Abstract
Background
In the global pandemic of the coronavirus disease 2019 (COVID-19), depression and post-traumatic stress disorder (PTSD) have commonly occurred among COVID-19 patients, whose experiences of infection and subsequent treatment might develop negative consequences on their mental well-being even after recovery. Despite the general recognition of efficacy of mindfulness-based interventions in reducing psychological distress among various populations, there were insufficient studies on the relationship between mindfulness and mental health among individuals who have recovered from COVID-19.
Objective
The current study aims to identify the prevalence of common mental health challenges among recovered COVID-19 patients in Jianghan District, Wuhan, China and to explore the potential mechanism through which mindfulness alleviate depression and PTSD.
Methods
A cross-sectional survey on mental health was conducted among a convenience sample of adults recovered from COVID-19 in Jianghan District, Wuhan, China. The study participants completed questionnaires under the assistance of trained investigators. The questionnaire included Chinese version of Five Facets of Mindfulness Questionnaire-Short Form (FFMQ-SF), Generalized Anxiety Disorder Questionnaire (GAD-7), Resilience Style Questionnaire (RSQ), Impact of Events Scale-Revised (IES-R), and Patient Health Questionnaire (PHQ-9) to measure mindfulness, anxiety, resilience, PTSD, and depression respectively. Structural equation modeling was used to explore the relationship between mindfulness and mental health outcomes of this population.
Results
1541 respondents (654 [42.4 %] men and 887 [57.6 %] women) completed the questionnaire between June 10 and July 25, 2021, of whom 36.2 % and 27.1 % had mild and severe levels of depressive and anxiety symptoms respectively, and 15.2 % was indicated with PTSD. The average score of mindfulness of the study participants was (3.100 ± 0.387), and that of resilience was (3.560 ± 0.877). The structural equation model fit the data well, demonstrating that mindfulness was negatively associated with depressive symptoms directly (β = −0.031, P = 0.021) or indirectly through the mediation effect of resilience (β = −0.019, P = 0.009) and anxiety symptoms (β = −0.208, P < 0.001), and was negatively associated with PTSD through the mediation effect of anxiety symptoms (β = −0.142, P < 0.001).
Conclusion
Individuals who have recovered from COVID-19 commonly experienced psychological distress. Mindfulness is associated with alleviation of depressive and PTSD symptoms directly or indirectly. Interventions based on mindfulness are suggested to improve the mental well-being of this population.
Keywords: Mindfulness, Mental health, Recovered patients, COVID-19, Structural equation modeling
1. Introduction
The coronavirus disease 2019 (COVID-19) has become a global pandemic since the outbreak, threatening public health security worldwide (Chan et al., 2020; Li et al., 2020b). There have been 298,915,721 confirmed cases and 5,469,303 deaths globally according to the data from World Health Organization (WHO) (WHO, 2022a), and 133,404 confirmed cases and 5699 deaths reported in China, as of January 07, 2022 (WHO, 2022b). Though there were scattered new cases across China in the past year, most of the infected individuals have recovered and discharged from the hospital; more attention has been paid to helping survivors of COVID-19 to rehabilitate their physical functions and mental health (Si et al., 2021).
Evidence suggested that the COVID-19 pandemic had psychological consequences on various populations, especially on COVID-19 patients (Ceban et al., 2022; Hao et al., 2020a; Renaud-Charest et al., 2021). Researches showed that COVID-19 infection can trigger the release of pro-inflammatory cytokines related to psychiatric morbidity, such as interleukin-6 (IL-6) and tumor necrosis factor alpha (TNF-α) (Conti et al., 2020; Guo et al., 2022). A qualitative study indicated that COVID-19 patients regarded COVID-19 infection as a major stress event for them due to high infectivity and potential lethality of COVID-19 infection, in addition, long hours of hospitalization and isolation may lead to their depressive disorders (Hao et al., 2020a). A systematic review on long COVID-19-related psychiatric complications demonstrated that the prevalence of depressive symptoms over 12 weeks in COVID-19 patients ranged from 11 % to 28 %, and depressive symptoms can affect neurocognitive functioning in post-COVID-19 syndromes of patients (Renaud-Charest et al., 2021). A meta-analysis also revealed that 22 % of the COVID-19 patients 12 or more weeks following diagnosis suffer from cognitive impairment (Ceban et al., 2022). Furthermore, some of the COVID-19 patients required intensive care and mechanical ventilation and had to spend three more weeks on average in the ICU compared with typical ICU populations (Choon-Huat Koh and Hoenig, 2020; Michel et al., 2020). Some with severe COVID-19 had respiratory symptoms, which could develop into respiratory failure (Xie et al., 2020). Most of them experienced traumatic stress during the treatment, due to fear of death and physical pains from interventional therapy (Kaseda and Levine, 2020). Even those patients with moderately severe illness, who did not undergo hospitalization or reported fear of death, might also face psychological distress after discharge (Kaseda and Levine, 2020).
Clinical sequelae associated with COVID-19 were known to exist in survivors (Demertzis et al., 2020). A longitudinal study conducted in Wuhan showed that nearly half of the individuals recovered from COVID-19 had certain sequelae, such as myalgia, joint pain, chillness, chest distress, and high blood pressure, etc. (Xiong et al., 2021). Besides, discrimination and stigma due to experience of infection were widely perceived by the COVID-19 survivors (Amadeo et al., 2021; Bao et al., 2020). These factors predispose COVID-19 survivors to be vulnerable to negative psychological consequences such as depression and PTSD. A cross-sectional survey conducted after the outbreak in Shanghai, China showed that >33 % of the people infected with COVID-19 reported symptoms of PTSD, 55.3 % with anxiety, and 60.2 % with depression (Guo et al., 2020). Another survey conducted in April 2020 in Wuhan indicated that 12.4 % of COVID-19 survivors had symptoms of PTSD, 42.7 % with anxiety, and 65.7 % with depression (Liu et al., 2020).
PTSD is often associated with depression and anxiety. Many individuals with trauma experience also experienced depression, which might be caused by exposure to negative events and subsequently evoked anxiety (de la Torre-Cruz et al., 2021; Kok et al., 2016; Nearchou and Douglas, 2021). Some empirical evidence revealed that the effect of stressful events on depression could be better interpreted through cognitive and emotional functions regarding anxiety, which indicated significant effect of anxiety or depression (Anyan et al., 2018). Meanwhile, anxiety was shown to be a strong determinant of PTSD; evidence suggested that one third of those who had anxiety after traumatic events might develop PTSD (Bjornsson et al., 2020; Kok et al., 2016).
Depression is the most common mental disorder coexisting with PTSD. Both disorders could result in high suicidal ideation and self-harm intention. They were also linked with poorer immune system functioning, which could have negative impact on physical health. Therefore, it's imperative to take measures to alleviate the depressive and PTSD symptoms among COVID-19 survivors (Flory and Yehuda, 2015; Marx et al., 2021; Mazza et al., 2020; Shen et al., 2020). Resilience is regarded as a dynamic process to positively adapt to adverse conditions (Waller, 2001). A systematic review demonstrated that resilience interventions could be helpful for the improvement of mental health in adult population (Ferreira et al., 2021). Some research indicated that a higher level of resilience could reduce PTSD symptoms, since it may serve as a translational endpoint in the treatment of PTSD (Gao et al., 2018; Rakesh et al., 2019). Other research showed that resilience is relevant to depression alleviation, and that a higher level of resilience was found to be associated with a lower level of depression (Liu et al., 2019; Xiang et al., 2020).
As mental ill-health is prevalent among COVID-19 survivors, it is significant to explore possible protective factors that can improve mental well-being among this population (Wang et al., 2021b). Mindfulness centers on cultivating intentional awareness in the unfolding of present-moment experiences (Kabat-Zinn, 2005). Mindfulness-based interventions have shown to be effective in alleviating symptoms related to depression, anxiety, and PTSD, as well as chronic pain in various populations (Goldberg et al., 2018; Hilton et al., 2017; Kirk et al., 2022; Mak et al., 2015). A meta-analysis on mindfulness and psychiatric disorders-related biomarkers demonstrated that mindfulness-based intervention could alleviate PTSD via the decreased methylation of serotonin transporter genes, and reduce depression and anxiety by decreasing levels of IL-6 and TNF-α (Sanada et al., 2020). A clinical study revealed that PTSD is also associated with L-6 and TNF-α (Kuffer et al., 2019). A longitudinal study showed that the practice of mindfulness could increase one's resilience level, and further reduce depressive symptoms (Antonini Philippe et al., 2021). Another study focused on the biomarkers and psychological resilience indicated that increased IL-6 level is associated with low psychological resilience, which provided biological evidence for the effect of mindfulness-based intervention on psychological resilience (Imai et al., 2019). In China, researchers have developed a mindfulness-based training protocol for COVID-19 survivors, named 6-week Mindful Living With Challenge (MLWC), whose aims were to investigate its effectiveness in cultivating mindfulness and alleviating psychological distress in this population through randomized controlled trial (Si et al., 2021). Studies have found mindfulness to be able to mitigate against psychological distress during COVID-19 pandemic (Antonova et al., 2021; Behan, 2020; Conversano et al., 2020; Zhu et al., 2021). However, the resilience mechanism through which mindfulness may be associated with reduced mental illness symptoms is yet to be investigated. The present cross-sectional study aimed to explore the prevalence of anxiety, depressive, and PTSD symptoms among COVID-19 survivors in Jianghan District, Wuhan, China, and to examine the potential mechanism of mindfulness that contributes to reducing psychological distress.
2. Material and methods
2.1. Measures
Demographic characteristics, including age, gender, education, and marital status, and items on COVID-19 infection, such as clinical classification and perceived mental health status were asked. In this study, participants' mindfulness, anxiety, resilience, depression and PTSD were measured by specific scales, and according to the previous studies, we hypothesized that resilience and anxiety could both serve as potential mediators between mindfulness and depression, and mindfulness and PTSD, respectively.
2.1.1. Mindfulness
The Five Facets of Mindfulness Questionnaire-Short Form (FFMQ-SF) in Chinese consists of 20 items that are rated on a 5-point Likert scaled from 1 to 5 and was used to assess the mindfulness level of participants during the past two weeks. It measures five facets of mindfulness: observing, describing, acting with awareness, nonjudging and nonreacting. For the items of “acting with awareness” and “nonjudging”, factors are reverse scored (Baer et al., 2006; Hou et al., 2014). Higher total or mean scores of the 20 items indicate higher levels of mindfulness. This instrument has been validated among various Chinese population (Arthur et al., 2018; Fong et al., 2021). According to the literature, due to the changing nature of the five facets of the instrument, the correlations between the facets could be negative or positive, which could reduce the internal consistency of the instrument superficially (Gu et al., 2016; Meng et al., 2019). In this case, the mean scores of the 20 items were employed to represent and reflect the mindfulness level of the subjects in the model of this study, and the Cronbach's alpha of the five facets in this study were 0.797, 0.811, 0.812, 0.755 and 0.782 respectively.
2.1.2. Anxiety
The Generalized Anxiety Disorder Questionnaire (GAD-7) consists of 7 items that are rated on a 4-point Likert scaled from 0 to 3. It is developed for measuring the severity of generalized anxiety symptoms during the past two weeks (Spitzer et al., 2006). The scores of the instrument range from 0 to 21. Scores between 5 and 9, 10 and 14, and 15 and higher represent mild, moderate and severe anxiety symptoms respectively. This instrument has demonstrated to be reliable and valid among Chinese population (Gong et al., 2021; Miao et al., 2021). In this study, the Cronbach's alpha of the instrument was 0.950.
2.1.3. Resilience
The Resilience Style Questionnaire (RSQ) consists of 16 items that are rated on a 5-point Likert scaled from 1 to 5. It is used to measure the level of individual's resilience during the past two weeks (Mak et al., 2019). Higher total or mean scores of the 16 items indicate greater ability to recover from negative events. This instrument was developed and validated among Chinese (Li et al., 2020a; Lin et al., 2020). In this study, the Cronbach's alpha of the instrument was 0.975.
2.1.4. Depression
The Patient Health Questionnaire (PHQ-9) is a 9-item questionnaire that is used for screening and monitoring depression of varying degrees of severity (Kroenke et al., 2001). The items of the PHQ-9 are rated on a 4-point Likert scaled ranging from 0 to 4. The total score is utilized to assess the degree of depression of participants during the past two weeks, with scores of <5 indicating no or minimal depression; 5–9 mild depression; 10–14 moderate depression; 15–19 moderately severe depression; and scores of ≥20 severe depression. This instrument has been validated among various Chinese population (Hou et al., 2021; Yao et al., 2021). In this study, the Cronbach's alpha of the instrument was 0.913.
2.1.5. PTSD
The Impact of Events Scale-Revised (IES-R) is a 22-item scale aiming at screening posttraumatic stress symptoms in adults or older people. The items of this instrument are rated on a 5-point Likert scaled from 0 to 4 (Horowitz et al., 1979; Weiss and Marmar, 1997). The IES-R contains three dimensions measuring intrusion, avoidance and hyperarousal. Respondents rate their degree of distress during the past seven days after they have identified a specific stressful life event occurred to them. A total score of equal or above 35 can be regarded as positive PTSD symptoms. This instrument has been proved valid and reliable among COVID-19 patients (Zheng et al., 2021). In this study, the Cronbach's alpha of the instrument was 0.963.
2.2. Sampling and participants
From June 10 to July 25, 2021, 1601 out of 4122 registered patients who have recovered from COVID-19 in 13 communities in Jianghan District, Wuhan City, Hubei Province, China were recruited to receive clinical re-examination and questionnaire survey at a Grade-A Tertiary Hospital in Jianghan District, Wuhan by community-based convenience sampling. All investigators and support staff in this study were trained based on the same protocol and required to have an educational background in medicine or public health. Those who had a history of COVID-19 infection and had recovered were invited to complete an online structured questionnaire from June to July 2021. Digital informed consent was obtained from all individuals to ensure their voluntary participation. Ethics approval for the questionnaire study was obtained from the Ethics Review Committee of the Institute of Pathogen Biology, Chinese Academy of Medical Sciences, Beijing, China (IPB-2020-22). The participants had to meet the following criteria: 1) Over 18 years old; 2) Have a history of COVID-19 infection; 3) Proficiency in Chinese; 4) Be able to independently cooperate with researchers to complete various scale assessments; 5) Have a mobile communication equipment such as a mobile phone, and a WeChat account; 6) Mobile equipment can access the Internet at any time; 7) Have not received medications for PTSD, depression, or anxiety within 1 month prior to enrollment in the study. Those who met any of the below criteria were excluded: 1) Have serious cognitive impairment; 2) Have serious heart, brain, lung, kidney, liver, and other medical diseases or tumors; 3) Difficult to cooperate with the questionnaire study. Finally, 1541 of them were selected as research sample based on the criterion above.
2.3. Data analysis
Descriptive analyses were used to examine participants' demographic characteristics. Partial least squares structural equation modeling (PLS-SEM) was primarily used to explore the relationship between various variables, with a focus on explaining the variance in the dependent variables (Hair et al., 2013). Structural equation model (SEM) with SmartPLS 3.3.3 was used to assess the model built. The standardized root mean square residual (SRMR) and root mean square residual covariance (RMStheta) were used to estimate the model fit, where SRMR≤0.08 and RMStheta ≤ 0.12 indicate good model fit (Hair et al., 2017); The composite reliability (CR) and average variance extracted (AVE) and were used to evaluate the reliability and convergent validity of the measurement model, where CR ≥ 0.7 and AVE ≥ 0.5 indicate good reliability and convergent validity of the measurement model (Fornell and Larcker, 1981); The heterotrait-monotrait (HTMT) criterion was used to assess discriminant validity of the measurement model, where HTMT values≤0.9 indicate good discriminant validity of the measurement model (Henseler et al., 2015); The coefficient of determination (R2) and Stone-Geisser's Q2 values of dependent variables, and path coefficients were employed to evaluate the structural model. The bootstrap analysis was performed to test the significance of the path and mediation effects in the model with 5000 bootstrap samples at the level of α = 0.05 (MacKinnon, 2008).
3. Results
3.1. Demographic characteristics
A total of 1541 individuals who have recovered from COVID-19 were recruited in the study. 42.4 % were males, 12.2 % had critical COVID-19 symptoms; over 70 % aged above 50; 87.7 % lived in city; 85.2 % were married; 14.1 % were at undergraduate or above educational level; 61.5 % had annual family income less than RMB 60000; 84.4 % had been hospitalized after COVID-19 infection; 15.3 % perceived good psychological status during infection; 45.7 % had other family members infected with COVID-19; 29.5 % had relatives or friends infected with COVID-19; 12.5 % were current smoker; 27.5 % drank and 59.8.2 % were of abnormal Body Mass Index (BMI). The detailed results of demographic characteristics are summarized in Table 1 .
Table 1.
Demographic characteristics of participants (N = 1541).
| Variable | n(%) |
|---|---|
| Gender | |
| Male | 654(42.4 %) |
| Female | 887(57.6 %) |
| Age (Year) | |
| 18–29 | 27(1.8 %) |
| 30–39 | 116(7.5 %) |
| 40–49 | 242(15.7 %) |
| 50–59 | 422(27.4 %) |
| 60–69 | 482(31.3 %) |
| ≥70 | 252(16.4 %) |
| Clinical classification of COVID-19 | |
| Mild | 90(5.8 %) |
| Moderate | 1113(72.2 %) |
| Severe | 151(9.8 %) |
| Critical | 187(12.2 %) |
| Residence place | |
| City | 1351(87.7 %) |
| Village | 190(12.3 %) |
| Marital status | |
| Unmarried | 228(14.8 %) |
| Married | 1313(85.2 %) |
| Educational level | |
| Senior high school or below | 1082(70.2 %) |
| Above senior school | 459(29.8 %) |
| Income for 2020(CNY/Year) | |
| <60,000 | 947(61.5 %) |
| ≥60,000 | 594(38.5 %) |
| Perceived mental health during infection | |
| Very bad | 114(7.4 %) |
| Bad | 235(15.2 %) |
| Common | 288(18.7 %) |
| Good | 790(51.3 %) |
| Very good | 114(7.4 %) |
| Have other family members infected with COVID-19 | |
| Yes | 705(45.7 %) |
| No | 836(54.3 %) |
| Have relatives or friends infected with COVID-19 | |
| Yes | 454(29.5 %) |
| No | 1077(69.9 %) |
| Current smoker | |
| Yes | 193(12.5 %) |
| No | 1348(87.5 %) |
| Alcohol use | |
| Yes | 424(27.5 %) |
| No | 1117(72.5 %) |
| BMI | |
| Thin(BMI < 18.5) | 48(3.12 %) |
| Normal(18.5 ≤ BMI<24) | 620(40.2 %) |
| Overweight(24 ≤ BMI<28) | 664(43.1 %) |
| Obese(BMI ≥ 28) | 209(13.6 %) |
3.2. Prevalence of depression, anxiety and PTSD of participants
In this sample, 36.2 % and 27.1 % reported mild to severe levels of depressive and anxiety symptoms; and 15.2 % were positively indicated for PTSD, as shown in Table 2 .
Table 2.
Prevalence of depression, anxiety and PTSD of participants.
| Variable | Rank | n(%) |
|---|---|---|
| Depression | Normal | 983(63.8 %) |
| Mild | 357(23.2 %) | |
| Moderate | 124(8.0 %) | |
| Moderately severe | 56(3.6 %) | |
| Severe | 21(1.4 %) | |
| Anxiety | Normal | 1123(72.9 %) |
| Mild | 331(21.5 %) | |
| Moderate | 52(3.4 %) | |
| Severe | 35(2.3 %) | |
| PTSD | Positive | 234(15.2 %) |
| Negative | 1307(84.8 %) |
3.3. Correlations between mindfulness and resilience of participants
Correlation between mindfulness and resilience among the participants are summarized in Table 3 . The diagonal elements in the correlation of factors matrix were the corresponding means and standard deviations. The average score of mindfulness was (3.100 ± 0.387), and resilience was (3.560 ± 0.877). All correlation coefficients were statistically significant (P ≤ 0.05).
Table 3.
Correlations between mindfulness and resilience of participants.
| Mindfulness | Observing | Describing | Nonreacting | Acting with awareness | Nonjudging | Resilience | |
|---|---|---|---|---|---|---|---|
| Mindfulness | 3.100 ± 0.387 | ||||||
| Observing | 0.696⁎⁎⁎ | 2.530 ± 0.938 | |||||
| Describing | 0.799⁎⁎⁎ | 0.679⁎⁎⁎ | 2.839 ± 0.956 | ||||
| Nonreacting | 0.722⁎⁎⁎ | 0.716⁎⁎⁎ | 0.740⁎⁎⁎ | 2.704 ± 0.926 | |||
| Acting with awareness | 0.162⁎⁎⁎ | −0.385⁎⁎⁎ | −0.263⁎⁎⁎ | −0.358⁎⁎⁎ | 3.885 ± 0.768 | ||
| Nonjudging | −0.320⁎⁎⁎ | −0.702⁎⁎⁎ | −0.612⁎⁎⁎ | −0.730⁎⁎⁎ | 0.564⁎⁎⁎ | 3.531 ± 0.867 | |
| Resilience | 0.484⁎⁎⁎ | 0.275⁎⁎⁎ | 0.398⁎⁎⁎ | 0.351⁎⁎⁎ | 0.162⁎⁎⁎ | −0.175⁎⁎⁎ | 3.560 ± 0.877 |
Note: All correlation coefficients were statistically significant.
P < 0.001.
3.4. Structural equation modeling analysis
3.4.1. Evaluation of model fit
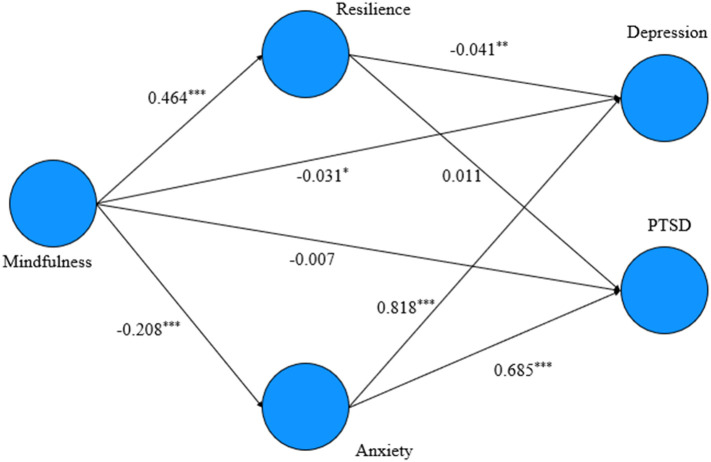
The model fit were as follows: SRMR = 0.065, RMStheta = 0.086, suggesting a well-fitting model in this study. The structural equation model built in this study is shown in Fig. 1 .
Fig. 1.
Structural equation modeling of factors affecting depression and PTSD among the recovered patients of COVID-19.
Note: *P < 0.05 **P < 0.01 ***P < 0.001.
3.4.2. Evaluation of measurement model
Measurement model evaluation is an essential step in a structural equation modeling analysis. The evaluation of reliability and convergent validity of the measurement model are shown in Table 4 . As indicated, the values of CR and AVE were larger than the recommended values 0.7 and 0.5 respectively for all constructs, which confirmed good reliability and convergent validity of the measurement model.
Table 4.
Reliability and convergent validity of measurement model.
| Construct | CR | AVE |
|---|---|---|
| Depression | 0.932 | 0.606 |
| Mindfulness | 1.000 | 1.000 |
| PTSD | 0.967 | 0.577 |
| Resilience | 0.978 | 0.738 |
| Anxiety | 0.959 | 0.770 |
Note: CR: composite reliability; AVE: Average variance extracted.
The evaluation of the discriminant validity indicated that HTMT values were all below the recommended value 0.9, which meant acceptable discriminant validity of the measurement model. The detailed information is shown in Table 5.
Table 5.
Discriminant validity of measurement model (HTMT).
| Construct | Depression | Mindfulness | PTSD | Resilience | Anxiety |
|---|---|---|---|---|---|
| Depression | |||||
| Mindfulness | 0.227 | ||||
| PTSD | 0.766 | 0.154 | |||
| Resilience | 0.233 | 0.469 | 0.157 | ||
| Anxiety | 0.887 | 0.213 | 0.714 | 0.215 |
Note: HTMT: heterotrait-monotrait.
3.4.3. Evaluation of structural model
In this study, the R2 of depression and PTSD were 0.697 and 0.474 respectively, indicating large amount of variance in depression and PTSD explained by all of the exogenous constructs linked to them. In addition, the Q2 values of the dependent constructs were all above 0, which proved the out-of-sample power of the model (Geisser, 1974; Stone, 1974).
The standardized path coefficients and their significance calculated by bootstrap sampling indicated that except the effect of resilience on depression and PTSD, all the other effects in the model were statistically significant. The detailed results of coefficients are shown in Table 6 .
Table 6.
Path analysis.
| Effect | β | S.E. | t | P | Bootstrap 95%CI |
|
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Resilience - > PTSD | −0.011 | 0.023 | 0.486 | 0.627 | −0.057 | 0.035 |
| Resilience - > Depression | −0.041⁎⁎ | 0.016 | 2.648 | 0.008 | −0.071 | −0.011 |
| Mindfulness - > PTSD | −0.007 | 0.022 | 0.311 | 0.756 | −0.053 | 0.032 |
| Mindfulness - > Resilience | 0.464⁎⁎⁎ | 0.020 | 23.195 | <0.001 | 0.421 | 0.502 |
| Mindfulness - > Depression | −0.031⁎ | 0.013 | 2.312 | 0.021 | −0.058 | −0.005 |
| Mindfulness - > Anxiety | −0.208⁎⁎⁎ | 0.021 | 9.843 | <0.001 | −0.249 | −0.166 |
| Anxiety - > PTSD | 0.685⁎⁎⁎ | 0.021 | 32.924 | <0.001 | 0.639 | 0.721 |
| Anxiety - > Depression | 0.818⁎⁎⁎ | 0.014 | 59.71 | <0.001 | 0.788 | 0.843 |
P < 0.05.
P < 0.01.
P < 0.001.
3.4.4. Mediation analysis
The results of the mediation analysis illustrated that resilience and anxiety both served as mediators between mindfulness and depression, and anxiety also mediated the relationship between mindfulness and PTSD, as shown in Table 7 .
Table 7.
Mediation analysis.
| Effect | Β | S.E. | t | P | Bootstrap 95%CI |
|
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Mindfulness - > Resilience - > PTSD | −0.005 | 0.011 | 0.485 | 0.628 | −0.027 | 0.016 |
| Mindfulness - > Resilience - > Depression | −0.019⁎⁎ | 0.007 | 2.628 | 0.009 | −0.034 | −0.005 |
| Mindfulness - > Anxiety - > PTSD | −0.142⁎⁎⁎ | 0.015 | 9.322 | <0.001 | −0.172 | −0.112 |
| Mindfulness - > Anxiety - > Depression | −0.170⁎⁎⁎ | 0.018 | 9.626 | <0.001 | −0.205 | −0.135 |
P < 0.01.
P < 0.001.
4. Discussion
In this study, the rates of depression, anxiety and PTSD among COVID-19 survivors were 36.2 %, 27.1 % and 15.2 % respectively, all lower than the results of a survey conducted in the beginning of the epidemic in 2020 among the hospitalized COVID-19 patients in Shanghai of China (Guo et al., 2020). The prevalence of anxiety and depression symptoms in this study was lower than the results of a survey conducted in April 2020 among the COVID-19 survivors in Wuhan of China, and the prevalence of PTSD was higher compared with the results of the Wuhan survey (12.4 %) in April 2020 (Liu et al., 2020). Although the mental health of the COVID-19 survivors could be improved to some extent over time, former studies showed that their mental health status was still worse than that of the population who had never been infected with COVID-19 (Johnson et al., 2020; Xu et al., 2021; Yue et al., 2020). Hence, the psychological effects of COVID-19 infection shouldn't be neglected in the long term (Si et al., 2021). In addition, mindfulness and resilience of the participants in this study were on a moderate level, similar with those of the general population during the COVID-19 pandemic (Antonini Philippe et al., 2021; Lee et al., 2021; Vos et al., 2021). These results indicated that the level of mindfulness and resilience were relatively stable regardless of being infected or not and might be improved via appropriate intervention, as suggested by previous studies (Saban et al., 2021; Wang et al., 2021a).
In the current study, the potential pathways of mindfulness associated with depression and PTSD were explored by structural equation modeling. The results of the model fit evaluation provided the basis for the reliability and validity of the model. The structural model indicated that mindfulness could have a direct negative effect on depression among COVID-19 survivors, which was consistent with previous research (Bergmann et al., 2021). Results of a randomized controlled trial indicated that mindfulness-based interventions delivered via mobile phones can reduce depressive symptoms of university students during the COVID-19 pandemic by 76.5 % compared with those who didn't receive interventions (Sun et al., 2021). Another study revealed that mindfulness-based intervention delivered via mobile phones could effectively reduce depressive symptoms among social workers during the pandemic (Hosseinzadeh Asl, 2021). A systematic review from the prospective of psychoneuroimmunology revealed that mindfulness-based intervention can lead to positive psychological consequences as well as positive biomarker outcomes such as decreased interleukin-6 (IL-6) and tumor necrosis factor alpha (TNF-α) in breast cancer survivors (Hulett and Armer, 2016). Another meta-analysis revealed that cytokines can lead to the dysregulation of neurogenesis in depressive disorder under a complicated mechanism, where IL-6 and TNF-α may play a key role in the pathogenesis of depressive disorders (Liu et al., 2012). Hence, the effect of mindfulness-based intervention on depressive disorders has the biological basis. Some researchers have also recommended integrating IL-6 and TNF-α into depression diagnosis and treatment, which further implied the positive effect of mindfulness-based intervention on depression (Hodes et al., 2016; Uzzan and Azab, 2021). Additionally, apart from the direct effect of mindfulness on depression, anxiety and resilience could both serve as mediators between mindfulness and depression, which is consistent with previous studies (Fenzel and Richardson, 2021; Wang et al., 2018). That is, improving mindfulness of COVID-19 survivors could help reduce anxiety symptoms and raise their resilience, which could further decrease the depressive symptoms. Those who had higher levels of mindfulness paid more attention to their current feelings, thoughts, and bodily sensations in an open and nonjudgmental way, which might enhance their awareness of their present conditions and improved their resilience in the face of negative events and reduced psychological distress, such as anxiety and depression. Higher levels of resilience enable individuals to take more positive coping strategies, mitigating the experience of depression (Xiang et al., 2020). The decrease in anxiety enables individuals to perceive stressful events as less dangerous and less threatening, and eliminate negative emotional experiences such as nervousness, thus reducing the possibility to develop into depression (Dzhambov et al., 2019; Grunberg et al., 2021; Kok et al., 2016; Ong et al., 2006; Southwick et al., 2005; Wang et al., 2018; Xiang et al., 2020). This finding revealed a pathway through which mindfulness may be associated with reduced depression among COVID-19 survivors. Therefore, it is worth considering mindfulness-based interventions among COVID-19 survivors as a viable approach to improve their resilience and reduce their anxiety symptoms, and further decrease the occurrence of their depression.
Besides depression, another key psychological outcome in this study was PTSD. Since PTSD might cause long-term negative consequences for the COVID-19 survivors, it is of great significance to explore effective ways to reduce or eliminate PTSD symptoms among this population (Moradian et al., 2020). The results indicated that mindfulness could not have direct impact on PTSD among COVID-19 survivors, which was consistent with a previous research (Aliche et al., 2021). In addition, the direct and indirect effects of resilience on PTSD were both statistically not significant. The main reason could be that mindfulness put emphasis on cultivating awareness and training the mind to stay in the present moment, while those who experienced PTSD during COVID-19 pandemic might have kept recalling and experiencing the trauma brought by their infection with COVID-19, which could offset the direct effect of mindfulness. It could also be associated with the intrusion and hyperarousal symptoms of PTSD among COVID-19 survivors (Weathers et al., 1993). A previous study showed that resilience was a potential protective factor against psychological distress, rather than against PTSD (Arnetz et al., 2013). However, the results of the current study suggested that anxiety fully mediated the effect between mindfulness and PTSD. That is, mindfulness could still be a predictor of PTSD among COVID-19 survivors by affecting anxiety first. Although previous cohort studies and randomized controlled trials showed that mindfulness reduced PTSD in various populations, the current study was the first that revealed its potential pathway among COVID-19 survivors.
The findings of this study revealed how mindfulness was associated with mental health, especially on depression and PTSD among COVID-19 survivors in Jianghan District, Wuhan, and provided evidence for mindfulness-based interventions among this population in the future. As suggested, the 6-week Mindful Living With Challenge (MLWC) training could be an option for interventions, since it integrated components of different forms of mindfulness-based interventions, such as Mindfulness-Based Stress Reduction (MBSR) and Mindful Awareness Practices (MAPs), and was specially designed for those experiencing challenging events in life, and has been systematically developed and written in a large-sample on-line randomized controlled trial protocol in Wuhan (Si et al., 2021). With the growing popularity of mobile services, more researchers attached importance to online mindfulness-based interventions (Cillessen et al., 2020; Spadaro and Hunker, 2021). Online interventions were more convenient and agreed with the rules of epidemic prevention and control in China (Ihm and Lee, 2021). In consistence with the recommendation proposed by the protocol, researchers could consider online MLWC interventions via WeChat, a popular instant messaging mobile application in China, and small programs it contains (Si et al., 2021; Tencent). Additionally, considering the psychoneuroimmunological impact of COVID-19 on mental health of patients, future telepsychiatry and immunopsychiatry services are needed to explore the association between pro-inflammatory cytokines and mental health in this population during the pandemic (Hao et al., 2020b).
This study has several limitations. First, we could not make a causal statement by drawing upon the findings of the current study due to its cross-sectional nature. Second, the mechanism of the association between mindfulness, anxiety, depression, and PTSD is yet controversial and different across studies. Contrary to the evidence and results mentioned in the current study, some studies indicated that PTSD would induce depression and anxiety, mindfulness might be a mediator between stress events and anxiety, and the association between depression and anxiety might be non-recursive (Liu et al., 2018; Tanguay-Garneau et al., 2020; Westfall et al., 2021). Third, we used the average score of FFMQ-SF scale to represent the levels of mindfulness, and explored the variables related to psychology only in the model. Fourth, selection bias due to the limited participants from one distinct and convenience sampling could reduce the representativeness of the research sample. To this end, further research employing randomized controlled trials could be considered to examine the effects of mindfulness-based interventions on the individual variables included in the model, and further meta-analyses are needed to determine the mechanism of the association between the variables mentioned in this study. Furthermore, more work is needed to investigate the relationship between specific facets of mindfulness and mental health, and to explore other possible variables mediating between mindfulness and mental health among the recovered COVID-19 patients like the related biomarkers.
5. Conclusions
There might exist a complicated mechanism, through which mindfulness affected depression and PTSD among COVID-19 survivors. The current study found that mindfulness had direct and indirect negative associations with depressive and PTSD symptoms of this population in Jianghan District, Wuhan. To reduce their depressive and PTSD symptoms, MLWC interventions delivered via mobile applications could be a choice.
CRediT authorship contribution statement
Xiaoyou Su, Zhenwei Dai, and Hao Wang prepared the first draft. Xiaoyou Su and Winnie W. S. Mak provided overall guidance. Zhenwei Dai, Hao Wang, Weijun Xiao, Yiman Huang, Mingyu Si, Jiaqi Fu, Xu Chen, Mengmeng Jia, Zhiwei Leng, Dan Cui, Liming Dong were responsible for the questionnaire survey and data analysis.
Source of funding
This work was supported by Asian Regional Special Cooperation Fund of National Health Commission of the People's Republic of China (grant numbers BLXM01); The Innovative Engineering Program sponsored by the Chinese Academy of Medical Sciences (grant numbers 2020-I2M-2-015).
Ethics approval and consent to participate
This study has been approved by the Ethics Review Committee of the Institute of Pathogen Biology, Chinese Academy of Medical Sciences, Beijing, China (IPB-2020-22).
Conflict of Interest
None.
Acknowledgements
None.
Data availability
The data that support the findings of this study are available on request from the corresponding author Xiaoyou Su.
References
- Aliche C.J., Ifeagwazi C.M., Yankouskaya A., Comoretto A., Wezyk A., Ventouris A., Panourgia C. Post-traumatic stress disorder and depressive symptoms following a herdsmen attack: the role of life meaning in mediating trait mindfulness. Stress. Health. 2021;37:528–537. [Google Scholar]
- Amadeo S., Rereao M., Vanquin David G., Nguyen N., Seguin M., Beauchamp G., Favro P., Trouche H., Malogne A., Goodfellow B., Gokalsing E., Spodenkiewicz M., Sy A., Bocage-Barthelemy Y., Sebti J., Tuheiava A., Jehel L., De Leo D. Suicide in French Polynesia: a retrospective analysis based on medicolegal documents and interview with family. J. Int. Med. Res. 2021;49 doi: 10.1177/03000605211003452. 3000605211003452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonini Philippe R., Schwab L., Biasutti M. Effects of physical activity and mindfulness on resilience and depression during the first wave of COVID-19 pandemic. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.700742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonova E., Schlosser K., Pandey R., Kumari V. Coping with COVID-19: mindfulness-based approaches for mitigating mental health crisis. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.563417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anyan F., Bizumic B., Hjemdal O. Specificity in mediated pathways by anxiety symptoms linking adolescent stress profiles to depressive symptoms: results of a moderated mediation approach. J. Affect. Disord. 2018;228:109–117. doi: 10.1016/j.jad.2017.12.011. [DOI] [PubMed] [Google Scholar]
- Arnetz J., Rofa Y., Arnetz B., Ventimiglia M., Jamil H. Resilience as a protective factor against the development of psychopathology among refugees. J. Nerv. Ment. Dis. 2013;201:167–172. doi: 10.1097/NMD.0b013e3182848afe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arthur D., Dizon D., Jooste K., Li Z., Salvador M., Yao X. Mindfulness in nursing students: the five facet mindfulness questionnaire in samples of nursing students in China, the Philippines, and South Africa. Int. J. Ment. Health Nurs. 2018;27:975–986. doi: 10.1111/inm.12405. [DOI] [PubMed] [Google Scholar]
- Baer R.A., Smith G.T., Hopkins J., Krietemeyer J., Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behan C. The benefits of meditation and mindfulness practices during times of crisis such as COVID-19. Ir. J. Psychol. Med. 2020;37:256–258. doi: 10.1017/ipm.2020.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergmann N., Hahn E., Hahne I., Zierhut M., Ta T.M.T., Bajbouj M., Pijnenborg G.H.M., Boge K. The relationship between mindfulness, depression, anxiety, and quality of life in individuals with schizophrenia Spectrum disorders. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.708808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjornsson A.S., Hardarson J.P., Valdimarsdottir A.G., Gudmundsdottir K., Tryggvadottir A., Thorarinsdottir K., Wessman I., Sigurjonsdottir O., Davidsdottir S., Thorisdottir A.S. Social trauma and its association with posttraumatic stress disorder and social anxiety disorder. J. Anxiety Disord. 2020;72 doi: 10.1016/j.janxdis.2020.102228. [DOI] [PubMed] [Google Scholar]
- Ceban F., Ling S., Lui L.M.W., Lee Y., Gill H., Teopiz K.M., Rodrigues N.B., Subramaniapillai M., Di Vincenzo J.D., Cao B., Lin K., Mansur R.B., Ho R.C., Rosenblat J.D., Miskowiak K.W., Vinberg M., Maletic V., McIntyre R.S. Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav. Immun. 2022;101:93–135. doi: 10.1016/j.bbi.2021.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan J.F., Yuan S., Kok K.H., To K.K., Chu H., Yang J., Xing F., Liu J., Yip C.C., Poon R.W., Tsoi H.W., Lo S.K., Chan K.H., Poon V.K., Chan W.M., Ip J.D., Cai J.P., Cheng V.C., Chen H., Hui C.K., Yuen K.Y. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choon-Huat Koh G., Hoenig H. How should the rehabilitation community prepare for 2019-nCoV? Arch. Phys. Med. Rehabil. 2020;101:1068–1071. doi: 10.1016/j.apmr.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cillessen L., van de Ven M.O., Compen F.R., Bisseling E.M., van der Lee M.L., Speckens A.E. Predictors and effects of usage of an online mindfulness intervention for distressed cancer patients: usability study. J. Med. Internet Res. 2020;22 doi: 10.2196/17526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conti P., Ronconi G., Caraffa A., Gallenga C.E., Ross R., Frydas I., Kritas S.K. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies. J. Biol. Regul. Homeost. Agents. 2020;34:327–331. doi: 10.23812/CONTI-E. [DOI] [PubMed] [Google Scholar]
- Conversano C., Di Giuseppe M., Miccoli M., Ciacchini R., Gemignani A., Orru G. Mindfulness, age and gender as protective factors against psychological distress during COVID-19 pandemic. Front. Psychol. 2020;11:1900. doi: 10.3389/fpsyg.2020.01900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demertzis Z.D., Dagher C., Malette K.M., Fadel R.A., Bradley P.B., Brar I., Rabbani B.T., Suleyman G. Cardiac sequelae of novel coronavirus disease 2019 (COVID-19): a clinical case series. Eur. Heart J. Case Rep. 2020;4:1–6. doi: 10.1093/ehjcr/ytaa179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzhambov A.M., Hartig T., Tilov B., Atanasova V., Makakova D.R., Dimitrova D.D. Residential greenspace is associated with mental health via intertwined capacity-building and capacity-restoring pathways. Environ. Res. 2019;178 doi: 10.1016/j.envres.2019.108708. [DOI] [PubMed] [Google Scholar]
- Fenzel L.M., Richardson K.D. The stress process among emerging adults: spirituality, mindfulness, resilience, and self-compassion as predictors of life satisfaction and depressive symptoms. J. Adult Dev. 2021;29:1–15. [Google Scholar]
- Ferreira M., Marques A., Gomes P.V. Individual resilience interventions: a systematic review in adult population samples over the last decade. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18147564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flory J.D., Yehuda R. Comorbidity between post-traumatic stress disorder and major depressive disorder: alternative explanations and treatment considerations. Dialogues Clin. Neurosci. 2015;17:141–150. doi: 10.31887/DCNS.2015.17.2/jflory. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong T.C.T., Wan A.H.Y., Wong V.P.Y., Ho R.T.H. Psychometric properties of the chinese version of five facet mindfulness questionnaire-short form in cancer patients: a bayesian structural equation modeling approach. Health Qual. Life Outcomes. 2021;19:51. doi: 10.1186/s12955-021-01692-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fornell C., Larcker D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981;18:39–50. [Google Scholar]
- Gao M., Xiao C., Zhang X., Li S., Yan H. Social capital and PTSD among PLWHA in China: the mediating role of resilience and internalized stigma. Psychol. Health Med. 2018;23:698–706. doi: 10.1080/13548506.2018.1426869. [DOI] [PubMed] [Google Scholar]
- Geisser S. A predictive approach to the random effect model. Biometrika. 1974;61:101–107. [Google Scholar]
- Goldberg S.B., Tucker R.P., Greene P.A., Davidson R.J., Wampold B.E., Kearney D.J., Simpson T.L. Mindfulness-based interventions for psychiatric disorders: a systematic review and meta-analysis. Clin. Psychol. Rev. 2018;59:52–60. doi: 10.1016/j.cpr.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong J., Chen G., Qi Z., Zhong S., Su T., Pan Y., Wang J., Huang L., Wang Y. Psychological effects of people isolated in Hubei due to COVID-19 epidemic. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.597894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grunberg V.A., Mace R.A., Bannon S.M., Greenberg J., Bakhshaie J., Vranceanu A.M. Mechanisms of change in depression and anxiety within a mind-body activity intervention for chronic pain. J. Affect. Disord. 2021;292:534–541. doi: 10.1016/j.jad.2021.05.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu J., Strauss C., Crane C., Barnhofer T., Karl A., Cavanagh K., Kuyken W. Examining the factor structure of the 39-item and 15-item versions of the five facet mindfulness questionnaire before and after mindfulness-based cognitive therapy for people with recurrent depression. Psychol. Assess. 2016;28:791–802. doi: 10.1037/pas0000263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Q., Zheng Y., Shi J., Wang J., Li G., Li C., Fromson J.A., Xu Y., Liu X., Xu H., Zhang T., Lu Y., Chen X., Hu H., Tang Y., Yang S., Zhou H., Wang X., Chen H., Wang Z., Yang Z. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav. Immun. 2020;88:17–27. doi: 10.1016/j.bbi.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y., Hu K., Li Y., Lu C., Ling K., Cai C., Wang W., Ye D. Targeting TNF-alpha for COVID-19: recent advanced and controversies. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.833967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hair J.F., Jr., Ringle C.M., Sarstedt M. Partial least squares structural equation modeling: rigorous applications, better results and higher acceptance. Long Range Plan. 2013;46:1–12. [Google Scholar]
- Hair J.F., Jr., Hult G.T.M., Jr., Ringle C.M., Jr., Sarstedt M., Jr. Second ed. SAGE; United States of America: 2017. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM) [Google Scholar]
- Hao F., Tam W., Hu X., Tan W., Jiang L., Jiang X., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., McIntyre R.S., Quek T., Tran B.X., Zhang Z., Pham H.Q., Ho C.S.H., Ho R.C.M. A quantitative and qualitative study on the neuropsychiatric sequelae of acutely ill COVID-19 inpatients in isolation facilities. Transl. Psychiatry. 2020;10:355. doi: 10.1038/s41398-020-01039-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Jiang X., McIntyre R.S., Tran B., Sun J., Zhang Z., Ho R., Ho C., Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henseler J., Ringle C.M., Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2015;43:115–135. [Google Scholar]
- Hilton L., Hempel S., Ewing B.A., Apaydin E., Xenakis L., Newberry S., Colaiaco B., Maher A.R., Shanman R.M., Sorbero M.E., Maglione M.A. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann. Behav. Med. 2017;51:199–213. doi: 10.1007/s12160-016-9844-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodes G.E., Menard C., Russo S.J. Integrating Interleukin-6 into depression diagnosis and treatment. Neurobiol. Stress. 2016;4:15–22. doi: 10.1016/j.ynstr.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz M., Wilner N., Alvarez W. Impact of event scale: a measure of subjective stress. Psychosom. Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Hosseinzadeh Asl N.R. A randomized controlled trial of a mindfulness-based intervention in social workers working during the COVID-19 crisis. Curr. Psychol. 2021:1–8. doi: 10.1007/s12144-021-02150-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou J., Wong S.Y., Lo H.H., Mak W.W., Ma H.S. Validation of a chinese version of the five facet mindfulness questionnaire in Hong Kong and development of a short form. Assessment. 2014;21:363–371. doi: 10.1177/1073191113485121. [DOI] [PubMed] [Google Scholar]
- Hou T., Xie Y., Mao X., Liu Y., Zhang J., Wen J., Chen Y., Luo Z., Cai W. The mediating role of loneliness between social support and depressive symptoms among chinese rural adolescents during COVID-19 outbreak: a comparative study between left-behind and non-left-behind students. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.740094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulett J.M., Armer J.M. A systematic review of spiritually based interventions and psychoneuroimmunological outcomes in breast cancer survivorship. Integr. Cancer Ther. 2016;15:405–423. doi: 10.1177/1534735416636222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ihm J., Lee C.J. Toward more effective public health interventions during the COVID-19 pandemic: suggesting audience segmentation based on social and media resources. Health Commun. 2021;36:98–108. doi: 10.1080/10410236.2020.1847450. [DOI] [PubMed] [Google Scholar]
- Imai R., Hori H., Itoh M., Lin M., Niwa M., Ino K., Ogawa S., Sekiguchi A., Kunugi H., Akechi T., Kamo T., Kim Y. Relationships of blood proinflammatory markers with psychological resilience and quality of life in civilian women with posttraumatic stress disorder. Sci. Rep. 2019;9:17905. doi: 10.1038/s41598-019-54508-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson S.U., Ebrahimi O.V., Hoffart A. PTSD symptoms among health workers and public service providers during the COVID-19 outbreak. PLoS One. 2020;15 doi: 10.1371/journal.pone.0241032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. Delta Trade Paperback/Bantam Dell; New York, NY, US: 2005. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness, 15th anniversary. [Google Scholar]
- Kaseda E.T., Levine A.J. Post-traumatic stress disorder: a differential diagnostic consideration for COVID-19 survivors. Clin. Neuropsychol. 2020;34:1498–1514. doi: 10.1080/13854046.2020.1811894. [DOI] [PubMed] [Google Scholar]
- Kirk M.A., Taha B., Dang K., McCague H., Hatzinakos D., Katz J., Ritvo P. A web-based cognitive behavioral therapy, mindfulness meditation, and yoga intervention for posttraumatic stress disorder: single-arm experimental clinical trial. JMIR Ment. Health. 2022;9:e26479. doi: 10.2196/26479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kok L., Sep M.S., Veldhuijzen D.S., Cornelisse S., Nierich A.P., van der Maaten J., Rosseel P.M., Hofland J., Dieleman J.M., Vinkers C.H., Joels M., van Dijk D., Group D.S., Hillegers M.H. Trait anxiety mediates the effect of stress exposure on post-traumatic stress disorder and depression risk in cardiac surgery patients. J. Affect. Disord. 2016;206:216–223. doi: 10.1016/j.jad.2016.07.020. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuffer A., Straus L.D., Prather A.A., Inslicht S.S., Richards A., Shigenaga J.K., Madden E., Metzler T.J., Neylan T.C., O'Donovan A. Altered overnight levels of pro-inflammatory cytokines in men and women with posttraumatic stress disorder. Psychoneuroendocrinology. 2019;102:114–120. doi: 10.1016/j.psyneuen.2018.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee E.K., Wong B., Chan P.H.S., Zhang D.D., Sun W., Chan D.C., Gao T., Ho F., Kwok T.C.Y., Wong S.Y. Effectiveness of a mindfulness intervention for older adults to improve emotional well-being and cognitive function in a Chinese population: a randomized waitlist-controlled trial. Int. J. Geriatr. Psychiatry. 2021;37 doi: 10.1002/gps.5616. [DOI] [PubMed] [Google Scholar]
- Li J., Chen Y.P., Zhang J., Lv M.M., Valimaki M., Li Y.F., Yang S.L., Tao Y.X., Ye B.Y., Tan C.X., Zhang J.P. The mediating role of resilience and self-esteem between life events and coping styles among rural left-behind adolescents in China: a cross-sectional study. Front Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.560556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S.M., Lau E.H.Y., Wong J.Y., Xing X., Xiang N., Wu Y., Li C., Chen Q., Li D., Liu T., Zhao J., Liu M., Tu W., Chen C., Jin L., Yang R., Wang Q., Zhou S., Wang R., Liu H., Luo Y., Liu Y., Shao G., Li H., Tao Z., Yang Y., Deng Z., Liu B., Ma Z., Zhang Y., Shi G., Lam T.T.Y., Wu J.T., Gao G.F., Cowling B.J., Yang B., Leung G.M., Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J., Ren Y.H., Gan H.J., Chen Y., Huang Y.F., You X.M. Factors associated with resilience among non-local medical workers sent to Wuhan, China during the COVID-19 outbreak. BMC Psychiatry. 2020;20:417. doi: 10.1186/s12888-020-02821-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Ho R.C., Mak A. Interleukin (IL)-6, tumour necrosis factor alpha (TNF-alpha) and soluble interleukin-2 receptors (sIL-2R) are elevated in patients with major depressive disorder: a meta-analysis and meta-regression. J. Affect. Disord. 2012;139:230–239. doi: 10.1016/j.jad.2011.08.003. [DOI] [PubMed] [Google Scholar]
- Liu Z., Sun Y.Y., Zhong B.L. Mindfulness-based stress reduction for family carers of people with dementia. Cochrane Database Syst. Rev. 2018;8 doi: 10.1002/14651858.CD012791.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W.J., Zhou L., Wang X.Q., Yang B.X., Wang Y., Jiang J.F. Mediating role of resilience in relationship between negative life events and depression among chinese adolescents. Arch. Psychiatr. Nurs. 2019;33:116–122. doi: 10.1016/j.apnu.2019.10.004. [DOI] [PubMed] [Google Scholar]
- Liu D., Baumeister R.F., Veilleux J.C., Chen C., Liu W., Yue Y., Zhang S. Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan, China. Psychiatry Res. 2020;292 doi: 10.1016/j.psychres.2020.113297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon D. Routledge Academic; Britain: 2008. Introduction to Statistical Mediation Analysis. [Google Scholar]
- Mak W.W., Chan A.T., Cheung E.Y., Lin C.L., Ngai K.C. Enhancing web-based mindfulness training for mental health promotion with the health action process approach: randomized controlled trial. J. Med. Internet Res. 2015;17 doi: 10.2196/jmir.3746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak W.W.S., Ng I.S.W., Wong C.C.Y., Law R.W. Resilience style questionnaire: development and validation among college students and cardiac patients in Hong Kong. Assessment. 2019;26:706–725. doi: 10.1177/1073191116683798. [DOI] [PubMed] [Google Scholar]
- Marx B.P., Fina B.A., Sloan D.M., Young-McCaughan S., Dondanville K.A., Tyler H.C., Blankenship A.E., Schrader C.C., Kaplan A.M., Green V.R., Bryan C.J., Hale W.J., Mintz J., Peterson A.L., Consortium S.S. Written exposure therapy for posttraumatic stress symptoms and suicide risk: design and methodology of a randomized controlled trial with patients on a military psychiatric inpatient unit. Contemp. Clin. Trials. 2021;110 doi: 10.1016/j.cct.2021.106564. [DOI] [PubMed] [Google Scholar]
- Mazza M.G., De Lorenzo R., Conte C., Poletti S., Vai B., Bollettini I., Melloni E.M.T., Furlan R., Ciceri F., Rovere-Querini P., Group C.-B.O.C.S., Benedetti F. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav. Immun. 2020;89:594–600. doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng Y., Mao K., Li C. Validation of a short-form five facet mindfulness questionnaire instrument in China. Front. Psychol. 2019;10:3031. doi: 10.3389/fpsyg.2019.03031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miao Q., Xie L., Xing B., Wang X., Tang S., Luo H. Emotional states and coping methods in nursing and non-nursing students responding to COVID-19: a cross-sectional study in China. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-054007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michel J.P., Maggi S., Ecarnot F. Raising awareness of the needs of older COVID patients after hospital discharge. Aging Clin. Exp. Res. 2020;32:1595–1598. doi: 10.1007/s40520-020-01620-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moradian S.T., Parandeh A., Khalili R., Karimi L. Delayed symptoms in patients recovered from COVID-19. Iran. J. Public Health. 2020;49:2120–2127. doi: 10.18502/ijph.v49i11.4729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nearchou F., Douglas E. Traumatic distress of COVID-19 and depression in the general population: exploring the role of resilience, anxiety, and Hope. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18168485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong A.D., Bergeman C.S., Bisconti T.L., Wallace K.A. Psychological resilience, positive emotions, and successful adaptation to stress in later life. J. Pers. Soc. Psychol. 2006;91:730–749. doi: 10.1037/0022-3514.91.4.730. [DOI] [PubMed] [Google Scholar]
- Rakesh G., Morey R.A., Zannas A.S., Malik Z., Marx C.E., Clausen A.N., Kritzer M.D., Szabo S.T. Resilience as a translational endpoint in the treatment of PTSD. Mol. Psychiatry. 2019;24:1268–1283. doi: 10.1038/s41380-019-0383-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renaud-Charest O., Lui L.M.W., Eskander S., Ceban F., Ho R., Di Vincenzo J.D., Rosenblat J.D., Lee Y., Subramaniapillai M., McIntyre R.S. Onset and frequency of depression in post-COVID-19 syndrome: a systematic review. J. Psychiatr. Res. 2021;144:129–137. doi: 10.1016/j.jpsychires.2021.09.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saban M., Dagan E., Drach-Zahavy A. The effects of a novel mindfulness-based intervention on Nurses' state mindfulness and patient satisfaction in the emergency department. J. Emerg. Nurs. 2021;47:412–425. doi: 10.1016/j.jen.2020.09.009. [DOI] [PubMed] [Google Scholar]
- Sanada K., Montero-Marin J., Barcelo-Soler A., Ikuse D., Ota M., Hirata A., Yoshizawa A., Hatanaka R., Valero M.S., Demarzo M., Campayo J.G., Iwanami A. Effects of mindfulness-based interventions on biomarkers and low-grade inflammation in patients with psychiatric disorders: a meta-analytic review. Int. J. Mol. Sci. 2020;21 doi: 10.3390/ijms21072484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen H., Gelaye B., Huang H., Rondon M.B., Sanchez S., Duncan L.E. Polygenic prediction and GWAS of depression, PTSD, and suicidal ideation/self-harm in a peruvian cohort. Neuropsychopharmacology. 2020;45:1595–1602. doi: 10.1038/s41386-020-0603-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Si M.Y., Xiao W.J., Pan C., Wang H., Huang Y.M., Lian J., Mak W.W.S., Leng Z.W., Su X.Y., Tang Q.P., Jiang Y., Feng L.Z., Yang W.Z., Wang C. Mindfulness-based online intervention on mental health and quality of life among COVID-19 patients in China: an intervention design. Infect. Dis. Poverty. 2021;10:69. doi: 10.1186/s40249-021-00836-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southwick S.M., Vythilingam M., Charney D.S. The psychobiology of depression and resilience to stress: implications for prevention and treatment. Annu. Rev. Clin. Psychol. 2005;1:255–291. doi: 10.1146/annurev.clinpsy.1.102803.143948. [DOI] [PubMed] [Google Scholar]
- Spadaro K.C., Hunker D.F. Experience of an 8-week online mindfulness intervention for nursing students: qualitative findings. Nurse Educ. 2021;46:187–191. doi: 10.1097/NNE.0000000000000881. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stone M. Cross-validatory choice and assessment of statistical predictions. J. R. Stat. Soc. Ser. B Methodol. 1974;36:111–133. [Google Scholar]
- Sun S., Lin D., Goldberg S., Shen Z., Chen P., Qiao S., Brewer J., Loucks E., Operario D. A mindfulness-based mobile health (mHealth) intervention among psychologically distressed university students in quarantine during the COVID-19 pandemic: a randomized controlled trial. J. Couns. Psychol. 2021;69:157–171. doi: 10.1037/cou0000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanguay-Garneau L., Boivin M., Feng B., Matte-Landry A., Brendgen M., Vitaro F., Dionne G. A genetic cross-lagged study of the longitudinal association between anxiety and depressive symptoms during childhood. Behav. Genet. 2020;50:105–118. doi: 10.1007/s10519-019-09988-1. [DOI] [PubMed] [Google Scholar]
- Tencent, n.d., Tencent , WeChat.
- de la Torre-Cruz T., Luis-Rico I., di Giusto-Valle C., Escolar-Llamazares M.C., Hortiguela-Alcala D., Palmero-Camara C., Jimenez A. A mediation model between self-esteem, anxiety, and depression in sport: the role of gender differences in speleologists. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18168765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uzzan S., Azab A.N. Anti-TNF-alpha compounds as a treatment for depression. Molecules. 2021;26 doi: 10.3390/molecules26082368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vos L.M.W., Habibovic M., Nyklicek I., Smeets T., Mertens G. Optimism, mindfulness, and resilience as potential protective factors for the mental health consequences of fear of the coronavirus. Psychiatry Res. 2021;300 doi: 10.1016/j.psychres.2021.113927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller M.A. Resilience in ecosystemic context: evolution of the concept. Am. J. Orthopsychiatry. 2001;71:290–297. doi: 10.1037/0002-9432.71.3.290. [DOI] [PubMed] [Google Scholar]
- Wang T., Li M., Xu S., Jiang C., Gao D., Wu T., Lu F., Liu B., Wang J. The factorial structure of trait anxiety and its mediating effect between mindfulness and depression. Front Psychiatry. 2018;9:514. doi: 10.3389/fpsyt.2018.00514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M., Hua Y., Liu X., Chen Y., Xiao T., Su X., Shao P., Ni C., Yang S. Effects of an empowerment-based intervention on health-related knowledge and resilience in patients with coronary artery stent implantation. Patient Educ. Couns. 2021;104:375–380. doi: 10.1016/j.pec.2020.07.023. [DOI] [PubMed] [Google Scholar]
- Wang P.R., Oyem P.C., Viguera A.C. Prevalence of psychiatric morbidity following discharge after COVID-19 hospitalization. Gen. Hosp. Psychiatry. 2021;69:131–132. doi: 10.1016/j.genhosppsych.2020.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F., Litz B., Herman D., Huska J.A., Keane T. Paper Presented at the Annual Convention of the International Society for Traumatic Stress Studies. 1993. The PTSD checklist (PCL): reliability, validity, and diagnostic utility. [Google Scholar]
- Weiss D.S., Marmar C.R. The Impact of Event Scale—Revised, Assessing psychological trauma and PTSD. The Guilford Press; New York, NY, US: 1997. pp. 399–411. [Google Scholar]
- Westfall S., Caracci F., Estill M., Frolinger T., Shen L., Pasinetti G.M. Chronic stress-induced depression and anxiety priming modulated by gut-brain-Axis immunity. Front. Immunol. 2021;12 doi: 10.3389/fimmu.2021.670500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2022. WHO Coronavirus (COVID-19) Dashboard. [Google Scholar]
- WHO . 2022. WHO Coronavirus (COVID-19) Dashboard of China. [Google Scholar]
- Xiang Y., Dong X., Zhao J. Effects of envy on depression: the mediating roles of psychological resilience and social support. Psychiatry Investig. 2020;17:547–555. doi: 10.30773/pi.2019.0266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Tong Z., Guan X., Du B., Qiu H., Slutsky A.S. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med. 2020;46:837–840. doi: 10.1007/s00134-020-05979-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong Q., Xu M., Li J., Liu Y., Zhang J., Xu Y., Dong W. Clinical sequelae of COVID-19 survivors in Wuhan, China: a single-Centre longitudinal study. Clin. Microbiol. Infect. 2021;27:89–95. doi: 10.1016/j.cmi.2020.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y., Su S., Jiang Z., Guo S., Lu Q., Liu L., Zhao Y., Wu P., Que J., Shi L., Deng J., Meng S., Yan W., Sun Y., Yuan K., Lin X., Sun S., Ravindran A.V., Chen S., Wing Y.K., Tang X., Ran M., Lu Y., Shi J., Huang G., Bao Y., Lu L. Prevalence and risk factors of mental health symptoms and suicidal behavior among university students in Wuhan, China during the COVID-19 pandemic. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.695017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y.Y., Wei Z.J., Zhang Y.C., Li X., Gong L., Zhou J.W., Wang Y., Zhang Y.Y., Wang R.P. Functional disability after ischemic stroke: a community-based cross-sectional study in Shanghai, China. Front. Neurol. 2021;12 doi: 10.3389/fneur.2021.649088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yue J., Zang X., Le Y., An Y. Anxiety, depression and PTSD among children and their parent during 2019 novel coronavirus disease (COVID-19) outbreak in China. Curr. Psychol. 2020:1–8. doi: 10.1007/s12144-020-01191-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y., Xiao L., Huang Y., Wang Q., Xie Y., Wang H., Wang G. Possible vicarious traumatization among psychiatric inpatients during the remission phase of the COVID-19: a single-center cross-sectional study. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.677082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J.L., Schülke R., Vatansever D., Xi D., Yan J., Zhao H., Xie X., Feng J., Chen M.Y., Sahakian B.J., Wang S. Mindfulness practice for protecting mental health during the COVID-19 pandemic. Transl. Psychiatry. 2021;11:329. doi: 10.1038/s41398-021-01459-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author Xiaoyou Su.