Abstract
The extracellular matrix (ECM) is a significant factor in cancer progression. Collagens, as the main component of the ECM, are greatly remodeled alongside cancer development. More and more studies have confirmed that collagens changed from a barrier to providing assistance in cancer development. In this course, collagens cause remodeling alongside cancer progression, which in turn, promotes cancer development. The interaction between collagens and tumor cells is complex with biochemical and mechanical signals intervention through activating diverse signal pathways. As the mechanism gradually clears, it becomes a new target to find opportunities to diagnose and treat cancer. In this review, we investigated the process of collagen remodeling in cancer progression and discussed the interaction between collagens and cancer cells. Several typical effects associated with collagens were highlighted in the review, such as fibrillation in precancerous lesions, enhancing ECM stiffness, promoting angiogenesis, and guiding invasion. Then, the values of cancer diagnosis and prognosis were focused on. It is worth noting that several generated fragments in serum were reported to be able to be biomarkers for cancer diagnosis and prognosis, which is beneficial for clinic detection. At a glance, a variety of reported biomarkers were summarized. Many collagen-associated targets and drugs have been reported for cancer treatment in recent years. The new targets and related drugs were discussed in the review. The mass data were collected and classified by mechanism. Overall, the interaction of collagens and tumor cells is complicated, in which the mechanisms are not completely clear. A lot of collagen-associated biomarkers are excavated for cancer diagnosis. However, new therapeutic targets and related drugs are almost in clinical trials, with merely a few in clinical applications. So, more efforts are needed in collagens-associated studies and drug development for cancer research and treatment.
Keywords: cancer, the extracellular matrix (ECM), collagen remodeling, interaction, mechanism, diagnosis, biomarker, therapeutic target, treatment
1. Introduction
Cancer is a serious disease for humans with high morbidity and death. The extracellular matrix (ECM) is a non-ignored factor in cancer progression due to the fact that it is the major component of tumor stroma, playing the roles of the physical scaffold and regulator of cell and tissue function. ECM could not only act as a medium to conduct signals but also elicits biochemical and biophysical signaling to excite cells [1,2]. The interaction between tumor cells and ECM is bidirectional and dynamical, which could reshape the morphology of perimalignant tissue continuously. Recent studies have shown that tumors could directly leverage ECM remodeling to create a microenvironment that promotes tumorigenesis and metastasis. Conversely, many cell behaviors are inspired by transformed ECM, such as adhesion, migration, angiogenesis, and canceration [3,4].
In the complex interaction between ECM and tumor cells, collagens play a significant role involved in multiple actions. Collagens are the major component in ECM, which constitute up to 30%—28 different collagens have been identified. Multiple subtype collagens participate in the construction of both matrices of ECM, i.e., base-membrane and interstitial matrix, and create special ECM compositions in different tissues [5,6]. Recently, many studies reported the abnormal appearance in the cancer progression, including degradation, remodeling, fragmentation settlement, linearization, and fasciculation. It is confirmed that collagens are relevant to the precancerous lesion and cancer progression. Based on the mechanisms of collagens involved in the multiple stages of cancer progression, the value of diagnosis and prognosis is developed. Moreover, it provides opportunities to identify new therapeutic targets for cancer treatment. This review investigated the complex response of collagens in cancer progression and summarized the interaction between collagens and cancer cells. Then, we focused on the diagnosis value of collagen-associated imaging and biomarkers. Finally, we discussed the therapeutic opportunities of targeting collagens for cancer treatment.
2. Collagen Is a Significant Concern for Cancer Research Associated with the ECM
2.1. Collagens Are the Major Component of ECM
Collagens are a superfamily comprising 28 members characterized by collagen α chains [6,7]. According to the supramolecular organization, collagens are divided into fibrillar collagens and non-fibrillar collagens. Fibrillar collagens occupy 90% of the totality, including types I, II, III, V, XI, XXIV, and XXVII. They show elongated, rod, or banded fibril structures under electron microscopy. In comparison, others are non-fibrillar collagens, which form other types of supramolecular structures. Non-fibrillar collagens are further subdivided into fibril-associated collagens with interrupted triple helices (types of IX, XII, XIV, XVI, XIX, XX, XXI, and XXII), network-forming collagens (types IV, VI, VIII, and X), beaded filament-forming collagens (types VI, XXVI, and XXVIII), anchoring fibrils (type VII) and transmembrane collagens (types XIII, XVII, XXIII, and XXV). Collagens participate in the formation of both forms of ECM, i.e., the base-membrane and interstitial matrix. Fibrillar collagens have a clear structural role of mechanical support and dimensional stability, which could provide three-dimensional frameworks for tissue and organs. As an example, type I collagen, as fibrillar collagen, is the main protein in skin, contributing to the tensile strength of skin [6,8]. Non-fibrillar collagens are also essential to maintain tissue structure; for instance, the type IV collagen network is the main scaffold structure of the base membrane. In addition, non-fibrillar collagens are the key regulators to anchor and organize the ECM meshwork. It has been reported that an anchoring bridge is created between the base membrane and the interstitial matrix by the regulation of type VI collagen [9].
2.2. The Observation Methods of Collagens in Research and Clinic
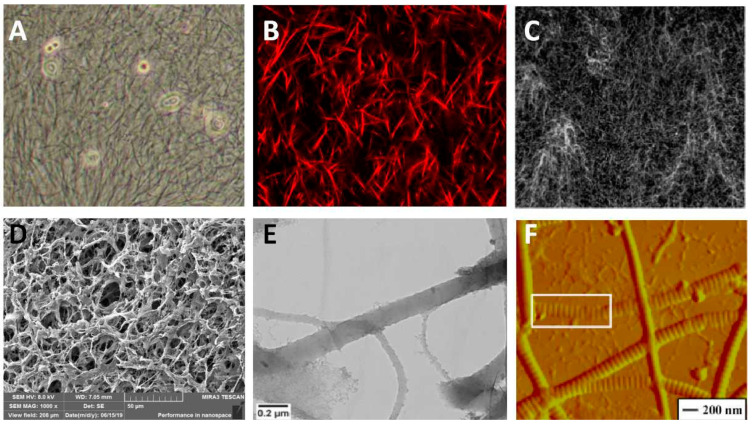
The paramorphia of collagens is a significant signal of many diseases, especially fibrosis and precancerosis. Several imaging modalities were developed for quantitative or qualitative analysis collagens. The coarse collagen fiber could be observed directly under the light field of optical microscopy, the visual scenes of which are shown in Figure 1A. However, the tiny collagen fibrils or soft networks are hard to be identified under optical microscopy. Pathological staining technology offers the assistance to catch high-recognition images under light fields, especially for clinicopathological sections. Of note, immunohistochemistry (IHC) could recognize the types of collagens with the assistance of optical microscopy. Fluorescence immunostaining is a method to mark the collagens with a fluorescence dye, then the marked collagens are highlighted under the excitation light of a fluorescence microscope from the background. This method is suitable for all subtypes of collagens, whether fibrous or not; however, this method is hard to apply in practical applications due to the fact that the fluorescence dye is hard to wash completely from the dense networks, causing significant interference to collagen identification. Collagen fiber is a non-centrosymmetry and high second-order nonlinear coefficient structure that could produce the signal of second-harmonic generation (SHG) under two-photon excitation. This provides an excellent opportunity to image collagens, and SHG imaging has been promoted to be a popular and effective approach to investigate collagens in the laboratory. As an example, SHG imaging is developed to investigate collagen fiber organization, which has a high resolution capable of recognizing faint signals [10]. In fact, SHG imaging of collagens is always used combining with confocal microscopy, which could catch the interior signals of the samples to reconstruct 3D images [11,12]. We took an SHG image of type I collagen fibers in an in vitro experiment using confocal microscopy shown in Figure 1B. Due to the fibrous structure differs from other matrices, the pure reflective mode of the confocal microscope is available to take the fiber signal, although the clarity is worse in contrast to SHG imaging [13,14,15]. Figure 1C exhibited the collagen network structure in an in vitro experiment using the reflective mode of the confocal microscope. Electron microscopy is an instrument manufactured by the principle of electron photons, which replaces light beams and optical lenses with electron beams and electron lenses to take the subtle structure imaged with a very high magnification. Fortunately, collagen fibers could be imaged by the two commonly types of electron microscopy, i.e., scanning electron microscopy (SEM) and transmission electron microscopy (TEM) [16,17,18]. SEM could see the morphology of collagens limited to surface and longitudinal. We took the porous structure by SEM, shown in Figure 1D. TEM could evaluate the cross sections through 3D imaging. Figure 1E is the structure of collagen type I under TEM. Cryo-TEM advanced the TEM technique allowing the sample examined to maintain the frozen-hydrated state and removing the step of heavy-metal staining. The early banding analysis of reconstituted collagen fibrils was performed from cryo-TEM images [19,20,21]. Atomic force microscopy (AFM) is another morphology detection instrument based on a completely different principle, i.e., van der Waals force. AFM could be used to confirm the inner assembly of collagen fibrils. As an example, Figure 1F exhibited the microstructure of a single collagen fibril in a high magnification AFM image. However, AFM could only scan the 3D topographic feature, but not the section structure inside the matrix [22,23,24].
Figure 1.
Several examples of collagen detecting methods. (A) light field of optical microscopy. (B) SHG imaging. (C) The reflection mode of confocal microscopy. Reprinted/adapted with permission from Ref. [3]. (D) SEM imaging. (E) TEM imaging. Reprinted/adapted with permission from Ref. [6]. (F) AFM imaging. Reprinted/adapted with permission from Ref. [12].
Clinically, medical imaging technology is an important contribution to disease diagnosis and surgical guidance, which is popular due to its non-invasive, including ultrasound, X-ray, computed tomography (CT), and nuclear magnetic resonance imaging (MRI). The medical imaging technology allows the sample to be examined in a close to physiological hydration state without chemical fixation of sectioning. Diffraction pattern signals are inspired by high-intensity X-rays scattering from the arranged collagen molecules and fibrils in the bulk matrix. So, X-ray is available to analysis the average diameter, lateral arrangement, and alignment of collagen fibrils; as an example, corneal ultrastructure is obtained by X-ray with a powerful synchrotron source [25,26]. CT and MRI are able to analyze the collagen fibers quantitatively. Karjalainen et al. used micro-computed tomography to analyze the three-dimensional collagen orientation of the human meniscus posterior horn in health and osteoarthritis [27]. Eder et al. used MRI to evaluate the regional collagen fiber network in the human temporomandibular joint disc [28]. Ultrasound is developed to assess collagen microstructure based on the integrated backscatter coefficient (IBC). Mercado, Karla P. et al. employed IBC as a quantitative ultrasound parameter to detect the quantify spatial variations of collagen fiber density and diameter [29]. Kenton et al. prospectively characterize the collagen organization in the Achilles and patellar tendon [30]. However, IHC still plays an irreplaceable role in the clinic due to its ability to recognize the types of collagens. Pathological detection based on IHC is the gold standard for tumor diagnosis in the clinic.
3. Collagen Remodeling Is a Significant Signal in Cancer Progression
3.1. Precancerous Lesions
Stromal alterations are the reference precursors to predict the progression of carcinoma, especially collagens, which is the main component of the ECM. The occurrence of fibrosis and the base membrane abnormality, which are mainly involved by collagens, are the important cues orienting to deterioration, having a significant clinical meaning. In precancerous lesions, it is likely to occur due to the abnormal ratio of collagen types, new collagen types secreted, and abnormal molecular structure, causing the abnormal ECM.
The fibrosis of organ tissue is an important cue to draw attention to, which is likely to be a stage of deterioration, such as liver fibrosis, lung fibrosis, oral submucosa fibrosis, and so on. Most hepatocellular carcinoma develops through the progression of chronic liver injury, hepatic inflammation, and fibrosis, so liver fibrosis is a precursor of cancerization. It has been confirmed that high fibrosis index is positively correlated with the risk of hepatocellular carcinoma [31,32]. The configuration of collagen types is changed greatly in the progression of fibrillation. In normal liver, the collagens in ECM are type IV and VI, which are non-fibrillar; however, a great accumulation of fibrillar collagens occurs in the fibrotic liver, such as collagen type I and III [33]. Similarly, idiopathic pulmonary fibrosis is considered to have a high risk of concomitant lung cancer in the clinic. What is worse, patients with idiopathic pulmonary fibrosis have a poor prognosis with a 2–5 year survival time, which is worse than liver fibrosis [34]. Enhancing nodules in post-radiation fibrosis in CT imaging could be an early detecting method of recurrent lung cancer [35]. The deposition of collagens in the interstitium is the direct reason for fibrosis. In early pulmonary fibrosis, collagen type III predominates in the matrix; however, the proportion is gradually replaced by collagen type I along the process of pulmonary fibrosis to the late stage [36]. Oral submucous fibrosis is a precancerous disorder and has a 1.5–15% chance of transforming into a malignant tumor. The characteristics of oral submucous fibrosis are abnormal collagen deposition. In oral submucous fibrosis cells, the collagen synthesis is increased and the ratio of the α1(I) to α2(I) chains of type I collagen is ~3:1 whereas ~2:1 in normal cells [37,38].
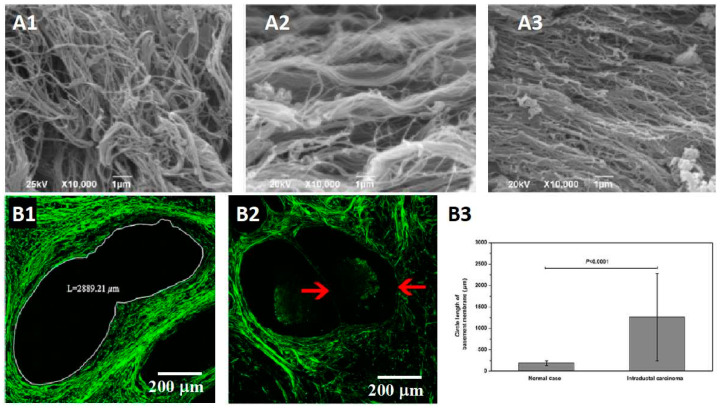
The analysis of collagen fibers is significant in predicting cancer. Despotovic et al. caught the SEM images of the perimalignant tissue shown in Figure 2A. They found that the altered organization of collagen fibers was observed at 10 cm and 20 cm away from the malignant tumor. The alignment of collagen fibers is step increased as proximity to the tumor [39]. Wu et al. focused on the base membrane in intraductal carcinoma, a precancerous lesion of invasive ductal carcinoma. They found that the base membrane was distorted and elongated compared with the normal cases (Figure 2B). Several types of gynecological cancers are reported differently in terms of precancerous lesions, such as breast cancer, ovarian cancer, and vulvar cancer. Castor et al. characterized the collagen fibers in preneoplastic lesions compared with normal tissue and squamous carcinoma in vulvar cancer using SHG microscopy. They found that the collagen fibers showed better organization in the normal tissue than in the other two stages. The devise parameters of collagen fibers showed reducing in squamous carcinoma and preneoplastic lesions compared with normal tissue, i.e., quantity, organization, and uniformity; however, no obvious difference was observed between squamous carcinoma and preneoplastic lesions [40]. In cervical precancers, several collagen-associated indicators directly affect the quantitative classification of precancerous stages, including the density and degree of linear arrangement, collagen degradation, and the breakage of collagen cross-links. Zaffar et al. focused on this valuable information by developing a series of studies of the spatial frequencies of collagens for cervical precancer detection [41,42]. The expression of collage IV seriously affects the integrity of the base membrane because collagen IV is the main complement of the base membrane. As a precancerous lesion of squamous cell carcinoma in malignant skin tumors, actinic keratosis has shown the premonition of collagen IV low expression. Hirakawa et al. compared the expression of collagen IV using immunohistochemical in actinic keratosis tissue. The result showed that collagen IV in dysplastic areas of actinic keratosis samples was lower than peri-lesional tissue and no longer continuous [43].
Figure 2.
Collagen remodeling in precancerous lesions is a signal of cancerization. (A1–A3) The SEM images of collagen fibers in the health tissue and 10 cm and 20 cm away from the malignant tumor [39] (A1) The collagen fibers in the health tissue are thin collagen fibers forming a dense network. (A2) The collagen fibers at 20 cm away from the tumor, thick and aligned. (A3) The collagen fibers at 10 cm away from the tumor, highly aligned. (B1–B3) The difference of base membrane in intraductal carcinoma, a precancerous lesion of invasive ductal carcinoma [44] (B1) The base membrane shows a distorted structure with a larger size. (B2) The base membrane is destroyed in the evolution from intraductal carcinoma to invasive ductal carcinoma. (B3) The statistics data of the circle length of base membrane. The circle length is elongated observably in precancerous lesions compared with normal cases.
3.2. Post-Cancerous
3.2.1. Breaching Base Membrane
In the development of cancer progression, collagens become from a passive barrier resisting cancer cells to an accomplice in promoting the progression. The base membrane is a baffle between tumor cells and normal tissue originally; however, it would be breached at the early stage of carcinogenesis. The main reason is collagen IV, which occupies the major complement of the base membrane, is degraded directly or indirectly by tumor cells. In the degrading progress, matrix metalloproteinase plays an indispensable role, which is secreted by tumor cells or stimulated epithelial or stromal cells. In the subsequent progression of cancer development, degrading collagens remains an effective strategy to create roads to invasion or migration. Yan et al. reported a period that collagens exhibited a significant loss in invasive ductal carcinoma compared to the normal case and precursor lesion [44]. Recently, another cue is revealed that cancer cells could break the base membrane just facilitated by physical forces, which is a completely different manner independent of protease. As evidence, the collagen IV meshwork exhibits a densified structure at the adjacent disruption; on the contrary, the collagen IV scaffold should be decreased under the degradation theory. Piercing filopodia is captured in further studies, which is proved to have a pivotal role in the mechanical response model. The force of push and pull by the contractility of piercing filopodia is considered an explanation of the base membrane non-protease disruption [45,46,47].
3.2.2. Enhancing ECM Stiffness
Enhancing the stiffness of ECM is another strategy to promote tumor cell migration and invasion through the pathway of activating integrins to increase the adhesion between cells and substrate. Castor et al. found that the parameters of collagen fibers present higher in metastatic vulvar cancer patients than in that without metastases [40]. High ECM stiffness is mainly realized by increasing the secretion of fibrous collagens and the deposition of non-fibrous collagens, most notably collagen type I and type IV [48,49]. In medical statistics, ECM stiffness is considered a reason for tumor rise incidence with aging because it is a fact that the aged tissues are stiffer due to containing more aberrant cross-linked collagens [50]. High collagen density in tumors is often closely correlated with poor prognosis; however, the association between collagen density and cancer progression is not completely clear. Recent reports studied it from various perspectives. The most accepted view is that ECM stiffness is closely related to cancer-associated fibroblasts (CAFs) [51,52,53,54]. This viewpoint is supported because CAFs are the main producer of abnormal collagen fibers. Shibata et al. reported that CAFs promote ECM stiffness in response to the signals from yes-associated protein 1 (YAP1) [55]. However, Farhat et al. found that abnormal activation and expression of the Lox family of proteins, a group of extracellular enzymes catalyzing the cross-linking of collagens, would lead to the ECM toward increased rigidity and fibrosis [56].
3.2.3. Orienting the Collagen Fibers
Orienting the collagen fibers is a significant manner of remodeling the ECM by cancer cells. The stress of tumor growth remodels the collagen fibers toward the tumor circumference at the tumor periphery. Those oriented collagen fibers provide a highway to cancer cell invasion directly [57,58,59,60]. Meanwhile, the tension of aligned collagen fiber bunches contributes to ECM stiffness [61]. Many studies reported the high orientation of collagen fibers in the tumor location [13,57,59,62]. The mechanism of collagen fibers orientation in the malignant tumor is still unclear. Many scientists dedicated themselves to this study, and they revealed it is a complex process, maybe participated in by tumor cells, CAFs, mesenchymal cells, and interstitial fluid. Tumor cells remodel the collagen fibers through various manners, including the stress of tumor growth, the pseudopod with contractility, the protease, and so on, which is a complex process with multiple pathways [61,63,64,65,66,67]. The examples are shown below. Ray et al. reported that the traction forces from the directed migration of cancer cell clusters are a mechanism of collagen fiber alignment [68]. Drifka et al., using a pancreatic ductal adenocarcinoma model, found that human pancreatic stellate cells could orchestrate the alignment of collagen fibers, and they further found that the aligned collagen fibers, in turn, enhanced cancer cell migration. Bayer et al. showed that the collagen receptor DDR2 in CAFs reorganizes collagen fibers at the tumor-stromal boundary [69]. Hanley et al. reported that CAFs could induce the formation of elongated collagen fibers [70]. Del Amo et al. constructed a collagen-based osteoblasts model in 3D microfluidic devices, and the data suggested that a high rate of interstitial fluid flow could modify the orientation of collagen fibers [71].
4. Remodeled Collagens Assist Cancer Progression
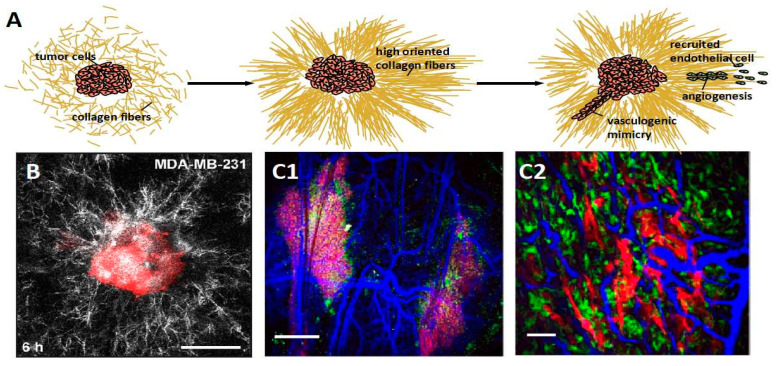
4.1. Promoting Angiogenesis
In cancer progression, limited oxygen and nutrients are always insufficient for the rapid growth of cancer cells. Angiogenesis is induced under a poor supply of oxygen and nutrient. The angiogenesis process is always accompanied by the upregulation of collagens and ECM-modifying enzymes, which has been confirmed in different human tumor types. That is because the collagen network provides the scaffold for recruited endothelial cells migrating during angiogenesis. Even the remote collagen fiber network is induced by tumor cells into orientation steers for angiogenesis. We illustrated the process of angiogenesis induced by collagen fibers in Figure 3A. Piotrowski-Daspit et al. took a confocal image of a representative tissue comprised of breast cancer cell MDA-MB-231. They found that the collagen fibers showed high alignment obviously (Figure 3B). The collagen network provides the intact physical connection with tumor tissue for vascular endothelial cells’ mechanical sensing, which is considered essential during angiogenesis [72]. Nathaniel et al. observed the fibril organization around angiogenic sprouts and growing neo-vessels in real time. They found that a strong association of fibrillar collagens occurred during vessel reconstitution and a substantial collagen fibril reorganization at the sites of sprout and neo-vessel tips [73]. Luthria et al. investigated the vasculature around the tumor in the dense collagen micro-environment—shown in Figure 3C [74]. Niels et al. reported that type VIII collagen was elevated in diseases associated with angiogenesis and vascular remodeling, such as pulmonary fibrosis and cancer [75].
Figure 3.
Tumor cells organize the disordered collagen fibers into orientation, further providing a scaffold to recruit endothelial cells (green cell in illustration) for angiogenesis or inducing vasculogenic mimicry constituted by tumor cells (red cell in illustration) without endothelial cells presenting. (A) The cartoon diagram displays the process of angiogenesis. (B) A confocal image of a representative tissue comprised of breast cancer cell MDA-MB-231. The collagen fibers around the tissue are aligned, obviously. Reprinted/adapted with permission from Ref. [76]. (C1,C2) The SHG images show the vasculature (blue) formed neighbor tumor within the micro-environment of high dense collagen matrix. Reprinted/adapted with permission from Ref. [74].
Another vasculature-like structure could also support tumors with blood, which is called vasculogenic mimicry constructed by cancer cells without endothelial cells. The primary trigger is dense collagen, inducing cancer cells to form interconnected networks [4]. Velez et al. found that the collagen matrixes with small pores and short fibers induced vasculogenic mimicry. The upregulation of β1-integrin is triggered by the collagen matrix architecture and is considered a significant reason in the follow-up research [77]. The non-fibril collagens contribute to vasculogenic mimicry, such as collagen type IV, VI, and XVI. Bedal et al. found the NC11 domain of human collagen XVI, one non-fibril collagen, induced vasculogenic mimicry in oral squamous cell carcinoma cells. The process is realized by triggering the generation of tubular-like net structures on a laminin-rich matrix [78].
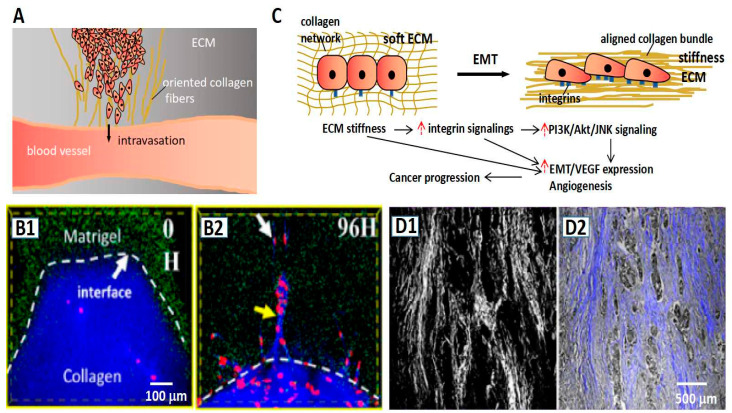
4.2. Promoting Invasion
Escaping from the primary site is another strategy employed by cancer cells to obtain supplies; collagens also play a significant role in this process. Collagen fibers induce cancer cell migration by contact guidance [68]. Especially, the aligned collagen fibers are confirmed to provide “a highway” to cancer cell invasion [79,80,81]. The guidance of collagen fibers runs through the major process of cancer progression. In the early stage, the collagen fibers that are perpendicular to the solid tumor provide conduits to escape and penetrate the base membrane [58,82]. In the following process, the interface between the collagen fiber bundle in ECM and the peripheral interstitial components provides the opportunity for breakthrough for tumor cells. We illustrated the intravasation guided by collagen fibers in Figure 4A. The role of the “highway” has been verified by several reports. In an experiment on the orientation of collagen fibers, cancer cells could break through the high density of Matrigel along with the collagen fibers, while they were unable to do that in the absence of oriented collagen fibers—shown in Figure 4B [59]. In the process of intravasation (cancer cell entering blood vessel) and extravasation (cancer cell exuding blood vessel), collagen fibers as important participators are remodeled firstly and, in turn, guide the cancer cell invasion [83,84,85,86]. Moreover, the orientation and the deposition of collagens make the matrix stiff. The stiffness of the ECM could induce the enhancement of transforming growth factor-β (TGF-β) to increase the cell adhesion to the substrate, further promoting the migration and invasion of tumor cells. Masoud et al. reported that ECM stiffness could make a bridge in the base membrane through the related pathway of transforming growth factor-β (TGF-β), which contributed to EMT [87]. Figure 4C illustrates the process of EMT induced by the high stiffness ECM. Han et al. displayed a merged image of the SHG signal and light field of the pathological section (Figure 4D). They found that the tumor cells invaded along with the direction of fibers [59]; however, the mechanism of the stiffness ECM acting on tumor cells is complex; there are other pathways being investigated as well. For instance, Anne et al. investigated the immune modulatory properties of collagens in cancer, and they revealed that collagens could affect the function and phenotype of various types of tumor-infiltrating immune cells, such as tumor-associated macrophages and T cells [88]. Yu et al., from the perspective of drug transport, revealed that ECM stiffness was a barrier to drug screening at the tumor site [89].
Figure 4.
Collagens promote cancer invasion. (A) The schematic representation of oriented collagen fibers providing a “highway” to guide cancer cells in realizing the intravasation process. (B1,B2) The fluorescent images show the stiffness Matrigel (green) region is invaded by cancer cells (red) in the guidance of the oriented collagen fibers (blue) [59]. (C) The schematic representation of stiffness ECM inducing EMT accompanied with high adhesion of tumor cells. (D1,D2) Tumor cells (gray color in (D2)) invade along with the direction of collagen fibers. (D1) The SHG signal of collagen fibers in the pathological section. (D2) The merge of the light field and SHG signal of the pathological section [59].
Non-fibril collagens also participate in the invasion process. Fang et al. reported that collagen type IV occurred a series of changes to provide a proper tumor microenvironment for cancer invasion. In the initial stage, collagen IV presents an irregular sheath in the base membrane, and then it is degraded and accompanied by linear redeposition to form invasion fronts, which would become the escape sites of cancer cells [90]. Zhang et al. reported that collagen XIII could promote invasive tumor growth, enhance the stemness of cancer cells, and induce anoikis resistance [91]. Karagiannis et al. investigated collagen type XII by immunohistochemistry and found that collagen XII was highly expressed in the invasion front of cancer cells [92]. Kumagai et al. found that the intercellular expression of type XVII collagen could promote collective invasion by producing intercellular adhesion sites for contact following [93]. Miyake et al. reported that collagen IV and collagen XIII played a pivotal role in tumor invasion by inducing tumor budding [94].
5. Collagens Provide Opportunities to Cancer Diagnosis and Prognosis
5.1. Collagen-Associated Biomarkers for Cancer Diagnosis
Collagens, as the main component of the ECM, would be abnormally expressed or deposited in the location or the pericarcinoma of the cancer site. It is for this reason that collagens are proposed as a diagnostic biomarker in cancer types. Type I collagen is reported to be a good diagnostic marker to detect the metastasis of lung cancer, the expression level of which is a significant indicator of distinct bone involvement happening or not in lung cancer metastasis [95]. The degradation products of type I collagen in serum are a significant reference for diagnosis and prognosis. Nurmenniemi et al. reported that type III collagen N-terminal telopeptide and type I collagen C-terminal telopeptide in serum, which are the degradation products of type I and III collagen, respectively, could be used as a prognostic marker in head and neck squamous cell carcinoma because they are proved closely associated with patient survival [96]. Another report revealed that the levels of matrix metalloproteinase (MMP) generated fragments of type I collagen in serum are valuable as a diagnostic biomarker for lung cancer [97]. The variety of collagens is valuable as a biomarker in the diagnosis of numerous cancers, and we collected and summarized them—we present this in Table 1. Of note, many generated fragments of collagens in serum are available for cancer diagnosis, which provides a convenient detection method through drawing peripheral blood.
Table 1.
The collagen-associated biomarkers and the applicating cancer types in cancer diagnostic.
| Collagen Type | Biomarker | Cancer Type | Reference |
|---|---|---|---|
| Type I | the expression level of collagen I | bone metastases of lung cancer; bladder cancer; colorectal cancer |
[95,98,99] |
| the carboxyl terminal peptide beta-special sequence, total type I procollagen amino terminal propeptide, alkaline phosphatase of collagen I in serum | bone metastases of lung cancer | [100] | |
| type I collagen C-terminal telopeptide in serum | head and neck squamous cell carcinoma | [96] | |
| MMP-generated fragments of type I collagen in serum | lung cancer; breast cancer |
[97,101] | |
| the expression level of collagen type I alpha 1 | hepatocellular carcinogenesis and metastasis | [102] | |
| the carboxyterminal collagen type I telopeptid | breast cancer with bone metastases | [103] | |
| the expression level of collagen type I alpha 2 | gastric cancer | [104] | |
| Type III | MMP-generated type III collagen fragment, procollagen type III N-peptide in serum | breast cancer | [101,105] |
| the propeptide of type III collagen in serum | pancreatic cancer | [106] | |
| the level of procollagen III aminoterminal propeptide | malignant head and neck cancer; cervical carcinoma |
[107,108] | |
| procollagen type III N-peptide in serum | gastric cancer; ovarian cancer; lung cancer |
[109,110,111] | |
| type III collagen in serum | hepatocellular carcinoma | [112] | |
| type III collagen in cancer tissue | malignant pleural mesothelioma | [113] | |
| the expression of collagen III and collagen III mRNA | Ewing’s sarcoma | [114] | |
| Type IV | the type IV collagen, MMP-generated type IV collagen fragment in serum in serum | breast cancer | [101,105] |
| 7S domain of type IV collagen in serum | gastric cancer; pancreatic cancer; lung cancer; extrahepatic cancer; hepatocellular carcinoma |
[111,115,116,117,118] | |
| the expression level of collagen IV | malignancy glioma | [119] | |
| the differential localization of the type IV collagen alpha5/alpha6 chains | colorectal epithelial tumors | [120] | |
| MMP-degradation of type IV collagen | ovarian cancer | [121] | |
| the expression level of collagen IV | prostate cancer | [122] | |
| the expression of collagen type IV |
urothelial carcinoma; oral squamous cell carcinoma |
[123,124] | |
| the expression of the type IV collagen alpha1 and alpha2 chains | hepatocarcinogenesis | [125] | |
| the expression of the type IV collagen alpha1 | bladder cancer | [126] | |
| the expression of collagen IV in tumor location | invasive adenocarcinoma | [127] | |
| serum N-terminal pro-peptide of type IV collagen 7S domain | hepatocellular carcinoma in patients with liver cirrhosis | [128] | |
| Type V | the expression level of collagen type V alpha 2 |
colorectal cancer; gastric cancer; |
[129,130] |
| the expression level of collagen type V | breast cancer; lung cancer |
[131,132] | |
| Type VI | MMP-generated type III collagen fragment | breast cancer; colon cancer; gastric cancer; malignant melanoma; lung cancer; ovarian cancer; pancreas cancer; prostate cancer | [133] |
| serum collagen type VI alpha 3 | pancreatic ductal adenocarcinoma | [134] | |
| stromal collagen type VI | salivary gland cancer | [135] | |
| the expression of COL6 | pancreatic cancer | [136] | |
| collagen type VI alpha 1chain | esophageal squamous cell carcinoma | [137] | |
| Type VII | the expression level of type VII collagen | identifying lung cancer subtypes; skin cancer; gastric cancer |
[138,139,140] |
| the expression level of collagen type VII a 1 chain | clear cell renal cell carcinoma | [141] | |
| Type VIII | the NC1 domain of human type VIII collagen a1 chain in serum | colorectal cancer | [142] |
| collagen type VIII alpha 1 chain |
breast cancer; colon Adenocarcinoma |
[143,144] | |
| Type XI | the expression level of Collagen Type XI Alpha 1 Chain | colorectal cancer; breast carcinoma invasiveness; colon cancer; gastric cancer; pancreatic ductal adenocarcinoma; pancreatic adenocarcinoma; pancreatic cancer |
[145,146,147,148,149,150,151] |
| the expression of procollagen XI Alpha 1 Chain | breast cancer | [152] | |
| type XIII | the expression of the type XIII collagen alpha1 | bladder cancer | [126] |
| Type XIV | the expression of type XIV collagen | breast cancer | [153] |
| Type XV | fragments of collagen XV collagen alpha1 in urine | gastrointestinal cancer | [154] |
| Type XVIII | the expression of type XVIII collagen | pancreatic ductal adenocarcinoma | [155] |
| serum endostatin (a fragment of collagen XVIII) levels | colorectal cancer | [156] | |
| Type XXIII | the expression of collagen type XXIII alpha 1 chain | clear cell renal cell carcinoma | [157] |
5.2. The Predictive Value of Collagens
Collagens have high value in monitoring cancer processes, prognosis, and recurrence. The predictive value is exhibited in many types of cancer, including breast cancer, prostate adenocarcinoma, lung cancer, hepatocellular carcinoma, colon cancer, and pancreatic cancer. In breast cancer, the qualitative descriptors of collagens at the boundaries between tumor and stroma are important indicators for tumor staging. In invasive breast cancer, the 5-year disease-free survival in patients with low tumor-stromal ratios is poorer than the patients with high tumor–stroma ratios. In lung cancer, high levels of collagen I in serum and tissue demonstrated a significant decrease in survival. Furthermore, collagen metabolic components and prolyl hydroxylases have been marked as the predictive factors of lung cancer presence, progression, and outcome. Abnormal collagen expression is associated with cancer overall survival (OS). The prognosis value is outstanding in enriched stromal cancers, such as pancreatic cancer and colon cancer. It is confirmed that the alignment of collagens was associated with the patient survival of pancreatic ductal adenocarcinoma (PDAC). Highly aligned collagen fibers report poor prognosis in PDAC, according to clinical statistics. Collagen types I, III, VI, and XI were shown to be associated with the diverse response of pancreatic cancers, such as proliferation, migration, decreasing E-cadherin expression, and cancer-associated fibroblasts [158]. Furthermore, the percent survival with a high level of collagen type I is observably lower than the low level. It was shown that the level of collagen type I had a negative correlation to OS for pancreatic cancer [159]. In colon cancer, the level of collagen expression is the key indicator to predicting the OS and risk, especially the types of COL1A1, COL1A2, COL3A1, COL4A3, and COL4A6. Please refer to reference [158] for more information on the predictive value of collagens.
6. Therapeutic Opportunities of Cancer Target to Collagens and the Collagen Associated Molecules
Collagen remodeling plays a significant role in cancer progression, as the content described above. It provides the possibility for therapeutic cancer targeting to collagens undergoing remodeling, including inhibiting the synthesis of collagens and interdicting the reactivator on the signal pathway. Of note, many small molecule inhibitors of collagen synthesis and functioning are available as anti-cancer drugs. They could accurately point to the target, avoiding damage to normal cells, which is an absolute advantage over conventional chemotherapeutic agents.
6.1. Inhibiting the Synthesis and Secretion of Collagens
Inhibiting collagen synthesis and secretion is a strategy for cancer therapeutics, which could prevent the series of effects initiated by collagen remodeling. For instance, as a catalyst in a key step of collagen biosynthesis, CP4H was linked with cancer metastasis in recent studies. Undoubtedly, CP4H has confirmed a new target for anti-cancer drugs. Several drugs targeted to CP4H have been developed as CP4H inhibitors, such as Ethyl 3,4-dihydroxybenzoate (EDHB) and 2-(5-carboxythiazol-2-yl) pyridine-5-carboxylic acid (pythiDC) [160]. Lysyl hydroxylation is a key step for collagen cross-link and deposition, which is a potential target to inhibit collagen synthesis. Aiming at the collagen remodeling induced by aberrant lysyl hydroxylation and collagen cross-link, lysyl hydroxylation is developed as a potential target for cancer therapeutic. Minoxidil, as an inhibitor of lysyl hydroxylation, is confirmed to have anti-invasive effects on human breast cancer [161]. Relatively, procollagen-lysine 2-oxoglutarate 5-dioxygenase (PLOD) drew much attention as the catalyzer of the process of lysyl hydroxylation. Increased PLOD expression has been detected in many types of cancer. Targeting PLODs is considered a potential strategy for cancer treatment; however, there are still no reports revealing the related anti-cancer drugs [162]. More available targets and the related drug aiming at collagen synthesis are summarized in Table 2.
Table 2.
A summary of drugs targeting the synthesis and secretion of collagens.
| Therapeutics Target | Drug | Mechanism | Cancer Type | Status | Reference |
|---|---|---|---|---|---|
| collagen type I | Baicalein | inhibiting collagen type I transcription by alleviating TGF-β1 stimulation | lung cancer, osteosarcoma cells, bladder cancer, breast cancer, pancreatic cancer, cervical cancer, oral cancer | a promising candidate awaiting further testing | [163,164,165] |
| Phenylbutyrate, sodium phenylbutyrate | as a weak histone deacetylase inhibitor decreasing collagen type I Alpha 1 mRNA transcription | lung cancer, prostate cancer, liver cancer, breast cancer, ovarian cancer, bladder cancer | a promising candidate awaiting further testing | [166,167,168,169,170,171] | |
| C9 | C9 inhibits collagen production by dissociating laribonucleoprotein domain family member 6 (LARP6) from type I collagen 50′SL RNA | - | awaiting further testing | [172] | |
| Ethyl 3,4-dihydroxybenzoate (EDHB), 2-(5-carboxythiazol-2-yl) pyridine-5-carboxylic acid (pythiDC) |
inhibiting collagen synthesis by inhibiting Prolyl 4-hydroxylases (P4Hs), which is a synthesis and regulatory factor of collagen type I | colorectal cancer, breast cancer | awaiting further testing | [160,173,174] | |
| Minoxidil | inhibiting collagen synthesis by inhibitor lysyl hydroxylases (LHs), which is a synthesis and regulatory factor of collagen type I | prostate cancer, breast cancer, ovarian cancer | a promising candidate awaiting further testing | [161,162,175,176] | |
| AK-778 | inhibiting collagen synthesis by mitigating the interaction between collagen and HSP47, which is a molecule required for collagen type I maturation. | - | a promising candidate awaiting further testing | [177,178] | |
| CCT365623 | decreasing collagen synthesis by inhibiting lysyl oxidase (LOX), which is a regulatory factor for collagen cross-linking | - | a promising candidate awaiting further testing | [179,180] | |
| collagen type XI | LY2157299 | inhibiting collagen XI alpha 1 chain (COL11A1) expression by inhibiting the transforming growth factor beta receptor 1 (TβRI) | ovarian cancer, pancreatic cancer, breast cancer | phase II clinical trial | [181,182,183,184,185] |
| SC66 | as an Akt inhibitor preventing the transcription of COL11A1 | colon cancer, ovarian cancer, bladder cancer, lung cancer | under clinical trials | [182,186,187,188,189] | |
| collagen type XI | AK778 and its cleavage product Col003 | disrupted collagen binding with the molecular chaperone HSP47 and inhibited collagen secretion | - | awaiting further clinical studies | [177,182] |
6.2. Interdicting the Receptors
The collagen receptors are the direct trigger of the interaction between cancer cells and collagens. Cancer cells sense the surrounding microenvironment by responding to the biochemical and mechanical properties of transmembrane receptors, including integrins and discoidin domain receptors (DDRs). Interdicting the receptors of collagens is another effectual strategy. We summarize the related targets and the corresponding drug below.
6.2.1. Integrins
Integrins are the important receptor of collagens on the cell membrane. It is a large family, at least including 24 different functional heterodimeric receptors distinguished by 18α-subunits and 8β-subunits [190,191]. According to the reports by far, the integrins of α1β1, α2β1, α3β1, α4β1, α5β1, α6β1, α9β1, α10β1, α11β1, α5β3, and α5β8 have been found to be involved in tumor growth and metastasis by the regulation of collagen-binding integrin signal [190,192,193,194,195,196,197,198,199,200]. Further, integrin-mediated pathways are reported many times to connect to drug resistance [201,202]. So, integrins are considered an attractive drug target for cancer therapeutics [203]. This concept is largely encouraged by preclinical studies. Cilengitide, an inhibitor of integrin αvβ3 and αvβv, has been developed as an anti-cancer drug in various tumor types. Several clinical trials were carried out on diverse cancers, such as lung cancer, breast cancer, glioblastoma, prostate cancer, melanoma, and squamous cell cancer [204,205]. Abituzumab (EMD 525797), a monoclonal antibody targeting integrin alpha nu heterodimers, was also demonstrated as an anti-cancer drug. The phase I clinical trial was completed in ovarian cancer patients with liver metastases and the phase II clinical trial was completed in metastatic colorectal cancer; however, successful clinical trials are few in number. For example, cilengitide failed to improve survival for glioblastoma patients in the phase III trial, despite the standard care. At the same time, the trial data of combining abituzumab showed no improvement in the progression-free survival of patients compared with the standard of care alone. So, further verified trials are essential based on stratifying the patient population [206]. Exploiting tumor-specific integrin expression profiles or downstream integrin effectors is also an alternative strategy to target for the development of anti-cancer drugs. Many typical integrin activation factors are noticed, such as FAK, LOX, mucins, and the corresponding inhibitors are developed for cancer therapeutic. Moreover, snake venom disintegrins were confirmed to inhibit integrins and further effected cancer treatment. We summarize the data in Table 3 below.
Table 3.
Integrin-associated therapy and the related drugs in cancer therapeutics.
| Therapeutics Target | Drug | Mechanism | Cancer Type | Status | Reference |
|---|---|---|---|---|---|
| integrin | Cilengitide | an inhibitor of integrin ανβ3, ανβ5, α5β1, αIIβ3 | lung cancer, breast cancer, glioblastoma, prostate cancer, melanoma, squamous cell cancer | in clinical trials | [203,207,208] |
| Abituzumab | inhibiting integrin ανβ1, ανβ3, ανβ5, ανβ6, ανβ8 | colorectal cancer. ovarian cancer |
in clinical trials | [203,209] | |
| Etaracizumab | inhibiting integrin ανβ3 | melanoma prostate cancer |
a phase II trial | [203] | |
| Intetumumab | inhibiting integrin ανβ1, ανβ3, ανβ5, ανβ6, ανβ8 | melanoma prostate cancer |
a phase II trial | [203] | |
| NCT02428270 | using a FAK inhibitor in combination with a MEK1 and MEK2 inhibitor | pancreatic cancer | a phase II trial | [206] | |
| NCT02546531 | using a FAK inhibitor in combination with a humanized antibody targeting programmed cell death protein 1 (PD1) and chemotherapy | solid tumors pancreatic cancer |
a phase I trial | [206] | |
| NCT01279603 | inhibit MUC1 cytoplasmic tail oligomerization | solid tumors | a phase I trial | [206] | |
| NCT00565721 | as valuable probes in cancer imaging studies to determine both prognosis and treatment efficacy | lung cancer Head & Neck cancer |
a phase II trial | [206] | |
| NCT02683824 | an αvβ6 integrin tracer to detect tumors and evaluate treatment response in patients with pancreatic cancer | pancreatic cancer | early phase I trial | [206] | |
| snake venom disintegrins | inhibiting integrins on transmembrane cellular surfaces | prostate breast cancer lung cancer sarcoma |
a promising candidate awaiting further testing | [208] |
6.2.2. DDRs
Another important receptor is DDRs family, including DDR1 and DDR2, which have been proved to regulate various cellular signaling pathways, including cell proliferation, adhesion, migration, and matrix remodeling. DDRs are a subfamily of receptor tyrosine kinases, activated by the triple-helical structure of collagens in the interaction. It is revealed that DDRs possess a special activation mechanism, which initiates the pathways leading to autophosphorylation through collagen binding. In the fibrillar collagens, DDR1 and DDR2 could respond to collagen type I, II, III, and V, while in the non-fibrillar collagens, type IV, VI, VIII, and X are also the activator. However, the mechanism of extracellular collagen binding and activation of the cytosolic kinase domain of the receptors is not clear so far. A recognized theory is that DDRs occur dimerization before the ligand binding with collagens, which is different from the other receptor tyrosine kinases undergoing dimerization after ligand binding [210]; then, the amino acid produces residues of collagens as the sites bind with DDRs dimerization [211]. In turn, the activated DDRs could trigger the signal transduction pathways of cell behaviors, such as proliferation, migration, and invasion [212]. In many cancers, overexpression of DDRs is associated with a poor prognosis. Deng et al. demonstrated that collagen-induced DDR1 activation in cancer cells could recruit tumor-associated neutrophils to form extracellular traps, enhancing the subsequent cancer cell invasion and metastasis [213]. The imbalance expression of DDRs has been demonstrated to be associated with most cancers. Huo et al. revealed that high expression of DDR1 was associated with poor prognosis in pancreatic ductal adenocarcinoma [214]. Xie et al. found that overexpression of DDR1 promoted the aggressive growth, migration, and invasion of bladder cancer cells, in which process collagen IV was a signal axis [215]. As DDRs play a significant role in cancer progression, DDRs would be new promising targets for cancer treatment, such as the design of DDR inhibitors for use in clinical settings. Some drugs were developed to inhibit DDR expression, such as dasatinib, imatinib, nilotinib, and ponatinib. Dasatinib was confirmed enabling to inhibit gastric cancer cell migration and invasion in the assays. Several clinical trials were completed in phases I and II, such as lung cancer, breast cancer, and prostate cancer. Nilotinib was reported to reduce metastatic colorectal cancer invasion by inhibiting DDR1 kinase activation. Many clinical trials are currently underway in several types of cancer, such as breast cancer, gastrointestinal stromal tumors, and so on. The antibody–drug conjugate targeting DDRs is utilized in anti-cancer drug development. As an example, T4H11-DM4 is demonstrated to be effective for colon cancer. Many other drugs were developed to target DDRs in recent years—shown in Table 4.
Table 4.
DDRs associated therapy and the related drugs in cancer therapeutics.
| Therapeutics Target | Drug | Mechanism | Cancer Type | Status | Reference |
|---|---|---|---|---|---|
| DDRs | nilotinib | inhibiting the kinase activity of DDR1 | colorectal cancer | [216] | |
| Dasatinib | inhibit DDRs | prostate cancer, glioblastoma, breast cancer, lung cancer, gastric cancer | in clinical trials | [217,218,219,220,221,222,223] | |
| Nilotinib | inhibit DDRs | colorectal cancer, colon cancer | in clinical trials | [217,224,225,226] | |
| Imatinib | inhibit DDRs | lung cancer, liver cancer | in clinical trials | [227,228,229,230] | |
| Ponatinib | inhibit DDRs | lung cancer | in clinical trials | [231,232] | |
| T4H11-DM4 | an antibody-drug conjugate targeting DDR1 | colon cancer | awaiting further clinical studies | [233] | |
| Actinomycin D | an antagonist of the DDR2-collagen interaction | rhabdomyosarcoma, Ewing’s sarcoma, trophoblastic neoplasia, and testicular carcinoma | in clinical application | [234,235] | |
| LCB 03-0110 | inhibiting collagen-induced activation of DDR1 and DDR2 receptors | - | awaiting further clinical studies | [236,237] | |
| pyrazolo-urea containing compounds 2a, 4a, 4b | inhibit DDR2 | - | awaiting further clinical studies | [238] | |
| 7rh | inhibited the kinase activity of DDR1 | gastric cancer, nasopharyngeal carcinoma, pancreatic ductal adenocarcinoma, breast cancer, uveal melanoma | in clinical trials | [218,239,240,241,242,243] | |
| 7rj | inhibited the kinase activity of DDR1 | - | awaiting further clinical studies | [235] | |
| DDR1-IN-1 | induced a significant inhibitory effect against DDR1 | colorectal cancer, lung cancer | awaiting further clinical studies | [232,244,245,246] | |
| DDR1-IN-2 | induced a significant inhibitory effect against DDR1 | - | awaiting further clinical studies | [235] | |
| miR-199a-5p, a targeted delivery of miRNAs | inhibit DDRs | colorectal cancer, renal cancer | awaiting further clinical studies | [247,248,249,250] | |
| monoclonal antibodies Fab 3E3, 48B3, H-126 | inhibit DDRs | ductal breast carcinoma | awaiting further clinical studies | [235,251] |
6.3. Targeting to Collagen-Induced Chemoresistance
More and more data implicated the desmoplastic reaction is substantially related to chemoresistance in chemotherapeutics. It is reported that the pancreatic cancer cells grown in collagens demonstrated low sensitivity to gemcitabine chemotherapy. A further study showed that three-dimensional collagens enabled an increase in ERK1/2 signaling, which is known to promote chemotherapy resistance in several cancers. In other malignancies, it is repeatedly reported that collagens protect cancer cells against chemotherapy. For instance, in lung cancer models, collagens are shown to provide survival signals to attenuate the effects of chemotherapy. In this regard, MT1-MMP plays a critical physiological role in modulating growth factors and integrin signaling to enhance ERK1/2 phosphorylation in the collagen microenvironment. Moreover, the increasing density of the ECM initiated by collagen fibers and collagen deposition attenuates the permeability of drug delivery in chemotherapy. Targeting collagen-induced chemoresistance is an effective strategy to promote the chemotherapy effect. Some drugs are developed targeting the intermediary in the signal pathway. Moreover, enhancing the collagen penetration of anticancer drugs is an available strategy for cancer therapeutics, which targets collagen-associated stiffness ECM and high dense collagen fibers, increasing the drug efficacy [252]. We summarize the related drugs in Table 5.
Table 5.
The drugs that target collagen-induced chemoresistance.
| Therapeutics Target | Drug | Mechanism | Cancer Type | Status | Reference |
|---|---|---|---|---|---|
| collagen | polyethylene glycol (PEG) & glutaraldehyde co-modified fluorinated chitosan (PGFCS) | as a collagen-targeted transepithelial penetration enhancer creating a tumor-targeted adhesive interface to open the transepithelial-delivery barrier at the tumor site | bladder cancer | awaiting further testing | [253] |
| losartan | reducing stromal collagen and hyaluronan production to decompress tumor vessels for enhancing drug delivery. | prostate cancer, colorectal cancer, pancreatic cancer, breast cancer, lung cancer, ovarian cancer, endometrial cancer | in clinical application | [254,255,256,257,258,259,260,261] | |
| Collagen type II | Ivosideni | a selective inhibitor of mutant IDH1, which is a gene mutant site of collagen type II | chondrosarcoma | waiting further clinical studies | [262] |
| ERK1/2 | JaZ-30 | downregulates phosphorylation of the extracellular signal-regulated ERK1/2 | melanoma | waiting further clinical studies | [263] |
7. Conclusions and Future Perspectives
Collagens are the main component of the ECM, and their remodeling occurs along with all processes of cancer progression. Collagens occur in abnormal morphology and distribution in precancerous lesions, which seriously affect the topography of the ECM. This provides a chance for clinicians to discover the pathology through medical imaging or pathological for cancer early diagnosis. In cancer development, collagens cause different stages of ECM topography, which contributes to cancer staging. Moreover, collagen-associated biochemical indicators are the significant biomarkers of cancer diagnosis and prognosis. Collagen participation in cancer progression is not only reflected in the remodeling under the influence of tumor cells or tumor-associated cells but is further revealed as the role of guider or inducer for cancer cell invasion. The “highway” for cancer cell invasion and the high stiffness of ECM are all enhanced by collagens, corresponding with the aligned collagen fiber bundle and collagen deposition, respectively. Based on the mechanism of the interaction between collagens and cancer cells, many opportunities for cancer therapeutics are revealed by disturbing or blocking the requirement in the interaction. The targets are diversely located across the pathway of collagen synthesis, binding to receptors, degradation, and drug transport. Overall, collagens provide many opportunities, whether for cancer diagnosis or cancer treatment; however, there are still many challenges from the exploration of therapeutic targets to drug development because there are only a few drugs allowed to enter the clinical application, while most of them are just in clinical trials or waiting for further clinical studies. Several questions and propositions are provided for further research. Firstly, the mechanism of collagen remodeling and its interaction with cancer cells is not completely clear. So further studies are essential on the mechanisms of collagen remodeling and the interaction between collagens and cancer cells. In our opinion, small molecule inhibitors are worth developing as anti-cancer drugs due to their excellent location and potential to cause no damage to normal cells. It would be a potential strategy to block the collagen remodeling; however, it is hard to implement for the reconstructed collagens. So, how to reduce the effectiveness of the reconstructed collagens is a valuable issue. In addition to the targets in the action pathway, we propose that ablating the reconstructed collagens is another strategy for cancer therapeutics. Moreover, to enhance the efficacy, we highlight the significance of finding a suitable nanocarrier to increase the drug transport capacity. Overall, further efforts are urgent in the collagen-associated mechanism and the therapeutic strategy for cancer.
Author Contributions
K.S. and Z.H., designed the study; Z.Y. and G.L. drew the schematic diagrams; K.S., X.Z. and Y.X. wrote and modified the paper. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Grants from the National Natural Science Foundation of China (Grant No. 12104134), key specialized research and development breakthrough of He’nan province (Grant No. 212102310887, No. 212102310741), key scientific research projects of He’nan colleges and universities (Grant No. 21A416005), Luoyang Public Security Project (Grant No. 2101024A).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Paszek M.J., Zahir N., Johnson K.R., Lakins J.N., Rozenberg G.I., Gefen A., Reinhart-King C.A., Margulies S.S., Dembo M., Boettiger D., et al. Tensional homeostasis and the malignant phenotype. Cancer Cell. 2005;8:241–254. doi: 10.1016/j.ccr.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 2.Butcher D.T., Alliston T., Weaver V.M. A tense situation: Forcing tumour progression. Nat. Rev. Cancer. 2009;9:108–122. doi: 10.1038/nrc2544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Theocharis A.D., Skandalis S.S., Gialeli C., Karamanos N.K. Extracellular matrix structure. Adv. Drug Deliv. Rev. 2016;97:4–27. doi: 10.1016/j.addr.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Winkler J., Abisoye-Ogunniyan A., Metcalf K.J., Werb Z. Concepts of extracellular matrix remodelling in tumour progression and metastasis. Nat. Commun. 2020;11:5120. doi: 10.1038/s41467-020-18794-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frantz C., Stewart K.M., Weaver V.M. The extracellular matrix at a glance. J. Cell Sci. 2010;123:4195–4200. doi: 10.1242/jcs.023820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ricard-Blum S. The Collagen Family. Cold Spring Harbor Perspect. Biol. 2011;3:a004978. doi: 10.1101/cshperspect.a004978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu Y.X., Ge G.X. Complexity of type IV collagens: From network assembly to function. Biol. Chem. 2019;400:565–574. doi: 10.1515/hsz-2018-0317. [DOI] [PubMed] [Google Scholar]
- 8.Bella J., Hulmes D.J.S. Fibrillar Collagens. In: Parry D.A.D., Squire J.M., editors. Fibrous Proteins: Structures and Mechanisms. Volume 82. Springer; Berlin/Heidelberg, Germany: 2017. pp. 457–490. [DOI] [PubMed] [Google Scholar]
- 9.Shamhart P.E., Meszaros J.G. Non-fibrillar collagens: Key mediators of post-infarction cardiac remodeling? J. Mol. Cell. Cardiol. 2010;48:530–537. doi: 10.1016/j.yjmcc.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 10.Ambekar R., Lau T.-Y., Walsh M., Bhargava R., Toussaint K.C., Jr. Quantifying collagen structure in breast biopsies using second-harmonic generation imaging. Biomed. Opt. Express. 2012;3:2021–2035. doi: 10.1364/BOE.3.002021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Belisle J., Zigras T., Costantino S., Cartier R., Butany J., Wiseman P.W., Leask R.L. Second harmonic generation microscopy to investigate collagen configuration: A pericarditis case study. Cardiovasc. Pathol. Off. J. Soc. Cardiovasc. Pathol. 2010;19:e125–e128. doi: 10.1016/j.carpath.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 12.Grethel Fuentes-Corona C., Licea-Rodriguez J., Younger R., Rangel-Rojo R., Potma E.O., Rocha-Mendoza I. Second harmonic generation signal from type I collagen fibers grown in vitro. Biomed. Opt. Express. 2019;10:6449–6461. doi: 10.1364/BOE.10.006449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohammed D., Pardon G., Versaevel M., Bruyere C., Alaimo L., Luciano M., Vercruysse E., Pruitt B.L., Gabriele S. Producing Collagen Micro-stripes with Aligned Fibers for Cell Migration Assays. Cell. Mol. Bioeng. 2020;13:87–98. doi: 10.1007/s12195-019-00600-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okoro C., Toussaint K.C., Jr. Second-harmonic patterned polarization-analyzed reflection confocal microscope. J. Biomed. Opt. 2017;22:086007. doi: 10.1117/1.JBO.22.8.086007. [DOI] [PubMed] [Google Scholar]
- 15.Olivares V., Condor M., Del Amo C., Asin J., Borau C., Manuel Garcia-Aznar J. Image-based Characterization of 3D Collagen Networks and the Effect of Embedded Cells. Microsc. Microanal. 2019;25:971–981. doi: 10.1017/S1431927619014570. [DOI] [PubMed] [Google Scholar]
- 16.Xu M.Y., Liu J., Sun J.Y., Xu X.R., Hu Y.C., Liu B. Optical Microscopy and Electron Microscopy for the Morphological Evaluation of Tendons: A Mini Review. Orthop. Surg. 2020;12:366–371. doi: 10.1111/os.12637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raspanti M., Reguzzoni M., Rita Basso P., Protasoni M., Martini D. Visualizing the Supramolecular Assembly of Collagen. Methods Mol. Biol. 2019;1952:33–44. doi: 10.1007/978-1-4939-9133-4_3. [DOI] [PubMed] [Google Scholar]
- 18.Oosterlaken B.M., Friedrich H., de With G. The effects of washing a collagen sample prior to TEM examination. Microsc. Res. Tech. 2022;85:412–417. doi: 10.1002/jemt.23915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quan B.D., Sone E.D. Cryo-TEM Analysis of Collagen Fibrillar Structure. In: Yoreo J.J.D., editor. Research Methods in Biomineralization Science. Volume 532. Elsevier; Amsterdam, The Netherlands: 2013. pp. 189–205. [DOI] [PubMed] [Google Scholar]
- 20.Oosterlaken B.M., van Rijt M.M.J., Joosten R.R.M., Bomans P.H.H., Friedrich H., de With G. Time-Resolved Cryo-TEM Study on the Formation of Iron Hydroxides in a Collagen Matrix. ACS Biomater. Sci. Eng. 2021;7:3123–3131. doi: 10.1021/acsbiomaterials.1c00416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Quan B.D., Sone E.D. Structural changes in collagen fibrils across a mineralized interface revealed by cryo-TEM. Bone. 2015;77:42–49. doi: 10.1016/j.bone.2015.04.020. [DOI] [PubMed] [Google Scholar]
- 22.Raspanti M., Protasoni M., Manelli A., Guizzardi S., Mantovani V., Sala A. The extracellular matrix of the human aortic wall: Ultrastructural observations by FEG-SEM and by tapping-mode AFM. Micron. 2006;37:81–86. doi: 10.1016/j.micron.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 23.Stylianou A. Assessing Collagen D-Band Periodicity with Atomic Force Microscopy. Materials. 2022;15:1608. doi: 10.3390/ma15041608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Youn Y.-S., Kim S. Real-time atomic force microscopy imaging of collagen fibril under ultraviolet irradiation. J. Ind. Eng. Chem. 2016;42:15–18. doi: 10.1016/j.jiec.2016.07.023. [DOI] [Google Scholar]
- 25.Meek K.M., Quantock A.J. The use of X-ray scattering techniques to determine corneal ultrastructure. Prog. Retin. Eye Res. 2001;20:95–137. doi: 10.1016/S1350-9462(00)00016-1. [DOI] [PubMed] [Google Scholar]
- 26.Meek K.M., Quantock A.J., Hayes S., Bell J. X-Ray Diffraction Imaging of Corneal Ultrastructure. Methods Mol. Biol. 2020;2145:231–247. doi: 10.1007/978-1-0716-0599-8_16. [DOI] [PubMed] [Google Scholar]
- 27.Karjalainen V.P., Kestila I., Finnila M.A., Folkesson E., Turkiewicz A., Onnerfjord P., Hughes V., Tjonstand J., Englund M., Saarakkala S. Quantitative three-dimensional collagen orientation analysis of human meniscus posterior horn in health and osteoarthritis using micro-computed tomography. Osteoarthr. Cartil. 2021;29:762–772. doi: 10.1016/j.joca.2021.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eder J., Tonar Z., Schmid-Schwap M., Bristela M., Skolka A., Traxler H., Piehslinger E., Egerbacher M., Trattnig S., Witter K. Regional Collagen Fiber Network in the Articular Disc of the Human Temporomandibular Joint: Biochemical 3-Tesla Quantitative Magnetic Resonance Imaging Compared to Quantitative Histologic Analysis of Fiber Arrangement. J. Oral Facial Pain Headache. 2018;32:266–276. doi: 10.11607/ofph.1879. [DOI] [PubMed] [Google Scholar]
- 29.Mercado K.P., Helguera M., Hocking D.C., Dalecki D. Noninvasive Quantitative Imaging of Collagen Microstructure in Three-Dimensional Hydrogels Using High-Frequency Ultrasound. Tissue Eng. Part C-Methods. 2015;21:671–682. doi: 10.1089/ten.tec.2014.0527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hagan K.L., Hullfish T., Casey E., Raxter J.R. Tendon structure quantified using ultrasound imaging differs based on location and training type. J. Appl. Physiol. 2018;125:1743–1748. doi: 10.1152/japplphysiol.00723.2018. [DOI] [PubMed] [Google Scholar]
- 31.Kim M.N., Kim S.U., Kim B.K., Park J.Y., Kim D.Y., Ahn S.H., Song K.J., Park Y.N., Han K.H. Increased risk of hepatocellular carcinoma in chronic hepatitis B patients with transient elastography-defined subclinical cirrhosis. Hepatology. 2015;61:1851–1859. doi: 10.1002/hep.27735. [DOI] [PubMed] [Google Scholar]
- 32.Suh B., Park S., Shin D.W., Yun J.M., Yang H.K., Yu S.J., Shin C.I., Kim J.S., Ahn E., Lee H., et al. High Liver Fibrosis Index FIB-4 Is Highly Predictive of Hepatocellular Carcinoma in Chronic Hepatitis B Carriers. Hepatology. 2015;61:1261–1268. doi: 10.1002/hep.27654. [DOI] [PubMed] [Google Scholar]
- 33.Baglieri J., Brenner D.A., Kisseleva T. The Role of Fibrosis and Liver-Associated Fibroblasts in the Pathogenesis of Hepatocellular Carcinoma. Int. J. Mol. Sci. 2019;20:1723. doi: 10.3390/ijms20071723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jeganathan N., Cleland D., Sathananthan M. The association of lung cancer with pulmonary fibrosis. ERJ Open Res. 2022;8:00505-2021. doi: 10.1183/23120541.00505-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saha R., Ryan D., Hanrahan E., Dodd J.D. Early detection of recurrent lung cancer: Enhancing-nodule in post-radiation fibrosis. Acta Radiol. Open. 2022;11:20584601211072280. doi: 10.1177/20584601211072280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Snijder J., Peraza J., Padilla M., Capaccione K., Salvatore M.M. Pulmonary fibrosis: A disease of alveolar collapse and collagen deposition. Expert Rev. Respir. Med. 2019;13:615–619. doi: 10.1080/17476348.2019.1623028. [DOI] [PubMed] [Google Scholar]
- 37.Liu C.M., Liao Y.W., Hsieh P.L., Yu C.H., Chueh P.J., Lin T.C., Yang P.Y., Yu C.C., Chou M.Y. miR-1246 as a therapeutic target in oral submucosa fibrosis pathogenesis. J. Formos. Med. Assoc. 2019;118:1093–1098. doi: 10.1016/j.jfma.2019.02.014. [DOI] [PubMed] [Google Scholar]
- 38.Shih Y.-H., Wang T.-H., Shieh T.-M., Tseng Y.-H. Oral Submucous Fibrosis: A Review on Etiopathogenesis, Diagnosis, and Therapy. Int. J. Mol. Sci. 2019;20:2940. doi: 10.3390/ijms20122940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Despotovic S.Z., Milkcvic D.N., Krmpot A.J., Pavlovic A.M., Zivanovic V.D., Krivokapic Z., Pavlovic V.B., Levic S., Nikolic G., Rabasovic M.D. Altered organization of collagen fibers in the uninvolved human colon mucosa 10 cm and 20 cm away from the malignant tumor. Sci. Rep. 2020;10:6359. doi: 10.1038/s41598-020-63368-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Fatima Cavalcanti Castor M.d.G., Torres L.C., Vieira de Mello R.J., Natal R.d.A., Vassallo J. Study on collagen parameters in vulvar cancer and preneoplastic lesions by Second Harmonic Generation microscopy. Sci. Rep. 2020;10:5568. doi: 10.1038/s41598-020-62346-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zaffar M., Pradhan A. Mapping of retardance, diattenuation and polarizance vector on Poincare sphere for diagnosis and classification of cervical precancer. J. Biophotonics. 2020;13:e201960139. doi: 10.1002/jbio.201960139. [DOI] [PubMed] [Google Scholar]
- 42.Zaffar M., Pradhan A. Assessment of anisotropy of collagen structures through spatial frequencies of Mueller matrix images for cervical pre-cancer detection. Appl. Opt. 2020;59:1237–1248. doi: 10.1364/AO.377105. [DOI] [PubMed] [Google Scholar]
- 43.Hirakawa Y., Futaki S., Tanizaki H., Furukawa F., Maemura K., Kondo Y., Moriwaki S. Enhanced expression of nidogen 1 around the nest of basal cell carcinoma compared with that around squamous cell carcinoma. Med. Mol. Morphol. 2019;52:99–105. doi: 10.1007/s00795-018-0207-x. [DOI] [PubMed] [Google Scholar]
- 44.Wu Y., Fu F.M., Lian Y.N., Nie Y.T., Zhuo S.M., Wang C., Chen J.X. Monitoring the progression from intraductal carcinoma to invasive ductal carcinoma based on multiphoton microscopy. J. Biomed. Opt. 2015;20:096007. doi: 10.1117/1.JBO.20.9.096007. [DOI] [PubMed] [Google Scholar]
- 45.Banerjee S., Lo W.C., Majumder P., Roy D., Ghorai M., Shaikh N.K., Kant N., Shekhawat M.S., Gadekar V.S., Ghosh S., et al. Multiple roles for basement membrane proteins in cancer progression and EMT. Eur. J. Cell Biol. 2022;101:151220. doi: 10.1016/j.ejcb.2022.151220. [DOI] [PubMed] [Google Scholar]
- 46.Chang J.L., Chaudhuri O. Beyond proteases: Basement membrane mechanics and cancer invasion. J. Cell Biol. 2019;218:2456–2469. doi: 10.1083/jcb.201903066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gaiko-Shcherbak A., Eschenbruch J., Kronenberg N.M., Teske M., Wolters B., Springer R., Gather M.C., Merkel R., Hoffmann B., Noetzel E. Cell Force-Driven Basement Membrane Disruption Fuels EGF- and Stiffness-Induced Invasive Cell Dissemination from Benign Breast Gland Acini. Int. J. Mol. Sci. 2021;22:3962. doi: 10.3390/ijms22083962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Luthold C., Hallal T., Labbe D.P., Bordeleau F. The Extracellular Matrix Stiffening: A Trigger of Prostate Cancer Progression and Castration Resistance? Cancers. 2022;14:2887. doi: 10.3390/cancers14122887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fang M., Yuan J., Peng C., Li Y. Collagen as a double-edged sword in tumor progression. Tumor Biol. 2014;35:2871–2882. doi: 10.1007/s13277-013-1511-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Levental K.R., Yu H.M., Kass L., Lakins J.N., Egeblad M., Erler J.T., Fong S.F.T., Csiszar K., Giaccia A., Weninger W., et al. Matrix Crosslinking Forces Tumor Progression by Enhancing Integrin Signaling. Cell. 2009;139:891–906. doi: 10.1016/j.cell.2009.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barbazan J., Vignjevic D.M. Cancer associated fibroblasts: Is the force the path to the dark side? Curr. Opin. Cell Biol. 2019;56:71–79. doi: 10.1016/j.ceb.2018.09.002. [DOI] [PubMed] [Google Scholar]
- 52.Bertero T., Oldham W.M., Grasset E.M., Bourget I., Boulter E., Pisano S., Hofman P., Bellvert F., Meneguzzi G., Bulavin D.V., et al. Tumor-Stroma Mechanics Coordinate Amino Acid Availability to Sustain Tumor Growth and Malignancy. Cell Metab. 2019;29:124–140.e10. doi: 10.1016/j.cmet.2018.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stylianou A., Gkretsi V., Louca M., Zacharia L.C., Stylianopoulos T. Collagen content and extracellular matrix cause cytoskeletal remodelling in pancreatic fibroblasts. J. R. Soc. Interface. 2019;16:20190226. doi: 10.1098/rsif.2019.0226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stylianou A., Gkretsi V., Stylianopoulos T. Transforming growth factor-beta modulates pancreatic cancer associated fibroblasts cell shape, stiffness and invasion. Biochim. Et Biophys. Acta-Gen. Subj. 2018;1862:1537–1546. doi: 10.1016/j.bbagen.2018.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shibata M., Ham K., Hoque M.O. A time for YAP1: Tumorigenesis, immunosuppression and targeted therapy. Int. J. Cancer. 2018;143:2133–2144. doi: 10.1002/ijc.31561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Farhat A., Ferns G.A., Ashrafi K., Arjmand M.-H. Lysyl Oxidase Mechanisms to Mediate Gastrointestinal Cancer Progression. Gastrointest. Tumors. 2021;8:33–40. doi: 10.1159/000511244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Azimzade Y., Saberi A.A., Sahimi M. Regulation of migration of chemotactic tumor cells by the spatial distribution of collagen fiber orientation. Phys. Rev. E. 2019;99:062414. doi: 10.1103/PhysRevE.99.062414. [DOI] [PubMed] [Google Scholar]
- 58.Geiger F., Schnitzler L.G., Brugger M.S., Westerhausen C., Engelke H. Directed invasion of cancer cell spheroids inside 3D collagen matrices oriented by microfluidic flow in experiment and simulation. PLoS ONE. 2022;17:e0264571. doi: 10.1371/journal.pone.0264571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Han W., Chen S., Yuan W., Fan Q., Tian J., Wang X., Chen L., Zhang X., Wei W., Liu R., et al. Oriented collagen fibers direct tumor cell intravasation. Proc. Natl. Acad. Sci. USA. 2016;113:11208–11213. doi: 10.1073/pnas.1610347113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Suveges S., Chamseddine I., Rejniak K.A., Eftimie R., Trucu D. Collective Cell Migration in a Fibrous Environment: A Hybrid Multiscale Modelling Approach. Front. Appl. Math. Stat. 2021;7:680029. doi: 10.3389/fams.2021.680029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gkretsi V., Stylianopoulos T. Cell Adhesion and Matrix Stiffness: Coordinating Cancer Cell invasion and Metastasis. Front. Oncol. 2018;8:145. doi: 10.3389/fonc.2018.00145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li H., Bera K., Gilmore H., Davidson N.E., Goldstein L.J., Madabhushi A. Histomorphometric measure of disorder of collagen fiber orientation is associated with risk of recurrence in ER plus breast cancers in ECOG-ACRIN E2197 and TCGA-BRCA. Cancer Res. 2020;80:615. [Google Scholar]
- 63.Lee B., Konen J., Wilkinson S., Marcus A.I., Jiang Y. Local alignment vectors reveal cancer cell-induced ECM fiber remodeling dynamics. Sci. Rep. 2017;7:39498. doi: 10.1038/srep39498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lewis D.M., Tang V., Jain N., Isser A., Xia Z., Gerecht S. Collagen Fiber Architecture Regulates Hypoxic Sarcoma Cell Migration. ACS Biomater. Sci. Eng. 2018;4:400–409. doi: 10.1021/acsbiomaterials.7b00056. [DOI] [PubMed] [Google Scholar]
- 65.Nan H., Liang L., Chen G., Liu L., Liu R., Jiao Y. Realizations of highly heterogeneous collagen networks via stochastic reconstruction for micromechanical analysis of tumor cell invasion. Phys. Rev. E. 2018;97:033311. doi: 10.1103/PhysRevE.97.033311. [DOI] [PubMed] [Google Scholar]
- 66.Wang H., Abhilash A.S., Chen C.S., Wells R.G., Shenoy V.B. Long-Range Force Transmission in Fibrous Matrices Enabled by Tension-Driven Alignment of Fibers. Biophys. J. 2014;107:2592–2603. doi: 10.1016/j.bpj.2014.09.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang J., Petefish J.W., Hillier A.C., Schneider I.C. Epitaxially Grown Collagen Fibrils Reveal Diversity in Contact Guidance Behavior among Cancer Cells. Langmuir. 2015;31:307–314. doi: 10.1021/la503254x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ray A., Provenzano P.P. Aligned forces: Origins and mechanisms of cancer dissemination guided by extracellular matrix architecture. Curr. Opin. Cell Biol. 2021;72:63–71. doi: 10.1016/j.ceb.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bayer S.V.H., Grither W.R., Brenot A., Hwang P.Y., Barcus C.E., Ernst M., Pence P., Walter C., Pathak A., Longmore G.D. DDR2 controls breast tumor stiffness and metastasis by regulating integrin mediated mechanotransduction in CAFs. Elife. 2019;8:e45508. doi: 10.7554/eLife.45508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hanley C.J., Noble F., Ward M., Bullock M., Drifka C., Mellone M., Manousopoulou A., Johnston H.E., Johnston H.E., Hayden A., et al. A subset of myofibroblastic cancer-associated fibroblasts regulate collagen fiber elongation, which is prognostic in multiple cancers. Oncotarget. 2016;7:6159–6174. doi: 10.18632/oncotarget.6740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Del Amo C., Olivares V., Condor M., Blanco A., Santolaria J., Asin J., Borau C., Garcia-Aznar J.M. Matrix architecture plays a pivotal role in 3D osteoblast migration: The effect of interstitial fluid flow. J. Mech. Behav. Biomed. Mater. 2018;83:52–62. doi: 10.1016/j.jmbbm.2018.04.007. [DOI] [PubMed] [Google Scholar]
- 72.Balcioglu H.E., van de Water B., Danen E.H.J. Tumor-induced remote ECM network orientation steers angiogenesis. Sci. Rep. 2016;6:22580. doi: 10.1038/srep22580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kirkpatrick N.D., Andreou S., Hoying J.B., Utzinger U. Live imaging of collagen remodeling during angiogenesis. Am. J. Physiol.-Heart Circ. Physiol. 2007;292:H3198–H3206. doi: 10.1152/ajpheart.01234.2006. [DOI] [PubMed] [Google Scholar]
- 74.Luthria G., Li R., Wang S., Prytyskach M., Kohler R.H., Lauffenburger D.A., Mitchison T.J., Weissleder R., Miller M.A. In vivo microscopy reveals macrophage polarization locally promotes coherent microtubule dynamics in migrating cancer cells. Nat. Commun. 2020;11:3521. doi: 10.1038/s41467-020-17147-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hansen N.U.B., Willumsen N., Sand J.M.B., Larsen L., Karsdal M.A., Leeming D.J. Type VIII collagen is elevated in diseases associated with angiogenesis and vascular remodeling. Clin. Biochem. 2016;49:903–908. doi: 10.1016/j.clinbiochem.2016.05.023. [DOI] [PubMed] [Google Scholar]
- 76.Piotrowski-Daspit A.S., Nerger B.A., Wolf A.E., Sundaresan S., Nelson C.M. Dynamics of Tissue-Induced Alignment of Fibrous Extracellular Matrix. Biophys. J. 2017;113:702–713. doi: 10.1016/j.bpj.2017.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Velez D.O., Tsui B., Goshia T., Chute C.L., Han A., Carter H., Fraley S.I. 3D collagen architecture induces a conserved migratory and transcriptional response linked to vasculogenic mimicry. Nat. Commun. 2017;8:1651. doi: 10.1038/s41467-017-01556-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bedal K.B., Grassel S., Spanier G., Reichert T.E., Bauer R.J. The NC11 domain of human collagen XVI induces vasculogenic mimicry in oral squamous cell carcinoma cells. Carcinogenesis. 2015;36:1429–1439. doi: 10.1093/carcin/bgv141. [DOI] [PubMed] [Google Scholar]
- 79.Fan H., Li H., Liu G., Cong W., Zhao H., Cao W., Zheng J. Doxorubicin combined with low intensity ultrasound suppresses the growth of oral squamous cell carcinoma in culture and in xenografts. J. Exp. Clin. Cancer Res. 2017;36:163. doi: 10.1186/s13046-017-0633-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nelson M.T., Short A., Cole S.L., Gross A.C., Winter J., Eubank T.D., Lannutti J.J. Preferential, enhanced breast cancer cell migration on biomimetic electrospun nanofiber ‘cell highways’. Bmc Cancer. 2014;14:825. doi: 10.1186/1471-2407-14-825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Su C.-Y., Burchett A., Dunworth M., Choi J.S., Ewald A.J., Ahn E.H., Kim D.-H. Engineering a 3D collective cancer invasion model with control over collagen fiber alignment. Biomaterials. 2021;275:120922. doi: 10.1016/j.biomaterials.2021.120922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gritsenko P.G., Ilina O., Friedl P. Interstitial guidance of cancer invasion. J. Pathol. 2012;226:185–199. doi: 10.1002/path.3031. [DOI] [PubMed] [Google Scholar]
- 83.Iuliano J.N., Kutscha P.D., Biderman N.J., Subbaram S., Groves T.R., Tenenbaum S.A., Hempel N. Metastatic bladder cancer cells distinctively sense and respond to physical cues of collagen fibril-mimetic nanotopography. Exp. Biol. Med. 2015;240:601–610. doi: 10.1177/1535370214560973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Soon L.L. A discourse on cancer cell chemotaxis: Where to from here? Iubmb Life. 2007;59:60–67. doi: 10.1080/15216540701201033. [DOI] [PubMed] [Google Scholar]
- 85.Yokoi K., Kojic M., Milosevic M., Tanei T., Ferrari M., Ziemys A. Capillary-Wall Collagen as a Biophysical Marker of Nanotherapeutic Permeability into the Tumor Microenvironment. Cancer Res. 2014;74:4239–4246. doi: 10.1158/0008-5472.CAN-13-3494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yudasaka M., Okamatsu-Ogura Y., Tanaka T., Saeki K., Kataura H. Cold-induced Conversion of Connective Tissue Skeleton in Brown Adipose Tissues. Acta Histochem. Et Cytochem. 2021;54:131–141. doi: 10.1267/ahc.21-00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Knudson K.M., Hicks K.C., Luo X., Chen J.Q., Schlom J., Gameiro S.R. M7824, a novel bifunctional anti-PD-L1/TGFβ Trap fusion protein, promotes anti-tumor efficacy as monotherapy and in combination with vaccine. Oncoimmunology. 2018;7:e1426519. doi: 10.1080/2162402X.2018.1426519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Romer A.M.A., Thorseth M.L., Madsen D.H. Immune Modulatory Properties of Collagen in Cancer. Front. Immunol. 2021;12:791453. doi: 10.3389/fimmu.2021.791453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yu Q., Xue Y.X., Liu J., Xi Z., Li Z., Liu Y.H. Fibronectin Promotes the Malignancy of Glioma Stem-Like Cells Via Modulation of Cell Adhesion, Differentiation, Proliferation and Chemoresistance. Front. Mol. Neurosci. 2018;11:130. doi: 10.3389/fnmol.2018.00130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fang M., Yuan J.-P., Peng C.-W., Liu S.-P., Li Y. Dynamic Changes of Collagen IV During Cancer Invasion and Migration: Pulse Mode. Prog. Biochem. Biophys. 2013;40:1056–1062. [Google Scholar]
- 91.Zhang H., Fredericks T., Xiong G., Qi Y., Rychahou P.G., Li J.-D., Pihlajaniemi T., Xu W., Xu R. Membrane associated collagen XIII promotes cancer metastasis and enhances anoikis resistance. Breast Cancer Res. 2018;20:116. doi: 10.1186/s13058-018-1030-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Karagiannis G.S., Petraki C., Prassas I., Saraon P., Musrap N., Dimitromanolakis A., Diamandis E.P. Proteomic Signatures of the Desmoplastic Invasion Front Reveal Collagen Type XII as a Marker of Myofibroblastic Differentiation During Colorectal Cancer Metastasis. Oncotarget. 2012;3:267–285. doi: 10.18632/oncotarget.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kumagai Y., Nio-Kobayashi J., Ishida-Ishihara S., Tachibana H., Omori R., Enomoto A., Ishihara S., Haga H. The intercellular expression of type-XVII collagen, laminin-332, and integrin-beta 1 promote contact following during the collective invasion of a cancer cell population. Biochem. Biophys. Res. Commun. 2019;514:1115–1121. doi: 10.1016/j.bbrc.2019.05.058. [DOI] [PubMed] [Google Scholar]
- 94.Miyake M., Hori S., Morizawa Y., Tatsumi Y., Toritsuka M., Ohnishi S., Shimada K., Furuya H., Khadka V.S., Deng Y., et al. Collagen type IV alpha 1 (COL4A1) and collagen type XIII alpha 1 (COL13A1) produced in cancer cells promote tumor budding at the invasion front in human urothelial carcinoma of the bladder. Oncotarget. 2017;8:36099–36114. doi: 10.18632/oncotarget.16432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Franjevic A., Pavicevic R., Bubanovic G. ICTP in bone metastases of lung cancer. Coll. Anthropol. 2011;35:43–47. [PubMed] [Google Scholar]
- 96.Nurmenniemi S., Koivula M.K., Nyberg P., Tervahartiala T., Sorsa T., Mattila P.S., Salo T., Risteli J. Type I and III collagen degradation products in serum predict patient survival in head and neck squamous cell carcinoma. Oral Oncol. 2012;48:136–140. doi: 10.1016/j.oraloncology.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 97.Willumsen N., Bager C.L., Leeming D.J., Smith V., Christiansen C., Karsdal M.A., Dornan D., Bay-Jensen A.C. Serum biomarkers reflecting specific tumor tissue remodeling processes are valuable diagnostic tools for lung cancer. Cancer Med. 2014;3:1136–1145. doi: 10.1002/cam4.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ghassemi H., Hashemnia M., Mousavibahar S.H., Hosseini H.M., Mirhosseini S.A. Positive Association of Matrix Proteins Alteration with TAZ and The Progression of High-Grade Bladder Cancer. Cell J. 2021;23:742–749. doi: 10.22074/cellj.2021.7661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Qin L.P., Zeng J.P., Shi N.N., Chen L., Wang L. Application of weighted gene co-expression network analysis to explore the potential diagnostic biomarkers for colorectal cancer. Mol. Med. Rep. 2020;21:2533–2543. doi: 10.3892/mmr.2020.11047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zhu Z.L., Yang G.Y., Pang Z.Z., Liang J.W., Wang W.Z., Zhou Y.L. Establishment of a regression model of bone metabolism markers for the diagnosis of bone metastases in lung cancer. World J. Surg. Oncol. 2021;19:27. doi: 10.1186/s12957-021-02141-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lipton A., Leitzel K., Ali S.M., Polimera H.V., Nagabhairu V., Marks E., Richardson A.E., Krecko L., Ali A., Koestler W., et al. High turnover of extracellular matrix reflected by specific protein fragments measured in serum is associated with poor outcomes in two metastatic breast cancer cohorts. Int. J. Cancer. 2018;143:3027–3034. doi: 10.1002/ijc.31627. [DOI] [PubMed] [Google Scholar]
- 102.Ma H.P., Chang H.L., Bamodu O.A., Yadav V.K., Huang T.Y., Wu A.T.H., Yeh C.T., Tsai S.H., Lee W.H. Collagen 1A1 (COL1A1) Is a Reliable Biomarker and Putative Therapeutic Target for Hepatocellular Carcinogenesis and Metastasis. Cancers. 2019;11:786. doi: 10.3390/cancers11060786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zulauf N., Bruggmann D., Groneberg D., Oremek G.M. Expressiveness of Bone Markers in Breast Cancer with Bone Metastases. Oncology. 2019;97:236–244. doi: 10.1159/000500675. [DOI] [PubMed] [Google Scholar]
- 104.Rong L., Huang W., Tian S.K., Chi X.B., Zhao P., Liu F.F. COL1A2 is a Novel Biomarker to Improve Clinical Prediction in Human Gastric Cancer: Integrating Bioinformatics and Meta-Analysis. Pathol. Oncol. Res. 2018;24:129–134. doi: 10.1007/s12253-017-0223-5. [DOI] [PubMed] [Google Scholar]
- 105.Narita T., Funahashi H., Satoh Y., Takagi H. Procollagen type III N-peptide and type IV collagen 7S-domain in the sera of breast cancer patients. Surg. Today. 1993;23:682–686. doi: 10.1007/BF00311705. [DOI] [PubMed] [Google Scholar]
- 106.Chen I.M., Willumsen N., Dehlendorff C., Johansen A.Z., Jensen B.V., Hansen C.P., Hasselby J.P., Bojesen S.E., Pfeiffer P., Nielsen S.E., et al. Clinical value of serum hyaluronan and propeptide of type III collagen in patients with pancreatic cancer. Int. J. Cancer. 2020;146:2913–2922. doi: 10.1002/ijc.32751. [DOI] [PubMed] [Google Scholar]
- 107.Mazurek K., Siemianowicz K., Likus W., Pierzchala E., Kwiatkowski R., Markowski J. Collagen Type III Metabolism Evaluation in Patients with Malignant Head and Neck Cancer Treated with Radiotherapy. BioMed Res. Int. 2018;2018:8702605. doi: 10.1155/2018/8702605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tomas C., Risteli J., Risteli L., Vuori J., Kauppila A. Use of various epithelial tumor markers and a stromal marker in the assessment of cervical carcinoma. Obstet. Gynecol. 1991;77:566–572. [PubMed] [Google Scholar]
- 109.Akazawa S., Harada A., Futatsuki K. Diagnostic values of type III Procollagen N-terminal peptide and combination assay of type III procollagen N-terminal peptide with CEA and CA 19-9 in gastric cancer. Gan To Kagaku Ryoho. Cancer Chemother. 1984;11:1434–1438. [PubMed] [Google Scholar]
- 110.Cracchiolo B.M., Hanauske-Abel H.M., Schwartz P.E., Chambers J.T., Holland B., Chambers S.K. Procollagen-derived biomarkers in malignant ascites of ovarian cancer. Independent prognosticators for progression-free interval and survival. Gynecol. Oncol. 2002;87:24–33. doi: 10.1006/gyno.2002.6798. [DOI] [PubMed] [Google Scholar]
- 111.Gabazza E.C., Taguchi O., Yamakami T., Machishi M., Ibata H., Tsutsui K., Suzuki S. Coagulation-fibrinolysis system and markers of collagen metabolism in lung cancer. Cancer. 1992;70:2631–2636. doi: 10.1002/1097-0142(19921201)70:11<2631::AID-CNCR2820701111>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 112.Attallah A.M., Albannan M.S., El-Deen M.S., Farid K., Khedr F.M., Attallah K.A., Abdallah S.O. Diagnostic role of collagen-III and matrix metalloproteinase-1 for early detection of hepatocellular carcinoma. Br. J. Biomed. Sci. 2020;77:58–63. doi: 10.1080/09674845.2019.1708534. [DOI] [PubMed] [Google Scholar]
- 113.Gueugnon F., Leclercq S., Blanquart C., Sagan C., Cellerin L., Padieu M., Perigaud C., Scherpereel A., Gregoire M. Identification of Novel Markers for the Diagnosis of Malignant Pleural Mesothelioma. Am. J. Pathol. 2011;178:1033–1042. doi: 10.1016/j.ajpath.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Tang M., Liu P.Q., Wu X.K., Gong J., Weng J.C., Gao G.Y., Liu Y.L., Gan L. COL3A1 and Its Related Molecules as Potential Biomarkers in the Development of Human Ewing’s Sarcoma. BioMed Res. Int. 2021;2021:7453500. doi: 10.1155/2021/7453500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kinoshita J., Fushida S., Harada S., Makino I., Nakamura K., Oyama K., Fujita H., Ninomiya I., Fujimura T., Kayahara M., et al. Type IV collagen levels are elevated in the serum of patients with peritoneal dissemination of gastric cancer. Oncol. Lett. 2010;1:989–994. doi: 10.3892/ol.2010.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Willumsen N., Bager C.L., Leeming D.J., Smith V., Karsdal M.A., Dornan D., Bay-Jensen A.C. Extracellular matrix specific protein fingerprints measured in serum can separate pancreatic cancer patients from healthy controls. BMC Cancer. 2013;13:554. doi: 10.1186/1471-2407-13-554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Seko Y., Sumida Y., Tanaka S., Taketani H., Kanemasa K., Ishiba H., Okajima A., Nishimura T., Yamaguchi K., Moriguchi M., et al. Predictors of malignancies and overall mortality in Japanese patients with biopsy-proven non-alcoholic fatty liver disease. Hepatol. Res. 2015;45:728–738. doi: 10.1111/hepr.12407. [DOI] [PubMed] [Google Scholar]
- 118.Sumida Y., Yoneda M., Seko Y., Ishiba H., Hara T., Toyoda H., Yasuda S., Kumada T., Hayashi H., Japan Study Group of NAFLD (JSG-NAFLD) et al. Surveillance of Hepatocellular Carcinoma in Nonalcoholic Fatty Liver Disease. Diagnostics. 2020;10:579. doi: 10.3390/diagnostics10080579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wang H.B., Liu Z.D., Li A., Wang J.L., Liu J.T., Liu B.F., Lian X.Y., Zhang B., Pang B., Liu L.Y., et al. COL4A1 as a novel oncogene associated with the clinical characteristics of malignancy predicts poor prognosis in glioma. Exp. Therapeutic Med. 2021;22:1224. doi: 10.3892/etm.2021.10658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hiki Y., Iyama K.-I., Tsuruta J., Egami H., Kamio T., Suko S., Naito I., Sado Y., Ninomiya Y., Ogawa M. Differential distribution of basement membrane type IV collagen alpha1(IV), alpha2(IV), alpha5(IV) and alpha6(IV) chains in colorectal epithelial tumors. Pathol. Int. 2002;52:224–233. doi: 10.1046/j.1440-1827.2002.01341.x. [DOI] [PubMed] [Google Scholar]
- 121.Bager C.L., Willumsen N., Leeming D.J., Smith V., Karsdal M.A., Dornan D., Bay-Jensen A.C. Collagen degradation products measured in serum can separate ovarian and breast cancer patients from healthy controls: A preliminary study. Cancer Biomark. 2015;15:783–788. doi: 10.3233/CBM-150520. [DOI] [PubMed] [Google Scholar]
- 122.Sameni M., Dosescu J., Yamada K.M., Sloane B.F., Cavallo-Medved D. Functional live-cell imaging demonstrates that beta1-integrin promotes type IV collagen degradation by breast and prostate cancer cells. Mol. Imaging. 2008;7:199–213. doi: 10.2310/7290.2008.00019A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ioachim E., Michael M., Stavropoulos N.E., Kitsiou E., Salmas M., Malamou-Mitsi V. A clinicopathological study of the expression of extracellular matrix components in urothelial carcinoma. BJU Int. 2005;95:655–659. doi: 10.1111/j.1464-410X.2005.05357.x. [DOI] [PubMed] [Google Scholar]
- 124.Chen C., Mendez E., Houck J., Fan W., Lohavanichbutr P., Doody D., Yueh B., Futran N.D., Upton M., Farwell D.G., et al. Gene expression profiling identifies genes predictive of oral squamous cell carcinoma. Cancer Epidemiol. Biomark. Prevent. 2008;17:2152–2162. doi: 10.1158/1055-9965.EPI-07-2893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Liu Y.L., Zhang J.Y., Chen Y., Sohel H., Ke X.R., Chen J.Q., Li Y.X. The correlation and role analysis of COL4A1 and COL4A2 in hepatocarcinogenesis. Aging-Us. 2020;12:204–223. doi: 10.18632/aging.102610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Miyake M., Morizawa Y., Hori S., Tatsumi Y., Onishi S., Owari T., Iida K., Onishi K., Gotoh D., Nakai Y., et al. Diagnostic and prognostic role of urinary collagens in primary human bladder cancer. Cancer Sci. 2017;108:2221–2228. doi: 10.1111/cas.13384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Yantiss R.K., Bosenberg M.W., Antonioli D.A., Odze R.D. Utility of MMP-1, p53, E-cadherin, and collagen IV immunohistochemical stains in the differential diagnosis of adenomas with misplaced epithelium versus adenomas with invasive adenocarcinoma. Am. J. Surg. Pathol. 2002;26:206–215. doi: 10.1097/00000478-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 128.Kayashima H., Maeda T., Harada N., Masuda T., Guntani A., Ito S., Matsuyama A., Hamatake M., Tsutsui S., Matsuda H., et al. Risk factors for incisional hernia after hepatic resection for hepatocellular carcinoma in patients with liver cirrhosis. Surgery. 2015;158:1670–1676. doi: 10.1016/j.surg.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 129.Wang J., Jiang Y.H., Yang P.Y., Liu F. Increased Collagen Type V alpha 2 (COL5A2) in Colorectal Cancer is Associated with Poor Prognosis and Tumor Progression. Oncotargets Ther. 2021;14:2991–3002. doi: 10.2147/OTT.S288422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ding Y.L., Sun S.F., Zhao G.L. COL5A2 as a potential clinical biomarker for gastric cancer and renal metastasis. Medicine. 2021;100:e24561. doi: 10.1097/MD.0000000000024561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wu M., Sun Q., Mo C.H., Pang J.S., Hou J.Y., Pang L.L., Lu H.P., Dang Y.W., Fang S.J., Tang D., et al. Prospective molecular mechanism of COL5A1 in breast cancer based on a microarray, RNA sequencing and immunohistochemistry. Oncol. Rep. 2019;42:151–175. doi: 10.3892/or.2019.7147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Balancin M.L., Teodoro W.R., Baldavira C.M., Prieto T.G., Farhat C., Velosa A.P., Souza P.D., Yaegashi L.B., Ab’Saber A.M., Takagaki T.Y., et al. Different histological patterns of type-V collagen levels confer a matrices-privileged tissue microenvironment for invasion in malignant tumors with prognostic value. Pathol. Res. Pract. 2020;216:153277. doi: 10.1016/j.prp.2020.153277. [DOI] [PubMed] [Google Scholar]
- 133.Willumsen N., Bager C., Karsdal M.A. Matrix Metalloprotease Generated Fragments of Type VI Collagen Have Serum Biomarker Potential in Cancer—A Proof of Concept Study. Transl. Oncol. 2019;12:693–698. doi: 10.1016/j.tranon.2019.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kang C.Y., Wang J., Axell-House D., Soni P., Chu M.L., Chipitsyna G., Sarosiek K., Sendecki J., Hyslop T., Al-Zoubi M., et al. Clinical Significance of Serum COL6A3 in Pancreatic Ductal Adenocarcinoma. J. Gastrointest. Surg. 2014;18:7–15. doi: 10.1007/s11605-013-2326-y. [DOI] [PubMed] [Google Scholar]
- 135.Angenendt L., Mikesch J.H., Gorlich D., Busch A., Arnhold I., Rudack C., Hartmann W., Wardelmann E., Berdel W.E., Stenner M., et al. Stromal collagen type VI associates with features of malignancy and predicts poor prognosis in salivary gland cancer. Cell. Oncol. 2018;41:517–525. doi: 10.1007/s13402-018-0389-1. [DOI] [PubMed] [Google Scholar]
- 136.Arafat H., Lazar M., Salem K., Chipitsyna G., Gong Q.K., Pan T.C., Zhang R.Z., Yeo C.J., Chu M.L. Tumor-specific expression and alternative splicing of the COL6A3 gene in pancreatic cancer. Surgery. 2011;150:306–315. doi: 10.1016/j.surg.2011.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Fan N.J., Gao C.F., Wang C.S., Zhao G., Lv J.J., Wang X.L., Chu G.H., Yin J., Li D.H., Chen X., et al. Identification of the up-regulation of TP-alpha, collagen alpha-1(VI) chain, and S100A9 in esophageal squamous cell carcinoma by a proteomic method. J. Proteom. 2012;75:3977–3986. doi: 10.1016/j.jprot.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 138.Wetzels R.H., Schaafsma H.E., Leigh I.M., Lane E.B., Troyanovsky S.M., Wagenaar S.S., Vooijs G.P., Ramaekers F.C. Laminin and type VII collagen distribution in different types of human lung carcinoma: Correlation with expression of keratins 14, 16, 17 and 18. Histopathology. 1992;20:295–303. doi: 10.1111/j.1365-2559.1992.tb00986.x. [DOI] [PubMed] [Google Scholar]
- 139.Pourreyron C., Chen M., McGrath J.A., Salas-Alanis J.C., South A.P., Leigh I.M. High levels of type VII collagen expression in recessive dystrophic epidermolysis bullosa cutaneous squamous cell carcinoma keratinocytes increases PI3K and MAPK signalling, cell migration and invasion. Br. J. Dermatol. 2014;170:1256–1265. doi: 10.1111/bjd.12715. [DOI] [PubMed] [Google Scholar]
- 140.Oh S.E., Oh M.Y., An J.Y., Lee J.H., Sohn T.S., Bae J.M., Choi M.G., Kim K.M. Prognostic Value of Highly Expressed Type VII Collagen (COL7A1) in Patients with Gastric Cancer. Pathol. Oncol. Res. 2021;27:1609860. doi: 10.3389/pore.2021.1609860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.He Z.H., Deng T., Duan X.L., Zeng G.H. Profiles of overall survival-related gene expression-based risk signature and their prognostic implications in clear cell renal cell carcinoma. Biosci. Rep. 2020;40:Bsr20200492. doi: 10.1042/BSR20200492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Willumsen N., Jorgensen L.N., Karsdal M.A. Vastatin (the NC1 domain of human type VIII collagen a1 chain) is linked to stromal reactivity and elevated in serum from patients with colorectal cancer. Cancer Biol. Ther. 2019;20:692–699. doi: 10.1080/15384047.2018.1550571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Peng W., Li J.D., Zeng J.J., Zou X.P., Tang D., Tang W., Rong M.H., Li Y., Dai W.B., Tang Z.Q., et al. Clinical value and potential mechanisms of COL8A1 upregulation in breast cancer: A comprehensive analysis. Cancer Cell Int. 2020;20:392. doi: 10.1186/s12935-020-01465-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Shang J., Wang F., Chen P.F., Wang X.B., Ding F., Liu S., Zhao Q. Co-expression Network Analysis Identified COL8A1 Is Associated with the Progression and Prognosis in Human Colon Adenocarcinoma. Digest. Dis. Sci. 2018;63:1219–1228. doi: 10.1007/s10620-018-4996-5. [DOI] [PubMed] [Google Scholar]
- 145.Zhang D.W., Zhu H.F., Harpaz N. Overexpression of alpha 1 chain of type XI collagen (COL11A1) aids in the diagnosis of invasive carcinoma in endoscopically removed malignant colorectal polyps. Pathol. Res. Pract. 2016;212:545–548. doi: 10.1016/j.prp.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 146.Freire J., Dominguez-Hormaetxe S., Pereda S., De Juan A., Vega A., Simon L., Gomez-Roman J. Collagen, type XI, alpha 1: An accurate marker for differential diagnosis of breast carcinoma invasiveness in core needle biopsies. Pathol. Res. Pract. 2014;210:879–884. doi: 10.1016/j.prp.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 147.Su C., Zhao J.B., Hong X.Y., Yang S.J., Jiang Y., Hou J.J. Microarray-based analysis of COL11A1 and TWIST1 as important differentially-expressed pathogenic genes between left and right-sided colon cancer. Mol. Med. Rep. 2019;20:4202–4214. doi: 10.3892/mmr.2019.10667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Zhao Y., Zhou T.H., Li A.Q., Yao H.M., He F., Wang L.J., Si J.M. A Potential Role of Collagens Expression in Distinguishing Between Premalignant and Malignant Lesions in Stomach. Anat. Rec.-Adv. Integr. Anat. Evol. Biol. 2009;292:692–700. doi: 10.1002/ar.20874. [DOI] [PubMed] [Google Scholar]
- 149.Wang H., Zhou H.C., Ni H., Shen X.H. COL11A1-Driven Epithelial-Mesenchymal Transition and Sternness of Pancreatic Cancer Cells Induce Cell Migration and Invasion by Modulating the AKT/GSK-3 beta/Snail Pathway. Biomolecules. 2022;12:391. doi: 10.3390/biom12030391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Zheng X.Y., Liu X.L., Zheng H.S., Wang H.N., Hong D.F. Integrated bioinformatics analysis identified COL11A1 as an immune infiltrates correlated prognosticator in pancreatic adenocarcinoma. Int. Immunopharmacol. 2021;90:106982. doi: 10.1016/j.intimp.2020.106982. [DOI] [PubMed] [Google Scholar]
- 151.Garcia-Pravia C., Galvan J.A., Gutierrez-Corral N., Solar-Garcia L., Garcia-Perez E., Garcia-Ocana M., Del Amo-Iribarren J., Menendez-Rodriguez P., Garcia-Garcia J., de los Toyos J.R., et al. Overexpression of COL11A1 by Cancer-Associated Fibroblasts: Clinical Relevance of a Stromal Marker in Pancreatic Cancer. PLoS ONE. 2013;8:e78327. doi: 10.1371/journal.pone.0078327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Fuentes-Martinez N., Garcia-Pravia C., Garcia-Ocana M., Menendez-Rodriguez P., Del Amo J., Suarez-Fernandez L., Galvan J.A., Toyos J.R.D., Barneo L. Overexpression of proCOL11A1 as a stromal marker of breast cancer. Histol. Histopathol. 2015;30:87–93. doi: 10.14670/HH-30.87. [DOI] [PubMed] [Google Scholar]
- 153.Goto R., Nakamura Y., Takami T., Sanke T., Tozuka Z. Quantitative LC-MS/MS Analysis of Proteins Involved in Metastasis of Breast Cancer. PLoS ONE. 2015;10:e0130760. doi: 10.1371/journal.pone.0130760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Husi H., MacDonald A., Skipworth R.J.E., Miller J., Cronshaw A., Greig C., Fearon K.C.H., Ross J.A. Urinary diagnostic proteomic markers for dynapenia in cancer patients. Biomed. Rep. 2018;8:547–556. doi: 10.3892/br.2018.1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Franklin O., Ohlund D., Lundin C., Oman M., Naredi P., Wang W.Z., Sund M. Combining conventional and stroma-derived tumour markers in pancreatic ductal adenocarcinoma. Cancer Biomark. 2015;15:1–10. doi: 10.3233/CBM-140430. [DOI] [PubMed] [Google Scholar]
- 156.Kantola T., Vayrynen J.P., Klintrup K., Makela J., Karppinen S.M., Pihlajaniemi T., Autio-Harmainen H., Karttunen T.J., Makinen M.J., Tuomisto A. Serum endostatin levels are elevated in colorectal cancer and correlate with invasion and systemic inflammatory markers. Br. J. Cancer. 2014;111:1605–1613. doi: 10.1038/bjc.2014.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Xu F.J., Chang K., Ma J., Qu Y.Y., Xie H.Y., Dai B., Gan H.L., Zhang H.L., Shi G.H., Zhu Y., et al. The Oncogenic Role of COL23A1 in Clear Cell Renal Cell Carcinoma. Sci. Rep. 2017;7:9846. doi: 10.1038/s41598-017-10134-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Angel P.M., Zambrzycki S.C. Predictive value of collagen in cancer. Adv. Cancer Res. 2022;154:15–45. doi: 10.1016/bs.acr.2022.02.004. [DOI] [PubMed] [Google Scholar]
- 159.Whatcott C.J., Diep C.H., Jiang P., Watanabe A., LoBello J., Sima C., Hostetter G., Shepard H.M., Von Hoff D.D., Han H. Desmoplasia in Primary Tumors and Metastatic Lesions of Pancreatic Cancer. Clin. Cancer Res. 2015;21:3561–3568. doi: 10.1158/1078-0432.CCR-14-1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Vasta J.D., Raines R.T. Collagen Prolyl 4-Hydroxylase as a Therapeutic Target. J. Med. Chem. 2018;61:10403–10411. doi: 10.1021/acs.jmedchem.8b00822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Qiu S., Fraser S.P., Pires W., Djamgoz M.B.A. Anti-invasive effects of minoxidil on human breast cancer cells: Combination with ranolazine. Clin. Exp. Metastasis. 2022;39:679–689. doi: 10.1007/s10585-022-10166-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Qi Y.F., Xu R. Roles of PLODs in Collagen Synthesis and Cancer Progression. Front. Cell Dev. Biol. 2018;6:66. doi: 10.3389/fcell.2018.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Shi W.Y., Cao C., Liu L. Interferon alpha Induces the Apoptosis of Cervical Cancer HeLa Cells by Activating both the Intrinsic Mitochondrial Pathway and Endoplasmic Reticulum Stress-Induced Pathway. Int. J. Mol. Sci. 2016;17:1832. doi: 10.3390/ijms17111832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Sun X.H., Cui X.J., Chen X.H., Jiang X.G. Baicalein alleviated TGF beta 1-induced type I collagen production in lung fibroblasts via downregulation of connective tissue growth factor. Biomed. Pharmacother. 2020;131:110744. doi: 10.1016/j.biopha.2020.110744. [DOI] [PubMed] [Google Scholar]
- 165.Tuli H.S., Aggarwal V., Kaur J., Aggarwal D., Parashar G., Parashar N.C., Tuorkey M., Kaur G., Savla R., Sak K., et al. Baicalein: A metabolite with promising antineoplastic activity. Life Sci. 2020;259:118183. doi: 10.1016/j.lfs.2020.118183. [DOI] [PubMed] [Google Scholar]
- 166.Rishikof D.C., Ricupero D.A., Liu H., Goldstein R.H. Phenylbutyrate decreases type I collagen production in human lung fibroblasts. J. Cell. Biochem. 2004;91:740–748. doi: 10.1002/jcb.10742. [DOI] [PubMed] [Google Scholar]
- 167.Xu Y.W., Zheng S.B., Chen B.S., Wen Y., Zhu S.W. Sodium phenylbutyrate antagonizes prostate cancer through the induction of apoptosis and attenuation of cell viability and migration. Oncotargets Ther. 2016;9:2825–2833. doi: 10.2147/OTT.S101794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Lee J.-S., Jin H.Y., Ko J.M., Kim S.H., Han N., Park B.K., Park M., Park H.J., Lee J.A. Hyperammonemic Encephalopathy Mimicking Ornithine Transcarbamylase Deficiency in Fibrolamellar Hepatocellular Carcinoma: Successful Treatment with Continuous Venovenous Hemofiltration and Ammonia Scavengers. Cancer Res. Treat. 2021;53:283–288. doi: 10.4143/crt.2020.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Rubio C., Avendano-Ortiz J., Ruiz-Palomares R., Karaivanova V., Alberquilla O., Sanchez-Dominguez R., Casalvilla-Duenas J.C., Montalban-Hernandez K., Lodewijk I., Rodriguez-Izquierdo M., et al. Toward Tumor Fight and Tumor Microenvironment Remodeling: PBA Induces Cell Cycle Arrest and Reduces Tumor Hybrid Cells’ Pluripotency in Bladder Cancer. Cancers. 2022;14:287. doi: 10.3390/cancers14020287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Wang Y.-Y., Lee K.-T., Lim M.C., Choi J.-H. TRPV1 Antagonist DWP05195 Induces ER Stress-Dependent Apoptosis through the ROS-p38-CHOP Pathway in Human Ovarian Cancer Cells. Cancers. 2020;12:1702. doi: 10.3390/cancers12061702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Wu Y., Zhao Y., He X., He Z., Wang T., Wan L., Chen L., Yan N. Hydroxypropyl-beta-cyclodextrin attenuates the epithelial-to-mesenchymal transition via endoplasmic reticulum stress in MDA-MB-231 breast cancer cells. Mol. Med. Rep. 2020;21:249–257. doi: 10.3892/mmr.2019.10802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Stefanovic B., Manojlovic Z., Vied C., Badger C.D., Stefanovic L. Discovery and evaluation of inhibitor of LARP6 as specific antifibrotic compound. Sci. Rep. 2019;9:326. doi: 10.1038/s41598-018-36841-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Agarwal S., Behring M., Kim H.G., Bajpai P., Chakravarthi B., Gupta N., Elkholy A., Al Diffalha S., Varambally S., Manne U. Targeting P4HA1 with a Small Molecule Inhibitor in a Colorectal Cancer PDX Model. Transl. Oncol. 2020;13:100754. doi: 10.1016/j.tranon.2020.100754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Gilkes D.M., Chaturvedi P., Bajpai S., Wong C.C., Wei H., Pitcairn S., Hubbi M.E., Wirtz D., Semenza G.L. Collagen Prolyl Hydroxylases Are Essential for Breast Cancer Metastasis. Cancer Res. 2013;73:3285–3296. doi: 10.1158/0008-5472.CAN-12-3963. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 175.Chen I.S., Chou C.-T., Liu Y.-Y., Yu C.-C., Liang W.-Z., Kuo C.-C., Shieh P., Kuo D.-H., Chen F.-A., Jan C.-R. The investigation of minoxidil-induced Ca2+ (i) rises and non-Ca2+-triggered cell death in PC3 human prostate cancer cells. J. Recept. Signal Transduct. 2017;37:1–7. doi: 10.3109/10799893.2015.1122041. [DOI] [PubMed] [Google Scholar]
- 176.Fukushiro-Lopes D., Jain M., Khalid M., Hegel A., Gentile S. Potassium channel activator minoxidil (Rogaine) as a novel single-agent or combination therapy in ovarian cancer. Clin. Cancer Res. 2018;24:66–67. doi: 10.1158/1557-3265.OVCA17-A52. [DOI] [Google Scholar]
- 177.Ito S., Ogawa K., Takeuchi K., Takagi M., Yoshida M., Hirokawa T., Hirayama S., Shin-ya K., Shimada I., Doi T., et al. A small-molecule compound inhibits a collagen-specific molecular chaperone and could represent a potential remedy for fibrosis. J. Biol. Chem. 2017;292:20076–20085. doi: 10.1074/jbc.M117.815936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Miyamura T., Sakamoto N., Kakugawa T., Taniguchi H., Akiyama Y., Okuno D., Moriyama S., Hara A., Kido T., Ishimoto H., et al. Small molecule inhibitor of HSP47 prevents pro-fibrotic mechanisms of fibroblasts in vitro. Biochem. Biophys. Res. Commun. 2020;530:561–565. doi: 10.1016/j.bbrc.2020.07.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Leung L., Niculescu-Duyaz D., Smithen D., Lopes F., Callens C., McLeary R., Saturno G., Davies L., Aljarah M., Brown M., et al. Anti-metastatic Inhibitors of Lysyl Oxidase (LOX): Design and Structure-Activity Relationships. J. Med. Chem. 2019;62:5863–5884. doi: 10.1021/acs.jmedchem.9b00335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Wang T.-H., Hsia S.-M., Shieh T.-M. Lysyl Oxidase and the Tumor Microenvironment. Int. J. Mol. Sci. 2017;18:62. doi: 10.3390/ijms18010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Kelley R.K., Gane E., Assenat E., Siebler J., Galle P.R., Merle P., Hourmand I.O., Cleverly A., Zhao Y., Gueorguieva I., et al. A Phase 2 Study of Galunisertib (TGF-β1 Receptor Type I Inhibitor) and Sorafenib in Patients with Advanced Hepatocellular Carcinoma. Clin. Transl. Gastroenterol. 2019;10:e00056. doi: 10.14309/ctg.0000000000000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Wu Y.-H., Chou C.-Y. Collagen XI Alpha 1 Chain, a Novel Therapeutic Target for Cancer Treatment. Front. Oncol. 2022;12:925165. doi: 10.3389/fonc.2022.925165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Chen J., Li S., Liu X., Liu S., Xiao C., Zhang Z., Li S., Li Z., Yang X. Transforming growth factor-beta blockade modulates tumor mechanical microenvironments for enhanced antitumor efficacy of photodynamic therapy. Nanoscale. 2021;13:9989–10001. doi: 10.1039/D1NR01552D. [DOI] [PubMed] [Google Scholar]
- 184.Wang Y., Gao Z., Du X., Chen S., Zhang W., Wang J., Li H., He X., Cao J., Wang J. Co-inhibition of the TGF-beta pathway and the PD-L1 checkpoint by pH-responsive clustered nanoparticles for pancreatic cancer microenvironment regulation and anti-tumor immunotherapy. Biomater. Sci. 2020;8:5121–5132. doi: 10.1039/D0BM00916D. [DOI] [PubMed] [Google Scholar]
- 185.Zhang Q., Hou X., Evans B.J., VanBlaricom J.L., Weroha S.J., Cliby W.A. LY2157299 Monohydrate, a TGF-beta R1 Inhibitor, Suppresses Tumor Growth and Ascites Development in Ovarian Cancer. Cancers. 2018;10:260. doi: 10.3390/cancers10080260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Wu Y.H., Huang Y.F., Chen C.C., Chou C.Y. Akt inhibitor SC66 promotes cell sensitivity to cisplatin in chemoresistant ovarian cancer cells through inhibition of COL11A1 expression. Cell Death Dis. 2019;10:322. doi: 10.1038/s41419-019-1555-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Cai X., Hu B., Liu S., Liu M., Huang Y., Lei P., Zhang Z., He Z., Zhang L., Huang R. Overexpression of close homolog of L1 enhances the chemosensitivity of lung cancer cells via inhibition of the Akt pathway. Oncol. Lett. 2020;20:111. doi: 10.3892/ol.2020.11972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Chen W., Zhao S., Yu W., Rao T., Ruan Y., Zhu S., Xia Y., Song H., Cheng F. SC66 inhibits the proliferation and induces apoptosis of human bladder cancer cells by targeting the AKT/beta-catenin pathway. J. Cell. Mol. Med. 2021;25:10684–10697. doi: 10.1111/jcmm.17005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Liu Y., Huang Y., Ding J., Liu N., Peng S., Wang J., Wang F., Zhang Y. Targeting Akt by SC66 triggers GSK-3 mediated apoptosis in colon cancer therapy. Cancer Cell Int. 2019;19:124. doi: 10.1186/s12935-019-0837-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Bourgot I., Primac I., Louis T., Noel A., Maquoi E. Reciprocal Interplay Between Fibrillar Collagens and Collagen-Binding Integrins: Implications in Cancer Progression and Metastasis. Front. Oncol. 2020;10:1488. doi: 10.3389/fonc.2020.01488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Ivaska J., Heino J. Adhesion receptors and cell invasion: Mechanisms of integrin-guided degradation of extracellular matrix. Cell. Mol. Life Sci. CMLS. 2000;57:16–24. doi: 10.1007/s000180050496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Coopman P.J., Thomas D.M., Gehlsen K.R., Mueller S.C. Integrin alpha 3 beta 1 participates in the phagocytosis of extracellular matrix molecules by human breast cancer cells. Mol. Biol. Cell. 1996;7:1789–1804. doi: 10.1091/mbc.7.11.1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Feng X., Jin L. Relationship between integrin alpha v beta 3 and alpha 6 beta 1 expression levels and clinicopathological characteristics of cervical cancer. Trop. J. Pharm. Res. 2020;19:2323–2328. [Google Scholar]
- 194.Gupta S.K., Oommen S., Aubry M.C., Williams B.P., Vlahakis N.E. Integrin alpha 9 beta 1 promotes malignant tumor growth and metastasis by potentiating epithelial-mesenchymal transition. Oncogene. 2013;32:141–150. doi: 10.1038/onc.2012.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Rentala S., Yalavarthy P.D., Mangamoori L.N. alpha 1 and beta 1 integrins enhance the homing and differentiation of cultured prostate cancer stem cells. Asian J. Androl. 2010;12:548–555. doi: 10.1038/aja.2010.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Sawai H., Okada Y., Funahashi H., Matsuo Y., Takahashi H., Takeyama H., Manabe T. Interleukin-1alpha enhances the aggressive behavior of pancreatic cancer cells by regulating the alpha6beta1-integrin and urokinase plasminogen activator receptor expression. BMC Cell Biol. 2006;7:8. doi: 10.1186/1471-2121-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Scalici J.M., Harrer C., Allen A., Jazaeri A., Atkins K.A., McLachlan K.R., Slack-Davis J.K. Inhibition of alpha 4 beta 1 integrin increases ovarian cancer response to carboplatin. Gynecol. Oncol. 2014;132:455–461. doi: 10.1016/j.ygyno.2013.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Subbaram S., DiPersio C.M. Integrin alpha 3 beta 1 as a breast cancer target. Expert Opin. Ther. Targets. 2011;15:1197–1210. doi: 10.1517/14728222.2011.609557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Wang H.-Y., Chen Z., Wang Z.-H., Wang H., Huang L.-M. Prognostic Significance of alpha 5 beta 1-integrin Expression in Cervical Cancer. Asian Pac. J. Cancer Prevent. 2013;14:3891–3895. doi: 10.7314/APJCP.2013.14.6.3891. [DOI] [PubMed] [Google Scholar]
- 200.Zhou M., Niu J., Wang J., Gao H., Shahbaz M., Niu Z., Li Z., Zou X., Liang B. Integrin alpha v beta 8 serves as a Novel Marker of Poor Prognosis in Colon Carcinoma and Regulates Cell Invasiveness through the Activation of TGF-beta 1. J. Cancer. 2020;11:3803–3815. doi: 10.7150/jca.43826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Hirata E., Girotti M.R., Viros A., Hooper S., Spencer-Dene B., Matsuda M., Larkin J., Marais R., Sahai E. Intravital imaging reveals how BRAF inhibition generates drug-tolerant microenvironments with high integrin β1/FAK signaling. Cancer Cell. 2015;27:574–588. doi: 10.1016/j.ccell.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Hanker A.B., Estrada M.V., Bianchini G., Moore P.D., Zhao J., Cheng F., Koch J.P., Gianni L., Tyson D.R., Sánchez V., et al. Extracellular Matrix/Integrin Signaling Promotes Resistance to Combined Inhibition of HER2 and PI3K in HER2(+) Breast Cancer. Cancer Res. 2017;77:3280–3292. doi: 10.1158/0008-5472.CAN-16-2808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Lasinska I., Mackiewicz J. Integrins as A New Target for Cancer Treatment. Anti-Cancer Agents Med. Chem. 2019;19:580–586. doi: 10.2174/1871520618666181119103413. [DOI] [PubMed] [Google Scholar]
- 204.Lautenschlaeger T., Perry J., Peereboom D., Li B., Ibrahim A., Huebner A., Meng W., White J., Chakravarti A. In vitro study of combined cilengitide and radiation treatment in breast cancer cell lines. Radiat. Oncol. 2013;8:246. doi: 10.1186/1748-717X-8-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Reardon D.A., Cheresh D. Cilengitide: A prototypic integrin inhibitor for the treatment of glioblastoma and other malignancies. Genes Cancer. 2011;2:1159–1165. doi: 10.1177/1947601912450586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Hamidi H., Ivaska J. Every step of the way: Integrins in cancer progression and metastasis. Nat. Rev. Cancer. 2018;18:533–548. doi: 10.1038/s41568-018-0038-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Massabeau C., Khalifa J., Filleron T., Modesto A., Bigay-Gamé L., Plat G., Dierickx L., Aziza R., Rouquette I., Gomez-Roca C., et al. Continuous Infusion of Cilengitide Plus Chemoradiotherapy for Patients With Stage III Non-Small-cell Lung Cancer: A Phase I Study. Clin. Lung Cancer. 2018;19:e277–e285. doi: 10.1016/j.cllc.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 208.Akhtar B., Muhammad F., Sharif A., Anwar M.I. Mechanistic insights of snake venom disintegrins in cancer treatment. Eur. J. Pharmacol. 2021;899:174022. doi: 10.1016/j.ejphar.2021.174022. [DOI] [PubMed] [Google Scholar]
- 209.Khanna D., Tashkin D.P., Wells A.U., Seibold J.R., Wax S., Vazquez-Mateo C., Fleuranceau-Morel P., Damian D., Denton C.P. STRATUS: A Phase II Study of Abituzumab in Patients With Systemic Sclerosis-associated Interstitial Lung Disease. J. Rheumatol. 2021;48:1295–1298. doi: 10.3899/jrheum.191365. [DOI] [PubMed] [Google Scholar]
- 210.Zhu J.J., Cheng H., Wang L., Xu W.D., Wang J.Q., Han Q., Lee J.H., Du L.Y., Lyu J.X. Discoidin domain receptor 1 promotes lung adenocarcinoma migration via the AKT/snail signaling axis. Mol. Biol. Rep. 2022;49:7275–7286. doi: 10.1007/s11033-022-07509-8. [DOI] [PubMed] [Google Scholar]
- 211.Matada G.S.P., Das A., Dhiwar P.S., Ghara A. DDR1 and DDR2: A review on signaling pathway and small molecule inhibitors as an anticancer agent. Med. Chem. Res. 2021;30:535–551. doi: 10.1007/s00044-020-02694-2. [DOI] [Google Scholar]
- 212.Gao Y., Zhou J.L., Li J. Discoidin domain receptors orchestrate cancer progression: A focus on cancer therapies. Cancer Sci. 2021;112:962–969. doi: 10.1111/cas.14789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Deng J.Y., Kang Y., Cheng C.C., Li X.Q., Dai B.B., Katz M.H., Men T., Kim M.P., Koay E.A., Huang H.C., et al. DDR1-induced neutrophil extracellular traps drive pancreatic cancer metastasis. JCI Insight. 2021;6:e146133. doi: 10.1172/jci.insight.146133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Huo Y.M., Yang M.W., Liu W., Yang J.Y., Fu X.L., Liu D.J., Li J., Zhang J.F., Hua R., Sun Y.W. High expression of DDR1 is associated with the poor prognosis in Chinese patients with pancreatic ductal adenocarcinoma. J. Exp. Clin. Cancer Res. 2015;34:88. doi: 10.1186/s13046-015-0202-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Xie X., He H.C., Zhang N., Wang X.J., Rui W.B., Xu D.F., Zhu Y. Overexpression of DDR1 Promotes Migration, Invasion, Though EMT-Related Molecule Expression and COL4A1/DDR1/MMP-2 Signaling Axis. Technol. Cancer Res. Treat. 2020;19:1533033820973277. doi: 10.1177/1533033820973277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Jeitany M., Leroy C., Tosti P., Lafitte M., Le Guet J., Simon V., Bonenfant D., Robert B., Grillet F., Mollevi C., et al. Inhibition of DDR1-BCR signalling by nilotinib as a new therapeutic strategy for metastatic colorectal cancer. EMBO Mol. Med. 2018;10:e7918. doi: 10.15252/emmm.201707918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Henriet E., Sala M., Abou Hammoud A., Tuariihionoa A., Di Martino J., Ros M., Saltel F. Multitasking discoidin domain receptors are involved in several and specific hallmarks of cancer. Cell Adhes. Migr. 2018;12:363–377. doi: 10.1080/19336918.2018.1465156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Lu Q.-P., Chen W.-D., Peng J.-R., Xu Y.-D., Cai Q., Feng G.-K., Ding K., Zhu X.-F., Guan Z. Antitumor activity of 7RH, a discoidin domain receptor 1 inhibitor, alone or in combination with dasatinib exhibits antitumor effects in nasopharyngeal carcinoma cells. Oncol. Lett. 2016;12:3598–3608. doi: 10.3892/ol.2016.5088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Alhalabi O.T., Fletcher M.N.C., Hielscher T., Kessler T., Lokumcu T., Baumgartner U., Wittmann E., Schlue S., Goettmann M., Rahman S., et al. A novel patient stratification strategy to enhance the therapeutic efficacy of dasatinib in glioblastoma. Neuro-Oncology. 2022;24:39–51. doi: 10.1093/neuonc/noab158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Araujo J.C., Poblenz A., Corn P.G., Parikh N.U., Starbuck M.W., Thompson J.T., Lee F., Logothetis C.J., Darnay B.G. Dasatinib inhibits both osteoclast activation and prostate cancer PC-3 cell-induced osteoclast formation. Cancer Biol. Ther. 2009;8:2153–2159. doi: 10.4161/cbt.8.22.9770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Johnson F.M., Saigal B., Talpaz M., Donato N.J. Dasatinib (BMS-354825) tyrosine kinase inhibitor suppresses invasion and induces cell cycle arrest and apoptosis of head and neck squamous cell carcinoma and non-small cell lung cancer cells. Pt 1Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2005;11:6924–6932. doi: 10.1158/1078-0432.CCR-05-0757. [DOI] [PubMed] [Google Scholar]
- 222.Kurashige J., Hasegawa T., Niida A., Sugimachi K., Deng N., Mima K., Uchi R., Sawada G., Takahashi Y., Eguchi H., et al. Integrated Molecular Profiling of Human Gastric Cancer Identifies DDR2 as a Potential Regulator of Peritoneal Dissemination. Sci. Rep. 2016;6:22371. doi: 10.1038/srep22371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Somlo G., Atzori F., Strauss L.C., Geese W.J., Specht J.M., Gradishar W.J., Rybicki A., Sy O., Vahdat L.T., Cortes J. Dasatinib plus Capecitabine for Advanced Breast Cancer: Safety and Efficacy in Phase I Study CA180004. Clin. Cancer Res. 2013;19:1884–1893. doi: 10.1158/1078-0432.CCR-12-0652. [DOI] [PubMed] [Google Scholar]
- 224.Ohashi K., Pao W. A New Target for Therapy in Squamous Cell Carcinoma of the Lung. Cancer Discov. 2011;1:23–24. doi: 10.1158/2159-8274.CD-11-0069. [DOI] [PubMed] [Google Scholar]
- 225.Leroy C., Robert B., Simon V., Roche S. The Abl tyrosine kinase inhibitor Nilotinib inhibits invasive properties of colon cancer cells by targeting the discoidin domain receptor 1. EJC Suppl. 2010;8:113. doi: 10.1016/S1359-6349(10)71243-X. [DOI] [Google Scholar]
- 226.Sirvent A., Lafitte M., Roche S. DDR1 inhibition as a new therapeutic strategy for colorectal cancer. Mol. Cell. Oncol. 2018;5:e1465882. doi: 10.1080/23723556.2018.1465882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Ahmed N., Vengalasetti Y., Haslam A., Prasad V. Association of Adjuvant or Metastatic Setting with Discontinuation of Cancer Drugs in Clinical Trials. Jama Netw. Open. 2022;5:e2212327. doi: 10.1001/jamanetworkopen.2022.12327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Italiano A. Next questions for the medical treatment of gastrointestinal stromal tumor. Curr. Opin. Oncol. 2022;34:348–353. doi: 10.1097/CCO.0000000000000845. [DOI] [PubMed] [Google Scholar]
- 229.Nazzal M., Sur S., Steele R., Khatun M., Patra T., Phillips N., Long J., Ray R., Ray R.B. Establishment of a Patient-Derived Xenograft Tumor from Hepatitis C-Associated Liver Cancer and Evaluation of Imatinib Treatment Efficacy. Hepatology. 2020;72:379–388. doi: 10.1002/hep.31298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Puri S., Kaur G., Piplani H., Sanyal S.N., Vaish V. Imatinib modulates pro-inflammatory microenvironment with angiostatic effects in experimental lung carcinogenesis. Inflammopharmacology. 2020;28:231–252. doi: 10.1007/s10787-019-00656-8. [DOI] [PubMed] [Google Scholar]
- 231.Copland M., Slade D., McIlroy G., Horne G., Byrne J.L., Rothwell K., Brock K., De Lavallade H., Craddock C., Clark R.E., et al. Ponatinib with fludarabine, cytarabine, idarubicin, and granulocyte colony-stimulating factor chemotherapy for patients with blast-phase chronic myeloid leukaemia (MATCHPOINT): A single-arm, multicentre, phase 1/2 trial. Lancet Haematol. 2022;9:E121–E132. doi: 10.1016/S2352-3026(21)00370-7. [DOI] [PubMed] [Google Scholar]
- 232.Canning P., Tan L., Chu K., Lee S.W., Gray N.S., Bullock A.N. Structural Mechanisms Determining Inhibition of the Collagen Receptor DDR1 by Selective and Multi-Targeted Type II Kinase Inhibitors. J. Mol. Biol. 2014;426:2457–2470. doi: 10.1016/j.jmb.2014.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Tao Y., Wang R., Lai Q., Wu M., Wang Y., Jiang X., Zeng L., Zhou S., Li Z., Yang T., et al. Targeting of DDR1 with antibody-drug conjugates has antitumor effects in a mouse model of colon carcinoma. Mol. Oncol. 2019;13:1855–1873. doi: 10.1002/1878-0261.12520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Grither W.R., Longmore G.D. Inhibition of tumor-microenvironment interaction and tumor invasion by small-molecule allosteric inhibitor of DDR2 extracellular domain. Proc. Natl. Acad. Sci. USA. 2018;115:E7786–E7794. doi: 10.1073/pnas.1805020115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Rammal H., Saby C., Magnien K., Van-Gulick L., Gamotel P., Buache E., El Btaouri H., Jeannesson P., Morjani H. Discoidin Domain Receptors: Potential Actors and Targets in Cancer. Front. Pharmacol. 2016;7:55. doi: 10.3389/fphar.2016.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Fowler A.J., Hebron M., Balaraman K., Shi W., Missner A.A., Greenzaid J.D., Chiu T.L., Ullman C., Weatherdon E., Duka V., et al. Discoidin Domain Receptor 1 is a therapeutic target for neurodegenerative diseases. Hum. Mol. Genet. 2020;29:2882–2898. doi: 10.1093/hmg/ddaa177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Fowler A.J., Hebron M., Missner A.A., Wang R., Gao X., Kurd-Misto B.T., Liu X., Moussa C.E.H. Multikinase Abl/DDR/Src Inhibition Produces Optimal Effects for Tyrosine Kinase Inhibition in Neurodegeneration. Drugs R D. 2019;19:149–166. doi: 10.1007/s40268-019-0266-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Richters A., Nguyen H.D., Trang P., Simard J.R., Gruetter C., Engel J., Rauh D. Identification of Type II and III DDR2 Inhibitors. J. Med. Chem. 2014;57:4252–4262. doi: 10.1021/jm500167q. [DOI] [PubMed] [Google Scholar]
- 239.Dai W., Liu S., Wang S., Zhao L., Yang X., Zhou J., Wang Y., Zhang J., Zhang P., Ding K., et al. Activation of transmembrane receptor tyrosine kinase DDR1-STAT3 cascade by extracellular matrix remodeling promotes liver metastatic colonization in uveal melanoma. Signal Transduct. Target. Ther. 2021;6:176. doi: 10.1038/s41392-021-00563-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Yao J., Li G., Jiao Y., Zheng Y., Liu Y., Wang G., Zhou L., Zhang H., Zhang X., Shuai J., et al. Biological gel-based microchamber array for tumor cell proliferation and migration studies in well-controlled biochemical gradients. Lab Chip. 2021;21:3004–3018. doi: 10.1039/D0LC00951B. [DOI] [PubMed] [Google Scholar]
- 241.Aguilera K.Y., Huang H., Du W., Hagopian M.M., Wang Z., Hinz S., Hwang T.H., Wang H., Fleming J.B., Castrillon D.H., et al. Inhibition of Discoidin Domain Receptor 1 Reduces Collagen-mediated Tumorigenicity in Pancreatic Ductal Adenocarcinoma. Mol. Cancer Ther. 2017;16:2473–2485. doi: 10.1158/1535-7163.MCT-16-0834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Shariati M., Evans K.W., Zheng X., Bristow C.A., Ng P.K.-S., Rizvi Y.Q., Tapia C., Yang F., Carugo A., Heffernan T.P., et al. Combined inhibition of DDR1 and CDK4/6 induces synergistic effects in ER-positive, HER2-negative breast cancer with PIK3CA/AKT1 mutations. Oncogene. 2021;40:4425–4439. doi: 10.1038/s41388-021-01819-0. [DOI] [PubMed] [Google Scholar]
- 243.Wei Z.-W., Zhang C.-H., He Y. 7rh, a novel selective discoidin domain receptor 1 (DDR1) inhibitor, enhances 5-fluorouracil response in gastric cancer. Ann. Oncol. 2017;28:iii18. doi: 10.1093/annonc/mdx261.017. [DOI] [Google Scholar]
- 244.de Moura C.R., Battistella M., Sohail A., Caudron A., Feugeas J.P., Podgorniak M.-P., Pages C., Dorval S.M., Marco O., Menashi S., et al. Discoidin domain receptors: A promising target in melanoma. Pigment Cell Melanoma Res. 2019;32:697–707. doi: 10.1111/pcmr.12809. [DOI] [PubMed] [Google Scholar]
- 245.Romayor I., Badiola I., Benedicto A., Marquez J., Herrero A., Arteta B., Olaso E. Silencing of sinusoidal DDR1 reduces murine liver metastasis by colon carcinoma. Sci. Rep. 2020;10:18398. doi: 10.1038/s41598-020-75395-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Kim H.-G., Tan L., Weisberg E.L., Liu F., Canning P., Choi H.G., Ezell S.A., Wu H., Zhao Z., Wang J., et al. Discovery of a Potent and Selective DDR1 Receptor Tyrosine Kinase Inhibitor. ACS Chem. Biol. 2013;8:2145–2150. doi: 10.1021/cb400430t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Li T., Zhang H., Wang Z., Gao S., Zhang X., Zhu H., Wang N., Li H. The regulation of autophagy by the miR-199a-5p/p62 axis was a potential mechanism of small cell lung cancer cisplatin resistance. Cancer Cell Int. 2022;22:120. doi: 10.1186/s12935-022-02505-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Yang X., Zheng Y., Tan J., Tian R., Shen P., Cai W., Liao H. MiR-199a-5p-HIF-1 alpha-STAT3 Positive Feedback Loop Contributes to the Progression of Non-Small Cell Lung Cancer. Front. Cell Dev. Biol. 2021;8:620615. doi: 10.3389/fcell.2020.620615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Hu Y., Liu J., Jiang B., Chen J., Fu Z., Bai F., Jiang J., Tang Z. MiR-199a-5p Loss Up-Regulated DDR1 Aggravated Colorectal Cancer by Activating Epithelial-to-Mesenchymal Transition Related Signaling. Digest. Dis. Sci. 2014;59:2163–2172. doi: 10.1007/s10620-014-3136-0. [DOI] [PubMed] [Google Scholar]
- 250.Krazinski B.E., Kiewisz J., Sliwinska-Jewsiewicka A., Kowalczyk A.E., Grzegrzolka J., Godlewski J., Kwiatkowski P., Dziegiel P., Kmiec Z. Altered Expression of DDR1 in Clear Cell Renal Cell Carcinoma Correlates With miR-199a/b-5p and Patients’ Outcome. Cancer Genom. Proteom. 2019;16:179–193. doi: 10.21873/cgp.20124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Ilbeigi S., Naeimzadeh Y., Davoodabadi Farahani M., Rafi Monjezi M., Dastsooz H., Daraei A., Farahani F., Dastgheib A., Mansoori Y., Tabei S.M.B. Clinical values of two estrogen receptor signaling targeted lncRNAs in invasive ductal breast carcinoma. Klin. Onkol. Cas. Ces. A Slov. Onkol. Spol. 2021;34:382–391. doi: 10.48095/ccko2021382. [DOI] [PubMed] [Google Scholar]
- 252.Najafi M., Farhood B., Mortezaee K. Extracellular matrix (ECM) stiffness and degradation as cancer drivers. J. Cell. Biochem. 2019;120:2782–2790. doi: 10.1002/jcb.27681. [DOI] [PubMed] [Google Scholar]
- 253.Li G., Tao T., Deng D., Zhang S., Chao Y., Dai Y., Li Y., Tao R., Yuan S., Liu Z., et al. Collagen-targeted tumor-specific transepithelial penetration enhancer mediated intravesical chemoimmunotherapy for non-muscle-invasive bladder cancer. Biomaterials. 2022;283:121422. doi: 10.1016/j.biomaterials.2022.121422. [DOI] [PubMed] [Google Scholar]
- 254.Chauhan V.P., Martin J.D., Liu H., Lacorre D.A., Jain S.R., Kozin S.V., Stylianopoulos T., Mousa A.S., Han X.X., Adstamongkonkul P., et al. Angiotensin inhibition enhances drug delivery and potentiates chemotherapy by decompressing tumour blood vessels. Nat. Commun. 2013;4:2516. doi: 10.1038/ncomms3516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Kasi A., Allen J., Mehta K., Dandawate P., Saha S., Bossmann S., Anant S., Sun W. Association of losartan with outcomes in metastatic pancreatic cancer patients treated with chemotherapy. J. Clin. Transl. Res. 2021;7:257–262. [PMC free article] [PubMed] [Google Scholar]
- 256.Zhao Y., Cao J., Melamed A., Worley M., Gockley A., Jones D., Nia H.T., Zhang Y., Stylianopoulos T., Kumar A.S., et al. Losartan treatment enhances chemotherapy efficacy and reduces ascites in ovarian cancer models by normalizing the tumor stroma. Proc. Natl. Acad. Sci. USA. 2019;116:2210–2219. doi: 10.1073/pnas.1818357116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Cardinale D., Sandri M.T., Colombo A., Salvatici M., Tedeschi I., Bacchiani G., Beggiato M., Meroni C.A., Civelli M., Lamantia G., et al. Prevention of Atrial Fibrillation in High-risk Patients Undergoing Lung Cancer Surgery the PRESAGE Trial. Ann. Surg. 2016;264:244–251. doi: 10.1097/SLA.0000000000001626. [DOI] [PubMed] [Google Scholar]
- 258.Choi C.H., Park Y.-A., Choi J.-J., Song T., Song S.Y., Lee Y.-Y., Lee J.-W., Kim T.-J., Kim B.-G., Bae D.-S. Angiotensin II type I receptor and miR-155 in endometrial cancers: Synergistic antiproliferative effects of anti-miR-155 and losartan on endometrial cancer cells. Gynecol. Oncol. 2012;126:124–131. doi: 10.1016/j.ygyno.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 259.Hashemzehi M., Rahmani F., Khoshakhlagh M., Avan A., Asgharzadeh F., Barneh F., Moradi-Marjaneh R., Soleimani A., Fiuji H., Ferns G.A., et al. Angiotensin Receptor Blocker Losartan Inhibits Tumor Growth of Colorectal Cancer. EXCLI J. 2021;20:506–521. doi: 10.17179/excli2020-3083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Yazdannejat H., Hosseinimehr S.J., Ghasemi A., Pourfallah T.A., Rafiei A. Losartan sensitizes selectively prostate cancer cell to ionizing radiation. Cell. Mol. Biol. 2016;62:30–33. [PubMed] [Google Scholar]
- 261.Zhao Q., He X., Qin X., Liu Y., Jiang H., Wang J., Wu S., Zhou R., Yu C., Liu S., et al. Enhanced Therapeutic Efficacy of Combining Losartan and Chemo-Immunotherapy for Triple Negative Breast Cancer. Front. Immunol. 2022;13:938439. doi: 10.3389/fimmu.2022.938439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Miwa S., Yamamoto N., Hayashi K., Takeuchi A., Igarashi K., Tsuchiya H. Therapeutic Targets and Emerging Treatments in Advanced Chondrosarcoma. Int. J. Mol. Sci. 2022;23:1096. doi: 10.3390/ijms23031096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Romanchikova N., Trapencieris P., Zemitis J., Turks M. A novel matrix metalloproteinase-2 inhibitor triazolylmethyl aziridine reduces melanoma cell invasion, angiogenesis and targets ERK1/2 phosphorylation. J. Enzym. Inhib. Med. Chem. 2014;29:765–772. doi: 10.3109/14756366.2013.855207. [DOI] [PubMed] [Google Scholar]