Abstract
Adherence to secondary prevention measures after acute coronary syndrome (ACS) is essential to prevent disease recurrence. In Brazil, the Brazilian Unified Health System (SUS, in Portuguese), and the private healthcare system (PHCS) coexist. We aimed to evaluate the adherence to secondary prevention in patients with ACS who were assisted by either SUS or PHCS. In this longitudinal prospective study, patients with ACS were admitted to the four cardiological reference hospitals of Sergipe, three of which assisted PHCS users, and one, SUS users. We analyzed the two patient care models with multiple logistic regression models for adherence to physical activity, pharmacotherapy, and smoking cessation. We enrolled 581 volunteers in this study: 44.1 % from SUS and 55.9 % from PHCS. PHCS users showed greater adherence to pharmacotherapy at both 30 and 180 (p = 0.001) days after ACS with better results in all classes of medications (p < 0.05) than SUS users did. They also showed better adherence to physical activity (p = 0.047). There was no distinction between the groups regarding smoking cessation. The secondary prevention measures after ACS were more effective in PHCS users than in SUS users due to better adherence, especially to pharmacotherapy and regular physical activity.
Keywords: Cardiovascular, Exercise, Global health, Healthcare quality, Recurrence
1. Introduction
Cardiovascular diseases, and acute coronary syndrome (ACS), among others, are important causes of morbidity and mortality in Brazil and across the world (World Health Organization. Global Status Report on Noncommunicable Diseases “Attaining the Nine Global Noncommunicable Diseases Targets; A Shared Responsibility.” Geneva, Switzerland: World Health Organization;, 2014, Piegas et al., 2015, Marasigan et al., 2020). The implementation of secondary prevention measures after an episode of ACS is a fundamental step to reducing the incidence of subsequent cardiovascular events (Wita et al., 2019). However, implementing them poses a challenge (Piepoli et al., 2016, Sakalaki et al., 2019) due to a brief hospital stay (Piepoli et al., 2016).
The guidelines recommend the use of evidence-based medication along with lifestyle interventions including smoking cessation, systemic blood pressure control, dietary counseling, weight management, and encouragement of physical activity (Piepoli et al., 2016, Steg et al., 2012, Herdy et al., 2014).
Adherence to secondary prevention therapies after hospital discharge in patients with ACS is a difficult goal to achieve, and the levels of adherence decrease after one year of the acute event (Cheng et al., 2015) which may have repercussions on the clinical outcomes and prognosis of these patients (Mehran et al., 2013, Steca et al., 2017, Oliveira et al., 2019). There is evidence that the healthcare model represents one of the factors that can influence adherence to treatment, and it is important to investigate possible disparities and their associations (Smolderen et al., 2013, Costa et al., 2019).
In Brazil, the two major healthcare systems are the Brazilian Unified Health System (SUS, in Portuguese), co-financed by the government, which provides universal coverage on which 150 million Brazilians depend on, and the private healthcare system (PHCS) with 50 million users (Brasil. Lei n. 8.080, de 19 de setembro de, 1990, Brasil. Adequação do atendimento pode reduzir mortes por infarto. Portal Brasil. Abril de, 2012). Although access to healthcare is a universally and an equitably established right for all Brazilians (Brasil. Lei n. 8.080, de 19 de setembro de, 1990), there are indications of distortions in the access and quality of these health services (Costa et al., 2019, Brasil. Lei n. 8.080, de 19 de setembro de, 1990, Brasil. Adequação do atendimento pode reduzir mortes por infarto. Portal Brasil. Abril de, 2012, Oliveira et al., 2019).
National registries documenting adherence to secondary prevention are scarce, especially those focusing on SUS and PHCS. Comparative studies between these systems allow us to evaluate the effectiveness of these measures in both contexts. The state of Sergipe, Brazil, being the smallest state in the nation with only four reference hospitals for cardiovascular diseases could serve as a laboratory for the initiative to measure the presumed disparity between SUS and PHCS in the care of ACS patients. Therefore, the objective of this research was to evaluate the adherence to secondary prevention measures in patients with ACS who were assisted by either SUS or PHCS.
The lack of adherence to medication treatment and lifestyle changes after ACS influences the emergence of subsequent cardiovascular events within the socioeconomic context and sedentary lifestyle.
2. Methods
2.1. Study design and location
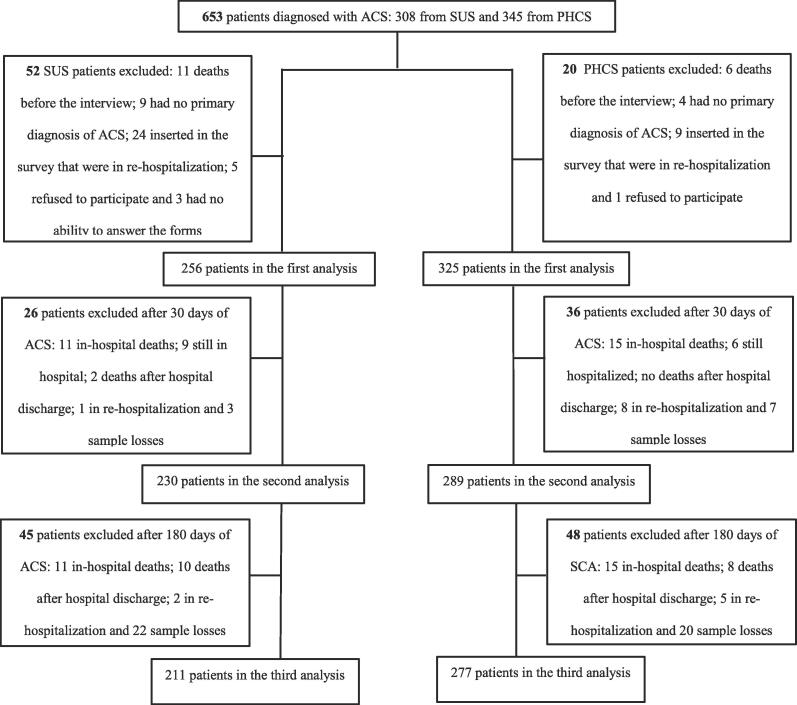
This observational, prospective, longitudinal study was carried out in four referral hospitals providing cardiology services in Aracaju City, Sergipe, Brazil. Among these hospitals, only one offers services through SUS and does not have an “open-door” service, which means that it requires the referral of patients from another health institution. The other three hospitals only offer PHCS, either through health insurance or disbursement. Our research followed the components of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) (Malta et al., 2010) protocol for observational studies, as shown in Fig. 1.
Fig. 1.
Organization chart of the process of inclusion, exclusion and loss of patient follow-up in the research.
2.2. Study sample
We adopted the “all-comers”’ sample type. This study enrolled 581 volunteers of both sexes, aged > 18 years. They were consecutively diagnosed with ACS, which was characterized by unstable angina (UA), acute myocardial infarction (AMI) without ST-segment elevation (NSTEMI), or AMI with ST-segment elevation (STEMI). Patients who did not agree to participate in the study by signing the informed consent form and/or who were unable to answer the study protocols were excluded from the study. The inclusion and exclusion process is shown in Fig. 1.
The diagnosis of ACS was based on the patients’ clinical history, with the onset of consistent symptoms of acute ischemia during the previous 24 h, including or not a series of increases in myocardial necrosis markers. These data were confirmed by electrocardiography, Doppler echocardiography, or cine coronary angiography. In some cases, the diagnosis was confirmed using more than one of the previously cited examinations (Eisen et al., 2016).
Our study was submitted to the Research Ethics Committee involving human beings at the Federal University of Sergipe (CEP/UFS). The committee approved our research (approval no. 302,544). All patients signed the informed consent form.
2.3. Data collection
Data were collected from October 2013 to March 2016. The study consisted of three stages: (1) initial evaluation after the diagnosis of ACS (hospitalization); (2) follow-up assessment 30 days after ACS; (3) final evaluation at 180 days after ACS. To this end, we used the Case Report Form which is composed of variables that provide information about patients’ sociodemographic and clinical conditions and levels of physical activity. To fill this form, data were obtained through interviews with the patient or one family member when the patients could not respond to the questionnaire by themselves. Their medical records were also analyzed.
The protocols of the medical teams of the hospitals followed national and international guidelines for patients with ACS (Nicolau et al., 2021, McDonagh and Metra, 2021, Bakker et al., 2020). At hospital discharge, individuals received general orientation regarding dietary intake, smoking cessation, physical activity, and adherence to drug treatment to prevent disease recurrence.
It is important to emphasize that at no time, the team of researchers of the study that originated this article performed interventions on the patients included in the research.
At admission and 180 days after ACS, the International Physical Activity Questionnaire (short version) (Committee, 2005, Matsudo et al., 2001) was used to assess adherence to physical activity recommendations. At 180 days after ACS, patients were surveyed about smoking cessation and information on new cardiovascular events.
In the context of secondary prevention, some classes of medications are labeled as “A” according to the Specialized Guidelines (Nicolau et al., 2021, McDonagh and Metra, 2021, Bakker et al., 2020), such as a) antithrombotics: acetylsalicylic acid (ASA) and/or a P2Y12 inhibitor (Prazygrel, Ticagrelor or Clopidogrel); b) β-blockers; c) statins; d) angiotensin-converting enzyme inhibitors (ACEI)/AT1 Receptor Blockers (ARB) and aldosterone receptor antagonist (spironolactone) in case of heart failure and/or left ventricular dysfunction. We collected the data related to the prescriptions of the medicines mentioned above from the medical records, and compared them to the prescriptions, with the patients present at the moment of hospital discharge. Patients were considered adherent at 30- and 180-days post ACS when they reported using all prescribed medications.
In relation to the socioeconomic level of the sample, the study is according to the Brazilian Economic Classification Criterion of the Brazilian Association of Research Companies (ABEP) (ABEP, 2008). For purposes of analysis, the eight economic levels, or economic classes, established by ABEP, were grouped and named as follows: A1, A2, and B1 in High Economic Level (A); B2, C1, and C2 in Medium Economic Level (M) and, D and E in Low Economic Level (B).
2.4. Data analysis
We performed the statistical analyses using the software R Core Team 2016, version 3.3.2, and adopted p < 0.05 as the level of statistical significance. Numerical variables were subjected to the Kolmogorov–Smirnov test to determine the type of distribution and were presented using the mean and standard deviation (SD). Categorical variables were described by the absolute (n) and relative (%) frequencies. For the comparison between the SUS and PHCS groups, we used the Mann-Whitney test for the quantitative variables. The analysis of association between the qualitative variables was performed using the chi-square test or Fisher's exact test, as appropriate.
We developed a multiple logistic regression model with adherence to pharmacotherapy, physical activity, and smoking cessation after ACS, and the dependent variables were adjusted for the socioeconomic variables (age, sex, schooling), clinical factors [presence of comorbidities such as systemic arterial hypertension, diabetes mellitus, dyslipidemia, overweight individuals, abdominal obesity], the healthcare model (SUS and PHCS), duration of hospitalization, and the number of medications prescribed at the time of discharge.
For making adjustments to the logistic regression model, we used the odds ratio (OR) for interpreting the results, and we adopted the 95 % confidence interval (CI) for the independent variables associated with adherence to medication, physical activity, and smoking cessation after ACS.
3. Results
A total of 581 individuals were admitted to the emergency services, 256 (44.1 %) from SUS and 325 (55.9 %) from PHCS. At 30 and 180 days after the ACS, we interviewed 519 (89.3 %) and 488 (84.0 %) patients, respectively.
Table 1 shows a comparison of the characteristics of the patients according to the healthcare model. The groups presented distinct characteristics except for the sedentary lifestyle. The SUS group had a significant higher number of males and patients with lower age, schooling, income, and socioeconomic status than the PHCS group. The SUS group also presented lower incidences of systemic arterial hypertension, diabetes mellitus, and dyslipidemia. Individuals in this group were also less likely to be overweight or exhibit central obesity. We also observed that SUS users had a higher frequency of STEMI, smoking, alcohol consumption, and a longer hospitalization time. It should be noted that at the time of hospital discharge, PHCS users were prescribed a greater number of medications, and after 30 and 180 days of the ACS, they received better medical care from cardiologists. At 180 days after the acute event, we observed similar behaviors between the groups concerning the cardiovascular outcomes and rehospitalization rates.
Table 1.
Socioeconomic, clinical characteristics and adherence to secondary prevention of patients with ACS, according to the type of healthcare, Aracaju, Sergipe, Brazil.
| Number of Valid Patients |
Type of Healthcare |
|||
|---|---|---|---|---|
| Categorical Variables | (%) | SUS (%) | PHCS (%) | p |
| Age group (Years)1 | ||||
| from 18 to 49 | 75 (12.9) | 51 (19.9) | 24 (7.4) | |
| from 50 to59 | 144 (24.8) | 68 (26.6) | 76 (23.4) | |
| from 60 to 69 | 197 (33.9) | 88 (34.4) | 109 (33.5) | <0.001 |
| from 70 to79 | 108 (18.6) | 38 (14.8) | 70 (21.5) | |
| ≥ 80 | 57 (9.8) | 11 (4.3) | 46 (14.2) | |
| Sex1 | ||||
| Male | 370 (63.7) | 181 (70.7) | 189 (58.2) | <0.002 |
| Female | 211 (36.3) | 75 (29.3) | 136 (41.8) | |
| Schooling (Years)1 | ||||
| No schooling or < 1 year | 44 (7.6) | 32 (12.5) | 12 (3.7) | |
| from 1 to 3 | 84 (14.5) | 64 (25.0) | 20 (6.1) | <0.001 |
| from 4 to 8 | 178 (30.6) | 99 (38.7) | 79 (24.3) | |
| 9 years or more | 275 (47.3) | 61 (23.8) | 214 (65.9) | |
| Familiar Income Per Capita (MW)2 | ||||
| ≤ 1 | 248 (43.0) | 196 (76.9) | 52 (16.2) | |
| > 1 and ≤ 3 | 216 (37.5) | 54 (21.1) | 162 (50.5) | <0.001 |
| > 3 and ≤ 5 | 50 (8.7) | 3 (1.2) | 47 (14.6) | |
| > 5 | 62 (10.8) | 2 (0.8) | 60 (18.7) | |
| ABEP Classification 1 | ||||
| Class A | 50 (8.6) | 3 (1.2) | 47 (14.5) | |
| Clases B1 and B2 | 179 (30.8) | 26 (10.1) | 153 (47.1) | <0.001 |
| Clases C1 and C2 | 207 (35.6) | 101 (39.5) | 106 (32.6) | |
| Clases D – E | 145 (25.0) | 126 (49.2) | 19 (5.8) | |
| ACS Classification 1 | ||||
| UA | 101 (17.4) | 20 (7.8) | 81 (24.9) | |
| NSTEMI | 213 (36.7) | 47 (18.4) | 166 (51.1) | <0.001 |
| STEMI | 267 (45.9) | 189 (73.8) | 78 (24.0) | |
| Systemic Arterial Hypertension1 | 464 (79.9) | 194 (75.8) | 270 (83.1) | 0.037 |
| Diabetes Mellitus1 | 208 (35.8) | 76 (29.7) | 132 (40.6) | 0.008 |
| Dyslipidemia 1 | 322 (55.4) | 104 (40.6) | 218 (67.1) | <0.001 |
| Overweight2 | 390 (67.7) | 153 (60.5) | 237 (73.4) | 0.001 |
| Abdominal Obesity 3 | 428 (75.3) | 171 (68.1) | 257 (81.1) | <0.001 |
| Sedentarism1 | 311 (53.5) | 131 (51.2) | 180 (55.4) | 0.353 |
| Alcoholism1 | 70 (12.0) | 39 (15.2) | 31 (9.5) | 0.049 |
| Smoking1 | ||||
| No | 268 (46.1) | 100 (39.1) | 168 (51.7) | <0.001 |
| Yes | 99 (17.0) | 63 (24.6) | 36 (11.1) | |
| Ex-smoker | 214 (36.9) | 93 (36.3) | 121 (37.2) | |
| Hospitalization time (Days)4 | 555 (100.0) | 11.44 (11.6)⸸ | 9.42 (10.6)⸸ | <0.001A |
| Prescribed Medications at Discharge 4 | 555 (100.0) | 6.67 (1.3)⸸ | 7.20 (1.5)⸸ | <0.001A |
| No medical care 30 days after ACS5 | 63 (12.1) | 45 (19.6) | 18 (6.2) | <0.001 |
| No medical care 180 days after ACS6 | 47 (9.6) | 31 (14.7) | 16 (5.8) | 0.002 |
| Presence of CV outcomes 180 days post-ACS7 | 581 (100.0) | 45 (17.6) | 54 (16.6) | 0.845 |
| ACS | 32 (12.5) | 36 (11.1) | 0.689 | |
| Stroke | 5 (2.0) | 4 (1.2) | 0.516 | |
| CHF | 7 (2.7) | 8 (2.5) | 0.987 | |
| Cardiac Arrest | 1 (0.4) | 6 (1.8) | 0.141 | |
| Rehospitalization8 | 513 (100.0) | 29 (13.0) | 51 (17.6) | 0.188 |
| Adherence to Secondary Prevention 30 days post-ACS | 519 (100.0) | |||
| Adherence to pharmacotherapy | ||||
| No | 180 (34.7) | 99 (43.0) | 81 (28.0) | 0.001 |
| Yes | 339 (65.3) | 131 (57.0) | 208 (72.0) | |
| Adherence to Acetylsalicylic Acid9 | 478 (96.0) | 204 (94.4) | 274 (97.2) | 0.193 |
| Adherence to Other Antiplatelets9 | 481 (93.9) | 206 (90.7) | 275 (96.5) | 0.012 |
| Adherence to Statins9 | 437 (89.4) | 175 (83.3) | 262 (93.9) | <0.001 |
| Adherence to β-Blockers9 | 432 (92.7) | 181 (88.7) | 251 (95.8) | 0.006 |
| Adherence to ACEI/ARB9 | 409 (90.9) | 169 (87.1) | 240 (93.8) | 0.024 |
| Smoking Cessation | ||||
| Smoker | 17 (3.3) | 7 (3.0) | 10 (3.5) | 0.986 |
| Non smoker | 502 (96.7) | 223 (97.0) | 279 (96.5) | |
| Adherence to Secondary Prevention 180 days post-ACS | 488 (100.0) | |||
| Adherence to pharmacotherapy | ||||
| No | 161 (33.0) | 88 (41.7) | 73 (26.4) | 0.001 |
| Yes | 327 (67.0) | 123 (58.3) | 204 (73.6) | |
| Adherence to Acetylsalicylic Acid9 | 434 (92.5) | 174 (88.3) | 260 (95.6) | 0.006 |
| Adherence to Other Antiplatelets9 | 428 (88.6) | 172 (82.3) | 256 (93.4) | <0.001 |
| Adherence to Statins9 | 388 (83.3) | 143 (72.6) | 245 (91.1) | <0.001 |
| Adherence to β-Blockers9 | 392 (88.9) | 157 (83.1) | 235 (93.3) | 0.001 |
| Adherence to ACEI/ARB9 | 357 (84.6) | 130 (74.3) | 227 (91.9) | <0.001 |
| Smoking Cessation | ||||
| Smoker | 25 (5.1) | 14 (6.6) | 11 (4.0) | 0.264 |
| Non smoker | 463 (94.9) | 197 (93.4) | 266 (96.0) | |
| Physical Activity | ||||
| Sedentary | 280 (57.4) | 133 (63.0) | 147 (53.1) | 0.034 |
| Active | 208 (42.6) | 78 (37.0) | 130 (46.9) | |
ACS = Acute Coronary Sindrome; MW = Minimum Wage; ABEP = Brazilian Asssociation of Research Companies (2015); UA = Unstable Angina; NSTEMI = non-ST elevation myocardial infarction; STEMI = ST elevation myocardial infarction; CV = Cardiovascular; CHF = Congestive Heart Failure; ACEI = Angiotensin Converting Enzyme Inhibitors; ARB = Angiotensin II Receptor Blockers; p = Fisher’s Exact Test or Pearson’s Chi-square Test; A = Mann-Whitney Test; ⸸Mean (±SD); 1 = 581; 2 = 576; 3 = 568; 4 = Patients excluded because of intra-hospital death (26 patients); 5 = 519; 6 = 488; 7 = Total number of patients admitted in the study, since new outcomes could arise during hospitalization of ACS; 8 = Patients who died in the hospital and sample losses were excluded (68 patients); 9 = Patients Indicated to use medication at hospital discharge.
Regarding adherence to secondary prevention, we observed that compared to PHCS users, SUS users showed a lower adherence to pharmacotherapy at the two time points of evaluation after ACS, as well as to physical activity at 180 days after the acute event. There was no distinction between the groups as regards smoking cessation after ACS (Table 1).
In the evaluation of adherence to medication of different classes based on the healthcare model, the results revealed that at 30 days after ACS, SUS users had a lower adherence to four classes of drugs (other antiplatelets, statins, beta-blockers, and ACEI/ARBs) than that seen in PHCS users. At 180 days of follow-up, SUS users showed a lower adherence to all classes of medications (Table 1).
Table 2 shows the number and percentage of patients using the various classes of medications after ACS. The adherence was the best for acetylsalicylic acid, while that for lipid-lowering agents was lower at the two assessment timepoints, with a reduction in the adherence level for all classes of medications at 180 days after the acute event.
Table 2.
Prescription and use of pharmacological therapy after Hospital Discharge in patients with ACS, Aracaju, Sergipe, Brazil.
| Pharmacological Therapy | Patients Indicated to use medication at HD | PI at 30 days post-ACS |
Patients Interviewed at 30 days post-ACS |
PI at 180 days post-ACS |
Patients Interviewed at 180 days post-ACS |
||
|---|---|---|---|---|---|---|---|
| WM (%) | NM (%) | WM (%) | NM (%) | ||||
| ASA | 532 (95.8) | 498 | 478 (96.0) | 20 (4.0) | 469 | 434 (92.5) | 35 (7.5) |
| Other Antiplatelets | 544 (98.0) | 512 | 481 (93.9) | 31 (6.1) | 483 | 428 (88.6) | 55 (11.4) |
| Statins | 521 (93.9) | 489 | 437 (89.4) | 52 (10.6) | 466 | 388 (83.3) | 78 (16.7) |
| β-Blockers | 493 (88.8) | 466 | 432 (92.7) | 34 (7.3) | 441 | 392 (88.9) | 49 (11.1) |
| ACEI/ARB | 473 (85.2) | 450 | 409 (90,9) | 41 (9.1) | 422 | 357 (84.6) | 65 (15.4) |
Patients who were discharged = 555; HD = Hospital discharge; ACS = Acute Coronary Syndrome; PI = Patients Interviewed; WM = With Medication; NM = No medication; ASA = Acetylsalicylic Acid; ACEI = Angiotensin Converting Enzyme Inhibitors; ARB = Angiotensin II Receptor Blockers.
The multiple logistic regression analysis showed that the adherence to physical activity at 180 days after ACS was better in younger patients, females, PHCS users, and those with no abdominal obesity (Table 3).
Table 3.
Multiple logistic regression models of adherence to physical activity, medication and smoking cessation as dependent variables, adjusted for socioeconomic variables, clinical and healthcare model in patients with ACS, Aracaju, Sergipe, Brazil.
|
Adherence to Physical Activity | ||||||
|---|---|---|---|---|---|---|
| Variables |
180 Days after ACSB |
|||||
| OR (CI 95 %) | Standard Error | p | ||||
| Hospitalization time1 | 0.79 (0.61; 1.04) | 0.14 | 0.096 | |||
| Age (Years) | 0.96 (0.94; 0.98) | 0.01 | <0.001 | |||
| Male Sex | 0.46 (0.30; 0.70) | 0.22 | <0.001 | |||
| Schooling | 1.02 (0.97; 1.07) | 0.03 | 0.421 | |||
| Private Healthcare System | 1.76 (1.21; 2.79) | 0.21 | 0.047 | |||
| SAH | 0.61 (0.36; 1.01) | 0.27 | 0.059 | |||
| Diabetes Mellitus | 1.29 (0.81; 2.04) | 0.24 | 0.286 | |||
| Dyslipidemia | 1.17 (0.77; 1.78) | 0.22 | 0.478 | |||
| Overweight | 1.74 (0.96; 3.17) | 0.31 | 0.072 | |||
| Abdominal Obesity | 0.97 (0.95; 0.99) | 0.01 | 0.006 | |||
| N° of prescribed medications2 | 0.90 (0.78; 1.05) | 0.08 | 0.198 | |||
| Adherence to Medication | ||||||
| Variables | 30 Days after ACSA | 180 Days after ACSB | ||||
| OR (CI 95 %) | Standard Error | p | OR (CI 95 %) | Standard Error | p | |
| Hospitalization time1 | 0.60 (0.44; 0.80) | 0.15 | 0.001 | 0.65 (0.49; 0.86) | 0.15 | 0.003 |
| Age (Years) | 0.98 (0.96; 1.00) | 0.01 | 0.027 | 0.98 (0.96; 1.00) | 0.01 | 0.050 |
| Male Sex | 1.04 (0.68; 1.59) | 0.22 | 0.844 | 1.21 (0.78; 1.88) | 0.23 | 0.405 |
| Schooling | 0.96 (0.91; 1.00) | 0.03 | 0.083 | 0.95 (0.90; 1.00) | 0.03 | 0.058 |
| Private Healthcare System | 2.38 (1.45; 3.95) | 0.26 | 0.001 | 2.48 (1.48; 4.19) | 0.27 | 0.001 |
| SAH | 0.74 (0.44; 1.22) | 0.26 | 0.244 | 0.63 (0.36; 1.10) | 0.29 | 0.112 |
| Diabetes Mellitus | 1.15 (0.73; 1.80) | 0.23 | 0.550 | 1.23 (0.77; 1.98) | 0.24 | 0.403 |
| Dyslipidemia | 1.37 (0.92; 2.05) | 0.21 | 0.130 | 1.64 (1.07; 2.52) | 0.22 | 0.024 |
| Overweight | 0.99 (0.55; 1.78) | 0.30 | 0.979 | 0.72 (0.39; 1.32) | 0.32 | 0.294 |
| Abdominal Obesity | 0.99 (0.97; 1.01) | 0.01 | 0.465 | 0.99 (0.97; 1.01) | 0.01 | 0.388 |
| N° of prescribed medications2 | 1.36 (0.48; 3.89) | 0.54 | 0.573 | 1.29 (0.43; 3.90) | 0.56 | 0.650 |
| Smoking CessationC | ||||||
| Variables | 30 Days after ACS | 180 Days after ACS | ||||
| OR (CI 95 %) | Standard Error | p | OR (CI 95 %) | Standard Error | p | |
| Hospitalization time1 | 0.93 (0.45; 1.98) | 0.34 | 0.838 | 1.04 (0.56; 1.90) | 0.30 | 0.907 |
| Age (Years) | 0.97 (0.93; 1.02) | 0.02 | 0.180 | 0.95 (0.91; 0.99) | 0.02 | 0.009 |
| Male Sex | 0.65 (0.23; 1.92) | 0.49 | 0.382 | 1.45 (0.53; 4.55) | 0.52 | 0.468 |
| Schooling | 0.93 (0.81; 1.06) | 0.06 | 0.243 | 0.92 (0.82; 1.03) | 0.06 | 0.143 |
| Private Healthcare System | 2.69 (0.73; 10.65) | 0.62 | 0.111 | 2.06 (0.66; 6.61) | 0.56 | 0.201 |
| SAH | 1.02 (0.33; 3.56) | 0.55 | 0.973 | 1.15 (0.43; 3.25) | 0.49 | 0.783 |
| Diabetes Mellitus | 0.49 (0.10; 1.77) | 0.64 | 0.275 | 0.43 (0.09; 1.45) | 0.65 | 0.197 |
| Dyslipidemia | 0.25 (0.07; 0.77) | 0.56 | 0.013 | 0.41 (0.14; 1.07) | 0.49 | 0.067 |
| Overweight | 0.41 (0.08; 1.86) | 0.71 | 0.217 | 0.25 (0.06; 0.92) | 0.66 | 0.036 |
| Abdominal Obesity | 1.01 (0.95; 1.07) | 0.03 | 0.681 | 0.99 (0.94; 1.05) | 0.03 | 0.808 |
| N° of prescribed medications2 | 1.15 (0.77; 1.66) | 0.18 | 0.438 | 1.03 (0.73; 1.43) | 0.17 | 0.857 |
ACS = Acute Coronary Syndrome; OR = Odds Ratio; CI = Confidence Interval; SAH = Systemic Arterial Hypertension; N°=number; 1 = In days (Logarithm); 2 = Logarithm; Adherence to physical activity: 0 = Sedentary (Non-adherence) and 1 = Active (Adherence). Adherence to medication: 0 = Non-adherence and 1 = Adherence; Smoking: 0 = Adherence to orientation (non-smoking) and 1 = Non-adherence (smoking); Age (years) in the interview; Gender: 0 = Female and 1 = Male; Schooling (years) in the interview; Healthcare model: 0 = SUS and 1 = PHCS; SAH: 0 = No and 1 = Yes. Diabetes mellitus: 0 = No and 1 = Yes; Dyslipidemia: 0 = No and 1 = Yes; Overweight: 0 = No and 1 = Yes; Abdominal obesity: 0 = No and 1 = Yes; Number of prescribed medications at hospital discharge. A = 519 patients evaluated; B = 488 patients evaluated; C = Performed with patients (99) who self-declared smokers on admission.
At 30 and 180 days after the acute event, we observed a positive correlation between PHCS users and a shorter hospitalization period, and adherence to pharmacotherapy. The data also demonstrated that younger individuals showed a greater adherence to medications at 30 days after ACS and dyslipidemic individuals displayed a greater adherence to pharmacotherapy at 180 days after the acute event (Table 3).
Patients with dyslipidemia were more likely to stop smoking at 30 days after ACS, whereas older and overweight individuals were more likely to quit smoking at 180 days after the acute event (Table 3).
4. Discussion
The objective of this research was to evaluate the adherence to secondary prevention measures (practice of physical activity, adherence to medications, and smoking cessation) in patients with ACS who were assisted by SUS and PHCS.
The main findings of the present study were as follows: PHCS users showed greater adherence to the drug therapy at both timepoints of evaluation than that seen in SUS patients. In addition, PHCS users showed a better adherence to all classes of medications at 180 days after the acute event. We also found that statins (83.3 %) and ACEI/ARB (84.6 %) were the medications associated with the lowest adherence, whereas acetylsalicylic acid was associated with the highest adherence (92.5 %). Utilization of private healthcare and a short period of hospitalization (30 days after ACS: OR = 0.60 (0.44; 0.80), p = 0.001). 180 days after ACS: OR = 0.65 (0.49; 0.86), p = 0.003) were associated with better adherence to medication at both time points.
The evaluation of the implementation of lifestyle changes in this study revealed a reduction in the frequency of smokers at 180 days after ACS (51 %) regardless of the type of healthcare provided to the patient. However, regarding physical activity, there was an increase in the percentage of sedentary individuals in the phase between hospital admission (51.2 %) and 180 days (63 %) after the acute event in the SUS group. We also observed that subjects who were younger (OR = 0.96 (0.94; 0.98), p < 0.001), female (OR = 0.46 (0.30; 0.70, p < 0.001), as well as PHCS users (OR = 1.76 (1.21; 2.79), p = 0.047) showed a better adherence to physical activity.
ACS remains a serious public health problem in Brazil and worldwide (Bakker et al., 2020, Cheng et al., 2015, Costa et al., 2019, Eisen et al., 2016, Herdy et al., 2014, Marasigan et al., 2020, Mehran et al., 2013, Nicolau et al., 2021, Oliveira et al., 2019, Oliveira et al., 2019, Piegas et al., 2015, Piepoli et al., 2016, Sakalaki et al., 2019, Smolderen et al., 2013, Steca et al., 2017, Steg et al., 2012, Wita et al., 2019, Nicolau et al., 2021), and it is essential to use evidence-based medications and lifestyle modifications as a form of secondary prevention in order to improve the prognosis of these patients (Piepoli et al., 2016, Nicolau et al., 2021, Barroso, et al., 2020).
Worryingly, there was a lower adherence to the pharmacotherapy recommended by the guidelines (Piegas et al., 2015, Piepoli et al., 2016, Nicolau et al., 2021) in individuals assisted by SUS compared to the adherence levels of those assisted by PHCS (30 days after ACS: PHCS = 72 %, SUS = 57 %, p = 0.001). 180 days after ACS: PHCS = 73.6 %, SUS = 58.3 %, p = 0.001. SUS users showed low adherence to drug treatment for all classes of drugs (Acetylsalicylic Acid: PHCS = 95.6 %, SUS = 88.3 %, p = 0.006. Other Antiplatelets: PHCS = 93.4 %, SUS = 82.3 %, p < 0.001. Statins: PHCS = 91.1 %, SUS = 72.6 %, p < 0.001. β-Blockers: PHCS = 93.3 %, SUS = 83.1 %, p = 0.001. ACEI/ARB: PHCS = 91.9 %, SUS = 74.3 %, p < 0.001), which revealed the vulnerability of those assisted exclusively by public healthcare. This finding was also confirmed by the logistic regression model analysis at both time points of evaluation (30 days after ACS: OR = 2.38 (1.45; 3.95), p = 0.001. 180 days after ACS: OR = 2.48 (1.48; 4.19), p = 0.001).
Drummond et al. (2020) observed that although SUS increased support for free drug therapy from 39.24 % in 1998 to 64.72 % in 2008, irregularities in public policy together with socioeconomic inequality associated with low education, poverty, and diseases. Acute disorders still compromise access to pharmacotherapy for the most vulnerable population (Barreto, 2020).
Barretto et al. (2020) also identified a similar pattern in hypertensive patients followed by SUS, 40 % of which had low adherence to drug treatment. The authors suggest that older age and income above 2 minimum wages are factors that contribute to greater adherence to pharmacotherapy.
The results of this research become even more relevant considering the evidence in the literature of the unequivocal benefits of pharmacological agents (Piegas et al., 2015, Nicolau et al., 2021, Barroso, et al., 2020, Drummond, 2020, Barreto, 2020, Stone et al., 2014). They also underlined the fact that secondary prevention therapies continue to be underused, as evidenced in the study by Cheng et al. (2015) (Cheng et al., 2015) when outlining the modifiable and non-modifiable reasons, as well as technological interventions to improve adherence to secondary prevention after ACS, and detected that non-adherence to pharmacology in volunteers was 40 % to 75 %9. It is also important to note that there is a tendency for adherence levels to decrease over time, as shown by Ulrich et al. (2020), detecting that 37.8 % of individuals were using Acetylsalicylic Acid, 70.4 % were using ACEI, and only 24.1 % were using statins, β-Blockers, ACEI, and an antiplatelet agent simultaneously after one year of the event.
In this study, the medications associated with lower levels of adherence were the statins (83.3 %) and ACEI/ARB (84.6 %). In the study conducted by Ho et al. (2014), it was verified that patients enrolled in an intervention program showed better adherence to statins (93.2 %), ACEI/ARB (93.1 %), and clopidogrel (86.8 %) than that of patients in the control group (71.3 %, 81.7 % and 70.7 %, respectively). Therefore, the need to establish strategies to improve adherence to secondary prevention measures, especially in patients assisted by SUS in the state of Sergipe became quite evident.
Another important fact observed in this research was the prolonged hospitalization (mean of 11.44 days (±11.6 SD)) for SUS users during the acute event, and this variable was shown to be an independent predictor for a decreased adherence to post-hospital pharmacotherapy. Thus, these findings reinforced that disparities in the quality of healthcare may have influenced PHCS users (mean 9.42 days (±10.6 SD), p < 0.001) which enabled them to adhere to the treatment proposed after ACS to a greater degree.
The literature states that disparities in the quality of health care offered can exert an influence on the prognosis of patients, as verified in the research conducted by Vallabhajosyula et al (2019) (Vallabhajosyula et al., 2019) when checking the level of in-hospital mortality resulting from acute myocardial infarction followed by cardiogenic shock. Urban university hospital (OR = 0.87 (0.84; 0.91), p < 0.001) and urban non-university hospital (OR = 0.81 (0.78; 0.84), p < 0.001) showed lower mortality than rural hospitals. Compared with smaller hospitals, admission to large hospitals was associated with lower mortality outcomes (OR = 0.94 (0.91; 0.98), p = 0.002). This reflects the differences in how health services can be accessed by different individuals and reveals the inequalities in healthcare meted out to such individuals (Costa et al., 2019, Malta et al., 2017, Mirkin et al., 2017, Costa et al., 2022).
According to the literature, smoking may be highlighted as a key risk factor (World Health Organization. Global Status Report on Noncommunicable Diseases “Attaining the Nine Global Noncommunicable Diseases Targets; A Shared Responsibility.” Geneva, Switzerland: World Health Organization;, 2014, Brasileiro, 2013, Yun et al., 2015) from among a set of risk factors responsible for the majority of deaths due to non-transmissible chronic diseases. Smoking is a modifiable cardiovascular risk factor (Costa et al., 2022, Stone et al., 2014, Brasileiro, 2013), and patients should be encouraged to abandon this habit after ACS in order to prevent the recurrence of the disease (Chomistek et al., 2015, Nicolau et al., 2021, Piepoli et al., 2016, Smolderen et al., 2013, Steg et al., 2012, Yun et al., 2015, Brasileiro, 2013, Nicolau et al., 2021).
In this study, we found that there was a reduction in the percentage of smokers (17 % vs 5.1 %) post ACS, and there was no distinction between the types of healthcare regarding this trend (p = 0.264). In addition, the number of smokers (5.1 %) after ACS was lower than that found in a research (18.5 %) that aimed to investigate the prevalence of a healthy lifestyle in individuals with a history of coronary artery disease or stroke (Teo et al., 2013).
Worldwide, physical inactivity contributes to 3.2 million deaths and 69.3 million disabilities per year (World Health Organization, 2014). While evaluating patients at 180 days after ACS, we noticed a large number of patients (57.4 %) with a sedentary lifestyle in the sample, with worse results in the SUS group than in the PHCS group (63 % vs 53.1 %; p = 0.034). The frequency of sedentarism in this sample population exceeded the frequency of sedentarism at the national (46 %), regional (44.3 %), and state (44.7 %) levels (Brasileiro, 2013).
In the study conducted by Goodwin et al (2019) (Goodwin et al., 2019) with the purpose of identifying factors associated with physical activity performance after hospital discharge in ACS patients, it was found that 39.7 % of participants were sedentary, with an association for female sex (OR = 2.76 (1.10; 6.95), p = 0.031) and older individuals (OR = 1.11 (1.06;1.17), p < 0.001).
Our data also revealed that younger individuals showed better adherence to the recommendations for physical activity (OR = 0.96 (0.94; 0.98), p < 0.001), but contrasted with the literature on that, this study revealed a higher number of active individuals of the female sex (OR = 0.46 (0.30; 0.70), p < 0.001).
Greater adherence to the recommendations for physical activity was also seen in PHCS users (OR = 1.76 (1.21; 2.79), p < 0.047), and we verified that this assistance model exerted a great influence on the decision of individuals to lead an active lifestyle. The data on sedentarism concerning the patients of this research are worrisome as the relationship between physical exercise, secondary prevention, and the prognosis of individuals following coronary artery disease has already been established in the literature (Piegas et al., 2015, Marasigan et al., 2020, Chomistek et al., 2015, Goodwin et al., 2019, Broers et al., 2020, Nakayama et al., 2020).
Rodrigues et al. (20177), in a systematic review, found that the socioeconomic level directly impacts the practice of physical activity, especially due to the low income that favors a greater workload and longer commuting time to work. In addition, the lack of knowledge of the importance of physical activity in the treatment due to the low level of education associated with socioeconomic inequality contributes to the higher prevalence of sedentary lifestyle. On the other hand, those with higher income, education and professional status have a higher level of activity.
We note that a study of individuals with cardiometabolic risk enrolled in an intervention program involving the practice of physical activity in association with guidelines for a healthy lifestyle proved to be a more effective strategy in reversing sedentary behavior (50 %) than receiving only lifestyle guidelines (21 %) (Ensenyat et al., 2020). Thus, the literature shows that intervention strategies can be promising in changing inactive behaviors in individuals with chronic conditions, including cardiovascular conditions (Dempsey et al., 2021).
This study had some limitations. First, we gathered the information on adherence to pharmacotherapy with simple self-report questions without using validated measuring instruments. Similarly, we did not validate the definitions of smoking cessation and persistence by measuring the nicotine levels. Second, the public hospital included in this study had discontinued healthcare services for SUS users in July 2014 and June 2015, a fact that may have contributed to a reduced number of patients assisted by this service. We suggest that future studies use validated instruments and/or methods to confirm our results. Finally, due to multicollinearity, it was not possible to insert the ABEP classification in the logistic regression model.
The findings of this investigation present evidence that social factors and possible disparities in healthcare quality influence the degree of adherence to secondary prevention measures after ACS in the State of Sergipe. It is important to emphasize that the use of a more circumscribed geographical area would probably represent a more realistic strategy considering the continental dimensions of Brazil. However, we can speculate that the results obtained from the sample population in Sergipe are a reflection of the situation at the national level.
5. Conclusions
We can conclude that PHCS was associated with better adherence to pharmacotherapy and with better results for all classes of medications at 180 days after ACS. Regarding lifestyle changes, high frequencies of sedentarism were detected in the study patients, and with worse results in the public service when compared to the private service. However, no distinction was found between the groups for adherence to smoking cessation guidelines. Thus, the findings of this research present evidence that social factors, besides disparities in the quality of care, influenced the difference in adherence to secondary prevention.
This study demonstrates that more effective measures will be needed to overcome the socioeconomic barrier in the prevention of ACS, through lifestyle changes (combating smoking and sedentary lifestyles) and better pharmacological adherence strategies for this population.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
All the patients that were willing to share their data with us and making this work possible.
Author Contributions
IMNBCC, DGS and ACSS conceptualized the study, coordinated the last follow-up with participants from the study, conducted the statistical analysis, and wrote the manuscript. MAAS and JGJ conceptualized the study and wrote the manuscript. JRSS conducted the statistical analysis. VBO, FAA, LMSMO, JOC, MFCS, SMV, FJA, VVA, JLMO, LMCP, LVSA, LSM, RRA and LB wrote the manuscript. Supervision: ACSS. All authors approved the final version.
Funding
This research was funded by the Higher Education Personnel Improvement Coordination (CAPES, Brazil) n° 1793619.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Research Ethics Committee of the Federal University of Sergipe, CAAE: 15868513.8.0000.5546/statement number: 302.544. (Date of approval: 07/06/2013).
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data availability
The authors are unable or have chosen not to specify which data has been used.
References
- ABEP. Associação Brasileira de Empresa e Pesquisa. CCEB. Critério de Classificação Econômica Brasil, 2008. Available at: http://www.abep.org.br . Accessed June 17, 2022.
- Bakker M., Uijl I., Hoeve N., et al. The Association between Exercise Capacity and Health-Related Quality of Life during and after Cardiac Rehabilitation in Acute Coronary Syndrome Patients: a substudy of the OPTICARE Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2020;101(4):650–657. doi: 10.1016/j.apmr.2019.11.017. [DOI] [PubMed] [Google Scholar]
- Barreto MNSC. Factors associated with adherence to pharmacological treatment and their influence on blood pressure control in hypertensive patients registered in the Pernambuco Family Health Strategy: RedeNut Study. 2020. Thesis (Doctorate in Public Health). Instituto Aggeu Magalhães, Fundação Oswaldo Cruz, Recife, 2020.
- Barroso, W.K.S. Rodrigues CIS, Bortolotto LA, et al. Diretrizes Brasileiras de Hipertensão Arterial – 2020. Arq Bras Cardiol. 2021;116(3):516-658. 10.36660/abc.20201238. [DOI] [PMC free article] [PubMed]
- Brasil. Adequação do atendimento pode reduzir mortes por infarto. Portal Brasil. Abril de 2012. Disponível em: http://www.brasil.gov.br/saude/2012/04/adequacao-do-atendimento-pode-reduzir-mortes-por-infarto Accessed November 08, 2017.
- Brasil. Lei n. 8.080, de 19 de setembro de 1990. Dispõe sobre as condições para a promoção, proteção e recuperação da saúde, a organização e o funcionamento dos serviços correspondentes e dá outras providências. http://www.planalto.gov.br/ccivil_03/Leis/L8080.htm. Accessed November 08, 2017.
- Instituto Brasileiro de Geografia e Estatística (IBGE). Ministério da Saúde. Ministério do Planejamento, Orçamento e Gestão. Pesquisa Nacional de Saúde 2013. Percepção do estado de saúde, estilos de vida e doenças crônicas. Rio de Janeiro; 2014. p. 1-53.
- Broers E.R., Gavidia G., Wetzels M., Ribas V., Ayoola I., Piera-Jimenez J., Widdershoven J.W.M.G., Habibović M. Usefulness of a lifestyle intervention in patients with cardiovascular disease. Am. J. Cardiol. 2020;125(3):370–375. doi: 10.1016/j.amjcard.2019.10.041. [DOI] [PubMed] [Google Scholar]
- Cheng K., Ingram N., Keenan J., Choudhury R.P. Evidence of poor adherence to secondary prevention after acute coronary syndromes: possible remedies through the application of new technologies. Open Heart. 2015;2(1):e000166. doi: 10.1136/openhrt-2014-000166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chomistek A.K., Chiuve S.E., Eliassen A.H., Mukamal K.J., Willett W.C., Rimm E.B. Healthy lifestyle in the primordial prevention of cardiovascular disease among young women. J. Am. Coll. Cardiol. 2015;65(1):43–51. doi: 10.1016/j.jacc.2014.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee IPAQR. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ). Retrieved November. 2005;15:2010. https://www.ipaq.ki.se/scoring.pdf. Accessed Maio 14, 2014.
- Costa I.M.N.B.C., Silva D.G., Oliveira J.L.M., Silva J.R.S., Andrade F.A., Jorge J.G., et al. Quality of life among patients with acute coronary syndromes receiving care from public and private health care Systems. Clin. Pract. 2022;12:513–526. doi: 10.3390/clinpract12040055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa I.M.N.B.C., Silva D.G., Barreto Filho J.A.S., Oliveira J.L.M., Silva J.R.S., Buarque M.D.B.M., Nascimento T., Jorge J.d.G., Almeida A.S., Almeida-Santos M.A., Sousa A.C.S. Diet quality of patients with acute coronary syndrome receiving public and private health care. Nutrition. 2019;59:131–137. doi: 10.1016/j.nut.2018.07.111. [DOI] [PubMed] [Google Scholar]
- Dempsey P.C., Friedenreich C.M., Leitzmann M.F., Buman M.P., Lambert E., Willumsen J., Bull F. Global Public Health Guidelines on Physical Activity and Sedentary Behavior for People Living With Chronic Conditions: A Call to Action. J Phys Act Health. 2021;18(1):76–85. doi: 10.1123/jpah.2020-0525. [DOI] [PubMed] [Google Scholar]
- Drummond, E.D. Socioeconomic inequalities in access to medication and adherence to pharmacotherapy in Brazil. Thesis in Public Health: epidemiology. Saúde Coletiva do Instituto René Rachou. Belo Horizonte, 2020.
- Eisen A., Giugliano R.P., Braunwald E. Updates on Acute Coronary Syndrome. A Review. Jama Cardiol. 2016;1(6):718–730. doi: 10.1001/jamacardio.2016.2049. [DOI] [PubMed] [Google Scholar]
- Ensenyat A., Tribo G.E., Silva L.M., Bergués X.S., Blanco A. Semisupervised Physical Exercise and Lifestyle Counseling in Cardiometabolic Risk Management in Sedentary Adults: Controlled Randomized Trial (BELLUGAT) J Phys Act Health. 2020;17(7):744–755. doi: 10.1123/jpah.2019-0409. [DOI] [PubMed] [Google Scholar]
- Goodwin A.M., Duran A.T., Kronish I.M., Moise N., Sanchez G.J., Garber C.E., Schwartz J.E., Diaz K.M. Factors associated with objectively measured exercise participation after hospitalization for acute coronary syndrome. Int. J. Cardiol. 2019;275:1–5. doi: 10.1016/j.ijcard.2018.09.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herdy A.H., López-Jiménez F., Terzic C., et al. Diretriz sul-americana de prevenção e reabilitação cardiovascular. Arq. Bras. Cardiol. 2014;103(2Supl1):1–31. doi: 10.5935/abc.2014s003. [DOI] [PubMed] [Google Scholar]
- Ho P.M., Lambert-Kerzner A., Carey E.P., Fahdi I.E., Bryson C.L., Melnyk S.D., Bosworth H.B., Radcliff T., Davis R., Mun H., Weaver J., Barnett C., Barón A., Del Giacco E.J. Multifaceted intervention to improve medication adherence and secondary prevention measures after acute coronary syndrome hospital discharge: a randomized clinical trial. JAMA Intern Med. 2014;174(2):186. doi: 10.1001/jamainternmed.2013.12944. [DOI] [PubMed] [Google Scholar]
- Malta M., Cardoso L.O., Bastos F.I., Magnanini M.M.F., Silva C.M.F.P. Iniciativa STROBE: subsídios para a comunicação de estudos observacionais. Rev Saúde Pública. 2010;44(3):559–565. doi: 10.1590/s0034-89102010000300021. [DOI] [PubMed] [Google Scholar]
- Malta D.C., Stopa S.R., Pereira C.A., Szwarcwald C.L., Oliveira M., Reis A.C. Cobertura de planos de saúde na população brasileira, segundo a Pesquisa Nacional de Saúde, 2013. Cien Saude Colet. 2017;22(1):179–190. doi: 10.1590/1413-81232017221.16782015. [DOI] [PubMed] [Google Scholar]
- Marasigan V., Perry I., Bennett K., Balanda K., Capewell S., Flaherty M.O., Kabir Z. Explaining the fall in Coronary Heart Disease mortality in the Republic of Ireland between 2000 and 2015-IMPACT modelling study. Int. J. Cardiol. 2020;310(1):159–161. doi: 10.1016/j.ijcard.2020.03.067. [DOI] [PubMed] [Google Scholar]
- Matsudo S., Araújo T., Matsudo V., et al. Questionário Internacional de Atividade Física (IPAQ): Estudo de validade e reprodutibilidade no Brasil. Rev Bras Ativid Fís & Saúde. 2001;6(2):5–12. doi: 10.12820/rbafs.v.6n2p5-18. [DOI] [Google Scholar]
- McDonagh Theresa A., Metra Marco, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. European Association of Preventive Cardiology (EAPC). 2021;42(36):3599–3726. doi: 10.1093/eurheartj/ehab368. Accessed June 17, 2022. [DOI] [PubMed] [Google Scholar]
- Mehran R., Baber U., Steg P.G., et al. Cessation of dual antiplatelet treatment and cardiac events after percutaneous coronary intervention (PARIS): 2 year results from a prospective observational study. The Lancet. 2013;382(9906):1714–1722. doi: 10.1016/S0140-6736(13)61720-1. [DOI] [PubMed] [Google Scholar]
- Mirkin K.A., Enomoto L.M., Caputo G.M., Hollenbeak C.S. Risk factors for 30-day readmission in patients with congestive heart failure. Heart Lung. 2017;46(5):357–362. doi: 10.1016/j.hrtlng.2017.06.005. [DOI] [PubMed] [Google Scholar]
- Nakayama A., Nagayama M., Morita H., Tajima M., Mahara K., Uemura Y., Tomoike H., Komuro I., Isobe M. A large-scale cohort study of long-term cardiac rehabilitation: A prospective cross-sectional study. Int. J. Cardiol. 2020;309:1–7. doi: 10.1016/j.ijcard.2020.03.022. [DOI] [PubMed] [Google Scholar]
- Nicolau, J.C., Feitosa-Filho, G.S., Petriz, J.L., et al. Diretrizes da Sociedade Brasileira de Cardiologia sobre angina instável e infarto agudo do miocárdio sem supradesnível do segmento ST - 2021. Arq Bras Cardiol. 2021;[online].ahead print,PP.0-0. 10.36660/abc.20210180. [DOI] [PMC free article] [PubMed]
- Nicolau J.C., Feitosa-Filho G., Petriz J.L., Furtado R.H.M., Précoma D.B., Lemke W., et al. Brazilian Society of Cardiology Guidelines on Unstable Angina and Acute Myocardial Infarction without STSegment Elevation – 2021. Arq Bras Cardiol. 2021;117(1):181–264. doi: 10.36660/abc.20210180. Accessed June 17, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveira L.M.S.M., Costa I.M.N.B.C., Silva D.G., et al. Reinternação de Pacientes com Síndrome Coronariana Aguda e seus Determinantes. Arq. Bras. Cardiol. 2019;113(1):42–49. doi: 10.5935/abc.20190104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveira J.C., Oliveira L.C.S., Oliveira J.C., et al. Disparidades no Uso de Stents Farmacológicos para Pacientes Diabéticos com Infarto Agudo do Miocárdio com Supradesnivelamento do Segmento ST Assistidos na Rede Pública versus Privada - Registro VICTIM. Arq. Bras. Cardiol. 2019;112(5):564–570. doi: 10.5935/abc.20190054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piegas L.S., Timerman A., Feitosa G.S., et al. Diretriz da Sociedade Brasileira de Cardiologia sobre tratamento do infarto agudo do miocárdio com supradesnível do segmento ST. Arq Bras Cardiol. 2015;105(2):1–121. doi: 10.5935/abc.20150107. Accessed June 10, 2017. [DOI] [PubMed] [Google Scholar]
- Piepoli M.F., Hoes A.W., Agewall S. European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) Eur Heart J. 2016;37(29):2315–2381. doi: 10.1093/eurheartj/ehw106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues P.A.F., Melo M.P., Assis M.R., Palma A. Socioeconomic conditions and practice of physical activity in adults and elderly: systematic review. Rev Bras Ativ Fís Saúde. 2017;22(3):217–232. [Google Scholar]
- Sakalaki M., Barywani S., Rosengren A., Bjorck L., Fu M. Determinants of suboptimal long-term secondary prevention of acute myocardial infarction: the structural interview method and physical examinations. BMC Cardiovasc. Disord. 2019;19(1):243. doi: 10.1186/s12872-019-1238-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smolderen K.G., Spertus J.A., Tang F., Oetgen W., Borden W.B., Ting H.H., Chan P.S. Treatment differences by health insurance among outpatients with coronary artery disease: insights from the national cardiovascular data registry. J. Am. Coll. Cardiol. 2013;61(10):1069–1075. doi: 10.1016/j.jacc.2012.11.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steca P., Monzani D., Greco A., et al. Stability and change of lifestyle profiles in cardiovascular patients after their first acute coronary event. PLoS One. 2017;12(8):e0183905. doi: 10.1371/journal.pone.0183905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steg G., James S.K., Atar D., et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 2012;33(20):2569–2619. doi: 10.1093/eurheartj/ehs215. [DOI] [PubMed] [Google Scholar]
- Stone N.J., Robinson J.G., Lichtenstein A.H., et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014;63(25PartB):2889–2934. doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- Teo K., Lear S., Islam S., et al. Prevalence of a healthy lifestyle among individuals with cardiovascular disease in high-, middle-and low-income countries: the Prospective Urban Rural Epidemiology (PURE) study. JAMA. 2013;309(15):1613. doi: 10.1001/jama.2013.3519. [DOI] [PubMed] [Google Scholar]
- Ulrich R., Pischon T., Robra B.P., Freier C., Heintze C., Herrmann W.J. Health care utilisation and medication one year after myocardial infarction in germany – a claims data analysis. Int. J. Cardiol. 2020;300:20–26. doi: 10.1016/j.ijcard.2019.07.050. [DOI] [PubMed] [Google Scholar]
- Vallabhajosyula S., Dunlay S.M., Barsness G.W., Rihal C.S., Holmes-Junior D.R., Prasad A. Hospital-level disparities in the outcomes of acute myocardial infarction with cardiogenic shock. The Am. J. Cardiol. 2019;124(4):491–498. doi: 10.1016/j.amjcard.2019.05.038. [DOI] [PubMed] [Google Scholar]
- Wita K., Wilkosz K., Wita M., Kułach A., Wybraniec M.T., Polak M., Matla M., Maciejewski Ł., Fluder J., Kalańska-Łukasik B., Skowerski T., Gomułka S., Turski M., Szydło K. Managed care after acute myocardial infarction (MC-AMI) – a poland’s nationwide program of comprehensive post-mi care - improves prognosis in 12-month follow-up. Preliminary experience from a single high-volume center. Int. J. Cardiol. 2019;296:8–14. doi: 10.1016/j.ijcard.2019.06.040. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Global Status Report on Noncommunicable Diseases “Attaining the Nine Global Noncommunicable Diseases Targets; A Shared Responsibility.” Geneva, Switzerland: World Health Organization; 2014. https://www.who.int/publications/i/item/9789241564854. Accessed November 19, 2017.
- Yun M., Li S., Sun D., Ge S., Lai C.-C., Fernandez C., Chen W., Srinivasan S.R., Berenson G.S. Tobacco smoking strengthens the association of elevated blood pressure with arterial stiffness: the Bogalusa Heart Study. J. Hypertens. 2015;33(2):266–274. doi: 10.1097/HJH.0000000000000410. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors are unable or have chosen not to specify which data has been used.