reported in experimental trials (32.2 % vs 25.6 %). The reported rates of attrition ranged between 11.2 % (Mier et al., 2011) and 62 % (Wexler et al., 2021). About twice as many experimental trials included reports of mediators (17.6 % vs 9.1 %) and moderators (29.4 % vs 13.6 %) compared to non–/quasi-experimental trials. Reported mediators included behavioural constructs from which the intervention was delivered (Fahrenwald et al., 2004) or perceived environmental and cognitive factors (Prins et al., 2019). Demographic factors, access to facilities (Goyder et al., 2014), or mental contrasting (Sheeran et al., 2013) were mentioned as moderators. Non–/quasi-experimental trials reported more frequently on aspects of cost effectiveness (31.8 % vs 11.8 %) and qualitative methods to measure this dimension (31.8 % vs 11.8 %) compared to experimental trials. Focus groups (Rabiee et al., 2015, Speck et al., 2007, Stewart et al., 2006) and semi-structured interviews (Goyder et al., 2014, Resnick et al., 2008, Gademan et al., 2012) were the most frequently used qualitative methods to obtain feedback on efficacy/effectiveness.
3.2.3. Adoption
Studies reported an average of 4.6 out of the 21 indicators for adoption, differences between experimental and non–/quasi-experimental trials were small (21.0 % vs 22.9 %). Most of the trials reported the number of participating sites (n = 28, 71.8 %) and described the targeted location (n = 30, 76.9 %) including low-income districts and neighbourhoods (Cohen et al., 2017, Cuthbert et al., 2017, Goyder et al., 2014, Wexler et al., 2021, Collins et al., 2004, Gademan et al., 2012, Hardcastle et al., 2012, Jenum et al., 2009), community centres (Hovell et al., 2008, Resnick et al., 2008, Speck et al., 2007), and low-income public housing apartments (Lowther et al., 2002, Tannis et al., 2019, Toto et al., 2012). For the latter, there was a clear difference between experimental trials and non–/quasi-experimental trials (58.8 % vs 90.9 %). A description of the intervention location was provided by 59 % of the studies (n = 23). In most cases, the interventions took place in community health centres (Keyserling et al., 2008, Wilson et al., 2010, Agomo et al., 2015, Speck et al., 2007, White et al., 2006). Two studies provided information on comparisons of targeted intervention sites and sites participating (Wexler et al., 2021, Wilson et al., 2010). At staff level, the level of expertise of delivery agents was the most reported indicator (n = 25, 64.1 %). Interventions were mainly delivered by practitioners (e.g., health educators, dietarians, sports instructors) (Albright et al., 2005, Coleman et al., 2012, Hovell et al., 2008, Keyserling et al., 2008, Resnick et al., 2008, Gademan et al., 2012, Luten et al., 2016, Toto et al., 2012, Agomo et al., 2015, Baba et al., 2017, Backman et al., 2011), researchers (Armitage and Arden, 2010, Pekmezi et al., 2009, Wexler et al., 2021, Griffin et al., 2020), or community members (e.g. local peers, trained community members) (Coleman et al., 2012, Goyder et al., 2014, Hovell et al., 2008, Wilson et al., 2010, Cochrane and Davey, 2008, White et al., 2006, Zoellner et al., 2010, Luten et al., 2016, Mier et al., 2011, Prins et al., 2019). Agomo et al. (Agomo et al., 2015) was the only study that reported demographic comparisons between staff and targeted staff (e.g., proportion Hispanic, proportion Spanish-speaking (Agomo et al., 2015).
3.2.4. Implementation
Studies reported an average of 3.5 indicators of implementation. Experimental trials reported slightly more indicators than non–/quasi-experimental trials (41.1 % vs 37.8 %). The timing of contacts (n = 30, 76.9 %) ranged from daily to monthly contacts. The number of contacts (n = 29, 74.4 %) was reported according to the respective intervention design and ranged between a series of four computer-generated newsletters sent to each participant (Kendzor et al., 2017) and 2–3 SMS contacts per day over a period of 12 weeks (Griffin et al., 2020). Timing and number of contacts were more frequently reported than their duration (n = 16, 41.0 %). Only two studies reported on overall costs. Agomo et al. (Agomo et al., 2015) identified “Be Wise” as a cost-effective program with a total cost of $965 (Agomo et al., 2015). Cohen et al. (Cohen et al., 2017) limited the cost of their park-based intervention to under $4000 per park to give community-based organizations a realistic budget for potential implementation (Resnick et al., 2008). Some studies inlucded nonspecific descriptions such as “intervention at relatively low cost” (Prins et al., 2019), while other studies reported more detail, such as providing a $53 monthly remuneration (Griffin et al., 2020).Non–/quasi-experimental trials reported the proportion of the intervention that participants received (36.4 % vs 23.5 %) and the use of qualitative methods to measure implementation (18.2 % vs 5.9 %) more frequently. Qualitative methods included focus groups (Baba et al., 2017, Speck et al., 2007), semi structural interviews with staff, volunteers, and directors (Stewart et al., 2006) and a discussion on the progress in program implementation with community members and the intervention team (Wilson et al., 2010).
3.2.5. Maintenance
On average, 1.6 indicators of maintenance were reported. Experimental trials reported indicators more frequently (21.1 % vs 15.6 %). At the individual level, an available description of follow-up outcome measures of individuals some duration after end of the intervention (n = 26, 66.7 %) and the attrition rate at follow-up (mean = 19.9 %) (n = 19, 48.7 %) were the most frequently reported indicators. At the organizational level, 8 studies (20.5 %) provided information on program continuation after the completion of the research trial. Two studies reported continuation of the programs for another year by the community (Wilson et al., 2010) and local funding (Speck et al., 2007). In one study, the program continued for more than five years after the end of the project phase (Jenum et al., 2009). None of the studies reported on alignment to the organization mission. Two non-experimental trials (Rabiee et al., 2015, Stewart et al., 2006) and one quasi-experimental trial (Cochrane and Davey, 2008) reported the integration of the intervention into the delivery system, none of the experimental trials reported this indicator. For example, Stewart et al. (Stewart et al., 2006) reported that the department provided one staff member each for set-up and registration and one for course instruction to continue the course (Stewart et al., 2006). In each case, only one study reported the site attrition at follow-up (attrition rate = 0 %) (Cohen et al., 2017) and the usage of qualitative measures to measure the organizational level of maintenance (Buscail et al., 2016). Baba et al. (Baba et al., 2017) used semi-structured interviews to explore the structural conditions contributing to the maintenance of their program (Buscail et al., 2016).
4. Discussion
To date, research has focused on the effectiveness of physical activity interventions in socioeconomically disadvantaged people, while knowledge on external validity of such intervention studies remains scarce (Cleland et al., 2013, Bull et al., 2018). To fill this gap, we conducted a RE-AIM review examining the degree to which intervention studies reported on the internal and external validity in order to inform the translation of interventions into practice. We identified an overall low reporting of factors of both internal and external validity. Regarding the reach, all studies provided at least brief descriptions of the broader target population and the sample size of the intervention. This finding is in line with other RE-AIM reviews of physical activity interventions (Bhuiyan et al., 2019, Galaviz et al., 2014). In contrast to the reporting of the broader target population, representativeness was hardly reported in either study design. This is also consistent with previous research findings showing that representativeness of samples in these interventions is rather rare (Matthews et al., 2014, Dzewaltowski et al., 2004). Such information on representativeness would however be desirable, since it allows a comparison between participants and non-participants. This can lead to insights on how to increase the reach of an intervention (Glasgow et al., 2019). This is highly relevant, since it has been shown that even programs designed for a specific target group (e.g., socioeconomically disadvantaged individuals) might have little success in reaching it (Yancey et al., 2006).
On the efficacy/effectiveness, studies reported about one-third of indicators for this dimension, which contrasts with previous RE-AIM reviews where this dimension of internal validity was identified as most frequently reported (McGoey et al., 2016, Antikainen and Ellis, 2011, White et al., 2009). One reason for this could be the use of different coding tools among reviews using the RE-AIM framework (Kennedy et al., 2021, Antikainen and Ellis, 2011). For most of the indicators of efficacy/effectiveness reporting was higher in experimental trials (e.g. report of mediators, report of moderators, imputation procedure) than in non– or quasi-experimental trails. Some references state that non-randomized trials often have enhanced external validity compared to experimental trials (Glasgow et al., 2006, Moffitt, 2004). The focus on efficacy may be due to the fact that funding agencies particularly ask for efficacy of interventions and that robust, controlled study designs are primarily required.
In the present review, there was an overall low reporting of external validity as adoption and maintenance were the least frequently reported dimensions for both study designs. This finding is consistent with previous RE-AIM reviews (McGoey et al., 2016, Matthews et al., 2014, White et al., 2009). However, understanding components of adoption is important for establishing sustainable and effective long-term programs (Cuthbert et al., 2017). To translate research-driven pilot studies into routine preventive services, health promotion practitioners require such knowledge on which level of expertise is needed among staff to carry out an intervention and in which settings such an intervention might be appropriate to be delivered.
The reporting for maintenance was particularly low. However, a closer look at the maintenance dimension reveals that while experimental trials reported more individual level indicators (refer to long-term effects of programs on outcomes after program completion), the opposite was true for the organizational level indicators (refer to the extent to which a program becomes institutionalised) (Holtrop et al., 2021). It is possible the majority of included studies did not have the goal of achieving maintenance. McGoey et al. (2015) made the argument, that studies focused on effectiveness should be designed to also include maintenance in order to determine which setting level variables promote or hinder the intervention’s ability to become institutionalized (McGoey et al., 2016). Obviously, reaching maintenance is particularly important for this target population, as they face additional barriers when attempting to participate in and sustain health promoting interventions (Baruth et al., 2014).
Based on our results, two main recommendations for the reporting of future studies are worth mentioning. First, the studies in this review rarely utilized qualitative means of inquiry. However, there has been a paradigm shift toward mixed-methods research in the evaluation of health-related interventions (World Health Organization, 2013). It would be advantageous for future studies to use quantitative and qualitative measures. Mixed method designs cancel out disadvantages of single methods, allow the collection of more comprehensive data to improve replication efforts and assist in understanding participant level and setting and staff level indicators (Craike et al., 2018). Targeting people with socioeconomic disadvantages demands complex interventions and generalisability beyond the context of a specific study setting. Mixed-methods designs, with qualitative data on feasibility and relevance of a program, are particularly appropriate for this applied research (Byrne and Humble, 2007). The second recommendation for future studies is to provide information on the costs of interventions. Almost no studies in this review mentioned total costs of their program. The costs of an intervention are one of the main elements in translating research findings into practice. Cost-effective interventions are particularly important for the successful long-term implementation and scaling up of public health interventions (Wanless, 2004). This is important when reaching socioeconomically disadvantaged groups, as costs for participants has been identified as a main barrier for participation (Withall et al., 2011).
Overall, our results reinforce the calls of previous RE-AIM reviews for a detailed report of external validity factors, as this forms the basis for transferring research findings into public health practice (McGoey et al., 2016, Galaviz et al., 2014). The lack of adequate reporting of external validity in this review may indicate that there has been little focus on the sustainable development and implementation of physical activity interventions for socioeconomically disadvantaged groups. Successfully scaled-up interventions are not those that have been implemented on a large scale. They also include interventions hat effectively promoted physical activity in the population, and become fully embedded in a system. The scaling-up of interventions can be better understood and enhanced by the use of systematic planning frameworks (Glanz and Bishop, 2010). Using the RE-AIM framework could be an opportunity for researchers to integrate and extend reporting on external validity factors of interventions, and thus increase their potential to be translated into a real-world setting.
But it also has to be recognized that the RE-AIM framework seems to follow a certain linear logic, which at times might be at odds with the challenges of promoting physical activity in socioeconomically disadvantaged groups. In the field of health promotion, community-based participatory research (CBPR) is frequently used to reach socially disadvantaged groups, and has demonstrated successes in doing so (Haldane et al., 2019). CBPR reaches such groups by creating opportunities for participation and achieving health-promoting effects at individual and structural levels (O’Mara-Eves et al., 2015). These interventions are often regarded as being highly context-dependent with multiple factors influencing their success, thus often requiring major adjustments to the interventions when transferred (Willis et al., 2016). This results in adaptations of these interventions, a process that rE-AIM does not account for with its rather strict focus on adoption. It is however necessary to consider potential adaptations during the implementation phase of an intervention. One reason for this is that adaptations can affect intervention effectiveness. Reilly et al. (Reilly et al., 2020) therefore emphasized the need for adaptations to be comprehensively recorded and assessed, as this provides useful insight into the components of interventions at different stages (Reilly et al., 2020). They expanded the implementation dimension by assessing indicators of adaptation prior to, during, and following implementation of the intervention, and in addition, included documentation on how the adaptation was consistent with the underlying evidence-based principles of the intervention as previously tested (Wiltsey Stirman et al., 2019).One tool that also addresses the adaptation-challenge is the “Practical Robust Implementation and Sustainability Model” (PRISM). This model includes RE-AIM outcomes but also addresses contextual factors and multilevel organizational perspectives and could be used as a practical guide in the process of planning, developing and evaluating future interventions for socioeconomically disadvantaged populations (Holtrop et al., 2021). Integrating models such as PRISM and RE-AIM allows for their application on the adoption-adaption spectrum of public health interventions.
The present review has several strengths. To our knowledge, it is one of the first to provide a quantitative estimate of the reporting of external validity in interventions to promote physical activity among socioeconomically disadvantaged people, in addition to internal validity. We used a comprehensive search strategy which was designed with the assistance of a trained librarian, well-defined inclusion and exclusion criteria and a comprehensive data extraction tool. However, some limitations need to be mentioned. We only included studies with at least one post assessment and a quantitative measure of physical activity outcomes which excluded some publications (Macmillan et al., 2018, Curran et al., 2016). Due to practical reasons, included studies were restricted to those published in English or German. Although the number of RE-AIM reviews is steadily increasing, there is no consensus regarding a specific tool. The majority of reviews [e.g., Cuthbert et al., 2017; Galaviz et al., 2014] used a smaller number of RE-AIM indicators which complicates the comparability between the results. However, by analysing 61 indicators, we were able to map a much more comprehensive picture of internal and external validity in this review compared to shorter RE-AIM tools. Some studies may have collected but not reported the analysed indicators. To address this issue, this review also considered companion articles on included publications and examined them for potential data.
5. Conclusion
Few intervention studies to promote physical activity in socioeconomically disadvantaged adults report indicators of internal and external validity for experimental and non–/quasi-experimental trials. In conclusion, we encourage future studies to improve reporting across all RE-AIM dimensions, as well as provide information on the representativeness of the study sample and the costs of an intervention to support the translation into real world settings.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Stephanie Linder, Email: stephanie.linder@fau.de.
Susanne Ferschl, Email: susanne.ferschl@tum.de.
Karim Abu-Omar, Email: karim.abu-omar@fau.de.
Heiko Ziemainz, Email: heiko.ziemainz@fau.de.
Anne Kerstin Reimers, Email: anne.reimers@fau.de.
References
- Agomo H.C., Andresen P.A., Deshmukh D. Be wise: Implementing a lifestyle intervention to reduce stroke risk in low-income midlife women. J. of Neurosci. Nurs. 2015;47:36–43. doi: 10.1097/JNN.0000000000000108. [DOI] [PubMed] [Google Scholar]
- Albright C.L., Pruitt L., Castro C., Gonzalez A., Woo S., King A.C. Modifying physical activity in a multiethnic sample of low-income women: one-year results from the IMPACT (Increasing Motivation for Physical ACTivity) project. Ann. Behav. Med. 2005;30:191–200. doi: 10.1207/s15324796abm3003_3. [DOI] [PubMed] [Google Scholar]
- Antikainen I., Ellis R. A RE-AIM evaluation of theory-based physical activity interventions. J. Sport Exerc. Psychol. 2011;33:198–214. doi: 10.1123/jsep.33.2.198. [DOI] [PubMed] [Google Scholar]
- Armitage C.J., Arden M.A. A volitional help sheet to increase physical activity in people with low socioeconomic status: a randomised exploratory trial. Psychol. Health. 2010;25:1129–1145. doi: 10.1080/08870440903121638. [DOI] [PubMed] [Google Scholar]
- Baba C.T., Oliveira I.M., Silva A.E.F., Vieira L.M., Cerri N.C., Florindo A.A., de Oliveira Gomes G.A. Evaluating the impact of a walking program in a disadvantaged area: using the RE-AIM framework by mixed methods. BMC Public Health. 2017;17:1–11. doi: 10.1186/s12889-017-4698-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backman D., Scruggs V., Atiedu A.A., Bowie S., Bye L., Dennis A., Hall M., Ossa A., Wertlieb S., Foerster S.B. Using a toolbox of tailored educational lessons to improve fruit, vegetable, and physical activity behaviors among African American women in California. J. Nutr. Educ. Behav. 2011;43:75–85. doi: 10.1016/j.jneb.2011.02.004. [DOI] [PubMed] [Google Scholar]
- Ball K., Carver A., Downing K., Jackson M., O’Rourke K. Addressing the social determinants of inequities in physical activity and sedentary behaviours. Health Promot. Int. 2015;30(suppl_2):ii8-ii19. doi: 10.1093/heapro/dav022. [DOI] [PubMed] [Google Scholar]
- Baruth M., Sharpe P.A., Parra-Medina D., Wilcox S. Perceived barriers to exercise and healthy eating among women from disadvantaged neighborhoods: results from a focus groups assessment. Women Health. 2014;54:336–353. doi: 10.1080/03630242.2014.896443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beenackers M.A., Kamphuis C.B.M., Giskes K., Brug J., Kunst A.E., Burdorf A., van Lenthe F.J. Socioeconomic inequalities in occupational, leisure-time, and transport related physical activity. Int. J. Behav. Nutr. Phys. Act. 2012;9:116. doi: 10.1186/1479-5868-9-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhuiyan N., Singh P., Harden S.M., Mama S.K. Rural physical activity interventions in the United States: a systematic review and RE-AIM evaluation. Int. J. Behav. Nutr. Phys. Act. 2019;16:1–11. doi: 10.1186/s12966-019-0903-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown B.B., Werner C.M. A new rail stop: tracking moderate physical activity bouts and ridership. Am. J. Prev. Med. 2007;33:306–309. doi: 10.1016/j.amepre.2007.06.002. [DOI] [PubMed] [Google Scholar]
- Bull F.C., Al-Ansari S.S., Biddle S., Borodulin K., Buman M.P., Cardon G., Carty C., Chaput J.-P., Chastin S., Chou R., Dempsey P.C., DiPietro L., Ekelund U., Firth J., Friedenreich C.M., Garcia L., Gichu M., Jago R., Katzmarzyk P.T., Lambert E., Leitzmann M., Milton K., Ortega F.B., Ranasinghe C., Stamatakis E., Tiedemann A., Troiano R.P., van der Ploeg H.P., Wari V., Willumsen J.F. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020;54(24):1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bull E.R., McCleary N., Li X., Dombrowski S.U., Dusseldorp E., Johnston M. Interventions to promote healthy eating, physical activity and smoking in low-income groups: a systematic review with meta-analysis of behavior change techniques and delivery/context. Int. J. Behav. Med. 2018;25:605–616. doi: 10.1007/s12529-018-9734-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buscail C., Menai M., Salanave B., Daval P., Painsecq M., Lombrail P., Hercberg S., Julia C. Promoting physical activity in a low-income neighborhood of the Paris suburb of Saint-Denis: effects of a community-based intervention to increase physical activity. BMC Public Health. 2016;16:1–9. doi: 10.1186/s12889-016-3360-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne, J., Humble, Á.M., 2007. An introduction to mixed method research. Vol. 1., Halifax: Atlantic Research Centre for Family-Work Issues. 1-4.81.
- Cleland V., Granados A., Crawford D., Winzenberg T., Ball K. Effectiveness of interventions to promote physical activity among socioeconomically disadvantaged women: A systematic review and meta-analysis. Obes. Rev. 2013;14:197–212. doi: 10.1111/j.1467-789X.2012.01058.x. [DOI] [PubMed] [Google Scholar]
- Cleland C.L., Tully M.A., Kee F., Cupple M.E. The effectiveness of physical activity interventions in socio-economically disadvantaged communities: a systematic review. Prev. Med. 2012;54:371–380. doi: 10.1016/j.ypmed.2012.04.004. [DOI] [PubMed] [Google Scholar]
- Cochrane T., Davey R.C. Increasing uptake of physical activity: a social ecological approach. J. R. Soc. Promo. Health. 2008;128:31–40. doi: 10.1177/1466424007085223. [DOI] [PubMed] [Google Scholar]
- Cohen J. A coefficient of agreement for nominal scales. Educational and Psychological Measurements. 1960;20(1):37–46. [Google Scholar]
- Cohen D.A., Han B., Derose K.P., Williamson S., Marsh T., Raaen L., McKenzie T.L. Promoting physical activity in high-poverty neighborhood parks: A cluster randomized controlled trial. Soc. Sci. Med. 2017;186:130–138. doi: 10.1016/j.socscimed.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman K.J., Farrell M.A., Rocha D.A., Hayashi T., Hernandez M., Wolf J., Lindsay S. Readiness to be physically active and self-reported physical activity in low-income Latinas, California WISEWOMAN, 2006–2007. Prev Chronic Dis. 2012;9:e87. [PMC free article] [PubMed] [Google Scholar]
- Collins R., Lee R.E., Albright C.L., King A.C. Ready to be physically active? The effects of a course preparing low-income multiethnic women to be more physically active. Health Edu. Behav. 2004;31:47–64. doi: 10.1177/1090198103255529. [DOI] [PubMed] [Google Scholar]
- Craike M., Wiesner G., Hilland T.A., Bengoechea E.G. Interventions to improve physical activity among socioeconomically disadvantaged groups: an umbrella review. Int. J. Behav. Nutr. Phys. Act. 2018;15:1–11. doi: 10.1186/s12966-018-0676-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran K., Drust B., Murphy R., Pringle A., Richardson D. The challenge and impact of engaging hard-to-reach populations in regular physical activity and health behaviours: an examination of an English Premier League ‘Football in the Community’men's health programme. Public Health. 2016;135:14–22. doi: 10.1016/j.puhe.2016.02.008. [DOI] [PubMed] [Google Scholar]
- Cuthbert, C.A., King-Shier, K., Ruether, D., Tapp, D.M., Culos-Reed, S.N., 2017. What is the state of the science on physical activity interventions for family caregivers? A systematic review and RE-AIM evaluation. J. Phys. Act. Health 14, 578-595. ttps://doi.org/10.1123/jpah.2016-0280. [DOI] [PubMed]
- D’Alonzo K.T., Smith B.A., Dicker L.H. Outcomes of a culturally tailored partially randomized patient preference controlled trial to increase physical activity among low-income immigrant Latinas. J. of Transcult. Nurs. 2018;29:335–345. doi: 10.1177/1043659617723073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzewaltowski D.A., Estabrooks P.A., Klesges L.M., Bull S., Glasgow R.E. Behavior change intervention research in community settings: how generalizable are the results? Health Promot. Int. 2004;19:235–245. doi: 10.1093/heapro/dah211. [DOI] [PubMed] [Google Scholar]
- Eldridge S., Ashby D., Bennett C., Wakelin M., Feder G. Internal and external validity of cluster randomised trials: systematic review of recent trials. BMJ. 2008;336:876–880. doi: 10.1136/bmj.39517.495764.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estabrooks P., Gyurcsik N. Evaluating the impact of behavioral interventions that target physical activity: issues of generalizability and public health. Psychol. Sport Exerc. 2003;4:41–55. doi: 10.1016/S1469-0292(02)00016-X. [DOI] [Google Scholar]
- Fahrenwald N.L., Atwood J.R., Walker S.N., Johnson D.R., Berg K. A randomized pilot test of “Moms on the Move”: a physical activity intervention for WIC mothers. Ann. Behav. Med. 2004;27:82–90. doi: 10.1207/s15324796abm2702_2. [DOI] [PubMed] [Google Scholar]
- Gademan M.G., Deutekom M., Hosper K., Stronk K. The effect of exercise on prescription on physical activity and wellbeing in a multi-ethnic female population: A controlled trial. BMC Public Health. 2012;12:1–9. doi: 10.1186/1471-2458-12-758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaglio B., Shoup J.A., Glasgow R.E. The RE-AIM Framework: A Systematic Review of Use Over Time. Am J Public Health. 2013;103(6):e38–e46. doi: 10.2105/AJPH.2013.301299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galaviz K.I., Harden S.M., Smith E., Blackman K.CA., Berrey L.M., Mama S.K., Almeida F.A., Lee R.E., Estabrooks P.A. Physical activity promotion in Latin American populations: a systematic review on issues of internal and external validity. Int. J. Behav. Nutr. Phys. Act. 2014;11(1) doi: 10.1186/1479-5868-11-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- German Institute for Economic Research. 1984-2017. Socio-Economic Panel-Core Version 34. Socio-Economic Panel. https://www.diw.de/sixcms/detail.php?id=diw_01.c.738729.en. (accessed 14 June 2022).
- Gidlow C., Johnston L.H., Crone D., Ellis N., James D. A systematic review of the relationship between socio-economic position and physical activity. Health Edu. J. 2006;65:338–367. doi: 10.1177/0017896906069378. [DOI] [Google Scholar]
- Glanz K., Bishop D.B. The role of behavioral science theory in development and implementation of public health interventions. Annu. Rev. Public Health. 2010;31:399–418. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- Glasgow R.E., Vogt T.M., Boles S.M. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am. J. Public Health. 1999;89:1322–1327. doi: 10.2105/AJPH.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow R.E., Lichtenstein E., Marcus A.C. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am. J. Public Health. 2003;93:1261–1267. doi: 10.2105/AJPH.93.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow R.E., Green L.W., Klesges L.M., Abrams D.B., Fisher E.B., Goldstein M.G., Hayman L.L., Ockene J.K., Orleans C.T. External validity: we need to do more. Ann. Behav. Med. 2006;31:105–108. doi: 10.1207/s15324796abm3102_1. [DOI] [PubMed] [Google Scholar]
- Glasgow R.E., Harden S.M., Gaglio B., Rabin B., Smith M.L., Porter G.C., Ory M.G., Estabrooks P.A. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Front. Public Health. 2019;7:64. doi: 10.3389/fpubh.2019.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyder E., Hind D., Breckon J., Dimairo M., Minton J., Everson-Hock E., Read S., Copeland R., Crank H., Horspool K., Humphreys L., Hutchison A., Kesterton S., Latimer N., Scott E., Swaile P., Walters S.J., Wood R., Collins K., Cooper C. A randomised controlled trial and cost-effectiveness evaluation of'booster'interventions to sustain increases in physical activity in middle-aged adults in deprived urban neighbourhoods. Health Technol. Assess. 2014;18(13) doi: 10.3310/hta18130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray P.M., Murphy M.H., Gallagher A.M., Simpson E.E.A. Motives and barriers to physical activity among older adults of different socioeconomic status. J. Aging Phys. Act. 2016;24:419–429. doi: 10.1123/japa.2015-0045. [DOI] [PubMed] [Google Scholar]
- Griffin J.B., Struempler B., Funderburk K., Parmer S.M., Tran C., Wadsworth D.D. My quest, a community-based mHealth intervention to increase physical activity and promote weight loss in predominantly rural-dwelling, low-income. Alabama women. Fam. Community Health. 2020;43(2):131–140. doi: 10.1097/FCH.0000000000000251. [DOI] [PubMed] [Google Scholar]
- Haldane V., Chuah F.L.H., Srivastava A., Singh S.R., Koh G.C.H., Seng C.K., Legido-Quigley H., Maulsby C. Community participation in health services development, implementation, and evaluation: A systematic review of empowerment, health, community, and process outcomes. PLoS One. 2019;14(5):e0216112. doi: 10.1371/journal.pone.0216112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallal P.C., Andersen L.B., Bull F.C., Guthold R., Haskell W., Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- Hardcastle S., Blake N., Hagger M.S. The effectiveness of a motivational interviewing primary-care based intervention on physical activity and predictors of change in a disadvantaged community. J. Behav. Med. 2012;35:318–333. doi: 10.1007/s10865-012-9417-1. [DOI] [PubMed] [Google Scholar]
- Holtrop J.S., Estabrooks P.A., Gaglio B., Harden S.M., Kessler R.S., King D.K., Kwan B.M., Ory M.G., Rabin B.A., Shelton R.C., Glasgow R.E. Understanding and applying the RE-AIM framework: clarifications and resources. J. Clin. Transl. Sci. 2021;5(1):e126. doi: 10.1017/cts.2021.789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovell M.F., Mulvihill M.M., Buono M.J., Liles S., Schade D.H., Washington T.A., Manzano R., Sallis J.F. Culturally tailored aerobic exercise intervention for low-income Latinas. Am. J. Health Promot. 2008;22:155–163. doi: 10.4278/ajhp.22.3.155. [DOI] [PubMed] [Google Scholar]
- Jenum A.K., Lorentzen C.A.N., Ommundsen Y. Targeting physical activity in a low socioeconomic status population: observations from the Norwegian “Romsås in Motion” study. Brit. J. Sports Med. 2009;43:64–69. doi: 10.1136/bjsm.2008.053637. [DOI] [PubMed] [Google Scholar]
- Kendzor D.E., Allicock M., Businelle M.S., Sandon L.F., Gabriel K.P., Frank S.G. Evaluation of a shelter-based diet and physical activity intervention for homeless adults. J. Phys. Act. Health. 2017;14:88–97. doi: 10.1123/jpah.2016-0343. [DOI] [PubMed] [Google Scholar]
- Kennedy S.G., Sanders T., Estabrooks P.A., Smith J.J., Lonsdale C., Foster C., Lubans D.R. Implementation at-scale of school-based physical activity interventions: A systematic review utilizing the RE-AIM framework. Obes. Rev. 2021;22:e13184. doi: 10.1111/obr.13184. [DOI] [PubMed] [Google Scholar]
- Keyserling T.C., Samuel Hodge C.D., Jilcott S.B., Johnston L.F., Garcia B.A., Gizlice Z., Gross M.D., Saviñon C.E., Bangdiwala S.I., Will J.C., Farris R.P., Trost S., Ammerman A.S. Randomized trial of a clinic-based, community-supported, lifestyle intervention to improve physical activity and diet: the North Carolina enhanced WISEWOMAN project. Prev. Med. 2008;46(6):499–510. doi: 10.1016/j.ypmed.2008.02.011. [DOI] [PubMed] [Google Scholar]
- Lowther M., Mutrie N., Scott E. Promoting physical activity in a socially and economically deprived community: a 12 month randomized control trial of fitness assessment and exercise consultation. J. Sports Sci. 2002;20:577–588. doi: 10.1080/026404102760000071. [DOI] [PubMed] [Google Scholar]
- Luten K.A., Reijneveld S.A., Dijkstra A., de Winter A.F. Reach and effectiveness of an integrated community-based intervention on physical activity and healthy eating of older adults in a socioeconomically disadvantaged community. Health Educ. Res. 2016;31:98–106. doi: 10.1093/her/cyv064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macmillan A.K., Mackie H., Hosking J.E., Witten K., Smith M., Field A., Woodward A., Hoskins R., Stewart J., van der Werf B., Baas P. Controlled before-after intervention study of suburb-wide street changes to increase walking and cycling: Te Ara Mua-Future Streets study design. BMC Public Health. 2018;18(1) doi: 10.1186/s12889-018-5758-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus B.H., Dunsiger S.I., Pekmezi D.W., Larsen B.A., Bock B.C., Gans K.M., Marquez B., Morrow K.M., Tilkemeier P. The Seamos Saludables study: A randomized controlled physical activity trial of Latinas. Am. J. Prev. Med. 2013;45:598–605. doi: 10.1016/j.amepre.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews L., Kirk A., MacMillan F., Mutrie N. Can physical activity interventions for adults with type 2 diabetes be translated into practice settings? A systematic review using the RE-AIM framework. Translat. Behav. Med. 2014;4:60–78. doi: 10.1007/s13142-013-0235-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGoey T., Root Z., Bruner M.W., Law B. Evaluation of physical activity interventions in youth via the Reach, Efficacy/Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework: A systematic review of randomised and non-randomised trials. Prev. Med. 2016;76:58–67. doi: 10.1016/j.ypmed.2015.11.004. [DOI] [PubMed] [Google Scholar]
- Mier N., Tanguma J., Millard A.V., Villareal E.K., Alen M., Ory M.G. A pilot walking program for Mexican-American women living in colonias at the border. Am. J. Health Promo. 2011;25:172–175. doi: 10.4278/ajhp.090325-ARB-115. [DOI] [PubMed] [Google Scholar]
- Moffitt R.A. The role of randomized field trials in social science research: a perspective from evaluations of reforms of social welfare programs. Am. Behav. Sci. 2004;47:506–540. doi: 10.1177/0002764203259292. [DOI] [Google Scholar]
- Müller-Riemenschneider F., Reinhold T., Willich S.N. Cost-effectiveness of interventions promoting physical activity. Brit. J. Sports Med. 2009;43:70–76. doi: 10.1136/bjsm.2008.053728. [DOI] [PubMed] [Google Scholar]
- Nocon M., Keil T., Willich S.N. Education, income, occupational status and health risk behaviour. J. Public Health. 2007;15(5):401–405. [Google Scholar]
- O’Donoghue G., Kennedy A., Puggina A., Aleksovska K., Buck C., Burns C., Cardon G., Carlin A., Ciarapica D., Colotto M., Condello G., Coppinger T., Cortis C., D’Haese S., De Craemer M., Di Blasio A., Hansen S., Iacoviello L., Issartel J., Izzicupo P., Jaeschke L., Kanning M., Ling F., Luzak A., Napolitano G., Nazare J.-A., Perchoux C., Pesce C., Pischon T., Polito A., Sannella A., Schulz H., Simon C., Sohun R., Steinbrecher A., Schlicht W., MacDonncha C., Capranica L., Boccia S., Henchoz Y. Socio-economic determinants of physical activity across the life course: A“ DEterminants of DIet and Physical ACtivity”(DEDIPAC) umbrella literature review. PLoS One. 2018;13(1):e0190737. doi: 10.1371/journal.pone.0190737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Mara-Eves A., Brunton G., Oliver S., Kavanagh J., Jamal F., Thomas J. The effectiveness of community engagement in public health interventions for disadvantaged groups: a meta-analysis. BMC Public Health. 2015;15:1–23. doi: 10.1186/s12889-015-1352-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paez D.C., Reis R.S., Parra D.C., Hoehner C.M., Sarmiento O.L., Barros M., Brownson R.C. Bridging the gap between research and practice: an assessment of external validity of community-based physical activity programs in Bogotá, Colombia, and Recife. Brazil. Transl. Behav. Med. 2015;5:1–11. doi: 10.1007/s13142-014-0275-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekmezi D.W., Neighbors C.J., Lee C.S., Gans K.M., Bock B.C., Morrow K.M., Marquez B., Dunsiger S., Marcus B.H. A culturally adapted physical activity intervention for Latinas: a randomized controlled trial. Am. J. Prev. Med. 2009;37(6):495–500. doi: 10.1016/j.amepre.2009.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins R., Kamphuis C., Van Lenthe F. The effects of small-scale physical and social environmental interventions on walking behaviour among Dutch older adults living in deprived neighbourhoods: results from the quasi-experimental NEW. ROADS study. Int. J. Behav. Nutr. Phys. Act. 2019;16:1–12. doi: 10.1186/s12966-019-0863-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabiee F., Robbins A., Khan M. Gym for Free: The short-term impact of an innovative public health policy on the health and wellbeing of residents in a deprived constituency in Birmingham. UK. Health Educ. J. 2015;74:691–704. doi: 10.1177/0017896914553957. [DOI] [Google Scholar]
- Reilly K.L., Kennedy S., Porter G., Estabrooks P. Comparing, contrasting, and integrating dissemination and implementation outcomes included in the RE-AIM and implementation outcomes frameworks. Front. Public Health. 2020;8:430. doi: 10.3389/fpubh.2020.00430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick B., Luisi D., Vogel A. Testing the Senior Exercise Self-efficacy Project (SESEP) for use with urban dwelling minority older adults. Public Health Nurs. 2008;25:221–234. doi: 10.1111/j.1525-1446.2008.00699.x. [DOI] [PubMed] [Google Scholar]
- Sheeran P., Harris P., Vaughan J., Oettingen G., Gollwitzer P.M. Gone exercising: Mental contrasting promotes physical activity among overweight, middle-aged, low-SES fishermen. Health Psychol. 2013;32:802–809. doi: 10.1037/a0029293. [DOI] [PubMed] [Google Scholar]
- Speck B.J., Hines-Martin V., Stetson B.A., Looney S.W. An environmental intervention aimed at increasing physical activity levels in low-income women. J. Cardiovasc. Nurs. 2007;22:263–271. doi: 10.1097/01.JCN.0000278957.98124.8a. [DOI] [PubMed] [Google Scholar]
- Spelt H., Tsiampalis T., Karnaki P., Kouvari M., Zota D., Linos A., Westerink J. Lifestyle E-coaching for physical activity level improvement: short-term and long-term effectivity in low socioeconomic status groups. Int. J. Environ. Res. Public Health. 2019;16:4427. doi: 10.3390/ijerph16224427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steckler A., McLeroy K.R. The importance of external validity. Am. J. Public Health. 2008;98(1):9–10. doi: 10.2105/AJPH.2007.126847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart A.L., Gillis D., Grossman M., Castrillo M., McLellan B., Sperber N., Pruitt L. PEER REVIEWED: Diffusing a Research-based Physical Activity Promotion Program for Seniors Into Diverse Communities: CHAMPS III. Prev. Chronic Dis. 2006;3 [PMC free article] [PubMed] [Google Scholar]
- Tannis C., Senerat A., Garg M., Peters D., Rajupet S., Garland E. Improving physical activity among residents of affordable housing: is active design enough? Int. J. Environ. Res. Public Health. 2019;16:151. doi: 10.3390/ijerph16010151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toto P.E., Raina K.D., Holm M.B., Schlenk E.A., Rubinstein E.N., Rogers J.C. Outcomes of a multicomponent physical activity program for sedentary, community-dwelling older adults. J. Aging Phys. Act. 2012;20:363–378. doi: 10.1123/japa.20.3.363. [DOI] [PubMed] [Google Scholar]
- Wanless D. HM Stationery Office; London: 2004. Securing good health for the whole population. [Google Scholar]
- Warburton D.E., Bredin S.S. Health benefits of physical activity: a systematic review of current systematic reviews. Curr. Opin. Cardiol. 2017;32:541–556. doi: 10.1097/HCO.0000000000000437. [DOI] [PubMed] [Google Scholar]
- Wen C.P., Wu X. Stressing harms of physical inactivity to promote exercise. Lancet [Series on physical activity] 2012;380:192–193. doi: 10.1016/S0140-6736(12)60954-4. [DOI] [PubMed] [Google Scholar]
- Wexler N., Fan Y., Das K.V., French S. Randomized Informational Intervention and Adult Park Use and Park-Based Physical Activity in Low-Income, Racially Diverse Urban Neighborhoods. J. Phys. Act. Health. 2021;18:920–928. doi: 10.1123/jpah.2020-0751. [DOI] [PubMed] [Google Scholar]
- White S.C., Agurto I., Araguas N. Promoting healthy behaviors to prevent chronic disease in Panama and Trinidad & Tobago: results of the women as agents of change project. J. Community Health. 2006;31:413–429. doi: 10.1007/s10900-006-9022-8. [DOI] [PubMed] [Google Scholar]
- White S.M., McAuley E., Estabrooks P.A., Courneya K.S. Translating physical activity interventions for breast cancer survivors into practice: an evaluation of randomized controlled trials. Ann. Behav. Med. 2009;37:10–19. doi: 10.1007/s12160-009-9084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis C.D., Riley B.L., Stockton L., Abramowicz A., Zummach D., Wong G., Robinson K.L., Best A. Scaling up complex interventions: insights from a realist synthesis. Health Res. Policy Syst. 2016;14:1–16. doi: 10.1186/s12961-016-0158-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson D.K., Trumpeter N.N., St. George S.M., Coulon S.M., Griffin S., Lee Van Horn M., Lawman H.G., Wandersman A., Egan B., Forthofer M., Goodlett B.D., Kitzman-Ulrich H., Gadson B. An overview of the “Positive Action for Today's Health”(PATH) trial for increasing walking in low income, ethnic minority communities. Contem. Clin. Trials. 2010;31(6):624–633. doi: 10.1016/j.cct.2010.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiltsey Stirman S., Bauman A.A., Miller C.J. The FRAME: an expanded framework for reporting adaptations and modifications to evidence-based interventions. Implement. Sci. 2019;14:1–10. doi: 10.1186/s13012-019-0898-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Withall J., Jago R., Fox K.R. Why some do but most don't. Barriers and enablers to engaging low-income groups in physical activity programmes: a mixed methods study. BMC Public Health. 2011;11:1–13. doi: 10.1186/1471-2458-11-507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2013. Physical activity promotion in socially disadvantaged groups: principles for action: PHAN Work Package 4 (No. WHO/EURO: 2013-4480-44243-62498). World Health Organization. Regional Office for Europe.
- Yancey A.K., Ory M.G., Davis S.M. Dissemination of Physical Activity Promotion Interventions in Underserved Populations. Am. J. Prev. Med. 2006;31:82–91. doi: 10.1016/j.amepre.2006.06.020. [DOI] [PubMed] [Google Scholar]
- Zoellner J., Connell C., Powers A., Avis-Williams A., Yadrick K., Bogle M.L. Does a six-month pedometer intervention improve physical activity and health among vulnerable African Americans? A feasibility study. J. Phys. Act. Health. 2010;7:224–231. doi: 10.1123/jpah.7.2.224. [DOI] [PubMed] [Google Scholar]