Abstract
Background
It is known that there has been an increase over the years in attacks by patients admitted to the emergency department (ED) on healthcare workers; it is unclear what effect the COVID-19 pandemic has on these attacks.
Aim
to verify through a long-term time analysis the effect of COVID-19 on ED attacks on healthcare workers.
Mothods
a quasi-experimental interrupted time-series analysis on attacks on healthcare workers was performed from January 2017 to August 2021. The main outcome was the monthly rate of attacks on healthcare workers per 1000 general accesses. The pandemic outbreak was used as an intervention point.
Results
1002 attacks on healthcare workers in the ED were recorded. The rate of monthly attacks on total accesses increased from an average of 13.5 (SD 6.6) in the pre-COVID-19 era to 27.2 (SD 9.8) in the pandemic months, p < 0.001. The pandemic outbreak led to a significant increase in attacks on healthcare workers from 0.05/1000 attacks per month (p = 0.018), to 4.3/1000 attacks per month (p = 0.005).
Conclusions
The COVID-19 pandemic has led to a significant increase in attacks on healthcare workers in the ED. Trends compared to pre-pandemic months do not seem to indicate a return to normality. Health institutions and policymakers should develop strategies to improve the safety of the working environment in hospitals and EDs.
Keywords: COVID-19, Pandemic, Healtcar workers, Aggressions, Violence, SARS-CoV-2
1. Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and its related novel Coronavirus disease 2019 (COVID-19) pandemic have become a major challenge for international public health. In this scenario, emergency departments play a key role in the early identification of infected patients requiring prompt treatment and hospitalization. The work overload due to the increased access of patients to the emergency department (ED), notoriously a stressful environment, the long work shifts, and the overwhelming psychological stress led to increased risk of fatigue, insomnia, emotional disturbances such as depression and anxiety, and burnout among healthcare personnel [1]. This situation was worsened by the increased stigmatization, intimidation, verbal and physical violence, and aggression against health personnel, which have been increasingly reported worldwide during the current pandemic [2,3]. This may reflect the negative emotional impact upon the general population exerted by the COVID-19 disruptions and restrictions of social and economic activities. The risk of violent or threatening behavior by patients and relatives is further increased by the adoption of measures to prevent and control the spread of Sars-COV-2 infection, such as quarantine and isolation [3]. Workplace violence against healthcare professionals is associated with negative consequences, including work dissatisfaction, medical errors, mental health problems, and reduced quality of patient care, and represents therefore a major public health issue [4], [5], [6], [7], [8], [9]. This has increasingly become a serious phenomenon worldwide and seems to affect personnel working in the ED more often and seriously compared with other clinical settings [10]. This could be attributed to overcrowding and long waiting times, although individual characteristics of perpetrators, such as alcohol, drug intoxication, or mental illness [11]. Several theories and frameworks have been proposed to provide an explanation of the causes and contributing factors of violence towards nurses in the emergency department which could be used to develop specific intervention strategies to effectively address this problem [12]. Specifically, an interactive model of workplace violence could arise from the interplay between characteristics of victims and perpetrators, as well as individual and workplace risk factors [12].
A recent comprehensive search of the literature (conducted in MEDLINE accessed through PubMed using the search strategy reported in the appendix on July 22, 2022) identified 78 articles on workplace violence during the COVID-19 pandemic. However, only few investigated the occupational violence against healthcare personnel in the ED before and during the pandemic [13], [14], [15], and only one has evaluated the temporal trend of this type of violence using a quantitative approach [13], [14], [15].
In this study, we aimed at evaluating whether and to what extent the outbreak of the COVID-19 pandemic has worsened the workplace violence against healthcare personnel in the emergency department.
2. Methods
2.1. Study design and setting
We conducted a single-center, retrospective observational study performing a quasi-experimental interrupted time-series analysis on all cases of workplace violence against health personnel that occurred at the Emergency Department (ED) of the general hospital of Merano (South Tyrol, Italy). This hospital is located in an Alpine region of Northern Italy and serves a vast mountainous area with more than 100,000 inhabitants and more than 2.5 million tourist nights spent annually. The ED of Merano Hospital had an average patient volume of 70,000 accesses per year before the COVID-19 pandemic. It is equipped with a security service continuously available 24 h a day, 7 days a week.
2.2. Study period
The analysis was carried out on the data available in the workplace aggression register from 1 January 2017 to 30 August 2021. This register is compiled by the internal surveillance personnel of the hospital in collaboration with the ED healthcare personnel and records information about the interventions by the security service in the entire hospital and the ED.
The aggression register is compiled monthly and the data are expressed as the number of interventions per month. The workplace violence variables used in our study and extrapolated from the register were: 1. the number of workplace attacks against ED health personnel that required the intervention of security service; 2 the number of workplace attacks against ED health personnel that required the intervention of the police; and, 3. the number of patients accompanied to the ED by the police because they had engaged in aggressive behavior against other people. The data were reported as an absolute number of events per month (monthly ED counts) and as a standardized rate every 1000 accesses/month (monthly rate).
Data from the province of Bolzano on new COVID-19 positive patients were described as the number of new cases per month and were obtained from the data provided by the Italian Institute of Health (Istituto Superiore di Sanità).
2.3. Ethical consideration
The study was approved by the Local Ethics Committee (Comitato etico per la sperimentazione clinica, Azienda Sanitaria dell'Alto Adige, Bolzano, Italia, approval number 57-2020) and was conducted according to the Declaration of Helsinki regarding the Ethical Principles for Medical Research Involving Human Subjects.
2.4. Statistical analysis
Single-group interrupted time-series analysis (ITSA) is a method for evaluating longitudinal observational data [16,17]. It adopts a quasi-experimental approach to assess the impact of an event on the study population and its effect on the variables analyzed. The dependent variable is a serially ordered time series and the impact of an intervention is analyzed by evaluating any change in the trend of the values of the post-event variable after extrapolation of the pre-event trend [18]. In the current study, we performed different ITSA models with one changepoint (i.e., March 2020, corresponding to the Sars-CoV-2 pandemic outbreak) to quantitatively assess the impact of the COVID-19 pandemic on the workplace violence against health workers in the ED. To this aim, we compared two time periods, i.e., before and after the onset of the pandemic. The dependent variables of the different ITSA models were the different aggression rates over 1000 accesses per month extracted from the aggression register.
The single group ITSA were conducted using the user-written STATA command "itsa" specifying the prais model (Supplementary material 1). This model automatically follows a first-order autoregressive [AR (1)] process that takes into account the correlation between the first-order errors [19].
In the different models, the time elapsed from the start of the study was entered as a continuous variable at regular monthly intervals. A p-value of less than 0.05 was considered significant. All analyses were performed in STATA version 16 (StataCorp).
3. Results
The total number of ED visits during the study period was 235,794 (monthly mean 4,240; SD 820). At the outbreak of the pandemic, the number of monthly accesses decreased from a mean of 4,721 (SD 222) monthly accesses in the pre-COVID period to an average of 3,225 (SD 681) accesses in the post-COVID period (p < 0.001).
The total number of workplace aggressions was 1,002. Overall, the monthly average of attacks against healthcare personnel was 17.9 (SD 10.1), increasing from 13.5 (SD 6.6) in the pre-COVID-19 era to 27.2 (SD 9.8) in the months following the outbreak of the pandemic (p < 0.001). Considering the overall monthly accesses to the ED, the rate of aggressions every 1000 accesses/month increased from 2.8 (SD 1.4) in the pre-COVID-19 period to 8.6 (SD 2.6) in the pandemic period.
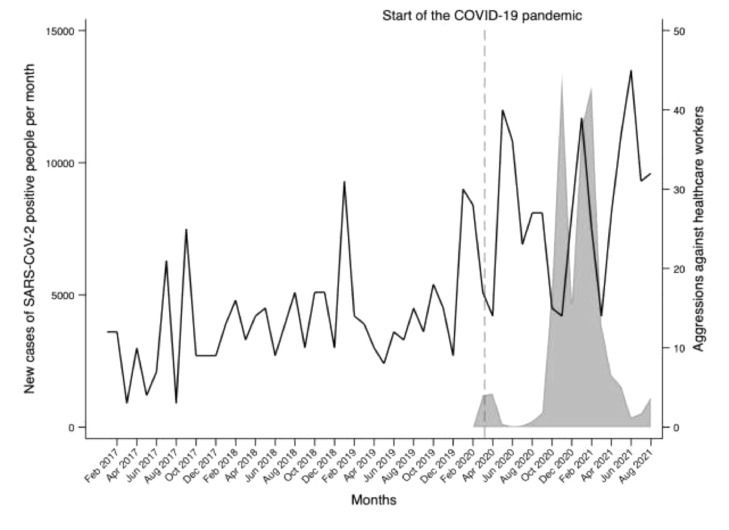
Fig. 1 shows the temporal trend of the new cases of SARS-CoV-2 in South Tyrol and the absolute number of attacks against health personnel of the ED per month. The temporal trend of aggressions remained stable during the months before the pandemic. Since March 2020, there was a trend of more aggressions during the pandemic with peaks temporally associated with the increase of new SARS-CoV-2 cases in South Tyrol. Furthermore, there was a clear temporal correlation between the number of aggressions against healthcare personnel and the introduction of government restrictions to the general population (Fig. 1).
Fig. 1.
Rate of attacks against healthcare peronnel in emergency departments standardized per 1000 emergency department visits and rate of new SARS-CoV-2 positive in South Tyrol from January 2017 to August 2021.
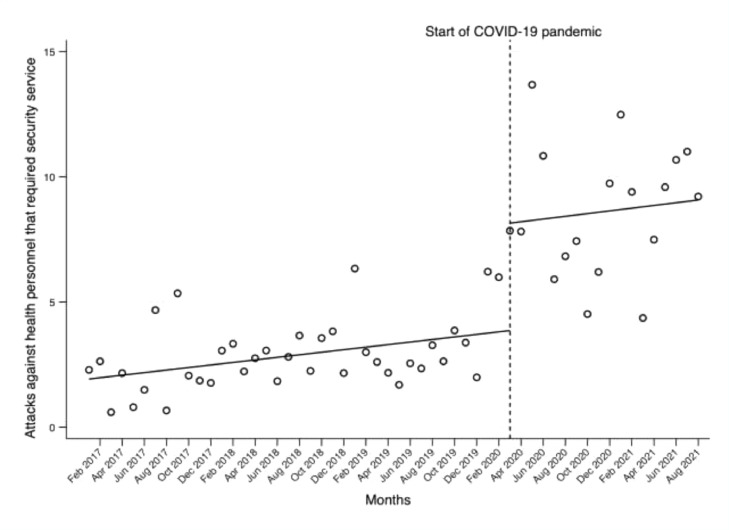
Fig. 2 shows the ITSA of attacks against health personnel that required the intervention of the security service. According to the effect analysis of the intervention performed through ITSA on the hypothetical global time series trend, in the pre-pandemic period there were 1.9 aggressions/1000 accesses per month (CI 95% 1.2-2.6, p < 0.001) with a significant increasing trend of 0.05 attacks/1000 accesses per month (CI 95% 0.00- 0.09, p = 0.018). In March 2020, the number of aggressions increased by 4.3/1000 accesses per month (CI 95% 1.4-7.2, p = 0.005) with a subsequent stable trend without significant changes (p = 0.977) (Fig. 2).
Fig. 2.
Interrupted time series analysis assessing the rate of attacks against health care workers that required the intervention of hospital security standardized per 1.000 monthly emergency department visits.
The mean monthly number of requests for police intervention in the ED was 7.3/month (SD 4.7) in the pre-COVID-19 months compared to 8.8/month (SD 3.4) after the outbreak of the pandemic (p = 0.226).
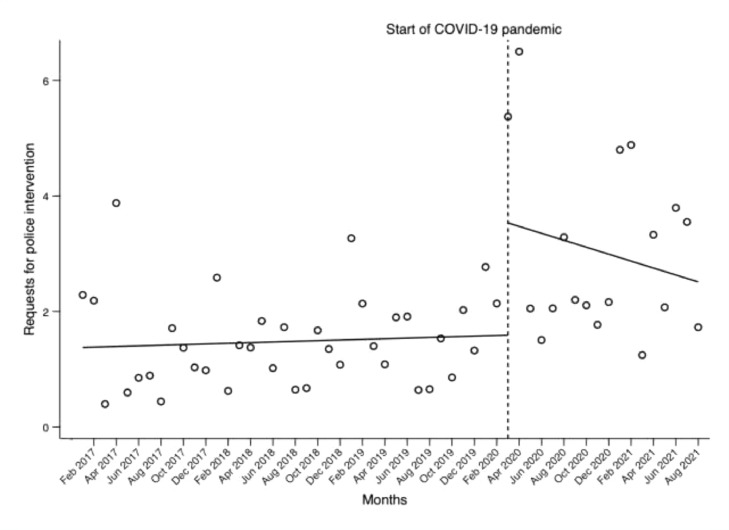
During the pre-pandemic period, the requests were 1.4/1000 accesses per month (CI 95% 0.8-1.9, p < 0.001) with a slight increase, although not significant, until the outbreak of COVID-19 (p = 0.654) (Fig. 3 ). In March 2020, the number of requests increased by 1.9/1000 accesses per month (CI 95% -0.1-3.9, p = 0.056) and then showed a non-significant decrease, which however did not reach pre-pandemic levels (p = 0.434) (Fig. 3).
Fig. 3.
Interrupted time series analysis assessing the rate of police intervention for attacks on healthcare workers in emergency departments standardized per 1.000 monthly emergency department visits.
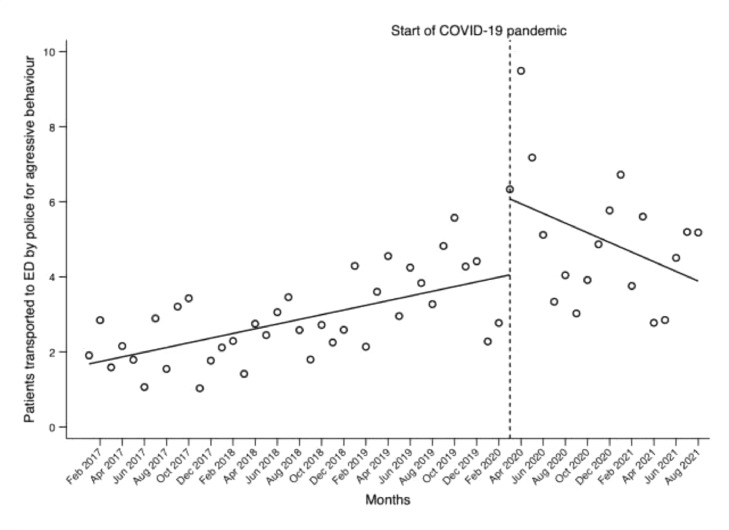
The number of patients accompanied to the ED by the police because they had been aggressive against other people was 1.7/1000 accesses per month (CI 95% 1.2-2.2, p < 0.001) in the pre-pandemic period, with a significant increasing trend of 0.06/1000 accesses per month (CI 95% 0.03-0.09, p < 0.001) up to March 2020. At the outbreak of the pandemic, no significant increase was observed, with a return to pre-pandemic levels at the end of the study period (Fig. 4 ).
Fig. 4.
Interrupted time series analysis assessing the rate of aggressive patients brought to the emergency department by the police standardized per 1.000 monthly emergency department visits.
4. Discussion
The main finding of this study is that the outbreak of the COVID-19 pandemic was associated with a significant increase in workplace violence against healthcare personnel working in the ED, requiring the intervention of the security service or the police.
Two recent systematic reviews of the literature have investigated the prevalence of workplace violence against healthcare personnel during the COVID-19 pandemic [20]. In one review including 17 studies (17,207 healthcare workers) found a prevalence of overall violence of 47% (95% CI: 34-61%), whereas the prevalence of physical and psychological violence was 17% (95% CI: 6-28%) and 44% (95% CI: 31-57%), respectively [20]. Of note, occupation violence was more frequently directed against physicians (68%; 95% CI: 31-95%) compared to other healthcare workers [20]. A second review (including 14 studies with 11,934 healthcare workers) yielded similar results: the pooled prevalence for violence was 42% (95% CI: 30%-54%) [21].So far, only two studies have compared workplace violence against healthcare professionals working in the ED before and during the COVID-19 pandemic [13,15]. One study evaluated the temporal trend of aggressions towards healthcare personnel before and during the COVID-19 pandemic using a quantitative approach. This study from the USA evaluated the influence of COVID-19 outbreak on workplace violence at an academic emergency department, showing a positive association between the monthly ED referrals of COVID-19 patients and the rate of workplace violent behavior in the ED (r = 0.24) [13]. Monthly incidents of ED violence from January 2019 to December 2020were obtained from an internal register of the security service and the electronic medical records and included reports of physical and verbal violence. The aggressions and violent incidents increased significantly during the pandemic (2.53 incidents per 1000 visits) compared to the 3 months prior (1.13 per 1000 visits, p < .001) and to the previous year (1.24 incidents per 1000 patient visits, p < .001). A higher incidence of assault during the pandemic compared to before was also reported by healthcare personnel in a survey (p = .019).
Our study confirms that the outbreak of the COVID-19 pandemic was temporally associated with a marked increase in workplace violence against healthcare personnel working in the ED and severe enough to require the prompt intervention of the security service or the police. Compared to the aforementioned study, the interrupted time series analysis technique allowed us to investigate temporal trends more innovatively and accurately, and to quantify their effect concerning the COVID-19 outbreak, the previous and the following period by providing a statistical comparison [13].
Furthermore, in the present study, we also evaluated the number of patients accompanied to the ED by the police because they had been violent towards other people, showing a significant increase compared to the period before the COVID-19 pandemic. This finding corroborates the hypothesis that the COVID-19 pandemic and its related restrictions of social and economic activities have exerted a negative emotional impact upon the general population, leading to increased aggressiveness, including domestic violence, also outside the hospital [22,23].
Several reasons could explain the increase in workplace violence against healthcare workers in the ED during the COVID-19 pandemic. This unprecedented health emergency has posed a huge burden to health systems and resources, which in turn could have negatively affected the quality of care, leading to increased dissatisfaction by patients and their family members [14]. The long working hours and heavy workload led to increased stress levels and exhaustion among healthcare professionals, which in turn could have facilitated conflicts with patients and their relatives, further exacerbated by the need to follow strict rules and regulations to prevent the spread of the infection [14].
The significant increase in workplace violence against healthcare professionals in the ED during the COVID-19 pandemic emphasizes the urgent need for implementing solutions aimed at improving their safety. The current pandemic has greatly increased the risks for healthcare workers. According to the latest figures from the International Committee of the Red Cross (ICRC), 848 violent incidents associated with Covid-19 were recorded from February to December 2020, and this figure is likely to be only “the tip of the iceberg” [24]. This led to the creation of the Health Care in Danger initiative, developed by the Red Cross and Red Crescent Movement with the aim of “reducing the incidence and the impact of violence against health care. This goal covers the violence during conflict and other emergencies, which encompasses not only military attacks on health-care facilities and staff, medical vehicles, and patients, but also obstruction, misuse and violence by individuals” (ICRC. ICRC institutional Health Care in Danger strategy 2020–2022 Protecting health care from violence and attacks in situations of armed conflict and other emergencies, page 7) [25]. Although never explicitly referring to the COVID-19 pandemic, this project includes a series of strategies to ensurerespect for health-care services and enable the safe delivery of health care, implement legislation to protect health care from violence, and educate healthcare providers to prevent violence and/or mitigate and cope with its impact [25].
Several further healthcare violence prevention programs have been implemented worldwide to educate health workers, identify risk factors, assess and manage violent patients, enhance personal safety in emergency situations, enhancing resilience in the workplace, and identify research needs in this field [26], [27], [28], [29], [30]. A further example of initiatives that address the problem of aggression and violence against healthcare personnel is the public-private coalition of Minnesota organizations created “to prevent violence toward staff in health care settings, and to provide resources to hospitals, long-term care facilities, clinics and other facilities to help them identify risks for violence and put effective strategies in place to respond” [31]. Through the work of this coalition, a useful list of sample policies and procedures, articles, staff education tools and other resourceswas created and summarized in an online “Prevention of Violence in Health Care Toolkit” [31].
As a response to counteract the increase in violence against health personnel during the COVID-19 pandemic, some countries have taken legislative measures to increase protection for health professionals and increase the penalties for anyone who assaults frontline clinicians or damage health facilities [5]. Furthermore, health institutions and policymakers should develop strategies to improve the safety of the working environment in hospitals and EDs, reduce the working hours of healthcare professionals, and regularly assess their stress levels and mental health [14]. Specific interventions for the management of violence in the ED could be implemented. They include consultation after an incident, increased education and training on violence management, reduction of workload, security measures (e.g., police presence and security cameras), sedation and restraint [11,32,33]. Finally, the use of social media and communication campaigns to prevent violence against healthcare professionals have been advocated as effective tools of primary prevention [5].
This could counteract the widespread and growing phenomenon of cyberbullying against healthcare personnel via social networks [34,35].
5. Conclusions
Compared to the only other study quantitatively evaluating the temporal trends of workplace violence related to the COVID-19 pandemic, our analysis includes a very long post-pandemic observation period, which can provide information over a longer course of time [13]. Furthermore, using ITSA we calibrated the post-pandemic on the pre-pandemic trend, obtaining information that could be used to track and perhaps predict the future trend of workplace violence against healthcare personnel in the ED, useful to develop and implement strategies to counteract the phenomenon. Finally, and perhaps most importantly, the number of workplace aggressions has been standardized according to the number of accesses to the ED.
Alongside these strengths, our study has a few limitations. Its monocentric nature could be associated with some biases related to the specificities of the territory and the type of population considered, which can limit the generalizability of results to other institutions or geographic regions. However, according to a very recent study, the phenomenon of workplace violence in the health sector is transversal and there are many similarities in the violence against healthcare professionals worldwide [36]. They include the wide belief that violence represents an intrinsic and almost inevitable experience in the ED, the perceived low administrative support compared to high support from peers, and the high prevalence of negative feelings, anxiety, burnout, depression, and acute and post-traumatic stress disorders. Despite some cultural differences across countries and various healthcare systems, the experiences of emergency nurses appear substantially analogous worldwide [36]. Hence, the generalizability of our results derived from a study conducted in the specific Italian context could be higher than expected. We deliberately removed the tourists from our analysis to perform a comparison between pre-pandemic and post-pandemic periods on a stable population. Furthermore, we did not evaluate the influence of the weekly incidence of newly diagnosed COVID-19 cases and the lockdown because the main aim of this study was the evaluation of temporal trends of workplace violence before and after the pandemic. Finally, the data were collected and analyzed monthly.
This study shows that workplace violence against healthcare workers has greatly increased following the outbreak of the COVID-19 pandemic. Health policies and strategies are urgently required to face up effectively to this serious phenomenon and major public issue. Raising public consciousness about this phenomenon and developing strategies to protect healthcare workers are required manoeuvres in health policy to contain this phenomenon.
Funding information
No funding was provided for this work
Declaration of Competing Interest
There is no conflict of interests.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.healthpol.2022.09.010.
Appendix
Search strategy used for a systematic search in MEDLINE (accessed through PubMed) carried out on July 22, 2022:
Search: (((occupational violence) OR (workplace violence)) AND (workplace violence)) AND (covid 19)
((("occupant"[All Fields] OR "occupant s"[All Fields] OR "occupants"[All Fields] OR "occupational"[All Fields] OR "occupations"[MeSH Terms] OR "occupations"[All Fields] OR "occupation"[All Fields]) AND ("violence"[MeSH Terms] OR "violence"[All Fields] OR "violence s"[All Fields] OR "violences"[All Fields])) OR ("workplace violence"[MeSH Terms] OR ("workplace"[All Fields] AND "violence"[All Fields]) OR "workplace violence"[All Fields])) AND ("workplace violence"[MeSH Terms] OR ("workplace"[All Fields] AND "violence"[All Fields]) OR "workplace violence"[All Fields]) AND ("covid 19"[All Fields] OR "covid 19"[MeSH Terms] OR "covid 19 vaccines"[All Fields] OR "covid 19 vaccines"[MeSH Terms] OR "covid 19 serotherapy"[All Fields] OR "covid 19 serotherapy"[Supplementary Concept] OR "covid 19 nucleic acid testing"[All Fields] OR "covid 19 nucleic acid testing"[MeSH Terms] OR "covid 19 serological testing"[All Fields] OR "covid 19 serological testing"[MeSH Terms] OR "covid 19 testing"[All Fields] OR "covid 19 testing"[MeSH Terms] OR "sars cov 2"[All Fields] OR "sars cov 2"[MeSH Terms] OR "severe acute respiratory syndrome coronavirus 2"[All Fields] OR "ncov"[All Fields] OR "2019 ncov"[All Fields] OR (("coronavirus"[MeSH Terms] OR "coronavirus"[All Fields] OR "cov"[All Fields]) AND 2019/11/01:3000/12/31[Date - Publication]))
Translations
occupational: "occupant"[All Fields] OR "occupant's"[All Fields] OR "occupants"[All Fields] OR "occupational"[All Fields] OR "occupations"[MeSH Terms] OR "occupations"[All Fields] OR "occupation"[All Fields]
violence: "violence"[MeSH Terms] OR "violence"[All Fields] OR "violence's"[All Fields] OR "violences"[All Fields]
workplace violence: "workplace violence"[MeSH Terms] OR ("workplace"[All Fields] AND "violence"[All Fields]) OR "workplace violence"[All Fields]
workplace violence: "workplace violence"[MeSH Terms] OR ("workplace"[All Fields] AND "violence"[All Fields]) OR "workplace violence"[All Fields]
covid 19: ("COVID-19" OR "COVID-19"[MeSH Terms] OR "COVID-19 Vaccines" OR "COVID-19 Vaccines"[MeSH Terms] OR "COVID-19 serotherapy" OR "COVID-19 serotherapy"[Supplementary Concept] OR "COVID-19 Nucleic Acid Testing" OR "covid-19 nucleic acid testing"[MeSH Terms] OR "COVID-19 Serological Testing" OR "covid-19 serological testing"[MeSH Terms] OR "COVID-19 Testing" OR "covid-19 testing"[MeSH Terms] OR "SARS-CoV-2" OR "sars-cov-2"[MeSH Terms] OR "Severe Acute Respiratory Syndrome Coronavirus 2" OR "NCOV" OR "2019 NCOV" OR (("coronavirus"[MeSH Terms] OR "coronavirus" OR "COV") AND 2019/11/01[PDAT]: 3000/12/31[PDAT]))
Appendix B. Supplementary materials
References
- 1.Lai J., Ma S., Wang Y., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. Published 2020 Mar 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Devi S. COVID-19 exacerbates violence against health workers. Lancet. 2020;396(10252):658. doi: 10.1016/S0140-6736(20)31858-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang Y., Li Y., An Y., et al. Workplace violence against chinese frontline clinicians during the COVID-19 pandemic and its associations with demographic and clinical characteristics and quality of life: a structural equation modeling investigation. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.649989. Published 2021 Apr 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aljohani B., Burkholder J., Tran Q.K., Chen C., Beisenova K., Pourmand A. Workplace violence in the emergency department: a systematic review and meta-analysis. Public Health. 2021;196:186–197. doi: 10.1016/j.puhe.2021.02.009. [DOI] [PubMed] [Google Scholar]
- 5.Bellizzi S., Pichierri G., Farina G., Cegolon L., Abdelbaki W. Violence against healthcare: a public health issue beyond conflict settings. Am J Trop Med Hyg. 2021 doi: 10.4269/ajtmh.21-0979. [published online ahead of print, 2021 Nov 22] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heponiemi T., Kouvonen A., Virtanen M., Vänskä J., Elovainio M. The prospective effects of workplace violence on physicians' job satisfaction and turnover intentions: the buffering effect of job control. BMC Health Serv Res. 2014;14:19. doi: 10.1186/1472-6963-14-19. Published 2014 Jan 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hüfner A., Dudeck M., Zellner J., Mahr D. Gewalt und Aggression im Krankenhaus – was, wenn das personal hilfe braucht? [Violence and aggression in hospitals-what if the personnel need help?] Unfallchirurg. 2020;123(6):424–434. doi: 10.1007/s00113-020-00806-6. [DOI] [PubMed] [Google Scholar]
- 8.Li N., Zhang L., Xiao G., Chen J., Lu Q. The relationship between workplace violence, job satisfaction and turnover intention in emergency nurses. Int Emerg Nurs. 2019;45:50–55. doi: 10.1016/j.ienj.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 9.Very E., Moncany A.H., Yrondi A., Marquet T., Bui E., Schmitt L. Facteurs de satisfaction et d’épuisement des psychiatres aux urgences [Work satisfaction and exhaustion among psychiatrists in psychiatric emergency services] Encephale. 2018;44(2):106–110. doi: 10.1016/j.encep.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 10.Cooper C.L., Swanson N. Workplace violence in the health sector: state of the art. World Health Organization. 2002. https://www.who.int/violence_injury_prevention/injury/en/WVstateart.pdf.
- 11.Timmins F., Catania G., Zanini M., et al. Nursing management of emergency department violence-can we do more? J Clin Nurs. 2022 doi: 10.1111/jocn.16211. [published online ahead of print, 2022 Jan 31] [DOI] [PubMed] [Google Scholar]
- 12.Ramacciati N., Ceccagnoli A., Addey B., Lumini E., Rasero L. Violence towards emergency nurses: a narrative review of theories and frameworks. Int Emerg Nurs. 2018;39:2–12. doi: 10.1016/j.ienj.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 13.McGuire S.S., Gazley B., Majerus A.C., Mullan A.F., Clements C.M. Impact of the COVID-19 pandemic on workplace violence at an academic emergency department. Am J Emerg Med. 2021;S0735-6757(21):00782–00788. doi: 10.1016/j.ajem.2021.09.045. [published online ahead of print, 2021 Sep 23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu R., Li Y., An Y., et al. Workplace violence against frontline clinicians in emergency departments during the COVID-19 pandemic. PeerJ. 2021;9:e12459. doi: 10.7717/peerj.12459. Published 2021 Nov 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Özdamar Ünal G., İşcan G., Ünal O. The occurrence and consequences of violence against healthcare workers in Turkey: before and during the COVID-19 pandemic. Fam Pract. 2022:cmac024. doi: 10.1093/fampra/cmac024. [published online ahead of print, 2022 Apr 8] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bernal J.L., Cummins S., Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1)):348–355. doi: 10.1093/ije/dyw098. [published correction appears in Int J Epidemiol. 2020 Aug 1;49(4):1414] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scortichini M., Schneider Dos Santos R., De' Donato F., et al. Excess mortality during the COVID-19 outbreak in Italy: a two-stage interrupted time-series analysis. Int J Epidemiol. 2021;49(6):1909–1917. doi: 10.1093/ije/dyaa169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Campbell D.T, Stanley J.C. Ravenio Books; 2015. Experimental and quasi-experimental designs for research. [Google Scholar]
- 19.Linden A. A matching framework to improve causal inference in interrupted time-series analysis. J Eval Clin Pract. 2018;24(2):408–415. doi: 10.1111/jep.12874. [DOI] [PubMed] [Google Scholar]
- 20.Ramzi Z.S., Fatah P.W., Dalvandi A. Prevalence of workplace violence against healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Front Psychol. 2022;13 doi: 10.3389/fpsyg.2022.896156. Published 2022 May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saragih I.D., Tarihoran D., Rasool A., Saragih I.S., Tzeng H.M., Lin C.J. Global prevalence of stigmatization and violence against healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. J Nurs Scholarsh. 2022 doi: 10.1111/jnu.12794. [published online ahead of print, 2022 Jul 12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rochford H.I., Brooks K., Berg M., Peek-Asa C. COVID-19-related violence trend data challenges & a resource for injury researchers. Inj Epidemiol. 2021;8(1):45. doi: 10.1186/s40621-021-00338-6. Published 2021 Jul 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shepherd J.P., Moore S.C., Long A., Mercer Kollar L.M., Sumner S.A. Association between COVID-19 lockdown measures and emergency department visits for violence-related injuries in Cardiff, Wales. JAMA. 2021;325(9):885–887. doi: 10.1001/jama.2020.25511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maurer P. 5 years on, there has not been significant change: access to health care continues to be impeded. ICRC. (2021). https://www.icrc.org/en/document/5-years-there-has-not-been-significant-change-access-health-care-continues-be-impeded.
- 25.ICRC. ICRC institutional health care in danger strategy 2020–2022 protecting health care from violence and attacks in situations of armed conflict and other emergencies. ICRC. 2020. https://healthcareindanger.org/wp-content/uploads/2020/10/ICRC-HCiD-strategy-2020-2022.pdf.
- 26.Paluzzi P., Gaffikin L., Nanda J. The American college of nurse-midwives' domestic violence education project: evaluation and results. J Midwifery Womens Health. 2000;45(5):384–391. doi: 10.1016/s1526-9523(00)00056-8. [DOI] [PubMed] [Google Scholar]
- 27.McKinnon B., Cross W. Occupational violence and assault in mental health nursing: a scoping project for a victorian mental health service. Int J Ment Health Nurs. 2008;17(1):9–17. doi: 10.1111/j.1447-0349.2007.00499.x. [DOI] [PubMed] [Google Scholar]
- 28.Mathiews A., Salmond S. Opening the door to improve visiting nurse safety: an initiative to collect and analyze protection practices and policies. Home Healthc Nurse. 2013;31(6):310–321. doi: 10.1097/NHH.0b013e318293634f. [DOI] [PubMed] [Google Scholar]
- 29.International council of nurses joins new initiative against workplace violence in health sector. Qld Nurse. 2003;22(1):20. [PubMed] [Google Scholar]
- 30.Sanchez L., Young V.B., Baker M. Active shooter training in the emergency department: a safety initiative. J Emerg Nurs. 2018;44(6):598–604. doi: 10.1016/j.jen.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 31.Minnesota Department of Health. Prevention of violence in health care. Available online at: https://www.health.state.mn.us/facilities/patientsafety/preventionofviolence/.
- 32.Dafny H.A., Beccaria G., Muller A. Australian nurses' perceptions about workplace violence management, strategies and support services. J Nurs Manag. 2021 doi: 10.1111/jonm.13522. [published online ahead of print, 2021 Nov 22] [DOI] [PubMed] [Google Scholar]
- 33.Carver M., Beard H. Managing violence and aggression in the emergency department. Emerg Nurse. 2021;29(6):32–39. doi: 10.7748/en.2021.e2094. [DOI] [PubMed] [Google Scholar]
- 34.La Regina M., Mancini A., Falli F., et al. Aggressions on social networks: what are the implications for healthcare providers? An exploratory research. Healthcare. 2021;9(7):811. doi: 10.3390/healthcare9070811. (Basel)Published 2021 Jun 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang Q., Tai-Seale M., Liu S., et al. Measuring public reaction to violence against doctors in China: interrupted time series analysis of media reports. J Med Internet Res. 2021;23(2):e19651. doi: 10.2196/19651. Published 2021 Feb 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ramacciati N., Ceccagnoli A., Addey B., Giusti G.D., Commentary on Tan M.F., et al. Nursing management of aggression in a Singapore emergency department: a qualitative study. Nurs Health Sci. 2016;18(2):270–271. doi: 10.1111/nhs.12248. Nursing and Health Sciences. 2015; 17: 307-312. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.