Abstract
School-related factors may influence retention in care and adherence to antiretroviral therapy (ART) among adolescents with human immunodeficiency virus (HIV). We analyzed data from in-depth interviews with 40 adolescents with HIV (aged 14 -19 years), 40 caregivers of adolescents with HIV, and 4 focus group discussions with healthcare workers to evaluate contextual factors affecting adherence to ART and clinic attendance among adolescents, with a focus on the school environment. Informed by Anderson’s Model of Health Services Utilization, transcripts were systematically coded and synthesized to identify school-related themes. All groups identified the school environment as a critical barrier to engagement in HIV care and medication adherence for adolescents with HIV. Adolescent participants reported inflexible school schedules and disclosure to school staff as the biggest challenges adhering to clinic appointments and ART. Adolescents described experiencing stigma and discrimination by peers and school staff and would adjust when, where and how often they took ART to avoid inadvertent disclosure. Boarding school students faced challenges because they had limited private space or time. Caregivers were often instrumental in navigating school permissions, including identifying a treatment supporter among school staff. Additional research engaging school staff may guide interventions for schools to reduce stigma and improve adherence and retention.
Introduction
In 2019, there were an estimated 1.7 million adolescents with human immunodeficiency virus (HIV), 170 000 new HIV infections and 33 000 deaths from acquired immune deficiency syndrome (AIDS)-related causes among adolescents aged 10–19 years [1]. The majority of adolescents with HIV (88%) live in sub-Saharan Africa [1]. Adolescents have suboptimal HIV testing, linkage to care, antiretroviral therapy (ART) coverage and lower rates of viral suppression compared with other groups [2, 3]. In Kenya, almost 40% of adolescents are not virally suppressed [4], and the population of adolescents with HIV is continuing to grow through a combination of incident infections among adolescents, as well as perinatally infected children aging into adolescence [5]. There is an expected lag of two decades before the number of perinatally infected adolescents decreases, highlighting the need for interventions addressing the challenges adolescents face [6].
Adolescence is a time of transition, including physical, psychosocial, emotional and cognitive changes as adolescents work toward independence [7]. For adolescents with HIV, these changes are compounded with the challenges of living with a chronic illness. Adolescents with HIV can experience poor growth, delayed pubertal development, chronic skin manifestations caused by HIV and physical changes associated with medication use, all of which may result in low self-esteem, depression and substance abuse [6, 8]. Additionally, adolescents typically transition from pediatric to adult HIV care and move from primary to secondary school during this time period. These contemporaneous changes can pose significant challenges to adolescents with HIV and contribute to decreased engagement in care and ART adherence [9, 10]. Existing interventions have not fully addressed the unique challenges adolescents face in managing their HIV disease during these transitions.
In 2016, 67% of adolescents in Kenya were enrolled in secondary school [11]. Although attending secondary school is an important milestone in adolescent development, the school context poses substantial challenges to ongoing engagement in care and adherence to ART, particularly for youth attending boarding schools [12]. For example, adolescents with HIV may miss classes to attend clinic, making it harder for them to excel in school. Conversely, rigid class schedules may pose challenges to consistent adherence to ART and clinic visits. Interventions tailored for adolescents with HIV attending school are necessary to address challenges with adherence [10, 12–14]. Understanding the specific barriers adolescents with HIV encounter and how they navigate them can inform the development of interventions tailored to adolescents with HIV attending school.
Health service utilization and health behaviors are often influenced by multiple barriers and facilitators and their complex interactions. Andersen’s Model of Health Services Utilization provides a framework to categorize how population, environmental and behavioral characteristics interact to influence health services utilization [15]. We conducted a secondary analysis of qualitative data using Anderson’s Model to characterize how the school environment interacts with population characteristics and affects adherence to ART and clinic attendance among adolescents with HIV in Kenya.
Methods
This secondary analysis used data collected from the Public Health Adolescent Services Evaluation (PHASE), a mixed methods evaluation of adolescent HIV services in Kenya. PHASE sought to assess the provision of HIV care, including adolescent-friendly services, and the uptake and acceptability of an Adolescent Package of Care (APOC). Quantitative data were collected from a nationally representative random sample of 102 large (>300 total patients) HIV care facilities. In addition to quantitative data, the evaluation included in-depth interviews (IDIs) with adolescents with HIV (aged 14–19) and primary caregivers of adolescents with HIV (aged 10–19), as well as focus group discussions (FGDs) with healthcare workers, from a subset of four facilities.
Data collection
Qualitative data were collected between February and March of 2017 from a subset of four PHASE evaluation facilities, two medium (456–866 patients) and two large (>869 patients), selected to capture variation in services by facility size. All four facilities were located in Western Kenya, the only region that had implemented APOC at the time of the study. A total of 10 IDIs with adolescents with HIV, 10 IDIs with caregivers of adolescents with HIV and 1 FGD with healthcare workers were conducted at each of the four facilities. Eligible adolescents with HIV were identified by healthcare workers at facilities and referred to study interviewers. Disclosure of HIV status and age were the primary criteria for inclusion. HIV disclosure was verified by healthcare workers prior to referral and again by interviewers prior to conducting interviews. For participants who met inclusion criteria, adolescents with HIV and caregiver participants were purposively recruited based on facility visit timing, with those having already scheduled visits during interview weeks being prioritized. All healthcare workers involved in providing adolescent services at selected facilities were invited to participate.
IDIs and FGDs used pilot-tested, semi-structured question guides that focused on understanding experiences with HIV care and treatment for adolescents with HIV in Kenya. Question guides explored topics, including HIV disclosure, barriers and facilitators to seeking and receiving HIV treatment services and the role of relationships in caring for adolescents with HIV. FGDs and IDIs were facilitated by trained Kenyan social scientists and conducted in the language preferred by study participants (English, Dholuo, Kiswahili or a combination of those languages). FGDs lasted ∼2 h and IDIs ∼60 min. All FGDs and IDIs were audio recorded, translated when necessary and transcribed verbatim.
Ethical approval
All study participants provided written informed consent if ≥18 years of age. Participants who were 14–17 years of age provided written assent, and their parent or guardian provided written consent.
Data analysis
In this secondary analysis, transcripts were analyzed using directed content analysis techniques, based on Andersen’s Model [15, 16]. Andersen’s Model was used to create broad categories of codes related to environmental and population characteristics of adolescents with HIV influencing adherence to medication and clinic visits. Inductive methods were used to identify specific factor codes falling within broader contextual and population categories that were derived directly from the transcripts (Fig. 1).
Fig. 1.
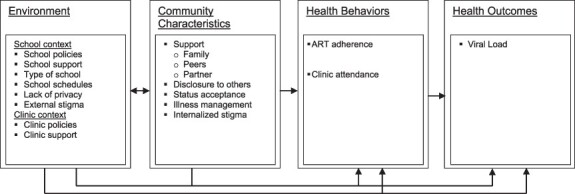
Adapted Andersen’s Model (analysis model).
The codebook was tested and refined through an iterative process of reviewing transcripts against the developing codebook and making revisions to ensure that all emerging concepts and themes were captured. Once the codebook had been finalized, transcripts were evenly divided between four coders (K.B.-S., S.L., K.W. and H.M.) and independently coded using ATLAS.ti (ATLAS.ti 8 Scientific Software Development GmbH). Coders exchanged and reviewed one another’s coded transcripts and noted discrepancies in code application and interpretation. Differences in code application and interpretation were reviewed and revised as a group. Queries were applied to coded transcripts to identify divergent and convergent themes. Thematic network analysis was used to group and visualize barriers and facilitators within and between the levels of Andersen’s Model [17, 18].
Results
Participant characteristics
Overall, 40 adolescents with HIV and 40 caregivers participated in IDIs, and 39 healthcare workers participated in 4 FGDs. A detailed description of participant demographic details have been previously published [19]. Briefly, the median age of adolescent participants was 16 years, and the majority were female (68%), consistent with East African HIV distribution between males and females [1]. All adolescents with HIV were currently enrolled in HIV care, and all but four were currently attending school. The majority of adolescents with HIV were enrolled in primary school class 7 (20%) or class 8 (25%) or in secondary school form 1 or 2 (25%). Caregivers had a median age of 46 years, and the majority (83%) were female. Most caregivers were parents (60%), with the remainder representing grandparents (13%), aunts/uncles (10%) and others (13%). Healthcare workers represented a range of cadres, including nurses, counselors and clinical officers, and a majority (74%) were female. Healthcare workers were a median age of 33 years and had a median of 3 years (IQR: 1–6) of experience providing care to adolescents with HIV. Healthcare workers had worked at current facilities for a median of 2 years.
Facilitators and barriers to adherence
Andersen’s Model facilitated the characterization of school-related barriers and facilitators that adolescents with HIV, caregivers and healthcare workers identified as affecting ART adherence and retention in care. Barriers were categorized into the specific model domains of school context, clinic context and community characteristics, as described later.
School context
Participants described how school policies, many developed before HIV and designed to promote student safety, could lead to challenges adhering to medication or lead to inadvertent or forced disclosure of HIV status. This was especially true for adolescents attending boarding school, where dorm and locker searches, as well as lack of privacy in dorm rooms, made it challenging to keep medication use private. In order to keep their living with HIV a secret, adolescents sometimes hid in the bathroom stalls to take their medication, discarded medication or did not take medication while attending school.
Many participants described how school policies required that adolescents store medications with school nurses, forcing disclosure of HIV status even if adolescents were not ready or did not feel comfortable disclosing. Adolescents feared that school nurses would not keep their information private and noted how daily visits with the nurse to take medications could inadvertently disclose their status to others.
“People are always wondering the kind of the disease that I suffer from that I have to see the nurse every night.” (17-year-old female)
Adolescents attending boarding schools who felt uncomfortable storing medications with school nurses described the challenges of trying to keep medications with them in their dorm rooms. Adolescents feared inadvertent disclosure through other students noticing the frequency with which they took pills.
“[H]iding the drugs is very difficult. You are supposed to take your drugs but maybe your friends are there. How will you do it if they don’t know that you [are living with HIV]?” (17-year-old male)
“Adolescents who are in boarding school, you find that most of them, they usually have high viral loads, and the reason is when they are in school, they are with others and they do not want to take their medication when others are observing them. So, they don’t adhere in fear of what their classmates and friends will say.” (Female healthcare worker)
Dorm and locker searches were described as common practice, and when medications were found during searches, school staff sometimes asked questions about the medications and why they had been hidden, leading to fear and anxiety about forced disclosure.
“A child is in school, and maybe the school authorities are not aware that maybe the child is in [HIV] care, so the child carries the drugs to school and maybe when they are doing the search in the dorms, the matron finds the drugs and takes them away.” (35-year-old female caregiver)
“Sometimes they do a search, and if they find you with drugs, you have to explain.” (35-year-old female caregiver)
Many adolescents noted fears of experiencing discrimination from other students if their status was discovered. A few adolescent participants experienced rumors being spread about them throughout the school and noted how this negatively influenced their life.
“Even when in school when you tell your friends about it, some change or even abuse you in reference to the drugs.” (14-year-old female)
“They can stigmatize you until anything that you touch, even a basin, they just throw it away saying that this one is sick, and she wants to infect us.” (46-year-old female caregiver)
Determining which school staff to trust and choosing whom to disclose was an ongoing challenge for adolescents with HIV. Many adolescents feared that if they shared their positive status with staff, they would spread rumors or tell other students. Deciding who to tell was often based on necessity and the person’s position in the school to avoid repercussions if the medications were found. The headmaster or matron was identified by many participants as someone commonly disclosed to because of his/her position of authority and ability to avoid problems during dorm searches.
“I go to the deputy, because my mum told the deputy that I usually come for checkup, so he gives me permission…, but I have always wanted to tell my class teacher about it.” (18-year-old female)
Adolescents and healthcare workers described the need for school staff to be informed about HIV care practices and the need for confidentiality and flexibility for adolescents with HIV attending school.
“School principals and the teachers should be empowered on how to handle the HIV positive adolescents in the school so that if at all they happen to have a child like that, they can help in monitoring maybe how the child is coming to the clinic and how the child is taking drugs and such.” (Female healthcare worker)
Confronted with rigid class schedules and long commuting times, adolescents described a lack of control over maintaining their medication schedule consistently.
“The problem is with the timing of taking the medication while he is in school because sometimes the teacher is in class and he doesn’t want anyone to move out of class…then he will have to pretend that he is going to the toilet so as to take his medication.” (46-year-old female caregiver)
In addition to the lack of privacy in the school environment making it difficult for adolescents with HIV to adhere to their medication, participants also struggled with being forced to take pills on empty stomachs due to school mealtimes. Side effects of some ART medications, including drowsiness, made it challenging to identify the ideal time to take medications, and medication side effects negatively influenced attending classes.
“I do feel very dizzy when I take this pill. I take my pills at 10pm, [and] it needs that I rest a lot but in school we wake up at around 4am. I still do feel dizzy, thus sometimes [it] makes me to miss going for my dawn classes.” (17-year-old female)
Clinic context
Clinic schedules and services that were not organized around school schedules negatively influenced adolescent adherence to clinic visits—for example, adolescent clinic days scheduled during the school week. Respondents from one facility mentioned how they had been helped when the adolescent clinic was moved to a weekend, although this was not always helpful since some adolescents still attended school activities on weekends. Clinic attendance during exam times was reported as being especially challenging, with many adolescents and caregivers having to choose between taking the exams and missing clinic.
“The common reason why I may miss coming [to clinic] is that sometimes I could be sitting for my exams and I have a clinic appointment and probably at that time I was not aware that we were going to have exams. So, you know I can’t miss sitting for my exams because I should be coming for my clinic visit; so sometimes I may postpone coming for my clinic visit with even two days until Saturday.” (16-year-old male)
Most adolescents with HIV reported being reluctant, or unable, to obtain permission to miss classes to attend clinic. When granted permission to attend clinic visits, adolescent and caregiver participants complained that they would often miss a full day of class because of long wait times at the facility.
“I used to face a lot of challenges because I could miss lessons each time I came for my visit, so that made other students to be ahead of me in class.” (16-year-old female)
Having clinic staff provide holistic, multi-level support for adolescents improved clinic attendance. Healthcare workers described taking time to contact caregivers when adolescents did not come to clinic and providing adolescents with adherence support to strategize medicine taking and manage drug side effects to minimize nonadherence.
“You know when I was introduced to them [ART] they told us that they have some side effects, so they encouraged us to be taking them when going to bed. Like when you are in school you should be going on with your lessons. So, for not interfering with your lessons because you are [being] affected, you take them after your preps then you sleep.” (17-year-old female)
Community characteristics
At the community level, adolescents relied heavily on support from caregivers to navigate barriers to adherence. Caregivers played a strong role in supporting both day and boarding students in the challenges they faced in school by disclosing the adolescent’s status to teachers for them.
“Because I go to school early, I take [my ART medicines] at 6……On the first day my grandfather talked to the head teacher and asked for my permission to leave school 10–15 minutes earlier even if the teacher is in class.” (14-year-old female)
Even caregivers who did not initially disclose their adolescent’s HIV status realized over time that it was in the adolescent’s best interest to disclose
“Yeah it was a challenge so taking it was such a big challenge now it just forced me to go to school and disclose and they told me that they have a lot of girls who are on care, so it was not an issue.” (46-year-old female caregiver)
Personal relationships and the emotional support adolescents received from caregivers, teachers and clinic staff were important in adolescents gaining the confidence and motivation to accept and manage their HIV status and cope with the stigma they faced
“The last topic that I remember us [adolescent and caregiver] talking about is that I should now learn to take care of myself. So, from that talk I got encouraged and I started having that positive… attitude. So, when I went back to school, I said to myself that there was nothing to worry about, it was all about my life and I have to live it as it is.” (19-year-old female)
Discussion
We found that different categories of barriers to health service utilization influenced health outcomes individually and also interacted and influenced one another. In this study, interactions between community characteristics and clinic and school contexts either facilitated or hindered adherence. Conflicts in scheduling between school and clinic contexts negatively affected clinic attendance by forcing adolescents to choose between clinic attendance and exams. Adherence was negatively affected by lack of disclosure, often due to fears of discrimination and stigma experienced post disclosure. School policies on medication storage that led to inadvertent or forced disclosure posed further barriers to medication adherence. Relationships with caregivers and healthcare workers and the support adolescents gained from them helped overcome school-related clinic attendance and mediation adherence barriers. Caregivers were an important source of support in disclosing the adolescents’ status to school staff and making arrangements that helped adolescents adhere to both medications and clinic visits. Adolescents gained advice about how to take medication to avoid disclosure or side effects from healthcare workers and received encouragement around status acceptance from caregivers.
Other studies have identified aspects of school as drivers of adolescent nonadherence, loss to follow-up and quality of life due to lack of privacy in boarding schools leading to inadvertent disclosure, stigma and discrimination [8, 10, 12–14]. Similar to our findings, other studies have also shown that side effects from medications, such as dizziness and nausea, also lead to missed classes and nonadherence [8, 10, 12–14]. Inaccurate HIV knowledge among teachers and lack of appropriate training to prepare them to educate adolescents about HIV have contributed to stigma within schools, and even policies intended to help adolescents with HIV in boarding schools, such as school staff holding medications or a student’s status being shared with teachers who are expected to provide support, can have negative effects [12, 13, 20].
Class schedules can be a barrier to clinic attendance, particularly for adolescents in boarding schools due to strict absenteeism rules and distance to clinics [10, 12, 13]. Another study also identified that nonadherence occurred when school and clinic schedules clashed [13]. Studies have explored the community or household context but have not compared barriers between these contexts and school [10, 12, 13]. Students attending boarding school struggle more than those living at home to adhere to ART due to the absence of the same social support they receive when home [14].
Our results showed that adolescents and their caregivers view status disclosure as both a positive and negative experience. Disclosure to school staff was recognized as key to garnering necessary support for medication and treatment adherence, but disclosure to the ‘wrong’ staff member could lead to stigmatizing reactions, including discrimination and judgment from friends and peers. While our data demonstrated that caregivers played a large role in disclosure for their adolescents, a systematic review focusing on the quality of life for adolescents with HIV failed to identify this theme in any of the included studies [12].
Our study had limitations. First, due to the recruitment process, all adolescents in this study had the support of a caregiver, which resulted in excluding perspectives of adolescents with HIV who have not disclosed to their caregivers and adolescents who are unaware of their HIV status. Second, discussion guides were written to identify general barriers and facilitators in adolescents’ lives that helped or hindered adherence. Although it was discussed at length by many participants, the study did not explicitly focus on the impact of the school environment on adolescent adherence in its question guides, demonstrating the strong impact of school on adolescent adherence. Finally, study participants were recruited from a small subset of health facilities in Western Kenya, and their experiences navigating school attendance may not be representative of all adolescents attending schools in Kenya. Strategic sampling to characterize school-going experiences from adolescents in other regions in Kenya may provide alternative perspectives on barriers and facilitators within the school environment.
Conclusion
School and clinic contexts, along with interpersonal interactions between adolescents with HIV and their caregivers, strongly influence an adolescent’s ability to adhere to both medication and clinic visits while they are attending school. This demonstrates the importance of involving adolescents with HIV, as well as school administrators and teachers, healthcare workers and caregivers in the development of interventions to safely optimize adherence among school-going adolescents with HIV. The negative experiences we observed illustrate barriers (such as stigma and the lack of control adolescents have over their school schedule) affecting some adolescents with HIV attending school. Given the complexity of these challenges, solutions will need to be multifaceted, including the engagement of policy makers to prioritize these young people’s health and safety, training for teachers to reduce stigma and provide support and encouraging healthcare facilities to work to accommodate school schedules. The positive experiences that some adolescents with HIV describe of gaining the necessary support in schools provide potential ‘best practice’ scenarios that could be replicated in other schools through training school and clinic staff. Through participatory research and further stakeholder engagement with Kenyan educators, policy makers, healthcare workers and adolescents, it will be important to develop effective strategies to address confidentiality, stigma and clinic/school scheduling conflicts.
Acknowledgements
We thank the PHASE study adolescents, caregivers and healthcare workers, without whom this research would not have been possible. We also thank the PHASE study team members and the University of Washington’s Global Center for Integrated Health of Women, Adolescents, and Children.
Contributor Information
Lisa Wiggins, Department of Child Family and Population Health Nursing.
Gabrielle O’Malley, Department of Global Health, University of Washington, Seattle, Washington.
Anjuli D Wagner, Department of Global Health, University of Washington, Seattle, Washington.
Immaculate Mutisya, Division of Global HIV & Tuberculosis, U.S. Centers for Disease Control and Prevention, Nairobi, Kenya.
Kate S Wilson, Department of Global Health, University of Washington, Seattle, Washington.
Sarah Lawrence, Department of Global Health, University of Washington, Seattle, Washington.
Hellen Moraa, Department of Pediatrics, University of Nairobi, Nairobi, Kenya.
John Kinuthia, Department of Research and Programs, Kenyatta National Hospital, Nairobi, Kenya.
Janet Itindi, Centre for Clinical Research, Kenya Medical Research Institute, Nairobi, Kenya.
Odylia Muhenje, Division of Global HIV & Tuberculosis, U.S. Centers for Disease Control and Prevention, Nairobi, Kenya.
Tai-Ho Chen, Division of Global HIV & Tuberculosis, U.S. Centers for Disease Control and Prevention, Nairobi, Kenya.
Benson Singa, Centre for Clinical Research, Kenya Medical Research Institute, Nairobi, Kenya.
Christine J Mcgrath, Department of Global Health, University of Washington, Seattle, Washington.
Evelyn Ngugi, Division of Global HIV & Tuberculosis, U.S. Centers for Disease Control and Prevention, Nairobi, Kenya.
Abraham Katana, Division of Global HIV & Tuberculosis, U.S. Centers for Disease Control and Prevention, Nairobi, Kenya.
Lucy Ng′ang′a, Division of Global HIV & Tuberculosis, U.S. Centers for Disease Control and Prevention, Nairobi, Kenya.
Grace John-Stewart, Department of Global Health, University of Washington, Seattle, Washington; Department of Epidemiology, University of Washington, Seattle, Washington; Department of Pediatrics, University of Washington, Seattle, Washington; Department of Medicine, University of Washington, Seattle, Washington.
Pamela Kholer, Department of Child Family and Population Health Nursing; Department of Global Health, University of Washington, Seattle, Washington.
Kristin Beima-Sofie, Department of Global Health, University of Washington, Seattle, Washington.
Funding
U.S. President’s Emergency Plan for AIDS Relief through the Centers for Disease Control and Prevention (NU2GGH002034, INU2GGH001956, U2GPS002047); National Institute of Mental Health (K01MH121124) to A.D.W.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the funding agencies.
References
- 1. United Nations Children’s Fund (UNICEF) . Adolescent HIV Prevention. Available at: https://data.unicef.org/topic/hivaids/adolescents-young-people/. Accessed: 5 January 2019.
- 2. Wood SM, Dowshen N, Lowenthal E. Time to improve the global human immunodeficiency virus/AIDS care continuum for adolescents: a generation at stake. JAMA Pediatr 2015; 169: 619–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zanoni BC, Archary M, Buchan S et al. Systematic review and meta-analysis of the adolescent HIV continuum of care in South Africa: the Cresting Wave. BMJ Glob Heal 2016; 1: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. NASCOP . Kenphia 2018 Preliminary Report. NASCOP. 2020; 1–26.doi: 10.1017/CBO9781107415324.004 [DOI]
- 5. UNICEF . Cross-Sector Indicators. 2018. Available at: https://data.unicef.org/resources/data_explorer/unicef_f/?ag=UNICEF&df=GLOBAL_DATAFLOW&ver=1.0&dq=.HVA_EPI_INF_ANN_15-24._T.&startPeriod=2015&endPeriod=2018. Accessed: 4 September 2020.
- 6. Lowenthal ED, Bakeera-kitaka S, Marukutira T et al. Perinatally acquired HIV infection in adolescents from sub-Saharan Africa : a review of emerging challenges. Lancet Infect Dis 2014; 14: 627–39.doi: 10.1016/S1473-3099(13)70363-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sanders RA. Adolescent psychosocial, social, and cognitive development. Pediatr Rev 2013; 34: 354–9. [DOI] [PubMed] [Google Scholar]
- 8. Gaitho D, Kumar M, Wamalwa D et al. Understanding mental health difficulties and associated psychosocial outcomes in adolescents in the HIV clinic at Kenyatta National Hospital, Kenya. Ann Gen Psychiatry 2018; 17: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Koech E, Teasdale CA, Wang C et al. Characteristics and outcomes of HIV-infected youth and young adolescents enrolled in HIV care in Kenya. AIDS (London, England) 2014; 28: 2729–38.doi: 10.1097/QAD.0000000000000473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wolf HT, Halpern-Felsher BL, Bukusi EA et al. “It is all about the fear of being discriminated [against]⋯the person suffering from HIV will not be accepted”: a qualitative study exploring the reasons for loss to follow-up among HIV-positive youth in Kisumu, Kenya. BMC Public Health 2014; 14: 1–11.doi: 10.1186/1471-2458-14-1154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ministry of Education R of K, UNICEF . Basic Education Stastics Booklet. 2014.
- 12. Kimera E, Vindevogel S, De Maeyer J et al. Challenges and support for quality of life of youths living with HIV/AIDS in schools and larger community in East Africa: a systematic review. Syst Rev 2019; 8: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Madiba S, Josiah U. Perceived stigma and fear of unintended disclosure are barriers in medication adherence in adolescents with perinatal HIV in Botswana: a qualitative study. Biomed Res Int 2019; 2019: 1–9.doi: 10.1155/2019/9623159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mutwa PR, Van Nuil JI, Asiimwe-Kateera B et al. Living situation affects adherence to combination antiretroviral therapy in HIV-infected adolescents in Rwanda: a qualitative study. PLoS One 2013; 8: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav 1995; 36: 1–10. [PubMed] [Google Scholar]
- 16. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005; 15: 1277–88. [DOI] [PubMed] [Google Scholar]
- 17. Attride-Sterling J. Thematic networks: an analytical tool for qualitative research. Qual Res 2001; 1: 385–405. [Google Scholar]
- 18. Andersen RM, Andersen R. National Health Surveys and the Behavioral Model of Health Services Use. 2008; 46. Available at: https://about.jstor.org/terms. Accessed: 21 January 2020. [DOI] [PubMed] [Google Scholar]
- 19. Lawrence S, Moraa H, Wilson K et al. “They just tell me to abstain:” variable access to and uptake of sexual and reproductive health services among adolescents living with HIV in Kenya. Front Reprod Heal 2021; 3: 1–10.doi: 10.3389/frph.2021.644832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Njue C, Nzioka C, Ahlberg B et al. “If you don’t abstain, you will die of AIDS”: AIDS education in Kenyan public schools. AIDS Educ Prev 2009; 21: 169–79. [DOI] [PubMed] [Google Scholar]


