Abstract
Spinal muscular atrophy (SMA) is a devastating neuromuscular disorder caused by recessive mutations in the SMN1 gene, globally affecting ~8–14 newborns per 100,000. The severity of the disease depends on the residual levels of functional survival of motor neuron protein, SMN. SMN is a ubiquitously expressed RNA binding protein involved in a plethora of cellular processes. In this review, we discuss the effects of SMN loss on mitochondrial functions in the neuronal and muscular systems that are the most affected in patients with spinal muscular atrophy. Our aim is to highlight how mitochondrial defects may contribute to disease progression and how restoring mitochondrial functionality may be a promising approach to develop new therapies. We also collected from previous studies a list of transcripts encoding mitochondrial proteins affected in various SMA models. Moreover, we speculate that in adulthood, when motor neurons require only very low SMN levels, the natural deterioration of mitochondria associated with aging may be a crucial triggering factor for adult spinal muscular atrophy, and this requires particular attention for therapeutic strategies.
Keywords: mitochondria, spinal muscular atrophy, SMN1, SMN2, motor neuron diseases, neurodegeneration, cellular homeostasis, neurodegenerative diseases, oxidative stress, mitochondria biogenesis and dynamics
1. Introduction
Spinal muscular atrophy (SMA) is a genetically common autosomal recessively inherited motor neuron (MN) disease, which in its natural development causes early childhood lethality in approximately half of all SMA patients [1]. It affects the proximal voluntary muscles symmetrically and extends to the distal muscles as the disease progresses [2,3]. There is increasing evidence of multisystem involvement, particularly in its severe form of manifestation [4]. The age-of-onset of SMA is very broad, ranging from prenatal (type 0) to the first 6 months of life (type I), after 6 months of life (type II), after 18 months of life (type III) or after 25 years (type IV). Motoric abilities range from never able to sit or stand (type 0 and I), able to sit (type II) and able to walk (type III and IV) [2,3].
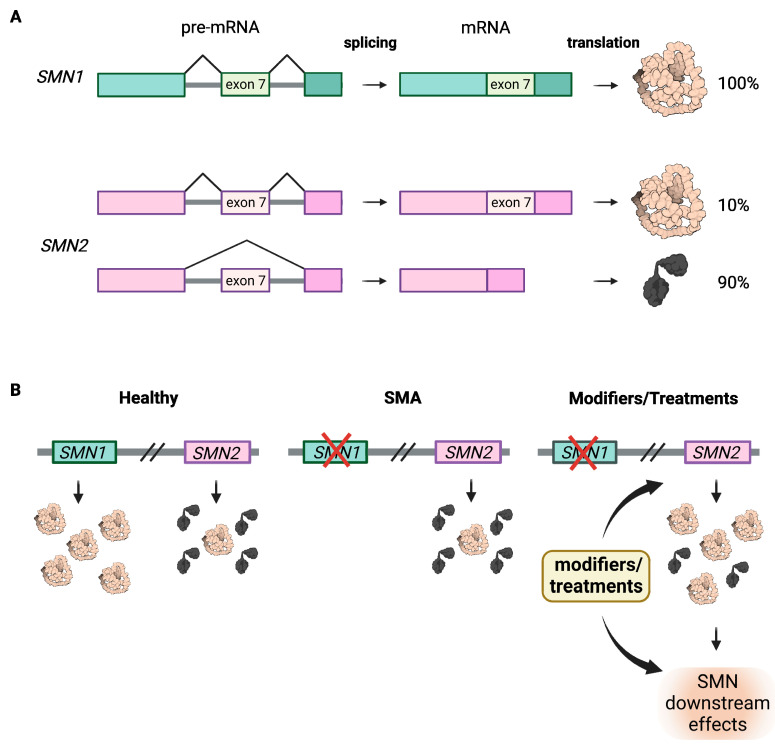
SMA is caused by homozygous loss of function of SMN1 [5], while disease severity is mainly determined by SMN2 copy number; both SMN genes are located close together on chromosome 5q13 [6,7]. SMN2 is an almost perfect copy of SMN1 with five nucleotide differences, only one of which is relevant as it affects splicing by disrupting an exonic splicing enhancer and creating a new exonic splicing silencer in exon 7 [8,9,10]. Consequently, 90% of SMN2 transcripts lack exon 7 and produce a protein that is truncated and unstable [11]. About 10% of SMN2 transcripts are correctly spliced and translated into a full-length protein identical to that produced by SMN1 (Figure 1A). However, the low SMN protein amount in patients cannot counteract the loss of SMN1, thus primarily affecting spinal motor neurons, which require high levels of SMN prenatally and in the first three months of life but very little in adolescence and adulthood [1,12].
Figure 1.
Genetic basis of SMA. (A) SMN1 and SMN2 genes are located on chromosome 5q13 and encode for SMN protein. In healthy conditions, the SMN1 pre-mRNA undergoes correct splicing, while SMN2 pre-mRNA mainly undergoes erroneous splicing, which results in the loss of the exon 7 and the translation of a truncated and non-functional SMN protein. (B) Healthy individual present physiological levels of SMN protein, deriving mainly from the SMN1 gene. In SMA patients, deletion of or missense mutations in SMN1 cause a dramatic reduction in SMN protein level that cannot be compensated by the SMN2 copy gene. The SMN protein levels can be (partially) restored by genetic modifiers or treatments that either boost the production of SMN protein (SMN2 copy number is a modifier in this sense) or act on the downstream functions of SMN to compensate its loss. The figure was created with BioReneder.com.
Although all SMA patients have a homozygous loss of functional SMN1, the copy number of SMN2 varies between 1–6, which is inversely correlated with disease severity [6,7]. The more SMN2 copies a patient has, the milder the phenotype. Therefore, SMN2 is the main modulator of the SMA disease phenotype and the main target for therapies (Figure 1B).
To date, three FDA- and EMA-approved drugs have been shown to be effective in ameliorating or restoring motor abilities, particularly if the therapy begins pre-symptomatically, as is the case when newborn screening has been implemented [13,14,15]. All three therapies aim to increase SMN levels, either through (i) antisense oligonucleotides that correct splicing by blocking an intronic silencer in intron 7 (intrathecal injection of nusinersen/Spinraza, Ionis Pharmaceuticals and Biogen), (ii) small molecules facilitating the recruitment of U1-snRNPs to the splice donor of intron 7 (systemic oral application of risdiplam/Evrisdy, Gentechen and Roche), or (iii) gene replacement therapy, using a self-complementary AAV9 expressing SMN1 cDNA under a strong ubiquitous promotor (systemic intravenous application of onasemnogene abeparvovec xioi/Zolgensma, AveXis and Novartis) [16,17,18,19,20,21].
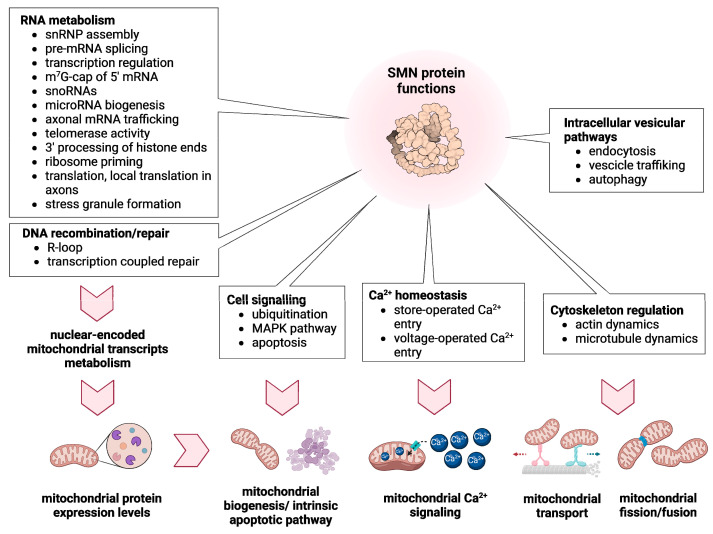
SMN is ubiquitously expressed but particularly high in the spinal cord [22,23] and has a plethora of housekeeping and cell-type specific functions, such as snRNP biogenesis, micro-RNA biogenesis, splicing, mRNA transport, translation, DNA-damage and degradation, R-loop formation, stress response, cell signaling, Ca2+ homeostasis, actin and microtubules dynamics, vesicle trafficking, autophagy, endocytosis and mitochondrial homeostasis (Figure 2) [13,24,25]. The SMN protein interacts directly or indirectly with >60 proteins [24,26]. This explains the dramatic effect seen in most cells, when levels drop below 10–20%, as in type 0 or I. However, when 30–40% of SMN remains, as in the case of SMA type II-IV, motor neurons are mainly affected, suggesting a very important and specific role of SMN in these cells [13]. Despite this, we still do not understand why certain motor neurons are more vulnerable than others are or why sensory neurons are not affected or are less affected than motor neurons, despite also having very long axons.
Figure 2.
Schematic summary of the known functions of SMN and their impact on mitochondrial homeostasis. As crucial regulator of RNA metabolism and DNA recombination/repair, SMN modulates the expression levels of many mitochondrial proteins that are essential for mitochondrial homeostasis (biogenesis, apoptosis induction, Ca2+ signaling, transport and dynamics). By interacting with a plethora of proteins, SMN is also involved in different cell signaling pathways and in the dynamic regulation of membranes and cytoskeleton. All these SMN functions are ultimately crucial for mitochondrial biogenesis, Ca2+ signaling, transport and dynamics. The figure was created with BioReneder.com.
Rarely, some individuals—most often siblings of SMA patients or parents of SMA children—carry homozygous SMN1 deletions and identical SMN2 copies as the affected sibling(s) but do not exhibit SMA symptoms, strongly indicating protection via SMA modifying gene (s). In humans, two protective modifiers/cellular processes have been reported so far: upregulation of plastin 3 (PLS3) and downregulation of neurocalcin delta (NCALD) [27,28,29]. PLS3 is an F-acting binding and bundling protein with an essential role in endocytosis, cell migration, Ca2+ homeostasis, translation and others [30], while NCALD is a neuronal calcium sensor protein involved in Ca2+ homeostasis, endocytosis and G-protein coupled receptor signaling transduction [29,31]. Both modifiers restore impaired endocytosis induced by reduced SMN levels and ameliorate the SMA phenotype not only in humans but across species [27,29,32,33,34]. A plethora of other potential SMA modifiers have been identified by genetic screens, protein interaction studies or pathway analysis, as described in detail in the following review [35].
Mitochondrial Function in SMA and SMA-Like Diseases
In recent years, an increasing number of studies, including clinical, structural and functional, have revealed various mitochondrial defects in motor neurons and muscles of many mammalian and non-mammalian SMA model systems. Mitochondria are crucial organelles present in eukaryotic cells that provide most of the cellular ATP supply. Mitochondrial ATP production occurs through a process called oxidative phosphorylation, mediated by the electron transport chain (ETC) complexes of the inner mitochondrial membrane. In addition to ATP production, mitochondria have many other important roles. They can store Ca2+ ions contributing to Ca2+ homeostasis and signaling, they are source of reactive oxygen species (ROS) and are the seat of many important metabolic pathways. Furthermore, mitochondria are crucial mediators of stress responses and cell death. Interestingly, in a recent study, we examined unsolved SMA-like cases by whole exome or whole genome sequencing, and in 47% of the solved cases we identified pathogenic variants in genes involved in mitochondrial dynamics (VPS13D, DNM1L), mtDNA replication and maintenance (POLG, MPV17), mitochondrial translation machinery (C12orf65) and respiratory chain (NDUFS6, FDXR, ECHS1) [36]. In other common neuromuscular disorders characterized by MN degeneration, such as amyotrophic lateral sclerosis (ALS) or Charcot-Marie-Tooth type II (axonal form), genes involved in mitochondrial function and biogenesis are often mutated [37,38,39]. These genetic associations strongly underlie and further support the essential role of mitochondria in motor neuron and muscle functionality.
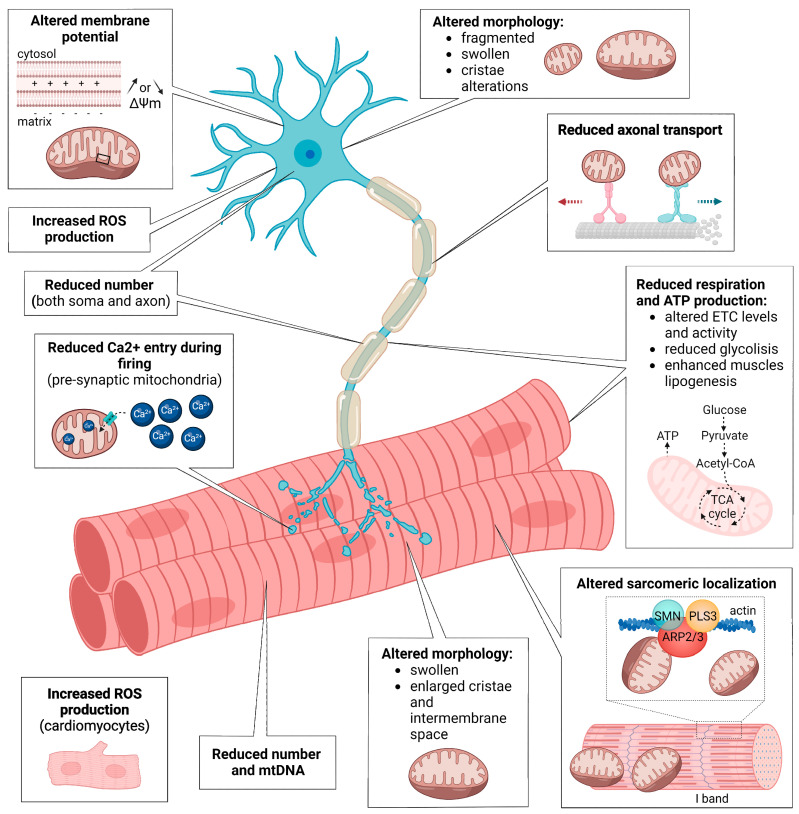
Here, we discuss the main findings, describing the different types of mitochondrial dysfunctions observed in SMA neurons and muscles (Figure 3) and how potential modifiers could ameliorate mitochondria-dependent SMA phenotypes. In the conclusion, we highlight the most burning open questions in the field and their implications for the development of potential new combinatorial therapies, especially in adults.
Figure 3.
Schematic summary of the mitochondrial defects observed in SMA neurons and SMA muscles. In both MNs and muscles, SMN loss causes mitochondrial morphology aberrations, reduced mitochondria number, altered respiration, ATP and ROS production. SMN depletion affects the cytoskeleton dynamics, resulting in altered mitochondrial transport in MN axons and defective mitochondrial localization in sarcomeres. In SMA MNs, mitochondria also present defective membrane potential and, at pre-synapses, reduced Ca2+ influx capacity. The figure was created with BioReneder.com.
2. Mitochondria Dysfunctions in SMA Neurons
2.1. Role of Mitochondria in Neurons
Neurons, the primary components of the nervous system, are highly polarized non-dividing cells that require vast amounts of energy to perform and maintain their functions. The human brain accounts for about 20% of the total energetic consumption [40], therefore, neuronal cells necessitate highly functional mitochondria. In both developing and mature neurons, mitochondria provide sufficient ATP for transcription, protein translation, actin cytoskeleton remodeling, trafficking of cargoes, regulation of transmembrane ion gradients and synaptic vesicles recycling [41]. In addition to ATP synthesis, mitochondria are key players in the regulation of Ca2+ homeostasis, lipid biogenesis and ROS signaling [41]. As neurons are extensively polarized and subspecialized cells, newly generated mitochondria undergo anterograde active transport to ensure energy supply in all compartments, while retrograde transport moves damaged mitochondria back to the soma [42]. In developing neurons, mitochondria are concentrated at growth cones and axonal branching sites; in mature neurons, mitochondria form functional domains—upon anchoring to actin cytoskeleton and microtubules—at pre- and post-synapses [43,44,45]. This distribution of mitochondria allows local Ca2+ buffering and ATP production to sustain local translation, actin dynamics, and finely regulate vesicles fusion/replenishment during firing [43,44,45]. At the same time, local protein synthesis of nuclear-encoded mitochondrial genes occurs in axons, and it is crucial to maintain mitochondria morphology and membrane potential [46,47,48].
In non-dividing cells, such as neurons, mitochondrial fusion and fission balance is essential to regulate mitochondrial size, number, morphology and proper turnover via biogenesis and mitophagy. Furthermore, in neurons, mitochondrial fission is required for efficient transport of mitochondria to the axon, since the trafficking of smaller organelles is facilitated [49]. The higher level of fission in axons, compared to dendrites, explains why axonal mitochondria are typically observed as small and punctuate (up to 3 µm of length), while dendritic mitochondria are long and tubular (up to 36 µm of length) [45,50,51]. Altered mitochondrial fusion/fission dynamics has important consequences for mitochondria functionality and is implicated in many neurodegenerative disorders, including Alzheimer’s disease (AD), Parkinson’s disease (PD), Huntington’s disease (HD) and ALS [49,52].
Although SMN protein is ubiquitously expressed, the predominant SMA feature is lower alpha motor neuron loss in the spinal cord, as shown by post-mortem studies in humans that revealed decreased number, atrophy and aberrant migration of anterior horn MNs in all SMA types [53,54,55]. These defects are accompanied by neuromuscular junction (NMJ) alterations, such as immature acetylcholine receptor clusters, synaptic vesicle trafficking defects and aberrant ultrastructure of nerve terminals [56]. Transmission electron microscopy analysis of SMA animal models confirmed these structural defects. In parallel, various cellular processes, which are all altered in SMA, such as splicing and miRNA processing [57,58], mRNAs trafficking to axons terminals [59,60,61], Ca2+ homeostasis [62], translation [63,64], endocytosis [32,65], and cytoskeletal dynamics [66,67,68] can lead to the mitochondrial dysfunctions observed in SMA and other MN disorders.
2.2. Mitochondrial Morphology, Dynamics and Transport in SMA Neurons
An important indicator of mitochondria functionality is mitochondrial morphology. Transmission electron microscopy and immunofluorescence staining revealed alterations of mitochondria shape both in tissues and in cultured MNs. In spinal cords from mouse models of different SMA-types, mitochondria are mainly fragmented (smaller and more spherical). In addition, some mitochondria display reduced cristae density and/or lamellar inclusions, while others are swollen or vestigial [69,70,71]. The examination of the nerve terminals at the NMJ of murine transverse abdominal muscle and diaphragm revealed similar defects [67,72,73]. General reduction in mitochondrial size is also observed in murine and human in vitro MN models of SMA [69,74,75,76]. All together, these results suggest that mitochondria fragmentation is enhanced from early stage of development in all SMA types. Increased mitochondrial fragmentation may result from impaired fusion [77] or excessive fission [49,52], both implicated in the pathogenesis of many neurodegenerative diseases. Of note, decreased mitochondrial size and, importantly, decreased cristae density, may lead to low ATP synthesis efficiency [78]. Moreover, mitochondrial fragmentation and swelling are associated with cellular apoptosis [79,80], frequently described as one of the mechanisms leading to MN death in SMA [81,82,83,84,85].
Many studies revealing altered mitochondrial morphology showed concomitant reduction in the number and density of mitochondria, especially along MN axons [66,71,75,86,87]. A general reduction in mitochondrial number may derive from altered biogenesis and/or excessive mitophagy, while defective mitochondria distribution along MN axons might be the result of an impaired transport. Live-imaging studies in primary MNs from different murine SMA models showed reduced retrograde axonal transport of mitochondria [69]. Similar trafficking alterations are present in MNs differentiated from human pluripotent stem cells, supporting the impact of SMN reduction on mitochondrial transport [74,76]. Cytoskeletal defects may explain the MN mitochondria trafficking alterations, since neurofilament accumulation and perturbed actin and microtubules dynamics are widely described in SMA [66,67,68,72,87]. Genetic manipulation of microtubules dynamics regulators can rescue SMA mitochondrial trafficking defects. Stathmin, a phosphoprotein that promotes microtubules depolymerization, and MAP1B, a microtubule-associated protein regulating α-tubulin detyrosination, are up-regulated in murine cellular SMA models, and their depletion restores proper mitochondrial transport and localization, as well as ameliorate SMA phenotypes [66,87]. Furthermore, the down-regulation of mitochondrial motor proteins, such as KIF1B and KIF1BP, upon SMN loss can also affect mitochondrial transport, as observed in SMA murine primary MNs [75].
2.3. Mitochondrial Respiration and Metabolism in SMA Neurons
Altered mitochondrial morphology has severe implications on mitochondrial functionality and bioenergetics [88]. Decreased basal and ATP-linked mitochondrial respiration rate, as well as decreased proton leak, occur in both SMA murine MN cultures and in Smn-depleted zebrafish embryos [69,89]. As a consequence, low levels of ATP are detected in murine cellular models and spinal cord homogenates [75,89,90]. A recent study demonstrated that neurons can face energy-demanding conditions by obtaining ATP through glycolysis [91]. Nevertheless, evidence suggests that in SMA the energy-deprivation status is not compensated by increased glycolysis [75,89]. Indeed, murine primary MNs showed reduced glucose uptake [75]. A comparative gene expression profiling of murine MN pools—with different SMA vulnerability—showed that phosphoglycerate kinase 1 (PGK1), a key glycolytic enzyme, is specifically down-regulated in SMA vulnerable MNs, and, when overexpressed or pharmacologically activated, can ameliorate SMA phenotype in zebrafish embryos [89]. These observations highlight the importance of glycolysis in specific MN pools to potentially counteract SMA mitochondrial bioenergetics defects. Altered regulation of ETC complexes [70,75], particularly of complex I [75], revealed by proteomic studies in murine MNs, may also cause abnormal mitochondrial respiration. In agreement with proteomics data, dysregulations of ETC complex I and IV activities were measured in murine SMA-like cells [90] and primary MNs [75]. On the other hand, a study in MNs and astrocytes differentiated from SMA patients-derived induced pluripotent stem cells (iPSCs) did not detect changes in the protein levels of complex II and IV [92], although this does not exclude a possible alteration of their activities. Interestingly, in one study the analysis of mitochondrial respiration both in murine primary spinal MNs and forebrain neurons showed defective respiration only in the former [69]. The fact that spinal MNs are fast fatigable, with high metabolic rate and under constant energetic stress, may explain why defects in mitochondrial respiration and ATP production predominantly affect this neuronal type.
2.4. Mitochondrial Oxidative Stress and Ca2+ Homeostasis in SMA Neurons
Altered mitochondrial respiration and ATP production often results in increased mitochondrial oxidative stress in neurons [93]. Many studies in post-mortem tissues from SMA patients and cellular models showed increased ROS levels both prior and after SMA-phenotype onset. Autopsies in children affected by SMA type I showed abnormal accumulation of 4-hydroxy-2-nonenal, a reactive lipid aldehyde, resulting from lipid peroxidation in brainstem and spinal MNs [94]. This is the only evidence for a specific type of ROS implicated in SMA neurons, since all the other studies in murine and human cellular models demonstrated a general increase in total or mitochondrial ROS production via unspecific probes or dyes [69,75,85,90,92,95]. Of note, one study, besides finding no evidence of altered mitochondrial respiratory complexes in iPSCs-derived MNs and astrocytes, reported normal mRNA levels of ROS markers and antioxidant enzymes, as well as no sign of DNA peroxidation and catalase alterations in spinal cords of SMA mice [92]. Another study also reported no signs of oxidative stress in SMA murine spinal cords [96], although no mitochondrial-specific ROS marker was analyzed. In contrast, most of the reports, suggest increased cellular and mitochondrial oxidative stress in SMA MNs, and contrasting findings can be attributed to the different model systems, the large variability in iPSCs-MNs cultures, and the time of development at which the measurements are performed. As the alteration of mitochondrial respiration was observed specifically in SMA-MNs [69], an increased mitochondrial ROS production was found in human stem cells-derived MNs and not in forebrain neurons [95], thus suggesting a role of mitochondrial oxidative stress in determining spinal MN-specific degeneration in SMA.
Presynaptic mitochondria have a fundamental role in buffering cytosolic Ca2+ and producing ATP to sustain the synaptic vesicle cycle during neuronal firing [44]. To the best of our knowledge, synaptic mitochondria Ca2+ dynamics during electric activity were investigated only recently ex vivo in motor nerve terminals from SMA mice [97]. This study revealed that Ca2+ entry during neural firing is significantly lower in SMA presynaptic mitochondria, while free Ca2+ levels in the mitochondrial matrix are normally at rest. This is likely due to an intrinsic reduction in the mitochondrial Ca2+ influx capacity, possibly due to defective influx rate through the mitochondrial calcium uniporter (MCU). However, this hypothesis was not investigated. Low Ca2+ influx capacity of mitochondria during electrical activity may decrease their ability to produce ATP to sustain synaptic vesicles fusion (exocytosis) and replenishment (endocytosis), both defective in SMA [32,67,86].
2.5. Mitochondrial Membrane Potential and Apoptosis in SMA Neurons
Alterations in respiratory complexes and increased mitochondrial oxidative stress are often associated with impaired mitochondrial membrane potential. Indeed, studies in murine and human stem cells-derived SMA MNs showed a reduction in mitochondrial membrane potential (ΔΨm) [69,74], which could result from the observed decrease in mitochondrial respiration [69], complex I activity [75] and ATP production [69,89]. Moreover, a decreased ΔΨm triggers mitophagy via fission or PINK1-Parkin pathways [52], and could explain the observed reduced number of total and functional mitochondria in SMA MNs not only in axons [66,71,74,75,76,86] but also in cell bodies [69,70]. On the other hand, another study in a murine SMA cellular model found increased ΔΨm attributed to a concomitant raise in complex IV activity [90]. These discrepancies might be due to different systems and probes used to detect ΔΨm. For example TMRE (tetramethylrhodamine-ethylester) or TMRM (tetramethylrhodamin-methylester) probes, that revealed mitochondrial depolarization, are considered as more reliable than JC1 dye because of their higher sensitivity [98]. Future studies should clarify whether mitochondrial depolarization or hyperpolarization is predominant in SMA neuronal mitochondria, since mitochondrial membrane potential abnormalities are strongly connected to cell death. In particular, mitochondrial persistent depolarization can lead to the opening of the mitochondrial permeability transition pore (mPTP) with consequent induction of mitochondrial swelling and apoptotic factors release [99].
Mitochondria can trigger cell death through the intrinsic apoptotic pathway, via cytochrome c release and subsequent activation of caspases 3/7 [100,101]. This can occur either following mitochondrial dysfunctions or as a consequence of internal stimuli, such as DNA damage, hypoxia, Ca2+ overload or oxidative stress. Evidence for MNs death through apoptotic pathways in SMA was provided by many studies both in patient tissues [81] and in animal and cellular models [82,83,102,103,104]. Some findings indicate mitochondrial mediation of apoptosis in SMA. For example, altered levels of mitochondrial pro-apoptotic proteins, such as BCL2, P53 and cytochrome c, were detected in spinal cords from SMA patients and in neuronal cellular SMA models [81,103]. Additionally, SMN is a putative interactor of both BCL2, a mitochondrial anti-apoptotic protein [105,106], and P53, a protein that can induce apoptosis through several mechanisms, including mitochondrial release of pro-apoptotic factors [107]. SMN interaction with these proteins prevents apoptosis onset [105,107], thereby suggesting involvement of the intrinsic apoptotic pathway in SMA cell death. Intrinsic apoptotic pathway can also be triggered by neuronal apoptosis inhibitory protein (NAIP) depletion, which is often present in SMA, since it is encoded by a gene located in the same genomic region of SMN1 [108]. Furthermore, recent studies on human stem cells-derived MNs showed that indirect boosting of mitochondrial function via Levetiracetam treatment results in a reduction in caspase 3/7-mediated apoptosis not accompanied by an increase in SMN levels [109]. We can conclude that the intrinsic apoptotic pathway in SMA is not merely triggered by the loss of SMN binding to mitochondrial-related apoptotic proteins, but it is also a direct consequence of mitochondrial dysfunctions.
2.6. Regulation of Transcription and Translation of Mitochondrial Proteins in SMA Neurons
The mentioned mitochondrial alterations and further potential dysfunctional mitochondrial pathways may be tracked back to altered levels of many nuclear-encoded mitochondrial transcripts in SMA-affected MNs (Table 1). There is also evidence of altered mitochondrial-mRNA levels specifically in somato-dendritic and axonal compartments of murine SMN-depleted MNs [110]. The direct connection between SMN protein loss and mitochondrial transcripts alteration has not yet been demonstrated. Nevertheless, given that SMN is directly involved in mRNA transcription [111], splicing [57], transport [59,60,61,63,112] and translation [63,64,75,113], it is tempting to speculate that SMN depletion may affect mitochondrial transcripts at all these different stages of their biogenesis. Importantly, transcripts encoding mitochondrial proteins are among the most abundantly enriched mRNAs in MN axons, remarking the strong impact that altered mRNA trafficking and local translation might have on mitochondria functionality. Here, collecting many transcriptome studies executed in SMA model systems and reporting all the mitochondrial transcripts that are either differentially expressed, or associated to SMN protein [114] or translated by SMN-primed ribosomes [113], we aim to give an overview that might help to shed light on the connection between SMN loss and dysfunctional mitochondria. An intriguing possibility is the identification of interesting candidates that might be transported via SMN-RNA granules or locally translated by SMN-primed ribosomes [113].
Table 1.
mRNA of genes encoding mitochondria-associated proteins that are either altered upon SMN loss, associated to SMN, translated by SMN-primed ribosomes or potential SMA modifiers.
| Mitochondrial Function | Accession Number | Gene Symbol | Tissue/Cell Type | Organism | Refs. |
|---|---|---|---|---|---|
| Altered mRNA Levels | |||||
| ROS signaling and oxidative stress | NM_001302272 | PRDX3 | iPSCs-motor neurons | human | [104] |
| NM_001286264 | MRS2 | ||||
| NM_000305 | PON2 | primary muscle cultures | human | [206] | |
| MGI:104887 | Gpx1 | spinal cord | mouse | [207] | |
| MGI:96916 | Maob | [208] | |||
| MGI:1921607 | Efhd1 | ||||
| MGI:104767 | Gpx4 | ||||
| MGI:1916617 | Glrx2 | spinal motor neurons | [69] | ||
| NM_001198532 | OXR1 | iPSCs-motor neurons, motor neurons (axonal compartment) | human, mouse | [104,110] | |
| OXPHOS | NM_001001935 | ATP5A1 | iPSCs-motor neurons | human | [104] |
| NM_001202469 | GBAS | ||||
| NM_001686 | ATP5B | ||||
| NM_001042546 | ATPAF1 | ||||
| NM_003366 | UQCRC2 | ||||
| NM_001282419 | NDUFA5 | ||||
| NM_006886 | ATP5E | ||||
| NM_001319036 | COX7A2L | ||||
| NM_001008215 | C2orf64 | ||||
| NM_002489 | NDUFA4 | ||||
| NM_001099668 | HIGD1A | ||||
| NM_001002258 | ATP5G3 | ||||
| NM_004374 | COX6C | ||||
| NM_001001973 | ATP5C1 | ||||
| NM_001865 | COX7A2 | ||||
| NM_001867 | COX7C | ||||
| NM_001864 | COX7A1 | primary muscle cultures | [206] | ||
| NM_004146 | NDUFB7 | muscle biopsy | [127] | ||
| MGI:192462 | C5orf63 | spinal cord | mouse | [208] | |
| MGI:1349919 | Ndufb11 | motor neurons (somatodendritic compartment) | [110] | ||
| MGI:106362 | Sco1 | motor neurons (axonal compartment) | |||
| MGI:1922656 | Ndufs7 | spinal motor neurons | [69] | ||
| MGI:107801 | Atp5b | ||||
| MGI:1343103 | Ndufa2 | ||||
| MGI:106100 | Etfdh | ||||
| Dr.113730 | latro | embryo | zebrafish | [209] | |
| T06D8.5 | cox-15 | larvae | worm | [210] | |
| NM_001916 | CYC1 | muscle biopsy, spinal motor neurons | human, mouse | [69,127] | |
| Fatty acid metabolism | NM_000182 | HADHA | iPSCs-motor neurons | human | [104] |
| NM_001007098 | SCP2 | ||||
| NM_016243 | CYB5R1 | primary muscle cultures | [206] | ||
| MGI:1859310 | Asah2 | spinal cord | mouse | [208] | |
| MGI:894291 | Acsl6 | motor neurons (somatodendritic compartment) | [110] | ||
| MGI:1928939 | Acot9 | motor neurons (axonal compartment) | |||
| MGI:1196345 | Agpat5 | ||||
| MGI:1914702 | Pnpla8 | ||||
| MGI:109501 | Crat | spinal motor neurons | [69] | ||
| CBG24278 | acaa-2 | larvae | worm | [210] | |
| Y48G9A.10 | cpt-3 | ||||
| F44C4.5 | ppt-1 | ||||
| Y45F3A.3a | acdh-11 | ||||
| E04F6.3 | maoc-1 | ||||
| NM_001318509 | ACSL4 | iPSCs-motor neurons, motor neurons (axonal compartment) | human, mouse | [104,110] | |
| Ca2+ homeostasis and signaling | MGI:88255 | Anxa6 | spinal cord | mouse | [207] |
| MGI:1338917 | S100a1 | [208] | |||
| MGI:1914065 | Mcub | motor neurons (axonal compartment) | [110] | ||
| MGI:109326 | Bnip3 | spinal motor neurons | [69] | ||
| MGI:1278343 | Nipsnap2 | ||||
| ZK816.5 | dhs-26 | larvae | worm | [210] | |
| Apoptosis | NM_001191 | BCL2L1 | iPSCs-motor neurons | human | [104] |
| NM_001199839 | BCL2L2 | ||||
| NM_001270729 | BCL2L13 | ||||
| NM_001029839 | C3orf23 | ||||
| NM_001008388 | CISD2 | ||||
| NM_007523 | Nbak1 | spinal cord | mouse | [207] | |
| MGI:1933786 | Dnaja3 | ||||
| MGI:1346325 | Gadd45g | ||||
| MGI:1197519 | Bcl2l11 | spinal motor neurons | [69] | ||
| MGI:1913744 | Prelid1 | ||||
| MGI:99702 | Bax | ||||
| F23B12.9 | egl-1 | larvae | worm | [210] | |
| NM_001196 | BID | iPSCs-motor neurons, spinal cord | human, mouse | [104,207] | |
| mtDNA maintenance, mitochondrial transcription and translation | NM_133259 | LRPPRC | iPSCs-motor neurons | human | [104] |
| NM_001182520 | MRPL3 | ||||
| NM_001243251 | NARS2 | ||||
| MGI:191904 | Mrps27 | spinal cord | mouse | [208] | |
| MGI:1922869 | Fastkd2 | motor neurons (axonal compartment) | [110] | ||
| MGI:2142973 | Lars2 | ||||
| MGI:1917297 | Trnt1 | ||||
| MGI:1889295 | Eral1 | ||||
| MGI:1913660 | Mterf3 | ||||
| MGI:2387629 | Tardbp | ||||
| MGI:1915541 | Mto1 | ||||
| MGI:1351639 | Mrpl15 | ||||
| MGI:1923776 | Gatc | ||||
| MGI:1920040 | Ssbp1 | ||||
| MGI:1923686 | Tufm | spinal motor neurons | [69] | ||
| MGI:2137215 | Mrpl11 | ||||
| MGI:1919049 | Ptcd1 | ||||
| MGI:1929864 | Myg1 | ||||
| MGI:107252 | Nsun2 | ||||
| MGI:1333820 | Mrpl30 | ||||
| MGI:107329 | Mrpl50 | ||||
| MGI:107810 | Tfam | ||||
| W09D10.3 | mrpl-12 | larvae | worm | [210] | |
| Y119D3B.16 | mrpl-16 | ||||
| C05D11.10 | mrps-17 | ||||
| F29C12.4 | gfm-1 | ||||
| Y46H3A.7a | mrpl-39 | ||||
| CBG13134a | mrpl-14 | ||||
| MGI:1919214 | Atad3a | motor neurons (axonal compartment), larvae | mouse, worm | [110,210] | |
| NM_016622 | MRPL35 | iPSCs-motor neurons, spinal motor neurons | human, mouse | [104] | |
| Mitochondria quality control | MGI:2135611 | Immp2l | spinal cord | mouse | [208] |
| MGI:1346017 | Clpx | spinal motor neurons | [69] | ||
| MGI:1926884 | Huwe1 | motor neurons (somatodendritic compartment) | [110] | ||
| MGI:1920209 | Lonrf2 | motor neurons (axonal compartment) | |||
| MGI:1891828 | Becn1 | ||||
| MGI:1915207 | Marchf5 | ||||
| F59H6.11 | bath-5 | larvae | worm | [210] | |
| C37H5.8 | hsp-6 | ||||
| Y47G6A.10 | spg-7 | ||||
| Mitochondrial dynamics, membrane trafficking | NM_001206651 | SH3GLB1 | iPSCs-motor neurons | human | [104] |
| NM_001033566 | RHOT1 | ||||
| NM_001256763 | FAM49B | ||||
| NM_001303249 | SLC25A46 | [104] | |||
| NM_001164730 | REEP1 | ||||
| NM_014394 | GHITM | ||||
| NM_213720 | C22orf16 | muscle biopsy | [127] | ||
| NM_017812 | CHCHD3 | ||||
| MGI:1313276 | Vamp1 | spinal cord | mouse | [208] | |
| MGI:1098586 | Rab11fip5 | motor neurons (axonal compartment) | [110] | ||
| MGI:1918953 | Armcx3 | motor neurons (axonal compartment) | |||
| MGI:1914977 | Stx17 | motor neurons (somatodendritic compartment) | |||
| MGI:2385189 | Rap1gds1 | spinal motor neurons | [69] | ||
| F21C10.10 | CELE_F21C10.10 | larvae | worm | [210] | |
| Y37E3.9 | phb-1 | ||||
| NM_006373 | VAT1 | iPSCs-motor neurons, spinal motor neurons | human, mouse | [69,104] | |
| Mitochondrial import, transport, translocation (metabolites, proteins, lipids, ions) | NM_014820 | TOMM70A | iPSCs-motor neurons | human | [104] |
| NM_001104647 | SLC25A36 | ||||
| NM_001321967 | ATAD1 | ||||
| NM_001322977 | SFXN1 | ||||
| NM_002635 | SLC25A3 | ||||
| NM_001270679 | CCDC90B | ||||
| NM_001135694 | VDAC3 | ||||
| NM_006335 | TIMM17A | ||||
| NM_014765 | TOMM20 | ||||
| NM_001184783 | VDAC2 | ||||
| NM_001151 | SLC25A4 | muscle biopsy | [127] | ||
| U94592 | UCP2 | primary muscle cultures | |||
| MGI:1343262 | Timm44 | motor neurons (axonal compartment) | [110] | ||
| MGI:1917560 | Plscr3 | ||||
| MGI:1917728 | Mipep | ||||
| MGI:1340062 | Sgk1 | spinal motor neurons | [69] | ||
| MGI:1349215 | Abcd1 | ||||
| R07E3.4 | CELE_R07E3.4 | larvae | worm | [210] | |
| C34C12.8 | C34C12.8 | ||||
| Y71G12B.24a | mppa-1 | ||||
| CBG01742 | timm-17b.1 | ||||
| B0432.4 | misc-1 | ||||
| F55C5.5 | tsfm-1 | ||||
| F56D1.3 | mrps-16 | ||||
| Dr.77108 | ucp4 | embryo | zebrafish | [209] | |
| NM_152407 | GRPEL2 | iPSCs-motor neurons, motor neurons (axonal compartment) | human, mouse | [104,110] | |
| Metabolic enzymes | NM_001242767 | MTHFD1L | iPSCs-motor neurons | human | [104] |
| NM_000663 | ABAT | ||||
| NM_001286220 | GOT2 | ||||
| NM_001183948 | ODC1 | ||||
| NM_001077180 | METTL9 | ||||
| NM_001282621 | PGRMC1 | ||||
| NM_001174097 | LDHB | ||||
| NM_001318900 | GLUD1 | ||||
| NM_001282403 | MDH2 | ||||
| NM_001482 | GATM | ||||
| NM_018464 | C10orf70 | muscle biopsy | human | [127] | |
| NM_002168 | IDH2 | ||||
| MGI:87990 | Alas2 | spinal cord | mouse | [208] | |
| MGI:2661364 | Neu4 | ||||
| MGI:1915871 | Mthfd2l | motor neurons (somatodendritic, axonal compartment) | [110] | ||
| MGI:2385311 | Dlat | motor neurons (axonal compartment) | |||
| MGI:1346064 | Eci2 | ||||
| MGI:1916296 | Isca1 | ||||
| MGI:1889278 | Pdss1 | ||||
| MGI:1099463 | Idh3g | ||||
| MGI:1918732 | Rdh13 | ||||
| MGI:88590 | Cyp1b1 | motor neurons (somatodendritic compartment) | |||
| MGI:1306824 | Suclg2 | ||||
| MGI:98731 | Tgm2 | ||||
| MGI:2159605 | Acot2 | spinal motor neurons | [69] | ||
| MGI:97770 | Prodh | ||||
| MGI:87867 | Acadm | ||||
| MGI:2180203 | Tmlhe | ||||
| T22B7.7 | CELE_T22B7.7 | larvae | worm | [210] | |
| C04E6.7 | CELE_C04E6.7 | ||||
| T05G5.6 | ech-6 | ||||
| F32D8.12b | CELE_F32D8.12 | ||||
| F57F4.1 | CELE_F57F4.1 | ||||
| T07D3.9b | CELE_T07D3.9 | ||||
| R12C12.1b | gldc-1 | ||||
| F54D5.12 | CELE_F54D5.12 | ||||
| F25B4.1 | gcst-1 | ||||
| ZK669.4 | dbt-1 | ||||
| C50F7.4 | sucg-1 | ||||
| F46G10.7a | sir-2.2 | ||||
| T02G5.8 | kat-1 | ||||
| F09F7.4b | hach-1 | ||||
| Y38F1A.6 | hphd-1 | ||||
| T20H4.5 | EC:7.1.1.2 | ||||
| F23B12.5 | dlat-1 | ||||
| ZK652.9 | coq-5 | ||||
| Mitochondrial regulation and signaling | NM_001001924 | MTUS1 | iPSCs-motor neurons | human | [104] |
| NM_001244974 | PPP1CC | ||||
| NM_001017963 | PTGES3 | ||||
| NM_001318067 | MAPK10 | ||||
| NM_001005 | RPS3 | ||||
| MGI:1929628 | Rsad2 | motor neurons (somatodendritic, axonal compartment) | mouse | [110] | |
| MGI:1101055 | Ifit3 | motor neurons (somatodendritic compartment) | |||
| MGI:1918836 | Ifih1 | ||||
| MGI:2446107 | Pde2a | ||||
| MGI:1344391 | Sh3bp5 | motor neurons (axonal compartment) | |||
| MGI:2159437 | Agtpbp1 | ||||
| MGI:1927243 | Rala | ||||
| MGI:1919792 | Pgam5 | ||||
| MGI:1913842 | Stoml2 | spinal motor neurons | [69] | ||
| MGI:1915864 | Letmd1 | ||||
| MGI:2441680 | Tmem8b | ||||
| C43E11.4 | tufm-1/2 | larvae | worm | [210] | |
| T24H7.1 | phb-2 | ||||
| C16C10.11 | har-1 | ||||
| Altered mRNA splicing | |||||
| Mitochondrial import, transport, translocation (metabolites, proteins, lipids, ions) | MGI:88025 | Ank2 | motor neuron, neuroblastoma cells | mouse | [211] |
| Mitochondrial regulation and signaling | MGI:98397 | Src | neuroblastoma cells | ||
| mRNA associated to SMN | |||||
| Ca2+ homeostasis and signaling | MGI:109326 | Bnip3 | NSC-34 cells | mouse | [114] |
| OXPHOS | MGI:1333806 | Cox17 | |||
| MGI:1855697 | Atp5e | ||||
| MGI:99927 | mt-Atp6 | ||||
| MGI:1930666 | Higd1a | ||||
| MGI:1316714 | Cox7a1 | ||||
| Mitochondrial import, transport, translocation (metabolites, proteins, lipids, ions) | MGI:1353433 | Timm8a1 | |||
| MGI:1347061 | Abcg2 | ||||
| Metabolic enzymes | MGI:1916884 | Clybl | |||
| MGI:1098623 | Acaa2 | ||||
| Mitochondria quality control | MGI:1921392 | Lonp1 | |||
| mtDNA maintenance, mitochondrial transcription and translation | MGI:1926237 | Mrps30 | |||
| MGI:2442510 | Dars2 | ||||
| MGI:2135755 | Cox4i2 | ||||
| mRNA enriched for SMN-primed ribosomes | |||||
| OXPHOS | MGI:2143558 | Chchd10 | brain | mouse | |
| MGI:104614 | Cox6c | ||||
| MGI:1316715 | Cox7a2 | ||||
| MGI:1914862 | Mettl9 | ||||
| MGI:1914514 | Ndufb8 | ||||
| MGI:2385112 | Ndufs2 | ||||
| MGI:1915903 | Samm50 | ||||
| MGI:1914175 | Sdhd | ||||
| MGI:107876 | Uqcrc1 | ||||
| MGI:1917794 | Tmem242 | ||||
| Fatty acid metabolism | MGI:894291 | Acsl6 | |||
| MGI:1915988 | Acss1 | ||||
| MGI:1351861 | D10Jhu81e | ||||
| Apoptosis | MGI:1339639 | Ogt | |||
| mtDNA maintenance, mitochondrial transcription and translation | MGI:2137221 | Mrpl20 | |||
| MGI:2153111 | Mrps6 | ||||
| MGI:2443470 | Mrm1 | ||||
| MGI:1914216 | Trit1 | ||||
| Mitochondria quality control | MGI:1916193 | Pink1 | |||
| MGI:98889 | Ubc | ||||
| MGI:2444207 | Vps13c | ||||
| Mitochondrial dynamics, membrane trafficking | MGI:88025 | Ank2 | |||
| MGI:1261831 | Hap1 | ||||
| MGI:108426 | Kif1b | ||||
| MGI:1349450 | Vat1 | ||||
| MGI:1913687 | Fis1 | ||||
| MGI:1928394 | Mtor | ||||
| MGI:1921393 | Opa1 | ||||
| MGI:1925498 | Armcx1 | ||||
| Mitochondrial import, transport, translocation (metabolites, proteins, lipids, ions) | MGI:1915517 | Slc25a22 | |||
| MGI:1100517 | Clpb | ||||
| MGI:2444911 | Slc25a29 | ||||
| MGI:2137681 | Sfxn5 | ||||
| Metabolic enzymes | MGI:1919289 | Mccc1 | |||
| MGI:2685870 | Pdp1 | ||||
| MGI:87989 | Alas1 | ||||
| MGI:88407 | Ckb | ||||
| MGI:1913637 | Nudt8 | ||||
| MGI:1918993 | Coasy | ||||
| MGI:2385920 | Dip2a | ||||
| MGI:1858208 | Ech1 | ||||
| MGI:2441982 | Aldh5a1 | ||||
| Mitochondrial regulation and signaling | MGI:97592 | Prkaca | |||
| MGI:97138 | Mpv17 | ||||
| Genes for mitochondrial proteins that modify SMN levels/activity | |||||
| OXPHOS | NM_001286264 | MRS2 | HEK293 cells | human | [200] |
| Apoptosis | NM_003334 | UBA1 | |||
| NM_001291921 | RXRA | larvae, NMJ between muscles 6/7 in A2 segment | D. melanogaster | [199] | |
| Mitochondrial dynamics, membrane trafficking | NM_004958 | RPS6KB1 | HEK293 cells | human | [200] |
| Mitochondrial import, transport, translocation (metabolites, proteins, lipids, ions) | NM_003356 | UCP3 | |||
| Metabolic enzymes | NM_001098 | ACO2 | |||
| Mitochondrial regulation and signaling | NM_001144012 | TXNDC14 | |||
3. Mitochondria Dysfunctions in SMA Muscles
3.1. Role of Mitochondria in Muscles
Muscles are high metabolic tissues that constitute almost 50% of the human body mass. Being high-energy consumption cells, myocytes contain 2–10% mitochondria by volume [115]. Skeletal and cardiac muscle cells, similar to neuronal cells, are non-dividing cells with an exceptionally complex and organized cytosol. Myocytes contain two distinct populations of mitochondria: the subsarcolemmal mitochondria, which supply ATP for gene transcription and membrane transport, and the intermyofibrillar mitochondria, which provide ATP for muscle contraction [116]. The intermyofibrillar mitochondria resemble a “power grid”, where organelles are compacted in cylinders (up to 1 µM diameter) between myofibrils and connected through protruding mitochondrial nanotunnels (diameter 26.1–204.2 nm) [117,118]. Unlike tissues with high cellular turnover where damaged mitochondria are segregated and dispersed among newly dividing cells, myocytes can only rely on mitochondrial quality control mechanisms to maintain a functional mitochondrial network [119]. Functional fusion, fission and transport are required to not only ensure uniform distribution of energy and metabolites but also of functioning mitochondria and to facilitate the clearance of the damaged organelles through mitophagy [120]. In addition to serving as an essential energy source for muscular fibers contraction, mitochondria are essential players in muscular Ca2+ and ROS signaling. Ca2+ is released and re-uptaken from the sarcoplasmic reticulum to induce muscle contraction. Intermyofibrillar mitochondria tethered to the sarcoplasmic reticulum actively participate to this process using the Ca2+-influx to stimulate ATP production [121] and, thus, defects in the muscle mitochondrial network morphology and Ca2+ homeostasis can ultimately affect mitochondrial respiration and cause oxidative stress [122].
Although the distinctive feature of SMA is low motor neuron degeneration, the loss—or partial loss—of SMN function affects most, if not all, tissues [123], and, in particular, smooth and skeletal muscles [124,125]. CT scan and histological analysis of muscle fibers from SMA patients show different levels of generalized atrophy that can vary even among the distinct muscle types of single individuals [126,127]. The diaphragm displays the earliest defects in both SMA patients and SMA model mice [70,72,73]. The cause of muscular atrophy in SMA is to be attributed to both progressive denervation [128,129] and loss of SMN specific functions in muscle cells. Nearly complete depletion of SMN (90%) in stable murine myoblast cell lines shows decreased number of gems, also observed in chicken cells [130], and decreased proliferation—but not increased cell death—and abnormal myotubes formation in vitro, due to impaired myoblast fusion [131]. Primary myoblasts derived from different SMA mouse models showed delay in skeletal muscle development due to decreased levels of expression of myogenic genes [132,133]. A recent study demonstrated that skeletal muscle-specific depletion of Smn (one copy of SMN2 still present to resemble severe SMA genotype) in mice is sufficient to recapitulate the muscular fibers abnormalities typical of SMA, and, more importantly, to cause NMJ defects, despite normal SMN expression in neuronal cells [134]. However, muscle-specific expression of SMN cannot rescue neither the phenotypes nor the survival of mice affected by SMA [135]. This is because the effects of SMN loss are synergically affected by the denervation. These observations further reinforce the systematic nature of SMA and the important role of SMN in development [136]. Given the crucial and ubiquitous role of SMN, its dysfunction causes alterations that are common across tissues and conserved from fish to mammals [137,138], albeit the cell-specific molecular mechanisms that induce muscle degeneration upon SMN deficiency are still unclear.
3.2. Mitochondria Morphology, Dynamics and Transport in SMA Muscles
Similar to neuronal cells, SMA muscle cells are characterized by heterogeneous mitochondrial defects. As discussed above, the overall muscle architecture is strongly impaired in SMA patients. In mice, SMA muscles displaying disarranged fibers and myofibril bundles, also present the loss of sarcomere structure along with decreased number of mitochondria [67,73]. Reduced number of functional mitochondria was also observed through histochemical and biochemical analysis of muscle specimens from SMA patients. Multiple studies reported decreased mitochondrial respiratory complex activity [139,140,141,142,143,144,145], together with decreased levels of enzymatic markers (e.g., citrate synthase, ETC complex I, II, IV) and mtDNA content [140,141,145,146]. Furthermore, the highly organized mitochondria power grid associated with the sarcoplasmic reticulum is collapsed, resulting in extremely swollen mitochondria with enlarged cristae and intermembrane space [129,147,148].
As previously mentioned, the morphology of the mitochondrial network has great impact on the homeostasis of these organelles. Proper mitochondrial morphology is maintained by the correct equilibrium between fusion and fission, and by the association of mitochondria to the cytoskeleton [149]. SMN loss affects the cytoskeleton by altering the expression of numerous factors implicated in actin and microtubule dynamics [27,66,87,150,151,152], with possible repercussions on mitochondria. Indeed, in C. elegans, muscles-specific knockout of smn-1 causes mitochondrial morphology and distribution defects in the sarcomere, due to the consequent decreased activity of ARP2/3 protein complex [153]. ARP2/3 complex is an actin nucleation factor, essential for actin filament polymerization and branching and for maintaining a functional actin cytoskeleton [154]. In particular, the ARP2/3 complex has a fundamental role in mitochondrial dynamics and transport, since it promotes actin polymerization at mitochondrial fission sites [155]. Interestingly, the SMA protective modifier PLS3 directly influences the ARP2/3-mediated actin-based dynamics and, thus, may influence mitochondrial dynamics and distribution [156].
Strong evidence for SMN involvement in actin dynamics and consequent impairment of myotubes formation and sarcomere structure is present in mammalian systems. For example, in murine myoblasts, SMN loss results in defects in cell migration and focal adhesion that ultimately prevent myoblast fusion in vitro [133]. In mammalian cells, SMN has been shown to directly interact with profilin2a, an actin-binding protein that regulates actin polymerization [150,151]. In healthy human muscle fibers, SMN co-localizes with profilin2a and titin in the sarcomere, as is also previously shown in D. melanogaster and mice [157,158]. In hypertrophic SMA myofibers, SMN localization is altered and is accompanied by aberrant accumulations of actin filaments, suggesting that SMN plays a role in actin proteostasis and the maintenance of the sarcomere architecture [159]. However, consequent potential alterations of the mitochondrial network have never been investigated in mammalian muscles cells.
3.3. Mitochondria Respiration and Metabolism in SMA Muscles
Decreased ADP-dependent O2 consumption, indicative of defective mitochondria respiration and OXPHOS, has been measured in mitochondria isolated from murine SMA muscles and in human SMA myoblasts [160,161]. The defects in energy production may arise from altered expression and regulation of the mitochondrial ETC components and/or enzymes involved in glycolysis, TCA cycle and fatty acid metabolism [162]. SMA mice display, indeed, reduced enzymatic activity of the ETC complex I, II and IV in muscles, together with enhanced lipogenesis [160]. Similarly, reduced glycolysis and increase in accumulation of triglycerides have been observed in murine SMA liver [163], and urine samples from SMA patients are also characterized by increased short-chain or medium-chain fatty acids caused by downregulation of beta-oxidation [164,165]. The systemic dysfunctional mitochondrial fatty acid metabolism may determine the development of obesity, insulin resistance and hyperinsulinemia observed in young SMA patients and mice [166,167,168,169,170].
3.4. Mitochondrial Oxidative Stress and Apoptosis in SMA Muscles
The impaired activity of enzymes involved in mitochondrial metabolism and respiration can generate ROS and cause oxidative stress. The analysis of SMA mice heart showed increasing levels of vascular angiotensin II type 1 receptor (AGTR1), indicator of oxidative stress in cardiac tissue [171,172]. Although myocardial fibrosis in SMA mice has been attributed to increased oxidative stress, the role of ROS in SMA pathogenesis in skeletal muscles has been overlooked [171].
ROS are physiologically produced during muscular contraction, as a by-product of enhanced mitochondrial respiration, and maintained at homeostatic concentrations by the balanced activity of ROS-producing and ROS-scavenging enzymes [173]. Transient increase in ROS production promotes muscle fiber adaptation to both strong contractions and immobility; on the contrary, oxidative stress caused by prolonged high ROS levels can directly affect proteins, lipids and nucleic acids, as well as trigger cell death signaling cascades [174,175]. Furthermore, it has been recently shown that SMN overexpression can reduce cytochrome c release and caspase-3 activation (mitochondrial apoptotic pathway [176]) in murine cardiomyocytes, by increasing the expression of BCL2 and decreasing the expression of BAX, anti- and pro-apoptotic factor, respectively [177]. In addition, chemically induced ROS production causes aberrant splicing of SMN2 in SMA mice in heart and skeletal muscle, resulting in even lower level of functional SMN protein [178]. Therefore, oxidative stress caused by mitochondrial dysfunctions and the consequent even lower levels of SMN protein could synergically enhance cell death rate and, thereby, promote muscular atrophy and cardiovascular abnormalities in SMA patients [179].
3.5. Regulation of Transcription and Translation of Mitochondrial Proteins in SMA Muscles
Since SMA is widely recognized as a motor neuron pathology, most of the studies investigating the cellular phenotypes, including mitochondrial functions, arising from SMN depletion are carried out in neural cell models [180]. Although muscular aberrations are often considered secondary lesions derived from loss of neuromuscular junction and denervation, we discussed in this review how SMN ablation is sufficient to cause cell-autonomous defects also in myocytes [131,134]. Mitochondria play a major role in muscle function and development, and, given that muscular phenotypes of SMA resemble many different mitochondriopathies [181,182], it is likely that mitochondrial dysfunctions also play a major role in SMA pathogenesis. Although there is currently no evidence of specific mitochondrial functions of SMN in myocytes, the expression of many essential mitochondrial proteins may be affected by SMN loss, as suggested from the transcriptome datasets summarized in Table 1. Further investigations in this direction could identify new modifying proteins/pathways that rescue or mitigate the mitochondrial defects caused by SMN deficiency in muscles.
Moderate exercise represents an accessible and effective therapeutic approach to stimulate and improve mitochondria functionality in muscle fibers [183]. SMA patients benefit of exercise therapy to improve muscular strength and size [184,185,186,187]. In SMA mice, mitochondrial function analysis showed that individuals subject to regular exercise display activation of the AMPK–p38–PGC-1α signaling axis and higher O2 consumption in skeletal muscles, ultimately resulting in decreased lipogenesis [160,188]. Similarly, chemical stimulation of the AMPK-p38 pathway using celecoxib, a cyclo-oxygenase 2 inhibitor, increases the lifespan and the motor function of SMA mice [189]. These observations suggest that targeting muscle-specific mitochondrial abnormalities could alleviate not only muscular weakness but also secondary systemic disorders, such as hyperglycemia, hyperglucagonemia, glucose resistance and dyslipidemia, observed in SMA patients [190,191]. Future studies must focus on the function of SMN on mitochondria homeostasis in muscle cell models to elucidate the molecular mechanisms that contribute to SMA etiology and to identify new potential modifiers and therapeutic targets.
4. Mitochondrial Functions: Potential SMA Modifiers?
The studies discussed here clearly demonstrate that mitochondrial dysfunctions are widespread in SMA tissues across species. Although the studies performed on motor neurons outnumber the studies in muscles or other cell types, SMA deserves to be considered and studied as multi-systemic disorder. Mitochondria dysfunctions arise from the early stages of SMA pathogenesis and may play a crucial role in the disease progression, even by impacting directly on SMN protein level. For example, increased mitochondrial ROS production can directly affect SMN2 splicing, further reducing functional SMN levels [178]. Additionally, mitochondrial mitofusin 2 (MFN2) mediate the transport of calpastatin along MN axons, locally inhibiting calpain protease activity and preventing NMJ degeneration [192]. As SMN degradation is also performed by calpains, altered mitochondrial transport might affect SMN turnover in axonal terminals [76].
Given the diversified functions of SMN protein, it is not surprising that mitochondria are downstream targets (Figure 2). Dysfunctional RNA metabolism affects a plethora of mitochondrial-related transcripts encoding for proteins involved in all mitochondrial functions (Table 1). Additionally, altered ubiquitination, due to defective UBA1 splicing, impacts on Wnt/β-catenin signaling, a strong activator of mitochondria biogenesis [193,194]. Furthermore, as previously discussed, cytoskeletal alterations linked to SMN deficiency strongly affect mitochondria transport, dynamics and morphology. Interestingly, many of the SMA modifiers described so far act on the above-mentioned pathways, resulting, in some cases, in complete reverse of the symptoms (e.g., PLS3 and NCALD). Thus, we speculate that boosting mitochondrial activity could lead to a partial rescue of SMA degenerative phenotypes. For instance, we already discussed how enhancing the activity of proteins involved in cytoskeletal dynamics, such as PLS3, stathmin, MAP1B and additionally CORO1C [195], have positive effects on both mitochondrial functionality and SMA phenotypes. In a recent study on Smn-depleted zebrafish, overexpression of necdin, a protein promoting mitochondrial biogenesis in neurons, could rescue axonal outgrowth defects [89]. Another known SMA modifier that may exert its protective function acting on mitochondria is stasimon, a suppressor of p38-MAPK cell death pathway that is decreased in SMA due to splicing defects [196]. A recent study shows that stasimon localizes in correspondence of ER-mitochondria contact sites, possibly participating to mitochondria quality control, dynamics and calcium-handling mechanisms [197]. Lastly, many other described SMA-modifiers, such as PTEN [84], ZPR-1 [198] and NAIP [108], reduce mitochondrial-induced apoptosis. These findings suggest that modulating the expression of modifier genes involved in mitochondrial functions may be an effective strategy to mitigate SMA phenotypes. Given the strong importance of mitochondria in all cell types, and especially in MNs and muscles, we are convinced that future studies should focus on the identification of new mitochondrial-related modifiers of SMA pathology. Genetic screenings for new modifiers recently conducted both in D. melanogaster [199] and human HEK cells [200] highlighted new potential mitochondrial candidates (Table 1).
Currently, there is only one pharmacological therapy specifically targeting mitochondria that reached the clinical trial stage for SMA patients: olexisome. Olexisome modulates the mitochondrial permeability transition pore preventing cell death induction [201]. Unfortunately, olexisome administration in phase II trial failed due to ineffective long-term results [202]. Nevertheless, given the promising effects of this compound in several in vitro and in vivo models of motor neuron disorders—including a severe mouse model of SMA—the possibility of using it in combinatorial therapies should not be neglected [201]. Nowadays, the research in the field of mitochondrial-targeted drugs is moving forward and an increasing number of new molecules will be available to be tested in many different SMA models [203]. Recently, in vitro studies on iPSCs-derived MNs showed efficacy of several compounds (some of them already used to treat ALS or epilepsy) in rescuing both mitochondrial dysfunctions and SMA phenotypes—with or without increasing SMN protein levels—adding new promising candidates for a therapy [74,76,85,109].
5. Conclusions
As key bioenergetics organelles, mitochondria may play a major role in SMA pathogenesis. The activity of SMN protein has an impact on many cellular processes and mitochondrial alterations are among the downstream effects of SMN loss (Figure 2). In SMA pathological conditions, specific mitochondrial abnormalities may affect other related mitochondrial functions, thereby amplifying SMN-dependent cellular alterations. Still, the causal link between SMN loss and mitochondrial dysfunctions is unknown. Future cellular studies must focus on the ambitious goal of unravelling the molecular mechanisms that directly connect SMN activity with mitochondrial homeostasis. We speculate that delving into the altered mitochondria-related transcripts, observed in various SMA models (Table 1), is key to advance our knowledge in this direction. Many known mutations in genes encoding mitochondrial proteins result in SMA-like disorders, further remarking the crucial role of mitochondria in the development of SMA phenotypes and symptoms. In fact, mitochondrial pathways represent a valuable target not to cure SMA, but rather to mitigate the symptoms, improve the life quality of patients and possibly slow down the development of the disease.
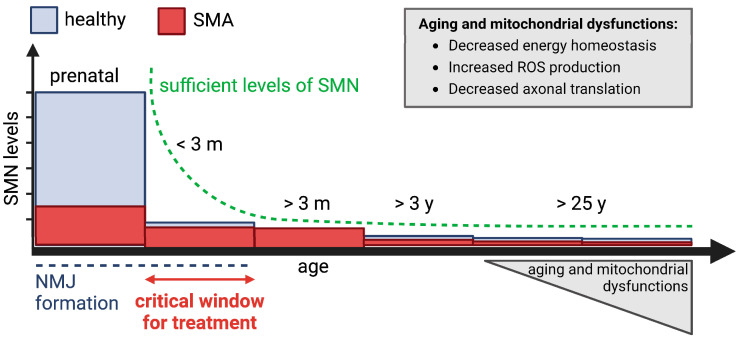
Many aspects of SMA etiology, however, are still poorly understood. Intriguingly, although in adulthood very low SMN levels are sufficient to maintain the health of MNs [12], there are patients carrying 4–6 SMN2 copies that develop SMA in adulthood, sometimes even after 30 years of age [7,204]. We hypothesize that in such cases, cellular aging—a natural phenomenon associated with increased ROS production, decreased mitochondrial bioenergetics and protein translation—affects the MNs (already vulnerable due to reduced SMN levels during development), dropping below a functional threshold that is compatible with health, and thereby triggering SMA onset (Figure 4). We speculate that the “watch and wait” strategy, adopted for SMA individuals with four or more SMN2 copies, may overshoot the most critical period when high SMN levels are required for NMJ development and maturation. Delaying the treatment, instead of starting it in the first post-natal months up to three years, may affect the efficacy of the therapy. Indeed, after 3 years of age, minimal SMN levels are required and there is no significant difference between SMA and healthy individuals [12]. Even more, it has been shown in mice that inducing constantly elevated SMN expression (scAAV9-SMN gene therapy) in MNs, above the endogenous levels, is neurotoxic in adult animals [205]. Therefore, even in newborns with four SMN2 copies, early treatment and supply of sufficient SMN protein during the critical time window of NMJ maturation may be key to support their best possible development and to confer resistance against deleterious aging effects later in life. For this purpose, SMA newborn screening is a determinant to identify SMA individuals pre-symptomatically and promptly start the treatment. Lastly, monitoring new therapeutic advances, especially when targeting mitochondrial processes, for the treatment of other late-onset MN disorders, such as ALS, might be extremely helpful. Indeed, we speculate that adult SMA patients may rather benefit from therapies ameliorating mitochondrial functions than therapies elevating SMN levels.
Figure 4.
Cellular aging and mitochondrial aberrations may decrease MN performance below their functional threshold in adult SMA. SMN protein functions are mainly required during the development; indeed, also in healthy individuals the levels of SMN protein drop already after birth by 6.5-fold. SMN is also required in the adulthood but only at low levels, not significantly different between healthy and SMA individuals [12]. Many aging factors, such as decreased bioenergetics, increased ROS production and decreased axonal translation, may drop the function of NMJs just slightly below the threshold, ultimately causing SMA in adults. The figure was created with BioReneder.com.
Author Contributions
Conceptualization, E.Z., V.P. and B.W.; figures, E.Z. and V.P.; writing, E.Z., V.P. and B.W.; review, and editing B.W. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
The work of BW was supported by the German Research Foundation [Wi 945/17-1 (project 398410809); Wi 945/18-1 (project 384170921); Wi 945/19-1 (project 417989143); KY96.1-2 (project 269018619); SFB1451 (project 431549029—A01), and GRK1960 (project ID 233886668)], the European Union’s Horizon 2020 Marie Skłodowska-Curie (project 956185; SMABEYOND) and the Center for Molecular Medicine Cologne (project C18).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wirth B., Karakaya M., Kye M.J., Mendoza-Ferreira N. Twenty-Five Years of Spinal Muscular Atrophy Research: From Phenotype to Genotype to Therapy, and What Comes Next. Annu. Rev. Genom. Hum. Genet. 2020;21:231–261. doi: 10.1146/annurev-genom-102319-103602. [DOI] [PubMed] [Google Scholar]
- 2.Finkel R.S., Mercuri E., Meyer O.H., Simonds A.K., Schroth M.K., Graham R.J., Kirschner J., Iannaccone S.T., Crawford T.O., Woods S., et al. Diagnosis and management of spinal muscular atrophy: Part 2: Pulmonary and acute care; medications, supplements and immunizations; other organ systems; and ethics. Neuromuscul. Disord. 2018;28:197–207. doi: 10.1016/j.nmd.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 3.Mercuri E., Finkel R.S., Muntoni F., Wirth B., Montes J., Main M., Mazzone E.S., Vitale M., Snyder B., Quijano-Roy S., et al. Diagnosis and management of spinal muscular atrophy: Part 1: Recommendations for diagnosis, rehabilitation, orthopedic and nutritional care. Neuromuscul. Disord. 2018;28:103–115. doi: 10.1016/j.nmd.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Yeo C.J.J., Darras B.T. Overturning the Paradigm of Spinal Muscular Atrophy as Just a Motor Neuron Disease. Pediatr. Neurol. 2020;109:12–19. doi: 10.1016/j.pediatrneurol.2020.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Lefebvre S., Burglen L., Reboullet S., Clermont O., Burlet P., Viollet L., Benichou B., Cruaud C., Millasseau P., Zeviani M., et al. Identification and characterization of a spinal muscular atrophy-determining gene. Cell. 1995;80:155–165. doi: 10.1016/0092-8674(95)90460-3. [DOI] [PubMed] [Google Scholar]
- 6.Feldkotter M., Schwarzer V., Wirth R., Wienker T.F., Wirth B. Quantitative analyses of SMN1 and SMN2 based on real-time lightCycler PCR: Fast and highly reliable carrier testing and prediction of severity of spinal muscular atrophy. Am. J. Hum. Genet. 2002;70:358–368. doi: 10.1086/338627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wirth B., Brichta L., Schrank B., Lochmuller H., Blick S., Baasner A., Heller R. Mildly affected patients with spinal muscular atrophy are partially protected by an increased SMN2 copy number. Hum. Genet. 2006;119:422–428. doi: 10.1007/s00439-006-0156-7. [DOI] [PubMed] [Google Scholar]
- 8.Lorson C.L., Hahnen E., Androphy E.J., Wirth B. A single nucleotide in the SMN gene regulates splicing and is responsible for spinal muscular atrophy. Proc. Natl. Acad. Sci. USA. 1999;96:6307–6311. doi: 10.1073/pnas.96.11.6307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cartegni L., Krainer A.R. Disruption of an SF2/ASF-dependent exonic splicing enhancer in SMN2 causes spinal muscular atrophy in the absence of SMN1. Nat. Genet. 2002;30:377–384. doi: 10.1038/ng854. [DOI] [PubMed] [Google Scholar]
- 10.Kashima T., Rao N., Manley J.L. An intronic element contributes to splicing repression in spinal muscular atrophy. Proc. Natl. Acad. Sci. USA. 2007;104:3426–3431. doi: 10.1073/pnas.0700343104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lorson C.L., Strasswimmer J., Yao J.M., Baleja J.D., Hahnen E., Wirth B., Le T., Burghes A.H., Androphy E.J. SMN oligomerization defect correlates with spinal muscular atrophy severity. Nat. Genet. 1998;19:63–66. doi: 10.1038/ng0598-63. [DOI] [PubMed] [Google Scholar]
- 12.Ramos D.M., d’Ydewalle C., Gabbeta V., Dakka A., Klein S.K., Norris D.A., Matson J., Taylor S.J., Zaworski P.G., Prior T.W., et al. Age-dependent SMN expression in disease-relevant tissue and implications for SMA treatment. J. Clin. Invest. 2019;129:4817–4831. doi: 10.1172/JCI124120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wirth B. Spinal Muscular Atrophy: In the Challenge Lies a Solution. Trends Neurosci. 2021;44:306–322. doi: 10.1016/j.tins.2020.11.009. [DOI] [PubMed] [Google Scholar]
- 14.Mercuri E., Pera M.C., Scoto M., Finkel R., Muntoni F. Spinal muscular atrophy—Insights and challenges in the treatment era. Nat. Rev. Neurol. 2020;16:706–715. doi: 10.1038/s41582-020-00413-4. [DOI] [PubMed] [Google Scholar]
- 15.Vill K., Schwartz O., Blaschek A., Glaser D., Nennstiel U., Wirth B., Burggraf S., Roschinger W., Becker M., Czibere L., et al. Newborn screening for spinal muscular atrophy in Germany: Clinical results after 2 years. Orphanet J. Rare Dis. 2021;16:153. doi: 10.1186/s13023-021-01783-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Finkel R.S., Chiriboga C.A., Vajsar J., Day J.W., Montes J., De Vivo D.C., Yamashita M., Rigo F., Hung G., Schneider E., et al. Treatment of infantile-onset spinal muscular atrophy with nusinersen: A phase 2, open-label, dose-escalation study. Lancet. 2016;388:3017–3026. doi: 10.1016/S0140-6736(16)31408-8. [DOI] [PubMed] [Google Scholar]
- 17.Mendell J.R., Al-Zaidy S., Shell R., Arnold W.D., Rodino-Klapac L.R., Prior T.W., Lowes L., Alfano L., Berry K., Church K., et al. Single-Dose Gene-Replacement Therapy for Spinal Muscular Atrophy. N. Engl. J. Med. 2017;377:1713–1722. doi: 10.1056/NEJMoa1706198. [DOI] [PubMed] [Google Scholar]
- 18.Baranello G., Darras B.T., Day J.W., Deconinck N., Klein A., Masson R., Mercuri E., Rose K., El-Khairi M., Gerber M., et al. Risdiplam in Type 1 Spinal Muscular Atrophy. N. Engl. J. Med. 2021;384:915–923. doi: 10.1056/NEJMoa2009965. [DOI] [PubMed] [Google Scholar]
- 19.Ratni H., Ebeling M., Baird J., Bendels S., Bylund J., Chen K.S., Denk N., Feng Z., Green L., Guerard M., et al. Discovery of Risdiplam, a Selective Survival of Motor Neuron-2 ( SMN2) Gene Splicing Modifier for the Treatment of Spinal Muscular Atrophy (SMA) J. Med. Chem. 2018;61:6501–6517. doi: 10.1021/acs.jmedchem.8b00741. [DOI] [PubMed] [Google Scholar]
- 20.Foust K.D., Wang X., McGovern V.L., Braun L., Bevan A.K., Haidet A.M., Le T.T., Morales P.R., Rich M.M., Burghes A.H., et al. Rescue of the spinal muscular atrophy phenotype in a mouse model by early postnatal delivery of SMN. Nat. Biotechnol. 2010;28:271–274. doi: 10.1038/nbt.1610. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 21.Hua Y., Sahashi K., Rigo F., Hung G., Horev G., Bennett C.F., Krainer A.R. Peripheral SMN restoration is essential for long-term rescue of a severe spinal muscular atrophy mouse model. Nature. 2011;478:123–126. doi: 10.1038/nature10485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lefebvre S., Burglen L., Frezal J., Munnich A., Melki J. The role of the SMN gene in proximal spinal muscular atrophy. Hum. Mol. Genet. 1998;7:1531–1536. doi: 10.1093/hmg/7.10.1531. [DOI] [PubMed] [Google Scholar]
- 23.Coovert D.D., Le T.T., McAndrew P.E., Strasswimmer J., Crawford T.O., Mendell J.R., Coulson S.E., Androphy E.J., Prior T.W., Burghes A.H. The survival motor neuron protein in spinal muscular atrophy. Hum. Mol. Genet. 1997;6:1205–1214. doi: 10.1093/hmg/6.8.1205. [DOI] [PubMed] [Google Scholar]
- 24.Singh R.N., Howell M.D., Ottesen E.W., Singh N.N. Diverse role of survival motor neuron protein. Biochim. Biophys. Acta. 2017;1860:299–315. doi: 10.1016/j.bbagrm.2016.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Groen E.J.N., Talbot K., Gillingwater T.H. Advances in therapy for spinal muscular atrophy: Promises and challenges. Nat. Rev. Neurol. 2018;14:214–224. doi: 10.1038/nrneurol.2018.4. [DOI] [PubMed] [Google Scholar]
- 26.Wirth B., Brichta L., Hahnen E. Spinal muscular atrophy: From gene to therapy. Semin. Pediatr. Neurol. 2006;13:121–131. doi: 10.1016/j.spen.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 27.Oprea G.E., Krober S., McWhorter M.L., Rossoll W., Muller S., Krawczak M., Bassell G.J., Beattie C.E., Wirth B. Plastin 3 is a protective modifier of autosomal recessive spinal muscular atrophy. Science. 2008;320:524–527. doi: 10.1126/science.1155085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heesen L., Peitz M., Torres-Benito L., Holker I., Hupperich K., Dobrindt K., Jungverdorben J., Ritzenhofen S., Weykopf B., Eckert D., et al. Plastin 3 is upregulated in iPSC-derived motoneurons from asymptomatic SMN1-deleted individuals. Cell. Mol. Life Sci. 2016;73:2089–2104. doi: 10.1007/s00018-015-2084-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Riessland M., Kaczmarek A., Schneider S., Swoboda K.J., Lohr H., Bradler C., Grysko V., Dimitriadi M., Hosseinibarkooie S., Torres-Benito L., et al. Neurocalcin Delta Suppression Protects against Spinal Muscular Atrophy in Humans and across Species by Restoring Impaired Endocytosis. Am. J. Hum. Genet. 2017;100:297–315. doi: 10.1016/j.ajhg.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wolff L., Strathmann E.A., Muller I., Mahlich D., Veltman C., Niehoff A., Wirth B. Plastin 3 in health and disease: A matter of balance. Cell. Mol. Life Sci. 2021;78:5275–5301. doi: 10.1007/s00018-021-03843-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ivings L., Pennington S.R., Jenkins R., Weiss J.L., Burgoyne R.D. Identification of Ca2+-dependent binding partners for the neuronal calcium sensor protein neurocalcin delta: Interaction with actin, clathrin and tubulin. Biochem. J. 2002;363:599–608. doi: 10.1042/bj3630599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hosseinibarkooie S., Peters M., Torres-Benito L., Rastetter R.H., Hupperich K., Hoffmann A., Mendoza-Ferreira N., Kaczmarek A., Janzen E., Milbradt J., et al. The Power of Human Protective Modifiers: PLS3 and CORO1C Unravel Impaired Endocytosis in Spinal Muscular Atrophy and Rescue SMA Phenotype. Am. J. Hum. Genet. 2016;99:647–665. doi: 10.1016/j.ajhg.2016.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dimitriadi M., Sleigh J.N., Walker A., Chang H.C., Sen A., Kalloo G., Harris J., Barsby T., Walsh M.B., Satterlee J.S., et al. Conserved genes act as modifiers of invertebrate SMN loss of function defects. PLoS Genet. 2010;6:e1001172. doi: 10.1371/journal.pgen.1001172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Walsh M.B., Janzen E., Wingrove E., Hosseinibarkooie S., Muela N.R., Davidow L., Dimitriadi M., Norabuena E.M., Rubin L.L., Wirth B., et al. Genetic modifiers ameliorate endocytic and neuromuscular defects in a model of spinal muscular atrophy. BMC Biol. 2020;18:127. doi: 10.1186/s12915-020-00845-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wirth B., Mendoza-Ferreira N., Torres-Benito L. Spinal Muscular Atrophy Disease Modifiers A2. In: Paushkin S., Ko C.-P., editors. Spinal Muscular Atrophy. Academic Press; Cambridge, MA, USA: 2017. pp. 191–210. Chapter 12. [DOI] [Google Scholar]
- 36.Keller N., Paketci C., Altmueller J., Fuhrmann N., Wunderlich G., Schrank B., Unver O., Yilmaz S., Boostani R., Karimiani E.G., et al. Genomic variants causing mitochondrial dysfunction are common in hereditary lower motor neuron disease. Hum. Mutat. 2021;42:460–472. doi: 10.1002/humu.24181. [DOI] [PubMed] [Google Scholar]
- 37.Jankovic M., Novakovic I., Gamil Anwar Dawod P., Gamil Anwar Dawod A., Drinic A., Abdel Motaleb F.I., Ducic S., Nikolic D. Current Concepts on Genetic Aspects of Mitochondrial Dysfunction in Amyotrophic Lateral Sclerosis. Int. J. Mol. Sci. 2021;22:9832. doi: 10.3390/ijms22189832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McCray B.A., Scherer S.S. Axonal Charcot-Marie-Tooth Disease: From Common Pathogenic Mechanisms to Emerging Treatment Opportunities. Neurotherapeutics. 2021;18:2269–2285. doi: 10.1007/s13311-021-01099-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Canto-Santos J., Grau-Junyent J.M., Garrabou G. The Impact of Mitochondrial Deficiencies in Neuromuscular Diseases. Antioxidants. 2020;9:964. doi: 10.3390/antiox9100964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Attwell D., Laughlin S.B. An energy budget for signaling in the grey matter of the brain. J. Cereb. Blood Flow Metab. 2001;21:1133–1145. doi: 10.1097/00004647-200110000-00001. [DOI] [PubMed] [Google Scholar]
- 41.Devine M.J., Kittler J.T. Mitochondria at the neuronal presynapse in health and disease. Nat. Rev. Neurosci. 2018;19:63–80. doi: 10.1038/nrn.2017.170. [DOI] [PubMed] [Google Scholar]
- 42.Vanhauwaert R., Bharat V., Wang X. Surveillance and transportation of mitochondria in neurons. Curr. Opin. Neurobiol. 2019;57:87–93. doi: 10.1016/j.conb.2019.01.015. [DOI] [PubMed] [Google Scholar]
- 43.Smith G.M., Gallo G. The role of mitochondria in axon development and regeneration. Dev. Neurobiol. 2018;78:221–237. doi: 10.1002/dneu.22546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lopez-Manzaneda M., Fuentes-Moliz A., Tabares L. Presynaptic Mitochondria Communicate With Release Sites for Spatio-Temporal Regulation of Exocytosis at the Motor Nerve Terminal. Front. Synaptic. Neurosci. 2022;14:858340. doi: 10.3389/fnsyn.2022.858340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rangaraju V., Lauterbach M., Schuman E.M. Spatially Stable Mitochondrial Compartments Fuel Local Translation during Plasticity. Cell. 2019;176:73–84.e15. doi: 10.1016/j.cell.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 46.Shigeoka T., Jung H., Jung J., Turner-Bridger B., Ohk J., Lin J.Q., Amieux P.S., Holt C.E. Dynamic Axonal Translation in Developing and Mature Visual Circuits. Cell. 2016;166:181–192. doi: 10.1016/j.cell.2016.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yoon B.C., Jung H., Dwivedy A., O’Hare C.M., Zivraj K.H., Holt C.E. Local translation of extranuclear lamin B promotes axon maintenance. Cell. 2012;148:752–764. doi: 10.1016/j.cell.2011.11.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cioni J.M., Lin J.Q., Holtermann A.V., Koppers M., Jakobs M.A.H., Azizi A., Turner-Bridger B., Shigeoka T., Franze K., Harris W.A., et al. Late Endosomes Act as mRNA Translation Platforms and Sustain Mitochondria in Axons. Cell. 2019;176:56–72.e15. doi: 10.1016/j.cell.2018.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Benarroch E. What Is the Role of Mitochondrial Fission in Neurologic Disease? Neurology. 2022;98:662–668. doi: 10.1212/WNL.0000000000200233. [DOI] [PubMed] [Google Scholar]
- 50.Popov V., Medvedev N.I., Davies H.A., Stewart M.G. Mitochondria form a filamentous reticular network in hippocampal dendrites but are present as discrete bodies in axons: A three-dimensional ultrastructural study. J. Comp. Neurol. 2005;492:50–65. doi: 10.1002/cne.20682. [DOI] [PubMed] [Google Scholar]
- 51.Lewis T.L., Jr., Kwon S.K., Lee A., Shaw R., Polleux F. MFF-dependent mitochondrial fission regulates presynaptic release and axon branching by limiting axonal mitochondria size. Nat. Commun. 2018;9:5008. doi: 10.1038/s41467-018-07416-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang D., Ying J., Wang X., Zhao T., Yoon S., Fang Y., Zheng Q., Liu X., Yu W., Hua F. Mitochondrial Dynamics: A Key Role in Neurodegeneration and a Potential Target for Neurodegenerative Disease. Front. Neurosci. 2021;15:654785. doi: 10.3389/fnins.2021.654785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Simic G., Mladinov M., Seso Simic D., Jovanov Milosevic N., Islam A., Pajtak A., Barisic N., Sertic J., Lucassen P.J., Hof P.R., et al. Abnormal motoneuron migration, differentiation, and axon outgrowth in spinal muscular atrophy. Acta Neuropathol. 2008;115:313–326. doi: 10.1007/s00401-007-0327-1. [DOI] [PubMed] [Google Scholar]
- 54.Harding B.N., Kariya S., Monani U.R., Chung W.K., Benton M., Yum S.W., Tennekoon G., Finkel R.S. Spectrum of neuropathophysiology in spinal muscular atrophy type I. J. Neuropathol. Exp. Neurol. 2015;74:15–24. doi: 10.1097/NEN.0000000000000144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kuru S., Sakai M., Konagaya M., Yoshida M., Hashizume Y., Saito K. An autopsy case of spinal muscular atrophy type III (Kugelberg-Welander disease) Neuropathology. 2009;29:63–67. doi: 10.1111/j.1440-1789.2008.00910.x. [DOI] [PubMed] [Google Scholar]
- 56.Martinez-Hernandez R., Bernal S., Also-Rallo E., Alias L., Barcelo M.J., Hereu M., Esquerda J.E., Tizzano E.F. Synaptic defects in type I spinal muscular atrophy in human development. J. Pathol. 2013;229:49–61. doi: 10.1002/path.4080. [DOI] [PubMed] [Google Scholar]
- 57.Custer S.K., Gilson T.D., Li H., Todd A.G., Astroski J.W., Lin H., Liu Y., Androphy E.J. Altered mRNA Splicing in SMN-Depleted Motor Neuron-Like Cells. PLoS ONE. 2016;11:e0163954. doi: 10.1371/journal.pone.0163954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Goncalves I., Brecht J., Thelen M.P., Rehorst W.A., Peters M., Lee H.J., Motameny S., Torres-Benito L., Ebrahimi-Fakhari D., Kononenko N.L., et al. Neuronal activity regulates DROSHA via autophagy in spinal muscular atrophy. Sci. Rep. 2018;8:7907. doi: 10.1038/s41598-018-26347-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rossoll W., Jablonka S., Andreassi C., Kroning A.K., Karle K., Monani U.R., Sendtner M. Smn, the spinal muscular atrophy-determining gene product, modulates axon growth and localization of beta-actin mRNA in growth cones of motoneurons. J. Cell Biol. 2003;163:801–812. doi: 10.1083/jcb.200304128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fallini C., Zhang H., Su Y., Silani V., Singer R.H., Rossoll W., Bassell G.J. The survival of motor neuron (SMN) protein interacts with the mRNA-binding protein HuD and regulates localization of poly(A) mRNA in primary motor neuron axons. J. Neurosci. 2011;31:3914–3925. doi: 10.1523/JNEUROSCI.3631-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Akten B., Kye M.J., Hao L.T., Wertz M.H., Singh S., Nie D., Huang J., Merianda T.T., Twiss J.L., Beattie C.E., et al. Interaction of survival of motor neuron (SMN) and HuD proteins with mRNA cpg15 rescues motor neuron axonal deficits. Proc. Natl. Acad. Sci. USA. 2011;108:10337–10342. doi: 10.1073/pnas.1104928108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jablonka S., Beck M., Lechner B.D., Mayer C., Sendtner M. Defective Ca2+ channel clustering in axon terminals disturbs excitability in motoneurons in spinal muscular atrophy. J. Cell Biol. 2007;179:139–149. doi: 10.1083/jcb.200703187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fallini C., Donlin-Asp P.G., Rouanet J.P., Bassell G.J., Rossoll W. Deficiency of the Survival of Motor Neuron Protein Impairs mRNA Localization and Local Translation in the Growth Cone of Motor Neurons. J. Neurosci. 2016;36:3811–3820. doi: 10.1523/JNEUROSCI.2396-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bernabo P., Tebaldi T., Groen E.J.N., Lane F.M., Perenthaler E., Mattedi F., Newbery H.J., Zhou H., Zuccotti P., Potrich V., et al. In Vivo Translatome Profiling in Spinal Muscular Atrophy Reveals a Role for SMN Protein in Ribosome Biology. Cell Rep. 2017;21:953–965. doi: 10.1016/j.celrep.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dimitriadi M., Derdowski A., Kalloo G., Maginnis M.S., O’Hern P., Bliska B., Sorkac A., Nguyen K.C., Cook S.J., Poulogiannis G., et al. Decreased function of survival motor neuron protein impairs endocytic pathways. Proc. Natl. Acad. Sci. USA. 2016;113:E4377–E4386. doi: 10.1073/pnas.1600015113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wen H.L., Lin Y.T., Ting C.H., Lin-Chao S., Li H., Hsieh-Li H.M. Stathmin, a microtubule-destabilizing protein, is dysregulated in spinal muscular atrophy. Hum. Mol. Genet. 2010;19:1766–1778. doi: 10.1093/hmg/ddq058. [DOI] [PubMed] [Google Scholar]
- 67.Torres-Benito L., Neher M.F., Cano R., Ruiz R., Tabares L. SMN requirement for synaptic vesicle, active zone and microtubule postnatal organization in motor nerve terminals. PLoS ONE. 2011;6:e26164. doi: 10.1371/journal.pone.0026164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hensel N., Claus P. The Actin Cytoskeleton in SMA and ALS: How Does It Contribute to Motoneuron Degeneration? Neuroscientist. 2018;24:54–72. doi: 10.1177/1073858417705059. [DOI] [PubMed] [Google Scholar]
- 69.Miller N., Shi H., Zelikovich A.S., Ma Y.C. Motor neuron mitochondrial dysfunction in spinal muscular atrophy. Hum. Mol. Genet. 2016;25:3395–3406. doi: 10.1093/hmg/ddw262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Neve A., Trub J., Saxena S., Schumperli D. Central and peripheral defects in motor units of the diaphragm of spinal muscular atrophy mice. Mol. Cell Neurosci. 2016;70:30–41. doi: 10.1016/j.mcn.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 71.Fulceri F., Biagioni F., Limanaqi F., Busceti C.L., Ryskalin L., Lenzi P., Fornai F. Ultrastructural characterization of peripheral denervation in a mouse model of Type III spinal muscular atrophy. J. Neural Transm. 2021;128:771–791. doi: 10.1007/s00702-021-02353-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kariya S., Park G.H., Maeno-Hikichi Y., Leykekhman O., Lutz C., Arkovitz M.S., Landmesser L.T., Monani U.R. Reduced SMN protein impairs maturation of the neuromuscular junctions in mouse models of spinal muscular atrophy. Hum. Mol. Genet. 2008;17:2552–2569. doi: 10.1093/hmg/ddn156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Voigt T., Meyer K., Baum O., Schumperli D. Ultrastructural changes in diaphragm neuromuscular junctions in a severe mouse model for Spinal Muscular Atrophy and their prevention by bifunctional U7 snRNA correcting SMN2 splicing. Neuromuscul. Disord. 2010;20:744–752. doi: 10.1016/j.nmd.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 74.Xu C.C., Denton K.R., Wang Z.B., Zhang X., Li X.J. Abnormal mitochondrial transport and morphology as early pathological changes in human models of spinal muscular atrophy. Dis. Models Mech. 2016;9:39–49. doi: 10.1242/dmm.021766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Thelen M.P., Wirth B., Kye M.J. Mitochondrial defects in the respiratory complex I contribute to impaired translational initiation via ROS and energy homeostasis in SMA motor neurons. Acta Neuropathol. Commun. 2020;8:223. doi: 10.1186/s40478-020-01101-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang Y., Xu C., Ma L., Mou Y., Zhang B., Zhou S., Tian Y., Trinh J., Zhang X., Li X.J. Drug screening with human SMN2 reporter identifies SMN protein stabilizers to correct SMA pathology. Life Sci. Alliance. 2019;2:e201800268. doi: 10.26508/lsa.201800268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chen H., Chomyn A., Chan D.C. Disruption of fusion results in mitochondrial heterogeneity and dysfunction. J Biol. Chem. 2005;280:26185–26192. doi: 10.1074/jbc.M503062200. [DOI] [PubMed] [Google Scholar]
- 78.Strauss M., Hofhaus G., Schroder R.R., Kuhlbrandt W. Dimer ribbons of ATP synthase shape the inner mitochondrial membrane. EMBO J. 2008;27:1154–1160. doi: 10.1038/emboj.2008.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Frank S., Gaume B., Bergmann-Leitner E.S., Leitner W.W., Robert E.G., Catez F., Smith C.L., Youle R.J. The role of dynamin-related protein 1, a mediator of mitochondrial fission, in apoptosis. Dev. Cell. 2001;1:515–525. doi: 10.1016/S1534-5807(01)00055-7. [DOI] [PubMed] [Google Scholar]
- 80.Wakabayashi T., Karbowski M. Structural changes of mitochondria related to apoptosis. Biol. Signals Recept. 2001;10:26–56. doi: 10.1159/000046874. [DOI] [PubMed] [Google Scholar]
- 81.Simic G., Seso-Simic D., Lucassen P.J., Islam A., Krsnik Z., Cviko A., Jelasic D., Barisic N., Winblad B., Kostovic I., et al. Ultrastructural analysis and TUNEL demonstrate motor neuron apoptosis in Werdnig-Hoffmann disease. J. Neuropathol. Exp. Neurol. 2000;59:398–407. doi: 10.1093/jnen/59.5.398. [DOI] [PubMed] [Google Scholar]
- 82.Piras A., Schiaffino L., Boido M., Valsecchi V., Guglielmotto M., De Amicis E., Puyal J., Garcera A., Tamagno E., Soler R.M., et al. Inhibition of autophagy delays motoneuron degeneration and extends lifespan in a mouse model of spinal muscular atrophy. Cell Death Dis. 2017;8:3223. doi: 10.1038/s41419-017-0086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sareen D., Ebert A.D., Heins B.M., McGivern J.V., Ornelas L., Svendsen C.N. Inhibition of apoptosis blocks human motor neuron cell death in a stem cell model of spinal muscular atrophy. PLoS ONE. 2012;7:e39113. doi: 10.1371/journal.pone.0039113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Godena V.K., Ning K. Phosphatase and tensin homologue: A therapeutic target for SMA. Signal Transduct. Target. Ther. 2017;2:17038. doi: 10.1038/sigtrans.2017.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ando S., Funato M., Ohuchi K., Kameyama T., Inagaki S., Seki J., Kawase C., Tsuruma K., Shimazawa M., Kaneko H., et al. Edaravone is a candidate agent for spinal muscular atrophy: In vitro analysis using a human induced pluripotent stem cells-derived disease model. Eur. J. Pharmacol. 2017;814:161–168. doi: 10.1016/j.ejphar.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 86.Kong L., Wang X., Choe D.W., Polley M., Burnett B.G., Bosch-Marce M., Griffin J.W., Rich M.M., Sumner C.J. Impaired synaptic vesicle release and immaturity of neuromuscular junctions in spinal muscular atrophy mice. J. Neurosci. 2009;29:842–851. doi: 10.1523/JNEUROSCI.4434-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bora G., Hensel N., Rademacher S., Koyunoglu D., Sunguroglu M., Aksu-Menges E., Balci-Hayta B., Claus P., Erdem-Yurter H. Microtubule-associated protein 1B dysregulates microtubule dynamics and neuronal mitochondrial transport in spinal muscular atrophy. Hum. Mol. Genet. 2021;29:3935–3944. doi: 10.1093/hmg/ddaa275. [DOI] [PubMed] [Google Scholar]
- 88.Lin M.T., Beal M.F. Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature. 2006;443:787–795. doi: 10.1038/nature05292. [DOI] [PubMed] [Google Scholar]
- 89.Boyd P.J., Tu W.Y., Shorrock H.K., Groen E.J.N., Carter R.N., Powis R.A., Thomson S.R., Thomson D., Graham L.C., Motyl A.A.L., et al. Bioenergetic status modulates motor neuron vulnerability and pathogenesis in a zebrafish model of spinal muscular atrophy. PLoS Genet. 2017;13:e1006744. doi: 10.1371/journal.pgen.1006744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Acsadi G., Lee I., Li X., Khaidakov M., Pecinova A., Parker G.C., Huttemann M. Mitochondrial dysfunction in a neural cell model of spinal muscular atrophy. J. Neurosci. Res. 2009;87:2748–2756. doi: 10.1002/jnr.22106. [DOI] [PubMed] [Google Scholar]
- 91.Ashrafi G., Wu Z., Farrell R.J., Ryan T.A. GLUT4 Mobilization Supports Energetic Demands of Active Synapses. Neuron. 2017;93:606–615.e3. doi: 10.1016/j.neuron.2016.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Patitucci T.N., Ebert A.D. SMN deficiency does not induce oxidative stress in SMA iPSC-derived astrocytes or motor neurons. Hum. Mol. Genet. 2016;25:514–523. doi: 10.1093/hmg/ddv489. [DOI] [PubMed] [Google Scholar]
- 93.Nicholls D.G. Oxidative stress and energy crises in neuronal dysfunction. Ann. N. Y. Acad. Sci. 2008;1147:53–60. doi: 10.1196/annals.1427.002. [DOI] [PubMed] [Google Scholar]
- 94.Hayashi M., Araki S., Arai N., Kumada S., Itoh M., Tamagawa K., Oda M., Morimatsu Y. Oxidative stress and disturbed glutamate transport in spinal muscular atrophy. Brain Dev. 2002;24:770–775. doi: 10.1016/S0387-7604(02)00103-1. [DOI] [PubMed] [Google Scholar]
- 95.Wang Z.B., Zhang X., Li X.J. Recapitulation of spinal motor neuron-specific disease phenotypes in a human cell model of spinal muscular atrophy. Cell Res. 2013;23:378–393. doi: 10.1038/cr.2012.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shababi M., Habibi J., Ma L., Glascock J.J., Sowers J.R., Lorson C.L. Partial restoration of cardio-vascular defects in a rescued severe model of spinal muscular atrophy. J. Mol. Cell. Cardiol. 2012;52:1074–1082. doi: 10.1016/j.yjmcc.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lopez-Manzaneda M., Franco-Espin J., Tejero R., Cano R., Tabares L. Calcium is reduced in presynaptic mitochondria of motor nerve terminals during neurotransmission in SMA mice. Hum. Mol. Genet. 2021;30:629–643. doi: 10.1093/hmg/ddab065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Perry S.W., Norman J.P., Barbieri J., Brown E.B., Gelbard H.A. Mitochondrial membrane potential probes and the proton gradient: A practical usage guide. Biotechniques. 2011;50:98–115. doi: 10.2144/000113610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bernardi P., Di Lisa F. The mitochondrial permeability transition pore: Molecular nature and role as a target in cardioprotection. J. Mol. Cell Cardiol. 2015;78:100–106. doi: 10.1016/j.yjmcc.2014.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kroemer G., Galluzzi L., Brenner C. Mitochondrial membrane permeabilization in cell death. Physiol. Rev. 2007;87:99–163. doi: 10.1152/physrev.00013.2006. [DOI] [PubMed] [Google Scholar]
- 101.You Y., Cheng A.C., Wang M.S., Jia R.Y., Sun K.F., Yang Q., Wu Y., Zhu D., Chen S., Liu M.F., et al. The suppression of apoptosis by alpha-herpesvirus. Cell Death Dis. 2017;8:e2749. doi: 10.1038/cddis.2017.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Parker G.C., Li X., Anguelov R.A., Toth G., Cristescu A., Acsadi G. Survival motor neuron protein regulates apoptosis in an in vitro model of spinal muscular atrophy. Neurotox. Res. 2008;13:39–48. doi: 10.1007/BF03033366. [DOI] [PubMed] [Google Scholar]
- 103.Trulzsch B., Garnett C., Davies K., Wood M. Knockdown of SMN by RNA interference induces apoptosis in differentiated P19 neural stem cells. Brain Res. 2007;1183:1–9. doi: 10.1016/j.brainres.2007.09.025. [DOI] [PubMed] [Google Scholar]
- 104.Ng S.Y., Soh B.S., Rodriguez-Muela N., Hendrickson D.G., Price F., Rinn J.L., Rubin L.L. Genome-wide RNA-Seq of Human Motor Neurons Implicates Selective ER Stress Activation in Spinal Muscular Atrophy. Cell Stem Cell. 2015;17:569–584. doi: 10.1016/j.stem.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Iwahashi H., Eguchi Y., Yasuhara N., Hanafusa T., Matsuzawa Y., Tsujimoto Y. Synergistic anti-apoptotic activity between Bcl-2 and SMN implicated in spinal muscular atrophy. Nature. 1997;390:413–417. doi: 10.1038/37144. [DOI] [PubMed] [Google Scholar]
- 106.Sato K., Eguchi Y., Kodama T.S., Tsujimoto Y. Regions essential for the interaction between Bcl-2 and SMN, the spinal muscular atrophy disease gene product. Cell Death Differ. 2000;7:374–383. doi: 10.1038/sj.cdd.4400660. [DOI] [PubMed] [Google Scholar]
- 107.Young P.J., Day P.M., Zhou J., Androphy E.J., Morris G.E., Lorson C.L. A direct interaction between the survival motor neuron protein and p53 and its relationship to spinal muscular atrophy. J. Biol. Chem. 2002;277:2852–2859. doi: 10.1074/jbc.M108769200. [DOI] [PubMed] [Google Scholar]
- 108.Roy N., Mahadevan M.S., McLean M., Shutler G., Yaraghi Z., Farahani R., Baird S., Besner-Johnston A., Lefebvre C., Kang X., et al. The gene for neuronal apoptosis inhibitory protein is partially deleted in individuals with spinal muscular atrophy. Cell. 1995;80:167–178. doi: 10.1016/0092-8674(95)90461-1. [DOI] [PubMed] [Google Scholar]
- 109.Ando S., Funato M., Ohuchi K., Inagaki S., Sato A., Seki J., Kawase C., Saito T., Nishio H., Nakamura S., et al. The Protective Effects of Levetiracetam on a Human iPSCs-Derived Spinal Muscular Atrophy Model. Neurochem. Res. 2019;44:1773–1779. doi: 10.1007/s11064-019-02814-4. [DOI] [PubMed] [Google Scholar]
- 110.Saal L., Briese M., Kneitz S., Glinka M., Sendtner M. Subcellular transcriptome alterations in a cell culture model of spinal muscular atrophy point to widespread defects in axonal growth and presynaptic differentiation. RNA. 2014;20:1789–1802. doi: 10.1261/rna.047373.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Zhao D.Y., Gish G., Braunschweig U., Li Y., Ni Z., Schmitges F.W., Zhong G., Liu K., Li W., Moffat J., et al. SMN and symmetric arginine dimethylation of RNA polymerase II C-terminal domain control termination. Nature. 2016;529:48–53. doi: 10.1038/nature16469. [DOI] [PubMed] [Google Scholar]
- 112.Fallini C., Rouanet J.P., Donlin-Asp P.G., Guo P., Zhang H., Singer R.H., Rossoll W., Bassell G.J. Dynamics of survival of motor neuron (SMN) protein interaction with the mRNA-binding protein IMP1 facilitates its trafficking into motor neuron axons. Dev. Neurobiol. 2014;74:319–332. doi: 10.1002/dneu.22111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lauria F., Bernabo P., Tebaldi T., Groen E.J.N., Perenthaler E., Maniscalco F., Rossi A., Donzel D., Clamer M., Marchioretto M., et al. SMN-primed ribosomes modulate the translation of transcripts related to spinal muscular atrophy. Nat. Cell Biol. 2020;22:1239–1251. doi: 10.1038/s41556-020-00577-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Rage F., Boulisfane N., Rihan K., Neel H., Gostan T., Bertrand E., Bordonne R., Soret J. Genome-wide identification of mRNAs associated with the protein SMN whose depletion decreases their axonal localization. RNA. 2013;19:1755–1766. doi: 10.1261/rna.040204.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bleck C.K.E., Kim Y., Willingham T.B., Glancy B. Subcellular connectomic analyses of energy networks in striated muscle. Nat. Commun. 2018;9:5111. doi: 10.1038/s41467-018-07676-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Willingham T.B., Ajayi P.T., Glancy B. Subcellular Specialization of Mitochondrial Form and Function in Skeletal Muscle Cells. Front. Cell Dev. Biol. 2021;9:757305. doi: 10.3389/fcell.2021.757305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Vincent A.E., White K., Davey T., Philips J., Ogden R.T., Lawless C., Warren C., Hall M.G., Ng Y.S., Falkous G., et al. Quantitative 3D Mapping of the Human Skeletal Muscle Mitochondrial Network. Cell Rep. 2019;27:321. doi: 10.1016/j.celrep.2019.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kuznetsov A.V., Javadov S., Margreiter R., Hagenbuchner J., Ausserlechner M.J. Analysis of Mitochondrial Function, Structure, and Intracellular Organization In Situ in Cardiomyocytes and Skeletal Muscles. Int. J. Mol. Sci. 2022;23:2252. doi: 10.3390/ijms23042252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Slavin M.B., Memme J.M., Oliveira A.N., Moradi N., Hood D.A. Regulatory networks coordinating mitochondrial quality control in skeletal muscle. Am. J. Physiol. Cell Physiol. 2022;322:C913–C926. doi: 10.1152/ajpcell.00065.2022. [DOI] [PubMed] [Google Scholar]
- 120.Leduc-Gaudet J.P., Hussain S.N.A., Barreiro E., Gouspillou G. Mitochondrial Dynamics and Mitophagy in Skeletal Muscle Health and Aging. Int. J. Mol. Sci. 2021;22:8179. doi: 10.3390/ijms22158179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Territo P.R., Mootha V.K., French S.A., Balaban R.S. Ca(2+) activation of heart mitochondrial oxidative phosphorylation: Role of the F(0)/F(1)-ATPase. Am. J. Physiol. Cell Physiol. 2000;278:C423–C435. doi: 10.1152/ajpcell.2000.278.2.C423. [DOI] [PubMed] [Google Scholar]
- 122.Michelucci A., Liang C., Protasi F., Dirksen R.T. Altered Ca(2+) Handling and Oxidative Stress Underlie Mitochondrial Damage and Skeletal Muscle Dysfunction in Aging and Disease. Metabolites. 2021;11:424. doi: 10.3390/metabo11070424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Singh N.N., Hoffman S., Reddi P.P., Singh R.N. Spinal muscular atrophy: Broad disease spectrum and sex-specific phenotypes. Biochim. Biophys. Acta-Mol. Basis Dis. 2021;1867:166063. doi: 10.1016/j.bbadis.2020.166063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hayhurst M., Wagner A.K., Cerletti M., Wagers A.J., Rubin L.L. A cell-autonomous defect in skeletal muscle satellite cells expressing low levels of survival of motor neuron protein. Dev. Biol. 2012;368:323–334. doi: 10.1016/j.ydbio.2012.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Khayrullina G., Moritz K.E., Schooley J.F., Fatima N., Viollet C., McCormack N.M., Smyth J.T., Doughty M.L., Dalgard C.L., Flagg T.P., et al. SMN-deficiency disrupts SERCA2 expression and intracellular Ca(2+) signaling in cardiomyocytes from SMA mice and patient-derived iPSCs. Skelet. Muscle. 2020;10:16. doi: 10.1186/s13395-020-00232-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Sambrook P., Rickards D., Cumming W.J. CT muscle scanning in the evaluation of patients with spinal muscular atrophy (SMA) Neuroradiology. 1988;30:487–495. doi: 10.1007/BF00339688. [DOI] [PubMed] [Google Scholar]
- 127.Millino C., Fanin M., Vettori A., Laveder P., Mostacciuolo M.L., Angelini C., Lanfranchi G. Different atrophy-hypertrophy transcription pathways in muscles affected by severe and mild spinal muscular atrophy. BMC Med. 2009;7:14. doi: 10.1186/1741-7015-7-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ling K.K., Gibbs R.M., Feng Z., Ko C.P. Severe neuromuscular denervation of clinically relevant muscles in a mouse model of spinal muscular atrophy. Hum. Mol. Genet. 2011;21:185–195. doi: 10.1093/hmg/ddr453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Fulceri F., Bartalucci A., Paparelli S., Pasquali L., Biagioni F., Ferrucci M., Ruffoli R., Fornai F. Motor neuron pathology and behavioral alterations at late stages in a SMA mouse model. Brain Res. 2012;1442:66–75. doi: 10.1016/j.brainres.2011.12.056. [DOI] [PubMed] [Google Scholar]
- 130.Feng W., Gubitz A.K., Wan L., Battle D.J., Dostie J., Golembe T.J., Dreyfuss G. Gemins modulate the expression and activity of the SMN complex. Hum. Mol. Genet. 2005;14:1605–1611. doi: 10.1093/hmg/ddi168. [DOI] [PubMed] [Google Scholar]
- 131.Shafey D., Cote P.D., Kothary R. Hypomorphic Smn knockdown C2C12 myoblasts reveal intrinsic defects in myoblast fusion and myotube morphology. Exp. Cell Res. 2005;311:49–61. doi: 10.1016/j.yexcr.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 132.Boyer J.G., Deguise M.O., Murray L.M., Yazdani A., De Repentigny Y., Boudreau-Lariviere C., Kothary R. Myogenic program dysregulation is contributory to disease pathogenesis in spinal muscular atrophy. Hum. Mol. Genet. 2014;23:4249–4259. doi: 10.1093/hmg/ddu142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Bricceno K.V., Martinez T., Leikina E., Duguez S., Partridge T.A., Chernomordik L.V., Fischbeck K.H., Sumner C.J., Burnett B.G. Survival motor neuron protein deficiency impairs myotube formation by altering myogenic gene expression and focal adhesion dynamics. Hum. Mol. Genet. 2014;23:4745–4757. doi: 10.1093/hmg/ddu189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kim J.K., Jha N.N., Feng Z., Faleiro M.R., Chiriboga C.A., Wei-Lapierre L., Dirksen R.T., Ko C.P., Monani U.R. Muscle-specific SMN reduction reveals motor neuron-independent disease in spinal muscular atrophy models. J. Clin. Investig. 2020;130:1271–1287. doi: 10.1172/JCI131989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Gavrilina T.O., McGovern V.L., Workman E., Crawford T.O., Gogliotti R.G., DiDonato C.J., Monani U.R., Morris G.E., Burghes A.H. Neuronal SMN expression corrects spinal muscular atrophy in severe SMA mice while muscle-specific SMN expression has no phenotypic effect. Hum. Mol. Genet. 2008;17:1063–1075. doi: 10.1093/hmg/ddm379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hamilton G., Gillingwater T.H. Spinal muscular atrophy: Going beyond the motor neuron. Trends Mol. Med. 2013;19:40–50. doi: 10.1016/j.molmed.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 137.Stump A.D., Dillon-White M., Gu S. Molecular evolution of the moonlighting protein SMN in metazoans. Comp. Biochem. Physiol. Part D Genomics Proteomics. 2013;8:220–230. doi: 10.1016/j.cbd.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 138.Osman E.Y., Bolding M.R., Villalon E., Kaifer K.A., Lorson Z.C., Tisdale S., Hao Y., Conant G.C., Pires J.C., Pellizzoni L., et al. Functional characterization of SMN evolution in mouse models of SMA. Sci. Rep. 2019;9:9472. doi: 10.1038/s41598-019-45822-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Gobernado J.M., Gosalvez M., Cortina C., Lousa M., Riva C., Gimeno A. Mitochondrial functions in chronic spinal muscular atrophy. J. Neurol. Neurosurg. Psychiatry. 1980;43:546–549. doi: 10.1136/jnnp.43.6.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ohtaki E. Secondarily reduced cytochrome c oxidase activity in various neuromuscular disorders. Brain Dev. 1990;12:326–333. doi: 10.1016/S0387-7604(12)80315-9. [DOI] [PubMed] [Google Scholar]
- 141.Pons R., Andreetta F., Wang C.H., Vu T.H., Bonilla E., DiMauro S., De Vivo D.C. Mitochondrial myopathy simulating spinal muscular atrophy. Pediatr. Neurol. 1996;15:153–158. doi: 10.1016/0887-8994(96)00118-X. [DOI] [PubMed] [Google Scholar]
- 142.Sperl W., Skladal D., Gnaiger E., Wyss M., Mayr U., Hager J., Gellerich F.N. High resolution respirometry of permeabilized skeletal muscle fibers in the diagnosis of neuromuscular disorders. Mol. Cell Biochem. 1997;174:71–78. doi: 10.1023/A:1006880529195. [DOI] [PubMed] [Google Scholar]
- 143.Vielhaber S., Winkler K., Kirches E., Kunz D., Buchner M., Feistner H., Elger C.E., Ludolph A.C., Riepe M.W., Kunz W.S. Visualization of defective mitochondrial function in skeletal muscle fibers of patients with sporadic amyotrophic lateral sclerosis. J. Neurol. Sci. 1999;169:133–139. doi: 10.1016/S0022-510X(99)00236-1. [DOI] [PubMed] [Google Scholar]
- 144.Jongpiputvanich S., Sueblinvong T., Norapucsunton T. Mitochondrial respiratory chain dysfunction in various neuromuscular diseases. J. Clin. Neurosci. 2005;12:426–428. doi: 10.1016/j.jocn.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 145.Ripolone M., Ronchi D., Violano R., Vallejo D., Fagiolari G., Barca E., Lucchini V., Colombo I., Villa L., Berardinelli A., et al. Impaired Muscle Mitochondrial Biogenesis and Myogenesis in Spinal Muscular Atrophy. JAMA Neurol. 2015;72:666–675. doi: 10.1001/jamaneurol.2015.0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Berger A., Mayr J.A., Meierhofer D., Fotschl U., Bittner R., Budka H., Grethen C., Huemer M., Kofler B., Sperl W. Severe depletion of mitochondrial DNA in spinal muscular atrophy. Acta Neuropathol. 2003;105:245–251. doi: 10.1007/s00401-002-0638-1. [DOI] [PubMed] [Google Scholar]
- 147.Bevan A.K., Hutchinson K.R., Foust K.D., Braun L., McGovern V.L., Schmelzer L., Ward J.G., Petruska J.C., Lucchesi P.A., Burghes A.H., et al. Early heart failure in the SMNDelta7 model of spinal muscular atrophy and correction by postnatal scAAV9-SMN delivery. Hum. Mol. Genet. 2010;19:3895–3905. doi: 10.1093/hmg/ddq300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Sheng L., Wan B., Feng P., Sun J., Rigo F., Bennett C.F., Akerman M., Krainer A.R., Hua Y. Downregulation of Survivin contributes to cell-cycle arrest during postnatal cardiac development in a severe spinal muscular atrophy mouse model. Hum. Mol. Genet. 2018;27:486–498. doi: 10.1093/hmg/ddx418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Chan D.C. Mitochondrial Dynamics and Its Involvement in Disease. Annu. Rev. Pathol. 2020;15:235–259. doi: 10.1146/annurev-pathmechdis-012419-032711. [DOI] [PubMed] [Google Scholar]
- 150.Bowerman M., Anderson C.L., Beauvais A., Boyl P.P., Witke W., Kothary R. SMN, profilin IIa and plastin 3: A link between the deregulation of actin dynamics and SMA pathogenesis. Mol. Cell. Neurosci. 2009;42:66–74. doi: 10.1016/j.mcn.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 151.Giesemann T., Rathke-Hartlieb S., Rothkegel M., Bartsch J.W., Buchmeier S., Jockusch B.M., Jockusch H. A role for polyproline motifs in the spinal muscular atrophy protein SMN. Profilins bind to and colocalize with smn in nuclear gems. J. Biol. Chem. 1999;274:37908–37914. doi: 10.1074/jbc.274.53.37908. [DOI] [PubMed] [Google Scholar]
- 152.Fan L., Simard L.R. Survival motor neuron (SMN) protein: Role in neurite outgrowth and neuromuscular maturation during neuronal differentiation and development. Hum. Mol. Genet. 2002;11:1605–1614. doi: 10.1093/hmg/11.14.1605. [DOI] [PubMed] [Google Scholar]
- 153.Schultz J., Lee S.J., Cole T., Hoang H.D., Vibbert J., Cottee P.A., Miller M.A., Han S.M. The secreted MSP domain of C. elegans VAPB homolog VPR-1 patterns the adult striated muscle mitochondrial reticulum via SMN-1. Development. 2017;144:2175–2186. doi: 10.1242/dev.152025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Egile C., Rouiller I., Xu X.P., Volkmann N., Li R., Hanein D. Mechanism of filament nucleation and branch stability revealed by the structure of the Arp2/3 complex at actin branch junctions. PLoS Biol. 2005;3:1902–1909. doi: 10.1371/journal.pbio.0030383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Moore A.S., Wong Y.C., Simpson C.L., Holzbaur E.L. Dynamic actin cycling through mitochondrial subpopulations locally regulates the fission-fusion balance within mitochondrial networks. Nat. Commun. 2016;7:12886. doi: 10.1038/ncomms12886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Giganti A., Plastino J., Janji B., Van Troys M., Lentz D., Ampe C., Sykes C., Friederich E. Actin-filament cross-linking protein T-plastin increases Arp2/3-mediated actin-based movement. J. Cell Sci. 2005;118:1255–1265. doi: 10.1242/jcs.01698. [DOI] [PubMed] [Google Scholar]
- 157.Rajendra T.K., Gonsalvez G.B., Walker M.P., Shpargel K.B., Salz H.K., Matera A.G. A Drosophila melanogaster model of spinal muscular atrophy reveals a function for SMN in striated muscle. J. Cell Biol. 2007;176:831–841. doi: 10.1083/jcb.200610053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Walker M.P., Rajendra T.K., Saieva L., Fuentes J.L., Pellizzoni L., Matera A.G. SMN complex localizes to the sarcomeric Z-disc and is a proteolytic target of calpain. Hum. Mol. Genet. 2008;17:3399–3410. doi: 10.1093/hmg/ddn234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Berciano M.T., Castillo-Iglesias M.S., Val-Bernal J.F., Lafarga V., Rodriguez-Rey J.C., Lafarga M., Tapia O. Mislocalization of SMN from the I-band and M-band in human skeletal myofibers in spinal muscular atrophy associates with primary structural alterations of the sarcomere. Cell Tissue Res. 2020;381:461–478. doi: 10.1007/s00441-020-03236-3. [DOI] [PubMed] [Google Scholar]
- 160.Houdebine L., D’Amico D., Bastin J., Chali F., Desseille C., Rumeau V., Soukkari J., Oudot C., Rouquet T., Bariohay B., et al. Low-Intensity Running and High-Intensity Swimming Exercises Differentially Improve Energy Metabolism in Mice With Mild Spinal Muscular Atrophy. Front. Physiol. 2019;10:1258. doi: 10.3389/fphys.2019.01258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Hellbach N., Peterson S., Haehnke D., Shankar A., LaBarge S., Pivaroff C., Saenger S., Thomas C., McCarthy K., Ebeling M., et al. Impaired myogenic development, differentiation and function in hESC-derived SMA myoblasts and myotubes. PLoS ONE. 2018;13:e0205589. doi: 10.1371/journal.pone.0205589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Brito M.D., Silva L., Siena A., Chipara M., Sarkar S., Rosenstock T.R. Oxygen Consumption Evaluation: An Important Indicator of Metabolic State, Cellular Function, and Cell Fate Along Neural Deregulation. Methods Mol. Biol. 2021;2240:207–230. doi: 10.1007/978-1-0716-1091-6_15. [DOI] [PubMed] [Google Scholar]
- 163.Deguise M.O., Pileggi C., De Repentigny Y., Beauvais A., Tierney A., Chehade L., Michaud J., Llavero-Hurtado M., Lamont D., Atrih A., et al. SMN Depleted Mice Offer a Robust and Rapid Onset Model of Nonalcoholic Fatty Liver Disease. Cell. Mol. Gastroenterol. Hepatol. 2021;12:354–377.e3. doi: 10.1016/j.jcmgh.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Harpey J.P., Charpentier C., Paturneau-Jouas M., Renault F., Romero N., Fardeau M. Secondary metabolic defects in spinal muscular atrophy type II. Lancet. 1990;336:629–630. doi: 10.1016/0140-6736(90)93426-P. [DOI] [PubMed] [Google Scholar]
- 165.Tein I., Sloane A.E., Donner E.J., Lehotay D.C., Millington D.S., Kelley R.I. Fatty acid oxidation abnormalities in childhood-onset spinal muscular atrophy: Primary or secondary defect(s)? Pediatr. Neurol. 1995;12:21–30. doi: 10.1016/0887-8994(94)00100-G. [DOI] [PubMed] [Google Scholar]
- 166.Djordjevic S.A., Milic-Rasic V., Brankovic V., Kosac A., Dejanovic-Djordjevic I., Markovic-Denic L., Djuricic G., Milcanovic N., Kovacevic S., Petrovic H., et al. Glucose and lipid metabolism disorders in children and adolescents with spinal muscular atrophy types 2 and 3. Neuromuscul. Disord. 2021;31:291–299. doi: 10.1016/j.nmd.2021.02.002. [DOI] [PubMed] [Google Scholar]
- 167.Sproule D.M., Montes J., Montgomery M., Battista V., Koenigsberger D., Shen W., Punyanitya M., De Vivo D.C., Kaufmann P. Increased fat mass and high incidence of overweight despite low body mass index in patients with spinal muscular atrophy. Neuromuscul. Disord. 2009;19:391–396. doi: 10.1016/j.nmd.2009.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Davis R.H., Miller E.A., Zhang R.Z., Swoboda K.J. Responses to Fasting and Glucose Loading in a Cohort of Well Children with Spinal Muscular Atrophy Type II. J. Pediatrics. 2015;167:1362–1368.e1. doi: 10.1016/j.jpeds.2015.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Bowerman M., Michalski J.P., Beauvais A., Murray L.M., DeRepentigny Y., Kothary R. Defects in pancreatic development and glucose metabolism in SMN-depleted mice independent of canonical spinal muscular atrophy neuromuscular pathology. Hum. Mol. Genet. 2014;23:3432–3444. doi: 10.1093/hmg/ddu052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Bowerman M., Swoboda K.J., Michalski J.P., Wang G.S., Reeks C., Beauvais A., Murphy K., Woulfe J., Screaton R.A., Scott F.W., et al. Glucose metabolism and pancreatic defects in spinal muscular atrophy. Ann. Neurol. 2012;72:256–268. doi: 10.1002/ana.23582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Shababi M., Habibi J., Yang H.T., Vale S.M., Sewell W.A., Lorson C.L. Cardiac defects contribute to the pathology of spinal muscular atrophy models. Hum. Mol. Genet. 2010;19:4059–4071. doi: 10.1093/hmg/ddq329. [DOI] [PubMed] [Google Scholar]
- 172.Escobales N., Nunez R.E., Javadov S. Mitochondrial angiotensin receptors and cardioprotective pathways. Am. J. Physiol. Heart Circ. Physiol. 2019;316:H1426–H1438. doi: 10.1152/ajpheart.00772.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Barbieri E., Sestili P. Reactive oxygen species in skeletal muscle signaling. J. Signal Transduct. 2012;2012:982794. doi: 10.1155/2012/982794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Pollack M., Phaneuf S., Dirks A., Leeuwenburgh C. The role of apoptosis in the normal aging brain, skeletal muscle, and heart. Ann. N. Y. Acad. Sci. 2002;959:93–107. doi: 10.1111/j.1749-6632.2002.tb02086.x. [DOI] [PubMed] [Google Scholar]
- 175.Musaro A., Fulle S., Fano G. Oxidative stress and muscle homeostasis. Curr. Opin. Clin. Nutr. Metab. Care. 2010;13:236–242. doi: 10.1097/MCO.0b013e3283368188. [DOI] [PubMed] [Google Scholar]
- 176.Pena-Blanco A., Garcia-Saez A.J. Bax, Bak and beyond—Mitochondrial performance in apoptosis. FEBS J. 2018;285:416–431. doi: 10.1111/febs.14186. [DOI] [PubMed] [Google Scholar]
- 177.Zhong X., Song Z., Song X. Survival motor neuron protein protects H9c2 cardiomyocytes from hypoxia-induced cell injury by reducing apoptosis. Clin. Exp. Pharmacol. Physiol. 2020;47:1808–1815. doi: 10.1111/1440-1681.13369. [DOI] [PubMed] [Google Scholar]
- 178.Seo J., Singh N.N., Ottesen E.W., Sivanesan S., Shishimorova M., Singh R.N. Oxidative Stress Triggers Body-Wide Skipping of Multiple Exons of the Spinal Muscular Atrophy Gene. PLoS ONE. 2016;11:e0154390. doi: 10.1371/journal.pone.0154390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Wijngaarde C.A., Blank A.C., Stam M., Wadman R.I., van den Berg L.H., van der Pol W.L. Cardiac pathology in spinal muscular atrophy: A systematic review. Orphanet J. Rare Dis. 2017;12:67. doi: 10.1186/s13023-017-0613-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Lin X., Li J.J., Qian W.J., Zhang Q.J., Wang Z.F., Lu Y.Q., Dong E.L., He J., Wang N., Ma L.X., et al. Modeling the differential phenotypes of spinal muscular atrophy with high-yield generation of motor neurons from human induced pluripotent stem cells. Oncotarget. 2017;8:42030–42042. doi: 10.18632/oncotarget.14925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Rubio-Gozalbo M.E., Smeitink J.A., Ruitenbeek W., Ter Laak H., Mullaart R.A., Schuelke M., Mariman E.C., Sengers R.C., Gabreels F.J. Spinal muscular atrophy-like picture, cardiomyopathy, and cytochrome c oxidase deficiency. Neurology. 1999;52:383–386. doi: 10.1212/WNL.52.2.383. [DOI] [PubMed] [Google Scholar]
- 182.Martin L.J. Biology of mitochondria in neurodegenerative diseases. Prog. Mol. Biol. Transl. Sci. 2012;107:355–415. doi: 10.1016/B978-0-12-385883-2.00005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Memme J.M., Erlich A.T., Phukan G., Hood D.A. Exercise and mitochondrial health. J. Physiol. 2021;599:803–817. doi: 10.1113/JP278853. [DOI] [PubMed] [Google Scholar]
- 184.Lewelt A., Krosschell K.J., Stoddard G.J., Weng C., Xue M., Marcus R.L., Gappmaier E., Viollet L., Johnson B.A., White A.T., et al. Resistance strength training exercise in children with spinal muscular atrophy. Muscle Nerve. 2015;52:559–567. doi: 10.1002/mus.24568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Sheikh A.M., Vissing J. Exercise therapy for muscle and lower motor neuron diseases. Acta Myol. 2019;38:215–232. [PMC free article] [PubMed] [Google Scholar]
- 186.Bartels B., Montes J., van der Pol W.L., de Groot J.F. Physical exercise training for type 3 spinal muscular atrophy. Cochrane Database Syst. Rev. 2019;3:CD012120. doi: 10.1002/14651858.CD012120.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Bora G., Subasi-Yildiz S., Yesbek-Kaymaz A., Bulut N., Alemdaroglu I., Tunca-Yilmaz O., Topaloglu H., Karaduman A.A., Erdem-Yurter H. Effects of Arm Cycling Exercise in Spinal Muscular Atrophy Type II Patients: A Pilot Study. J. Child Neurol. 2018;33:209–215. doi: 10.1177/0883073817750500. [DOI] [PubMed] [Google Scholar]
- 188.Ng S.Y., Mikhail A., Ljubicic V. Mechanisms of exercise-induced survival motor neuron expression in the skeletal muscle of spinal muscular atrophy-like mice. J. Physiol. 2019;597:4757–4778. doi: 10.1113/JP278454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Farooq F., Abadia-Molina F., MacKenzie D., Hadwen J., Shamim F., O’Reilly S., Holcik M., MacKenzie A. Celecoxib increases SMN and survival in a severe spinal muscular atrophy mouse model via p38 pathway activation. Hum. Mol. Genet. 2013;22:3415–3424. doi: 10.1093/hmg/ddt191. [DOI] [PubMed] [Google Scholar]
- 190.Deguise M.O., Baranello G., Mastella C., Beauvais A., Michaud J., Leone A., De Amicis R., Battezzati A., Dunham C., Selby K., et al. Abnormal fatty acid metabolism is a core component of spinal muscular atrophy. Ann. Clin. Transl. Neurol. 2019;6:1519–1532. doi: 10.1002/acn3.50855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Deguise M.O., Chehade L., Kothary R. Metabolic Dysfunction in Spinal Muscular Atrophy. Int. J. Mol. Sci. 2021;22:5913. doi: 10.3390/ijms22115913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Wang L., Gao J., Liu J., Siedlak S.L., Torres S., Fujioka H., Huntley M.L., Jiang Y., Ji H., Yan T., et al. Mitofusin 2 Regulates Axonal Transport of Calpastatin to Prevent Neuromuscular Synaptic Elimination in Skeletal Muscles. Cell Metab. 2018;28:400–414.e408. doi: 10.1016/j.cmet.2018.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Powis R.A., Karyka E., Boyd P., Come J., Jones R.A., Zheng Y., Szunyogova E., Groen E.J., Hunter G., Thomson D., et al. Systemic restoration of UBA1 ameliorates disease in spinal muscular atrophy. JCI Insight. 2016;1:e87908. doi: 10.1172/jci.insight.87908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Bernkopf D.B., Jalal K., Bruckner M., Knaup K.X., Gentzel M., Schambony A., Behrens J. Pgam5 released from damaged mitochondria induces mitochondrial biogenesis via Wnt signaling. J. Cell Biol. 2018;217:1383–1394. doi: 10.1083/jcb.201708191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Behrens J., Solga R., Ziemann A., Rastetter R.H., Berwanger C., Herrmann H., Noegel A.A., Clemen C.S. Coronin 1C-free primary mouse fibroblasts exhibit robust rearrangements in the orientation of actin filaments, microtubules and intermediate filaments. Eur. J. Cell Biol. 2016;95:239–251. doi: 10.1016/j.ejcb.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 196.Simon C.M., Van Alstyne M., Lotti F., Bianchetti E., Tisdale S., Watterson D.M., Mentis G.Z., Pellizzoni L. Stasimon Contributes to the Loss of Sensory Synapses and Motor Neuron Death in a Mouse Model of Spinal Muscular Atrophy. Cell Rep. 2019;29:3885–3901.e5. doi: 10.1016/j.celrep.2019.11.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Van Alstyne M., Lotti F., Dal Mas A., Area-Gomez E., Pellizzoni L. Stasimon/Tmem41b localizes to mitochondria-associated ER membranes and is essential for mouse embryonic development. Biochem. Biophys. Res. Commun. 2018;506:463–470. doi: 10.1016/j.bbrc.2018.10.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Ahmad S., Wang Y., Shaik G.M., Burghes A.H., Gangwani L. The zinc finger protein ZPR1 is a potential modifier of spinal muscular atrophy. Hum. Mol. Genet. 2012;21:2745–2758. doi: 10.1093/hmg/dds102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Chang H.C., Dimlich D.N., Yokokura T., Mukherjee A., Kankel M.W., Sen A., Sridhar V., Fulga T.A., Hart A.C., Van Vactor D., et al. Modeling spinal muscular atrophy in Drosophila. PLoS ONE. 2008;3:e3209. doi: 10.1371/journal.pone.0003209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.McCormack N.M., Abera M.B., Arnold E.S., Gibbs R.M., Martin S.E., Buehler E., Chen Y.C., Chen L., Fischbeck K.H., Burnett B.G. A high-throughput genome-wide RNAi screen identifies modifiers of survival motor neuron protein. Cell Rep. 2021;35:109125. doi: 10.1016/j.celrep.2021.109125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Bordet T., Berna P., Abitbol J.L., Pruss R.M. Olesoxime (TRO19622): A Novel Mitochondrial-Targeted Neuroprotective Compound. Pharmaceuticals. 2010;3:345–368. doi: 10.3390/ph3020345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Muntoni F., Bertini E., Comi G., Kirschner J., Lusakowska A., Mercuri E., Scoto M., van der Pol W.L., Vuillerot C., Burdeska A., et al. Long-term follow-up of patients with type 2 and non-ambulant type 3 spinal muscular atrophy (SMA) treated with olesoxime in the OLEOS trial. Neuromuscul. Disord. 2020;30:959–969. doi: 10.1016/j.nmd.2020.10.008. [DOI] [PubMed] [Google Scholar]
- 203.Xu J., Du W., Zhao Y., Lim K., Lu L., Zhang C., Li L. Mitochondria targeting drugs for neurodegenerative diseases-Design, mechanism and application. Acta Pharm. Sin. B. 2022;12:2778–2789. doi: 10.1016/j.apsb.2022.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Zerres K., Rudnik-Schoneborn S., Forkert R., Wirth B. Genetic basis of adult-onset spinal muscular atrophy. Lancet. 1995;346:1162. doi: 10.1016/S0140-6736(95)91835-3. [DOI] [PubMed] [Google Scholar]
- 205.Van Alstyne M., Tattoli I., Delestree N., Recinos Y., Workman E., Shihabuddin L.S., Zhang C., Mentis G.Z., Pellizzoni L. Gain of toxic function by long-term SMN overexpression in the mouse motor circuit; Proceedings of the Cure SMA Meeting 2020; Orlando, FL, USA. 11–14 June 2020. [Google Scholar]
- 206.Anderson K.N., Baban D., Oliver P.L., Potter A., Davies K.E. Expression profiling in spinal muscular atrophy reveals an RNA binding protein deficit. Neuromuscul. Disord. 2004;14:711–722. doi: 10.1016/j.nmd.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 207.Balabanian S., Gendron N.H., MacKenzie A.E. Histologic and transcriptional assessment of a mild SMA model. Neurol. Res. 2007;29:413–424. doi: 10.1179/016164107X159243. [DOI] [PubMed] [Google Scholar]
- 208.Staropoli J.F., Li H., Chun S.J., Allaire N., Cullen P., Thai A., Fleet C.M., Hua Y., Bennett C.F., Krainer A.R., et al. Rescue of gene-expression changes in an induced mouse model of spinal muscular atrophy by an antisense oligonucleotide that promotes inclusion of SMN2 exon 7. Genomics. 2015;105:220–228. doi: 10.1016/j.ygeno.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 209.See K., Yadav P., Giegerich M., Cheong P.S., Graf M., Vyas H., Lee S.G., Mathavan S., Fischer U., Sendtner M., et al. SMN deficiency alters Nrxn2 expression and splicing in zebrafish and mouse models of spinal muscular atrophy. Hum. Mol. Genet. 2014;23:1754–1770. doi: 10.1093/hmg/ddt567. [DOI] [PubMed] [Google Scholar]
- 210.Gao X., Xu J., Chen H., Xue D., Pan W., Zhou C., Ma Y.C., Ma L. Defective Expression of Mitochondrial, Vacuolar H(+)-ATPase and Histone Genes in a C. elegans Model of SMA. Front. Genet. 2019;10:410. doi: 10.3389/fgene.2019.00410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Huo Q., Kayikci M., Odermatt P., Meyer K., Michels O., Saxena S., Ule J., Schumperli D. Splicing changes in SMA mouse motoneurons and SMN-depleted neuroblastoma cells: Evidence for involvement of splicing regulatory proteins. RNA Biol. 2014;11:1430–1446. doi: 10.1080/15476286.2014.996494. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.