Abstract
Background: Polymethyl methacrylate (PMMA) is used in fabricating acrylic denture bases. Repairing a fractured acrylic denture base can be done by self-cured PMMA, yet this is still a weak point after repair. The aim of this study was to evaluate the effect of incorporating 5% weight titanium oxide nanoparticles (TiO2) to self-cured PMMA on flexural strength, surface micro-hardness, roughness, and water sorption. Methods: A total of 160 acrylic–resin specimens were used in this study. They were divided in two main groups; (a) control group, prepared by mixing self-cured PMMA powder to its liquid monomer, (b) treated group, prepared by blending 5% weight TiO2 nanoparticles to self-cured PMMA powder then this blend was mixed with the liquid monomer. Flexure strength, surface micro-hardness, roughness, and water sorption were evaluated. Data were analyzed using independent sample t-tests (p ≤ 0.05). Results: There was a significant increase in the flexural strength of PMMA of the treated group after the addition of TiO2 (137.6 MPa) compared with the control (75.4 MPa) (p ≤ 0.001). No significant difference between the two groups in terms of micro-hardness (p = 0.385) and surface roughness (p = 0.269). Water sorption showed a significant reduction in the treated group (p ≤ 0.001). Conclusions: Addition of 5% weight TiO2 nanoparticles to the self-cured acrylic resin improved its flexural strength and reduced its water-sorption without impairing the surface micro-hardness and roughness.
Keywords: polymethyl methacrylate (PMMA), flexural strength, micro-hardness, surface roughness, water sorption, titanium oxide nanoparticles, self-cure acrylic resin
1. Introduction
Polymers represent a widespread material used in the dental field [1,2,3]. Acrylic resins are one of the most used materials for removable denture base constructions. Heat or self-cured acrylic resins are composed of polymethyl methacrylate (PMMA). Denture base fabrication depends mainly on heat-cured acrylic resin. Denture repairs are carried out by self-cured acrylic resin to avoid warpage and destruction of the fractured parts of the denture [4,5]. Fractures of denture bases may happen inside the mouth mostly due to high flexural stresses occurring during mastication on a long-term service [6]. However, fracture outside the mouth is mainly by accident such as the dropping of the denture [7]. Repairing or rebasing of the fractured denture base by self-cured (chemical cured) acrylic resins is considered a good approach, thus preserving time and costs if deciding to construct a new denture [8].
Acrylic denture base fractures mainly arise from impact and or flexure forces. An impact force may cause denture fracture when sudden dropping occurs. Fracture of dentures due to flexure force could happen on repeated flexing [9]. Despite the desired properties of PMMA, there is a great demand for improvement of their mechanical properties [10].The minimal standard limit for flexural strength of the acrylic resin should be no less than 50 MPa according to the ISO international standard for dentistry base polymers [11]. The higher the flexural strength, the more prolonged the clinical service lifespan of the denture [12].
Self-cured acrylic resin is one of the most used denture repair materials. The flexural strength of self-cured acrylic resins is lower than that of the heat-cured type; therefore, recurring fractures can be predicted. Concern should be shown to modifying the repaired dentures through reinforcement of the repairing materials [13].
There have been many attempts to reinforce PMMA-based materials by incorporating fillers into their composition. The use of fibers, ceramics or metals to PMMA produces beneficial effects [14,15,16,17,18]. The introduction of nanotechnology offers a new approach for the enhancement of the mechanical properties of polymers [10,19,20]. Particularly, the incorporation of hard and strong nano-filler particles into the polymeric matrix affects significantly the mechanical properties and structural integrity of the polymeric-based dental materials [14,15].
Heat-cured PMMA acrylic resins tried to be reinforced in previous studies. However, there are few studies conducted about the reinforcement of self-cured PMMA acrylic [21,22,23,24]. Modifications have been done to improve the flexural strength of self-cured acrylic denture base material to counteract the problem of their great possibility to fracture [25]. One approach to strengthening the PMMA material is by addition of rubber in what is called a high-impact denture base to avoid fracture under impact force [26]. Another approach depends on the addition of reinforcement materials such as aluminum oxides and glass fiber nanoparticles [25,27,28].
Although there are many types of nano-metals such as silver and cobalt–chromium, titanium dioxide (TiO2) nanoparticles have a great value due to their cardinal features, such as: being non-toxic; safe; chemically inert; having antimicrobial properties; having high flexural strength; fracture toughness; and micro-hardness [29,30,31].
Flexural strength of acrylic denture bases is considered as an important factor of clinical failure [30,32]. Therefore, a high mechanical strength property of denture base materials is considered the most important requirement for successful denture base materials [33]. Micro-hardness indicates the abrasiveness of the denture base material. The surface properties of acrylic denture bases are affected by micro-hardness, which denote resistance to scratching during service and upon denture cleansing [34]. Moreover, surface roughness and irregularities of a PMMA denture base promotes stains and plaque accumulation affecting negatively the aesthetics and biological properties of acrylic denture with time [35]. In addition, water sorption by polymeric matrix of denture has a detrimental effect on mechanical properties of acrylic denture base, thus it should be minimal [18].
There is insufficient data on the impact of the addition of TiO2 nanoparticle on the mechanical and physical properties of the self-cured acrylic resin used for denture repair or rebase. Thus, the aim of this study was to evaluate the effect of incorporation of 5% weight TiO2 nanoparticles on the mechanical properties of self-cured PMMA regarding flexural strength, surface micro-hardness, roughness, and water sorption.
The null hypothesis is that addition of 5% TiO2 nanoparticles does not change the flexural strength of the self-cured PMMA in comparison to the unmodified group.
2. Materials and Methods
Self-cured acrylic resin was used in this study (Acrostone Cold Cure Acrylic Resin, Acrostone Co., London, UK). TiO2 nanoparticles were purchased from Sigma Aldrich (Sigma-Aldrich Chemie GmbH, Schnelldorf, Germany) with an average particle size < 25 nm. A total of 160 acrylic–resin specimens were used in this study. They were divided in two main groups; (a) the control group was prepared by mixing self-cured PMMA powder to its liquid monomer in ratio 3:1 by volume according to the manufacturer’s instructions, (b) the treated group was prepared by adding 5% TiO2 nanoparticles to self-cured PMMA powder (95%) (by weight). Manual mixing was performed by blending the two powders by rotation motion for 10 min using a spatula, followed by shaking in a sealed container for an additional 10 min. Then, the blended powder was added as one unit to liquid monomer in a ratio 3:1 by volume as previously mentioned.
When the mixed acrylic resin reached the dough stage, it was packed in special molds according to the test. According to the manufacture, the polymerization process was carried out for 10 min, after that the prepared specimens were removed out of the molds and visually inspected to verify the presence of a smooth and flat surface, showing no defects, voids, or porosity; otherwise, they were discarded. After that, the specimens were immersed in distilled water at 37 °C for 24 h before testing [18,36].
The parameters measured in this study were flexural strength, surface micro-hardness, roughness and water sorption. For each test, 20 specimens were prepared from each group (control and treated).
2.1. Flexural Strength Test
The flexural strength was determined by a 3-point bending flexural strength test in accordance with ISO 20795-1 [11,18]. Specimens of 64 mm (length) × 10 mm (width) × 3.3 mm (thickness) were prepared using stainless [11,18]. The specimens were investigated using a universal testing machine (Model 3345; Instron Industrial Products, Norwood, MA, USA) with two supports 20 mm apart, at a crosshead speed of 5 mm/min. The load at fracture was recorded in Newtons (N) and the flexural strength (FS) was calculated in MPa with the following equation [18,37]:
| FS = PL/wb2, | (1) |
where; (P) is the maximum load at fracture, (L) is the distance between the supports (=20 mm), (w) is the specimen thickness, and (b) is the height. The specimens’ measurement was done with a digital caliper.
2.2. Micro-Hardness Test
Surface micro-hardness was determined using Digital Vickers hardness tester (NEXUS 400TM, INNOVATEST, model no. 4503, Maastricht, The Netherlands). Specimens of dimension (65 mm × 10 mm × 2.5 mm) were fabricated in a stainless-steel mold [27,38]. The indentations were made within 20 s from the loading 500 g at 20× magnification [27,38].
The Vickers micro-hardness number (VHN) value was calculated automatically using the equation:
| VHN = 1.8544 P/d2 | (2) |
where; (P) is the applied force in kilogram, (d) is the mean of the two diagonals gained from the indentation in mm.
2.3. Surface Examination and Surface Roughness Test
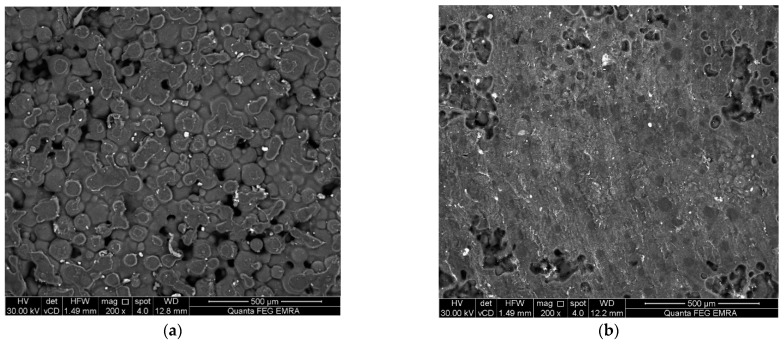
The morphology of the surfaces was examined using non-destructive environmental scanning electron microscopy (Model Quanta 250 FEG, FEI company, Eindhoven, The Netherlands) with 200× magnification [39,40]. Disc specimens were obtained from a stainless-steel mold (10 mm diameter × 2 mm height) [41]. The same specimens were then used for the surface roughness test using the SEM micrograph [42,43,44]. SEM images were converted into 3rd dimension images by imaging analysis system Scandium Solution Height (Olympus soft imaging solutions, GMBH, Muenster, Germany). The average surface roughness values of each specimen (Ra) were recorded.
2.4. Water Sorption Evaluation
The water sorption test was accomplished by the preparation of disc specimens (50 mm diameter and 0.5 mm in thickness) [31]. Specimens were placed inside a desiccator containing a dried silica gel and stored in an incubator (CBM, S.r.l. Medical Equipment, 2431/V, Cremona, Italy) at 37 ± 1° for 24 h. Specimens were weighed using an electronic balance (Adam equipment 4 digits precision weighing balance, Adam Equipment Inc., Oxford, UK) until their weight was constant. The initial weight was termed as W1 (μg). Specimens were then immersed in distilled water at 37 ± 1 °C and stored into the incubator for 15 days [45]. Specimens were removed from the water, gently dried with an absorbent paper and air sprayed for 15 s. Specimens were weighed again and were termed as W2 (μg).
The diameter and thickness of each specimen was measured by digital caliper. The volume (V) of each specimen was calculated following equations:
| V = π × r2 × h | (3) |
where r is the mean specimen radius (diameter/2) in millimeters and h is the mean specimen thickness in millimeters.
The water sorption was attained from the difference between the initial and wet weighing (W2 − W1). The values of water sorption (Wsp) in μg/mm3, for each specimen were calculated using the following equations:
| Wsp = (W2 − W1)/V | (4) |
2.5. Statistical Analysis
The statistical analysis was performed using the Statistical Package for the Social Sciences (IBM SPSS Statistics for Windows, Version 23.0, IBM Corporation, Armonk, NY, USA). An independent sample t-test was used to compare mean values of flexural strength between two groups (control PMMA and treated PMMA with TiO2). The significance level was set at p ≤ 0.05. Similarly, the same test was used to compare the results of micro-hardness as well as surface roughness and water sorption between the two groups.
3. Results
The mean, standard deviation values for flexural strength (MPa), Vickers micro-hardness number (VHN), SEM surface examination images, 3-D surface roughness (Ra), and water sorption (μg/mm3) are presented in Table 1 and Figure 1, Figure 2 and Figure 3. There was a significant increase in flexural strength of PMMA of the treated group after the addition of TiO2 (137.6 MPa) compared with the control group (75.4 MPa). No significant difference was seen between the two groups in results of micro-hardness as well as surface roughness. On the other hand, the water sorption showed a significant reduction after the addition of TiO2 (0.36 µg/mm3), in comparison to the control group.
Table 1.
Mean and standard deviation values of flexural strength, micro-hardness, surface rough-ness and water sorption tests of the two groups.
| Test/Group | Control Group | Treated Group | p Value |
|---|---|---|---|
| Flexural strength (MPa) | 75.4 ± 2.1 | 137.6 ± 3.2 | ≤0.001 * |
| Micro-hardness (VHN) | 15 ± 1.3 | 15.7 ± 0.8 | 0.385 |
| Surface roughness (Ra) | 16 ± 2.8 | 13.7 ± 3.2 | 0.269 |
| Water sorption (μg/mm3) | 0.63 ± 0.01 | 0.36 ± 0.01 | ≤0.001 * |
*: significant (p < 0.05).
Figure 1.
Representative 3-D surface roughness images (Ra) (a) control group; (b) Treated group.
Figure 2.
Representative SEM micrographs (200× magnification) (a) control group; (b) Treated group.
Figure 3.
Representative SEM micrographs (500× magnification) (a) control group; (b) Treated group.
Moreover, SEM micrograph showed that the surface of non-treated specimens (control) exhibited a honeycomb appearance and porous surface. Meanwhile, the treated specimens (filled with TiO2) demonstrated a less porous surface compared with the control.
4. Discussion
The effect of addition of TiO2 nanoparticle on flexural strength of PMMA depends on both concentration of nanoparticles and their interaction with the acrylic resin polymer. The ideal concentration of the fillers is still under investigation [46].
A previous study investigating the interaction between TiO2 nanoparticle and PMMA found that TiO2 nanoparticles interact chemically with PMMA through their reaction with the ester functional group COOR (oxygen double-bound to carbon–carbonyl along with an OR group attached to the same carbon). The ester is a carboxylic acid derivative in which the OH is replaced by and OR (oxygen reaction variable). Moreover, the loading of TiO2 nanoparticles within the resinous matrix hinders polymer chain movements due to the strong bond between the TiO2 nanoparticle and PMMA providing a cross-linking action [47].
In this study, the null hypothesis is rejected, as the treated PMMA by addition of 5% weight TiO2 nanoparticles showed higher flexural strength than the control group. These values exceed the minimum requirements of flexural strength which is not less than 50 MPa [11]. This may be due to the chemical and physical interaction between TiO2 nanoparticles and PMMA as mentioned earlier.
Surface hardness and roughness of the denture are two crucial factors to avoid scratching of denture on service or collection of food, bacterial and fungal to avoid their adhesion to denture surface with subsequent candidiasis and inflammation [48]. Recent investigation suggested the addition of 5% TiO2 nanoparticle which was considered suitable to raise conventional and high impact heat cured acrylic resin surface hardness to significant values [30,49].
The micro-hardness and surface roughness revealed no significant difference among all tested groups which may be attributed to the low concentration of the homogenously blended TiO2 nano-sized particles fillers within the polymer matrix. There was no statistically significant difference in the surface roughness values among all tested groups, but the reduced surface roughness in the treated groups may be beneficial to decrease the possibilities of stains and plaque accumulation.
The SEM micrograph of the control specimens displayed a honeycomb appearance with an irregular and porous structure. This may be attributed to the presence of pre-polymerized PMMA beads region as a major component of PMMA powder surrounded by in-situ PMMA which was formed by the polymerization reaction of methyl methacrylate monomer liquid. The SEM micrograph of treated specimens displayed a homogenous less porous structure. This can be explained by the uniform distribution of the titanium dioxide nanoparticle fillers within the polymer matrix.
The nature of the denture base resin material allows some degree of water sorption. Water molecules entrances and acts as a plasticizer that affects the dimensional stability and durability of the denture base [50]. The water sorption was evaluated by the increase in mass per unit volume. According to ISO standards 1567:1999 specification, water sorption for heat-cured or self-cured materials should not exceed 32 μg/mm3 [50,51].
The decrease in water sorption in the treated group may be attributed to the fact that the addition of TiO2 nanoparticles to acrylic–resin spaces reduces the ability of the treated PMMA denture base to absorb water molecules due to their cross-linking effects of TiO2 nanoparticles. Furthermore, TiO2 nanoparticles are considered an insoluble hydrophobic element [52].
Despite the rise in the flexural strength of PMMA modified by the addition of 5% TiO2 nanoparticles, the manual blending of the two powders may exert some limitations in the conducted research.
5. Conclusions
Addition of 5% weight TiO2 nanoparticles to dental self-cured acrylic PMMA resin improved its flexural strength and reduced its water sorption without the impairment of the surface micro-hardness and roughness.
Author Contributions
Conceptualization, R.M.A. and T.M.H.; data curation, T.M.H.; formal analysis, R.E.B. and T.M.H.; funding acquisition, R.M.A. and R.E.B.; investigation, T.M.H.; methodology, T.M.H.; supervision, R.M.A., R.E.B. and T.M.H.; writing—original draft, T.M.H.; writing—review and editing; R.M.A., R.E.B. and T.M.H. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abdelraouf R.M. Chemical analysis and microstructure examination of extended-pour alginate impression versus conventional one (characterization of dental extended-pour alginate) Int. J. Polym. Mater. Polym. Biomater. 2018;67:612–618. doi: 10.1080/00914037.2017.1362636. [DOI] [Google Scholar]
- 2.Abdelraouf R.M., Bayoumi R.E., Hamdy T.M. Effect of powder/water ratio variation on viscosity, tear strength and detail reproduction of dental alginate impression material (In vitro and clinical study) Polymers. 2021;13:2923. doi: 10.3390/polym13172923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abdelraouf R.M., Mohammed M., Abdelgawad F. Evaluation of shear-bond-strength of dental self-adhering flowable resin-composite versus total-etch one to enamel and dentin surfaces: An in-vitro study. Open Access Maced. J. Med. Sci. 2019;7:2162–2166. doi: 10.3889/oamjms.2019.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hadi A.F., Jassim M.M., HA M. Evaluating some Mechanical and Physical Properties of Vertex Thermosens Denture base Material in Comparison with Heat Cure Acrylicdenture Base Material. Int. J. Sci. Res. 2017;6:394–397. doi: 10.21275/ART20172925. [DOI] [Google Scholar]
- 5.Hamouda I.M. Retention of Probase Hot Versus the Conventional Heat-Cured Acrylic Resin Denture Bases. Biomed. J. Sci. Tech. Res. 2017;1:906–911. doi: 10.26717/BJSTR.2017.01.000329. [DOI] [Google Scholar]
- 6.Minami H., Suzuki S., Kurashige H., Minesaki Y., Tanaka T. Flexural strengths of denture base resin repaired with autopolymerizing resin and reinforcements after thermocycle stressing. J. Prosthodont. 2005;14:12–18. doi: 10.1111/j.1532-849X.2005.00006.x. [DOI] [PubMed] [Google Scholar]
- 7.Alhareb A.O., Akil H.M., Ahmad Z.A. Impact strength, fracture toughness and hardness improvement of PMMA denture base through addition of nitrile rubber/ceramic fillers. Saudi J. Dent. Res. 2017;8:26–34. doi: 10.1016/j.sjdr.2016.04.004. [DOI] [Google Scholar]
- 8.DAR-ODEH N.S., HARRISON A., ABU-HAMMAD O. An evaluation of self-cured and visible light-cured denture base materials when used as a denture base repair material. J. Oral Rehabil. 2008;24:755–760. doi: 10.1111/j.1365-2842.1997.tb00272.x. [DOI] [PubMed] [Google Scholar]
- 9.Choksi R.H., Mody P.V. Flexural properties and impact strength of denture base resins reinforced with micronized glass flakes. J. Indian Prosthodont. Soc. 2016;16:264–270. doi: 10.4103/0972-4052.176532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Naji S.A., Behroozibakhsh M., Kashi T.S.J., Eslami H., Masaeli R., Mahgoli H., Tahriri M., Lahiji M.G., Rakhshan V. Effects of incorporation of 2.5 and 5 wt% TiO2 nanotubes on fracture toughness, flexural strength, and microhardness of denture base poly methyl methacrylate (PMMA) J. Adv. Prosthodont. 2018;10:113–121. doi: 10.4047/jap.2018.10.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dentistry—Base Polymers—Part 1: Denture Base Polymers. 2nd ed. International Organization for Standardization; Geneva, Switzerland: 2013. [(accessed on 7 September 2022)]. 35p. Available online: https://www.iso.org/obp/ui/#iso:std:iso:20795:-1:ed-2:v1:en. [Google Scholar]
- 12.Meng T.R., Latta M.A. Physical properties of four acrylic denture base resisns. J. Contemp. Dent. Pract. 2005;6:93–100. doi: 10.5005/jcdp-6-4-93. [DOI] [PubMed] [Google Scholar]
- 13.Ibrahim M.H., Alaa M. Effect of aluminum oxide powder reinforcement on degree of conversion, monomer release and flexural strength of heat-cured acrylic resin. Biomed. Res. Clin. Rev. 2020;1:1–5. doi: 10.31579/2692-9406/020. [DOI] [Google Scholar]
- 14.Zaki D.Y., Safwat E.M., Nagi S.M., Salem H.N., Hamdy T.M., Moharam L.M., Hassan M.L., Hamzawy E.M.A. A novel dental re-mineralizing blend of hydroxyethyl-cellulose and cellulose nanofibers oral film loaded with nepheline apatite glass: Preparation, characterization and in vitro evaluation of re-mineralizing effect. Carbohydr. Polym. Technol. Appl. 2021;2:100035. doi: 10.1016/j.carpta.2021.100035. [DOI] [Google Scholar]
- 15.Hamdy T.M., Mousa S.M.A., Sherief M.A. Effect of Incorporation of Lanthanum and Cerium-doped Hydroxyapatite on Acrylic Bone Cement Produced from Phosphogypsum Waste. Egypt. J. Chem. 2019;63:1823–1832. doi: 10.21608/ejchem.2019.17446.2069. [DOI] [Google Scholar]
- 16.Abdelnabi A., Hamza M.K., El-Borady O.M., Hamdy T.M. Effect of Different Formulations and Application Methods of Coral Calcium on its Remineralization Ability on Carious Enamel. Open Access Maced. J. Med. Sci. 2020;8:94–99. doi: 10.3889/oamjms.2020.4689. [DOI] [Google Scholar]
- 17.Hamdy T.M. Polymerization shrinkage in contemporary resin-based dental composites: A Review Article. Egypt. J. Chem. 2021;64:3087–3092. doi: 10.21608/ejchem.2021.60131.3286. [DOI] [Google Scholar]
- 18.Fonseca R.B., Kasuya A.V.B., Favarão I.N., Naves L.Z., Hoeppner M.G. The influence of polymerization type and reinforcement method on flexural strength of acrylic resin. Sci. World J. 2015;2015:919142. doi: 10.1155/2015/919142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gad M.M., Fouda S.M., Al-Harbi F.A., Näpänkangas R., Raustia A. PMMA denture base material enhancement: A review of fiber, filler, and nanofiller addition. Int. J. Nanomed. 2017;12:3801–3812. doi: 10.2147/IJN.S130722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hamdy T.M., Saniour S.H., Sherief M.A., Zaki D.Y. Effect of incorporation of 20 wt% amorphous nano-hydroxyapatite fillers in poly methyl methacrylate composite on the compressive strength. Res. J. Pharm. Biol. Chem. Sci. 2015;6:1136–1141. doi: 10.5281/zenodo.4399399. [DOI] [Google Scholar]
- 21.Alhotan A., Yates J., Zidan S., Haider J., Silikas N. Flexural strength and hardness of filler-reinforced pmma targeted for denture base application. Materials. 2021;14:2659. doi: 10.3390/ma14102659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tandra E., Wahyuningtyas E., Sugiatno E. The effect of nanoparticles TiO2 on the flexural strength of acrylic resin denture plate. Padjadjaran J. Dent. 2018;30:35. doi: 10.24198/pjd.vol30no1.16110. [DOI] [Google Scholar]
- 23.Alqahtani M. Mechanical properties enhancement of self-cured PMMA reinforced with zirconia and boron nitride nanopowders for high-performance dental materials. J. Mech. Behav. Biomed. Mater. 2020;110:103937. doi: 10.1016/j.jmbbm.2020.103937. [DOI] [PubMed] [Google Scholar]
- 24.Kumar G.V.S., Nigam A., Naeem A., Gaur A., Pandey K.K., Deora A. Reinforcing heat-cured poly-methyl-methacrylate resins using fibers of glass, polyaramid, and nylon: An in vitro study. J. Contemp. Dent. Pract. 2016;17:948–952. doi: 10.5005/jp-journals-10024-1960. [DOI] [PubMed] [Google Scholar]
- 25.Vijay A., Prabhu N., Balakrishnan D., Narayan A.I. Comparative study of the flexural strength of high impact denture base resins reinforced by silver nanoparticles and e-glass fibres: An in-vitro study. J. Clin. Diagn. Res. 2018;12:22–26. doi: 10.7860/JCDR/2018/36931.12285. [DOI] [Google Scholar]
- 26.Faot F., Panza L.H.V., Garcia R.C.M.R., Cury A.A.D.B. Impact and Flexural Strength, and Fracture Morphology of Acrylic Resins With Impact Modifiers. Open Dent. J. 2009;3:137–143. doi: 10.2174/1874210600903010137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Farina A.P., Cecchin D., Soares R.G., Botelho A.L., Takahashi J.M.F.K., Mazzetto M.O., Mesquita M.F. Evaluation of Vickers hardness of different types of acrylic denture base resins with and without glass fibre reinforcement. Gerodontology. 2012;29:e155–e160. doi: 10.1111/j.1741-2358.2010.00435.x. [DOI] [PubMed] [Google Scholar]
- 28.Vojdani M., Bagheri R., Khaledi A.A.R. Effects of aluminum oxide addition on the flexural strength, surface hardness, and roughness of heat-polymerized acrylic resin. J. Dent. Sci. 2012;7:238–244. doi: 10.1016/j.jds.2012.05.008. [DOI] [Google Scholar]
- 29.Hamdy T.M., Galal M., Ismail A.G., Abdelraouf R.M. Evaluation of flexibility, microstructure and elemental analysis of some contemporary nickel-titanium rotary instruments. Open Access Maced. J. Med. Sci. 2019;7:3647–3654. doi: 10.3889/oamjms.2019.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ashour Ahmed M., El-Shennawy M., Althomali Y.M., Omar A.A. Effect of Titanium Dioxide Nano Particles Incorporation on Mechanical and Physical Properties on Two Different Types of Acrylic Resin Denture Base. World J. Nano Sci. Eng. 2016;6:111–119. doi: 10.4236/wjnse.2016.63011. [DOI] [Google Scholar]
- 31.Nevarez-Rascón A., Hurtado-Macías A., Esparza-Ponce H.E., Nevarez-Rascón M.M., González-Hernández J., Yacamán M.J. Nano-structured hydroxyapatite and titanium dioxide enriching PENTA /UDMA adhesive as aesthetic coating for tooth enamel. Dent. Mater. 2021;37:e290–e299. doi: 10.1016/j.dental.2021.01.019. [DOI] [PubMed] [Google Scholar]
- 32.Yadav N.S., Elkawash H. Flexural strength of denture base resin reinforced with aluminum oxide and processed by different processing techniques. J. Adv. Oral Res. 2011;2:33–36. doi: 10.1177/2229411220110107. [DOI] [Google Scholar]
- 33.Lee H.H., Lee C.J., Asaoka K. Correlation in the mechanical properties of acrylic denture base resins. Dent. Mater. J. 2012;31:157–164. doi: 10.4012/dmj.2011-205. [DOI] [PubMed] [Google Scholar]
- 34.Bahrani F., Vojdani M., Safari A., Karampoor G. Comparison of Hardness and Surface Roughness of Two Denture bases Polymerized by Different Methods. World J. Dent. 2012;3:171–175. doi: 10.5005/jp-journals-10015-1151. [DOI] [Google Scholar]
- 35.Kumar G.V., Devi R., Anto N. Evaluation and Comparison of the Surface Roughness and Porosity of Different Provisional Restorative Materials: An in vitro Study. CODS J. Dent. 2016;8:39–45. doi: 10.5005/jp-journals-10063-0010. [DOI] [Google Scholar]
- 36.Tolga Demirtaş T., Kaynak G., Gümüşderelioğlu M. Bone-like hydroxyapatite precipitated from 10×SBF-like solution by microwave irradiation. Mater. Sci. Eng. C. 2015;49:713–719. doi: 10.1016/j.msec.2015.01.057. [DOI] [PubMed] [Google Scholar]
- 37.Fonseca R.B., Favarão I.N., Kasuya A.V.B., Abrão M., da Luz N.F.M., Naves L.Z. Influence of Glass Fiber wt% and Silanization on Mechanical Flexural Strength of Reinforced Acrylics. J. Mater. Sci. Chem. Eng. 2014;2:11–15. doi: 10.4236/msce.2014.22003. [DOI] [Google Scholar]
- 38.Shah J., Bulbule N., Kulkarni S., Shah R., Kakade D. Comparative evaluation of sorption, solubility and microhardness of heat cure polymethylmethacrylate denture base resin & flexible (thermoplastic polyamide nylon) denture base resin. J. Clin. Diagn. Res. 2014;8:ZF01. doi: 10.7860/JCDR/2014/8707.4770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gad M.M., Rahoma A., Al-Thobity A.M., ArRejaie A.S. Influence of incorporation of ZrO2 nanoparticles on the repair strength of polymethyl methacrylate denture bases. Int. J. Nanomed. 2016;11:5633–5643. doi: 10.2147/IJN.S120054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Al-Kheraif A.A.A. The effect of mechanical and chemical polishing techniques on the surface roughness of heat-polymerized and visible light-polymerized acrylic denture base resins. Saudi Dent. J. 2014;26:56–62. doi: 10.1016/j.sdentj.2013.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yahya N.A., Gonzalez M.A., Ibrahim M.S., Wen Y.K. Surface Roughness of Tooth Coloured Restorative Materials. Ann. Dent. 2020;27:41–49. doi: 10.22452/adum.vol27no7. [DOI] [Google Scholar]
- 42.Paluszyński J., Slówko W. Measurements of the surface microroughness with the scanning electron microscope. J. Microsc. 2009;233:10–17. doi: 10.1111/j.1365-2818.2008.03090.x. [DOI] [PubMed] [Google Scholar]
- 43.Van Pham K., Vo C.Q. A new method for assessment of nickel-titanium endodontic instrument surface roughness using field emission scanning electronic microscope. BMC Oral Health. 2020;20:240. doi: 10.1186/s12903-020-01233-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Martelo J.B., Andersson M., Liguori C., Lundgren J. Three-dimensional scanning electron microscopy used as a profilometer for the surface characterization of polyethylene-coated paperboard. Nord. Pulp Pap. Res. J. 2021;36:276–283. doi: 10.1515/npprj-2021-0003. [DOI] [Google Scholar]
- 45.Tekale R., Mowade T., Radke U. Comparative evaluation of water sorption of heat-polymerized polymethyl methacrylate denture base resin reinforced with different concentrations of silanized titanium dioxide nanoparticles: An in vitro study. Contemp. Clin. Dent. 2019;10:269–273. doi: 10.4103/ccd.ccd_499_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gad M.M., Abualsaud R. Behavior of PMMA denture base materials containing titanium dioxide nanoparticles: A literature review. Int. J. Biomater. 2019;2019:6190610. doi: 10.1155/2019/6190610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chatterjee A. Properties improvement of PMMA using nano TiO2. J. Appl. Polym. Sci. 2010;118:2890–2897. doi: 10.1002/app.32567. [DOI] [Google Scholar]
- 48.Kreve S., Dos Reis A.C. Denture Liners: A Systematic Review Relative to Adhesion and Mechanical Properties. Sci. World J. 2019;2019:6913080. doi: 10.1155/2019/6913080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hashem M., Al Rez M.F., Fouad H., Elsarnagawy T., Elsharawy M.A., Umar A., Assery M., Ansari S.G. Influence of titanium oxide nanoparticles on the physical and thermomechanical behavior of poly methyl methacrylate (pmma): A denture base resin. Sci. Adv. Mater. 2017;9:938–944. doi: 10.1166/sam.2017.3087. [DOI] [Google Scholar]
- 50.Tham W.L., Chow W.S., Ishak Z.A.M. Simulated body fluid and water absorption effects on poly(methyl methacrylate)/hydroxyapatite denture base composites. Express Polym. Lett. 2010;4:517–528. doi: 10.3144/expresspolymlett.2010.66. [DOI] [Google Scholar]
- 51.Dentistry—Denture Base Polymers. ISO; Geneva, Switzerland: 1999. [(accessed on 26 August 2022)]. Available online: https://www.iso.org/standard/20266.html. [Google Scholar]
- 52.Alwan S.A., Alameer S.S. The Effect of the Addition of Silanized Nano Titania Fillers on Some Physical and Mechanical Properties of Heat Cured Acrylic Denture Base Materials. J. Baghdad Coll. Dent. 2015;27:86–91. doi: 10.12816/0015269. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.