Abstract
Background
Overactive bladder is a common, long‐term symptom complex, which includes frequency of micturition, urgency with or without associated incontinence and nocturia. Around 11% of the population have symptoms, with this figure increasing with age. Symptoms can be linked to social anxiety and adaptive behavioural change. The cost of treating overactive bladder is considerable, with current treatments varying in effectiveness and being associated with side effects. Acupuncture has been suggested as an alternative treatment.
Objectives
To assess the effects of acupuncture for treating overactive bladder in adults, and to summarise the principal findings of relevant economic evaluations.
Search methods
We searched the Cochrane Incontinence Specialised Register, which contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (including In‐Process, Epub Ahead of Print, Daily), ClinicalTrials.gov and WHO ICTRP (searched 14 May 2022). We also searched the Allied and Complementary Medicine database (AMED) and bibliographic databases where knowledge of the Chinese language was necessary: China National Knowledge Infrastructure (CNKI); Chinese Science and Technology Periodical Database (VIP) and WANFANG (China Online Journals), as well as the reference lists of relevant articles.
Selection criteria
We included randomised controlled trials (RCTs), quasi‐RCTs and cross‐over RCTs assessing the effects of acupuncture for treating overactive bladder in adults.
Data collection and analysis
Four review authors formed pairs to assess study eligibility and extract data. Both pairs used Covidence software to perform screening and data extraction. We assessed risk of bias using Cochrane's risk of bias tool and assessed heterogeneity using the Chi2 testand I2 statistic generated within the meta‐analyses. We used a fixed‐effect model within the meta‐analyses unless there was a moderate or high level of heterogeneity, where we employed a random‐effects model. We used the GRADE approach to assess the certainty of evidence.
Main results
We included 15 studies involving 1395 participants in this review (14 RCTs and one quasi‐RCT). All included studies raised some concerns regarding risk of bias. Blinding of participants to treatment group was only achieved in 20% of studies, we considered blinding of outcome assessors and allocation concealment to be low risk in only 25% of the studies, and random sequence generation to be either unclear or high risk in more than 50% of the studies.
Acupuncture versus no treatment
One study compared acupuncture to no treatment. The evidence is very uncertain regarding the effect of acupuncture compared to no treatment in curing or improving overactive bladder symptoms and on the number of minor adverse events (both very low‐certainty evidence). The study report explicitly stated that no major adverse events occurred. The study did not report on the presence or absence of urinary urgency, episodes of urinary incontinence, daytime urinary frequency or episodes of nocturia.
Acupuncture versus sham acupuncture
Five studies compared acupuncture with sham acupuncture. The evidence is very uncertain about the effect of acupuncture on curing or improving overactive bladder symptoms compared to sham acupuncture (standardised mean difference (SMD) ‐0.36, 95% confidence interval (CI) ‐1.03 to 0.31; 3 studies; 151 participants; I2 = 65%; very low‐certainty evidence). All five studies explicitly stated that there were no major adverse events observed during the study. Moderate‐certainty evidence suggests that acupuncture probably makes no difference to the incidence of minor adverse events compared to sham acupuncture (risk ratio (RR) 1.28, 95% CI 0.30 to 5.36; 4 studies; 222 participants; I² = 0%). Only one small study reported data for the presence or absence of urgency and for episodes of nocturia. The evidence is of very low certainty for both of these outcomes and in both cases the lower confidence interval is implausible. Moderate‐certainty evidence suggests there is probably little or no difference in episodes of urinary incontinence between acupuncture and sham acupuncture (mean difference (MD) 0.55, 95% CI ‐1.51 to 2.60; 2 studies; 121 participants; I2 = 57%). Two studies recorded data regarding daytime urinary frequency but we could not combine them in a meta‐analysis due to differences in methodologies (very low‐certainty evidence).
Acupuncture versus medication
Eleven studies compared acupuncture with medication. Low‐certainty evidence suggests that acupuncture may slightly increase how many people's overactive bladder symptoms are cured or improved compared to medication (RR 1.25, 95% CI 1.10 to 1.43; 5 studies; 258 participants; I2 = 19%). Low‐certainty evidence suggests that acupuncture may reduce the incidence of minor adverse events when compared to medication (RR 0.34, 95% CI 0.26 to 0.45; 8 studies; 1004 participants; I² = 51%). The evidence is uncertain regarding the effect of acupuncture on the presence or absence of urinary urgency (MD ‐0.40, 95% CI ‐0.56 to ‐0.24; 2 studies; 80 participants; I2 = 0%; very low‐certainty evidence) and episodes of urinary incontinence (MD ‐0.33, 95% CI ‐2.75 to 2.09; 1 study; 20 participants; very low‐certainty evidence) compared to medication. Low‐certainty evidence suggests there may be little to no effect of acupuncture compared to medication in terms of daytime urinary frequency (MD 0.73, 95% CI ‐0.39 to 1.85; 4 studies; 360 participants; I2 = 28%). Acupuncture may slightly reduce the number of nocturia episodes compared to medication (MD ‐0.50, 95% CI ‐0.65 to ‐0.36; 2 studies; 80 participants; I2 = 0%, low‐certainty evidence).
There were no incidences of major adverse events in any of the included studies. However, major adverse events are rare in acupuncture trials and the numbers included in this review may be insufficient to detect these events.
Authors' conclusions
The evidence is very uncertain about the effect acupuncture has on cure or improvement of overactive bladder symptoms compared to no treatment. It is uncertain if there is any difference between acupuncture and sham acupuncture in cure or improvement of overactive bladder symptoms. This review provides low‐certainty evidence that acupuncture may result in a slight increase in cure or improvement of overactive bladder symptoms when compared with medication and may reduce the incidence of minor adverse events.
These conclusions must remain tentative until the completion of larger, higher‐quality studies that use relevant, comparable outcomes. Timing and frequency of treatment, point selection, application and long‐term follow‐up are other areas relevant for research.
Plain language summary
Acupuncture for treating overactive bladder in adults
Review question
Is acupuncture a safe and effective treatment for treating overactive bladder in adults?
Background
Overactive bladder is the term used to describe a group of urinary symptoms, including an urgent need to pass urine, frequent voiding (emptying), urinary incontinence and waking one or more times at night to pass urine (nocturia). Sufferers may have one or more of these symptoms. Overactive bladder is a common complaint and can affect both men and women of any age, though it is more common in older people. Treatment can include bladder education, pelvic floor exercises, medication, botox injections into the bladder wall, sacral neuromodulation and surgery.
Acupuncture refers to the practice of inserting fine needles into defined points on the body in order to achieve an improvement in health. It is used in a wide range of conditions and has been suggested as a possible treatment for overactive bladder symptoms.
How up‐to‐date is this review?
This review includes all studies that met our eligibility criteria, published up to 14 May 2022. We are aware of six ongoing studies and two studies that we cannot obtain in full, which were not included in our review.
Study characteristics
We included 15 studies involving a total of 1395 participants with overactive bladder. The majority of the studies had small numbers of participants and we had some reservations about the study designs, processes or both in the majority of the studies.
Study funding sources
Of the 15 included studies, four were supported by Chinese Government‐funded research grants and two were funded by Higher Education institutions. The open access publishing fee for one study was paid by the Norwegian Acupuncture Association. Eight studies did not report any source of funding.
Key results
The different methods used by the studies made the comparison of results difficult.
Compared to no treatment, the effect of acupuncture on curing or improving overactive bladder symptoms and the amount of minor side effects is very uncertain. No major adverse events took place. The were no reports on the effect of acupuncture compared to no treatment with regard to reducing urinary urgency, daytime urinary frequency, episodes of urinary incontinence or episodes of nocturia.
Compared to sham (fake) acupuncture, the effect of acupuncture on curing or improving overactive bladder symptoms is uncertain. Acupuncture probably makes little or no difference to the number of minor adverse events compared to sham acupuncture. No major adverse events took place in any of the studies. The evidence is very uncertain regarding the effect of acupuncture on the presence of absence of urinary urgency, daytime urinary frequency or episodes of nocturia. There is probably no difference between acupuncture and sham acupuncture in terms of episodes of urinary incontinence.
Acupuncture may result in a slight improvement in overactive bladder symptoms when compared with medication and may result in a reduced number of minor adverse events. No major adverse events took place. The effect of acupuncture compared to medication is very uncertain with regard to urinary urgency and episodes of incontinence. Acupuncture may have the same effect as medication on urinary frequency and may slightly reduce episodes of nocturia.
Certainty of the evidence
The majority of the evidence in this review is of very low or low certainty because the included studies had flaws in their design and/or execution. Many had small numbers of participants and were conducted over a short period of time. Given these issues, it is difficult to draw conclusions regarding how effective acupuncture is for treating overactive bladder. Further well‐designed, large‐scale studies are required to answer this question.
Summary of findings
Summary of findings 1. Acupuncture compared to no treatment for overactive bladder in adults.
| Acupuncture compared to no treatment for overactive bladder in adults | ||||||
| Patient or population: overactive bladder in adults Setting: outpatient clinics Intervention: acupuncture Comparison: no treatment | ||||||
| Anticipated absolute effects* (95% CI) | ||||||
| Outcomes | Risk with no treatment | Risk with acupuncture | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Overactive bladder symptoms cured or improved Assessed with ICIQ‐SF | One study compared active treatment with acupuncture to women on a waiting list (no treatment group). Urinary symptoms were assessed using the ICIQ‐SF after 12 weeks. The acupuncture group had a median score of 6.5 (IQR 4); the no treatment group had a median score of 10 (IQR 7.3). There were 12 participants in both groups. | — | 24 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b | The evidence is very uncertain about the effect of acupuncture versus no treatment on the cure or improvement of overactive bladder symptoms. | |
| Number of major adverse events | There were no incidences of major adverse events in the included study. | — | 24 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b | The evidence is very uncertain about the effect of acupuncture on the number of major adverse events. | |
| Number of minor adverse events | There were 2 minor adverse events reported in the acupuncture group; 1 of tiredness and 1 of an initial increase in urinary symptoms. There were no reports of minor adverse events in the no treatment group. | — | 24 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b | The evidence is very uncertain about the effect of acupuncture on the number of minor adverse events. | |
| Presence or absence of urinary urgency | This outcome was not reported. | |||||
| Episodes of urinary incontinence in a 24‐hour period | This outcome was not reported. | |||||
| Daytime urinary frequency | This outcome was not reported. | |||||
| Episodes of nocturia | This outcome was not reported. | |||||
| * The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; ICIQ‐SF: International Consultation on Incontinence Questionnaire‐Urinary Incontinence Short Form; IQR: interquartile range; RCT: randomised controlled trial | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded once for serious risk of bias: concerns surrounding lack of blinding of participants, study personnel and outcome assessors.
bDowngraded once for very serious imprecision: small sample sizes.
Summary of findings 2. Acupuncture compared to sham acupuncture for overactive bladder in adults.
| Acupuncture compared to sham acupuncture for overactive bladder in adults | ||||||
| Patient or population: overactive bladder in adults Setting: outpatient clinics Intervention: acupuncture Comparison: sham acupuncture | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with sham acupuncture | Risk with acupuncture | |||||
| Overactive bladder symptoms cured or improved Assessed with a validated urinary symptoms patient reported outcome measure | — | — | SMD ‐0.36 (‐1.03 lower to 0.31 higher) | 151 (3 RCTs) |
⊕⊝⊝⊝ Very lowa, b, c |
The evidence is very uncertain about the effect of acupuncture on the cure or improvement of urinary symptoms. |
| Number of major adverse events | There were no incidences of major adverse events in any of the included studies. | 236 (5 RCTs) |
⊕⊕⊝⊝ Lowd |
The number of participants is too low to detect a rare event. | ||
| Number of minor adverse events | 28 per 1000 |
36 per 1000 (8.4 to 150) |
RR 1.28 (0.30 to 5.36) |
222 (4 RCTs) |
⊕⊕⊕⊝ Moderatec |
There is no evidence of a difference in the number of minor adverse events |
| Presence or absence of urinary urgency Assessed with bladder diary data ‐ episodes per day | Mean 7.69 episodes per day | Mean 3.17 episodes per day (0 to 9.98) |
MD 4.52 lower (11.33 lower to 2.29 higher) |
25 (1 RCT) |
⊕⊝⊝⊝ Very lowe, f |
The evidence is very uncertain about the effect of acupuncture on the presence or absence of urinary urgency. The lower confidence interval is implausible. |
| Episodes of urinary incontinence in a 24‐hour period | Mean 2.5 episodes in a 24‐hour period | Mean 3.05 episodes in a 24‐hour period (0.99 to 5.1) |
MD 0.55 higher (1.51 lower to 2.60 higher) |
121 (2 RCTs) |
⊕⊕⊕⊝ Moderatec |
Acupuncture probably results in little to no difference in episodes of urinary incontinence in a 24‐hour period. |
| Daytime urinary frequency Assessed with bladder diary data ‐ episodes per day | Two studies reported on frequency of micturition. One study reported the number of voiding episodes in a 24‐hour period: true acupuncture mean 11.58 versus sham acupuncture mean 13.62. One study compared time between voids. Following treatment, 11 in the acupuncture group could delay more than 2 hours between voids versus 0 in the sham acupuncture group. |
77 (2 RCTs) |
⊕⊝⊝⊝ Very lowg, h |
The evidence is very uncertain about the effect of acupuncture on daytime urinary frequency | ||
| Episodes of nocturia Assessed with bladder diary data ‐ episodes per night | Mean3.85 episodes of nocturia per night | Mean1.33 (0 to 4.09) |
MD 2.52 lower (4.80 lower to 0.24 lower) |
25 (1 RCT) |
⊕⊝⊝⊝ Very lowe, f |
The evidence is very uncertain about the effect of acupuncture on episodes of nocturia. The lower confidence interval is implausible. |
| * The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; MD: mean difference; RCT: randomised controlled trial; RR: risk ratio; SMD: standardised mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded once for serious risk of bias: lack of blinding of outcome assessors.
bDowngraded once for serious inconsistency: moderate heterogeneity between studies.
cDowngraded once for serious imprecision: small sample sizes.
dDowngraded twice for very serious imprecision: small numbers of participants to detect a rare event.
eDowngraded once for serious risk of bias: lack of blinding to group allocation for all outcomes.
fDowngraded twice for very serious imprecision: small participant numbers and very wide confidence intervals.
gDowngraded once for serious risk of bias: lack of blinding of outcome assessors.
hDowngraded once for indirectness: different ways of measuring the outcome used.
Summary of findings 3. Acupuncture compared to medication for overactive bladder in adults.
| Acupuncture compared to medication for overactive bladder in adults | ||||||
| Patient or population: overactive bladder in adults Setting: outpatient clinics Intervention: acupuncture Comparison: medication | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with medication | Risk with acupuncture | |||||
| Overactive bladder symptoms cured or improved Assessed with total effective rate | 703 per 1000 |
879 per 1000 (773 to 1000) |
RR 1.25 (1.10 to 1.43) |
258 (5 RCTs) |
⊕⊕⊝⊝ Lowa, b |
Acupuncture may result in a slight increase in cure or improvement in urinary symptoms. The upper limit in the risk with acupuncture group is implausible. |
| Number of major adverse events | No studies reported any major adverse effects | 927 (14 RCTs) |
⊕⊕⊝⊝ Lowc |
The number of participants is too low to detect a rare event. | ||
| Number of minor adverse events | 307 per 1000 |
77 per 1000 (56 to 107) |
RR 0.34 (0.26 to 0.45) |
1004 (8 RCTs) |
⊕⊕⊝⊝ Lowd, e |
Acupuncture may reduce the number of minor adverse events. |
| Presence or absence of urinary urgency Assessed with episodes per day | Mean 2.36 episodes per day | Mean 1.96 (1.8 to 2.12) |
MD 0.4 lower (0.56 lower to 0.24 lower) |
80 (2 RCTs) |
⊕⊝⊝⊝ Very lowf, g |
The evidence is uncertain about the effect of acupuncture on presence or absence of urinary urgency. |
|
Daytime urinary frequency Assessed with voids per day |
Mean 8.47 voids per day | Mean9.2 (8.1 to 10.3) |
MD 0.73 higher (0.39 lower to 1.85 higher |
360 (4 RCTs) |
⊕⊕⊝⊝ Lowb,h |
Acupuncture may result in little to no effect on daytime frequency. |
| Episodes of urinary incontinence in a 24‐hour period | Mean 1.17 episodes per day | Mean 0.84 (0 to 3.26) |
MD 0.33 lower (2.75 lower to 2.09 higher) |
20 (1 RCT) |
⊕⊝⊝⊝ Very lowi |
The evidence is very uncertain about the effect of acupuncture on episodes of urinary incontinence in a 24‐hour period. |
| Episodes of nocturia Assessed with episodes per night | Mean 1.63 episodes per night | Mean 1.13 (0.98 to 1.27) |
MD 0.5 lower (0.65 lower to 0.36 lower) |
80 (2 RCTs) |
⊕⊕⊝⊝ Lowf,g |
Acupuncture may reduce episodes of nocturia slightly. |
| * The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; MD: mean difference; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded once for serious risk of bias: two studies have at least one category judged at high risk of bias.
bDowngraded once for serious imprecision: small numbers of participants.
cDowngraded twice for very serious imprecision: low participant numbers to detect a rare event.
dDowngraded once for serious imprecision: wide confidence intervals.
eDowngraded once for serious imprecision: high heterogeneity between studies.
fDowngraded once for serious risk of bias: unclear risk of bias in several categories in both studies.
gDowngraded twice for very serious imprecision: small numbers of participants and very wide confidence intervals in both studies.
hDowngraded once for serious risk of bias: all studies had at least one category judged at unclear risk of bias.
iDowngraded twice for very serious imprecision due to very small numbers of participants.
Background
For a glossary of terms used, see Appendix 1.
Description of the condition
Overactive bladder (OAB) is defined by the International Continence Society as "urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence, in the absence of urinary tract infection or other obvious pathology" (Abrams 2017). Overactive bladder can be further categorised into "OAB‐dry" (where urinary incontinence is absent) and "OAB‐wet" (where urinary incontinence is present) (Abrams 2017). Abrams 2012 reported that urinary frequency accompanies overactive bladder in 20% to 25% of cases, and nocturia in 70% to 75% of cases. Around one in three people with overactive bladder also experience urinary incontinence (Irwin 2006).
Overactive bladder is common. An epidemiological study conducted in five countries (Canada, Sweden, Italy, Germany and the UK), including 19,165 participants, reported that 11.8% of the population had overactive bladder symptoms, with slightly more women affected (12.8%) than men (10.8%) (Irwin 2006). This is equivalent to one in nine of the general adult population (Irwin 2006). Furthermore, the prevalence of overactive bladder increases with age: symptoms are reported to occur in 40% of men and 46% of women aged 65 years or over (Sexton 2011).
The exact pathophysiology underlying overactive bladder is not fully understood but several processes are believed to contribute to developing symptoms (Malde 2018). These processes include: abnormal secretion of acetylcholine during bladder filling, which may result in afferent activation; compounds released by urothelial cells, which may affect cell signalling; alteration in smooth muscle properties; abnormal afferent activity resulting in increased efferent responses, which compromises voluntary bladder control; and altered cognitive responses, specifically in the orbitofrontal cortex.
Overactive bladder is usually diagnosed by a thorough history and physical examination. Validated symptom questionnaires are used to document and quantify symptoms, while clinical examination can help to exclude other causes of lower urinary tract symptoms (LUTS). A bladder diary can assess the frequency and severity of symptoms (NICE 2019).
Overactive bladder is most often present when there is no underlying neurological disease; this is known as idiopathic overactive bladder. However, it is also sometimes associated with neurological conditions, including stroke, Parkinson's disease, multiple sclerosis and spinal cord injury. People presenting with overactive bladder should be screened to rule out neurological causes (Tse 2016).
In one survey, 88% of participants reported experiencing symptoms for over 10 years (Rantell 2017). Participants reported negative effects on physical, social, domestic, occupational and sexual domains. Overactive bladder is a long‐term condition that reduces quality of life, leading to increased anxiety and depression and a negative effect on self‐esteem (Lai 2016; Tubaro 2004; Wein 2009). Additionally, it has been reported that people with LUTS and depression are at a greater risk of developing dementia (Ou 2019).
Given the high prevalence of overactive bladder, treatment costs are significant. The National Overactive Bladder Evaluation Programme (NOBLE) cited the cost of treating overactive bladder in the USA as USD 12.02 billion (Hu 2003). A further study estimated that the cost of providing care would rise with an aging population; projected costs for 2020 were USD 82.6 billion per annum (Ganz 2010). In addition to the clinical implications and quality of life implications associated with overactive bladder, there are significant implications associated with its management. For example, a recent review found that direct overactive bladder related costs in the US ranged between USD 656 to 860 per patient annually (USD 2016) (Powell 2018). This demonstrates the importance of finding management strategies that are both clinically effective in managing symptoms and also a good use of resources for the healthcare system.
Description of the intervention
Initial treatment for overactive bladder includes lifestyle modification, pelvic floor exercises and fluid management. Where these are unsuccessful, people are offered anticholinergic drugs or β3‐adrenoreceptor agonists. If medications do not control symptoms, surgical interventions may be required. Surgical treatment for overactive bladder includes intravesical botulinum toxin injection, sacral neuromodulation, augmentation cystoplasty and urinary diversion (NICE 2019). Although acupuncture is not currently offered universally as a treatment for overactive bladder, there is a growing body of literature that reports positive outcomes for overactive bladder sufferers (Aydoğmuş 2014; Yuan 2015; Zhao 2018).
Acupuncture refers to the practice of inserting multiple fine needles throughout the body in order to achieve a positive physiological response (White 2009). Needling can be performed: within the dermatome of the affected area; at prominent acupoints found throughout the body which, according to Traditional Chinese Medicine (TCM) theory, have specific effects on symptoms; on the visible part of the ear (the auricle); and with the addition of electrical stimulation (electroacupuncture). Acupuncture has been adapted by specific cultures (for example, Japanese and Korean acupuncture) and can take many alternative forms.
Acupuncture is practised widely throughout Asia, Europe and Northern America and has a low adverse event risk profile, with the most common adverse events being reported as transient (Clarkson 2015; MacPherson 2001). Examples of adverse events reported in the literature include bleeding at the site of needle insertion, pain at the site of the inserted needle or an initial increase in pain at the site of injury (Witt 2009).
A typical acupuncture session may last between 15 and 40 minutes. Needles may be stimulated, either manually by the clinician (needles turned in the acupoint) periodically throughout the session, or continually through an electroacupuncture device that delivers an electrical current. The frequency and duration of treatment may vary depending on clinician preference and patient response.
How the intervention might work
While the exact mechanism by which acupuncture may influence overactive bladder remains unclear, several theories exist. Sensory information from afferent nerves from the pelvic, pudendal and hypogastric nerve roots directly relate to the lower urinary tract (Pullman 2016). Needling within the skin and muscles that these nerves supply may reduce overactive bladder through inhibition of peripheral nerves (Hino 2010), via brain areas that control bladder activity (Wang 2012). Furthermore, the brain bladder control matrix, where the periaqueductal gray, limbic system and prefrontal cortex are believed to have a large influence upon the bladder’s function, have been found to alter during and after a course of acupuncture (Dhond 2008; Huang 2012). This infers that the beneficial effects of acupuncture on overactive bladder symptoms could be partially explained through signalling changes from the central nervous system to the bladder. Acupuncture has been shown to exert an effect on the autonomic nervous system (Napadow 2013), further endorsing the view that acupuncture can influence the nervous system and therefore may affect symptoms arising from a disturbance in this system.
In Traditional Chinese Medicine (TCM) theory, the maintenance of health and well‐being is dependent upon the quality of energy (Qi), which emanates from the visceral organs. When Qi becomes unbalanced, symptoms of ill health occur. In the case of overactive bladder, this would be attributable to deficient kidney and bladder Qi (Maciocia 2007). In TCM, Qi is thought to pass through the body via channels called meridians. These are not anatomical structures and some dispute their existence. Acupoints on the bladder, kidney and spleen meridians are believed to directly benefit urinary symptoms by restoring Qi balance (Maciocia 2007). There is debate between acupuncture practitioners regarding the concepts described and further high‐quality research is required to explore the putative mechanisms underpinning the observed effects of acupuncture.
Why it is important to do this review
There are specific concerns and side effects linked to some treatments for overactive bladder. The additive effect of anticholingeric medications may be linked to the development of dementia (Gray 2015). Surgical treatments are invasive, may be contraindicated, or carry a significant risk in older people who are more likely to have co‐morbidities. Surgical interventions have a significantly higher risk profile and recovery period when compared to acupuncture (NICE 2019; Witt 2009). In light of this, it is important to investigate alternative strategies for managing overactive bladder.
Published Cochrane Reviews concerning the treatment of overactive bladder include: anticholinergics (Madhuvrata 2012); implanted sacral neuromodulation (Herbison 2009); onabotulinumtoxin A (Duthie 2011); and bladder training (Wallace 2004). Currently, the role of acupuncture in the treatment of overactive bladder has not been assessed in a Cochrane Review. The efficacy of acupuncture is uncertain; there is no consensus with regard to treatment protocols and it is anticipated that some of the research available may be of poor quality (Forde 2016). Therefore, this review aims to establish the risk of bias and quality of reporting and clinical outcomes of existing acupuncture research for overactive bladder.
Objectives
To assess the effects of acupuncture for treating overactive bladder in adults.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), quasi‐RCTs (in which randomisation may be predictable, such as the allocation of participants by day of the week, date of birth or sequence of entry into the trial), and cross‐over trials of acupuncture for treating overactive bladder in adults.
Types of participants
We included studies of adults aged over 18 years with a diagnosis of overactive bladder that fits the criteria defined by the International Continence Society as "urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence, in the absence of urinary tract infection or other obvious pathology" (Abrams 2017).
This review addresses treatment for idiopathic overactive bladder; we therefore excluded participants who have overactive bladder symptoms that are a manifestation of a neurological condition (e.g. multiple sclerosis, Parkinson's disease, stroke).
Types of interventions
We included studies of acupuncture that intended to treat the symptoms of overactive bladder, which involved needle insertion at defined acupuncture points. This includes body acupuncture, scalp acupuncture, auricular acupuncture and electro‐acupuncture. We sought clarification from study authors if the type of acupuncture used in a trial was not clear.
Sham acupuncture is designed to assist with blinding participants about the type of treatment they are receiving. It can be delivered using a needle that appears to pierce the skin but does not, or by inserting needles at non‐acupuncture points.
We included the following comparators.
Acupuncture versus no treatment
Acupuncture versus sham acupuncture
Acupuncture versus conservative treatments (including bladder retraining, fluid management, pelvic floor rehabilitation, weight loss and smoking cessation)
Acupuncture versus medication for overactive bladder
We believe that the comparisons of particular interest to patients and practitioners are acupuncture versus no treatment or sham acupuncture, and acupuncture versus medication for symptoms of overactive bladder.
Types of outcome measures
We included validated urinary symptom and incontinence‐specific, patient‐reported outcome measures in this review.
Primary outcomes
Number of participants whose overactive bladder symptoms were cured or improved, assessed using validated urinary symptom and incontinence‐specific patient‐reported outcome measures (e.g. the Bristol Female Lower Urinary Tract Symptoms questionnaire (BFLUTS) (Hiller 2002), International Consultation on Incontinence Questionnaire‐Urinary Incontinence (ICIQ‐UI) (Avery 2004), three‐day bladder diaries (Jimenez‐Cidre 2015)). Numbers of participants defined as cured in studies were reported. Where cure rates were not used, we used symptom improvement rates.
Number of major adverse events (i.e. death, serious infection from needle insertion, pneumothorax from needle insertion, any complication resulting in hospitalisation as an inpatient or an outpatient).
Number of minor adverse events (i.e. fainting, vomiting, pain on needle insertion, bleeding on needle removal, bruising and fatigue).
Secondary outcomes
Presence or absence of urinary urgency (measured by patient‐reported outcomes).
Daytime urinary frequency (i.e. number of voids during waking hours measured by patient‐reported outcomes).
Episodes of urinary incontinence in a 24‐hour period (measured by patient‐reported outcomes).
Episodes of nocturia (i.e. number of voids after going to sleep and prior to waking measured by patient‐reported outcomes).
Improvement in objective measures of urinary incontinence (i.e. urodynamic testing parameters).
Improvement in general quality of life (assessed using validated scores, e.g. EQ‐5D (Rabin 2001), medical outcomes SF‐36 (Ware 1992), ICEpop CAPability measure for Adults (ICECAP A) (Al‐Janabi 2013)).
Timing of outcome assessment
We included outcome measures that are applied as follows.
Within three weeks of randomisation (baseline measurement)
Within 12 weeks of commencing treatment (short‐term outcomes)
Longer than 12 weeks after commencing treatment (long‐term outcomes)
Acupuncture treatments for overactive bladder symptoms are usually applied on at least a weekly basis. Studies varied in the number of treatments given, with usual practice between 4 and 12 treatments. Acupuncture is thought to have a carryover treatment effect and so the measurement of long‐term outcomes is of interest in this review.
Main outcomes for summary of findings tables
Number of participants whose overactive bladder symptoms were cured or improved
Number of major adverse events
Number of minor adverse events
Presence or absence of urinary urgency
Daytime urinary frequency
Episodes of urinary incontinence in a 24‐hour period
Episodes of nocturia (i.e. number of voids after going to sleep and prior to waking)
Where not otherwise indicated, all outcomes for the summary of findings tables were measured within 12 weeks of commencing treatment (i.e. short‐term).
Search methods for identification of studies
We did not impose any language or other limitations on any of the searches described below.
Electronic searches
Search for clinical effectiveness studies
We identified relevant trials from the Cochrane Incontinence Specialised Register. For more details of the search methods used to build the Specialised Register, please see the Group's webpages where details of the Register's development (from inception) and the most recent searches performed to populate the Register can be found. To summarise, the Register contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, MEDLINE In‐Process, In‐Data‐Review and Other Non‐Indexed Citations, MEDLINE Epub Ahead of Print, MEDLINE Daily, ClinicalTrials.gov, WHO ICTRP and handsearching of journals and conference proceedings. Many of the trials in the Cochrane Incontinence Specialised Register are also contained in CENTRAL.
The date of the most recent search of the Cochrane Incontinence Specialised Register for this review is 14 May 2022.
The terms that we used to search the Cochrane Incontinence Specialised Register are given in Appendix 2.
We also searched the Allied and Complementary Medicine database (AMED) on EBSCOhost.
The date of the most recent search was on 14 May 2022.
The terms that we used to search AMED are given in Appendix 3.
In addition, two of the review authors searched the following electronic bibliographic databases, where knowledge of the Chinese language is necessary.
China National Knowledge Infrastructure (CNKI);
Chinese Science and Technology Periodical Database (VIP); and
WANFANG (China Online Journals).
The date of the most recent search of these databases was 10 February 2021 and the search strategies used are given in Appendix 4.
Search for economic evaluations
We performed additional searches for the brief economic commentary (BEC). We searched the Cochrane Incontinence Specialised Register of Economic Evaluations, which consists of searches of:
NHS Economic Evaluation Database (NHS EED) on the UK Centre for Reviews and Dissemination (CRD) website (covering from the earliest record in NHS EED, dating from 1968, up to and including 31 December 2014 when their coverage ended).
As NHS EED is no longer actively updated, we performed additional searches of the following databases to identify eligible studies added to these databases from 1 January 2015 onwards:
MEDLINE on OvidSP (covering 1 January 1946 to June Week 5 2022); and
Embase (on OvidSP) (covering 1 January 1974 to 2022 Week 27).
The date of the most recent search was 11 July 2022 and the details of the searches performed can be found in Appendix 5.
Searching other resources
We searched the reference lists of included studies and relevant systematic reviews.
Data collection and analysis
We conducted data collection and analysis in accordance with methods specified in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019).
Selection of studies
As we anticipated that a proportion of studies would be available only in Mandarin, four review authors formed pairs to select studies and extract data (EH and CC for English language studies and YYZ and XWZ for Mandarin language studies). Both pairs of review authors used the same software, screening and data extraction processes.
Using Covidence, the above pairs of review authors independently screened the titles and abstracts identified by the search. We obtained the full text of potentially relevant reports and assessed these against the review's inclusion criteria. We compared and discussed their results and resolved disagreements by consulting another review author (KB).
Data extraction and management
Using Covidence, pairs of review authors (EH and CC for English language studies and YYZ and XWZ for Mandarin language studies) independently extracted data from the included studies. We compared and discussed data extraction forms for each study. A third review author (GB) resolved any disagreements.
Assessment of risk of bias in included studies
We used Cochrane's risk of bias tool to assess the risk of bias in the included studies (Higgins 2011). Two pairs of review authors (EH and CC for English language studies and YYZ and XWZ for Mandarin language studies) individually assessed each of the identified studies against the six domains: random sequence generation, allocation concealment, blinding of participants and study personnel, blinding of outcome assessors, incomplete outcome data, selective outcome reporting and any other source of potential bias. For each domain, we rated the study as either at ‘high', ‘low' or ‘unclear' risk of bias. A third review author (KB) arbitrated any disagreements.
Measures of treatment effect
We used Review Manager Web (RMW) to perform statistical analysis of the data collected from the selected studies (RevMan Web 2020). One review author (EH) was responsible for data entry into RevManWeb and a second review author (CC) checked the process.
For dichotomous outcome data, we measured the treatment effect using risk ratios (RR) with 95% confidence intervals (CIs). For continuous outcome data, we used mean difference (MD) values with 95% CIs to measure treatment effect.
If identified studies used differing scales to measure the same outcome, it was necessary to use the standardised mean difference (SMD) with 95% CIs. We considered this necessary in order to express the size of the intervention effect in each study, relative to the between‐participant variability in outcome measurements observed in studies as per guidance given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019).
Unit of analysis issues
We intended to include studies using a cross‐over design if they met the inclusion criteria and would have applied the guidance of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019). Where studies are available in future updates, the risk of bias assessment will pay particular attention to the dropout rate following first treatment, the randomisation process to first treatment and the reporting of these events. If the dropout rate following the first treatment is high and the study reports first treatment only data, we will exclude these studies. An assessment of the effect of carryover from treatment one to treatment two will be made and, if it is felt that the treatment carryover would significantly affect the reported results, these studies will be excluded from the review.
If insufficient detail is reported in studies to make the judgements described above, we will contact study authors in order to obtain the details required.
If there is a group of cross‐over studies reporting the results of a paired analysis (i.e. as a MD), we could use the generic inverse‐variance method (GIV) to perform a meta‐analysis or meta‐regression as required.
In studies using multiple arm designs where treatments were studied in isolation and as a combined treatment, we used only the data from the stand‐alone arms.
Dealing with missing data
We included studies reporting results using an intention‐to‐treat (ITT) analysis if the participants were analysed in the study arm to which they were originally assigned.
If there were missing data reported that could be calculated using recognised statistical methods, we performed these calculations. We used the conventional analysis of meta‐analysis only if individuals with available data were adequate and when we were confident that the data were missing at random (MAR) in every study (i.e. that the probability of missing data does not depend on unobserved outcomes, conditional on observed variables).
However, if data were not missing at random, we used two methods based on plausible assumptions about the missing data. We imputed missing values based on the distribution of reasons for missing data. After specifying the magnitude and uncertainty of possible departures from the missing at random assumption, we used these to correct bias and re‐weight the studies by employing a pattern mixture model and describing how the outcome in the missing participants is related to the outcome in the completers. This relationship was informed using expert opinion in the review author team.
Assessment of heterogeneity
We assessed the heterogeneity of studies by producing forest plots and using the Chi² test and I² statistic in the RMW software (RevMan Web 2020). This allowed us to assess heterogeneity and decide whether a meaningful meta‐analysis could be performed. The assessment of heterogeneity was guided by the Cochrane Handbook for Systematic Reviews of Interventions as follows (Higgins 2019).
0% to 40%: might not be important
30% to 60%: may represent moderate heterogeneity
50% to 90%: may represent substantial heterogeneity
75% to 100%: considerable heterogeneity
Assessment of reporting biases
Had sufficient studies been identified, we would have produced funnel plots to explore publication bias.
Data synthesis
We synthesised the data collected using RevMan Web (RevMan Web 2020). We generated forest plots for each outcome and used a fixed‐effect model. We examined the heterogeneity of effect sizes using the Chi2 test and I2 statistic. If data were homogeneous, we used a fixed‐effect model and if the data were heterogeneous, we used a random‐effects model. Where meta‐analyses were not possible, we undertook a narrative synthesis of results.
Subgroup analysis and investigation of heterogeneity
We planned to perform the following subgroup analyses, had the data allowed.
Sex (male versus female)
Form of acupuncture (body acupuncture versus electro‐acupuncture versus auricular)
Age (under 65 years versus over 65 years)
Sensitivity analysis
Had the data allowed, we planned to employ sensitivity analysis to examine the effect of a single study on the overall estimation, if the data suggested this was required (i.e. if the eligibility of some included studies was dubious due to missing data).
Had the data allowed, we planned to perform a cumulative meta‐analysis using Stata software (Stata 2019), where studies are added one at a time in a specified order according to date of publication or quality to check the contribution of added studies.
Incorporating economic evidence
Following the search outlined in the Search methods for identification of studies, we would have developed a BEC to summarise the availability and principal findings of the full economic evaluations that compare acupuncture with other treatments, had any relevant studies been found (Aluko 2022). This BEC would have encompassed full economic evaluations (i.e. cost‐effectiveness analyses, cost‐utility analyses and cost‐benefit analyses) conducted as part of a single empirical study, such as a RCT, a model based on a single such study, or a model based on several such studies.
Summary of findings and assessment of the certainty of the evidence
We prepared summary of findings tables using the GRADEpro GDT software for the three comparisons pre‐stated in the Types of interventions: acupuncture versus no treatment, acupuncture versus sham acupuncture and acupuncture versus medication for overactive bladder.
We used the GRADE approach to assess the certainty of evidence related to the ‘Main outcomes for summary of findings tables' as listed in the Types of outcome measures (Schünemann 2019). We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) and graded the certainty of the evidence as high, moderate, low or very low. We justified all decisions to downgrade the certainty of trials using footnotes.
Results
Description of studies
Results of the search
Search for clinical effectiveness studies
An initial literature search was undertaken on 27 January 2020 and further searches were conducted on 1 March 2021 and 14 May 2022. We identified 592 reports and removed 82 of these as duplicates. We screened 510 abstracts against the review criteria and excluded 390. We obtained 120 full‐text reports and excluded 84; the reasons for exclusion are detailed in the Excluded studies section. There were eight reports of six studies that we classified as ongoing and two studies are awaiting classification. We included 15 studies (25 reports) in the review. The flow of studies through the assessment process is represented in Figure 1.
1.
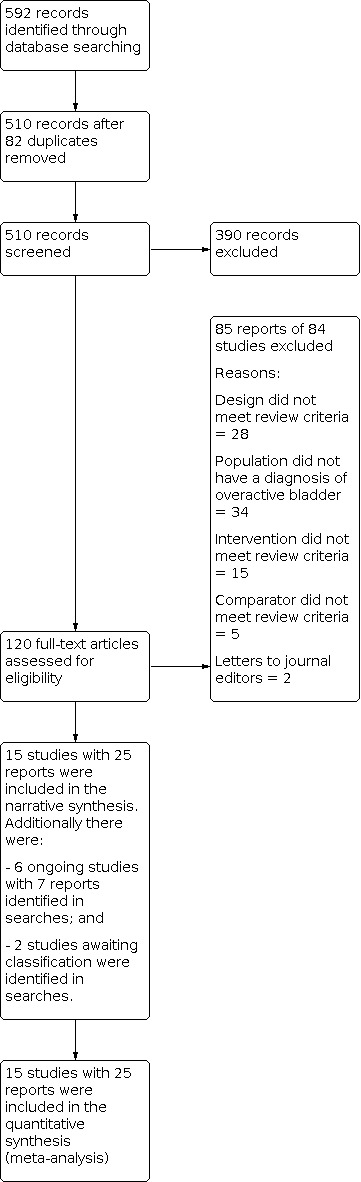
PRISMA flow diagram ‐ clinical effectiveness studies
Search for economic evaluations
The search for potentially relevant records produced a total of 437 records to screen. The results of the economic search yielded no economic evaluations assessing the use of acupuncture for treating overactive bladder in adults. The flow of literature through the assessment process is shown in Figure 2.
2.
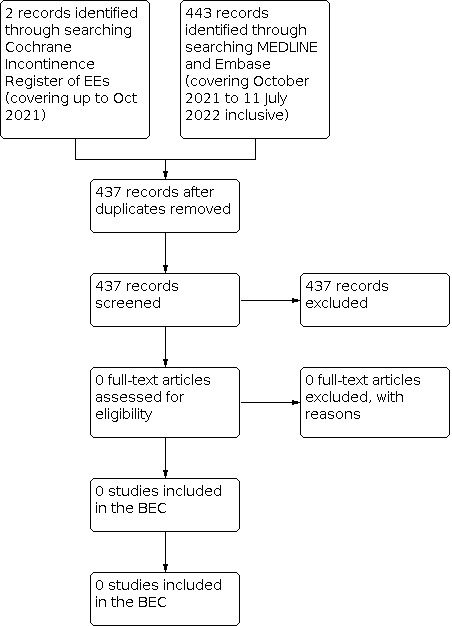
PRISMA flow diagram ‐ brief economic commentary (BEC)
Included studies
Fifteen studies met the inclusion criteria. Full details are included in the Characteristics of included studies table.
Design
Of the 15 included studies, 14 were RCTs and one was a quasi‐RCT (Hong 2015). Three studies incorporated three arms in their design (Aydoğmuş 2014; Solberg 2016; Yang 2016).
Sample sizes
In total, the 15 included studies involved 1395 participants. The mean number of participants per study was 93. Overall, the sample sizes in the included studies were small; only 40% of studies had more than 50 participants (Aydoğmuş 2014; Hong 2015; Lin 2020; Liu 2019; Wang 2013a; Yuan 2015). Two studies contributed 53% of the total participants included in the review, with 500 and 240 participants respectively (Liu 2019; Yuan 2015).
Setting
The majority of the studies were conducted in China (Chen 2009; Hong 2015; Liu 2019; Lin 2020; Shen 2020; Wang 2011; Wang 2013a; Yang 2016; Yu 2012; Yuan 2015; Zhang 2015). Other studies were conducted in: the USA (Engberg 2009); the UK (Kelleher 1994); Turkey (Aydoğmuş 2014); and Norway (Solberg 2016).
Thirteen studies were conducted in hospitals (Aydoğmuş 2014; Chen 2009; Hong 2015; Kelleher 1994; Lin 2020; Liu 2019; Shen 2020; Wang 2011; Wang 2013a; Yang 2016; Yu 2012; Yuan 2015; Zhang 2015). Two were conducted in university settings (Engberg 2009; Solberg 2016).
Thirteen studies were conducted on a single site (Aydoğmuş 2014; Chen 2009; Engberg 2009; Hong 2015; Kelleher 1994; Shen 2020; Solberg 2016; Wang 2011; Wang 2013a; Yang 2016; Yu 2012; Yuan 2015; Zhang 2015). One study was a multicentre trial conducted across 10 sites (Liu 2019), while another study was conducted at two sites in Hong Kong (Lin 2020).
Funding sources
Of the 15 included studies, four were supported by Chinese Government‐funded research grants (Hong 2015; Lin 2020; Liu 2019; Shen 2020), and two were funded by Higher Education institutions (Engberg 2009; Wang 2013a). The open access publishing fee for one study was paid by the Norwegian Acupuncture Association (Solberg 2016). Eight studies did not report any source of funding (Aydoğmuş 2014; Chen 2009; Kelleher 1994; Wang 2011; Yang 2016; Yu 2012; Yuan 2015; Zhang 2015).
Participants
The presenting condition for all participants was overactive bladder or overactive bladder‐predominant mixed urinary incontinence (MUI). How this diagnosis was made varied between studies. Four studies used Chinese national diagnostic criteria (Hong 2015; Shen 2020; Yang 2016; Yu 2012). Four studies used the International Continence Society definition of overactive bladder (Aydoğmuş 2014; Lin 2020; Wang 2011; Zhang 2015). Five studies used self‐reported symptoms including urinary urgency, urge incontinence and frequency of urination (Chen 2009; Kelleher 1994; Solberg 2016; Wang 2013a; Yuan 2015). Two studies used objective measures of urinary symptoms, including three‐day bladder diaries and validated questionnaires (Engberg 2009; Liu 2019).
Ten studies included only women (Aydoğmuş 2014; Engberg 2009; Kelleher 1994; Liu 2019; Shen 2020; Solberg 2016; Wang 2011; Wang 2013a; Yuan 2015; Zhang 2015). One study only included men (Chen 2009), while two studies included both sexes (Lin 2020; Yu 2012). Two studies did not report the sex of participants (Hong 2015; Yang 2016).
The mean age of participants was recorded in 11 studies (Aydoğmuş 2014; Chen 2009; Engberg 2009; Hong 2015; Kelleher 1994; Lin 2020; Liu 2019; Solberg 2016; Yang 2016; Yuan 2015; Zhang 2015). The mean age of participants in these 11 studies was 49.6 years with a range of 18 to 87 years. Two studies reported the age range of participants: 51 to 79 years (Wang 2011), and 35 to 60 years (Wang 2013a). One study described the median age of participants as 35.2 years (Yu 2012), while one study did not report the age of participants (Shen 2020).
Studies varied widely in the amount of demographic data collected on participants. However, there were some identifiable themes, including body mass index (BMI) (Engberg 2009; Liu 2019; Zhang 2015), duration of symptoms (Hong 2015; Kelleher 1994; Liu 2019), race (Engberg 2009; Liu 2019), presence of co‐morbidities (Engberg 2009; Liu 2019), and parity (Aydoğmuş 2014; Liu 2019; Solberg 2016). Four studies did not report any demographic baseline data apart from sex (Shen 2020; Wang 2011; Wang 2013a; Yu 2012).
Interventions
This review included studies that employed acupuncture that pierced the skin, including body, scalp and auricular acupuncture practices with or without electrical stimulation. No studies employed solely scalp or auricular acupoints. Traditional acupuncture was used in nine studies (Aydoğmuş 2014; Engberg 2009; Kelleher 1994; Lin 2020; Solberg 2016; Wang 2011; Wang 2013a; Yu 2012; Yuan 2015). Electro‐acupuncture was used in six studies (Chen 2009; Hong 2015; Liu 2019; Shen 2020; Yang 2016; Zhang 2015).
The number of treatments, number of needles used and length of follow‐up are summarised in Table 4. Individual study treatment protocols are documented in the Characteristics of included studies.
1. Study duration, treatment frequency and follow‐up period.
| Study ID | Number/sex of participants | Length of intervention | Number of acupuncture treatments performed | Number of points used | Follow‐up |
| Aydoğmuş 2014 | 90 women | 4 weeks | 8 | 15 | No |
| Chen 2009 | 48 men | 2 weeks | 14 | 6 | No |
| Engberg 2009 | 11 women | 6 weeks | 12 | 12 | 4 weeks after treatment was completed |
| Hong 2015 | 66 ‐ sex not stated | 4 weeks | 20 | 8 | No |
| Kelleher 1994 | 39 women | 6 weeks | 6 | 16 | No |
| Lin 2020 | 45 men 55 women |
8 weeks | 16 | 13 | 3 months after treatment was completed |
| Liu 2019 | 500 women | 12 weeks | 36 | 4 | 24 weeks after treatment was completed |
| Shen 2020 | 45 women | 4 weeks | 12 | 10 | No |
| Solberg 2016 | 34 women | 12 weeks | 12 | 14 | No |
| Wang 2011 | 40 women | 4 weeks | 28 | 13 | No |
| Wang 2013a | 60 women | 4 weeks | 28 | 15 | No |
| Yang 2016 | 33 men and women ‐ ratios not stated | 8 weeks | 24 | 4 | No |
| Yu 2012 | 44 men and women ‐ ratios not stated | 2 weeks | 28 | 6 | No |
| Yuan 2015 | 240 women | 4 weeks | 4 | 7 | No |
| Zhang 2015 | 45 women | 6 weeks | 30 | 6 | No |
Comparators were grouped into: sham acupuncture (five studies: Aydoğmuş 2014: Engberg 2009; Lin 2020; Yang 2016; Zhang 2015); conservative treatments (one study: Solberg 2016); and medication for overactive bladder (11 studies: Aydoğmuş 2014; Chen 2009; Hong 2015; Kelleher 1994; Liu 2019; Shen 2020; Wang 2011; Wang 2013a; Yang 2016; Yu 2012; Yuan 2015).
Medication used included solifenacin (Aydoğmuş 2014; Liu 2019; Wang 2013a), tolterodine (Chen 2009; Hong 2015; Shen 2020; Wang 2011; Yu 2012; Yuan 2015), and oxybutynin (Kelleher 1994).
Four sham studies employed non‐penetrating needles (Aydoğmuş 2014; Engberg 2009; Lin 2020; Yang 2016). One sham study used penetrating needles at non‐acupuncture point 15 mm to the side of known points (Zhang 2015).
Three studies used either a combined comparator arm of medication plus pelvic floor training (Liu 2019), or medication plus bladder retraining techniques (Hong 2015; Yu 2012). These studies were included as the combination of treatments used met the criteria of this review. However, we acknowledge that this inclusion does add complexity when considering the effects of interventions as it is not clear which of the active ingredients in the combined treatment gives rise to the effect reported.
No studies were identified where no treatment was the sole comparator. However, Solberg 2016 used no intervention as one of three arms in their study. Two multi‐arm studies compared acupuncture with both medication and sham acupuncture (Aydoğmuş 2014; Yang 2016). Solberg 2016 compared acupuncture with pelvic floor muscle training or no treatment.
Outcomes
Outcomes reported by the included studies varied greatly, making meaningful comparisons more challenging.
Reported cure or improvement in overactive bladder symptoms using validated patient‐reported outcome measures (PROMs)
Four studies used the International Consultation on Incontinence Questionnaire‐Short Form (ICIQ‐SF) (Aydoğmuş 2014; Hong 2015; Liu 2019; Solberg 2016). However, scores were reported in differing formats, including mean and standard deviation, median and interquartile range and percentage change scores from baseline, preventing meta‐analysis of this information. Other PROMs reported by research teams included the Overactive Bladder Symptom Score (OABSS) (Lin 2020; Zhang 2015), the Urinary Distress Inventory (UDI) (Engberg 2009; Lin 2020), and the Incontinence Impact Questionnaire (IIQ) (Engberg 2009; Lin 2020).
Number of major adverse events
Ten studies specifically reported in the text of the report that no major adverse events had occurred during the study (Aydoğmuş 2014; Engberg 2009; Hong 2015; Lin 2020; Liu 2019; Shen 2020; Solberg 2016; Yang 2016; Yuan 2015; Zhang 2015). Five studies made no mention of major adverse events (Chen 2009; Kelleher 1994; Wang 2011; Wang 2013a; Yu 2012). See the information contained in Table 5.
2. Adverse events reported in included studies.
| Study | Major adverse event reporting | Type of minor adverse event | Number in acupuncture group | Number in comparator group |
| Aydoğmuş 2014 | Specifically reported no major adverse events in the text of the report | Dry mouth | 0 | 19 |
| Chen 2009 | No explicit discussion in the study report regarding major adverse events | No reported | Not reported | Not reported |
| Engberg 2009 | Specifically reported no major adverse events in the text of the report | Drowsiness and/or |
3 | 0 |
| bleeding at needling site | 2 | 0 | ||
| Hong 2015 | Specifically reported no major adverse events in the text of the report | Pain at needling site | 1 | 0 |
| Bruising | 1 | 0 | ||
| Kelleher 1994 | No explicit discussion in the study report regarding major adverse events | Dry mouth | 0 | 19 |
| Lin 2020 | Specifically reported no major adverse events in the text of the report | Pain at needling site | 1 | 0 |
| Allergic reaction to adhesive tape used to secure sham needles | 0 | 1 | ||
| Liu 2019 | Specifically reported no major adverse events in the text of the report | Bruising | 10 | 0 |
| Digestive system disorders | 4 | 21 | ||
| Dry mouth | 0 | 62 | ||
| Unrelated fracture | 0 | 1 | ||
| Shen 2020 | Specifically reported no major adverse events in the text of the report | Discomfort at needling site | 3 | 0 |
| Dry mouth | 0 | 5 (including 3 withdrawn) | ||
| Solberg 2016 | Specifically reported no major adverse events in the text of the report | Tiredness | 1 | 0 |
| Wang 2011 | No explicit discussion in the study report regarding major adverse events | Dry mouth | 0 | 2 |
| Wang 2013a | No explicit discussion in the study report regarding major adverse events | None reported | Not reported | Not reported |
| Yang 2016 | Specifically reported no major adverse events in the text of the report | Dry mouth | 0 | 8 |
| Yu 2012 | No explicit discussion in the study report regarding major adverse events | None reported | Not reported | Not reported |
| Yuan 2015 | Specifically reported no major adverse events in the text of the report | Dry mouth | 0 | 11 |
| Needling pain | 9 | 0 | ||
| Zhang 2015 | Specifically reported no major adverse events in the text of the report | Minor pain at needling site | 2 | 3 |
Number of minor adverse events
Twelve studies reported minor adverse events (Aydoğmuş 2014; Engberg 2009; Hong 2015; Kelleher 1994; Lin 2020; Liu 2019; Shen 2020; Solberg 2016; Wang 2011; Yang 2016; Yuan 2015; Zhang 2015). The details can be found in Table 5. Three studies did not mention adverse events (Chen 2009; Wang 2013a; Yu 2012). In all studies, minor adverse events were discussed in the text of the report and data were restricted to counts of events.
Presence or absence of urinary urgency (measured by patient‐reported outcomes)
Six studies reported on the presence or absence of urinary urgency (Kelleher 1994; Liu 2019; Shen 2020; Wang 2013a; Yang 2016; Yuan 2015). The method of reporting urgency varied between studies. Counts of events in a participant‐completed bladder diary was the most common method employed and was used by five research teams (Kelleher 1994; Liu 2019; Wang 2013a; Yang 2016; Yuan 2015). In addition to bladder diary data, Kelleher 1994 used a visual analogue scale (VAS) to judge the bothersomeness of overactive bladder symptoms, including urgency. One study referred to urinary urgency scores but were not explicit regarding the scale used (Shen 2020). All studies reported a reduction in the frequency of urinary urgency in acupuncture groups.
Daytime urinary frequency
Six studies reported on urinary frequency (Kelleher 1994; Liu 2019; Wang 2011; Wang 2013a; Yang 2016; Yuan 2015). Data regarding frequency of micturition were gathered using participant‐reported bladder diary information for all six studies and all studies reported a reduction in the frequency of daytime micturition in acupuncture groups. In addition, Kelleher 1994 used a VAS to measure bothersomeness of frequency of micturition, which gave a reduction in perceived bothersomeness of frequency.
Episodes of urinary incontinence in a 24‐hour period
Four studies reported on the frequency of urinary incontinence episodes (Lin 2020; Liu 2019; Yang 2016; Yuan 2015). All studies used participant‐completed bladder diaries to collect data relating to incontinence episodes and all reported a reduction in the episodes of urinary incontinence in acupuncture groups. In addition, Kelleher 1994 used a VAS to measure bothersomeness of incontinence, which gave a reduction in perceived bothersomeness of incontinence.
Episodes of nocturia
Five studies reported on episodes of nocturia (Kelleher 1994; Liu 2019; Wang 2013a; Yang 2016; Yuan 2015). All studies used participant‐completed bladder diaries to collect data on nocturia and all reported a reduction in episodes in acupuncture groups.
Improvement in objective measures of urinary symptoms
Four studies reported objective measures of urinary symptoms (Aydoğmuş 2014; Kelleher 1994; Lin 2020; Zhang 2015). Two studies reported measures from urodynamic testing (Kelleher 1994; Zhang 2015). Measures reported included:
bladder volume in mL at first sensation (Zhang 2015);
bladder volume in mL at first urge (Kelleher 1994; Zhang 2015);
maximum bladder capacity (Kelleher 1994; Zhang 2015);
maximum flow rate (Kelleher 1994; Zhang 2015);
post void residual (Kelleher 1994; Zhang 2015); and
rise in detrusor pressure during filling (Kelleher 1994).
Two studies measured nerve growth factor (NGF) levels in participants' urine samples (Aydoğmuş 2014; Lin 2020).
Improvement in general quality of life
Three studies reported quality of life scores in their results (Aydoğmuş 2014; Engberg 2009; Shen 2020). Two studies were not specific about the scale used or whether an increased or decreased score showed improvement (Aydoğmuş 2014; Shen 2020). Engberg 2009 applied the SF‐36 to measure quality of life on both the physical and mental health components.
Length of studies and follow‐up
The length of time studies were conducted across varied greatly; these are summarised in Table 4.
We included outcome measures that were applied as follows.
Within three weeks of randomisation (baseline measurement)
Within 12 weeks of commencing treatment (short‐term outcomes)
Longer than 12 weeks after commencing treatment (long‐term outcomes)
Thirteen studies recorded only short‐term outcomes (Aydoğmuş 2014; Chen 2009; Engberg 2009; Hong 2015; Kelleher 1994; Shen 2020; Solberg 2016; Wang 2011; Wang 2013a; Yang 2016; Yu 2012; Yuan 2015; Zhang 2015). Two studies collected data after 12 weeks (Lin 2020; Liu 2019). However, the data from these studies could not be meaningfully combined to give an indication of the short‐term effects of acupuncture compared to long‐term effects of acupuncture for overactive bladder.
Excluded studies
Eighty‐four studies were excluded from the review for a variety of reasons, including:
the patient population did not have a diagnosis of overactive bladder (N = 34);
the study design did not fit the review criteria (N = 29);
the intervention did not fit the review criteria (N = 14);
the comparator did not fit the review criteria (N = 5); or
it was a letter to the editor of a journal (N = 2).
Further details can be found in the Characteristics of excluded studies table.
Risk of bias in included studies
Figure 3 and Figure 4 summarise the risk of bias assessments across the included studies.
3.

4.

Allocation
Random sequence generation
We considered six studies (40%) to have adequate sequence generation, using centralised, computer‐generated randomisation, suggesting a low risk of selection bias (Engberg 2009; Lin 2020; Liu 2019; Shen 2020; Yuan 2015; Zhang 2015). In eight studies (53.3%), the method used for random sequence generation was unclear, with the text referring to randomisation but without an explanation of how this was undertaken (Aydoğmuş 2014; Chen 2009; Kelleher 1994; Solberg 2016; Wang 2011; Wang 2013a; Yang 2016; Yu 2012). We judged one study to be at high risk of bias for sequence generation (Hong 2015).
Allocation concealment
Three studies (20%) reported sufficient detail regarding allocation concealment techniques that resulted in a judgement of low risk of allocation concealment bias (Lin 2020; Liu 2019; Yuan 2015). These techniques included computer‐generated sequences and staff who where otherwise not involved in the intervention. Twelve studies (80%) did not provide a sufficiently detailed report regarding allocation concealment to make a clear judgement (Aydoğmuş 2014; Chen 2009; Engberg 2009; Hong 2015; Kelleher 1994; Shen 2020; Solberg 2016; Wang 2011; Wang 2013a; Yang 2016; Yu 2012; Zhang 2015).
Blinding
Blinding of participants and personnel
Due to the nature of acupuncture, it is difficult to blind participants to group allocation unless a sham acupuncture procedure is employed in the study design. Five studies (33.3%) used sham acupuncture in their design (Aydoğmuş 2014; Engberg 2009; Lin 2020; Yang 2016; Zhang 2015). Of these, we judged three studies to represent low risk of bias for blinding procedures (Engberg 2009; Lin 2020; Zhang 2015). Aydoğmuş 2014 and Yang 2016 were three‐arm trials with acupuncture, sham acupuncture and medication acting as comparators. The mechanism for preserving blinding was not reported in sufficient detail and, as one third of the participants were treated with medication, they were not blinded to their intervention. This led to a judgement of high risk of bias for these studies.
Ten studies (66.6%) did not employ a sham acupuncture procedure within their design (Chen 2009; Hong 2015; Kelleher 1994; Liu 2019; Shen 2020; Solberg 2016; Wang 2011; Wang 2013a; Yu 2012; Yuan 2015). Participants within these studies were aware of their treatment allocation and thus we judged them to have a high risk of performance bias. We also judged acupuncturists delivering interventions in these studies to have a high risk of performance bias.
Blinding of outcome assessment
Four studies (26.7%) were explicit in reporting that outcome assessors had been blinded to treatment group in the text of study reports, so we judged them to be at low risk of detection bias (Engberg 2009; Lin 2020; Liu 2019; Yuan 2015). Nine studies (60%) mentioned that outcome assessors were blinded to allocation group but gave insufficient detail of the processes employed to allow for a judgement of risk to be made and we therefore classified them as having unclear risk of bias (Aydoğmuş 2014; Chen 2009; Kelleher 1994; Shen 2020; Solberg 2016; Wang 2013a; Yang 2016; Yu 2012; Zhang 2015). Two studies (13.3%) did not mention blinding of outcome assessors in study reports and we judged them as having high risk of bias (Hong 2015; Wang 2011).
Incomplete outcome data
Outcome data were completely reported, including number and reasons for study attrition, in 11 studies (73.3%) (Chen 2009; Engberg 2009; Hong 2015; Kelleher 1994; Lin 2020; Liu 2019; Shen 2020; Wang 2011; Wang 2013a; Yang 2016; Zhang 2015). We therefore judged these studies as being at low risk of attrition bias. In four studies (26.7%) there was a lack of clarity regarding some data and dropouts, leading to a judgement of unclear risk of attrition bias (Aydoğmuş 2014; Solberg 2016; Yu 2012; Yuan 2015).
Selective reporting
We judged 12 studies (80%) to have reported on all expected outcomes fully and they therefore represented a low risk of reporting bias (Chen 2009; Hong 2015; Kelleher 1994; Lin 2020; Liu 2019; Shen 2020; Solberg 2016; Wang 2011; Wang 2013a; Yang 2016; Yu 2012; Zhang 2015). We judged two studies to have a high risk of bias for selective reporting. Engberg 2009 used multiple questionnaires to assess baseline status and change following the intervention but not all outcomes were fully reported. Yuan 2015 referred to adverse events in the text of the report but did not publish the data to support this. Aydoğmuş 2014 failed to give any detail regarding the format of the Turkish ICIQ‐SF and did not specify what quality of life scale was used in the study; we therefore judged the study to be at an unclear risk of reporting bias.
Other potential sources of bias
In 14 studies (93.3%), there were no concerns about other sources of bias (Chen 2009; Engberg 2009; Hong 2015; Kelleher 1994; Lin 2020; Liu 2019; Shen 2020; Solberg 2016; Wang 2011; Wang 2013a; Yang 2016; Yu 2012; Yuan 2015; Zhang 2015). We felt one study (6.7%) to be at an unclear risk of potential bias. Aydoğmuş 2014 inadequately reported baseline data to demonstrate that the groups were comparable.
Effects of interventions
See: Table 1; Table 2; Table 3
Acupuncture versus no treatment
One study with a total of 34 participants compared acupuncture with no treatment (Solberg 2016).
Primary outcomes
Number of participants whose overactive bladder symptoms were cured or improved
Solberg 2016 used the International Consultation on Incontinence Questionnaire Short Form (ICIQ‐SF) to assess urinary symptoms. The ICIQ‐SF measure has a score ranging between 0 and 21 with higher scores indicating more symptoms. The evidence is very uncertain about the effect of acupuncture versus no treatment in terms of cure or improvement at 12 weeks (Analysis 1.1; Table 1; very low‐certainty evidence).
1.1. Analysis.
Comparison 1: Acupuncture versus no treatment, Outcome 1: Cure or improvement in overactive bladder symptoms
| Cure or improvement in overactive bladder symptoms | ||||||
| Study | Acupuncture group median score | IQR | Number | No treatment group median score | IQR | Number |
| Solberg 2016 | 6.5 | 4 | 12 | 10 | 7.3 | 12 |
Number of major adverse events
Solberg 2016 reported that there were no major adverse events during the study.
Number of minor adverse events
Solberg 2016 reported two instances of minor adverse events. In the acupuncture group, one woman reported tiredness following treatment and one woman initially noticed an increase in urinary symptoms. There were no reports of minor adverse events in the no treatment group. However, the evidence is very uncertain about the effect of acupuncture on the number of minor adverse events (Table 1; very low‐certainty evidence).
Secondary outcomes
Presence or absence of urinary urgency
Not reported.
Daytime urinary frequency
Not reported.
Episodes of urinary incontinence in a 24‐hour period
Not reported.
Episodes of nocturia
Not reported.
Improvement in objective measures of urinary incontinence
Not reported.
Improvement in general quality of life
Not reported.
Acupuncture versus sham acupuncture
Five studies including a total of 279 participants compared acupuncture with sham acupuncture (Aydoğmuş 2014; Engberg 2009; Lin 2020; Yang 2016; Zhang 2015).
Primary outcomes
Number of participants whose overactive bladder symptoms were cured or improved
The evidence is very uncertain about the effect of acupuncture on curing or improving overactive bladder symptoms compared to sham acupuncture within 12 weeks of commencing treatment (standardised mean difference (SMD) ‐0.36, 95% confidence interval (CI) ‐1.03 to 0.31; 3 studies; 151 participants; I2 = 65%; Analysis 2.1; Table 2; very low‐certainty evidence).
2.1. Analysis.

Comparison 2: Acupuncture versus sham acupuncture, Outcome 1: Cure or improvement in urinary symptoms
Number of major adverse events
All five studies reported that there were no major adverse events.
Number of minor adverse events
Of the five studies included, two studies reported that there were no minor adverse events in the acupuncture or sham groups (Aydoğmuş 2014; Yang 2016). Three studies recorded the number of participants who had at least one minor adverse event from either the acupuncture or sham acupuncture group (Engberg 2009; Lin 2020; Zhang 2015). The data from Engberg 2009 could not be included in the meta‐analysis as the absolute numbers of participants who had at least one minor adverse event were not reported; instead, the team reported the percentage of participants who reported each particular complaint. Therefore, we included data from four studies in the meta‐analysis.
There is probably no evidence of a difference in the number of minor adverse events with acupuncture compared with sham acupuncture within eight weeks of treatment (risk ratio (RR) 1.28, 95% CI 0.30 to 5.36; 4 studies; 222 participants; I² = 0%; Analysis 2.2; Table 2; moderate‐certainty evidence). The types of minor adverse events reported in the studies are recorded in Table 5.
2.2. Analysis.

Comparison 2: Acupuncture versus sham acupuncture, Outcome 2: Number of minor adverse events
Secondary outcomes
Presence or absence of urinary urgency
One study reported on the presence or absence of urinary urgency with data taken from bladder diaries and reported as episodes per day following eight weeks of treatment (Yang 2016). The evidence is very uncertain about the effect of acupuncture on the presence or absence of urinary urgency compared to sham acupuncture (mean difference (MD) ‐4.52, 95% CI ‐11.33 to 2.29; 1 study; 25 participants; Analysis 2.3; Table 2; very low‐certainty evidence). The lower CI is implausible given the nature of the outcome in question.
2.3. Analysis.

Comparison 2: Acupuncture versus sham acupuncture, Outcome 3: Presence or absence of urinary urgency
Daytime urinary frequency
Two studies reported on frequency of micturition (Aydoğmuş 2014; Yang 2016). The evidence is very uncertain about the effect of acupuncture on daytime urinary frequency within eight weeks of treatment (2 studies; 77 participants; Table 2; very low‐certainty evidence). Yang 2016 reported mean number of voids in a 24‐hour period. The acupuncture group had a mean number of voids of 11.58 compared to mean number of voids in the sham acupuncture group of 13.62. Aydoğmuş 2014 compared the time between voids. Following acupuncture, 11 of 28 participants could delay voiding for more than two hours. Following sham acupuncture, 0 of 24 participants could delay voiding for more than two hours.
Episodes of urinary incontinence in a 24‐hour period
Two studies reported on episodes of incontinence (Lin 2020; Yang 2016). Acupuncture probably results in little to no difference in episodes of urinary incontinence in a 24‐hour period compared with sham acupuncture following eight weeks of treatment (MD 0.55, 95% CI ‐1.51 to 2.60; I2 = 57%; 2 studies; 121 participants; Analysis 2.4; Table 2; moderate‐certainty evidence).
2.4. Analysis.

Comparison 2: Acupuncture versus sham acupuncture, Outcome 4: Episodes of urinary incontinence in a 24‐hour period
Episodes of nocturia
One study reported on episodes of nocturia (Yang 2016). The evidence is very uncertain about the effect of acupuncture on episodes of nocturia compared with sham acupuncture following eight weeks of treatment (MD ‐2.52, 95% CI ‐4.80 to ‐0.24; 1 study; 25 participants; Analysis 2.5; Table 2; very low‐certainty evidence). The lower CI is implausible given the nature of the outcome in question.
2.5. Analysis.

Comparison 2: Acupuncture versus sham acupuncture, Outcome 5: Episodes of nocturia
Improvement in objective measures of urinary incontinence
Zhang 2015 reported on urodynamic testing parameters following six weeks of treatment, including:
1st sensation of filling in millilitres (MD 17.20, 95% CI 4.66 to 29.74; 1 study; 45 participants; Analysis 2.6);
volume at first urge in millilitres (MD ‐10.00, 95% CI ‐28.57 to 8.57; 1 study; 45 participants; Analysis 2.7);
maximum cystometric capacity in millilitres (MD 53.80, 95% CI 26.68 to 80.92; 1 study; 45 participants; Analysis 2.8);
QMax in millilitres (MD ‐1.40, 95% CI ‐3.65 to 0.85; 1 study; 45 participants; Analysis 2.9); and
post void residual in millilitres (MD 0.90, 95% CI ‐2.81 to 4.61; 1 study; 45 participants; Analysis 2.10).
2.6. Analysis.

Comparison 2: Acupuncture versus sham acupuncture, Outcome 6: Improvement in objective measures of urinary incontinence (first sensation of filling in mL)
2.7. Analysis.

Comparison 2: Acupuncture versus sham acupuncture, Outcome 7: Improvement in objective measures of urinary incontinence (first urge in mL)
2.8. Analysis.

Comparison 2: Acupuncture versus sham acupuncture, Outcome 8: Improvement in objective measures of urinary incontinence (maximum cystometric capacity in mL)
2.9. Analysis.

Comparison 2: Acupuncture versus sham acupuncture, Outcome 9: Improvement in objective measures of urinary incontinence (QMax mL/sec)
2.10. Analysis.

Comparison 2: Acupuncture versus sham acupuncture, Outcome 10: Improvement in objective measures of urinary incontinence (post void residual in mL)
The reported difference between the acupuncture and sham acupuncture groups is extremely small and is unlikely to result in a functional difference.
Improvement in general quality of life
Zhang 2015 reported a general quality of life measure, using the Kings Fund Questionnaire. It is scored from 0 (best) to 900 (worst) and a lower score indicates a better quality of life. Although the results suggest an improvement in quality of life in the acupuncture group compared to the sham acupuncture group after six weeks of treatment (MD ‐260.00, 95% CI ‐314.60 to ‐205.40; 1 study; 45 participants; Analysis 2.11), the number of participants was small and the follow‐up period was short, leading to a low certainty of evidence.
2.11. Analysis.

Comparison 2: Acupuncture versus sham acupuncture, Outcome 11: Improvement in general quality of life
Acupuncture versus conservative treatments
Two studies including a total of 522 participants compared acupuncture to conservative treatments (Liu 2019; Solberg 2016). Liu 2019 compared acupuncture with both medication and pelvic floor muscle training, while Solberg 2016 compared acupuncture with pelvic floor muscle training alone.
Primary outcomes
Number of participants whose overactive bladder symptoms were cured or improved
The results from the two studies could not be pooled as although they both used the same outcome measure, the ICIQ‐SF, they chose to report differently.
Liu 2019 used the ICIQ‐SF to measure change in urinary symptoms and reported the outcomes as change scores with adjusted mean (95% CIs) following 12 weeks of treatment. The acupuncture group were reported as 3.96 (95% CI ‐3.61 to 4.32), while the solifenacin and pelvic floor muscle training group were reported as 3.73 (95% CI ‐3.37 to 4.09).
Solberg 2016 used the ICIQ‐SF to assess change in urinary symptoms and reported as change scores with median and interquartile range (IQR). The acupuncture group had a median of 6.5 (IQR 4) following 12 weeks of treatment, while the pelvic floor muscle training group had a median of 5 (IQR 5.3).
Number of major adverse events
Both studies reported that there were no major adverse events.
Number of minor adverse events
Two studies reported that there may be a reduction in minor adverse events with acupuncture compared to conservative treatments following 12 weeks of treatment (RR 0.33, 95% CI 0.26 to 4.1; 519 participants; I2 = 52%; Analysis 3.1).
3.1. Analysis.

Comparison 3: Acupuncture versus conservative treatment, Outcome 1: Minor adverse events
Secondary outcomes
Presence or absence of urinary urgency
Liu 2019 reported the change in urgency episodes over a 72‐hour period with bladder diary data using adjusted mean and 95% CIs. In both groups the episodes of urgency reduced following the intervention following 12 weeks of treatment (acupuncture group 2.62, 95% CI ‐2.05 to 3.2; solifenacin/pelvic floor muscle training group 2.99, 95% CI ‐2.41 to 3.85).
Daytime urinary frequency
Liu 2019 reported the change in micturition episodes over a 72‐hour period using bladder diary data. The study reported using adjusted mean episodes and 95% CIs. In both groups the episodes of frequency reduced following 12 weeks of treatment (acupuncture group 3.23, 95% CI ‐2.53 to 3.93; solifenacin/pelvic floor muscle training group 3.62, 95% CI ‐2.91 to 4.33).
Episodes of urinary incontinence in a 24‐hour period
Liu 2019 reported the change in episodes of incontinence over a 72‐hour period using bladder diary data. The study reported using adjusted mean and 95% CIs and percentage change. In both groups the episodes of incontinence reduced following 12 weeks of treatment (acupuncture group 7.38, 95% CI ‐6.53 to 8.23, ‐37.83%; solifenacin/pelvic floor muscle training group 7.51 95% CI 6.61 to 8.42, ‐36.49%).
Episodes of nocturia
Liu 2019 reported the change in episodes of nocturia over a 72‐hour period using bladder diary data. The study reported using adjusted mean number of episodes and 95% CIs. In both groups the episodes of nocturia reduced following 12 weeks of treatment (acupuncture group 0.79, 95% CI ‐0.5 to 1.01; solifenacin/pelvic floor muscle training group 0.87, 95% CI ‐0.65 to 1.09).
Improvement in objective measures of urinary incontinence
Not reported.
Improvement in general quality of life
Not reported.
Acupuncture versus medication
A total of 11 studies including a total of 1192 participants compared acupuncture with medication for overactive bladder. Four studies used solifenacin (Aydoğmuş 2014; Liu 2019; Wang 2013a; Yang 2016), six studies used tolterodine (Hong 2015; Chen 2009; Shen 2020; Wang 2011; Yu 2012; Yuan 2015), and one study used oxybutynin (Kelleher 1994).
Primary outcomes
Number of participants whose overactive bladder symptoms were cured or improved
Five studies reported cure or improvement rates using participant subjective opinion scales (total effective rates). Acupuncture may result in a slight increase in cure or improvement of overactive bladder symptoms compared with medication within four weeks of treatment (RR 1.25, 95% CI 1.10 to 1.43; 5 studies; 258 participants; I2 = 19%; Analysis 4.1; Table 3; low‐certainty evidence).
4.1. Analysis.

Comparison 4: Acupuncture versus medication, Outcome 1: Cure or improvement in urinary symptoms
Number of major adverse events
All studies reported that there were no major adverse events.
Number of minor adverse events
Eight studies reported minor adverse events (Aydoğmuş 2014; Hong 2015; Kelleher 1994; Liu 2019; Shen 2020; Wang 2011; Yang 2016; Yuan 2015). Acupuncture may reduce the number of minor adverse events compared to medication within 12 weeks of treatment (RR 0.34, 95% CI 0.26 to 0.45; 8 studies; 1004 participants; I² = 51%; Analysis 4.2; Table 3; low‐certainty evidence). The details of the types of minor adverse events are summarised in Table 5.
4.2. Analysis.

Comparison 4: Acupuncture versus medication, Outcome 2: Number of minor adverse events
Secondary outcomes
Presence or absence of urinary urgency
Two studies addressed this outcome (Wang 2013a; Yang 2016). The evidence is uncertain about the effect of acupuncture on the presence or absence of urinary urgency following four weeks of treatment (MD ‐0.40, 95% CI ‐0.56 to ‐0.24; 2 studies; 80 participants; I² = 0%; Analysis 4.3; Table 3; very low‐certainty evidence).
4.3. Analysis.

Comparison 4: Acupuncture versus medication, Outcome 3: Presence or absence of urinary urgency
Daytime urinary frequency
Four studies reported on this outcome, assessing voids per day from bladder diary data (Wang 2011; Wang 2013a; Yang 2016; Yuan 2015). Acupuncture may result in little to no difference in urinary frequency compared to medication for overactive bladder symptoms following four weeks of treatment (MD 0.73, 95% CI ‐0.39 to 1.85; 4 studies; 360 participants; I² = 28%; Analysis 4.4; Table 3; low‐certainty evidence).
4.4. Analysis.

Comparison 4: Acupuncture versus medication, Outcome 4: Daytime urinary frequency
Episodes of urinary incontinence in a 24‐hour period
One study reported on this outcome, assessing episodes per 24 hours from bladder diary data (Yang 2016). The evidence is very uncertain about the effect of acupuncture on episodes of incontinence in a 24‐hour period when compared to medication following eight weeks of treatment (MD ‐0.33, 95% CI ‐2.75 to 2.09; 1 study; 20 participants; Analysis 4.5; Table 3; very low‐certainty evidence).
4.5. Analysis.

Comparison 4: Acupuncture versus medication, Outcome 5: Episodes of urinary incontinence in a 24‐hour period
Episodes of nocturia
Two studies reported on this outcome, assessing episodes per night from bladder diary data (Wang 2013a; Yang 2016). Acupuncture may slightly reduce the number of episodes of nocturia compared with medication following four weeks of treatment (MD ‐0.50, 95% CI ‐0.65 to ‐0.36; 2 studies; 80 participants; I² = 0%; Analysis 4.6; Table 3; low‐certainty evidence).
4.6. Analysis.

Comparison 4: Acupuncture versus medication, Outcome 6: Episodes of nocturia
Improvement in objective measures of urinary incontinence
Volume of urine voided in millilitres was reported by one study (Wang 2013a) (MD ‐4.00, 95% CI ‐20.71 to 12.71; 1 study; 60 participants; Analysis 4.7). There is a very small difference between the acupuncture and medication groups that is unlikely result in a functional difference.
4.7. Analysis.

Comparison 4: Acupuncture versus medication, Outcome 7: Improvement in objective measures of urinary incontinence (volume of urine voided)
Improvement in general quality of life
Not reported.
Discussion
Acupuncture has been suggested as an alternative treatment modality for overactive bladder. We discovered a wide variety of acupuncture techniques, treatment regimens, comparators used, lengths of follow‐up, outcomes used for measuring efficacy and ways in which outcome data were reported. This led to difficulty in pooling the data to answer the question of whether acupuncture is an effective treatment for overactive bladder in adults.
Summary of main results
This review had three primary outcomes of interest.
Cure or improvement of overactive bladder symptoms
Only one study compared acupuncture to no treatment (Solberg 2016). The main focus of this study was feasibility and the number of participants was very small (n = 24). Improvement was measured by applying the International Consultation on Incontinence Questionnaire Short Form (ICIQ‐SF). The minimal clinically important difference for the ICIQ‐SF is 4 points (Lim 2019); only the acupuncture group achieved this level of reduction, reducing the median ICIQ‐SF from 13 at baseline to 6.5 after 12 weeks of intervention. Acupuncture may improve symptoms of overactive bladder compared to no treatment but the evidence is very uncertain, as we only have one feasibility study to draw upon (Table 1).
Five studies addressed the comparison of acupuncture with sham acupuncture (Aydoğmuş 2014; Engberg 2009; Lin 2020; Yang 2016; Zhang 2015). The type, application and duration of acupuncture, and outcomes chosen, all varied considerably between studies, making pooling data difficult. The meta‐analysis suggests that acupuncture results in little to no difference in cure or improvement in overactive bladder symptoms when compared to sham acupuncture but the evidence is very low‐certainty due to risk of bias in study design, inconsistency between studies and small participant numbers (Table 2).
Eleven studies compared acupuncture with medications for symptoms of overactive bladder (Aydoğmuş 2014; Chen 2009; Hong 2015; Kelleher 1994; Liu 2019; Shen 2020; Wang 2011; Wang 2013a; Yang 2016; Yu 2012; Yuan 2015). Acupuncture may result in a slight increase in cure or improvement in overactive bladder symptoms compared to medication but the certainty of evidence is low due to risk of bias in study design, in particular the lack of participant blinding to intervention group and imprecision due to small participant numbers (Table 3). Three studies in this comparison combined medication with an additional conservative treatment, pelvic floor muscle training or bladder retraining (Hong 2015; Liu 2019; Yu 2012). Whilst these designs reflect how clinical care is delivered in a 'real world' situation, it is impossible to define which of the treatments used was responsible for the effects observed. This therefore makes interpretation of the results difficult.
Number of major adverse events
There were 1395 participants in the included studies and no reports of major adverse events (Table 1; Table 2; Table 3). However, major adverse events are a rare occurrence in acupuncture treatment (MacPherson 2001), so the number of participants included in this review is likely too small to detect such an occurrence.
Number of minor adverse events
Twelve studies included information with regard to minor adverse events (Aydoğmuş 2014; Engberg 2009; Hong 2015; Kelleher 1994; Lin 2020; Liu 2019; Shen 2020; Solberg 2016; Wang 2011; Yang 2016; Yuan 2015; Zhang 2015). The reported types of minor adverse event included pain on needle insertion and bleeding on needle removal for acupuncture groups, allergy to adhesive tape in the sham acupuncture groups and dry mouth in the medication groups. There is moderate‐certainty evidence that acupuncture probably leads to a slight increase in the number of minor adverse events compared to sham acupuncture (Table 2). However, small numbers of participants leads to caution regarding these findings. In comparison, acupuncture may lead to fewer minor adverse events when compared to medication for overactive bladder; however, the evidence is of low certainty due to high heterogeneity between studies and wide confidence intervals (Table 3).
Overall completeness and applicability of evidence
Each outcome selected for this review was measured in at least one study. The included studies related to the population stipulated in the review question and the interventions and comparators of interest were all present in at least one included study. The search strategy used was extensive and covered studies published in English and Chinese. We used Google Translate to identify whether two studies found (one in German and one in Spanish) fitted the criteria for inclusion; both were excluded.
The number of studies identified in the searches demonstrates the level of interest in this subject. However, only 15 studies were finally included in the review, indicating that there is considerable variation in the way research is being conducted. There was a lack of consistency in:
how a diagnosis of overactive bladder was defined;
study design;
outcome measures used;
application of acupuncture in terms of point selection, type and depth of insertion, use of electrical or manual stimulation, length of treatment and frequency of treatment;
follow‐up assessment; and
assessment of longevity of effect.
Sample sizes in the majority of studies were lower than 50 and the total number of participants included was 1395. The current evidence does not address differences that may be observed between subgroups of people with overactive bladder, i.e. men and women, pre and post menopausal women, or populations grouped by age. There is a lack of evidence regarding the rationale underpinning the acupuncture approach, for example the traditional Chinese medicine approach versus a western acupuncture approach.
There is also debate regarding sham acupuncture procedures (Deng 2015). This relates to whether any stimulation applied at a known acupuncture point may exert a physiological effect. This may in part explain the lack of difference in effect between acupuncture and sham acupuncture applications.
Most studies were conducted over a short time period with few having follow‐up periods of any length. Therefore, the long‐term effects of acupuncture treatment on overactive bladder symptoms is yet to be established.
The review team conclude that the current literature does not fully answer all the outstanding questions regarding the role of acupuncture in the treatment of overactive bladder and its applicability in healthcare services
Quality of the evidence
GRADE assessment of the evidence resulted in low‐ or very low‐certainty evidence for the majority of outcomes. We downgraded the evidence largely due to risk of bias in study designs, as well as imprecision due to the small numbers of participants included in studies and wide confidence intervals. Most included studies had small numbers of participants and there was heterogeneity in design, comparators, type of intervention, length of intervention and length of follow‐up. All these factors reduced our ability to pool data, with some analyses performed only containing one small study and giving implausible confidence intervals given the type of outcome being considered.
A further contribution to the downgrading of evidence was the inadequate blinding of participants, which is difficult to achieve in acupuncture protocols and resulted in many studies being judged at high risk of performance bias. Sham acupuncture procedures exist but there are arguments regarding their efficacy (Deng 2015), while the preservation of blinding needs to be assessed as part of the study procedures. The majority of included studies either did not use a sham procedure or did not provide sufficient evidence of the preservation of blinding. Only one study provided both (Lin 2020).
Potential biases in the review process
We undertook extensive searching of both English and Chinese language databases during this review to minimise the risk of missing relevant studies due to language barriers. We used two teams of review authors and divided the work into reports available in English and those only available in Chinese. Both review teams used Covidence software to complete risk of bias assessments and extract data and consensus was agreed without the need for arbitration by a third review author. These steps involve subjective assessment and may carry some risk of bias. During the production of the review report there was constant communication between review authors to ensure that the Chinese studies were accurately reported and presented.
Agreements and disagreements with other studies or reviews
A systematic review was conducted in 2018 addressing the efficacy and safety of using acupuncture to treatment symptoms of overactive bladder in adults (Zhao 2018). This review included trials using acupuncture combined with other treatments, as well as acupuncture as a standalone intervention. Therefore, the focus of our review differs from this review. All studies included in this review have acupuncture as a standalone arm in the study design. Zhao 2018 concluded that acupuncture may reduce episodes of urinary frequency, urge incontinence and nocturia but the conclusions of the review were limited by the quality of the evidence, small sample sizes and heterogeneity in study designs. Our review agrees with the limitations expressed by Zhao 2018. The diversity of comparisons used, outcomes measured and methods of reporting have limited the conclusions that can be drawn from the evidence we collected.
Brief economic commentary
To supplement the main review of the use of acupuncture for treating overactive bladder in adults, we sought to identify relevant economic evaluations as part of the review. No economic studies were identified that analysed the use of acupuncture in adults with overactive bladder. The apparent shortage of relevant economic evaluations indicates that there is a paucity of economic evidence as to the efficiency of acupuncture for treating overactive bladder in adults.
Authors' conclusions
Implications for practice.
The question of whether acupuncture is an effective treatment for overactive bladder symptoms remains unresolved. Care providers and patients may wish to consider the use of acupuncture to treat overactive bladder symptoms where other treatment modalities are unsuccessful, carry a significant risk of side effects or are considered undesirable by the patient.
If used, patients should be made aware that the mechanisms underlying the effects of acupuncture remain poorly understood and that, as with other treatments, it does not produce a significant reduction in symptoms in all patients.
Implications for research.
Further sufficiently powered, well‐designed studies are required to answer the question posed by this review. Areas for consideration in future studies should include:
a core outcome set for overactive bladder treatment studies derived from stakeholder engagement;
acupuncture regimens to include a standardised point selection, application, treatment length, with or without stimulation, and follow‐up length; and
the use of a sham arm should be considered to assess the possible mechanisms that may underpin the physiological effects of acupuncture.
Adoption to the STRICTA guidelines (reporting standards for acupuncture studies) is also recommended (MacPherson 2010).
The use of combined treatments in future studies should be regarded with caution. While the use of combined treatments in both intervention and comparator arms may reflect 'real world' clinical treatments, it poses difficulties when analysing the results of trials (i.e. it is not possible to know which of the treatments is responsible for the observed effects). Consideration of whether or not acupuncture is a cost‐effective treatment for a long‐term condition should be addressed.
History
Protocol first published: Issue 1, 2020
Acknowledgements
We are grateful for the guidance of Lindsey Elstub, Eugenie Johnson, Sheila Wallace and Luke Vale in the production of the review. We are also grateful to Caroline Smith, Sergio Ferreira and Wendy Free for valuable comments on this work. We acknowledge the assistance of Hannah O'Keefe in uploading the Chinese searches to Covidence. We are grateful for advice and guidance regarding software use from the RevManWeb, Covidence and GRADEpro support teams.
Appendices
Appendix 1. Glossary of terms
Acetylcholine: a substance that transmits nerve impulses within the central and peripheral nervous systems.
Acupuncture: a treatment derived from ancient Chinese medicine. Fine needles are inserted at certain sites in the body for therapeutic or preventative purposes.
Acupuncture point: a point of the body where an acupuncture needle may be inserted. Acupuncture points are identified by anatomical landmarks and palpation.
Acupoint: a shorthand way of referring to an acupuncture point.
Afferent nerve: a nerve that bring information from the body to the brain.
Anticholingeric: a substance that blocks the action of the neurotransmitter acetylcholine at synapses in the central and the peripheral nervous system. Medications used to treat symptoms of overactive bladder (OAB) include anticholinergic agents.
Augmentation cystoplasty: a procedure that involves making the bladder bigger by adding a piece of tissue from the intestine into the bladder wall. This may improve the ability of the bladder to store urine. It is rarely performed for symptoms of OAB and is viewed as a treatment of last resort.
Bladder brain control matrix: the complex nerve pathways governing bladder function.
Bladder retraining: the first‐line treatment for urinary symptoms associated with OAB. It involves teaching the bladder to hold more urine and helps to reduce urinary frequency.
β3‐adrenoreceptor agonists: a medication that relaxes smooth muscle and so can have a beneficial effect on OAB symptoms.
Comorbidities: the presence of one or more additional conditions co‐occurring with a primary condition.
Dermatome: an area of sensory nerves near the skin that are supplied by a specific spinal nerve root. The body can be divided into regions that are mainly supplied by a single spinal nerve. Dermatomes are named according to their spinal nerve root.
Economic evaluation: the application of analytical methods to identify measure and value both the costs and benefits of alternative interventions in order to provide evidence regarding technical or allocative efficiency and aid decision making for resource allocation (definition taken from the Campbell and Cochrane Economics Methods Group's Glossary).
Efferent nerve: a nerve that brings information from the brain to the body.
Electroacupuncture: an acupuncture technique that applies small electrical currents to needles that have been inserted at specific points on the body.
Intravesical botulinum toxin injection: a form of treatment where botulinum toxin is injected into the smooth muscle of the bladder wall (the detrusor muscle) in order to treat symptoms of OAB.
Limbic system: interconnected structures in the midline of the brain involved with emotion, memory and regulatory systems.
Meridians: a concept in Traditional Chinese Medicine (TCM) about a path through which the life‐energy known as "Qi" flows.
Nocturia: the number of times urine is passed during the main sleep period.
Overactive bladder(OAB): a group of symptoms affecting the urinary system that includes urinary urgency (a sudden and intense desire to pass urine that is hard to defer), frequency (passing urine more frequently than 5 to 8 times in a 24‐hour period), nocturia (waking to pass urine at night), urinary incontinence (involuntary passing urine).
OAB‐dry: OAB symptoms without urinary incontinence.
OAB‐wet: OAB symptoms with urinary incontinence.
Orbitofrontal cortex: a region in the frontal lobes of the brain that is involved in the cognitive process of decision‐making.
Prefrontal cortex: the anterior part of the frontal lobe of the brain, which is highly developed in humans and concerned with complex cognitive, emotional and behavioural functions.
Peri‐aqueductal gray (PAG): a mid‐brain structure that plays a critical role in autonomic function and behavioural responses to threatening stimuli.
Qi: believed to be a vital force forming part of any living entity in TCM.
Traditional Chinese Medicine(TCM): a system of medicine traditionally practised in China; acupuncture is one component of this system.
Sacral neuromodulation: a form of treatment where a small nerve stimulator device is implanted in the body to provide stimulation to the sacral nerves. This stimulation is thought to have an effect on the nerves passing between the bladder and the brain and relieve the symptoms of OAB.
Smooth muscle: a type of muscle tissue that contracts without conscious control. The detrusor muscle that forms the bladder wall is made of smooth muscle.
Urinary diversion: a procedure where the tubes that lead from the kidneys to the bladder (ureters) are redirected to outside of the body. The urine is then collected directly without it flowing into the bladder. Urinary diversion is only performed if other treatments have been unsuccessful or are unsuitable.
Urinary incontinence (UI): involuntary passing of urine.
Urothelial cells: the cells that form the lining of the bladder.
Appendix 2. Search of the Cochrane Incontinence Specialised Register for clinical effectiveness studies
The search terms used to search the Cochrane Incontinence Specialised Register are given below:
((design.cct*) OR (design.rct*)) AND ((topic.urine.incon*) OR (topic.urine.overactive*)) AND (intvent.phys.acupuncture*) All searches were of the keywords field of EndNote (EndNote 2018).
Appendix 3. Allied and Complementary Medicine Database (AMED) search terms
The search terms used to search the Allied and Complementary Medicine Database (AMED) on EBSCOhost are given below:
(overactive bladder OR overactive bladder syndrome OR urgency OR oab OR urinary incontinence OR sensitive bladder) AND (acupuncture OR acupuncture therapy OR acupuncture treatment OR electroacupuncture OR dry needling)
Appendix 4. Chinese database search terms
The search terms used to search the Chinese databases are given below:
| Databases | Search terms | Search terms (Pinyin) |
| CNKI | SU=('膀胱过度活动'+'OAB'+'OAS'+'尿急综合征'+'尿频‐尿急综合征'+’尿急’+’尿频’+’尿失禁’) and SU=(‘针’+'针刺'+'耳针'+'头针'+'电针'+'经皮电刺激') and FT=('随机'+'半随机'+'交叉对照') and NOT TI=('动物'+'鼠'+'犬'+'兔'+’猴’) |
SU=('Pangguang Guodu Huodong'+'OAB'+'OAS'+'Niaoji Zonghezheng'+'Niaopin‐Niaoji Zonghezheng'+’Niaoji’+’Niaopin’+’Niaoshijin’) and SU=(‘Zhen’+'Zhenci'+'Erzhen'+'Touzhen'+'Dianzhen'+'Jingpi Dianciji') and FT=('Suiji'+'Ban Suiji'+'Jiaocha Duizhao') and NOT TI=('Dongwu'+'Shu'+'Quan'+'Tu'+'Hou') |
| WANFANG | 主题:(膀胱过度活动症 or OAB or 膀胱过度活动综合征 or OAS or 尿急综合征or 尿频‐尿急综合征) * 主题:(针刺 or 耳针 or 电针 or 头针or 经皮电针 )* (随机 or 半随机 or 交叉对照) | Topic:(Pangguang Guodu Huodong Zheng or OAB or Pangguang Guodu Huodong Zonghezheng or OAS or Niaoji Zonghezheng or Niaopin‐Niaoji Zonghezheng) * Topic:(Zhenci or Erzhen or Dianzhen or Touzhen or Jingpi Dianzhen )* (Suiji or Ban Suiji or Jiaocha Duizhao) |
| VIP | (M=膀胱过度活动症+M=OAB+M=膀胱过度活动综合征+M=OAS+M=尿急综合征+M=尿频‐尿急综合征)*(M=针刺+M=耳针+M=头针+M=电针+M=经皮电刺激)*U=随机 | (M=Pangguang Guodu Huodong Zheng+M=OAB+M=Pangguang Guodu Huodong Zonghezheng+M=OAS+M=Niaoji Zonghezheng+M=Niaopin‐Niaoji Zonghezheng)*(M=Zhenci+M=Erzhen+M=Touzhen+M=Dianzhen+M=Jingpi Dianciji)*U=Suiji |
Appendix 5. Search methods for the brief economic commentary (BEC)
We performed electronic searches designed to identify published reports of relevant economic evaluations to inform the brief economic commentary (BEC) (see 'Incorporating economic evidence' in the Methods).
We searched the Cochrane Incontinence Specialised Register of Economic Evaluations (EEs) which consists of searches of:
NHS Economic Evaluation Database (EED) on the UK Centre for Reviews and Dissemination (CRD) website (covering from the earliest record in NHS EED, dating from 1968, up to and including 31 December 2014 when their coverage ended)
As NHS EED is no longer actively updated, we performed additional searches of the following databases to identify eligible studies added to these databases from 1 January 2015 onwards:
MEDLINE on OvidSP (covering 1 January 1946 to June Week 5 2022); and
Embase (on OvidSP) (covering 1 January 1974 to to 2022 Week 27).
The search terms used to search the Cochrane Incontinence Specialised Register of Economic Evaluations are given below:
((topic.urine.incon*) OR (topic.urine.overactive*)) AND (intvent.phys.acupuncture*) All searches were of the keywords field of EndNote (EndNote 2018).
The economic evaluation search filters applied to our MEDLINE and Embase search strategies were those formerly used by the CRD to identify published reports of full economic evaluations for indexing on NHS EED. These economic evaluation search filters remain freely available on the CRD Database web-pages (CRD 2015). The other search lines in the MEDLINE and Embase search strategies were adapted from the electronic search strategies run for our Cochrane Incontinence Specialised Register of clinical effectiveness studies related to urinary incontinence/overactive bladder. Similarly, our NHS EED search strategy was adapted from search strategies run for our Specialised Register and based on text word and MeSH terms (capturing relevant P‐I‐C concepts) used to identify eligible studies of intervention effects. We followed the current economic methods guidance (Aluko 2022).
The search for the Cochrane Incontinence Specialised Register of EEs was only current up to 20 October 2021 and so one of the review authors (AK) screened an updated search of MEDLINE and Embase (conducted on 11 July 2022) to bring the Specialised Register search for EEs up to date. The search strategies used in MEDLINE and Embase to populate the Cochrane Incontinence Specialised Register of EEs are given below. The original search of NHS EED to begin populating the Specialised Register of EEs is given at the end of this Appendix.
MEDLINE on OvidSP (covering 1 January 1946 to June Week 5 2022) was last searched on 11 July 2022
| 1. | Economics/ |
| 2. | exp "costs and cost analysis"/ |
| 3. | Economics, Dental/ |
| 4. | exp economics, hospital/ |
| 5. | Economics, Medical/ |
| 6. | Economics, Nursing/ |
| 7. | Economics, Pharmaceutical/ |
| 8. | (economic$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. |
| 9. | (expenditure$ not energy).ti,ab. |
| 10. | value for money.ti,ab. |
| 11. | budget$.ti,ab. |
| 12. | or/1‐11 |
| 13. | ((energy or oxygen) adj cost).ti,ab. |
| 14. | (metabolic adj cost).ti,ab. |
| 15. | ((energy or oxygen) adj expenditure).ti,ab. |
| 16. | or/13‐15 |
| 17. | 12 not 16 |
| 18. | letter.pt. |
| 19. | editorial.pt. |
| 20. | historical article.pt. |
| 21. | or/18‐20 |
| 22. | 17 not 21 |
| 23. | exp animals/ not humans/ |
| 24. | 22 not 23 |
| 25. | (incontinen$ or continen$).tw. |
| 26. | exp urinary incontinence/ |
| 27. | nycturia.tw. |
| 28. | ((bladder or detrusor or vesic$) adj5 (instability or stab$ or unstable or irritab$ or hyperreflexia or dys?ynerg$ or dyskinesi$ or irritat$)).tw. |
| 29. | (urin$ adj2 (leak$ or urge$ or frequen$)).tw. |
| 30. | dribbl$.tw. |
| 31. | bladder, neurogenic/ |
| 32. | ((bladder or detrusor or vesic$) adj2 (hyper$ or overactiv$)).tw. |
| 33. | (spinal adj2 bladder$).tw. |
| 34. | (bladder$ adj2 (neuropath$ or neurogen$ or neurolog$)).tw. |
| 35. | (nervous adj1 (pollakisur$ or pollakiur$)).tw. |
| 36. | urinary bladder, overactive/ |
| 37. | exp enuresis/ |
| 38. | enure$.tw. |
| 39. | bedwet$.tw. |
| 40. | bed‐wet$.tw. |
| 41. | (bed adj5 wet$).tw. |
| 42. | (diurnal adj5 wet$).tw. |
| 43. | diurnal‐wet$.tw. |
| 44. | ((daytime or day‐time or nighttime or night‐time or nightime) adj5 wet$).tw. |
| 45. | (void$ adj2 dysfunct$).tw. |
| 46. | ((urin$ or bladder) adj5 sphincter$).tw. |
| 47. | (urethra$ adj2 sphincter$).tw. |
| 48. | (bladder adj2 neck).tw. |
| 49. | (vesic$ adj1 (neck$ or cervi$)).tw. |
| 50. | (detrusor adj1 sphincter$).tw. |
| 51. | or/25‐50 |
| 52. | 24 and 51 |
Embase (on OvidSP) (covering 1 January 1974 to to 2022 Week 27) was last searched on 11 July 2022
| 1. | Health Economics/ |
| 2. | exp Economic Evaluation/ |
| 3. | exp Health Care Cost/ |
| 4. | pharmacoeconomics/ |
| 5. | (econom$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. |
| 6. | (expenditure$ not energy).ti,ab. |
| 7. | (value adj2 money).ti,ab. |
| 8. | budget$.ti,ab. |
| 9. | or/1‐8 |
| 10. | letter.pt. |
| 11. | editorial.pt. |
| 12. | note.pt. |
| 13. | or/10‐12 |
| 14. | 9 not 13 |
| 15. | (metabolic adj cost).ti,ab. |
| 16. | ((energy or oxygen) adj cost).ti,ab. |
| 17. | ((energy or oxygen) adj expenditure).ti,ab. |
| 18. | 15 or 16 or 17 |
| 19. | 14 not 18 |
| 20. | animal/ |
| 21. | exp animal experiment/ |
| 22. | nonhuman/ |
| 23. | (rat or rats or mouse or mice or hamster or hamsters or animal or animals or dog or dogs or cat or cats or bovine or sheep).ti,ab,sh. |
| 24. | 20 or 21 or 22 or 23 |
| 25. | exp human/ |
| 26. | human experiment/ |
| 27. | 25 or 26 |
| 28. | 24 not (24 and 27) |
| 29. | 19 not 28 |
| 30. | conference abstract.pt. |
| 31. | 29 not 30 |
| 32. | incontinence/ or mixed incontinence/ or stress incontinence/ or urge incontinence/ or urine incontinence/ |
| 33. | continence/ |
| 34. | overactive bladder/ |
| 35. | micturition disorder/ or lower urinary tract symptom/ or pollakisuria/ |
| 36. | urinary dysfunction/ or bladder instability/ or detrusor dyssynergia/ or neurogenic bladder/ or urinary urgency/ or urine extravasation/ |
| 37. | (incontinen$ or continen$).tw. |
| 38. | ((bladder or detrusor or vesic$) adj5 (instab$ or stab$ or unstab$ or irritab$ or hyperreflexi$ or dys?ynerg$ or dyskinesi$ or irritat$)).tw. |
| 39. | (urin$ adj2 leak$).tw. |
| 40. | ((bladder or detrusor or vesic$) adj2 (hyper$ or overactiv$)).tw. |
| 41. | (bladder$ adj2 (neuropath$ or neurogen* or neurolog$)).tw. |
| 42. | (nervous adj pollakisur$).tw. |
| 43. | or/32‐42 |
| 44. | 31 and 43 |
NHS EED on CRD website was searched on 14 June 2019 (in all fields)
| Line | Search |
| 1 | MeSH DESCRIPTOR pelvic floor EXPLODE ALL TREES IN NHSEED |
| 2 | MeSH DESCRIPTOR pelvic floor disorders EXPLODE ALL TREES IN NHSEED |
| 3 | MeSH DESCRIPTOR Urinary Bladder, Neurogenic EXPLODE ALL TREES IN NHSEED |
| 4 | MeSH DESCRIPTOR Urinary Bladder, overactive EXPLODE ALL TREES IN NHSEED |
| 5 | ((incontinen* ) OR (continen*)) IN NHSEED |
| 6 | ((floor adj2 pelvi* ) OR (pelvi* adj2 floor)) IN NHSEED |
| 7 | ((nycturia)) IN NHSEED |
| 8 | (((urin* or bladder) adj5 sphincter*) OR (sphincter* adj5 (urin* or bladder))) IN NHSEED |
| 9 | (((bladder OR detrusor OR vesic*) ADJ5 (instability OR stab* OR unstable OR irritab* OR hyperreflexia OR dysynerg* OR dyskinesi* OR irritat*)) OR ((instability OR stab* OR unstable OR irritab* OR hyperreflexia OR dysynerg* OR dyskinesi* OR irritat*) ADJ5 (bladder OR detrusor OR vesic*) )) IN NHSEED |
| 10 | ((urethra* ADJ2 sphincter*) OR (sphincter* ADJ2 urethra* )) IN NHSEED |
| 11 | ((bladder ADJ2 neck) OR (neck ADJ2 bladder )) IN NHSEED |
| 12 | ((urin* ADJ2 (leak* OR urge* OR frequen*)) OR ((leak* OR urge* OR frequen*) ADJ2 urin* )) IN NHSEED |
| 13 | (dribbl*) IN NHSEED |
| 14 | ((vesic* ADJ1 (neck* OR cervi*)) OR ((neck* OR cervi*) ADJ1 vesic*)) IN NHSEED |
| 15 | (((bladder OR detrusor OR vesic*) ADJ2 (hyper* OR overactiv*)) OR ((hyper* OR overactiv*) ADJ2 (bladder OR detrusor OR vesic*))) IN NHSEED |
| 16 | ((detrusor ADJ1 sphincter*) OR (sphincter* ADJ1 detrusor)) IN NHSEED |
| 17 | ((spinal ADJ2 bladder*) OR (bladder* ADJ2 spinal)) IN NHSEED |
| 18 | ((bladder* ADJ2 (neuropath* OR neurogen* OR neurolog*)) OR ((neuropath* OR neurogen* OR neurolog*) ADJ2 bladder*)) IN NHSEED |
| 19 | ((nervous ADJ1 (pollakisur* OR pollakiur*)) OR ((pollakisur* OR pollakiur*) ADJ1 nervous)) IN NHSEED |
| 20 | (MeSH DESCRIPTOR urinary incontinence EXPLODE ALL TREES) IN NHSEED |
| 21 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 |
Key: $ or * = truncation symbol; tw. = titles and abstracts; / = MeSH or Emtree term; exp = exploded MeSH or Emtree term; adjn = within n words, in any order on Ovid, in fixed order on CRD; ? character may or may not be present.
Data and analyses
Comparison 1. Acupuncture versus no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Cure or improvement in overactive bladder symptoms | 1 | Other data | No numeric data |
Comparison 2. Acupuncture versus sham acupuncture.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Cure or improvement in urinary symptoms | 3 | 151 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐1.03, 0.31] |
| 2.2 Number of minor adverse events | 4 | 222 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.30, 5.36] |
| 2.3 Presence or absence of urinary urgency | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | ‐4.52 [‐11.33, 2.29] |
| 2.4 Episodes of urinary incontinence in a 24‐hour period | 2 | 121 | Mean Difference (IV, Fixed, 95% CI) | 0.55 [‐1.51, 2.60] |
| 2.5 Episodes of nocturia | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | ‐2.52 [‐4.80, ‐0.24] |
| 2.6 Improvement in objective measures of urinary incontinence (first sensation of filling in mL) | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 17.20 [4.66, 29.74] |
| 2.7 Improvement in objective measures of urinary incontinence (first urge in mL) | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | ‐10.00 [‐28.57, 8.57] |
| 2.8 Improvement in objective measures of urinary incontinence (maximum cystometric capacity in mL) | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 53.80 [26.68, 80.92] |
| 2.9 Improvement in objective measures of urinary incontinence (QMax mL/sec) | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | ‐1.40 [‐3.65, 0.85] |
| 2.10 Improvement in objective measures of urinary incontinence (post void residual in mL) | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐2.81, 4.61] |
| 2.11 Improvement in general quality of life | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | ‐260.00 [‐314.60, ‐205.40] |
Comparison 3. Acupuncture versus conservative treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Minor adverse events | 2 | 519 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.26, 0.41] |
Comparison 4. Acupuncture versus medication.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Cure or improvement in urinary symptoms | 5 | 258 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [1.10, 1.43] |
| 4.2 Number of minor adverse events | 8 | 1004 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.26, 0.45] |
| 4.3 Presence or absence of urinary urgency | 2 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐0.56, ‐0.24] |
| 4.4 Daytime urinary frequency | 4 | 360 | Mean Difference (IV, Random, 95% CI) | 0.73 [‐0.39, 1.85] |
| 4.5 Episodes of urinary incontinence in a 24‐hour period | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐0.33 [‐2.75, 2.09] |
| 4.6 Episodes of nocturia | 2 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐0.50 [‐0.65, ‐0.36] |
| 4.7 Improvement in objective measures of urinary incontinence (volume of urine voided) | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐4.00 [‐20.71, 12.71] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aydoğmuş 2014.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel‐group |
|
| Participants |
Country: Turkey Setting: Urology Department Ankara Training Hospital Number of participants: 90 Sex: women Mean age (SD): 38 (12.9) Mean parity: 2.25 Inclusion criteria: OAB symptoms in line with ICS criteria; diagnosis confirmed using the International Consultation on Incontinence‐Short Form (Turkish) (ICIQ‐SF‐T) Exclusion criteria: previous urogenital surgery; pelvic radiotherapy; chronic neurological or endocrine disease; cystocele; stress incontinence; urinary tract infection; medication impacting on urinary symptoms |
|
| Interventions |
Group I (n = 30): solifenacin 5 mg once per day for 4 weeks Group II (n = 30): acupuncture; 25 mm needles were inserted at LI4, SP 6, ST 36, LIV3, KI3, KI5 bilaterally and at CV4, DU22 and Ying Tang as single needles. DeQi was achieved then needles were left unstimulated for 20 mins. Twice a week for 8 sessions, 20 minutes duration. Group III (n = 30): sham acupuncture. Points used as per acupuncture group but with non‐penetrating needles. Frequency as per acupuncture group. |
|
| Outcomes | Outcomes were collected at baseline and following 4 weeks of treatment Primary outcomes
Secondary outcomes
|
|
| Identification |
Sponsorship source: none reported Conflicts of interest: not reported |
|
| Notes | All participants were OAB dry Duration: 4 weeks Follow‐up: no Withdrawals/dropouts: 8 ITT analysis: no |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Although the paper says the participants were randomly assigned, there is no detail on how this was achieved. |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment in the study report. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | There was not uniform blinding of participants in the study. The medication arm was not blinded, whereas the acupuncture and sham acupuncture arms may or may not have been aware of the treatment they were receiving. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | There was no discussion in the paper regarding the blinding of assessors to participant group allocation when measuring outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Exclusions were reported (9% attrition rate) but the reasons were not discussed. Their data were omitted from the final analysis. |
| Selective reporting (reporting bias) | Unclear risk | All the outcomes stated as of interest are reported in the results but there is no detail around the tools used to assess quality of life and there is no description of the ICIQ SF‐T in terms of how the tool is scored and if it varies from the English version. |
| Other bias | Unclear risk | Baseline characteristics reported for the whole group and stated no significant difference between groups but no detail on how this conclusion was drawn. |
Chen 2009.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel‐group |
|
| Participants |
Country: China Setting: Second Affiliated Hospital of Heilongjiang University of Chinese Medicine Number of participants: 48 Sex: men Age range: 51 (26 to 76) Inclusion criteria: diagnosed with overactive bladder from urology and outpatient clinics, who have urinary urgency, urinary incontinence or frequency Exclusion criteria: endocrine and neurological diseases |
|
| Interventions |
Group I (n = 24): electro‐acupuncture. BL32, BL35, CV1, CV2. Sterile needles, vertical insertion, needles rotated until DeQi achieved then left in place with disperse‐dense wave (electronic stimulation) for 30 minutes. Once per day for 2 weeks. Group II (n = 48): medication; oral tolterodine 2 mg twice a day for 2 weeks |
|
| Outcomes | Total effective rate assessed at the end of treatment in all cases | |
| Identification |
Sponsorship source: no sources identified Conflicts of interest: no declared conflicts of interest |
|
| Notes |
Duration: 2 weeks Follow‐up: no Withdrawals/dropouts: none reported ITT analysis: no |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | There was no description of sequence generation except "randomly grouped". |
| Allocation concealment (selection bias) | Unclear risk | Only mentions "random" without concealment methods. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | There was no description of blinding of participants and personnel, but we infer that participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not mentioned in report. We were unable to assess if outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The number of participants recruited and the number whose outcomes were reported were the same. |
| Selective reporting (reporting bias) | Low risk | There is only one outcome and it is fully reported. |
| Other bias | Low risk | No other sources of bias detected. |
Engberg 2009.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel‐group |
|
| Participants |
Country: USA Setting: university Number of participants: 11 Sex: women Mean age (SD): 54.9 (8) years Mean years of formal education (SD): 16.1 (3.1) Inclusion criteria: women who had a least 2 episodes of incontinence and documented urge or mixed incontinence symptoms in their 7‐day bladder diary Exclusion criteria: post void residual of 200 mL or more; grade 2 pelvic organ prolapse; previous experience of acupuncture for any condition; unable or unwilling to complete a bladder diary; treatment with loop diuretics, corticosteroids or warfarin; pregnancy |
|
| Interventions |
Group I (n = 5): acupuncture. Points used: Bl 23, 31, 32, 33, Ki 3, Sp 6. DeQi achieved. 12 sessions over 6 weeks (twice per week). Group II (n = 6): sham acupuncture. Blunted needles with telescopic retraction, performed over acupuncture points as per treatment group. Needles were secured in place with a basal ring and double sided tape. 12 sessions over 6 weeks (twice per week). |
|
| Outcomes | Outcomes were measured at baseline, at 6 weeks when treatment was completed and at 4 weeks following cessation of treatment
|
|
| Identification |
Sponsorship source: Ruth Perkins Kuehn award Conflicts of interest: not reported |
|
| Notes |
Duration: 10 weeks Follow‐up: yes Withdrawals/dropouts: 2 ITT analysis: no OAB diagnosis: to be eligible for this study women had to report urge incontinence at least twice per week for more than 3 months thereby fulfilling the criteria for a diagnosis of OAB |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple computer‐generated randomisation used. |
| Allocation concealment (selection bias) | Unclear risk | No discussion of methods to prevent research staff from knowing or predicting the allocation to an intervention group. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | In this small population the blinding using sham needles appears to have been successful. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Text stated that investigators were blinded to intervention group. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reported dropouts and reasons why. |
| Selective reporting (reporting bias) | High risk | Multiple questionnaires used but not all reported. |
| Other bias | Low risk | No other sources of bias detected. |
Hong 2015.
| Study characteristics | ||
| Methods |
Study design: quasi‐RCT Study grouping: parallel‐group |
|
| Participants |
Country: China Setting: Handan People's Hospital Internal and Neurology Medicine Clinic Number of participants: 66 Sex: not reported Mean age (SD): 56.91 years (12.85) Course of disease (SD): 7.78 years (5.66) Inclusion criteria: meet the diagnostic criteria of mixed urinary incontinence; can co‐operate with relevant examinations and treatments; no contraindications for electro‐acupuncture treatment; sign informed consent and voluntarily participate in the research Exclusion criteria: participants who did not meet the diagnostic criteria of MUI; history of previous surgical treatment of urinary incontinence or pelvic floor surgery; symptomatic urinary tract infection; patients who were taking medicines affect the function of bladder; pregnancy or lactation; severe heart, brain, kidney and other system; mental illness; those who cannot co‐operate with treatment |
|
| Interventions |
Group I (n = 32): electro‐acupuncture. CV 3, CV4, SP 6, ST 36, LR 10. Sterile needles, vertical insertion to 2.5 to 4.0 cm depth in LR10, ST36, SP 6; oblique insertion 4 to 5 cm in CV3, CV 4. Needles rotated clockwise until DeQi achieved; electronic stimulation with 20 to 30 Hz in ST36, SP 6. Five times a week per week for 4 weeks, 30 mins each time. Group II (n = 33): medication; oral tolterodine 2 mg twice a day for 4 weeks plus bladder training |
|
| Outcomes | Outcomes were measured at baseline and after 4 weeks of treatment
|
|
| Identification |
Sponsorship source: Handan Science and Technology Research and Development Plan Project, No.: 1323108090‐3 Conflicts of interest: not reported |
|
| Notes |
Duration: 4 weeks Follow‐up: no Withdrawals/dropouts: 1 ITT analysis: no OAB diagnosis: participants had a diagnosis of OAB that conformed to the ICS definition |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "with random number table, randomly divided participants according to admission sequence." |
| Allocation concealment (selection bias) | High risk | There was no description of allocation concealment except "quasi‐random". |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding and the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding and the outcome measurement is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Clear reasons given for missing outcome data. |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it is clear that the published report included all expected outcomes. |
| Other bias | Low risk | No other sources of bias detected. |
Kelleher 1994.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel‐group |
|
| Participants |
Country: UK Setting: outpatient hospital clinics Number of participants: 39 Sex: women Mean age: 49.65 years Mean duration of symptoms: 5.05 years Inclusion criteria: irritative bladder symptoms; negative mid‐stream culture Exclusion criteria: known to have non‐neurogenic pathology likely to impair bladder compliance (e.g. previous radiotherapy or large fibroid uterus) |
|
| Interventions |
Group I (n = 20): acupuncture. Performed by an experienced acupuncturist, using 36 gauge, 3 cm long, disposable needles and a minimal stimulation technique i.e. the needles were merely flicked into the skin through an introducer. Fifteen needles were used at each visit and needles were left in situ a few mm below the skin without further stimulation for 10 minutes. The acupuncture points used were bilateral Spleen 6 (SP6), Stomach 36 (ST36), Conception Vessel 3 or 4 (CV3 or 4), Bladder 23 and 28 (BL23 & 28). Two further para‐vertebral, lumbar, segmental points and 4 sacral, segmental points were employed. These were specifically chosen for possible autonomic effect. 10 minutes per session, 6 sessions, once per week Group II (n = 19): medication; oxybutynin (Ditropan) at a dose of 5 mg. Twice a day for 6 weeks and once weekly visit to hospital department. |
|
| Outcomes | Applied at baseline and after 6 weeks of treatment
|
|
| Identification |
Sponsorship source: none specified Conflicts of interest: not reported |
|
| Notes |
Duration: 6 weeks Follow‐up: no Withdrawals/dropouts: 4 ITT analysis: no OAB diagnosis: this study refers to irritative bladder symptoms rather than OAB but describes these symptoms as including "urgency, urge incontinence, frequency and nocturia" thereby fulfilling the diagnosis of OAB required for inclusion in this review |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random number table used; method not detailed. |
| Allocation concealment (selection bias) | Unclear risk | No mention in paper of steps taken to prevent research staff from being able to predict the sequence of allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and research staff were not blinded to intervention group. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It appears that assessments were not carried out by the allocation or intervention staff but there is no explicit referral to blinding of the assessors. Unclear if "another doctor" (p.10) was aware of group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts and reasons for dropouts recorded. |
| Selective reporting (reporting bias) | Low risk | No evidence of non‐reporting but no published protocol pre‐study. |
| Other bias | Low risk | No other sources of bias detected |
Lin 2020.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel‐group |
|
| Participants |
Country: Hong Kong, China Setting: The Chinese University of Hong Kong Chinese Medicine Centre for Training and Research Number of participants: 100 Sex: men (n = 45) and women (n = 55) Mean age (SD): 68.45 (6.2) years Inclusion criteria: aged between 60 to 90 years old; diagnosed as OAB according to the diagnosis criteria of the ICS; physically and mentally able to complete the 3‐day voiding diary, Urinary Distress Inventory (UDI‐6) and Incontinence Impact Questionnaire (IIQ‐7); able to give written informed consent (by patients themselves or by their caretakers) Exclusion criteria: OAB symptom caused by stroke or spinal injury; life‐threatening infection; unconsciousness or severe cognitive deficits; dementia caused by Alzheimer’s disease or other neurodegenerative diseases; undergone incontinence surgery previously; taking short‐term active diuretic treatment or taking diuretic medication; had received acupuncture treatment for OAB within 2 months prior to the study; pregnancy; suffering from untreated urinary tract infection, urogenital tumours, prostate tumour, benign prostatic hyperplasia, chronic urinary retention |
|
| Interventions |
Group I (n = 51): acupuncture. Based on the traditional acupuncture theory, previous relevant studies, and opinion of acupuncture experts of the research team, the following acupuncture points were selected for treatment: BL32 (Ciliao, 次髎) (bilateral), BL23 (Shenshu, 腎俞) (bilateral), SP6 (Sanyinjiao, 三陰交) (bilateral), KI3 (Taixi, 太溪) (bilateral), BL39 (Weiyang, 委陽) (bilateral), BL28 (Pangguangshu, 膀胱俞) (bilateral) and CV4 (Guanyuan, 關元). 30‐minute acupuncture sessions, twice a week for 8 weeks. Group II (n = 49): sham acupuncture. Sham needles with retractable shafts were used on the same points described for the true acupuncture group. The needle tips were blunted to prevent skin penetration. Needles were secured to the skin using adhesive tape. 30‐minute acupuncture sessions, twice a week for 8 weeks. |
|
| Outcomes | Outcomes were applied at baseline, after 8 weeks of treatment and 3 months following completion of treatment
|
|
| Identification |
Funding source: supported by the Health and Medical Research Fund of the Food and Health Bureau, Hong Kong Special Administrative Region Government (Project no. 13141941) Conflicts of interest: the authors stated there were no conflicts of interest |
|
| Notes |
Duration: 20 weeks Follow‐up: 12 weeks after 8‐week intervention Withdrawals/dropouts: 4 ITT analysis: yes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Remote sequence generation; block randomisation by someone not involved in patient care. |
| Allocation concealment (selection bias) | Low risk | Allocation concealment safeguarded. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Measured using the Blinding Index and found to have attained effective blinding. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of the outcome assessors confirmed in study report. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All dropouts and reasons for dropouts were included. ITT analysis performed. |
| Selective reporting (reporting bias) | Low risk | Authors acknowledged in results the NGF measurements were not successfully extracted. NGF not reported in methods sections, but explanation for exclusion provided in results. |
| Other bias | Low risk | No other sources of bias detected. |
Liu 2019.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel‐group |
|
| Participants |
Country: China Setting: 10 sites Number of participants: 500 Sex: women Mean age (SD): 54.2 (9.75) years Mean disease duration: 3.85 (5.2) years Inclusion criteria: 35 to 75 years of age with mixed urinary incontinence for at least 3 months; positive cough stress test results; presented with moderate to severe symptoms according to the Urinary Incontinence Severity Index (3 points); a 72‐hour IEF (incontinence episode frequency) of at least 2 at baseline Exclusion criteria: pure stress, urgency or other types of urinary incontinence; pelvic organ prolapse of at least second degree; post‐void residual urinary volume greater than 30 mL; maximum urinary flow rate less than 20 mL/s; history of pelvic floor surgery |
|
| Interventions |
Group I (n = 249): electro‐acupuncture. Acupuncture procedures were performed by licensed acupuncturists with more than 2 years experience. Acupuncture points BL33 and BL35 on both sides were used in the electro‐acupuncture group. Needles were inserted at an angle of 30 to 45 degrees and a depth of 50 to 60 mm. All the needles were stimulated by manual rotation to reach DeQi sensation. The electrodes of the electric stimulator were placed on the needle handles of bilateral acupoints with a spare‐dense wave, 10/50 Hz, 0.1 to 5.0 mA. 30 minutes of electro‐acupuncture treatment 3 times a week for a total of 36 treatment sessions over a 12‐week period. Bladder health advice was to lose weight if body mass index was greater than 30 (calculated as the weight in kilograms divided by the height in metres squared), minimising daily fluid intake to 1.5 to 2 L, and reducing caffeine intake. Group II (n = 248): PFMT plus solifenacin. Physiotherapy‐led classes plus home DVD; 5 mg per day. Weekly classes during weeks 1 to 12, 4 weekly class during weeks 13 to 36. Participants were also encouraged to carry out a home exercise programme from weeks 1 to 36 and were given a DVD and exercise log to assist with the completion of the programme. Bladder health advice: lose weight if body mass index was greater than 30 (calculated as the weight in kilograms divided by the height in meters squared), minimising daily fluid intake to 1.5 to 2 L, and reducing caffeine intake. |
|
| Outcomes | Outcomes measured at baseline and after 12 weeks of intervention
|
|
| Identification |
Sponsorship source: this study was supported and funded by the programme of "the 12th Five‐year" National Science and Technology Pillar Program (2012BAI24B01; 2012BAI24B02) by the Ministry of Science and Technology of the People’sRepublic of China Conflicts of interest: authors declared there were no conflicts of interest |
|
| Notes |
Duration: 36 weeks Follow‐up: yes Withdrawals/dropouts: 33 ITT analysis: no OAB diagnosis: women included in this study had evidence of both OAB and stress incontinence symptoms and were classified as having mixed urinary incontinence |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomly allocated at a ratio of 1:1 to receive electro‐acupuncture or PFMT+Solifenacin via a central randomisation system. The randomisation schedule was stratified by enrolment site." |
| Allocation concealment (selection bias) | Low risk | Allocation performed by staff not involved in other study processes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Both groups were aware of the intervention they were receiving. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The outcome assessors, data manager, and statisticians were unaware of group allocation." Comment: independent assessor for outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "497 (249 in the electro‐acupuncture group and 248 in the PFMT+Solifenacin group) received at least 1 treatment session and were included in the full analysis set." Comment: detailed notes on reasons for missing data and how calculations had taken account of these. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcome measures were reported in the results section of the paper. |
| Other bias | Low risk | No other sources of bias detected. |
Shen 2020.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel‐group |
|
| Participants |
Country: China Setting: Department of Urology Number of participants: 45 Sex: women Mean age (SD): 39 years (9.9) Inclusion criteria: women diagnosed as OAB; aged between 18 and 60; have not used any Chinese or Western medicine in 1 week prior to commencing the study; signed informed consent Exclusion criteria: urinary system infections; urinary tract obstruction; urinary calculi; neurogenic bladder; urethral dysfunction; urinary retention; myasthenia gravis; ulcerative colitis; narrow‐angle glaucoma; mental disorders; allergic to tolterodine tablets; residual urine volume > 50 mL; those who are equipped with a pacemaker; allergic to metals; severely afraid of needles or fainting; pregnant or breastfeeding |
|
| Interventions |
Group I (n = 23): electro‐acupuncture. BaLiao (8 sacral foramina) and Sanyinjiao (SP6). The needles were 0.30 mm × 50 mm and 0. 30 mm × 75 mm. Density wave 50 Hz. Three times a week, 30 minutes each treatment for 4 weeks, 12 times in total. Group II (n =22): medication; tolterodine tablet 4 mg once per day for 4 weeks |
|
| Outcomes | Outcome measures were applied at baseline, after 2 weeks of treatment and after 4 weeks of treatment
|
|
| Identification |
Sponsorship: Basic Research Operating Funds of the Central Public Welfare Research Institutes, and Beijing Municipal Science and Technology Commission Conflicts of interest: the authors reported that there were no conflicts of interest |
|
| Notes |
Duration: 4 weeks Follow‐up: no Withdrawals/dropouts: no ITT analysis: no |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random allocation was used. |
| Allocation concealment (selection bias) | Unclear risk | The exact method that was used to protect allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Group allocation not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | There is no specific reporting of blinding outcome assessors. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The dropouts were low and comparable in the two groups. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias detected. |
Solberg 2016.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel‐group |
|
| Participants |
Country: Norway Setting: unclear Number of participants: 34 Sex: women Mean age: 66 Mean parity: 2 Inclusion criteria: 18 years of age; mixed urinary incontinence; not pregnant or planning to become pregnant during the study Exclusion criteria: women who had given birth within 12 months before the onset of the current study; women using medication for the incontinence; women who had undergone surgery for incontinence |
|
| Interventions |
Group I (n = 12): acupuncture. CV3, CV4, CV6, SP6, KI3, KI7 (PC6, LR3 and SP3 with related symptoms) were used with patients in a supine position, and BL 31–34, BL 23, BL 28, SP6, GV4 and GV20 (forward needling) (BL 14, 18 and 20 with symptoms) were used when the patient was in prone position. 30 minutes; 12 sessions over a 12‐week period at the convenience of the participant. Group II (n = 10): PFMT; 45 minutes (20 minutes general exercise); 12 weekly sessions with a physiotherapist Group III (n = 12): no intervention. The women randomised to this group received no treatment and were asked to fill in the questionnaires after 12 weeks. |
|
| Outcomes | Outcomes were applied at baseline and following 12 weeks of treatment
|
|
| Identification |
Sponsorship source: the Norwegian Acupuncture Association funded the open access fee Conflicts of interest: authors stated no conflicts of interest |
|
| Notes |
Duration: 12 weeks Follow‐up: no Withdrawals/dropouts: yes ‐ accounted for in text of article ITT analysis: no OAB diagnosis: women included in this study had evidence of both OAB and stress incontinence symptoms and were classified as having mixed urinary incontinence |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "All women meeting the inclusion criteria were randomly assigned to the treatment groups using the SurveyMonkey tool. Four women were not Internet users. They answered the questions by phone, and results were manually entered into SurveyMonkey by the first author (MS) before randomisation." Comment: an online tool was used to perform the allocation but this tool did not allow for stratification. The authors acknowledged that the baseline characteristics demonstrated that the women in the acupuncture group had a higher median symptom score than the other two groups. |
| Allocation concealment (selection bias) | Low risk | As an online remote system was used to perform the randomisation, the researcher involved in the allocation of participants was less likely to be able to influence this procedure. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not attempted due to obvious differences in interventions. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | There is no mention in the paper regarding blinding of outcome assessors. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Excluded dropouts from analysis. |
| Selective reporting (reporting bias) | Low risk | All stated outcomes were reported. |
| Other bias | Low risk | No other sources of bias detected. |
Wang 2011.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel‐group |
|
| Participants |
Country: China Setting: outpatients of Traditional Chinese Medicine Academy of Jilin Province Number of participants: 40 Sex: female Age range: 51 to 79 Inclusion criteria: diagnosed as OAB by western medicine diagnostic criteria (Clinical Guidelines for Overactive Bladder) or traditional Chinese medicine diagnostic criteria Exclusion criteria: not reported |
|
| Interventions |
Group I (n = 20): acupuncture. CV3, LR 28, LR23, CV6, CV4, SP6,BL32, CV20. Sterile needles, vertical insertion with reinforcing method. Once per day for 4 weeks, 20 mins each time. Group II (n = 20): medication; oral tolterodine, 2 mg twice a day for 4 weeks |
|
| Outcomes |
|
|
| Identification |
Sponsorship source: no sources identified Conflicts of interest: this was not mentioned in the study report |
|
| Notes |
Duration: 4 weeks Follow‐up: no Withdrawals/dropouts: none reported ITT analysis: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | There was no description of sequence generation except "randomly grouped". |
| Allocation concealment (selection bias) | Unclear risk | There was no description of allocation concealment except "randomly grouped". |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | There was no description of blinding of participants and personnel but due to the nature of the interventions we infer that participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding and the outcome measurement is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The outcome data were complete. |
| Selective reporting (reporting bias) | Low risk | Outcomes were completely reported, including adverse reactions and follow‐up. |
| Other bias | Low risk | No other sources of bias were detected. |
Wang 2013a.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel‐group |
|
| Participants |
Country: China Setting: university hospital ‐ urology department Number of participants: 60 Sex: women Age range: 35 to 60 years Inclusion criteria: clinical diagnosis of overactive bladder; symptoms for more than 6 months; no other treatment or drugs that affect urination have been used within 2 weeks Exclusion criteria: average urine output > 200 mL; frequency of urination < 8 times at day and < 2 times at night; patients with bladder outlet obstruction or stress urinary incontinence; use of anticholinergic drugs; presence of other urological symptoms ‐ neurogenic bladder; acute and chronic urinary tract infections, tumours, kidney stones |
|
| Interventions |
Group I (n = 30): acupuncture. Sterile needles. Participant treated in the supine and prone position, vertical insertion on CV3, CV4, ST28, LR 10, SP 9 with light stimulation and reinforcing method; intensive stimulation for 1 minute with reducing method on BL29, LR28, BL32, CV3. 30 minutes each time and manipulations were implemented every 10 minutes. Once per day for 4 weeks. Group II (n = 30): medication; oral solifenacin 5 mg once a day for 4 weeks |
|
| Outcomes | Outcomes were measured at baseline and after 4 weeks of treatment
|
|
| Identification |
Sponsorship source: Scientific and Technological Research Project of Traditional Chinese Medicine and Ethnic Medicine of Guizhou Provincial Administration of Traditional Chinese Medicine (No. QZYY2011) Conflicts of interest: there was no mention of this in the study report |
|
| Notes |
Duration: 4 weeks Follow‐up: no Withdrawals/dropouts: none ITT analysis: no |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "the female patients (=60) with OAB divided into acupuncture group and Solifenacin group were randomly grouped" Comment: there was no description of sequence generation except "randomly grouped". |
| Allocation concealment (selection bias) | Unclear risk | There was no description of allocation concealment except "randomly grouped". |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | There was no description of blinding of participants and personnel and we infer that participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | There was no description of blinding of outcome assessors. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The outcome data were complete. |
| Selective reporting (reporting bias) | Low risk | All the outcomes mentioned were reported in the study. |
| Other bias | Low risk | No other sources of bias detected. |
Yang 2016.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel‐group |
|
| Participants |
Country: China Setting: university hospital ‐ urology department Number of participants: 33 Sex: men and women ‐ numbers of each not reported Mean age (SD): 57.5 (16.3) years Inclusion criteria: aged 18 to 75 years old; meet the diagnostic criteria for bladder hyperactivity; urination frequency (average daily urination times ≥ 8 times); no drug treatment related to this research was performed within 2 weeks before participating in the research, and no acupuncture treatment within 1 month before the research, or participating in other clinical research; disease course of the patients who participated in this study is at least 3 months; volunteer to participate in this study, and be able to ensure that they co‐operate with the treatment arrangement and complete the urination journal Exclusion criteria: frequent and urgent urination symptoms caused by other diseases; patients with a history of botulinum bladder or pelvic muscle treatment in the past year; patients with urinary tract infection or vaginal infection; patients currently undergoing treatment with implantable pelvic stimulators; patients who are currently applying electrical stimulation to the pelvic area, back and leg areas; patients who have a history of treatment with the ingenious device of this research and related drugs of this research within the past 4 weeks; patients who are participating in clinical research related to gynaecology, urinary system or renal function; patients with blood coagulation dysfunction or taking anticoagulants, or patients with severe liver, liver or kidney damage, or patients whose general condition is poor and unable to co‐operate; those who have a pacemaker; severely afraid of needles, dizziness or metal allergy; patients during pregnancy or lactation |
|
| Interventions |
Group I (n = 12): electro‐acupuncture. Bladder 33, Bladder 35. Sterile needles with diameter of 0.3 mm and length of 9 cm. Participant treated in the prone position, skin prepared with 75% alcohol pads, oblique insertion to 6 cm depth. Needles rotated clockwise until DeQi achieved then left in place with 10 HZ, 5 mA electronic stimulation for 30 minutes. Three times a week for 8 weeks, 30 minutes each time. Group II (n = 13): sham acupuncture. Bladder 33, Bladder 35. Sterile blunt needles with diameter of 0.3 mm and length of 4.5 cm. Participant treated in the prone position. Stick acupuncture fixed pad on acupoints and then acupressure it with blunt needle then add electronic stimulation with 10 HZ, 5 mA. Three times a week for 8 weeks, 30 minutes each time. Group III (n = 8): medication; oral solifenacin, 5 mg once a day for 8 weeks |
|
| Outcomes | Outcomes measured at baseline, after 4 weeks of treatment and after 8 weeks of treatment
|
|
| Identification |
Sponsorship source: no sources of funding were reported Conflicts of interest: this was not mentioned in the study report |
|
| Notes |
Duration: 8 weeks Follow‐up: no Withdrawals/dropouts: yes ITT analysis: not reported OAB diagnosis: the authors of this study refer to bladder hyperactivity rather than OAB. However, the criteria for a diagnosis of OAB, namely urgency, frequency of micturition, nocturia and urge incontinence were highlighted in the outcome measures collected (bladder diary data) so the review team felt this study did meet the criteria stated in the protocol for inclusion in the review. This study is only available in Chinese and it was felt that the difference in terms used may be a translational effect. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Centralised computer randomisation is suggested in the text but not clearly specified. |
| Allocation concealment (selection bias) | Unclear risk | Central allocation mentioned in text but not clearly defined. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of how blinding was conducted but as a sham group was employed blinding is inferred. However, a medication arm was also employed, which would un‐blind this group. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The text was not clear regarding blinding of outcome assessors. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Small number of dropouts and reasons reported. |
| Selective reporting (reporting bias) | Low risk | All the outcomes were reported, including adverse reactions. |
| Other bias | Low risk | No other sources of bias detected. |
Yu 2012.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel‐group |
|
| Participants |
Country: China Setting: Traditional Chinese Medicine Hospital Number of participants: 44 Median age: 35.2 Sex: men and women ‐ the number of each was not reported Inclusion criteria: patients diagnosed as having OAB using the Chinese Guidelines of Diagnosis and Treatment in Urological Diseases Exclusion criteria: none stated |
|
| Interventions |
Group I (n = 24): acupuncture. Needles placed at BL23, BL28 and ST 36 bilaterally. Twice per day for 2 weeks. Bladder training: delaying urination, gradually increasing urine volume voided to over 300 mL, urination at regular times and pelvic floor exercises Group II (n = 20): medication; oral tolterodine 2 mg twice per day. Bladder training: delaying urination, gradually increasing urine volume voided to over 300 mL, urination at regular times and pelvic floor exercises |
|
| Outcomes | Outcome assessed following 2 weeks of treatment Treatment effect (participant opinion with guiding criteria) |
|
| Identification |
Sponsorship source: none given Conflicts of interest: this was not documented in the study report |
|
| Notes |
Duration: 2 weeks Follow‐up: no Withdrawals/dropouts: none reported ITT analysis: no |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not reported. |
| Allocation concealment (selection bias) | Unclear risk | Method not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No discussion regarding blinding of participants or assessors. Due to the nature of the two interventions it is not possible to blind participants to their group allocation using the methodology employed in this study. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding of outcomes assessors not documented in the study report. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No CONSORT diagram to track recruitment, intervention and dropouts. |
| Selective reporting (reporting bias) | Low risk | Outcomes stated were fully reported. |
| Other bias | Low risk | No other sources of bias detected. |
Yuan 2015.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel‐group |
|
| Participants |
Country: China Setting: university hospital ‐ urology department Number of participants: 240 Sex: women Mean age (SD): 57.85 (11.8) years Inclusion criteria: aged over 18; urinary urgency and nocturia with or without urgency incontinence or frequency for at least 6 months Exclusion criteria: urinary tract infections; interstitial cystitis; polyuria; bladder tumour; underlying neurologic abnormalities (e.g. neuropathic bladder); taking medications for OAB or receiving acupuncture for any condition; pregnant or recently gave birth (i.e. within 6 months preceding referral); previous prolapse or incontinence surgery; not beginning sexual activities (due to ethics problems) |
|
| Interventions |
Group I (n = 118): acupuncture. Sp6, Sp9, Ki 3 and CV4. Sterile needles 35 mm x 50 mm. The participant was treated in the supine position, skin prepared with 75% alcohol pads, vertical insertion to 1 to 1.5 cm depth. Needles rotated clockwise until DeQi achieved then left in place without further stimulation for 20 minutes. Once per week for 4 weeks. Group II (n = 122): medication; oral tolterodine 2 mg twice a day for 4 weeks |
|
| Outcomes | Outcomes were applied at baseline and after 4 weeks of treatment
|
|
| Identification |
Sponsorship source: no sources identified Conflicts of interest: no declared conflicts of interest |
|
| Notes |
Duration: 4 weeks Follow‐up: no Withdrawals/dropouts: yes ‐ reasons for missing data reported ITT analysis: no Contacted authors on 8 April 2020 regarding clarification on methodology ‐ no reply received OAB diagnosis: a clear definition of OAB fitting the ICS definition was given in this study |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computer generated list of random numbers was used, and the allocation sequence was concealed in sequentially numbered, sealed and opaque envelopes by a doctor who did not participate in group assignment, data collection or statistical analysis." Comment: does not mention if the randomisation was simple or block but otherwise there is no evidence that the nurses performing the allocation could predict the sequence of allocation. |
| Allocation concealment (selection bias) | Low risk | Quote: "The registered nurses on duty in the urological wards, outpatient clinic randomly assigned the enrolled patients to the weekly acupuncture treatment group (intervention) or the twice daily 2 mg Tolteradine treatment group at admission or first referral, using a concealed allocation sequence. A computer‐generated list of random numbers was used, and the allocation sequence was concealed in sequentially numbered, sealed and opaque envelopes by a doctor who did not participate in group assignment, data collection or statistical analysis. Envelopes were opened sequentially only after participant details had been written on the envelope." Comment: the allocation was performed by an independent person who was otherwise not involved in the trial and so unable to influence the allocation process. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Blinding of the group assignment for the nurses and patients was not possible, but in this study, the data collection, processing and analysis were conducted by other doctors who did not participate in group assignment. What is more, the doctors who made the diagnosis of OAB and recruited the subjects did not also participate in group assignment, patients’ treatments, and data analysis." Comment: participants aware of allocation, therefore risk of bias is high. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "the data collection, processing and analysis were conducted by other doctors who did not participate in group assignment. What is more, the doctors who made the diagnosis of OAB and recruited the subjects did not also participate in group assignment, patients’ treatments, and data analysis." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Ten women in the intervention group were lost of follow‐up and did not complete the study because of personal reasons, such as difficulty in scheduling the treatment sessions around their work schedules. Two women discontinued intervention because of unsuccessful treatment or no significant symptom relief and switched to drug therapy. While in the control group six women were lost to follow‐up because of personal reasons, and six discontinued treatment because of unsuccessful treat‐ ment, no significant symptom relief or moderate to severe dry mouth, three of which switched to bladder training and acupuncture treatment." Comment: Table 4 gives number for each group, which is equal to baseline. However, nothing in the text states whether dropouts were included in the final analysis. |
| Selective reporting (reporting bias) | High risk | Adverse events mentioned in the text but no data reported to support this. |
| Other bias | Low risk | No other sources of bias detected. |
Zhang 2015.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel‐group |
|
| Participants |
Country: China Setting: Ninth People’s Hospital of Chongqing Number of participants: 45 Sex: women Mean age (SD): 41.25 (9.3) Inclusion criteria: women aged 18 to 65 years; diagnosis of OAB according to the definition set out by the International Continence Society in 2002; score for urinary urgency of ≥ 2 points and total overactive bladder symptom score (OABSS) of ≥ 3 points; symptoms persisting for > 6 months; previous treatment with a first line anticholinergic drug (e.g. tolterodine, solifenacin) for 3 months that was unsuccessful; volunteered to join the study and gave signed informed consent Exclusion criteria: neurogenic bladder dysfunction; lower urinary tract symptoms due to urinary tract infection, urinary stone or interstitial cystitis; active sexually transmitted diseases (e.g. syphilis, gonorrhoea); serious medical condition such as congestive heart failure, arrhythmia with or without cardiac pacemaker, chronic pulmonary obstructive disease and hepatic failure; previous acupuncture treatment within the past 6 months; skin infection or fear of needles |
|
| Interventions |
Group I (n = 23): electro‐acupuncture. Electro‐acupuncture (EA) was performed using 6 disposable stainless steel needles (0.3 mm diameter, 75 mm length) inserted into the bilateral Bladder (BL) 32 (Ciliao), BL33 (Zhongliao) and BL34 (Xialiao) points, as standardised by the World Health Organization. The needles were inserted into points in the medial direction at an angle of 60° horizontal and 30° sagittal with a sufficient depth (about 50 mm) to reach the sacral periosteum and a DeQi sensation was obtained, defined as a heavy and numb sensation around the point after the needle is inserted. Electrodes of the electric stimulator (Huatuo brand SDZ‐II; Electro‐Acu Stimulators, Suzhou Medical Supply & Equipment, Jiangsu,China) were then attached to the handle of the needles bilaterally. The electrode pairs were connected across the spine at each pair of the same points, positive electrodes were attached on the left and negative electrodes on the right. Disperse‐dense waves, 4 Hz and 20 Hz electric current were used in the study. The intensity of the electric current was increased to the patient’s maximum tolerance and then slightly reduced to an acceptable level. 30 sessions, 5 per week for 6 weeks, each lasting 30 minutes. Group II (n = 22): sham electro‐acupuncture. The sham electro‐acupuncture (SEA) protocol included the same number and type of needles, duration and frequency of sessions as for the EA treatment, but the treatment was delivered superficially at non‐points 15 mm lateral to each corresponding points. The patients experienced a pricking sensation instead of DeQi. The points were not stimulated electrically, but the sound of the pulse generator was heard by the participants. 30 sessions, 5 per week for 6 weeks, each lasting 30 minutes. |
|
| Outcomes | Outcomes applied at baseline and after 6 weeks
|
|
| Identification |
Sponsorship source: none recorded Conflicts of interest: authors stated there were no conflicts of interests |
|
| Notes |
Duration: 6 weeks Follow‐up: no Withdrawals/dropouts: yes ITT analysis: no |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "After enrolment the 50 women were randomised 1:1 to the EA group or the sham EA (SEA) group using a computer‐generated random block design." Comment: online randomisation tool. |
| Allocation concealment (selection bias) | Unclear risk | Text infers that those involved with allocation were separate to these delivering intervention and different from those carrying out outcome assessments. However, there is no direct report of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "After enrolment the 50 women were randomised 1:1to the EA group or the sham EA (SEA) group using a computer‐generated random block design. Participants did not know to which group they were assigned. The study was single‐blind; acupuncturists could not be blinded to the treatment assignment, but were excluded from examining and enrolling patients and from all outcome assessments" Comment: we assigned unclear risk as acupuncturists could not be blinded but this was explicitly stated in the design and these research staff did not participate in other study processes. It is unclear if the lack of blinding resulted in the two groups being treated differently. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "The study was single‐blind; acupuncturists could not be blinded to the treatment assignment, but were excluded from examining and enrolling patients and from all outcome assessments" Comment: text infers that those involved in delivering the intervention were different from those assessing outcomes but does not state that the outcome assessors were blinded to intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts explained, were small in number and were equal between the groups. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported were consistent throughout the paper. |
| Other bias | Low risk | No other sources of bias detected. |
BL 14, 18, 20: bladder 14, 18, 20 acupuncture points
BL 23, 28, 31, 32, 33, 34: bladder acupuncture points
ICIQ‐SF: International Consultation on Incontinence Questionnaire ‐ Short Form
CV3: conception vessel 3 acupuncture point
CV 4: conception vessel acupuncture point
CV 6: conception vessel 6 acupuncture point
DeQi: sensation of aching, tingling, heaviness experienced during an acupuncture treatment
DU 22: cranial acupuncture point
GV 4: governor vessel 4 acupuncture point
GV 20: governor vessel 20 acupuncture point
ICIF‐SF: International Consultation on Incontinence ‐ Short Form
ICIQ‐SF‐T: International Consultation on Incontinence ‐ Short Form (Turkish)
ICS: International Continence Society
IEF: incontinence episode frequency
IIQ: Incontinence Impact Questionnaire
ITT analysis: intention‐to‐treat analysis
KHQ: King's Health Questionnaire
KI 3: kidney 3 acupuncture point
KI 5: kidney 5 acupuncture point
KI 17: kidney 17 acupuncture point
LI 4: large intestine 4 acupuncture point
LIV 3: liver 3 acupuncture point
LR 4: liver 4 acupuncture point
MUI: mixed urinary incontinence
NGF: nerve growth factor
OAB: overactive bladder
OABSS: Overactive Bladder Symptom Score
PC 6: pericardium 6 acupuncture point
PFMT: pelvic floor muscle training
RCT: randomised controlled trial
SD: standard deviation
SF‐36: Short‐Form 36
SP 3: spleen 3 acupuncture point
SP 6: spleen 6 acupuncture point
SP 9: spleen 9 acupuncture point
ST 36: stomach 36 acupuncture point
UDI: Urogenital Distress Inventory
VAS: visual analogue scale
Ying Tang: facial acupuncture point
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Anhari 2011 | Study design does not meet review criteria |
| Cai 2017 | Study design does not meet review criteria |
| Carmona 2013 | Intervention does not meet review criteria |
| Chen 2003 | Study design does not meet review criteria |
| Chen 2005a | Intervention does not meet review criteria |
| Chen 2005b | Patient population does not have a diagnosis of OAB |
| Chen 2012 | Study design does not meet review criteria |
| Chen 2015a | Patient population does not have a diagnosis of OAB |
| Chen 2015b | Intervention does not meet review criteria |
| Chen 2015c | Study design does not meet review criteria |
| Cheung 2018 | Intervention does meet review criteria |
| Dunning 2017 | Patient population does not have a diagnosis of OAB |
| Ellis 1990 | Study design does not meet review criteria |
| Emmons 2005 | Comparator does not meet review criteria |
| Enberg 2006 | Patient population does not have a diagnosis of OAB |
| Feng 2011 | Study design does not meet review criteria |
| Feng 2014 | Study design does not meet review criteria |
| Guo 2016 | Intervention does not meet review criteria |
| He 2016 | Patient population does not have a diagnosis of OAB |
| He 2018 | Comparator does not meet review criteria |
| Hong 1996 | Study design does not meet review criteria |
| Hu 2005 | Study design does not meet review criteria |
| Hu 2015 | Study design does not meet review criteria |
| Hu 2016 | Intervention does not meet review criteria |
| Jiao 2019 | Patient population does not have a diagnosis of OAB |
| Johnstone 2003 | Patient population does not have a diagnosis of OAB |
| Kim 2008 | Patient population does not have a diagnosis of OAB |
| Kubista 1976 | Patient population does not have a diagnosis of OAB |
| Kwon 2014 | Intervention does not meet review criteria |
| Lee 2016 | Intervention does not meet review criteria |
| Liao 2007 | Patient population does not have a diagnosis of OAB |
| Liao X 2007 | Intervention does not meet review criteria |
| Lillie 2014 | Not a research paper: letter to the journal editor |
| Liu 1998 | Patient population does not have a diagnosis of OAB |
| Liu 2010 | Study design does not meet review criteria |
| Liu 2013 | Patient population does not have a diagnosis of OAB |
| Liu 2015a | Patient population does not have a diagnosis of OAB |
| Liu 2015b | Study design does not meet review criteria |
| Liu 2016 | Patient population does not have a diagnosis of OAB |
| Liu 2017 | Patient population does not have a diagnosis of OAB |
| Lu 2002 | Patient population does not have a diagnosis of OAB |
| Mao 2012 | Intervention does not meet review criteria |
| Miao 2015 | Study design does not meet review criteria |
| Nam 2017 | Comparator does not meet review criteria |
| Pang 2018 | Comparator does not meet review criteria |
| Penson 2018 | Patient population does not have a diagnosis of OAB |
| Philp 1988 | Study design does not meet review criteria |
| Qu 2013 | Study design does not meet review criteria |
| Ren 2020 | Intervention does not meet review criteria |
| Rong 2015 | Study design does not meet review criteria |
| Ruan 2018 | Patient population does not have a diagnosis of OAB |
| Shen 2012a | Patient population does not have a diagnosis of OAB |
| Shen 2012b | Patient population does not have a diagnosis of OAB |
| Su 2013 | Patient population does not have a diagnosis of OAB |
| Su 2020a | Study design does not meet review criteria |
| Su 2020b | Study design does not meet review criteria |
| Suen 2015 | Patient population does not have a diagnosis of OAB |
| Tang 2016 | Patient population does not have a diagnosis of OAB |
| Wan 2019 | Intervention does not meet review criteria |
| Wang 2008 | Comparator does not meet review criteria |
| Wang 2013b | Study design does not meet review criteria |
| Wang 2015 | Patient population does not have a diagnosis of OAB |
| Wang 2016 | Patient population does not have a diagnosis of OAB |
| Wang 2017a | Not a research paper: letter to the journal editor |
| Wang 2017b | Intervention does meet review criteria |
| Wang 2019 | Patient population does not have a diagnosis of OAB |
| Xie 2020 | Intervention does not meet review criteria |
| Xiong 2020 | Study design does not meet review criteria |
| Xu 2010 | Patient population does not have a diagnosis of OAB |
| Xu 2016 | Patient population does not have a diagnosis of OAB |
| Yang 2020 | Study design does not meet review criteria |
| Zhang 1999 | Study design does not meet review criteria |
| Zhang 2012 | Study design does not meet review criteria |
| Zhao 2012 | Study design does not meet review criteria |
| Zhao 2013 | Patient population does not have a diagnosis of OAB |
| Zhao 2013a | Intervention does not meet review criteria |
| Zhao 2016 | Patient population does not have a diagnosis of OAB |
| Zheng 1990 | Study design does not meet review criteria |
| Zheng 1992 | Patient population does not have a diagnosis of OAB |
| Zheng 2015 | Patient population does not have a diagnosis of OAB |
| Zhishun 2002 | Patient population does not have a diagnosis of OAB |
| Zhong 2016 | Study design does not meet review criteria |
| Zhu 2018 | Study design does not meet review criteria |
| Zhu 2021 | Patient population does not have a diagnosis of OAB |
OAB: overactive bladder
Characteristics of studies awaiting classification [ordered by study ID]
Bulut 2014.
| Methods | 2‐group comparative method but it is unclear from the abstract if the participants were randomly allocated |
| Participants | 20 women diagnosed with OAB |
| Interventions | Group A: 10 sessions of electro‐acupuncture n = 10; no details were given on the acupuncture points used or the treatment regime Group B: 2 mg tolterodine twice daily orally for 3 months n = 10 |
| Outcomes | Urodynamic parameters Authors reported that both groups demonstrated significant improvement but there was no statistically significant difference between groups |
| Notes | These details were taken from a conference abstract. We have been unable to contact the research team or source a full‐text version of the report. |
Han 2011.
| Methods | RCT |
| Participants | 48 male outpatients diagnosed with overactive bladder |
| Interventions | Electro‐acupuncture group: electro‐acupuncture with acupoints Huyang (BL 35), Ciliao (BL 32), Qugu (CV 2), Huiyin (CV 1). Needles were retained for 30 minutes, once a day, for 14 days. Control group: tolterodine tartrate tablets 2 mg taken orally, 2 mg, twice a day, for 14 days |
| Outcomes | Electro‐acupuncture group: 62.5% patients were cured and 87.5% patients showed effective Control group: 54.2% patients were cured and 79.2% patients showed effective There was significant difference between the two groups (P < 0.01) |
| Notes | This information was taken from an abstract published only in Chinese. The Chinese speaking review authors were unable to locate the full paper this information relates to. |
OAB: overactive bladder; RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
Huang 2020.
| Study name | Randomized controlled trial for the efficacy of electroacupuncture in the treatment of urge urinary incontinence: a clinical study protocol |
| Methods | Study design: RCT |
| Participants | 100 men and women (as stated in the published protocol) Inclusion criteria: diagnosed with urge urinary incontinence by a urologist; 18 to 75 years; frequent urination, urgency and urinary incontinence; no drug treatment during the study and no acupuncture treatment within 1 month prior to the study; not participating in other clinical studies within 2 weeks prior to this study; course of disease at least 3 months; patient’s vital signs are stable, and is conscious enough to be examined and treated; signed an informed consent form to volunteer in the study Exclusion criteria: history of botulinum toxin injection of the bladder or pelvic muscles in the past year; urinary tract infections or vaginal infections during the study period; undergoing implantable pelvic stimulator therapy during the study period; electrostimulation applied to patients in the pelvic region, back and leg areas during the study period; use of drugs that can influence the outcomes before or during the study; participating in other clinical research related to gynaecology, urinary system or kidney function; coagulopathy or taking anticoagulants; severe heart, liver or kidney damage; pregnancy or lactation; patients who are generally in poor condition and are unable to co‐operate; pacemaker; severely afraid of needles; prone to fainting; metal allergy |
| Interventions |
Group I: electro‐acupuncture. Using points Bladder 32, 33 and 35. Acupuncture points are continuously stimulated with 100 Hz wave and a 1 to 5 mA electric current for 30 minutes. Participants will receive treatment 3 times per week for 8 weeks, a total of 24 treatments. Follow‐up continues for 24 weeks. Group II: sham electro‐acupuncture. Using non‐acupuncture points located 20 mm lateral to Bladder 32, 33 and 35. Electrical stimulation will be attached but no power will be applied. The participants are told that an effective slight current input will be applied that may not result in a sensation of stimulation. Participants will receive treatment 3 times per week for 8 weeks, a total of 24 treatments. Follow‐up continues for 24 weeks. |
| Outcomes |
Primary: measured at baseline, 4 weeks (during treatment), 8 weeks (after treatment), 24 weeks (1st follow‐up visit) and 32 weeks (2nd follow‐up visit)
Secondary: measured at baseline, 8 weeks (treatment completion) and 32 weeks (2nd follow‐up visit)
|
| Starting date | January 2020 |
| Contact information | Qian Mo e‐mail: 1404326639@qq.com |
| Notes | Study lead contacted by email on 12 August 2021 regarding study progress OAB diagnosis: the ICS definition of OAB includes urge urinary incontinence. A diagnosis of OAB requires the person to have one or more of the following: urgency, frequency, urge urinary incontinence and nocturia. This study focuses on the incontinence element of OAB but sufferers would be compliant with the definition set out by the ICS. |
Jia 2015.
| Study name | The effectiveness, superiority and safety of electro‐acupuncture on overactive bladder: multi‐centre RCT |
| Methods | Study design: RCT |
| Participants | 180 participant, 60 in each arm Inclusion criteria: aged 18 to 75; men or women; clinical diagnosis of overactive bladder; more than 8 voids per day; no relevant drug use within 2 weeks and no acupuncture treatment within 1 month before enrolling in the study; symptoms for longer than 3 months; capable of giving informed consent; willing to follow study procedures Exclusion criteria: OAB symptoms secondary to other diseases; stress incontinence; urinary tract infections or vaginal infections; implanted pelvic stimulator; current use of electric therapy on pelvic/back/legs; current use of botox on vesical or pelvic muscles; undergoing clinical investigation of gynaecological, urological or renal systems; other severe diseases impacting cognition and ability to participate; pregnant or breastfeeding women; coagulation disorders or taking anti‐coagulation drugs; cardiac pace maker; metal allergy; needle phobia; electro‐acupuncture or taking solifenacin within 4 weeks of commencing the study |
| Interventions |
Group I: electro‐acupuncture. Using Bladder 33 point bilaterally ‐ 75 mm needles at a depth of 50 mm to 60 mm with 60 degree angle. Electrical stimulation applied for 30 mins x 3 per week for 8 weeks, 24 treatments in total. Group II: sham electro‐acupuncture. Blunt needles are inserted into an adhesive pad but do not pierce the skin at the Bladder 33 point ‐ the needles are lifted, thrust and twirled to simulate insertion. The electrical stimulation unit has been modified to appear to deliver current but no current is passed into the participants' tissues. The treatment regime was the same as the active EA regime. Group III: medication; 5 mg solifenacin tablets once per day 30 minutes before eating for 8 weeks |
| Outcomes |
Primary outcome
Secondary outcomes
|
| Starting date | October 2014 |
| Contact information | Jia Baohui |
| Notes | Registration last updated 25 May 2015 |
Pang 2021.
| Study name | Acupuncture for overactive bladder in adults |
| Methods | RCT |
| Participants | 110 men and women Inclusion criteria:
Exclusion criteria:
|
| Interventions | Group A Participants will receive acupuncture, 3 times per week for 8 weeks. The selected acupoints include bilateral BL33, BL35, SP6 and ST36. All acupoint areas have been sterilised before acupuncture. For BL33, a needle (Ф0.40 × 100 mm) will be inserted with an angle of 60° in an inferomedial direction at a depth of 90 mm to 100 mm. For BL35, the same needle will be inserted with a direction to the ischial rectal fossa at a depth of 60 mm to 70 mm deep. For SP6 and ST36, needles (Ф0.30 × 50mm) will be directly inserted at a depth of 25 mm to 30 mm deep. After the needles are inserted, a portable electro‐acupuncture machine will be connected to the handles of needles located in BL33 and BL35 to provide the electrical stimulation for 30 minutes with a disperse‐dense wave (4/20 Hz). All current intensities will be as high as can be tolerated. Group B The sham acupoints will be located at 20 mm outward to BL33, BL35, SP6 and ST36, and the needless will be inserted with a depth of 2 mm. BL33 and BL35 will not receive any electrical stimulation, though the handles of the needles will be connected to the same machine as the acupuncture group, and the parameter setting and course are also the same. |
| Outcomes |
Primary outcome
Secondary outcomes
|
| Starting date | Last update 2 March 2022 ‐ status "Not yet recruiting" |
| Contact information | Lead author email address pangran2002@sina.com |
| Notes | — |
Shen 2019.
| Study name | A randomised controlled trial for the efficacy and safety of electro‐acupuncture in the treatment of female overactive bladder |
| Methods | Study design: RCT |
| Participants | 68 female participants Inclusion criteria: compliance with diagnostic criteria; women aged between 18 and 60; Chinese or western medicines for OAB have not been used for 1 month prior to entry into study; give informed written consent Exclusion criteria: UTI or lower urinary tract construction; neurogenic bladder; urethral dysfunction; post void residual of more than 50 mL; myasthenia gravis; ulcerative colitis; glaucoma; allergies or contra‐indications to tolterodine; unable to comply with study procedures (judged by research staff); pregnancy or breastfeeding; pacemaker; metal allergy; severe needle phobia; non‐compliance with study procedures leading to incomplete data |
| Interventions |
Group I (n = 34): electro‐acupuncture. No further details available. Group II (n = 34): medicine. No further details available. |
| Outcomes |
|
| Starting date | 1 May 2019 |
| Contact information | Jianwu Shen |
| Notes | Study lead contacted 12 August 2021 for progress update |
Sheyn 2017.
| Study name | Comparison of electro‐acupuncture to mirabegron on symptoms of overactive bladder in women who have failed anti‐cholinergic therapy |
| Methods | Study design: RCT |
| Participants | 80 females Inclusion criteria: 18 years and older; female; informed written consent; documented symptoms of OAB for more than 6 months; have failed at least one anti‐cholinergic medication defined as no change or unsatisfactory improvement in symptom severity after 6 weeks of a daily regimen Exclusion criteria: under 18 years; unable or willing to provide informed consent; illiterate; non‐English speaking or reading; current UTI; history of interstitial cystitis; bleeding disorder; currently taking anti‐coagulation medication; are currently or have in the past taken mirabegron; currently having acupuncture for another condition; currently undergoing pelvic floor training; receiving treatment for a gynaecological or urological cancer; pregnancy; implanted pacemaker; poorly or uncontrolled hypertension |
| Interventions |
Group I: electro‐acupuncture; 30 minutes once per week for 6 weeks Group II: medication; 50 mg mirabegron once daily for 6 weeks |
| Outcomes | All outcomes assessed 3 weeks after initiating treatment, 6 weeks after therapy initiation and monthly intervals for 3 months from therapy initiation for the acupuncture group
|
| Starting date | 1 July 2017 |
| Contact information | David Sheyn |
| Notes | Registration last updated 27 March 2017 |
Wen 2020.
| Study name | Efficacy evaluation for electro‐acupuncture in the treatment of neurogenic urinary retention and overactive bladder |
| Methods | Study design: RCT |
| Participants | 420 men and women; 140 in each arm Inclusion criteria: symptoms of OAB that meet ICS and AUA criteria; aged 18 to 75; symptoms for more than 3 months; overactive bladder symptom score (OABSS) of more than 6; give informed written consent to participate Exclusion criteria: OAB symptoms secondary to another disease; mixed incontinence; presence of UTI; pelvic organ prolapse of grade 2 or more; post void residual of more than 100 mL; metal allergy; fear of acupuncture; solifenacin is contraindicated; uncontrolled diabetes; severe heart, liver or kidney disease; mental illness; coagulation dysfunction; pacemaker; pregnancy or breastfeeding; taking medication for OAB or having acupuncture within 1 month of commencing the trial; participating in any other trial |
| Interventions |
Group I: electro‐acupuncture; performed 3 times per week for the first 4 weeks and twice a week for the following 8 weeks ‐ 28 treatments in total Group II: weak electro‐acupuncture; performed 3 times per week for the first 4 weeks and twice a week for the following 8 weeks ‐ 28 treatment in total Group III: drug treatment; solifenacin 5 mg once per day for 32 weeks |
| Outcomes | All measures applied at the end of weeks 4, 8, 12, 20 and 32
|
| Starting date | 1 January 2019 |
| Contact information | Li Ning |
| Notes | Study lead contacted by email on 12 August 2021 regarding study progress |
EA: electro‐acupuncture
ICIQ‐SF: International Consultation on Incontinence Questionnaire ‐ Urinary Incontinence Short Form
ICS: International Continence Society
IIQ‐7: Incontinence Impact Questionnaire
IQoL: Incontinence Quality of Life
OAB: overactive bladder
OAB‐Q: Overactive Bladder Questionnaire
OABSS: overactive bladder symptom score
RCT: randomised controlled trial
UDI‐6: Urogenital Distress Inventory
UTI: urinary tract infection
Differences between protocol and review
In the protocol we undertook to search five Chinese databases:
China National Knowledge Infrastructure (CNKI);
Chinese Medical Literature Database (CBM);
Chinese Medical Current Content (CMCC);
Chinese Science and Technology Periodical Database (VIP); and
WANFANG (China Online Journals).
Following test search strategies it became clear that the CBM and CMCC produced duplicate searches to the three main Chinese language databases (CNKI, VIP and WANFANG), therefore the search strategy documented in Appendix 4 was used to conduct Chinese language searches and the methods section of the review was amended to reflect this.
Three included studies used a combined comparator as follows:
Liu 2019: comparator combines medication and pelvic floor training;
Hong 2015: comparator combines medication and bladder retraining;
Yu 2012: comparator combines medication and bladder retraining.
Combinations of conservative interventions are used to treat overactive bladder and the combinations selected in these studies are reflective of common practice. In the protocol for this review, we chose to group conservative interventions (e.g. pelvic floor training, bladder retraining, lifestyle changes) and medication for overactive bladder as separate entities. Many clinicians would argue that they are all conservative treatments and as such can be combined for the purposes of this review. We have chosen to include these studies as they reflect treatment in a 'real world' setting.
Contributions of authors
EH: reference screening, data extraction, risk of bias assessment, data input and editing, wrote text of review and edited, liaison with Cochrane Incontinence and Covidence support team. KB: review and editing of text, arbiter for data extraction. GB: review and editing of text, arbiter for bias assessment and GRADE assessment. CH: review and editing of text. YYZ: searching of Chinese databases, reference screening, data extraction, risk of bias assessment, review and editing of text. XWZ: searching of Chinese databases, reference screening, data extraction, risk of bias assessment, review and editing of text. NBK: statistical advice and review. CEC: reference screening, data extraction, risk of bias assessment, review and editing of text.
Sources of support
Internal sources
No sources of support provided
External sources
-
National Institute for Health Research (NIHR), UK
This project was supported by the NIHR, via Cochrane Infrastructure funding to Cochrane Incontinence. The views and opinions expressed therein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, the NIHR, the National Health Service (NHS), or the Department of Health. The NIHR is the largest single funder of Cochrane Incontinence.
-
National Center for Complementary and Integrative Health (NCCIH), USA
This work was partially funded by Grant Number R24 AT001293 from the National Center for Complementary and Integrative Health (NCCIH). The contents of this systematic review are solely the responsibility of the authors and do not necessarily represent the official views of the NCCIH or the National Institutes of Health.
Declarations of interest
In accordance with Cochrane's Commercial Sponsorship Policy, the following declarations are applicable for the three years prior to the publication date of this review.
EH: is a practising NHS physiotherapist (Newcastle upon Tyne Hospital NHS Foundation Trust) and uses acupuncture as one of a number of relevant interventions within their practice. KB: none to declare. GB: none to declare. CH: is a subject matter specialist engaged with several parties including Medronic, Allergan, Astellas and Teleflex Medical, and is the guidelines panel chair for the European Association of Urology. YYZ: none to declare. NBK: none to declare. XZ: none to declare. CEC: provides acupuncture education courses, including a course on acupuncture for women's health that discusses overactive bladder treatment strategies.
New
References
References to studies included in this review
Aydoğmuş 2014 {published data only}
- Aydoğmuş Y, Sunay M, Arslan H, Aydın A, Adiloğlu AK, Şahin H. Acupuncture versus solifenacin for treatment of overactive bladder and its correlation with urine nerve growth factor levels: a randomized, placebo-controlled clinical trial. Urologia Internationalis 2014;93(4):437-43. [DOI: 10.1159/000358202] [sr-incont64828] [DOI] [PubMed] [Google Scholar]
Chen 2009 {published data only}
- Chen Z, Han C, Wang G. 24 cases of overactive bladder treated by electroacupuncture [for information only English title translated via Google Translate™] [电针治疗膀胱过度活动症24例]. Journal of Clinical Acupuncture and Moxibustion 2009;25(8):22. [sr-incont99150] [Google Scholar]
Engberg 2009 {published data only}
- Engberg S, Cohen S, Sereika SM. The efficacy of acupuncture in treating urge and mixed incontinence in women: a pilot study. Journal of Wound, Ostomy and Continence Nursing 2009;36(6):661-70. [DOI: 10.1097/WON.0b013e3181bd82dd] [sr-incont35463] [DOI] [PubMed] [Google Scholar]
Hong 2015 {published data only}
- Hong LJ, Zhao J, Zheng GH. Clinical study on electro-acupuncture for the treatment of mixed urinary incontinence [电针治疗混合性尿失禁的临床研究]. Journal of Clinical Acupuncture and Moxibustion 2015;31(11):1-4. [sr-incont70299] [Google Scholar]
Kelleher 1994 {published data only}
- Kelleher CJ, Filshie J, Burton G, Khullar V, Cardozo LD. Acupuncture and the treatment of irritative bladder symptoms. Acupuncture in Medicine 1994;12(1):9-12. [Google Scholar]
Lin 2020 {published data only}
- Chan YT, Zhang HW, Guo YQ, Chan TNH, Kwan YK, Lee CK, et al. Effectiveness and safety of acupuncture for elderly overactive bladder population in Hong Kong: study protocol for a randomized controlled trial. Trials 2018;19(1):376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Z, Chan YT. A randomized controlled trial to assess the effectiveness and safety of acupuncture for overactive bladder: a study in Hong Kong patient population [針刺治療膀胱過度活躍症的臨床試驗研究]. chictr.org.cn/hvshowproject.aspx?id=11255 (first received 19 February 2016). [ChiCTR-INR-16010048] [sr-incont77989]
- Lin ZX, Chan NH, Kwan YK, Chan YT, Zhang H, Tam KS, et al. A randomized controlled trial to assess the effectiveness and safety of acupuncture for overactive bladder: a study in Hong Kong population. Chinese Medicine 2020;15(1):108. [DOI: 10.1186/s13020-020-00388-w] [ChiCTR-INR-16010048] [sr-incont90242] [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2019 {published data only}
- Kang J, Sun Y, Su T, Liu Y, Liang F, Liu Z. Electroacupuncture for balanced mixed urinary incontinence: secondary analysis of a randomized non-inferiority controlled trial. International Urogynecology Journal 2021;32(2):325-34. [NCT02047032] [sr-incont89529] [DOI] [PubMed] [Google Scholar]
- Liu B, Liu Y, Qin Z, Zhou K, Xu H, He L, et al. Electroacupuncture versus pelvic floor muscle training plus solifenacin for women with mixed urinary incontinence: a randomized noninferiority trial. Mayo Clinic Proceedings 2019;94(1):54-65. [DOI: 10.1016/j.mayocp.2018.07.021] [NCT02047032] [sr-incont78561] [DOI] [PubMed] [Google Scholar]
- Liu B, Wang Y, Xu H, Chen Y, Wu J, Mo Q, et al. Effect of electroacupuncture versus pelvic floor muscle training plus solifenacin for moderate and severe mixed urinary incontinence in women: a study protocol. BMC Complementary and Alternative Medicine 2014;14:301. [DOI: 10.1186/1472-6882-14-301] [NCT02047032] [sr-incont62533] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z, NCT02047032. Effect of electroacupuncture versus PFMT plus solifenacin for mixed urinary incontinence [Effect of electroacupuncture versus PFMT plus solifenacin for moderate and severe mixed urinary incontinence in female: a multicenter, noninferiority, randomized controlled trial]. clinicaltrials.gov/show/NCT02047032 (first received 28 January 2014). [NCT02047032] [sr-incont60908]
- Sun Y, Liu Y, Liu S, Wang W, Liu Z. Electroacupuncture for women with urgency-predominant mixed urinary incontinence: secondary analysis of a randomized noninferiority trial. World Journal of Urology 2020;38(4):1035-42. [DOI: 10.1007/s00345-019-02828-1] [NCT02047032] [sr-incont87623] [DOI] [PubMed] [Google Scholar]
Shen 2020 {published data only}
- Shen J, Luo YR, Meng YJ, Zhang YL, Qin PG, Ke LP, et al. Clinical study of electro-acupuncture in the treatment of female overactive bladder [for information only English title translated via Google Translate™] [电针疗法治疗女性膀胱过度活动症的临床研究]. Chinese Journal of Integrative Medicine 2020;40(8):1000-4. [DOI: 10.7661/j.cjim.20200531.068] [sr-incont99172] [DOI] [Google Scholar]
Solberg 2016 {published data only}
- Solberg M, Alræk T, Mdala I, Klovning A. A pilot study on the use of acupuncture or pelvic floor muscle training for mixed urinary incontinence. Acupuncture in Medicine 2016;34(1):7-13. [DOI: 10.1136/acupmed-2015-010828] [sr-incont70460] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2011 {published data only}
- Lui J. Clinical Study on Treatment of Female Kidney-Qi Insufficiency Type Overactive Bladder by Electro-Acupuncture at Weizhong and Feiyang Point [Masters thesis]. Chengdu, Sichuan Province (China): Chengdu University of Traditional Chinese Medicine, 2019. [DOI: 10.26988/d.cnki.gcdzu.2019.000151] [DOI] [Google Scholar]
- Wang XL, Shi YZ. Clinical study on acupuncture for overactive bladder (kidney-qi deficiency type) in elderly women [for information only English title translated via Google Translate™] [针刺治疗老年女性膀胱过度活动症(肾气亏虚型)的临床研究]. Guide of Chinese Medicine 2011;9(32):176-7. [ISSN: 1671-8194] [sr-incont99173] [Google Scholar]
Wang 2013a {published data only}
- Wang B, Xiao YP, Fan K, Huang CJ. Treatment of female overactive bladder with acupuncture [针灸治疗女性膀胱过度活动症的临床研究]. Journal of Beijing University of Traditional Chinese Medicine 2013;36(10):713-6. [ISSN: 1006-2157] [sr-incont99174] [Google Scholar]
Yang 2016 {published data only}
- Yang WY. 电针中髎, 会阳穴治疗膀胱过度活动症临床疗效观察 [Masters thesis] [Clinical Observation of Electroacupuncture at Zhongliao and Huiyang Points in the Treatment of Overactive Bladder. For information only English title translated via Google Translate™]. Beijing (China): Beijing University of Chinese Medicine, 2016. [sr-incont89283] [Google Scholar]
Yu 2012 {published data only}
- Yu, HZ. 电针治疗膀胱过度活动症的临床初探 [Masters thesis] [Clinical Preliminary Study on Electroacupuncture for Overactive Bladder. For information only English title translated via Google Translate™]. Beijing (China): Beijing University of Chinese Medicine, 2015. [sr-incont89282] [Google Scholar]
- Yu X, Wang J. 24 cases of overactive bladder treated by acupuncture [for information only English title translated via Google Translate™] [针刺治疗膀胱过度活动症24例]. Shandong Journal of Traditional Chinese Medicine 2011;30(4):245-6. [DOI: 10.16295/j.cnki.0257-358x.2011.04.039] [sr-incont99177] [DOI] [Google Scholar]
- Yu X, Wang J. Acupuncture therapy in treating 24 cases of overactive bladder. International Journal of Clinical Acupuncture 2012;21(3):113-4. [sr-incont72480] [Google Scholar]
Yuan 2015 {published data only}
- Yuan Z, He C, Yan S, Huang D, Wang H, Tang W. Acupuncture for overactive bladder in female adult: a randomized controlled trial. World Journal of Urology 2015;33(9):1303-8. [DOI: 10.1007/s00345-014-1440-0] [ChiCTR-TRC-14005243] [sr-incont69329] [DOI] [PubMed] [Google Scholar]
- Yuan Z, He C. Acupuncture for overactive bladder in female adult: a randomized controlled trial (Abstract number 125). In: 45th Annual Meeting of the International Continence Society (ICS); 2015 Oct 6-9; Montreal, Canada. 2015. [ChiCTR-TRC-14005243] [sr-incont68771]
Zhang 2015 {published data only}
- Zhang J, Cheng W, Cai M. Effects of electro-acupuncture on overactive bladder refractory to anticholinergics: a single-blind randomised controlled trial. Acupuncture in Medicine 2015;33(5):368-74. [DOI: 10.1136/acupmed-2015-010770] [sr-incont69268] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Anhari 2011 {published data only}
- Anhari I. Comparative effects acupuncture and tolterodine on decreasing overactive bladder symptom score on overactive bladder. International Journal of Clinical Acupuncture 2011;20(2):49. [Google Scholar]
Cai 2017 {published data only}
- Cai S. Clinical study on acupuncture and nursing intervention in the treatment of female overactive bladder [针灸及护理干预治疗女性膀胱过度活动症的临床研究]. Chinese Community Doctors 2017;33(8):123, 125. [Google Scholar]
Carmona 2013 {published data only}
- Carmona MV, Molleja ÁM, Ríos IL, Torronteras AR, Tamajón VM, Obrero IG. Percutaneous tibial nerve stimulation versus neurostimulation of SP 6 (Sanyinjiao) in urge incontinence [Neuroestimulación percutánea del nervio tibial posterior frente a neuroestimulación de B 6 (Sanyinjiao) en incontinencia urinaria de urgencia]. Revista Internacional De Acupuntura 2013;7(4):124-30. [DOI: 10.1016/S1887-8369(13)70102-9] [DOI] [Google Scholar]
Chen 2003 {published data only}
- Chen YL, Chen GM, Ge LB, Ha LF, Zong L. Effect of acupuncture different points on unstable bladder. Journal of Acupuncture and Tuina Science 2003;1(3):22-4. [Google Scholar]
Chen 2005a {published data only}
- Chen Yl, Cen J, Hou WG, Gao ZQ, Wang XY, Peng HD. Clinical study on different needling methods for unstable bladder of kidney deficiency [不同针刺方法对肾虚型不稳定膀胱排尿状况的临床研究]. Shanghai Journal of Traditional Chinese Medicine 2005;39(7):43-4. [Google Scholar]
Chen 2005b {published data only}
- Chen YL, Ha LF, Cen J, Huang QR, Hou WG, Gao ZQ. Comparative observation on therapeutic effects of electroacupuncture and manual acupuncture on female urethral syndrome. Chinese Acupuncture and Moxibustion 2005;25(6):425-6. [PubMed] [Google Scholar]
Chen 2012 {published data only}
- Chen YL, Feng WJ, Zhang XL. Parkinson’s disease combined with overactive bladder syndrome treated with acupuncture and medication [针药结合治疗帕金森病合并膀胱过度活动症]. Chinese Acupuncture and Moxibustion 2012;32(3):215-8. [PubMed] [Google Scholar]
Chen 2015a {published data only}
- Chen YX, Ma RJ. Clinical observation of electroacupuncture at Huiyang (BL35) and Zhongliao (BL33) plus scalp acupuncture for female stress urinary incontinence [电针会阳、中髎穴结合头针治疗女性压力性尿失禁临床观察]. Shanghai Journal of Acupuncture and Moxibustion 2015;34(12):1159-61. [Google Scholar]
Chen 2015b {published data only}
- 陈楚红, 龚旻, 顾勇刚, 胡巍. Acupuncture combined with doxazosin mesylate controlled-release tablets in the treatment of chronic prostatitis complicated with overactive bladder [for information only English title translated via Google Translate™] [针刺联合甲磺酸多沙唑嗪控释片治疗慢性前列腺炎合并膀胱过度活动症]. In: 第十次全国中西医结合男科学术大会、第六次广西中医、中西医结合男科学术大会、全国中西医结合男科疾病诊疗新进展学习班. 2015.
Chen 2015c {published data only}
- Chen X, Chen J, Tang SL. Efficacy observation of electroacupuncture combined with tolterodine in the treatment of 48 cases of female overactive bladder [for information only English title translated via Google Translate™] [电针联合托特罗定治疗女性膀胱过度活动症48例疗效观察]. Hainan Medical Journal 2015;26(1):127-8. [Google Scholar]
Cheung 2018 {published data only}
- Cheung YK, Law PM, Lee LL, Ng K, Chan SC. Acupuncture for urinary incontinence in Chinese women: a randomized controlled trial (Abstract 30). Neurourology and Urodynamics 2018;37(Suppl 5):S78-9. [Google Scholar]
Dunning 2017 {published data only}
- Dunning J, NCT03238716. Neuromuscular re-eduaction, [sic] exercise and electric dry needling vs. neuromuscular re-education and exercise for stress urinary incontinence [Neuromuscular re-education, impairment-based exercise and electric dry needling vs. neuromuscular re-education and impairment-based exercise for stress urinary incontinence]. clinicaltrials.gov/show/NCT03238716 (first received 3 August 2017).
Ellis 1990 {published data only}
- Ellis N, Briggs R, Dowson D. The effect of acupuncture on nocturnal urinary frequency and incontinence in the elderly. Complementary Medicine Research 1990;4(1):16-8. [Google Scholar]
Emmons 2005 {published data only}
- Emmons SL, Otto L. Acupuncture for overactive bladder: a randomized controlled trial. Obstetrics and Gynecology 2005;106(1):138-43. [DOI] [PubMed] [Google Scholar]
Enberg 2006 {published data only}
- Engberg S, NCT00297427. Acupuncture for urinary incontinence [Efficacy of acupuncture in treating urinary incontinence]. clinicaltrials.gov/show/NCT00297427 (first received 28 February 2006). [NCT00177450 (obsolete)]
Feng 2011 {published data only}
- Feng W, Chen Y, Zhang X. Research on acupuncture combined with small dose of tolterodine in the treatment of overactive bladder symdrom in Parkinson's disease [针刺联合小剂量托特罗定治疗帕金森病合并膀胱过度活动症]. Chinese Journal of Practical Nervous Diseases 2011;14(16):7-10. [ISSN: 1673-5110] [Google Scholar]
Feng 2014 {published data only}
- Feng QT, He B, Chen XL, Li RH. Clinical observation of different acupuncture methods for treating overactive bladder syndrome. Journal of New Chinese Medicine 2014;46(12):188-90. [CENTRAL: CN-01427256] [Google Scholar]
Guo 2016 {published data only}
- Guo Y, Yang X, Wang Y, Wang X, Jiang Y, Xiong W. A comparative study on the application of pure acupuncture and solifenacin succinate in the treatment of women with overactive bladder [for information only English title translated via Google Translate™] [应用单纯针灸疗法与琥珀酸索利那新治疗女性膀胱过度活动症的对比性研究]. Journal of Emergency in Traditional Chinese Medicine 2016;25(11):2193-5. [DOI: 10.3969/j.issn.1004-745X.2016.11.062] [DOI] [Google Scholar]
He 2016 {published data only}
- He E, Chen Y, Tian H, Zhao J. Effective observation of electroacupuncture with different courses for female stress urinary incontinence. Chinese Acupuncture and Moxibustion 2016;36(4):351-4. [PubMed] [Google Scholar]
He 2018 {published data only}
- He T, Mo Q, ChiCTR1800018176. A randomized controlled trial for comparing electroacupuncture and warm acupuncture in the treatment of overactive bladder. chictr.org.cn/showproj.aspx?proj=30705 (first received 3 September 2018).
Hong 1996 {published data only}
- Hong Z. Combination of scalp acupuncture with body acupuncture for treating senile urinary incontinence. Journal of Chinese Medicine 1996;52:10-1. [Google Scholar]
Hu 2005 {published data only}
- Hu J. Acupuncture treatment of frequent urination. Journal of Traditional Chinese Medicine 2005;25(3):238-40. [PMID: ] [PubMed] [Google Scholar]
Hu 2015 {published data only}
- Hu B, Zheng DB, Jing ZT, Wang JF. 30 cases of female urgent urinary incontinence treated by acupoint application of traditional Chinese medicine [for information only English title translated via Google Translate™] [中药穴位贴敷治疗女性急迫性尿失禁30 例]. 西部中医药 2015;28(12):109-10. [Google Scholar]
Hu 2016 {published data only}
- 胡碧川. A randomized controlled clinical study of oral tolterodine tablets combined with electroacupuncture on the four sacral points in the treatment of overactive bladder [for information only English title translated via Google Translate™] [口服托特罗定片联合电针骶四穴疗法治疗膀胱过度活动症的随机对照临床研究]. In: 中国中西医结合学会泌尿外科专业委员会第十四次全国学术会议暨2016年广东省中西医结合学会泌尿外科专业委员会学术年会. 2016.
Jiao 2019 {published data only}
- Jiao R, Liu Y, Liu B, Liu Z. Risk factors related to acupuncture response in postmenopausal women with stress urinary incontinence: secondary analysis of a randomized controlled trial. Medicine 2019;98(16):e15220. [CLINICAL TRIAL: NCT01784172] [DOI: 10.1097/MD.0000000000015220] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnstone 2003 {published data only}
- Johnstone PA, Bloom TL, Niemtzow RC, Crain D, Riffenburgh RH, Amling CL. A prospective, randomized pilot trial of acupuncture of the kidney-bladder distinct meridian for lower urinary tract symptoms. Journal of Urology 2003;169(3):1037-9. [DOI: 10.1097/01.ju.0000044925.03113.ab] [DOI] [PubMed] [Google Scholar]
Kim 2008 {published data only}
- Kim JH, Nam D, Park MK, Lee ES, Kim SH. Randomized control trial of hand acupuncture for female stress urinary incontinence. Acupuncture and Electro-Therapeutics Research 2008;33(3-4):179-92. [DOI: 10.3727/036012908803861122] [DOI] [PubMed] [Google Scholar]
Kubista 1976 {published data only}
- Kubista E, Altmann P, Kucera H, Rudelstorfer B. Electro-acupuncture's influence on the closure mechanism of the female urethra in incontinence. American Journal of Chinese Medicine 1976;4(2):177-81. [DOI: 10.1142/s0192415x76000226] [DOI] [PubMed] [Google Scholar]
Kwon 2014 {published data only}
- Kwon JN, NCT02271607. The effect and safety of moxibustion therapy for overactive bladder patients [A pilot study about the effects of indirect-moxibustion on bladder- functional improvement and symptoms management in patients with overactive bladder: a randomized controlled trial]. clinicaltrials.gov/show/NCT02271607 (first received 22 October 2014).
Lee 2016 {published data only}
- Lee LL, Chan SS, ChiCTRINR16007766. Acupuncture for urinary incontinence in Chinese women: a randomized controlled trial [針灸用於處理華人婦女小便失禁問題之隨機研究]. chictr.org.cn/showproj.aspx?proj=13144 (first received 11 January 2016).
Liao 2007 {published data only}
- Liao X, Tang H, Xiao P. 35 cases of overactive bladder treated by electroacupuncture at Zhongliao point [for information only English title translated via Google Translate™] [电针中髎穴为主治疗膀胱过度活动症35例]. Journal of Clinical Acupuncture and Moxibustion 2007;23(1):35-6. [Google Scholar]
Liao X 2007 {published data only}
- 廖小七, 唐华, 肖鹏. 35 cases of overactive bladder treated by electroacupuncture at Zhongliao point [for information only English title translated via Google Translate™] [电针中髎穴为主治疗膀胱过度活动症35例]. Journal of Clinical Acupuncture and Moxibustion 2007;23(1):35-6. [Google Scholar]
Lillie 2014 {published data only}
- Lillie R. News from the front: Professor Si-you Wang: pudendal nerve stimulation for incontinence. Journal of the Acupuncture Association of Chartered Physiotherapists 2014;Autumn(1):129-30. [ISSN: 1748-8656] [Google Scholar]
Liu 1998 {published data only}
- Liu ZS, Shao SJ, Ye YM, Li YS, Huang M, Zhang H, et al. Analysis of the curative effect of electro-acupuncture at Ciliao & Huiyang points to treat senile urinary incontinence [电针次 、会阳治疗老年尿失禁疗效分析]. Shanghai Journal of Acupuncture and Moxibustion 1998;17(3):14-5. [Google Scholar]
Liu 2010 {published data only}
- 刘超. 中西医结合治疗膀胱过度活动症的临床观察 [Masters thesis] [Clinical Observation on Treatment of Overactive Bladder with Integrated Traditional Chinese and Western Medicine. For information only English title translated via Google Translate™]. Hubei (China): 湖北中医药大学, 2010. [Google Scholar]
Liu 2013 {published data only}
- Liu B, NCT01784172. Efficacy and safety study of electroacupuncture for simple female stress urinary incontinence-a multicenter trial [The efficacy and safety study of electro-acupuncture for simple female stress urinary incontinence - a multicenter, randomized controlled trial]. clinicaltrials.gov/show/NCT01784172 (first received 5 February 2013).
Liu 2015a {published data only}
- Liu ZS, Xu HF, NCT02445573. Efficacy of electroacupuncture (EA) for women with pure stress urinary incontinence (SUI) [A pilot randomized placebo controlled trial of electroacupuncture for women with pure stress urinary incontinence]. clinicaltrials.gov/show/NCT02445573 (first received 15 May 2015).
Liu 2015b {published data only}
- Liu Z, Chen H, Wu W, Luo Q, Huang X, Shen T, et al. The clinical observation in treating overactive bladder by the combination of tolterodine and electroacupuncture [托特罗定联合电针治疗膀胱过度活动症临床观察]. China Medical Innovation 2015;12(1):52-4. [DOI: 10.3969/j.issn.1674-4985.2015.01.018] [DOI] [Google Scholar]
Liu 2016 {published data only}
- Liu YM, Jin HY, Li ZQ. Effect of pelvic floor biofeedback combined with Huiyang acupuncture and moxibustion on muscle potential and quality of life in patients with postpartum urinary incontinence [盆底生物反馈结合针灸会阳穴对产后尿失禁患者肌电位及生活质量的影响]. Maternal and Child Health Care of China 2016;31(14):2799-801. [Google Scholar]
Liu 2017 {published data only}
- Liu Z, Liu Y, Xu H, He L, Chen Y, Fu L, et al. Effect of electroacupuncture on urinary leakage among women with stress urinary incontinence: a randomized clinical trial. JAMA 2017;317(24):2493-501. [DOI: 10.1001/jama.2017.7220] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lu 2002 {published data only}
- Lu ZQ. Clinical analysis on scalp-plus body-acupuncture for treatment of senile urinary incontinence. World Journal of Acupuncture-Moxibustion 2002;12(2):50-2. [ISSN: 1003-5257] [Google Scholar]
Mao 2012 {published data only}
- Hou C, Gao W, Hu S. Clinical observation of M receptor antagonist combined with acupuncture in the treatment of overactive bladder [for information only English title translated via Google Translate™] [M受体拮抗剂与针刺疗法联合治疗膀胱过度活动症的临床观察]. Hubei Journal of Traditional Chinese Medicine 2014;36(3):40-1. [Google Scholar]
- Mao HH. 针刺联合M受体拮抗剂优化治疗膀胱过度活动症的临床研究 [Masters thesis] [Acupuncture Combined M Receptor Antagonist Optimization Overactive BIadder CIinicaI Research]. Wuhan, Hubei (China): Hubei University of Traditional Chinese Medicine, 2012. [Google Scholar]
Miao 2015 {published data only}
- Miao G, Jia M, Zhang X. Efficacy observation of electroacupuncture combined with pelvic floor muscle training in the treatment of female overactive bladder [for information only English title translated via Google Translate™] [电针联合盆底肌训练治疗女性膀胱过度活动症的疗效观察]. Journal of Emergency in Traditional Chinese Medicine 2015;24(11):2054-6. [Google Scholar]
Nam 2017 {published data only}
- Nam EY, Kim DI, NCT03260907. Efficacy and safety of electroacupuncture and acupuncture in postmenopausal women with overactive bladder [Efficacy and safety of electroacupuncture and acupuncture in postmenopausal women with overactive bladder; a multicenter, randomized, controlled, parallel clinical trial]. clinicaltrials.gov/show/NCT03260907 (first received 24 August 2017).
Pang 2018 {published data only}
- Pang R, NCT03450902. Chinese herbal therapy combined with acupuncture for female mixed urinary incontinence [Combination therapy with Chinese herbal formula, Yiqi Suoquan granule, and acupuncture for female mixed urinary incontinence]. clinicaltrials.gov/show/NCT03450902 (first received 1 March 2018).
Penson 2018 {published data only}
- Penson DF. Re: effect of electroacupuncture on urinary leakage among women with stress urinary incontinence: a randomized clinical trial. Journal of Urology 2018;199(1):35-6. [DOI: 10.1016/j.juro.2017.09.112] [DOI] [PubMed] [Google Scholar]
Philp 1988 {published data only}
- Philp T, Shah PJ, Worth PH. Acupuncture in the treatment of bladder instability. British Journal of Urology 1988;61(6):490-3. [DOI: 10.1111/j.1464-410x.1988.tb05086.x] [DOI] [PubMed] [Google Scholar]
Qu 2013 {published data only}
- Qu Y, Chen X, Qu M, Zhao R, Yu J, Wang S. 32 cases of overactive bladder treated by electroacupuncture [for information only English title translated via Google Translate™] [电针治疗膀胱过度活动症 32 例]. 中国保健营养: 下半月 2013;3:641. [Google Scholar]
Ren 2020 {published data only}
- Ren TT. Comparison of effects of acupuncture and solifenacin succinate tablets in treatment of female overactive bladder patients [for information only English title translated via Google Translate™] [针灸和琥珀酸索利那新片治疗女性膀胱过度活动症患者的效果比较]. Medical Journal of Chinese People’s Health 2020;32(6):115-7. [Google Scholar]
Rong 2015 {published data only}
- Rong Q. The quality of life effects acupuncture treatment for the female pelvic floor dysfunction [针灸治疗压力性尿失禁60例临床观察]. Chinese Journal of Ethnomedicine and Ethnopharmacy 2015;24(21):92-3; 95. [Google Scholar]
Ruan 2018 {published data only}
- Ruan L, ChiCTR1800014351. Clinical study of pelvic floor electrical stimulation combined with traditional Chinese medicine and acupoint sticking in the treatment of postpartum urinary incontinence [Clinical study of pelvic floor electrical stimulation combined with traditional Chinese medicine and acupoint sticking in the treatment of postpartum urinary incontinence (Qi Deficiency syndrome)]. trialsearch.who.int/Trial2.aspx?TrialID=ChiCTR1800014351 (first received 7 January 2018).
Shen 2012a {published data only}
- Shen YZ, Lin X, Lin Q. Overactive bladder after transurethral resection of prostate treated with electroacupuncture therapy and tolterodine [电针联合托特罗定治疗经尿道前列腺电切术后膀胱过度活动症]. Chinese Acupuncture and Moxibustion 2012;32(5):404-8. [PubMed] [Google Scholar]
Shen 2012b {published data only}
- Shen YZ, Shen L. Electroacupuncture for overactive bladder after transurethral resection of prostate [电针治疗经尿道前列腺电切术后膀胱过度活动症效果]. Medical Journal of Qilu 2012;27(4):341-2, 5. [Google Scholar]
Su 2013 {published data only}
- Su TS, NCT01940432. The efficacy of electroacupuncture for treatment of simple female stress urinary incontinence: comparison with pelvic floor muscle training-a multicenter randomized controlled trial. clinicaltrials.gov/ct2/show/NCT01940432 (first received 12 September 2013).
Su 2020a {published data only}
- Su YY, Zhao D, Lin MQ. Clinical observation of urine three-needling combined with tolterodine in treating overactive bladder [尿三针联合托特罗定治疗膀胱过度活动症的临床疗效观察]. Journal of Guangzhou University of Traditional Chinese Medicine 2020;37(8):1495-500. [Google Scholar]
Su 2020b {published data only}
- Su Y, Zhao D, Lin MQ. Clinical observation of urine three-needling combined with tolterodine in the treatment of overactive bladder [尿三针联合托特罗定治疗膀胱过度活动症的临床疗效观察]. Journal of Guangzhou University of Traditional Chinese Medicine 2020;37(8):1495-500. [Google Scholar]
Suen 2015 {published data only}
- Suen LK, NCT02330107. Auriculotherapy on lower urinary tract symptoms in elderly men [Effectiveness of auriculotherapy on lower urinary tract symptoms in elderly men: a randomized controlled feasibility study]. clinicaltrials.gov/show/NCT02330107 (first received 1 January 2015).
Tang 2016 {published data only}
- Tang KM, Shen R, Jiang F, Wang Q, Xie XB, Chen YL. Therapeutic evaluation of acupuncture for female stress urinary incontinence [针刺治疗女性单纯性压力性尿失禁临床疗效评价]. Shanghai Journal of Acupuncture and Moxibustion 2016;35(12):1439-41. [Google Scholar]
Wan 2019 {published data only}
- Wan OY, Cheung YK, Law MP, Lee LL, Chan SS. A randomized controlled trial on the effect of acupuncture on urinary incontinence and quality of life in women (Abstract 96). Female Pelvic Medicine and Reconstructive Surgery 2019;25(5 Suppl):S74-5. [DOI: 10.1097/SPV.0000000000000763] [DOI] [Google Scholar]
Wang 2008 {published data only}
- Wang HX, Cui H. Observation on the effect of electroacupuncture on senile urge urinary incontinence [for information only English title translated via Google Translate™] [电针治疗老年急迫性尿失禁疗效观察]. Chinese Journal of Information on Traditional Chinese Medicine 2008;15(2):70. [Google Scholar]
Wang 2013b {published data only}
- Wang YF, Pan ZL, Chen JJ, Zhang W, Meng L. Clinical study of electroacupuncture in the treatment of overactive bladder [for information only English title translated via Google Translate™] [电针疗法治疗膀胱过度活动症的临床研究]. Practical Clinical Journal of Integrated Traditional Chinese and Western Medicine 2013;13(3):1-3. [Google Scholar]
Wang 2015 {published data only}
- Wang S, NCT02599831. Efficacy of electrical pudendal nerve stimulation for patients with post prostatectomy urinary incontinence. clinicaltrials.gov/show/NCT02599831 (first received 9 November 2015).
Wang 2016 {published data only}
- Wang S, Lv J, Feng X, Wang G, Lv T. Efficacy of electrical pudendal nerve stimulation in treating female stress incontinence. Urology 2016;91:64-9. [DOI: 10.1016/j.urology.2016.02.027] [DOI] [PubMed] [Google Scholar]
Wang 2017a {published data only}
- Wang M. Acupuncture for stress urinary incontinence. JAMA 2017;318(15):1500. [DOI: 10.1001/jama.2017.13424] [DOI] [PubMed] [Google Scholar]
Wang 2017b {published data only}
- Wang S, NCT02311634. A comparison of electrical pudendal nerve stimulation and transvaginal electrical stimulation for urge incontinence [A comparison of efficacies of electrical pudendal nerve stimulation versus transvaginal electrical stimulation in treating urge incontinence]. clinicaltrials.gov/show/NCT02311634 (first received 8 December 2014).
- Wang SY, Lv JW, Feng XM, Lv TT. Efficacy of electrical pudendal nerve stimulation versus transvaginal electrical stimulation in treating female idiopathic urgency urinary incontinence. Journal of Urology 2017;197(6):1496-501. [DOI: 10.1016/j.juro.2017.01.065] [DOI] [PubMed] [Google Scholar]
Wang 2019 {published data only}
- Wang W, Liu Y, Sun S, Liu B, Su T, Zhou J, et al. Electroacupuncture for postmenopausal women with stress urinary incontinence: secondary analysis of a randomized controlled trial. World Journal of Urology 2019;37(7):1421-7. [DOI: 10.1007/s00345-018-2521-2] [DOI] [PubMed] [Google Scholar]
Xie 2020 {published data only}
- Xie N, Yang Y, Jiang HY. Clinical observation of applying acupuncture and nursing intervention in the treatment of overactive bladder [针灸及护理干预治疗膀胱过度活动症临床观察]. Journal of Sichuan of Traditional Chinese Medicine 2020;38(7):202-5. [Google Scholar]
Xiong 2020 {published data only}
- Xiong C, Tang Y, Shi R, Zhou YH, Sun S, Xiang Y, et al. Therapeutic effect of myofascial trigger point electroacupuncture technology on the treatment of overactive bladder syndrome in female [电针刺激肌筋膜触发点治疗女性膀胱过度活动症的临床疗效]. Journal of Central South University (Medical Science) 2020;45(2):155-9. [DOI] [PubMed] [Google Scholar]
Xu 2010 {published data only}
- 徐海蓉. 针刺治疗膀胱过度活动症的系统评价及中风后急迫性尿失禁电针疗效的 RCT 研究 [PhD thesis] [A Systematic Review of Acupuncture for Overactive Bladder and an RCT Study on the Efficacy of Electroacupuncture for Post-Stroke Urge Urinary Incontinence. For information only English title translated via Google Translate™]. 北京: 中国中医科学院, 2010. [Google Scholar]
Xu 2016 {published data only}
- Xu H, Liu B, Wu J, Du R, Liu X, Yu J, et al. A pilot randomized placebo controlled trial of electroacupuncture for women with pure stress urinary incontinence. PLOS One 2016;11(3):e0150821. [DOI: 10.1371/journal.pone.0150821] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yang 2020 {published data only}
- Xie N, Yue J, Jiang HY. Clinical observation of applying acupuncture and nursing intervention in the treatment of overactive bladder [针灸及护理干预治疗膀胱过度活动症临床观察]. Journal of Sichuan of Traditional Chinese Medicine 2020;38(7):202-5. [Google Scholar]
Zhang 1999 {published data only}
- Zhang H. Scalp acupuncture plus body acupuncture for senile urinary incontinence. International Journal of Clinical Acupuncture 1999;10:101-4. [Google Scholar]
Zhang 2012 {published data only}
- Zhang GT, Bao ZH, Zhang LD. Efficacy of solifenacin combined with electrical stimulation in the treatment of women with overactive bladder [for information only English title translated via Google Translate™] [索利那新联合电刺激治疗女性膀胱过度活动症的疗效]. Journal of Practical Medicine 2012;28(23):3990-2. [ISSN: 1006-5725] [Google Scholar]
Zhao 2012 {published data only}
- Zhao L. Acusector Overactive Bladder in 68 Cases of Disease Clinical Observation [电针参与治疗膀胱过度活动症68例临床观察] [Masters thesis]. Zhengzhou (China): Henan College of Traditional Chinese Medicine, 2012. [Google Scholar]
Zhao 2013 {published data only}
- Zhao L, Wang SY. Treatment frequency and long-term efficacy observation on electric pudendal nerve stimulation for stress urinary incontinence. Journal of Acupuncture and Tuina Science 2013;11(3):177-80. [DOI: 10.1007/s11726-013-0684-3] [DOI] [Google Scholar]
Zhao 2013a {published data only}
- Zhao L, Wang SY. Efficacy impacts of the different treatment frequencies on female stress urinary incontinence. Chinese Acupuncture and Moxibustion 2013;33(12):1088-90. [PubMed] [Google Scholar]
Zhao 2016 {published data only}
- Zhao J, Cui X, Lu Y, He X, Wen C. Clinical study of acupuncture combined with aconite cake-separated moxibustion in treating senile female stress urinary incontinence [针刺联合隔附子饼灸治疗老年女性压力性尿失禁临床研究]. World Chinese Medicine 2016;11(5):891-3. [Google Scholar]
Zheng 1990 {published data only}
- Zheng H, Sun Y, Xu Z, Hao M, Cao X. Urodynamic study of acupuncture and moxibustion on female stress urinary incontinence [for information only English title translated via Google Translate™] [针灸对女性压力性尿失禁的尿流动力学研究]. Shanghai Journal of Acupuncture and Moxibustion 1990;9(3):1-3. [Google Scholar]
Zheng 1992 {published data only}
- Zheng H, Sun Y, Xu Z, Hou M. Flow dynamics of urine in female patients with stress urinary incontinence treated by acupuncture and moxibustion. International Journal of Clinical Acupuncture 1992;3(3):243-7. [Google Scholar]
Zheng 2015 {published data only}
- Zheng HM, Xu SF, Yin P, Tang KM, Chen YL. Observation on short-term and long-term therapeutic effects of electro-acupuncture on mild and moderate stress urinary incontinence [电针治疗轻中度女性压力性尿失禁的近远期疗效观察]. World Journal of Integrated Traditional and Western Medicine 2015;10(2):191-3, 209. [Google Scholar]
Zhishun 2002 {published data only}
- Zhishun L, Baoyan L, Tao Y, Yongming Y, Hong Z, Wei Z, et al. Clinical study of electroacupuncture treatment of senile urge urinary incontinence. International Journal of Clinical Acupuncture 2002;13(4):255-62. [Google Scholar]
Zhong 2016 {published data only}
- Zhong P, Yu H, Zhou Q, Lu Z, Yang C. Clinical study of electroacupuncture combined with M receptor antagonist in optimal treatment of overactive bladder [for information only English title translated via Google Translate™] [电针联合M 受体拮抗剂优化治疗膀胱过度活动症的临床研究]. In: 中国中西医结合学会泌尿外科专业委员会第十四次全国学术会议暨 2016 年广东省中西医结合学会泌尿外科专业委员会学术年会论文集 2016 [The 14th National Academic Conference of the Urology Professional Committee of the Chinese Society of Chinese and Western Medicine and the 2016 Academic Conference of the Professional Committee of Urology of the Chinese and Western Medical Association of Guangdong Province. For information only English title translated via Google Translate™]. Vol. 1. 2016:1604-7.
Zhu 2018 {published data only}
- 朱彬彬, 童钟, 周世超, 成慧慧, 赵嫦莹, 萧韵雅. Observation of curative effect of acupuncture at Bliao point combined with injection of botulinum toxin type A in the treatment of overactive bladder after spinal cord injury [for information only English title translated via Google Translate™] [针刺八髎穴联合A型肉毒毒素注射治疗脊髓损伤后膀胱过度活动症疗效观察]. 河北中医 2018;40(5):759-62. [Google Scholar]
Zhu 2021 {published data only}
- Zhu Z, Bi Q. Analysis of the value of acupuncture in the treatment of frequent urination [for information only English title translated via Google Translate™] [针刺治疗尿频的价值分析]. Clinical Research 2021;29(2):113-4. [Google Scholar]
References to studies awaiting assessment
Bulut 2014 {published data only}
- Bulut BB, Kilic MA, Resim S, Efe E, Bahar MR, Koluş E. S231: Comparison between acupuncture treatment and tolteradine in overactive bladder. European Urology Supplements 2014;13(7):e1556. [DOI: 10.1016/S1569-9056(14)61758-9] [sr-incont99190] [DOI] [Google Scholar]
Han 2011 {published data only}
- Han C. Clinical observation of electroacupuncture on 48 cases of overactive bladder [for information only English title translated via Google Translate™] [电针治疗膀胱过度活动症48例临床疗效观察]. In: 首届全国脑外伤治疗与康复学术大会论文汇编 (下) [First National Academic Conference on Treatment and Rehabilitation of Brain Trauma (Part 2) For information only English title translated via Google Translate™]. 2011. [sr-incont99545]
References to ongoing studies
Huang 2020 {published data only}
- Huang Y, Mo Q, ChiCTR1900027846. Randomized controlled trial for the efficacy of electroacupuncture in the treatment of acute urinary incontinence. chictr.org.cn/showprojen.aspx?proj=45632 (first received 30 November 2019). [ChiCTR1900027846] [sr-incont85138] [PARTNER REGISTRY: ChiMCTR1900025384]
- Huang Y, Qi S, Wu X, Zhi N, He T, Shen M, et al. Randomized controlled trial for the efficacy of electroacupuncture in the treatment of urge urinary incontinence: a clinical study protocol. Medicine 2020;99(9):e19315. [DOI: 10.1097/MD.0000000000019315] [ChiCTR1900027846] [sr-incont85335] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jia 2015 {published data only}
- Jia BH, NCT02452879. Treatment, parallel assignment, double blind (subject, outcomes assessor), efficacy study [The effectiveness, superiority and safety of EA on OAB: multi-center randomized controlled trial]. clinicaltrials.gov/show/NCT02452879 (first received 25 May 2015). [NCT02452879] [sr-incont68790]
Pang 2021 {published data only}
- Pang R, NCT05158361. Acupuncture for overactive bladder in adults [Effectiveness and safety of acupuncture for overactive bladder in adults: a random control clinical trial]. clinicaltrials.gov/show/NCT05158361 (first received 15 December 2021). [NCT05158361] [sr-incont98453]
Shen 2019 {published data only}
- Shen J, ChiCTR1900021372. A randomized controlled trial for the efficacy and safety of electro-acupuncture in the treatment of female overactive bladder [电针治疗女性膀胱过度活动症的有效性和安全性的随机对照试验]. chictr.org.cn/showproj.aspx?proj=36078 (first received 14 January 2019). [ChiCTR1900021372] [sr-incont78551]
Sheyn 2017 {published data only}
- Sheyn D, NCT03087578. Comparison of electroacupuncture to mirabegron for treatment of overactive bladder [Comparison of electroacupuncture to mirabegron on symptoms of overactive bladder in women who have failed anti-cholinergic therapy]. clinicaltrials.gov/show/NCT03087578 (first received 22 March 2017). [NCT03087578] [sr-incont76095]
Wen 2020 {published data only}
- Ning L, Qian W, ChiCTR1800019928. Clinical study for relieving symptoms of moderate and severe overactive bladder by electroacupuncture [Efficacy evaluation for electroacupuncture in the treatment of neurogenic urinary retention and overactive bladder]. chictr.org.cn/showproj.aspx?proj=33670 (first received 9 December 2018). [ChiCTR1800019928] [sr-incont78573]
- Wen Q, Li N, Wang X, Li H, Tian F, Chen W, et al. Effect of electroacupuncture versus solifenacin for moderate and severe overactive bladder: a multi-centre, randomized controlled trial study protocol. BMC Complementary Medicine and Therapies 2020;20(1):224. [ChiCTR1800019928] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Abrams 2012
- Abrams P, Chapple CR, Jünemann KP, Sharpe S. Urinary urgency: a review of its assessment as the key symptom of the overactive bladder syndrome. World Journal of Urology 2012;30(3):385-92. [DOI] [PubMed] [Google Scholar]
Abrams 2017
- Abrams P, Cardozo L, Wagg A, Wein A. Incontinence: 6th International Consultation on Incontinence. Bristol (UK): ICI-ICS. International Continence Society, 2017. [ISBN: 978-09569607-3-3] [Google Scholar]
Al‐Janabi 2013
- Al-Janabi H, Peters TJ, Brazier J, Bryan S, Flynn TN, Clemens S, et al. An investigation of the construct validity of the ICECAP - a capability measure. Quality of Life Research 2013;22(7):1831-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aluko 2022
- Aluko P, Graybill E, Craig D, Henderson C, Drummond M, Wilson EC, et al, on behalf of the Campbell and Cochrane Economics Methods Group. Chapter 20: Economic evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Avery 2004
- Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourology and Urodynamics 2004;23(4):322-30. [DOI: 10.1002/nau.20041] [DOI] [PubMed] [Google Scholar]
Clarkson 2015
- Clarkson CE, O'Mahony D, Jones DE. Adverse event reporting in studies of penetrating acupuncture during pregnancy: a systematic review. Acta Obstetricia et Gynecologica Scandinavica 2015;94(5):453-64. [DOI: 10.1111/aogs.12587] [DOI] [PubMed] [Google Scholar]
Covidence [Computer program]
- Covidence. Version accessed 2 January 2020. Melbourne, Australia: Veritas Health Innovation. Available at covidence.org.
CRD 2015
- Centre for Reviews and Dissemination (CRD). CRD database: search strategies. 2015. crd.york.ac.uk/crdweb/ (accessed 14 June 2019).
Deng 2015
- Deng S, Zhao X, Du R, He SI, Wen Y, Huang L, et al. Is acupuncture no more than a placebo? Extensive discussion required about possible bias. Experimental and Therapeutic Medicine 2015;10(4):1247-52. [DOI: 10.3892/etm.2015.2653] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dhond 2008
- Dhond RP, Witzel T, Hämäläinen M, Kettner N, Napadow V. Spatiotemporal mapping the neural correlates of acupuncture with MEG. Journal of Alternative and Complementary Medicine 2008;14(6):679-88. [DOI: 10.1089/acm.2007.0824] [DOI] [PMC free article] [PubMed] [Google Scholar]
Duthie 2011
- Duthie JB, Vincent M, Herbison GP, Wilson DI, Wilson D. Botulinum toxin injections for adults with overactive bladder syndrome. Cochrane Database of Systematic Reviews 2011, Issue 12. Art. No: CD005493. [DOI: 10.1002/14651858.CD005493.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
EndNote 2018 [Computer program]
- EndNote. Version X8.2. Philadelphia (PA): Clarivate Analytics, 2018.
Forde 2016
- Forde JC, Jaffe E, Stone BV, Te AE, Espinosa G, Chughtai B. The role of acupuncture in managing overactive bladder; a review of the literature. International Urogynecology Journal 2016;27(11):1645-51. [DOI: 10.1007/s00192-015-2935-y] [DOI] [PubMed] [Google Scholar]
Ganz 2010
- Ganz ML, Smalarz AM, Krupski TL, Anger JT, Hu JC, Wittrup-Jensen KU, et al. Economic costs of overactive bladder in the United States. Urology 2010;75(3):526-32, 532.e1-18. [DOI: 10.1016/j.urology.2009.06.096] [DOI] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Version accessed 2 January 2020. Hamilton (ON): McMaster University (developed by Evidence Prime). Available at gradepro.org.
Gray 2015
- Gray SL, Anderson ML, Dublin S, Hanlon JT, Hubbard R, Walker R, et al. Cumulative use of strong anticholinergics and incident dementia: a prospective cohort study. JAMA Internal Medicine 2015;175(3):401-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Herbison 2009
- Herbison GP, Arnold EP. Sacral neuromodulation with implanted devices for urinary storage and voiding dysfunction in adults. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No: CD004202. [DOI: 10.1002/14651858.CD004202.pub2] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2019
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated August 2019). Cochrane, 2019. Available from training.cochrane.org/handbook.
Hiller 2002
- Hiller L, Radley S, Mann CH, Radley SC, Begum G, Pretlove SJ, et al. Development and validation of a questionnaire for the assessment of bowel and lower urinary tract symptoms in women. BJOG 2002;109(4):413-23. [DOI] [PubMed] [Google Scholar]
Hino 2010
- Hino K, Honjo H, Nakao M, Kitakoji H. The effects of sacral acupuncture on acetic acid-induced bladder irritation in conscious rats. Urology 2010;75(3):730-4. [DOI] [PubMed] [Google Scholar]
Hu 2003
- Hu TW, Wagner TH, Bentkover JD, LeBlanc K, Piancentini A, Stewart WF, et al. Estimated economic costs of overactive bladder in the United States. Urology 2003;61(6):1123-8. [DOI] [PubMed] [Google Scholar]
Huang 2012
- Huang W, Pach D, Napadow V, Park K, Long X, Neumann J, et al. Characterizing acupuncture stimuli using brain imaging with FMRI--a systematic review and meta-analysis of the literature. PLOS One 2012;7(4):e32960. [DOI] [PMC free article] [PubMed] [Google Scholar]
Irwin 2006
- Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. European Urology 2006;50(6):1306-14; discussion 1314-5. [DOI] [PubMed] [Google Scholar]
Jimenez‐Cidre 2015
- Jimenez-Cidre MA, Lopez-Fando L, Esteban-Fuertes M, Prieto-Chaparro L, Llorens-Martinez FJ, Salinas-Casado J, et al. The 3-day bladder diary is a feasible, reliable and valid tool to evaluate the lower urinary tract symptoms in women. Neurourology and Urodynamics 2015;34(2):128-32. [DOI] [PubMed] [Google Scholar]
Lai 2016
- Lai HH, Shen B, Rawal A, Vetter J. The relationship between depression and overactive bladder/urinary incontinence symptoms in the clinical OAB population. BMC Urology 2016;16(1):60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lim 2019
- Lim R, Liong ML, Lim KK, Leong WS, Yuen KH. The minimum clinically important difference of the International Consultation on Incontinence Questionnaires (ICIQ-UI SF and ICIQ-LUTSqol). Urology 2019;133:91-5. [DOI] [PubMed] [Google Scholar]
Maciocia 2007
- Maciocia G. The practice of Chinese medicine: the treatment of diseases with acupuncture and Chinese herbs. 2nd edition. London (UK): Churchill Livingstone, 2007. [ISBN: 9780443074905] [Google Scholar]
MacPherson 2001
- MacPherson H, Thomas K, Walters S, Fitter M. The York acupuncture safety study: prospective survey of 34 000 treatments by traditional acupuncturists. BMJ 2001;323(7311):486-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
MacPherson 2010
- MacPherson H, Altman DG, Hammerschlag R, Youping L, Taixiang W, White A, et al, on behalf of the STRICTA Revision Group. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. PLOS One 2010;7(6):e1000261. [DOI: 10.1371/journal.pmed.1000261] [PMC2882429] [DOI] [PMC free article] [PubMed] [Google Scholar]
Madhuvrata 2012
- Madhuvrata P, Cody JD, Ellis G, Herbison GP, Hay-Smith EJ. Which anticholinergic drug for overactive bladder symptoms in adults. Cochrane Database of Systematic Reviews 2012, Issue 1. Art. No: CD005429. [DOI: 10.1002/14651858.CD005429.pub2] [DOI] [PubMed] [Google Scholar]
Malde 2018
- Malde S, Fry C, Schurch B, Marcelissen T, Averbeck M, Digesu A, et al. What is the exact working mechanism of botulinum toxin A and sacral nerve stimulation in the treatment of overactive bladder/detrusor overactivity? ICI-RS 2017. Neurourology and Urodynamics 2018;37(S4):S108-16. [DOI] [PubMed] [Google Scholar]
Napadow 2013
- Napadow V, Lee J, Kim J, Cina S, Maeda Y, Barbieri R, et al. Brain correlates of phasic autonomic response to acupuncture stimulation: an event-related fMRI study. Human Brain Mapping 2013;34(10):2592-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
NICE 2019
- National Institute for Health and Care Excellence (NICE). Urinary incontinence and pelvic organ prolapse in women: management. NICE guideline [NG123]. Published: 2 April 2019; last updated: 24 June 2019. Available at nice.org.uk/guidance/ng123 (accessed 6 November 2019).
Ou 2019
- Ou MJ, Huang CC, Wang YC, Chen YL, Ho CH, Wu MP, et al. Depression is a major risk factor for the development of dementia in people with lower urinary tract symptoms: A nationwide population-based study. PLOS One 2019;14(6):e0217984. [DOI] [PMC free article] [PubMed] [Google Scholar]
Powell 2018
- Powell LC, Szabo SM, Walker D, Gooch K. The economic burden of overactive bladder in the United States: a systematic literature review. Neurourology and Urodynamics 2018;37(4):1241-9. [DOI: 10.1002/nau.23477] [DOI] [PubMed] [Google Scholar]
Pullman 2016
- Pullman M. Acupuncture for urogenital conditions. In: Filshie J, White A, Cummings M, editors(s). Medical Acupuncture: a Western Scientific Approach. 2nd edition. London (UK): Elsevier Health Sciences, 2016:475-86. [ISBN: 0702068551, 9780702068553] [Google Scholar]
Rabin 2001
- Rabin R, Charro F. EQ-5D: a measure of health status from the EuroQol Group. Annals of Medicine 2001;33(5):337-43. [DOI] [PubMed] [Google Scholar]
Rantell 2017
- Rantell A, Cardozo L, Khullar V. Personal goals and expectations of OAB patients in the UK. Neurourology and Urodynamics 2017;36(4):1194-200. [DOI] [PubMed] [Google Scholar]
RevMan Web 2020 [Computer program]
- Review Manager Web (RevManWeb). Version 2.3.0. The Cochrane Collaboration, 2020. Available at revman.cochrane.org.
Schünemann 2019
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from training.cochrane.org/handbook.
Sexton 2011
- Sexton CC, Coyne KS, Thompson C, Bavendam T, Chen CI, Markland A. Prevalence and effect on health-related quality of life of overactive bladder in older Americans: results from the epidemiology of lower urinary tract symptoms study. Journal of the American Geriatrics Society 2011;59(8):1465-70. [DOI] [PubMed] [Google Scholar]
Stata 2019 [Computer program]
- Stata. Version 16. College Station, TX, USA: StataCorp LLC, 2019. Available at www.stata.com.
Tse 2016
- Tse V, King J, Dowling C, English S, Gray K, Millard R, et al. Conjoint Urological Society of Australia and New Zealand (USANZ) and Urogynaecological Society of Australasia (UGSA) Guidelines on the management of adult non-neurogenic overactive bladder. BJU International 2016;117(1):34-47. [DOI] [PubMed] [Google Scholar]
Tubaro 2004
- Tubaro A. Defining overactive bladder: epidemiology and burden of disease. Urology 2004;64(6 Suppl 1):2-6. [DOI] [PubMed] [Google Scholar]
Wallace 2004
- Wallace SA, Roe B, Williams K, Palmer M. Bladder training for urinary incontinence in adults. Cochrane Database of Systematic Reviews 2004, Issue 1. Art. No: CD001308. [DOI: 10.1002/14651858.CD001308.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2012
- Wang H, Tanaka Y, Kawauchi A, Miki T, Kayama Y, Koyama Y. Acupuncture of the sacral vertebrae suppresses bladder activity and bladder activity-related neurons in the brainstem micturition center. Neuroscience Research 2012;72(1):43-9. [DOI] [PubMed] [Google Scholar]
Ware 1992
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care 1992;30(6):473-83. [PubMed] [Google Scholar]
Wein 2009
- Wein AJ, Coyne KS, Tubaro A, Sexton CC, Kopp ZS, Aiyer LP. The impact of lower urinary tract symptoms on male sexual health: EpiLUTS. BJU International 2009;103(Suppl 3):33-41. [DOI] [PubMed] [Google Scholar]
White 2009
- White A, Editorial Board of Acupuncture in Medicine. Western medical acupuncture: a definition. Acupuncture in Medicine 2009;27(1):33-5. [DOI] [PubMed] [Google Scholar]
Witt 2009
- Witt CM, Pach D, Brinkhaus B, Wruck K, Tag B, Mank S, et al. Safety of acupuncture: results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forschende Komplementärmedizin 2009;16(2):91-7. [DOI] [PubMed] [Google Scholar]
Zhao 2018
- Zhao Y, Zhou J, Mo Q, Wang Y, Yu J, Liu Z. Acupuncture for adults with overactive bladder: a systematic review and meta-analysis of randomized controlled trials. Medicine 2018;97(8):e9838. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Hargreaves 2020
- Hargreaves E, Baker K, Barry G, Harding C, Zhang Y, Kandala NB, et al. Acupuncture for treating overactive bladder in adults. Cochrane Database of Systematic Reviews 2020, Issue 1. Art. No: CD013519. [DOI: 10.1002/14651858.CD013519] [DOI] [PMC free article] [PubMed] [Google Scholar]


