Abstract
The coronavirus disease 2019 caused by the Severe Acute Respiratory Syndrome Coronavirus-2 has resulted in many confirmed cases around the world. Sars-CoV-2 remains viable and infectious in aerosols dispersed in air and is viable on surfaces up to several days. Symptomatic patients are the main reservoir for transmission. Evidence suggests that asymptomatic patients and patients during their incubation period can shed and transmit Sars-CoV-2. The infective potential can be reduced through the use of personal protective equipment. Healthcare professionals especially the oral maxillofacial surgeons are at increased risk of being infected by the virus. Oral maxillofacial injuries typically involve vital structures in the upper aerodigestive tract and are emergent. Facial trauma surgery cannot be delayed or deferred in a pandemic. This review focuses on precautions surgeons should adopt while managing facial trauma patients in the emergency department and whilst performing emergency surgeries on these patients during the current COVID-19 pandemic. Strict and effective infection control protocols for facial trauma management are needed to minimise this risk of transmission. This review was part of the lecture given by Professor Melvyn Yeoh at the 14th Asian congress on Oral and Maxillofacial Surgery recently held virtually in Singapore due to the pandemic.
Keywords: COVID-19, SARS-CoV-2, Maxillofacial trauma, Precautions
1. Introduction
Coronavirus are enveloped non segmented positive-sense RNA viruses belonging to the family Coronaviridae and the order Nidovirales. They are broadly distributed in humans and other mammals. The coronavirus disease 2019 originating in Wuhan was declared a global pandemic by WHO on March 9, 2020 [1], [2].
Patients who are COVID-19 positive are the main source of infection. They are especially infectious during the incubation period which is 1–14 days after being infected. The person to person transmission routes of 2019-nCoV include direct aerosolisation transmission through coughing, sneezing, droplet inhalation and also through contact transmission such as contact with oral, nasal and eye mucous membranes. Infection control measures are necessary to prevent the virus from being further disseminated [3], [4].
The oral maxillofacial surgeon normally comes into contact with the patient’s oral cavity, airway and secretions during the diagnosis and treatment processes. It puts them in situations of high risk of contracting the infection and subsequently becoming the source of contagion [5], [6].
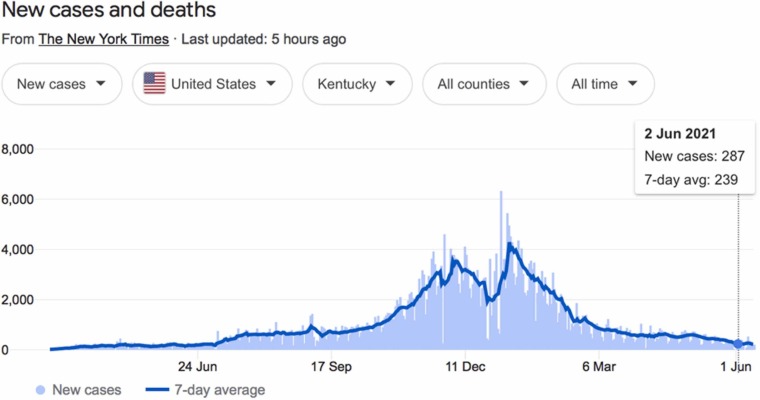
In the state of Kentucky, infection rates are over 460,000 people since the start of Covid 19 pandemic with positivity rates being greater than 12% at the peak. Elective surgeries were halted by Governor of Kentucky for two months from March to May of 2020. Surgeries and provision of Oral and Maxillofacial surgery care and resources were greatly impaired (See Fig. 1). At this time of writing, the United States is emerging from the crisis and resuming normal clinical service and productivity [7]. Yet elsewhere in the World especially in Asia; with certain countries such as Taiwan, India and Singapore, they are entering a resurgence of the pandemic. Literature on precautions in dental care in the COVID-19 pandemic is plenty [4], [8], [9]. This has been reviewed by Ng et al. [10].
Fig. 1.
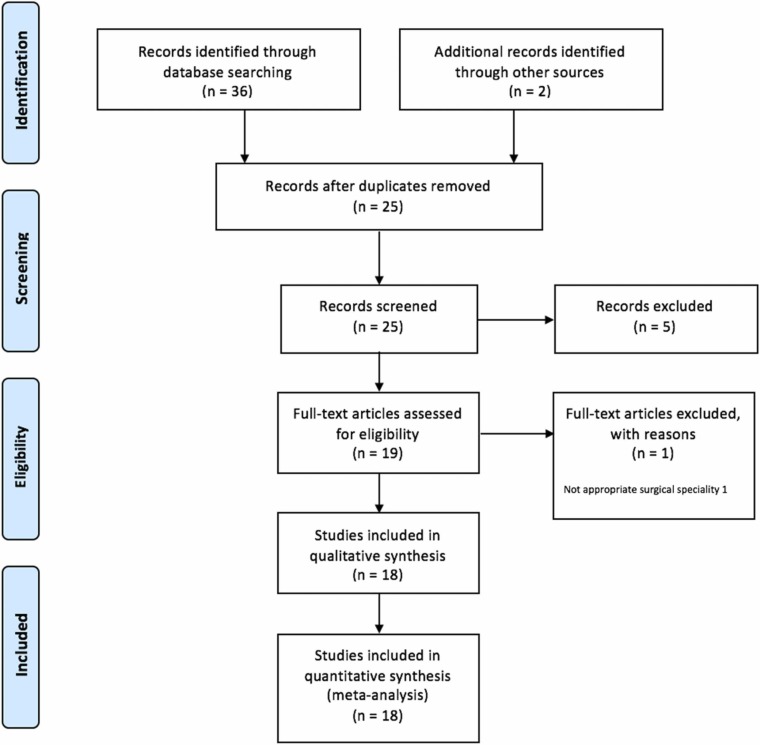
The PRISMA flow diagram of results of database literature searching.
Source: https://www.nytimes.com/interactive/2021/us/kentucky-covid-cases.html.
The aim of this work is to present an overview of current prevailing protocols to streamline triage, precautions to care for facial trauma patients whilst minimising the risks of infection to the providers and patients. Employment of such protocol had ensured zero transmission in the Division of Oral and Maxillofacial Surgery in the University of Kentucky during the time March 18 to May 6, 2020 when there were restrictions [7].
2. Materials and methods
All published articles and guidelines were searched from Pubmed, Google Scholar, Cochrane, Embase and all peer-reviewed articles were sought. Multiple search terms were employed. These search terms included facial trauma, COVID-19, Sar-CoV-2 guidelines, precautions, personal protective equipment, aerosolization and oral maxillofacial trauma. This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [11] (See Fig. 2). The Newcastle-Ottawa Scale was used for the appraisal of the methodological quality of the guidelines included. The authors independently collected the descriptive data for each included articles and guidelines. The study quality was assessed by categorising it into three dimensions: selection, comparability, outcome and applicability. A star system was used as a semi quantitative assessment of the study quality. A study was awarded a maximum of one star for each numbered item within the selection and exposure categories. A maximum of two stars were awarded for comparability. The number of stars ranged from zero to nine (high-quality, ≥7 stars; medium-quality, 4–6 stars; poor-quality, < 4 stars) [12] (See Table 1). A summary of current published guidelines in the literature were tabulated in the following paragraphs (See Table 2).
Fig. 2.
The Covid 19 situation at that the time where this protocol was applied and that transmission to the Department of Oral Maxillofacial Surgery was none.
Source: The New York Times https://www.nytimes.com/interactive/2021/us/kentucky-covid-cases.html.
Table 1.
Risk of bias assessment using Newcastle-Ottawa score.
| Study | Selection | Comparability | Outcome | Overall star rating |
|---|---|---|---|---|
| Abramowicz S | **** | * | * | 7 |
| Alterman M | **** | * | * | 7 |
| Barca I | **** | * | ** | 7 |
| Barca I | *** | ** | * | 6 |
| Blackhall KK | *** | * | * | 6 |
| DeSerres JJ | **** | ** | ** | 8 |
| Grant M | **** | ** | ** | 8 |
| Ghai S | **** | ** | ** | 8 |
| Holmes S | **** | ** | ** | 8 |
| Hsieh T | *** | ** | ** | 7 |
| Myatra SN | **** | ** | ** | 8 |
| Panesar K | **** | ** | ** | 8 |
| Parker Hu | *** | ** | ** | 7 |
| Piombino P | *** | ** | * | 6 |
| Siad M | *** | ** | * | 6 |
| Selvaraj DSS | **** | ** | * | 7 |
| Ye MJ | *** | ** | ** | 7 |
| Zhang T | **** | ** | ** | 8 |
A star system was used to allow a semi quantitative assessment of study quality. A study was awarded a maximum of one star for each numbered item within the selection and exposure categories. A maximum of two stars were awarded for comparability. The NOS ranges from zero to nine stars. We considered high-quality studies as those that received seven or more stars, medium quality studies those with four to six stars, and poor quality studies those with fewer than four stars.
Table 2.
All available recommendations at the time of study.
| Author | Publication | Recommendations |
|---|---|---|
| Abramowicz S | Management of paediatric facial fractures during COVID-19 pandemic Oral Surg Oral Med Oral Path Oral Radiol 2021; 17: in press. |
Non-surgical intervention preferred Decrease operating time |
| Alterman M | The efficacy of a protective protocol for oral and maxillofacial surgery procedures in a COVID-19 pandemic area – results from 1471 patients Clin Oral Investig 2021; 25: 5001–5008. |
Protective protocol may assist oral surgeons in continuing dental services in a safe manner |
| Barca I | Management in oral and maxillofacial surgery during the COVID-19 pandemic: our experience Br J Oral Maxillofac Surg 2020; 58: 687–691. |
Repetition of triage Preoperative testing 48 h prior to surgery Single hospital room accommodation Swift execution of preoperative preparation and plan |
| Barca I | Telemedicine in Oral and Maxillofacial surgery: an effective alternative in post COVID-19 pandemic Int J Environ Res Public Health 2020; 17: 7365. |
Telemedicine usage in triage |
| Blackhall KK | Provision of emergency maxillofacial service during the COVID-19 pandemic: a collaborative five centre UK study Br J Oral Maxillofac Surg 2020; 58: 698–703. |
Remote consultation Limit direct patient contact |
| DeSerres JJ | Best practices guidelines for the management of acute craniomaxillofacial trauma during the COVID-19 pandemic J Craniofac Surg 2020; 31: e626-e630. |
Emergent CMF injuries Urgent CMF injuries Algorithm for management of CMF trauma |
| Grant M | AO CMF international task force recommendations on best practices for maxillofacial procedures during COVID-19 pandemic 2020. Available at http://aocmf3.aofoundation | Surgical considerations Fracture location specific considerations Closed reduction with self-drilling MMF screws where possible in mandibular fracture |
| Ghai S | Facial trauma management during the COVID-19 era: a primer for surgeons Curr Med Res Pract 2020; 10: 169–173. |
Site specific management of facial trauma as conservative as possible |
| Holmes S | Toward a consensus view in the management of acute facial injuries during the Covid-19 pandemic Br J Oral Maxillofac Surg 2020; 58: 571–576. |
Stratification of facial fracture patterns Planning of surgical protocols |
| Hu P | Early comprehensive testing for COVID-19 is essential to protect trauma centres J Trauma Acute Care Surg 2020; 89: 698–702. |
Trauma Bay PPE requirement Staff exposure and testing |
| Hsieh TY | A guide to facial trauma triage and precautions in the COVID-19 Pandemic Fac Plast Surg Aesth Med 2020; 22: 164–169. |
Enhanced airway precaution Extreme airway precaution Fracture location specific considerations |
| Myatra SN | Anesthesia for oral surgeries during the COVID-19 pandemic J Anaesthesiol Clin Pharmacol 2020; 36: S96-S104. |
Operating room preparation |
| Panesar K | Evolution of COVID-19 guidelines for University of Washington Oral and Maxillofacial surgery patient care J Oral Maxillofac Surg 2020; 78:1136–1146. |
Preoperative testing Mask types PPE stewardship Surgical scheduling Education and training |
| Piombino P | Guidelines and recommendations for patient management, surgical activities and safety in the maxillofacial unit and head and neck department during COVID-19 pandemic J Craniofac Surg 2020; 31: e630-e633. |
Telephone triage First visit and checks Inpatient management |
| Said M | Navigating telemedicine for facial trauma during the COVID-19 pandemic Laryngoscope Investig Otolaryngol 2020; 5: 649–656. |
Facial trauma follow-up with telemedicine |
| Selvaraj DSS | Conservative approach for treatment of isolated mandibular fractures, the adaptations during COVID 19 pandemic J Maxillofac Oral Surg 2021; 3:1–7. |
IMF, arch bars and wires when resources are limited |
| Ye MJ | Aerosol and droplet generation from mandible and midface fixation: surgical risk in the pandemic Am J Otolaryngol 2021; 42: 102829. |
Significant increases in aerosolized particles were recorded after electrocautery and during powered drilling. |
| Zhang T | Instructions for management of oral and maxillofacial trauma during prevention and control stage of the novel coronavirus Chin J Oral Maxillofac Surg 2020; 2: 100–104. |
Perioperative management of the maxillofacial trauma patient |
2.1. Facial trauma and triage
During the pandemic and the lockdown, every patient whom arrived in the emergency department for any complaint was assumed to be positive for COVID-19. When a facial trauma patient arrived in the emergency department, every precaution was undertaken to ensure the prevention of the infection to the surgeon on call and all other healthcare provider. The oral and maxillofacial surgery residents and the attending staff wore personal protective equipment (PPE). Teleconsulting, tele-triaging was preferred where possible to prevent unnecessary exposure of the scarce healthcare providers especially oral and maxillofacial surgeons and to avoid the unnecessary quarantine of the oral and maxillofacial surgeons already working in teams [13].
In cases of major facial injuries where physical examination of the facial trauma by the surgeon becomes imperative, the availability of the PPE for the facial trauma surgeon becomes essential. The examination of the patient by the surgeon involves close proximity with the patient. The upper aerodigestive tract carries a high viral load of Sar-CoV-2 and extreme precaution is needed. The surgeon’s familiarity with the proper donning and doffing technique in PPE kits is essential and this has been reviewed [14], [15].
2.2. Triaged patient categories
In general, patients are triaged in unknown or positive COVID-19 status. Since there is a high risks of transmission in the management of facial trauma owing to the high viral load in the oral cavity and naso-oropharyngeal region, triaging the patients to decide the type of personal protective equipment and treatment plays key role in the current pandemic.
Patients are triaged into the emergent and urgent (non-emergent) case categories based upon their injuries. In the emergent cases, there is usually no opportunity to clarify the COVID-19 status prior to the start of the case. Emergent patients include patients with imminent compromise of vision, airway or uncontrollable bleeding, combined intracranial and upper facial injuries necessitating craniotomy as well as composite extensive soft and bony injuries requiring debridement, bony stabilisation and soft tissue coverage to prevent infection (See Table 3, for review see DeSerres et al.) [16]. In the urgent cases where the patients are more stable, rapid antigen testing or PCR test must be obtained prior to operating room (OR).
Table 3.
Patient categories of emergent facial trauma vs urgent facial trauma.
| Emergent Facial Trauma | Unstable facial fracture with airway compromise Vascular compromisation Open fractures with exposed brain Extensive soft tissue injuries Ocular injuries (Treated as Covid-19 positive in negative pressure operating theatres and PAPR donned) |
| Urgent Facial Trauma | Unstable fracture with malocclusion Facial fractures with muscle and/or bony impingement Large complex open facial fracture Open fractures and facial lacerations (2 PCR or rapid antigen tests 48 h prior to OR) |
During surgery of the emergent cases where the COVID-19 status is unknown or if the patient is positive, only absolutely required persons are allowed in the theatre. All operators should don the required or appropriate PPE, double gloves and perform hand hygiene. Powered Air Purifying Respirator (PAPR) is worn in emergent cases. Filtering facepiece FFP3 mask with visors or goggles should be worn [14], [15], [16].
2.3. Procedure specific requirements
All surgical procedures should be streamlined and pre-planned before the OR. Team huddle should be carried out to allow clear communication of the surgical plan. The number and types of surgical equipment should be reduced. The types of surgical equipment used should minimise aerosolization. The intubation for general anaesthesia should be performed by an experienced doctor (a consultant or attending) to avoid unneeded exposure to patient’s oral fluid and secretions and the generation of aerosols during the endotracheal intubation procedure. The intubation and extubation should be carried in a negative pressure environment. The majority of the operating rooms are positive pressure environments and thus many of the intubation and extubation are carried outside the OR. The patient is then transferred to the OR with care and with minimal cross-overs and possible transmission [17], [18].
Preoperative and post-operative use of mouthrinse containing 1 % hydrogen peroxide or 0.2 % povidine is encouraged. Studies have shown the povidine iodine reduces the number of droplets and aerosol produced during oral operations [19].
The principles of the simplification of surgery should also be adopted to reduce operating times in the theatre. In Kentucky, other procedural modifications were included (See Table 3). Examples include the use of transcutaneous approach over open mucosal incision where possible. Scalpels are used over mono-cautery and bipolar cautery on lower power for haemostasis or coagulation. Other suggestions employed have been included in AO CMF protocols. These included lower speed drilling with minimal irrigation, osteotomies for osteotomizing older fractures instead of the power saw. (See Table 4, for review see Grant et al.) [20].
Table 4.
Facial trauma management principles in COVID-19 pandemic.
| Assessment Apply simplification Treat as conservatively as possible Closed procedures where possible Teleconsultation and safe imaging and preparation of patients Covid-19 status testing (2 tests separated by 24 h) Cleared route to operating room |
| Peri-procedural Team huddle prior to OR Preoperative povidone iodine swish and spit Transcutaneous or Percutaneous where possible Avoidance of mucosal incisions Scalpel over monopolar for incision Closed reduction and MMF where possible Self-drilling screws and battery powered instrumentation Minimize drilling Consider osteotomies Avoid repeating and irrigation where possible As short as possible theatre time as possible Extubation in PACU or ICU Minimize armamentarium OR runners not allowed in the OR |
| Post-procedural Patient isolation in the wards Reduced hospitalisation where possible Telemedicine and remote patient review or recall Absorbable used where possible |
2.4. Post trauma surgery care
All patients should be followed up as preventive measures allow. Patients should have reduced hospitalisation where possible. Emergent facial trauma injuries should be treated within 24 h. Urgent facial trauma cases should have appropriate segregation and treated when opportunity allows and to shorten hospital stay where possible. Covid-19 positive cases should be segregated or managed in designated wards with ventilation [14], [15], [16], [17], [18].
Conservatively-managed patients may be even allowed telemedicine follow-up reviews. This has been proven effective in some centres [13], [21], [22].
3. Discussion
Facial trauma surgery involves the nasopharyngeal and oropharyngeal regions; these are the sites where the virus SARS-CoV-2 is found in high concentrations. The surgical site itself may also be contaminated. COVID-19 infection spreads via droplet infection but it can also spread through aerosols and droplets of contaminated fluids [19], [23].
The WHO recommends airborne precautions for circumstances and settings in which aerosol generating procedures are performed. Airborne transmission may be possible during common procedure done during treatment i.e. endotracheal intubation, open suction, manual ventilation, tracheostomy, manipulation and fixation [24], [25], [26].
Although most of the facial trauma occurs due to road traffic accidents and sports injuries that have reduced due to the COVID-19 pandemic. Current epidemiology studies showed the continued presence of both emergent and urgent facial trauma injuries. This was not abated by the safe distancing measures put in place by countries and governments [27], [28], [29], [30].
It is possible that the World may take some time to emerge from the crisis as different parts of the world go through resurgences while other parts are emerging. A review of current adaptation and protocol in facial trauma management is thus pertinent and crucial. Our current review showed that there were numerous guidelines available and the present review is the first to review all of the available published guidelines on facial trauma management in the COVID-19 pandemic.
4. Conclusion
The current COVID-19 pandemic has taken a toll on the medical fraternity especially the oral maxillofacial surgeons in the provision of care. There is a high risk of cross-infection in management of facial trauma due to the high viral load in the oral cavity and nasopharyngeal region.
Changes and adjustments to current practice already being used on oral maxillofacial surgery, can help in a preventive way to provide best possible care to the facial trauma patients. From all currently available recommendations, oral maxillofacial surgeons around the world can make use of the guidance to assess the risk at triage, ensure both patient and healthcare professional’s safety, preserve available resources, adopt efficiencies and apply current universal precautions to the pandemic.
Declaration of Competing of interest
We have no conflicts of interests to declare.
Acknowledgements
This review article received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Ksiazek T.G., Erdman D., Goldsmith C.S., Zaki S.R., Peret T., Emery S., et al. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med. 2003;348:1953–1966. doi: 10.1056/NEJMoa030781. [DOI] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 4.Ren Y., Feng C., Rasubala L., Malmstrom H., Eliav E. Risk for dental healthcare professionals during the COVID-19 global pandemic: an evidence-based assessment. J Dent. 2020;101 doi: 10.1016/j.jdent.2020.103434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li H., Wang Y., Ji M., Pei F., Zhao Q., Zhou Y., et al. Transmission routes analysis of SARS-CoV-2: a systematic review and case report. Front Cell Dev Biol. 2020;8:618. doi: 10.3389/fcell.2020.00618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The New York Times. Tracking coronavirus in Kentucky: latest map and case count, 2 June 2021. Available: 〈https://www.nytimes.com/interactive/2021/us/kentucky-covid-cases.html〉 Accessed on 13 June 2021.
- 8.Ather A., Patel B., Ruparel N.B., Diogenes A., Hargreaves K.M. Coronavirus disease 19 (COVID-19): implications for clinical dental care. J Endod. 2020;46:584–595. doi: 10.1016/j.joen.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shi A.H., Guo W., Chng C.K., Chan B.H. Precautions when providing dental care during coronavirus disease 2019 (COVID-19) pandemic. Ann Acad Med. 2020;49:312–319. [PubMed] [Google Scholar]
- 10.Ng C.H., Tan C., Stassen L.F.A. Cornucopia and highlights of Internet resources on the web for COVID-19. Oral Health Case Rep. 2020;6:3. 〈http://www.hilarispublisher.com/open-access/cornucopia-and-highlights-of-internet-resources-on-theweb-for-covid19.pdf〉 (Available at) [Google Scholar]
- 11.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Brit Med J. 2009;339 [PMC free article] [PubMed] [Google Scholar]
- 12.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 13.Barca I., Novembre D., Giofre E., Caruso D., Cordaro R., Kallaverja E., et al. Telemedicine in oral and maxillofacial surgery: an effective alternative in post COVID-19 pandemic. Int J Environ Res Pub Health. 2020;17:7365. doi: 10.3390/ijerph17207365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zimmermann M., Nkenke E. Approaches to the management of patients in oral and maxillofacial surgery during COVID-19 pandemic. J Craniomaxillofac Surg. 2020;48:521–526. doi: 10.1016/j.jcms.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Panesar K., Dodson T., Lynch J., Bryson-Cahn C., Chew L., Dillon J. Evolution of COVID-19 guidelines for University of Washington Oral and Maxillofacial surgery patient care. J Oral Maxillofac Surg. 2020;78:1136–1146. doi: 10.1016/j.joms.2020.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DeSerres J.J., Al-Shaqsi S.Z., Antonyshyn O.M., Fialkov J.A. Best practice guidelines for the management of acute craniomaxillofacial trauma during the COVID-19 pandemic. J Craniofac Surg. 2020;31:e626–e630. doi: 10.1097/SCS.0000000000006654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jamal M., Shah M., Almarzooqi S.H., Aber H., Khawaja S., El Abed R., et al. Overview of transnational recommendations for COVID-19 transmission control in dental care settings. Oral Dis. 2021;27(Suppl 3):655–664. doi: 10.1111/odi.13431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marui V.C., Souto M.L.S., Rovai E.S., Romito G.A., Chambrone L., Pannuti C.M. Efficacy of preprocedural mouthrinses in the reduction of microorganisms in aerosol: a systematic review. J Am Dent Assoc. 2019;150:1015–1026. doi: 10.1016/j.adaj.2019.06.024. [DOI] [PubMed] [Google Scholar]
- 20.Grant M., Buchbinder D., Dodson T.B., Fusetti S., Leung M.Y.Y., Aniceto G.S., et al. AO CMF international task force recommendations on best practices for maxillofacial procedures during COVID-19 pandemic. Craniomaxillofac Trauma Reconstr. 2020;13:151–156. doi: 10.1177/1943387520948826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Robiony M., Bocin E., Sembronio S., Costa F., Bresadola V., Tel A. Redesigning the paradigms of clinical practice for oral and maxillofacial surgery in the era of lockdown for COVID-19: from tradition to telesemeiology. Int J Environ Res Public Health. 2020;17:6622. doi: 10.3390/ijerph17186622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Said M., Ngo V., Hwang J., Hom D.B. Navigating telemedicine for facial trauma during the COVID-19 pandemic. Laryngoscope Investig Otolaryngol. 2020;5:649–656. doi: 10.1002/lio2.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamedani S., Farshidfar N., Ziaei A., Pakravan H. The dilemma of COVID-19 in dental practice concerning the role of saliva in transmission: a brief review of current evidence. Eur Oral Res. 2020;54:92–100. doi: 10.26650/eor.20200050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health organization. Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations, 29 Mar 2020. Available at 〈https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations〉. Accessed on 1 October 2021.
- 25.Banakar M., Lankarani K.B., Jafarpour D., Moayedi S., Banakar M.H., Sadeghi A.M. COVID-19 transmission risk and protective protocols in dentistry: a systematic review. BMC Oral Health. 2020;20:275. doi: 10.1186/s12903-020-01270-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kathree B.A., Khan S.B., Ahmed R., Maart R., Layloo N., Asia-Michaels W. COVID-19 and its impact in the dental setting: a scoping review. PLOS One. 2020;15 doi: 10.1371/journal.pone.0244352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pabst A., Zeller A.N., Sader R., Wiegner J.U., Schneider M., Ehrenfeld M., et al. The influence of the SARS-CoV-2 pandemic on oral and maxillofacial surgery: a nationwide survey among 54 hospitals and 240 private practices in Germany. Clin Oral Investig. 2021;25:3853–3860. doi: 10.1007/s00784-020-03715-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maffia F., Fontanari M., Vellone V., Cascone P., Mercuri L.G. Impact of COVID-19 on maxillofacial surgery practice: a worldwide survey. Int J Oral Maxillofac Surg. 2020;49:827–835. doi: 10.1016/j.ijom.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Puglia F.A., Hills A., Dawoud B., Magennis P., Chiu G.A., et al. Management of oral and maxillofacial trauma during the first wave of the COVID-19 pandemic in the United Kingdom. Br J Oral Maxillofac Surg. 2021;59:867–874. doi: 10.1016/j.bjoms.2020.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Salzano G., Dell’Aversana Orabona G., Audino G., Vaira L.A., Trevisiol L., D’Agostino A., et al. Have there been any changes in the epidemiology and etiology of maxillofacial trauma during the COVID-19 Pandemic? An Italian multicentre study. J Craniofac Surg. 2020;32:1445–1447. doi: 10.1097/SCS.0000000000007253. [DOI] [PMC free article] [PubMed] [Google Scholar]