Abstract
Atypical Candida spp. infections are rising, mostly due to the increasing numbers of immunocompromised patients. The most common Candida spp. is still Candida albicans; however, in the last decades, there has been an increase in non-Candida albicans Candida species infections (e.g., Candida glabrata, Candida parapsilosis, and Candida tropicalis). Furthermore, in the last 10 years, the reports on uncommon yeasts, such as Candida lusitaniae, Candida intermedia, or Candida norvegensis, have also worryingly increased. This review summarizes the information, mostly related to the last decade, regarding the infections, diagnosis, treatment, and resistance of these uncommon Candida species. In general, there has been an increase in the number of articles associated with the incidence of these species. Additionally, in several cases, there was a suggestive antifungal resistance, particularly with azoles, which is troublesome for therapeutic success.
Keywords: Candida kefyr, Candida lusitaniae, Candida famata, Candida guilliermondii, Candida rugosa, Candida nivariensis, Candida lipolytica, Candida bracarensis, Candida africana, Candida blankii, Candida pulcherrima
1. Introduction
Deaths from fungal diseases may be five to six times higher than what is actually reported and may yield an economic burden of USD $24.3 billion [1]. Although most, but not all, yeasts belonging to the Candida genus are commensal microorganisms, they are commonly linked to superficial or candidemia infections [2,3], being associated with high mortality and morbidity rates [4,5]. Indeed, Candida albicans is still the most common Candida spp. described in candidiasis; however, non-Candida albicans Candida species (NCACs) have been rising [6,7]. Candida albicans, Candida glabrata (updated nomenclature Nakaseomyces glabrataa [8,9]), Candida tropicalis, Candida parapsilosis, and Candida krusei (updated nomenclature: Pichia kudriavzevii [8,9]) are responsible for, approximately, 9 out of 10 fungal infections [3,10]. Notably, in the last decade, emerging and atypical yeasts have been reported as an increased cause of fungal infections in immunocompromised and/or hospitalized patients [11,12]. Preventing or treating these infections successfully requires nationwide epidemiological and etiological data [13].
CHROMagar™ Candida, Polimerase Chain Reaction (PCR), or Matrix-Assisted Laser Desorption/Ionisation Time-Of-Flight Mass Spectrometry (MALDI-TOF MS) are commonly used to quickly identify yeast species [14]. With regards to the antibiotic susceptibility tests, the Minimal Inhibitory Concentrations (MIC) of antifungals (e.g., amphotericin B, 5-fluorocytosine, fluconazole, and caspofungin) must be determined according to the reference document (European Committee on Antimicrobial Susceptibility Testing, EUCAST [15], or Clinical and Laboratory Standards Institute, CLSI [16], guidelines) [14]. For most rare Candida spp., there is a lack of information on clinical breakpoints and antifungal susceptibility profiles. This is a serious issue in clinical practice, for both interpretations and for choosing the appropriate therapy [17,18]. Nonetheless, it has been described that the prevalence of these non-common Candida spp. and their susceptibility profiles can differ; therefore, their correct identification is critical [10]. The use of molecular methods (e.g., PCR) [10]. or retrospective reexamination of isolates help can reveal ambiguous species [14].
For any fungal infection, it is considered that the reference methodologies for the susceptibility tests are strongly recommended and important to guide antifungal therapy. Additionally, individualized approaches should also be considered [17,19].
This review intends to gather reported information on candidiasis related to atypical Candida spp. from the last decade. For this, we used the National Library of Medicine website (NIH, PubMed®—Medline), the words “Candida” + “infection” + “x”—x meaning “kefyr”, “norvegensis”, “inconspicua”, “famata”, “guilliermondii”, “lipolytica”, “rugosa”, “pararugosa”, “lusitaniae”, “pelliculosa”, “nivariensis”, “bracarensis”, “intermedia”, “africana”, “blankii”, and “pulcherrima” using the NCBI filters, mostly for years 2011–2021. Non-C. albicans, non-C. parapsilosis complex, non-C. glabrata complex, non-C. tropicalis, and non-C. krusei which have been particularly critical in terms of candidiasis the last years were included in this review.
2. Uncommon Candida spp.: Infections, Treatment, and Resistance
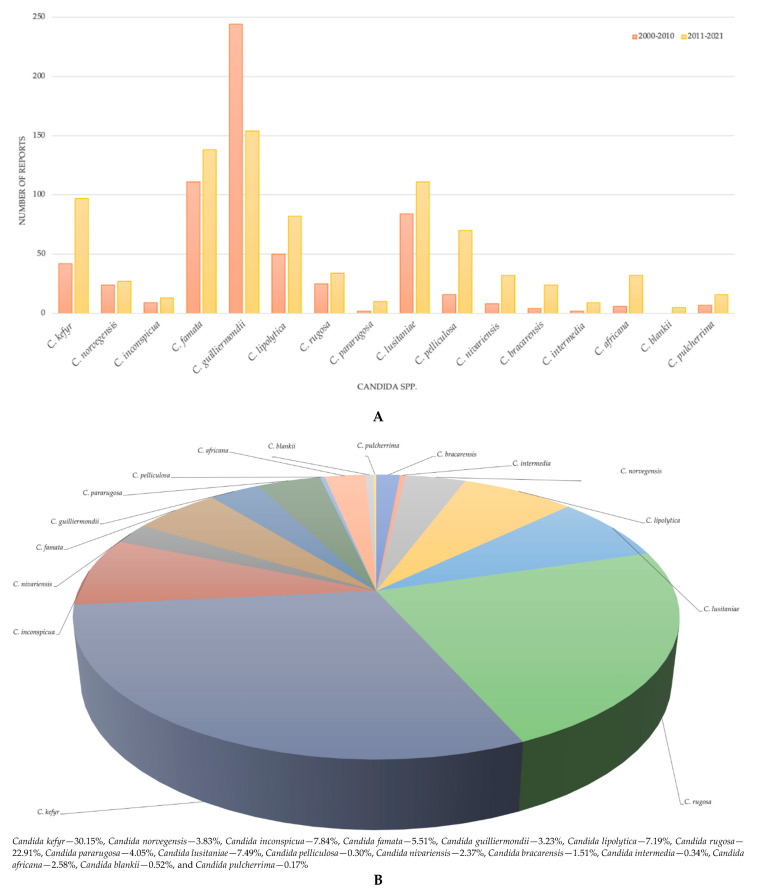
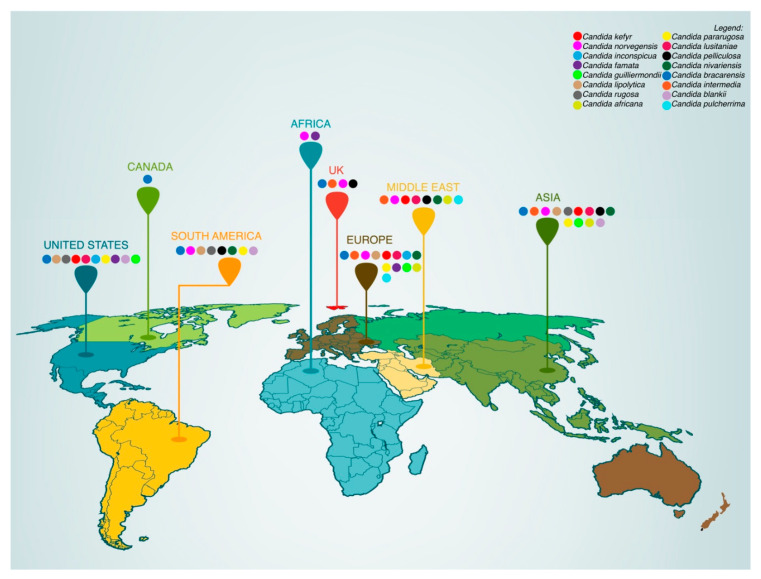
There have been several reports describing the association of uncommon NCACs to fungal infections. Among them, Candida kefyr, Candida norvegensis, Candida inconspicua, Candida famata, Candida guilliermondii, Candida lipolytica, Candida rugosa, Candida pararugosa, Candida lusitaniae, Candida pelliculosa, Candida nivariensis, Candida bracarensis, Candida intermedia, Candida africana, Candida blankii, and Candida pulcherrima are discussed in particular (Figure 1A,B and Figure 2).
Figure 1.
(A) Number of reports published between 2000 and 2010 and 2011 and 2021 associated with rare Candida sp. (B) Data/Statistics: (A) the number of reports determined using PubMed® filters; (B) percentages calculated from the n of each rare Candida species and n of all rare Candida species considered in this review, the reports between 2011 and 2021, according to the search made in NIH and PubMed®—Medline.
Figure 2.
Worldwide incidence distribution of rare Candida species. (Data/Statistics: countries reported in papers published between 2011 and 2021, according to the search made in NIH and PubMed®—Medline).
It is relevant to note that, although they are no longer considered as members of the genus Candida [8,9], the authors continued to address them here as Candida, as other reports have doing since the new names have been published. This will ease its recognition and the association between the infection and the case reports. The name of the new nomenclature will be displayed in parentheses in each section. The next sections describe the infections, treatment, and resistance reported for these Candida species.
2.1. Candida kefyr (New Nomenclature: Kluyveromyces marxianus or Candida pseudotropicalis)
Candida kefyr is an emerging and uncommon NCACs that is becoming more frequent over recent years. This fungal pathogen is diagnosed by histology, PCR, and DNA sequencing and has been reported in both superficial and systemic infections. Infections are of big concern in highly immunocompromised patients, and recent surveillance studies have reported that many isolates of C. kefyr are susceptible [20,21,22,23,24,25,26], but some have higher rates of resistance against established antifungals (amphotericin B, itraconazole, voriconazole, posaconazole, fluconazole, caspofungin micafungin, and anidulafungin) [27,28,29,30,31] (Table 1). A study at John’s Hopkins Hospital, USA, was performed, in which 83 patients were included and 8 patients (9.6%) were reported with C. kefyr colonization [29]. An unusual case of C. kefyr was reported in the bloodstream of an immunocompromised patient [30]. Biofilms of C. kefyr were reported in certain patient populations of Hungary, and amphotericin B, fluconazole, caspofungin, and micafungin were used for the treatment [31]. The treatment options for patients affected by these fungal infections have increased over the last few years; however, studies have also shown that delays (mostly due to the diagnosis and identification of C. kefyr) in the initiation of appropriate antifungal therapy ended in poor clinical compliance and outcomes [32]. This uncommon infection possesses additional diagnostic and therapeutic challenges [32]. C. kefyr has shown a particular high propensity (due to colonization) to cause disease and, therefore, resistance against the above-mentioned antifungals, worsening the treatment strategies [32]. Table 1 provides the compiled information of this species.
Table 1.
General information and characteristics of the candidiasis described for Candida kefyr.
| Invasive/Noninvasive Candidiasis (n Human Cases/Strains/Isolates) |
Identification Methods |
Imaging Test |
Antifungal Susceptibility |
Antifungal Resistance |
Antifungal Treatment |
Other Treatments (e.g., Probiotics, Natural Compounds, Antivirals) |
Outcome (n) |
Reference(s) |
|---|---|---|---|---|---|---|---|---|
| (noninvasive) Cutaneous candidiasis (n = 1) |
Carbohydrate fermentation test |
Microscopy | Yes | NR | Miconazole cream and fusidic cream |
Tenofovir, lamivudine, and efavirenz |
Alive (n = 1) |
[22] |
| (invasive) Bloodstream infection (n = 1) |
Culture | Microscopy | No at low dose (100-200 mg fluconazole) | Yes | Fluconazole (high and prolonged dose) |
NR | Successfully treated with 3 months use of fluconazole (n = 1) |
[30] |
| (noninvasive) Infection at the interface of graft and host cornea (n = 1) |
MIC | Optical coherence tomography | Yes | No | Fluconazole, voriconazole | Dexamethasone | Alive (n = 1) |
[33] |
| (invasive) Infection at blood, respiratory, and urine samples (n = 69) |
PCR, antifungal susceptibility testing | NR | Some strains were susceptible | Fluconazole and voriconazole, caspofungin and micafungin, amphotericin B | Fluconazole, voriconazole, caspofungin, micafungin, amphotericin B | NR | NA | [27] |
| (invasive) Bloodstream infection (n = 1) |
MIC, genome sequencing | MRI | Yes | NR | Fluconazole, posaconazole | Trimethoprim, sulfamethoxazole |
Alive (n = 1) |
[25] |
| (invasive) Tubo-ovarian abscess (n = 1) |
Culture | CT scan | Yes | No | Fluconazole | Consumption of organic dairy products |
Alive (n = 1) |
[23] |
| (invasive and noninvasive) Superficial and/or invasive infections (n = 2) |
Anti-fungal susceptibility testing, Mass spectrometry | NR | Yes | No | Amphotericin B, itraconazole, voriconazole, posaconazole, fluconazole, caspofungin micafungin, anidulafungin | NR | NA | [34] |
| (invasive) Derived from blood, urine, bronchus, abdominal, and throat samples (n = 10) |
Antifungal susceptibility testing, | Scanning electron microscopy | Lower in vitro susceptibility |
Development of resistance | Fluconazole, amphotericin B, caspofungin, micafungin | No | NA | [31] |
| (noninvasive) Mucocutaneous candidiasis (n = 10) |
Antifungal susceptibility testing, PCR, Sequencing | NR | Yes | No | Fluconazole, itraconazole amphotericin B | No | NA | [24] |
| (invasive) Bloodstream infection (n = 3) |
Biochemical and molecular methods | NR | Susceptible to most of the antifungals | Amphotericin B | Fluconazole, voriconazole, caspo/anidulafungin, amphotericin B |
No | NA | [28] |
| (invasive) Bloodstream infection (n = 1) |
PCR, sequencing of the ITS region ofrDNA | NR | Yes | No | Amphotericin B, itraconazole, voriconazole, posaconazole, fluconazole, caspofungin micafungin, anidulafungin |
No | NA | [21] |
| (invasive) Bloodstream infection (n = 2) |
Gram staining, and germ tube test | Microscopy | Yes | No | Azoles, echinocandins |
No | NA | [20] |
| (invasive) (n = 83) |
Antifungal susceptibility testing, PCR | NR | No | Yes | Micafungin, liposomal amphotericin B, flucytosine | Yogurt | All alive (n = 83) |
[29] |
| (invasive) Fungal sinusitis (n = 1) |
Germ tube and sugar assimilation test | NR | Yes | No | Amphotericin B | No | Recovered completely (n = 1) |
[35] |
| (invasive) Blood, bile and stool infection (n = 1) |
Antifungal susceptibility testing, PCR | NR | No | Yes | Caspofungin, micafungin, and anidulafungin | No | Recovered completely (n = 1) |
[36] |
|
Saliva (n = 92) |
Antifungal susceptibility testing, RAPD | NR | Yes | No | Fluconazole and itraconazole |
No | Alive (n = 92) |
[37] |
| (invasive and noninvasive) Blood, saliva, urine, broncho alveolar lavage (n = 410) |
Germ tube and chlamydospore production tests | NR | Yes | Resistant to Itraconazole | Ketoconazole, itraconazole, voriconazole, caspofungin, amphotericin B | No | No death reported | [38] |
| (invasive) Systemic candidiasis (n = 1) |
Ellipsometer test, PCR | NR | Yes | No | Liposomal amphotericin B, fluconazole | Broad spectrum antibiotics |
Recovered completely (n = 1) |
[39] |
| (invasive) Blood and urine samples (n = 3) |
Culture, RAPD, ophthalmologic | Echocardiography, ultrasound check | Yes | No | Liposomal amphotericin B, fluconazole, and itraconazole | No | No death reported (n = 3) |
[40] |
MIC: Minimal inhibitory concentrations; NA: Not applicable, because the research is performed on fungal strains/clinical isolates; NR: Not reported; MALDI-TOF MS: matrix-assisted laser desorption ionization mass spectrometry.
2.2. Candida norvegensis (New Nomenclature: Pichia norvegensis)
Candida norvegensis was identified in the sputum of three asthmatic patients in 1954, Norway [41], and the first case of a C. norvegensis peritonitis linked with peritoneal dialysis was reported in a renal transplant patient who developed C. norvegensis peritonitis [42]. Since then, only a few cases of C. norvegensis infection have been reported, mostly occurring in patients with cancer or HIV (Table 1) [43,44,45]. According to a recent study, the rate of C. norvegensis isolation grew by 5–10-fold in the previous decade [18]. The susceptibility of C. norvegensis to fluconazole and voriconazole showed that 41% of the isolates were resistant to fluconazole and 92% were sensitive to voriconazole, despite a recent increase in the number of voriconazole-resistant strains. Amphotericin B has long been regarded as the treatment of choice for C. norvegensis infections, even though the level of evidence is relatively poor due to the uncommon reports of infection [46]. The toxicity of amphotericin B, on the other hand, may limit its usage in solid organ transplant patients. Several reports have shown that C. norvegensis isolates are susceptible to echinocandins [47,48,49] (Table 2).
Table 2.
General information and characteristics of candidiasis described for Candida norvegensis.
| Invasive/Noninvasive Candidiasis (n Human Cases/Strains/Isolates) |
Identification Methods |
Imaging Test |
Antifungal Susceptibility | Antifungal Resistance |
Antifungal Treatment |
Other Treatments (e.g., Probiotics, Natural Compounds, Antivirals) |
Outcome (n) |
Reference(s) |
|---|---|---|---|---|---|---|---|---|
| (invasive) Clinical isolates (n = 14) |
MIC, Fungicidal and fungistatic activity | NR | Amphotericin B | Fluconazole, itraconazole, voriconazole, posaconazole |
NA | NA | NA | [50] |
| (invasive) Oral and systemic candidiasis of HIV patients (n = 1) |
Growth on Hicrome Candida, germ tube test, clamydospore formation on corn meal agar, and API20C for sugar assimilation | NR | Amphotericin B, fluconazole | NA | NA | NA | NA | [51] |
| (invasive) Clinical isolate from HIV patient (n = 1) |
Culture | microscopy | Fluconazole itraconazole voriconazole amphotericin B | NA | No treatment with antifungal or antimicrobial agents | NA | NA | [52] |
| (invasive) Oropharyngeal candidiasis in HIV patient (2.9% had C. norvegensis infection) (n = 4) |
Culture, germ tube and chlamydosporulation tests | microscopy | ND | ND | Nystatin and clotrimazole | NA | NA | [53] |
| (invasive) Clinical Isolates from oral cavity, stools/anal, respiratory, urine and, blood/catheter of Candidemia patients (n = 2) |
Aux- anogram panel ID 32C Gene sequencing |
NR | Itraconazole, voriconazole, amphotericin B, caspofungine, posaconazole |
Fluconazole | Fluconazole | Antibiotic | All alive | [54] |
| (invasive candidiasis) in HCV-related cirrhosis and hepatocarcinoma (n = 1) |
blood cultures polymerase chain reaction-sequencing |
NR | Anidulafungin | Azoles | Anidulafungin | Vancomycin and piperacillin/tazobactam, and linezolid plus meropenem | Alive | [55] |
| (invasive candidiasis) in hepatocarcinoma (n = 1) |
Blood cultures MALDI-TOF MS |
NR | Amphotericin B, itraconazole, voriconazole, caspofungin | Flucytosine Fluconazole |
Fluconazole, anidulafungin |
Meropenem, vancomycin, amikacin, and prophylactic | Died | [56] |
| (invasive candidiasis) in peritonitis (n = 1) |
Blood culture | CT Scan-abdomen | Voriconazole | NA | Fluconazole, itraconazole | NA | Alive | [57] |
MIC: Minimal inhibitory concentrations; NA: Not applicable, because the research is performed on fungal strains/clinical isolates; NR: Not reported; MALDI-TOF MS: matrix-assisted laser desorption ionization mass spectrometry.
2.3. Candida inconspicua (New Nomenclature: Pichia cactophila)
The relative global incidence of C. inconspicua (formerly Torulopsis inconspicua) is rare but recurrent, and its prevalence has increased over 10-fold in the last few years [58]. Complications were also mostly reported from immunocompromised patients [59]. C. inconspicua was reported to be resistant to azoles but showed a susceptibility pattern with other antifungals, such as echinocandins and amphotericin B [54,59,60,61]. Due to the distinguished increase in reports of fluconazole resistance in this species of Candida, echinocandins are currently the first choice for the treatment of this infection (Table 3). Novel insights on the emergence, genetic diversity, infection pattern, molecular characteristics, and other associated information are needed for C. inconspicua [62].
Table 3.
General information and characteristics of candidiasis described for Candida inconspicua.
| Invasive/Noninvasive Candidiasis (n Human Cases/Strains/Isolates) |
Identification Methods |
Imaging Test |
Antifungal Susceptibility |
Antifungal Resistance |
Antifungal Treatment |
Other Treatments (e.g., Probiotics, Natural Compounds, Antivirals) |
Outcome (n) |
Reference(s) |
|---|---|---|---|---|---|---|---|---|
| (noninvasive) Sample collected from alcoholic beverages (n = NR) |
PCR, Sequencing, Enzyme profiling | NR | Amphotericin B and micafungin | Itraconazole, fluonazole, |
Itraconazole, fluconazole, amphotericin B and micafungin | No | NA | [40] |
| (invasive and noninvasive) Samples from oral cavity, anal/stools, urine respiratory, blood/catheter (n = 12) |
Ellipsometer test, MIC | NR | Caspofungin | Fluconazole-resistant | Itraconazole, voriconazole, posaconazole isavuconazole, fluconazole, amphotericin B and caspofungin | Broad-spectrum antibiotic |
Died (n = 1) |
[42] |
| (invasive) Blood sample (n = 2) |
MIC, Fungicidal and fungistatic activity | NR | Echinocandins | Azoles | Fluconazole, caspofungin | No | NA | [43] |
| (invasive) Systemic mycosis (n = 168) |
Antifungal susceptibility and Ellipsometer test, MALDI-TOF MS | NR | Susceptible to echinocandins, polyenes | Azoles | Itraconazole, voriconazole, posaconazole, isavuconazole, fluconazole, Caspofungin, micafungin, anidulafungin, Amphotericin B, |
No | NA | [44] |
MIC: Minimal inhibitory concentrations; NA: Not applicable, because the research is performed on fungal strains/clinical isolates; NR: Not reported; MALDI-TOF MS: matrix-assisted laser desorption ionization mass spectrometry.
2.4. Candida lipolytica (New Nomenclature: Yarrowia lipolytica)
Candida lipolytica can be found in the environment, as well in meat and dairy products, particularly cheese [63]. It is occasionally discovered as a colonizer, in asymptomatic people’s feces, oropharyngeal swabs, sputum, and skin swabs [64]. Aromatic compounds, organic acids, polyalcohols, emulsifiers, and surfactants are all produced by their strong secretory activity, which is widely used in the food, detergent, and pharmaceutical sectors [63,65,66]. Although C. lipolytica was once thought to have a low virulence, it is now widely recognized as a cause of sporadic cases and nosocomial clusters of human infections, particularly catheter-related suppurative thrombophlebitis and fungemia associated with biofilm formation in immunocompromised or critically ill patients who require long-term care (Table 4) [45,48,49]. Other clinical conditions have been documented, including non-catheter-related fungemia, traumatic eye infection, and the acute aggravation of chronic sinusitis [64,67]. Most of the research on C. lipolytica infections were case reports or short case series [64,67,68]. Trabelsi and colleagues detailed the epidemiological risk factors and clinical outcomes of 55 cases of C. lipolytica fungemia in Tunisia, as well as some information on the isolates’ in vitro sensitivity to a few antifungal medications [65]. However, in this large case series, data concerning the correlative microbiological features, such as phenotypic and genotypic identification, as well as in vitro susceptibility test findings for newer antifungal medications such as echinocandins and posaconazole, were absent. Recently, Zhao et al. described the epidemiological and clinical features of 13 cases of C. lipolytica fungemia in this multicenter, a prospective surveillance study in China, as well as the in vitro susceptibility of this emerging fungal pathogen to nine antifungal drugs, including the newer azoles and echinocandins [69]. In that study, the authors summarized that all isolates had low MICs to voriconazole, amphotericin B, and echinocandins but also demonstrated the need to establish standardized protocols to determine the in vitro antifungal susceptibility for C. lipolytica using different testing methods [69].
Table 4.
General information and characteristics of candidiasis described for C. lypolitica.
| Invasive/Noninvasive Candidiasis (n Human Cases/Strains/Isolates) |
Identification Methods |
Imaging Test |
Antifungal Susceptibility |
Antifungal Resistance |
Antifungal Treatment |
Other Treatments (e.g., Probiotics, Natural Compounds, Antivirals) |
Outcome (n) |
Reference(s) |
|---|---|---|---|---|---|---|---|---|
| (invasive) Clinical isolates (n = 27) |
MIC, Fungicidal and fungistatic activity | NR | Amphotericin B, voriconazole |
Anidulafungin, micafungin |
NR | NA | NR | [50] |
| (invasive) Catheter-related candidemia/Acute pancreatitis (n = 1) |
Blood culture using VITEK 2 YST system | NR | Itraconazole, voriconazole, 5-flucytosine, amphotericin B |
NA | Fluconazole, micafungin |
Flomoxef | Alive | [67] |
| (invasive) Catheter-related candidemia/severe oral mucositis (n = 1) |
Blood cultures | Microscopy | Fluconazole, itraconazole, amphotericin B and caspofungin | 5-flucytosine | Caspofungin, fluconazole |
Cefoperazone-sulbactam and amikacin meropenem, teicoplanin |
Alive | [70] |
| (invasive) Bloodstream infections/ (invasive) Clinical isolates (n = 20) (endocarditis, fungemia) |
Blood cultures and RNA Sequencing |
Microscopy | Amphotericin B, posaconazole, voriconazole, caspofungin | Fluconazole, flucytosine | NR | NA | NR | [71] |
| (invasive) Yarrowia lipolytica fungemia (n = 13) |
Blood cultures | Microscopy | Voriconazole, caspofungin, micafungin, anidulafungin, amphotericin B |
Fluconazole, itraconazole and posaconazole |
Fluconazole | NA | Alive (n = 10) 3 patients died even after treatment with fluconazole |
[69] |
| Invasive candidiasis (n = 16) isolates of C. lipolytica | Vitek and API yeast identification systems | NR | Voriconazole echinocandins | Amphotericin B, fluconazole | Amphotericin B | NA | NR | [72] |
| (invasive) Fungemia (n = 2) |
Blood cultures | Microscopy | Voriconazole, caspofungin, amphotericin B, posaconazole, itraconazole, ketoconazole |
Fluconazole | Caspofungin, voriconazole |
NA | All alive | [73] |
| (invasive) Catheter-Related Candidemia caused by C. lipolytica/blood and the central venous catheter (n = 1) |
Blood cultures Biochemical tests |
NR | Amphotericin B | Azoles | Trimethoprim-sulfamethoxazole, amphotericin B |
Cyclosporine, acyclovir |
Died | [74] |
| (invasive) Catheter-Related Fungemia caused by C. lipolytica (n = 3) |
Blood culturesBiochemical tests (2) Corneal biopsy culture (1) |
NR | Fluconazole, Micafungin (n = 2); Itraconazole, voriconazole, amphotericin B (n = 1) |
Fluconazole and 5-flucytosine (n = 1) | Fluconazole | Natamycin, imipenem |
All alive | [68] |
| (invasive) Candida lipolytica fungemia (n = 5) (paediatric patients) |
Blood cultures | Microscopy | Amphotericin B. Very low susceptibility to fluconazole and itraconazole |
NR | Patient 1 and 5: fluconazole Patient 2: no treatment Patient 3 and 4: amphotericin B |
NA | All alive | [75] |
| (invasive) Fungemia/Clinical isolates (n = 58) from blood samples, urine, and vaginal site |
Blood culture Biochemical tests DNA sequencing |
Microscopy | Fluconazole, posaconazole, itraconazole | Low susceptibility to flucytosine, amphotericin B (n = 3), ketoconazole (n = 2), caspofungin (n = 2), both voriconazole and caspofungin (n = 1) both amphotericin B and ketoconazole (n = 21) |
NR | NA | NA | [76] |
| (invasive) C. lipolytica fungemia/septicemia (n = 32) |
Blood cultures | Microscopy | Amphotericin B (97% of the isolates), fluconazole (69% of the isolates) |
NR | NR | NA | Died (n = 12) Alive (n = 20) |
[77] |
| (invasive) C. lipolytica fungemia (n = 1) |
Diabetic mellitus, renal failure/blood cultures | Microscopy | Itraconazole, voriconazole, amphotericin B, posaconazole, isavuconazole, anidulafungin |
Fluconazole | Caspofungin | NA | Died | [78] |
| (invasive) Y. lipolytica fungemia associated with central venous catheter (n = 14) |
Blood cultures sequencing |
Microscopy | Caspofungin, micafungin, anidulafungi, amphotericin B | Azoles | Fluconazole | NA | Died (n = 3) Alive (n = 11) |
[69] |
MIC: Minimal inhibitory concentrations; NA: Not applicable, because the research is performed on fungal strains/clinical isolates; NR: Not reported; MALDI-TOF MS: matrix-assisted laser desorption ionization mass spectrometry.
2.5. Candida lusitaniae (Updated Nomenclature: Clavispora lusitaniae)
Candida lusitaniae accounts for 0.2–9.4% of all Candida isolates from blood or other sterile places [79] and has been linked to amphotericin B resistance in the past (Table 5). Although there are no standardized protocols for assessing Candida susceptibility to amphotericin B, the current recommendations propose that any Candida species with an amphotericin B MIC > 1 g/mL be deemed resistant [80]. According to recent research [81], 98% of C. lusitaniae initial bloodstream isolates were amphotericin B (MIC 0.313–0.625 µg/mL)-sensitive, and 96% were fluconazole-susceptible. Another investigation found that clinical isolates collected before antifungal medication had significant frequencies of amphotericin B resistance [82]. There was no mention of the subsequent susceptibility patterns or clinical outcomes in any of these studies. Others have reported clinical failures associated with increases in amphotericin B MICs during amphotericin B treatment [81,83,84], and C. lusitaniae is known to switch between amphotericin B susceptibility and resistance in vitro [85]. Sometimes, even an extremely high concentration of amphotericin B (1 g/mL) failed to treat C. lusitaniae fungemia [83]. It can be speculated that this resistance might be related to mutations in the ergosterol biosynthetic pathway, with direct effects on gene expression. Then, a selective gene expression in the adaptive response to amphotericin B may occur, with high-frequency reversible phenotypic switching from susceptibility to resistance associated with distinct morphologies, as it happens with other Candida spp. [86].
Table 5.
General information and characteristics of candidiasis described for Candida lusitaniae.
| Invasive/Noninvasive Candidiasis (n Human Cases/Strains/Isolates) |
Identification Methods |
Imaging Test |
Antifungal Susceptibility |
Antifungal Resistance |
Antifungal Treatment |
Other Treatments (e.g., Probiotics, Natural Compounds, Antivirals) |
Outcome (n) |
Reference(s) |
|---|---|---|---|---|---|---|---|---|
| (invasive) C. lusitaniae (n = 2) |
Blood culture Urine culture |
Microscopy Chest radiograph |
Liposomal Amphotericin-B, Fluconazole, 5-flucytosine |
NR | Liposomal Amphotericin B Vancomycin Amphotericin B deoxycholate |
NA | Died (n = 1) Alive (n = 1) |
[87] |
| (invasive) C. lusitaniae (n = 1) |
Blood culture | Microscopy | NR | NR | Fluconazole | Vancomycin, piperacillin/tazobactam, and levofloxacin | Alive | [88] |
| (invasive) C. lusitaniae (n = 8) |
Blood culture | Microscopy PCR |
Amphotericin B, fluconazole, voriconazole, caspofungin, micafungin, anidulafungin | Fluconazole (Only two isolates) | Amphotericin B Fluconazole, Caspofungin (in 2 only) |
Ampicillin and amikacin | Died (n = 3) Alive (n = 5) |
[89] |
| (invasive) C. lusitaniae Candidemia (n = 1) |
Blood culture | Microscopy | Fluconazole | Amphotericin B | Amphotericin B, fluconazole | NA | Alive | [90] |
| (invasive) C. lusitaniae Candidemia (n = 1) |
Blood culture | Microscopy | Amphotericin B, fluconazole 5-flucytosine Itraconazole, |
NR | Fluconazole | NA | Alive | [91] |
| (invasive) C. lusitaniae Candidemia (n = 2) |
Blood culture Stool culture |
Microscopy | AmphotericinB flucytosine | Ketoconazole and miconazole | Amphotericin B ketoconazole |
NA | Died (n = 1) Alive (n = 1) |
[92] |
| (invasive) C. lusitaniae fingemia (n = 1) |
Blood culture Stool culture |
Microscopy | NR | AmphotericinB | Fluconazole | Doxycycline clarithromycin |
Alive | [93] |
MIC: Minimal inhibitory concentrations; NA: Not applicable, because the research is performed on fungal strains/clinical isolates; NR: Not reported; MALDI-TOF MS: matrix-assisted laser desorption ionization mass spectrometry.
2.6. Candida famata (New Nomenclature: Debaryomyces hansenii)
Very rare cases of candidemia have been reported with Candida famata (Table 6). They are found in food, marine, and terrestrial environments and are being recognized as potential emerging pathogens that cause human candidiasis. A 16-year old patient with Hodgkin’s disease undergoing chemotherapy was reported with this fungus. The patient received voriconazole for 3 weeks and improved [94]. Another study involved eight C. famata samples that showed resistance to fluconazole but susceptibility to posaconazole and caspofungin [95]. In another report involving two hospitalized patients with central venous catheters, C. famata isolates reduced their susceptibility to azoles and echinocandins. The patients were treated and cured with liposomal amphotericin B therapy [96]. Septic shock has been reported in healthy young multi-traumatic immunocompetent male patients due to this yeast. After the initiation of amphotericin B, the patient quickly recovered from sepsis and was discharged from the hospital [97]. These few case reports summarized the routine antifungal susceptibility testing in patients with candidemia to guide the optimal antifungal therapy.
Table 6.
General information and characteristics of candidiasis described for Candida famata and Candida guilliermondii.
| Invasive/NonInvasive Candidiasis (n Human Cases/Strains/Isolates) |
Identification Methods |
Imaging Test |
Antifungal Susceptibility |
Antifungal Resistance |
Antifungal Treatment |
Other Treatments (e.g., Probiotics, Natural Compounds, Antivirals) |
Outcome (n) |
Reference(s) |
|---|---|---|---|---|---|---|---|---|
| Candida famata | ||||||||
| (invasive) C. famata (n = 1) |
Hodgkin’s disease, blood culture | Microscopy | Voriconazole | NR | voriconazole | NA | Alive | [94] |
| (invasive) C. famata (n = 8) |
Urine culture | Microscopy | Posaconazole, caspofungin |
Fluconazole | Posaconazole | NA | No death | [95] |
| (invasive) C. famata (n = 2) |
Blood culture | Microscopy | Reduced to echinocandins, azoles |
Azole resistance reported | Liposomal amphotericin B | NA | No death | [96] |
| (invasive) C. famata (n = 1) |
Blood cultures | Partial amplification and sequencing of the 26S ribosomal DNA gene | Anidulafungin and micafungin | Fluconazole | Amphotericin B | NA | Alive | [97] |
| Candida guilliermondii | ||||||||
| (non-invasive) C. guilliermondii (n = 17) |
Blood sample | Amplification and sequencing of the ITS1-5.8S-ITS2 region | NR | Fluconazole and echinocandins | Amphotericin B | NA | NR | [98] |
| (invasive) C. guilliermondii (n = 1) |
Blood cultures | Microscopy | NR | Fluconazole | Patient died despite of amphotericin B therapy | NA | Died despite of amphotericin B therapy | [99] |
| (invasive) C. guilliermondii (n = 47) |
Blood cultures | PCR- restriction fragment length polymorphism | Caspofungin, micafungin and anidulafungin | NR | NR | NA | No | [100] |
2.7. Candida guilliermondii (New Nomenclature: Meyerozyma guilliermondii)
Candida guilliermondii is a rarely isolated and reported fungal pathogen from a clinical specimen. A very low mortality rate was associated with this species; however, it is known to be an opportunistic emerging pathogen causing candidiasis often associated with cancer patients [98]. The C. guilliermondii complex has been described by high antifungal resistance to fluconazole and echinocandins in 22 patients with Candida infection (C. guilliermondii (n = 17) and C. fermentati (n = 5)) [98]. In 1985, Dick et al. reported a case of a 52-year-old woman with candidemia due to C. guilliermondii [99]. The patient died regardless of amphotericin B therapy [99]. Fifty-two patients with infections from the C. guilliermondii complex (C. guilliermondii (n = 77) and C. fermentati (n = 5)) were studied by Chen et al. [100]. In this study, 98%, 100%, and 98% of C. guilliermondii isolates were susceptible to caspofungin, micafungin, and anidulafungin, respectively. There was a good in vitro activity of the above-mentioned antifungals against C. guilliermondii complex isolates (Table 6) [101].
2.8. Candida rugosa (New Nomenclature: Diutina rugosa)
Candida rugosa has lately been highlighted as one of the emerging fungal pathogens [101] and a source of invasive fungal diseases [102]. Before 1985, when catheter-related fungemia was documented at two distinct institutions in the United States, fungemia caused by C. rugosa remained unknown [103,104]. Thereafter, Dube et al. [105] reported 15 cases of candidemia caused by C. rugosa in burned patients treated with topical nystatin in a U.S. hospital. The infections had no evident cause, but the isolates were determined to be resistant to nystatin and had a reduced sensitivity to amphotericin B and fluconazole [105]. A cluster of six occurrences of candidemia caused by C. rugosa has recently been described in Brazil [106]. Two of the cases included breakthrough infections in patients being treated with amphotericin B, and all four patients who were given this medication died [106]. C. rugosa was a common colonizer of high-risk patients, accounting for 44% of 32 consecutive episodes of fungemia at one Brazilian tertiary care hospital, according to the follow-up monitoring study [107] (Table 7). These data suggest that C. rugosa can lead to catheter-related fungemia in critically ill patients. It can be transmitted from patient to patient in hospitals and be endemic in some institutions. It may also be resistant to polyenes and fluconazole [101]. In addition to these observations, nothing much is known about the epidemiology, frequency, and antifungal susceptibility profile of this rare Candida species. [102].
Table 7.
General information and characteristics of the candidiasis described for Candida rugosa.
| Invasive/Noninvasive Candidiasis (n Human Cases/Strains/Isolates) |
Identification Methods |
Imaging Test |
Antifungal Susceptibility |
Antifungal Resistance |
Antifungal Treatment |
Other Treatments (e.g., Probiotics, Natural Compounds, Antivirals) |
Outcome (n) |
Reference(s) |
|---|---|---|---|---|---|---|---|---|
| (invasive) C. rugosa bloodstream infection (n = 19) |
Blood culture PCR |
Microscopy | 5-flucytosine, voriconazole and amphotericin B | Fluconazole (only 4) | Fluconazole amphotericin B |
NA | Died (n = 13) Alive (n = 6) |
[108] |
| (invasive) C. rugosa bloodstream infection (n = 25) |
Blood culture PCR |
Microscopy | 5-flucytosine, voriconazole | Fluconazole and itraconazole (only 4) | Fluconazole amphotericin B |
NA | Died (n = 18) Alive (n = 7) |
[109] |
| (invasive) C. rugosa Candidemia (n = 6) |
Blood culture PCR |
Microscopy | Amphotericin B, fluconazole, and 5-flucytosine | NR | Amphotericin B | NA | Died (n = 5) Alive (n = 1) |
[106] |
| (invasive) C. rugosa bloodstream infection (n = 25) |
Blood culture | Microscopy | 5-flucytosine, voriconazole, fluconazole amphotericin B itraconazole |
Voriconazole, flluconazole | Fluconazole amphotericin B |
NA | NR | [110] |
| (invasive) C. rugosa fungemia (n = 1) |
Blood culture | Microscopy | NR | NR | Fluconazole | NA | Alive | [111] |
MIC: Minimal inhibitory concentrations; NA: Not applicable, because the research is performed on fungal strains/clinical isolates; NR: Not reported; MALDI-TOF MS: matrix-assisted laser desorption ionization mass spectrometry.
2.9. Candida pararugosa (New Numenclature: Wickerhamiella pararugosa)
Candida pararugosa is an emerging and rare yeast pathogen reported in both humans and animals in different organs and biological liquids (Table 2) [112]. Initially, in 1998, it was reported from human feces and then isolated from the oral cavity, where it was thought to illustrate colonization rather than a true infection [113]. The yeast was isolated from two different blood cultures in a 39-year-old-woman who developed post-abdominal surgery sepsis and surgical wound necrotizing fasciitis. Treatment with micafungin improved the patient’s clinical signs; however, it was not clear that sepsis resulted from candidemia or necrotizing fasciitis [113]. Concerning the literature, C. pararugosa seems to mainly leads to invasive fungal infection (IFI), predominantly in children and adults [112,114].
Candidemia caused by C. pararugosa is associated with a high morbidity and mortality, especially among immunocompromised patients [115]. Therefore, the precise identification of causative agents of the bloodstreams of particularly uncommon Candida species has paid high attention recently because of changing the epidemiology of candidemia. Moreover, clinical laboratories should be aware to identify the rare yeasts in specimens accurately for a faster treatment [34,116].
There are few available data for C. pararugosa infections regarding its identification, antifungal susceptibility testing, clinical significance, and treatment protocols [113]; however, the number of reports related to different aspects of C. pararugosa has recently risen worldwide, as we are witnessing an increase in the prevalence of C. pararugosa. In a case report by Piatti et al., C. pararugosa was isolated from the blood culture of a 65-year-old woman diagnosed with metastatic lobular breast cancer carrying a central venous catheter that was under a chemotherapy regime [112]. Interestingly, an elevated level of glucan was also detected in the blood analysis. Based on the antifungal susceptibility testing results, C. pararugosa showed a lower MIC against fluconazole. Hence, she underwent fluconazole therapy (initially with a load dose, 800 mg orally, on day 1 and then with 400 mg daily for two weeks). Nonetheless, the patient died due to malignancy [112].
A retrospective study was carried out from 2008 to 2020 in the largest tertiary Greek pediatric hospital. Fourteen different rare fungal species in 33 neonates and children with IFI hospitalized in the intensive care (ICU) and oncology units isolated from central catheters, peritoneal, pleural, blood, and pericardial fluid specimens were involved. C. pararugosa was identified using conventional, molecular, and MALDI–TOF MS methods, and the antifungal susceptibility profile was performed according to CLSI. Disappointedly, no official antifungal breakpoints have been defined for these rare yeasts [114]. Stavrou et al. reported that clinical isolates of C. pararugosa elevated MICs against common antifungal drugs (according to the EUCAST broth microdilution method). Amphotericin B was the most efficient drug, whereas azoles and echinocandins had high MICs. Surprisingly, voriconazole had the broadest efficacy among azole drugs [50]. Similarly, in another study in 2019, the identification of rare yeast isolates of clinical origin was attained by MALDI-TOF MS or internal transcribed spacer sequencing. The antifungal susceptibility patterns were generated for azoles, echinocandins, and amphotericin B using the commercial E-test and the EUCAST broth microdilution method. The findings showed that C. pararugosa had elevated echinocandin MICs (MIC50 ≥ 0.06 mg/L) and shared high fluconazole MICs, suggesting that the MIC values generated with E-test cannot be directly compared with the EUCAST results [61]. According to a report at a tertiary teaching hospital in Malaysia, seven isolates of the C. rugosa complex and one isolate of C. pararugosa were included to determine the antifungal susceptibility testing, biofilm formation, and enzyme activity of isolates. The E-test showed that both species have elevated MICs compared to C. albicans and C. tropicalis. All isolates exhibited high proteinase activity with a high capacity for biofilm formation, while none of the isolates exhibited phospholipase activity [117]. In a retrospective study in Italy, 156 yeast isolates were collected during 17 months from clinical samples of the microbiology department; approximately 2.1% of isolates were identified as C. pararugosa using MALDI-TOF MS [34]. The increase in the prevalence of the NCACs throughout the years was reported in Brazil (2007–2010) [34,116]. Yeasts from the blood of 104 patients were isolated, and the Candida spp. Were characterized by phenotypic and genotypic methods, and C. pararugosa was detected in one of these cases [34,116]. In Qatar, pediatric and elderly patients with fungemia have also been positive for C. pararugosa. MALDI-TOF MS provided the correct identifications compared with molecular analysis testing of the same isolates. All yeasts showed low MICs against isavuconazole and voriconazole as well [78].
The importance of accurate identification of the C. rugosa complex is much clearer when a molecular analysis of the sequences of the D1/D2 domains and the internal transcribed spacer (ITS) region of the ribosomal genes were used. In this context, a study by Parades et al. to distinguish 24 clinical isolates that phenotypically identified as C. rugosa revealed that only 10 (41.6%) isolates belong to that species, and the rest of the isolates identified as C. pararugosa and C. pseudorugosa and C. neorugosa, respectively, based on the similar D1/D2 sequences [118].
2.10. Candida pelliculosa (New Nomenclature: Wickerhamomyces anomalus)
Candida pelliculosa (formerly Pichia anomala or Hansenula anomala) is an ecological fungal species causing infections in immunocompromised hosts. Surprisingly, it has been proposed for many biotechnological applications in the food industry [119]. Feed and food supplemented with certain C. pelliculosa strains show an improved quality due, for example, to the addition of advantageous proteins and phytase activity [120].
C. pelliculosa was isolated from pigeons and their droppings as reservoirs and carriers of yeast that affect public health [121]. Only a few cases in the literature globally have illustrated that C. pelliculosa infects patients, particularly neonates hospitalized in the neonatal intensive care unit resulting in outbreaks of neonatal candidemia [122,123,124,125]. It has been reported that the common symptoms of C. pelliculosa candidemia were fever, cyanosis, polypnea, hypoactivity, and apnea. Mostly, as other Candida spp., immunosuppressed individuals using broad-spectrum antimicrobials or a long-term stay at the hospital are probably linked to the risk of infection with C. pelliculosa [126]. Isolates from neonates diagnosed with candidemia caused by C. pelliculosa in China showed high susceptibility to the antifungal activity of fluconazole, voriconazole, amphotericin B, and 5-fluorocytosine, which were from two different clones of C. pelliculosa [127]. It is recommended that monitoring rare strains isolated from immunodeficient hosts is critical to prevent possible outbreaks and control hospital-acquired infections, due to the clinical signs of disease nonspecific in the patients [127]. C. pelliculosa, Candida utilis, and Candida fabianii are hard to discriminate using common biochemical tests; however, an accurate identification of C. pelliculosa can be reached by biochemical kits, MALDI-TOF MS, and qPCR [119,128]. In 2015 was the first report of a nosocomial candidemia outbreak involving 11 patients in two ICUs and two general wards caused by C. pelliculosa in South Korea. The study showed that these isolates were similar in the randomly amplified polymorphic DNA (RAPD) assay [123]. Medical staff and staying in the interventional radiology procedure room were risk factors for the development of fungemia, and the outbreak was eradicated using strict hand washing, disinfecting medical equipment, and contact precautions [123].
Several findings demonstrated the antimicrobial potential activity and wide range of biotechnological characteristics of C. pelliculosa that received considerable attention [120]. Anti-idiotypic antibodies generating an “internal image” of a killer protein have been found to possess therapeutic activity against a broad range of microorganisms [120]. Particularly, a purified protein with a molecular weight of 140 kDa was isolated from a specific strain of C. pelliculosa isolated from Anopheles stephensi—namely, WaF17.12—corresponding to a high molecular weight, β-glucosidase produced a killer toxin with strong anti-plasmodial activity [129]. Consistently, the production of glucanases coded by the “killer genes” WaEXG1 and WaEXG2 of C. pelliculosa has been investigated as a biocontrol agent to play a role in the ability of yeast to inhibit other fungi [130]. Additionally, the antifungal activities of new N-donor bitriazolic tripods were reported against the fungal strain C. pelliculosa. Molecular docking studies of some compounds indicated that they could act as inhibitors for the biotin carboxylase enzyme [131]. In a study by Paris et al., the mycocin activity was obtained from the cell wall of environmental C. pelliculosa (WA40, WA45, and WA92), which exhibited antifungal activity against thirty C. albicans strains from candidemia [132]. Similarly, another mycotoxin was isolated from the culture supernatant of C. pelliculosa—exo-β-1,3 glucanase—characterized by MALDI-TOF MS, which had antifungal activity against Candida mesorugosa but not against C. albicans, C. parapsilosis, and C. krusei [133]. Moreover, secondary metabolites by Streptomyces spp. TUR-10, indicated antifungal activity against the clinical isolate of C. pelliculosa with significant antifungal activity values ranging from 15.6 to 250 μg/mL, suggesting abundant potential for further research [134]. Some cases have been reported to be associated with C. pelliculosa infections in patients globally, which is shown in Table 8.
Table 8.
General information and characteristics of the candidiasis described for Candida pelliculosa.
| Invasive/Non- invasive Candidiasis (No. of Human Cases/Strains/Isolates) |
Identification Methods |
Antifungal Susceptibility |
Antifungal Resistance |
Antifungal Treatment |
Other Treatments (e.g., Probiotics, Natural Compounds, Antivirals) |
Outcome (n) |
Reference(s) |
|---|---|---|---|---|---|---|---|
| (invasive) Candidemia (n = 1) |
Blood culture, Vitek-2 kit |
Fluconazole, flucytosine caspofungin, voriconazole, and amphotericin B |
No | Intravenous fluconazole for 2 weeks | NA | Alive (n = 1) | [122] |
| (noninvasive) Endophthalmitis (n = 1) |
Culture of anterior chamber | Intraocular amphotericin B | Topical fluconazole | Multiple intraocular amphotericin B |
Netilmicin sulfate cyclopentolate HCl eye drops | Alive (n = 1) | [135] |
| (noninvasive) Dacryocystitis with cacosmia (n = 1) |
fungal hyphae observed on the excised lacrimal sac wall. DNA sequencing |
NR | NR | Antifungal agent and washing of the nasolacrimal duct | NA | Alive (n = 1) | [136] |
| (invasive) Candidemia (n = 6) |
Blood culture, API-32C and Mini API system, RAPD |
2 isolates were resistant to Amphotericin B and low susceptibility to Itraconazole | Fluconazole, voriconazole, and micafungin | Amphotericin B and fluconazole |
NA | Alive (n = 5) Died (n = 1) |
[125] |
| (invasive) Candidemia (n = 1) |
Blood culture, VITEC2, (ITS) region amplification and sequencing | Amphotericin B, ketoconazole, itraconazole, voriconazole, and fluconazole | No | Fluconazole and amphotericin B |
Ceftriaxone, cefepime. and oxacillin | Alive (n = 1) | [137] |
| (noninvasive) Fungal keratitis (n = 1) |
Morphological characteristics and ITS region amplification and sequencing | NR | NR | Topical micafungin | No | Alive (n = 1) | [138] |
| (invasive) Meningitis in HIV patient caused by C. pelliculosa (n = 1) |
Phenotypic and molecular methods, Histopathological staining(PAS) from autopsy |
NR | NR | NR | Combination antiretroviral therapy (tenofovir, abacavir and atazanavir/ritonavir) |
Died (n = 1) | [139] |
RAPD: randomly amplified polymorphic DNA; ITS: internal transcribed spacer; NA: not applicable/available; PAS: periodic acid–Schiff.
2.11. Candida nivariensis (New Nomenclature: Nakaseomyces nivariensisa)
Candida nivariensis is closely related to the Candida glabrata complex and has become a global increasingly emerging and cryptic fungal species. It was described for the first time in 2005 by DNA sequencing [140]. Little is known regarding C. nivariensis and Candida bracarensis. Although there have been efforts to isolate C. nivariensis from large samples of the C. glabrata complex, these species have not been identified in some countries [141]. Nonetheless, several patients receiving fluconazole (treatment or prophylaxis) for C. nivariensis have been experiencing an increased rate of therapeutic failure in the UK. Therefore, a rapid and efficient yeast identification would be clinically important to decide whether fluconazole would be a suitable treatment for members of the Nakaseomyces clade, especially C. nivariensis [142]. Although Candida glabrata complex species are difficult to identify by traditional laboratory methods, there are cost-effective methods that can properly identify different species [141,143,144,145]. To date, MALDI-TOF MS is sensitive and has a practical applicability in the rapid detection of the C. glabrata species complex, indicating promising results for such a purpose [140]. The high-resolution melting curve (HRM) method targeted the ITS region to design a specific primer of clinical isolates that consists of DNA sequencing. The method allows for the early and targeted treatment of patients with invasive candidiasis [146].
Compared to C. albicans, C. nivariensis is more virulent and resistant to antifungal drugs [147]. The efficacy of the most common drugs against C. nivariensis isolates was evaluated in an in vivo model, Caenorhabditis elegans. The results showed that echinocandins had a higher efficacy to treat C. nivariensis infections [148]. The available data on antifungal susceptibility profiles of the C. glabrata complex are still very few [149]; yet, some reports are accessible. The first case of candidemia was reported in an 81-year-old man who was hospitalized for the surgical treatment of intestinal fistula caused by C. nivariensis (associated with a catheter). Due to a failure treatment with fluconazole and to a positive blood culture during treatment, the antifungal treatment was successfully changed to intravenous caspofungin for 2 weeks [150]. In another report (Poland), 24 C. nivariensis isolates were isolated from 445 clinical samples. Ninety-two percent of C. nivariensis were resistant to itraconazole, and half were resistant to posaconazole. Eighty-three percent of C. nivariensis were susceptible to voriconazole, while all strains were fluconazole-resistant. This clearly indicates that C. nivariensis should be considered as an emerging pathogen, with a relevant resistance to azoles [151]. Shi et al. evaluated several MIC geometric means of antifungal drugs (e.g., caspofungin, fluconazole, itraconazole, and amphotericin B) in women with vulvovaginal candidiasis (VVC). The authors showed that the C. nivariensis isolates were higher than those in C. albicans and that the level of resistant genes ERG11, CDR1, and CDR2 and virulent genes YPS1, AWP3, and EPA1 mRNA expression were higher in C. nivariensis isolates compared to C. glabrata, which is clinically serious [147]. In another study, all C. nivariensis isolates were susceptible to nystatin and susceptible or susceptible dose-dependently to fluconazole, itraconazole, miconazole, and clotrimazole. Importantly, the therapeutic efficacy in the patients was poor and inconsistent with the observed in vitro antifungal susceptibility; thus, extra studies are required [152]. Moreover, four Delhi patients with VVC related to C. nivariensis were resistant to fluconazole but susceptible to voriconazole, itraconazole, posaconazole, isavuconazole, amphotericin B, and echinocandins Similarly, in Iran, 4 out of 213 clinical C. glabrata species complex isolated from candidemia cases and identified as C. nivariensis were susceptible to amphotericin B, fluconazole, itraconazole, posaconazole, voriconazole, anidulafungin, and micafungin [143]. Not long ago, the antifungal susceptibility profile of 122 C. glabrata complex strains (including 5 C. nivariensis and 3 C. bracarensis strains) were evaluated and compared with the findings of the FKS gene mutations. Except for one isolate, no echinocandin resistance was detected, which was consistent with the MIC results. FKS sequencing results of the C. glabrata isolates were different from C. nivariensis [153]. Biofilm studies involving C. nivariensis have also been reported. The biofilm formation and antifungal susceptibility profile were evaluated in a clinical strain of C. nivariensis compared with the standard strains for the first time in Brazil. All strains showed low planktonic MICs to amphotericin B, caspofungin, and voriconazole while resistant to fluconazole. However, increasing the planktonic MICs to Posaconazole and itraconazole, the isolates produced a high level of protease enzyme as a virulence factor [144]. Finally, a C. elegans model was used for the simulation of C. glabrata and C. bracarensis infection. The results demonstrated an easy eradication of the infection by amphotericin B and azoles, while echinocandins were more effective against C. nivariensis [148,154].
2.12. Candida bracarensis (New Nomenclature: Nakaseomyces bracarensisa)
Fifteen years ago, during Candida species epidemiological research that took place in Braga (Portugal), the new name “Candida bracarensis” was given to a strain phylogenetically close to Candida glabrata [155,156]. Due to developments in molecular methods and the results of detailed analyses, C. glabrata was introduced as a complex of C. glabrata, C. nivariensis, and C. bracarensis [146,148,157]. In fact, the accurate identification of ambiguous species such as C. nivariensis and C. bracarensis is important, but in several geographical areas, these species remain unclear [148], and, currently, there is still a lack of information about C. bracarensis epidemiology or virulence factors [154]. Reports have described C. bracarensis, together with C. nivariensis, as etiological agents of VVC [152], since some strains have been isolated from a vaginal swab [154] or from samples of symptomatic pregnant women [152]. Since then, vaginal presumptive C. glabrata isolates were also retrospectively rechecked for C. nivariensis and C. bracarensis [152]. The data about clinical therapeutic efficacy and the in vitro antifungal susceptibility of C. bracarensis is still poor [152], but it seems that C. bracarensis has a slightly distinct phenotype and antifungal susceptibility profile from C. glabrata [158]. Obviously, an early, fast, and exact identification system that distinguishes these three species is crucial for targeted medication [146,158] Nowadays, reexamination is performed for the control of previously identified strains. In fact, numerous isolates of C. glabrata that have been reassessed, C. glabrata sensu stricto was confirmed for all of them [159]. The first identification of the phenotypes is commonly realized by cultivation using CHROMagar Candida medium [160], but another option is identified by the API® Candida system [152]. The results of traditional laboratory methods can be supported by denaturing high-performance liquid chromatography (dHPLC), which is fast and provides an up-to-date multiple analysis of Candida species in various samples [158]. Furthermore, as previously explained, molecular diagnostic methods have proven to be highly efficient in the correct identification of pathogenic yeasts, including C. bracarensisis and C. nivariensis (e.g., DNA sequencing is highly specific, using the rDNA ITS region, which offers an accurate diagnostic and can be applied as a reference tool [161], ITS2-MCA [145], HRM evaluation [146], mPCR, and three species-specific single-plex PCR [161,162]). In Spain, sequencing analysis indicated that 3 of 143 isolates (2%) were C. bracarensis [161]. Over 300 C. glabrata isolates from children and adults were initially biochemically distinguished via multiplex PCR, sequencing, and MALDI-TOF MS. One strain was found to be C. bracarensis [161]. Vitek MS® Research Use Only system and Bruker ClinProTools software proved 100% capable of discrimination and cross-validation for C. bracarensis and C. nivariensis [163]. Another retrospective re-examination of the vaginal C. glabrata samples via the ITS1 region, and the 5.8S ribosomal RNA gene assays pointed out that 293 in 301 isolates were correctly identified (C. glabrata). By sequencing, it was confirmed that the remaining isolates were C. nivariensis (7) and one as C. bracarensis [152]. In another study related to isolates of the C. glabrata complex, none of the C. bracarensis strains were found (via sequencing the D1/D2 region of 26S rRNA)[160]. It is also relevant to note that a single primer pair targeting the RPL31 gene (a gene coding for a protein component of the large ribosomal subunit) can also be used as a potential tool to distinguish between C. glabrata, C. bracarensis, and C. nivariensis [144].
Presently, there are only a few reports about the antifungal susceptibility pattern of C. bracarensis [159], but in candidiasis, generally, the most often selected triazole for patients is fluconazole, both for the therapy of candidiasis but also for prophylaxis [142]. C. bracarensis is also found in Mexico. This isolate was determined as susceptible to echinocandins (caspofungin, anidulafungin, and micafungin; MIC = 0.031 μg/mL). Interestingly, the authors also observed a noticeable activity of aspartyl proteinase, phospholipase, and hemolysin in this strain [144,156]. An extensive 15-year survey concerning 82 species of uncommonly occurring yeasts and yeast-like fungi (e.g., members of the Nakaseomyces clade: C. glabrata, C. nivariensis, and C. bracarensis) showed no antifungal resistance patterns of C. bracarensis samples. The drugs included amphotericin B, fluconazole, itraconazole, voriconazole, posaconazole, and anidulafungin [142]. Another research concluded that azoles (e.g., fluconazole, itraconazole, miconazole, and clotrimazole) and nystatin (a polyene) were effective against all tested C. bracarensis and C. nivariensis isolates [152].Using conventional mycological methods in oral samples, C. glabrata; C. parapsilosis; and their cryptic species: C. bracarensis, C. nivariensis, C. metapsilosis, and C. orthopsilosis were detected and identification was confirmed by molecular assays. Disk diffusion and microdilution results of the in vitro susceptibility assay showed the efficacy of miconazole and nystatin against most C. glabrata isolates, but they were resistant to fluconazole and itraconazole [156]. The FKS genes analysis of mutations (for echinocandins resistance) did not show any evidence of echinocandins resistance in C. glabrata complex strains (five C. nivariensis and three C. bracarensis) [164]. Finally, the ability to form a biofilm of C. bracarensis strains was described as an important virulence factor [156]: while planktonic cells are susceptible to antifungals, amphotericin B or fluconazole were not able to stop biofilm development [156]. Table 9 summarizes the information on C. bracarensis-reported cases.
Table 9.
General information and characteristics of candidiasis described for Candida bracarensis and Candida intermedia.
| Invasive/Noninvasive Candidiasis (n Human/Cases/Isolate) |
Identification Methods |
Imaging Test |
Antifungal Susceptibility |
Antifungal Resistance |
Antifungal Treatment | Other Treatments(e.g., Probiotics, Natural Compounds, Antivirals, etc) | Outcome (n) |
Reference (s) |
|---|---|---|---|---|---|---|---|---|
| Candida bracarensis | ||||||||
| (noninvasive) Vulvovaginal candidiasis (n = 1) |
API Candida system; ITS1 region and the 5.8S ribosomal RNA gene; sequencing | Microscopy (Germ tube test, chlamydospore test) |
Susceptible to nystatin and azoles (fluconazole, itraconazole, miconazole, clotrimazole) | NR | NR | NR | NR | [152] |
| (invasive) Peripheral neuropathy in type 1 diabetes (patient’s stool positive for C. bracarensis) (n = 1) |
CHROMagar Candida; multiplex PCR; sequencing; MALDI-TOF MS analysis | NR | Amphotericin B, flucytosine, fluconazole, voriconazole, anidulafungin and caspofungin | Itraconazole (MIC ≥ 32 mg/L), posaconazole (MIC ≥ 32 mg/L) | NR | NR | NR | [161] |
| Candida intermedia | ||||||||
| (invasive) Candidemia (with diabetes bloody sputum, fever, and dyspnea) (n = 1) |
API ID32C; molecular identification - D1/D2 domain of the large-subunit 26S rRNA gene | NR | Amphotericin B, flucytosine, fluconazole, itraconazole, miconazole, micafungin | NR | Several antifungals |
Antibiotic treatment, mechanical ventilation, steroid therapy | Alive, discharged on the 34th hospital day (n = 1) |
[165] |
MIC: Minimal Inhibitory Concentrations; NA: Not applicable, because the research is performed on fungal strains/clinical isolates; NR: Not reported; MALDI-TOF MS: matrix-assisted laser desorption ionization mass spectrometry; ITS: internal transcribed spacer.
2.13. Candida intermedia
Candida intermedia has been mainly reported in cases related to bloodstream infections in Asia [165]. The first case was confirmed using the molecular method (D1/D2 domain of the large subunit 26S rRNA gene), but there was an initial misidentification with the phenotype test that revealed a false result for Cryptococcus humicola [165]. In Iran, there is particular care on the surveillance of rarely occurring Candida species that cause candidemia in intensive care units, because candidiasis is still a serious problem in this country (Table 4). Indeed, C. intermedia belonged to this group of main pathogens, accounting for about 11% together with C. orthopsilosis, C. glabrata, Candida dubliniensis, Candida lusitaniae, and Candida kefyr [166]. In Qatar, C. intermedia has been identified in pediatric and elderly patient samples, using molecular identification and MALDI-TOF MS. The results of the antifungal susceptibility testing showed only rare cases of resistance, and isavuconazole and voriconazole successfully inhibited the tested species [78]. Furthermore, C. intermedia was one of the 82 vulvovaginal isolates verified by conventional mycological methods, with a high proteinase activity [167]. Curiously, it was also detected from the soil by the D1/D2 domain of the 26S rRNA gene amplification, sequence determination, and the phylogenetic analysis [168]. Table 9 has more information related to this species.
2.14. Candida africana
Candida africana is a newly described opportunistic yeast pathogen that is related to invasive and VVC [169,170] (Table 10). Based on biochemical, morphological, and physiological characteristics, this pathogen was first described, in 1995, as an atypical chlamydospore-negative C. albicans strain and subsequently proposed as a new Candida species that is different from typical C. albicans isolates [170]. Presently, the prevalence of C. africana species and its epidemiological assessment in clinical samples are still unknown, mostly because diagnostic laboratories use phenotypic identification systems that do not always allow discrimination between variants or closely related species of Candida. In fact, in a recent retrospective study with 52 culture collection isolates, two isolates were found to be C. africana using molecular methods [171]. However, initially, most of the isolates of C. africana were isolated from female genitalia [172], and vaginal tracts are frequently affected by this species [170,171,172,173,174]. One isolate of C. africana was recovered from a blood culture in Chile, South America, and it is also possible that C. africana may be associated with a wider clinical spectrum [174].
Table 10.
General information and characteristics of the candidiasis described for Candida africana.
| Invasive/Noninvasive Candidiasis (n Human Cases/Strains/Isolates) |
Identification Methods |
Imaging Test |
Antifungal Susceptibility |
Antifungal Resistance |
Antifungal Treatment |
Other Treatments (e.g., Probiotics, Natural Compounds, Antivirals) |
Outcome (n) |
Reference(s) |
|---|---|---|---|---|---|---|---|---|
| (invasive) C. africana (n = 2) |
MALDI-TOF MS and PCR | Microscopy | Ketoconazole (one) Fluconazole (one) Itraconazole (both) Amphotericin B (one) |
Ketoconazole (one) Fluconazole (one) Amphotericin B (one) |
NR | NA | Alive | [185] |
|
Candida vaginitis (n = 10) |
PCR-RFLP and sequencing CHROMagar Candida |
Microscopy | Fluconazole | NR | NR | NA | NA | [181] |
| (invasive) C. africana (n = 2) |
CHROMagar and PCR | Microscopy | Amphotericin B, fluconazole, and itraconazole | Fluconazole and itraconazole | NR | NA | NA | [180] |
| (invasive) C. africana (n = 3) |
CHROMagar MALDI-TOF MS | Microscopy | Fluconazole; voriconazole; ketoconazole; amphotericin B; anidulafungin; micafungin | NR | NR | NA | NA | [178] |
| (invasive) C. africana (n = 1) |
CHROMagar and PCR | Microscopy | Amphotericin B, nystatin, fluconazole, itraconazole Voriconazole, clotrimazole, terbinafine | NR | NR | NA | NA | [186] |
| (invasive) C. africana (n = 5) |
CHROMagar and PCR | Microscopy | Caspofungin, anidulafungin, micafungin, itraconazole, voriconazole, posaconazole | NR | NR | NA | All alive | [179] |
| (invasive) C. africana (n = 15) |
CHROMagar and PCR | Microscopy | Fluconazole, itraconazole, miconazole, clotrimazole, | NR | NR | NA | All alive | [187] |
| (invasive) C. africana (n = 4) |
CHROMagar and PCR sequencing | Microscopy | Nystatin, clotrimazole, isavuconazole, ketoconazole, miconazole and posaconazole |
NR | NR | NA | All alive | [177] |
| (invasive) C. africana (n = 15) |
CHROMagar and PCR sequencing | Microscopy | Amphotericin B, nystatin, Itraconazole, miconazole, econazole, and ketoconazole |
NR | NA | Alive (14) Dead (1) |
[183] | |
| (invasive) C. africana (n = 2) |
CHROMagar and PCR | Microscopy | amphotericin B, 5-fluorocytosine, Fluconazole, itraconazole, ketoconazole, voriconazole, posaconazole and caspofungin |
NR | NR | NA | Alive | [188] |
| (invasive) C. africana (n = 1) |
CHROMagar and PCR | Microscopy | Amphotericin B, 5-fluorocytosine fluconazole itraconazole, ketoconazole voriconazole | NR | NR | NA | Alive | [173] |
MALDI-TOF MS: matrix-assisted laser desorption ionization mass spectroscopy; PCR: polymerase chain reaction; NR: not reported; NA: nonapplicable.
Due to C. africana infection, most candidiasis cases have been reported from seven countries of the African continent [169,175,176]. One hundred and fifteen (40.6%) patients with C. africana candidiasis belong to this region. Madagascar and Angola had the majority of the cases (n = 93, 80.8%). The tropical and subtropical climate and high temperatures in Angola and Madagascar may contribute to C. africana prevalence. However, 87.6% of the infections with this species have been reported from the genital specimens of South African patients, and the distribution of C. africana infections was relatively higher among age groups of 18–35 years compared to others. Due to a weakened immune system, frequent sexual activities, and the use of oral contraceptives, pregnancy should be considered more as the main reason associated with a more prone condition to C. africana vaginitis. The overall prevalence of C. africana vaginal infections (1.9%) was close to the reports (1.4%) in India [177], (0.4%) Turkey [170,178], and (0.3%) Saudi Arabia [170]. However, it was lower as compared to those reported in Iran (3.2%, 5%, and 8.4%) [179,180,181]; China (6.3%) [182]; and the UK (5.9%) [183]. Environmental factors and differences among the study participants, including non-pregnant and pregnant women, symptomatic and asymptomatic conditions, immunity, personal hygiene practice, and patients’ socioeconomic status might explain this inconsistency. Although antifungal susceptibility testing in vaginal isolates is recommended because vaginal candidiasis is one of the reasons for frequent antimycotic medication among women of reproductive ages., C. africana isolates remain susceptible to commonly used antifungal agents with increasing antifungal resistance [184]. In this study, the high susceptibility of C. africana was also observed against all tested antifungals, and a resistance to flucytosine, voriconazole, and terbinafine have been reported against C. africana isolates [170,184].
2.15. Candida blankii
In 1968, Buckley and van Uden described a newly discovered nonfermenting yeast—C. blankii—from an infected mink in Canada, and the name was given in honor of Dr. Blank, who identified it [189]. The species was considered as nonpathogenic until 2015. Thereafter, it was isolated from the airways of patients with cystic fibrosis and reported to cause bloodstream infections (Table 11) [190]. Chowdhary and colleagues (2020) identified an outbreak of nosocomial fungemia caused by multidrug-resistant C. blankii (nine positive blood samples) in neonatal care in India for 7 months. Four of the neonates died. Importantly, the average MICs of two different antifungal drugs: fluconazole (8 mg/L) and anidulafungin (2 mg/L) were increased, and the genome sequencing results showed high probable antifungal resistance development [191]. Another study reported the death of a preterm neonate with a confirmed bloodstream infection due to C. blankii (PCR sequencing of rDNA), receiving combination antifungal therapy with amphotericin B and caspofungin [192]. In 2021, a case report concerning an adult immunocompromised patient with C. blankii endocarditis was published for the first time. Although there are still no official guidelines for the treatment of candidiasis caused by this opportunistic pathogen, the treatment was successful using a combination of polyene and echinocandins [193]. The assesment of marine fungal diversity on the Vietnam coast, by ITS sequencing, revealed an ecosystem composed of over 70 fungal isolates. Surprisingly, C. blankii was the most abundant species with 15 strains, originating from all surface coastal marine habitats, except two beaches [194].
Table 11.
General information and characteristics of the candidiasis described for Candida blankii.
| Invasive/Noninvasive Candidiasis (n Human Cases/Strains/Isolates) |
Identification Methods |
Imaging Test |
Antifungal Susceptibility |
Antifungal Resistance |
Antifungal Treatment |
Other Treatments (e.g., Probiotics, Natural Compounds, Antivirals) |
Outcome (n) |
Reference(s) |
|---|---|---|---|---|---|---|---|---|
| (invasive) C. blankii bloodstream infection (n = 1) |
Blood sample, CHROMagar Candida, PCR sequencing of rDNA |
Microscopy | Voriconazole, itraconazole, posaconazole, amphotericin B, caspofungin, Micafungin, anidulafungin, | Reduced susceptibility to fluconazole b (≥12 μg/mL) |
Amphotericin B, fluconazole, caspofungin |
Amikacin, ampicillin, cefotaxime, meropenem, teicoplanin, Piperacillin/tazobactam, vancomycin | Died (n = 1) |
[192] |
| (invasive) C. blankii fungaemia (n = 9) |
ITS and D1/D2 region sequencing | NR |
Isavuconazole, posaconazole, itraconazole, voriconazole, micafungin, |
Fluconazole had higher MIC (8 μg/mL), Anidulafungin MIC (2 μg/mL) had high MICs |
Fluconazole | Broad-spectrum antibiotics |
Alive (n = 5), Died (n = 4) |
[191] |
| (invasive) C. blankii fungemia and possible endocarditis (n = 1) |
Blood culture | NR | Amphotericin B, anidulafungin, 5-flucytosine, itraconazole, micafungin, posaconazole, voriconazole |
Fluconazole had higher MIC (16 μg/mL), caspofungin higher MIC (1 μg/mL), | Fluconazole, micafungin and liposomal amphotericin B, voriconazole |
Vancomycin, aztreonam, linezolid, daptomycin, meropenem | Alive (n = 1) |
[193] |
| (invasive) C. blankii bloodstream infection (n = 1) |
Blood cultures, CHROMagar, sequence analysis of the ITS1, and D1D2of the rRNA |
NR | Voriconazole, amphotericin B, micafungin | Fluconazole had higher MIC (16 μg/mL), anidulafungin (1 μg/mL) | Liposomal amphotericin B, micafungin | Teicoplanin, meropenem, cotrimoxazole | Alive (n = 1) |
[190] |
MIC: Minimal inhibitory concentrations; NR: not reported; PCR: polymerase chain reaction; ITS: internal transcribed spacer.
2.16. Candida pulcherrima (Updated Nomenclature: Metschnikowia pulcherrima)
In 2012, C. pulcherrima was reported by Berkenzi et al. for the first time in a premature newborn girl in an invasive fungemia due to a catheter (parenteral nutrition). The strain was identified by microbiological and molecular assay (e.g., sequencing of a fragment of internal transcribed spacer ITS 1 and ITS 4 regions). The patient was treated by amphotericin B lipid complex therapy (5 mg/kg/d), since, initially, fluconazole therapy was not successful [195]. Similarly, a case report (Greece, 2016) of a neonate with prematurity and respiratory distress syndrome indicated fungemia because of C. pulcherrima, successfully treated with a combination of liposomal amphotericin B and micafungin [196]. The first case of a community acquired candidemia by C. pulcherrima was detected in a 48-year-old man in 2016. The final identification was carried out using MALDI-TOF MS, and contrary to the hospital isolates (abovementioned studies), the patient underwent fluconazole therapy with a satisfied outcome [197]. On the other hand, in a respective study between 2012 and 2017, 50 hospitalized patients with different predisposing factors were enrolled. From the Candida species isolation tests, C. albicans was dominant, followed by NCACs. Meaningfully, the C. pulcherrima recovered was from 2% of the patients. The highest antifungal sensitivity rates (>90%) were measured for amphotericin B, voriconazole, and echinocandins (Table 12) [198]. In another respective study involving 107 hospitalized patients with candidemia, 109 Candida species were identified. C. albicans was the most isolated, followed by NCACs: C. parapsilosis complex, C. glabrata complex, C. tropicalis, C. krusei, C. lipolytica, Candida membranaefaciens, and one Candida pulcherrima. The major risk factor was, in both adults and children, catheter use. Additionally, 8.5% of those NCACs were resistant to fluconazole [199].
Table 12.
General information and characteristics of the candidiasis described for Candida pulcherrima.
| Invasive/Noninvasive Candidiasis (n Human Cases/Strains/Isolates) |
Identification Methods |
Imaging Test |
Antifungal Susceptibility |
Antifungal Resistance |
Antifungal Treatment |
Other treatments (e.g., Probiotics, Natural Compounds, Antivirals) |
Outcome (n) |
Reference(s) |
|---|---|---|---|---|---|---|---|---|
| (invasive) C.pulcherrima (n = 1) |
Blood culture | Microscopy and ITS sequencing | Amphotericin B lipid complex | NR | Amphotericin B lipid complex | NA | Alive | [195] |
| (invasive) C.pulcherimma (n = 1) |
Blood culture | MALDI-TOF MS | Fluconazole | NR | Fluconazole | NA | Alive | [197] |
| (invasive) C. pulcherimma (n = 1) |
Blood culture | Microscopy and ITS sequencing | Liposomal amphotericin B, fluconazole, voriconazole, posoconazole, micafungin, anidulafungin |
NR | Liposomal amphotericin B and micafungin | NA | Alive | [196] |
| (invasive) C. pulcherimma (n = 1) |
Blood cultures | Microscopy and MALDI-TOF MS | Amphotericin B, azoles, echinocandins |
NR | Amphotericin B, voriconazole, echinocandins |
NA | Alive | [196] |
MIC: Minimal inhibitory concentrations; NR: not reported; NA: nonapplicable: PCR: polymerase chain reaction; MALDI-TOF MS: matrix-assisted laser desorption ionization mass spectroscopy; ITS: internal transcribed spacer.
Curiously, the antimicrobial activity of a new strain of C. pulcherrima was examined against fungal and bacterial species. Strong antagonistic activities of the C. pulcherrima strain were detected on the human pathogens Escherichia coli, C. albicans, C. parapsilosis, C. krusei, and Trichosporon mucoides. This was directly perceived by the same amount of the pigment pulcherrimin with different levels of antimicrobial effects on various species [200].
3. Conclusions
In the last decade, atypical Candida spp. have been related to several human fungal infections, from superficial to systemic diseases. The key case reports show that these yeast pathogens have, in some cases, a noteworthy profile of resistance to antifungal drugs, especially to azoles; however, resistance to polyenes and echinocandins has also been increasing.
Pointedly, the absence of official clinical breakpoints and antifungal susceptibility profiles for most of the uncommon Candida spp. cited here makes the interpretation and treatment options a clinical challenge. In fact, one of the major problems that the scientific and clinical community faces with uncommon Candida spp. is that there is no official information on antifungal drug MIC values (both EUCAST and CLSI), and even the great majority of the analyzed reports do not present these values. Unsurprisingly, this makes it difficult to evaluate the antifungal profile and, therefore, to guide the treatment of fungal diseases, in this case, of Candida spp. infection. Additionally, defining “sensible/tolerant/resistant” inference is done by comparing MIC values with Candida common species (which already have official clinical breakpoints). This, of course, brings up several drawbacks in terms of the effectiveness of the antifungal therapy applied in these cases.
It is also important to note that there is a limitation in our work: in some countries, certain species (such as Candida uncommon species) are only used in research and not in clinical data (e.g., no final identifications, misidentification, and no/few/inadequate equipment/methods available). Obviously, an overview of the problem in terms of the evaluation of the epidemiology scenario is difficult, because, in these cases, there are no reports or because the available reports mislead us to common species that are, in fact, misidentified. Taken together, since the emerging and cryptic clinically important species are augmented, periodic surveillance, including the use of molecular identification methods, seems to be necessary for enlightening their frequency, geographical distribution, and susceptibility profile [201].
Due to the above, the scientific and clinical community must make efforts to publish breakpoints for a far higher range of Candida spp., increasing and focusing research on novel quick methods of diagnostic and new treatment strategies, to be able to fight these challenging infections in a timely manner.
Author Contributions
Conceptualization: C.F.R. and L.Č.; methodology: C.F.R. and L.Č. validation: C.F.R.; investigation: all authors; writing—original draft preparation: all authors; writing—review and editing: all authors; and supervision, C.F.R. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
S.K. and A.K. thank the Shri Ramswaroop Memorial University, Barabanki (UP), India, and the National Institute of Technology, Raipur (CG), India, for the continuous support and assistance during the work and scientific writing. L.Č. thanks the Slovak Research and Development Agency under contract No. APVV-21-0302 and the grant of VEGA 1/0537/19 from the Ministry of Education, Science, Research, and the Sport of the Slovak Republic.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Benedict K., Whitham H.K., Jackson B.R. Economic Burden of Fungal Diseases in the United States. Open Forum Infect. Dis. 2022;9:ofac097. doi: 10.1093/ofid/ofac097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gharehbolagh S.A., Fallah B., Izadi A., Ardestani Z.S., Malekifar P., Borman A.M., Mahmoudi S. Distribution, antifungal susceptibility pattern and intra-Candida albicans species complex prevalence of Candida africana: A systematic review and meta-analysis. PLoS ONE. 2020;15:e0237046. doi: 10.1371/journal.pone.0237046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Turner S.A., Butler G. The Candida Pathogenic Species Complex. Cold Spring Harb. Perspect. Med. 2014;4:a019778. doi: 10.1101/cshperspect.a019778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rodrigues C.F., Alves D.F., Henriques M. Combination of Posaconazole and Amphotericin B in the Treatment of Candida glabrata Biofilms. Microorganisms. 2018;6:123. doi: 10.3390/microorganisms6040123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ostrosky-Zeichner L., Harrington R., Azie N., Yang H., Li N., Zhao J., Koo V., Wu E.Q. A Risk Score for Fluconazole Failure among Patients with Candidemia. Antimicrob. Agents Chemother. 2017;61:e02091-16. doi: 10.1128/AAC.02091-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Černáková L., Roudbary M., Brás S., Tafaj S., Rodrigues C.F. Candida auris: A Quick Review on Identification, Current Treatments, and Challenges. Int. J. Mol. Sci. 2021;22:4470. doi: 10.3390/ijms22094470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Logan C., Martin-Loeches I., Bicanic T. Invasive candidiasis in critical care: Challenges and future directions. Intensiv. Care Med. 2020;46:2001–2014. doi: 10.1007/s00134-020-06240-x. [DOI] [PubMed] [Google Scholar]
- 8.Borman A.M., Johnson E.M. Name Changes for Fungi of Medical Importance, 2018 to 2019. J. Clin. Microbiol. 2021;59:1811–1831. doi: 10.1128/JCM.01811-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brandt M.E., Lockhart S.R. Recent Taxonomic Developments with Candida and Other Opportunistic Yeasts. Curr. Fungal Infect. Rep. 2012;6:170. doi: 10.1007/s12281-012-0094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pemán J., Cantón E., Quindós G., Eraso E., Alcoba J., Guinea J., Merino P., Ruiz-Pérez-De-Pipaon M.T., Pérez-Del-Molino L., Linares-Sicilia M.J., et al. Epidemiology, species distribution and in vitro antifungal susceptibility of fungaemia in a Spanish multicentre prospective survey. J. Antimicrob. Chemother. 2012;67:1181–1187. doi: 10.1093/jac/dks019. [DOI] [PubMed] [Google Scholar]
- 11.Aslani N., Janbabaei G., Abastabar M., Meis J.F., Babaeian M., Khodavaisy S., Boekhout T., Badali H. Identification of uncommon oral yeasts from cancer patients by MALDI-TOF mass spectrometry. BMC Infect. Dis. 2018;18:24. doi: 10.1186/s12879-017-2916-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miceli M.H., Diaz J.A., Lee S.A. Emerging opportunistic yeast infections. Lancet Infect. Dis. 2011;11:142–151. doi: 10.1016/S1473-3099(10)70218-8. [DOI] [PubMed] [Google Scholar]
- 13.Ergon M.C., Dereli M.D., Ener B., Atalay M.A., Koç A.N., Çerikçioğlu N., Erturan Z., Aksaray S. Türkiye’de Altı Yıllık Zaman Dilimi İçerisinde Kan Kültürlerinden Soyutlanan Maya Mantarlarının Tür Dağılımı: Çok Merkezli Bir Çalışma. Distribution of Yeast Species Isolated from Blood Cultures for a Six Year Period in Turkey: A Multicentre Study. Mikrobiyoloji Bulteni. 2020;54:638–646. doi: 10.5578/mb.69837. [DOI] [PubMed] [Google Scholar]
- 14.Morales S., Taverna C.G., Bosco-Borgeat M.E., Maldonado I., Vivot W., Szusz W., Garcia-Effron G., Córdoba S.B. Candida glabrata species complex prevalence and antifungal susceptibility testing in a culture collection: First description of Candida nivariensis in Argentina. Mycopathologia. 2016;181:871–878. doi: 10.1007/s11046-016-0052-1. [DOI] [PubMed] [Google Scholar]
- 15.Arendrup M., Friberg N., Mares M., Kahlmeter G., Meletiadis J., Guinea J., Andersen C., Arikan-Akdagli S., Barchiesi F., Chryssanthou E., et al. How to interpret MICs of antifungal compounds according to the revised clinical breakpoints v. 10.0 European committee on antimicrobial susceptibility testing (EUCAST) Clin. Microbiol. Infect. 2020;26:1464–1472. doi: 10.1016/j.cmi.2020.06.007. [DOI] [PubMed] [Google Scholar]
- 16.Bourbeau P., Cerwinka P.L., Abramson J., Finn S., Hindiyeh M.Y., Loeffelholz M.J., Maliff E.S., Nugent C.T., IV, Peat C.R., Sharples N., et al. M40-A2 CLSI Guideline—Quality Control of Microbiological Transport Systems. Clinical and Laboratory Standards Institute; Malvern, PA, USA: 2014. [Google Scholar]
- 17.Mellinghoff S.C., Hoenigl M., Koehler P., Kumar A., Lagrou K., Lass-Flörl C., Meis J.F., Menon V., Rautemaa-Richardson R., Cornely O.A. EQUAL Candida Score: An ECMM score derived from current guidelines to measure QUAlity of Clinical Candidaemia Management. Mycoses. 2018;61:326–330. doi: 10.1111/myc.12746. [DOI] [PubMed] [Google Scholar]
- 18.Pfaller M.A., Diekema D.J., Gibbs D.L., Newell V.A., Ellis D.J., Tullio V., Rodloff A.C., Fu W., Ling T.A., Global Antifungal Surveillance Group Results from the ARTEMIS DISK Global Antifungal Surveillance Study, 1997 to 2007: A 10.5-Year Analysis of Susceptibilities of Candida Species to Fluconazole and Voriconazole as Determined by CLSI Standardized Disk Diffusion. J. Clin. Microbiol. 2010;48:1366–1377. doi: 10.1128/JCM.02117-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen S.C.-A., Perfect J., Colombo A.L., A Cornely O., Groll A.H., Seidel D., Albus K., de Almedia J.N., Garcia-Effron G., Gilroy N., et al. Global guideline for the diagnosis and management of rare yeast infections: An initiative of the ECMM in cooperation with ISHAM and ASM. Lancet Infect. Dis. 2021;21:e375–e386. doi: 10.1016/S1473-3099(21)00203-6. [DOI] [PubMed] [Google Scholar]
- 20.Dos Santos Abrantes P.M., McArthur C.P., Africa C.W.J. Multi-drug resistant oral Candida species isolated from HIV-positive patients in South Africa and Cameroon. Diagn. Microbiol. Infect. Dis. 2014;79:222–227. doi: 10.1016/j.diagmicrobio.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 21.Khan Z., Ahmad S., Al-Obaid K., Joseph L., Chandy R. Candida kefyr as a cause of bloodstream infection and adjunctive role of biomarkers in its diagnosis. J. Mycol. Med. 2014;25:71–75. doi: 10.1016/j.mycmed.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 22.Nurdin R.S.C., Vitayani S., Amin S., Kadir D., Djamaluddin W., Adriani A. Cutaneous candidiasis caused by Candida kefyr. Pan Afr. Med. J. 2021;38:178. doi: 10.11604/pamj.2021.38.178.28054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Okmen F., Ekici H., Ari S.A. Case Report of a Tubo-ovarian Abscess Caused by Candida kefyr. J. Obstet. Gynaecol. Can. 2018;40:1466–1467. doi: 10.1016/j.jogc.2018.04.025. [DOI] [PubMed] [Google Scholar]
- 24.Mohammadi R., Salehi F., Esmaeili M. Isolation of Candida Species from Gastroesophageal Lesions among Pediatrics in Isfahan, Iran: Identification and Antifungal Susceptibility Testing of Clinical Isolates by E-test. Adv. Biomed. Res. 2017;6:103. doi: 10.4103/2277-9175.213662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seth-Smith H.M.B., Büchler A.C., Hinic V., Medinger M., Widmer A.F., Egli A. Bloodstream infection with Candida kefyr/Kluyveromyces marxianus: Case report and draft genome. Clin. Microbiol. Infect. 2020;26:522–524. doi: 10.1016/j.cmi.2019.11.014. [DOI] [PubMed] [Google Scholar]
- 26.Arastehfar A., Daneshnia F., Farahyar S., Fang W., Salimi M., Salehi M., Hagen F., Weihua P., Roudbary M., Boekhout T. Incidence and spectrum of yeast species isolated from the oral cavity of Iranian patients suffering from hematological malignancies. J. Oral Microbiol. 2019;11:1601061. doi: 10.1080/20002297.2019.1601061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ahmad S., Khan Z., Al-Sweih N., Alfouzan W., Joseph L., Asadzadeh M. Candida kefyr in Kuwait: Prevalence, antifungal drug susceptibility and genotypic heterogeneity. PLoS ONE. 2020;15:e0240426. doi: 10.1371/journal.pone.0240426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dagi H.T., Findik D., Senkeles C., Arslan U. Identification and antifungal susceptibility of Candida species isolated from bloodstream infections in Konya, Turkey. Ann. Clin. Microbiol. Antimicrob. 2016;15:36. doi: 10.1186/s12941-016-0153-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dufresne S.F., Marr K.A., Sydnor E., Staab J.F., Karp J.E., Lu K., Zhang S.X., Lavallée C., Perl T.M., Neofytos D. Epidemiology of Candida kefyr in Patients with Hematologic Malignancies. J. Clin. Microbiol. 2014;52:1830–1837. doi: 10.1128/JCM.00131-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jyothi L., Reddy N.P., Naaz S. An Unusual Case of Candida kefyr Fungemia in an Immunocompromised Patient. Cureus. 2021;13:e14138. doi: 10.7759/cureus.14138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nagy F., Bozó A., Tóth Z., Daróczi L., Majoros L., Kovács R. In vitro antifungal susceptibility patterns of planktonic and sessile Candida kefyr clinical isolates. Med. Mycol. 2017;56:493–500. doi: 10.1093/mmy/myx062. [DOI] [PubMed] [Google Scholar]
- 32.Bellmann R., Smuszkiewicz P. Pharmacokinetics of antifungal drugs: Practical implications for optimized treatment of patients. Infection. 2017;45:737–779. doi: 10.1007/s15010-017-1042-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aldejohann A.M., Theuersbacher J., Haug L., Lamm O.S., Walther G., Kurzai O., Hillenkamp J., Kampik D. First case of Kluyveromyces marxianus (Candida kefyr) late onset keratitis after lamellar endothelial corneal graft. Med. Mycol. Case Rep. 2021;32:21–24. doi: 10.1016/j.mmcr.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Scapaticci M., Bartolini A., del Chierico F., Accardi C., di Girolamo F., Masotti A., Muraca M., Putignani L. Phenotypic Typing and Epidemiological Survey of Antifungal Resistance of Candida Species Detected in Clinical Samples of Italian Pa-tients in a 17 Months’ Period. Germs. 2018;8:58–66. doi: 10.18683/germs.2018.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Swarajyalakshmi M., Jyothilakshmi G. Candida kefyr in Invasive Paranasal Sinusitis. Indian J. Otolaryngol. Head Neck Surg. 2012;66:371–374. doi: 10.1007/s12070-012-0500-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fekkar A., Meyer I., Brossas J.Y., Dannaoui E., Palous M., Uzunov M., Nguyen S., Leblond V., Mazier D., Datry A. Rapid Emergence of Echinocandin Resistance during Candida kefyr Fungemia Treatment with Caspofungin. Antimicrob. Agents Chemother. 2013;57:2380–2382. doi: 10.1128/AAC.02037-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.De Freitas E.M., Nobre S.A.M., de Oliveira Pires M.B., Faria R.V.J., Batista A.U.D., Bonan P.R.F. Oral Candida species in head and neck cancer patients treated by radiotherapy. Auris Nasus Larynx. 2013;40:400–404. doi: 10.1016/j.anl.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 38.Badiee P., Alborzi A., Shakiba E., Farshad S., Japoni A. Susceptibility of Candida species isolated from immunocompromised patients to antifungal agents. East. Mediterr. Health J. 2011;17:425–430. doi: 10.26719/2011.17.5.425. [DOI] [PubMed] [Google Scholar]
- 39.Weichert S., Reinshagen K., Zahn K., Geginat G., Dietz A., Kilian A.K., Schroten H., Tenenbaum T. Candidiasis caused by Candida kefyr in a neonate: Case report. BMC Infect. Dis. 2012;12:61. doi: 10.1186/1471-2334-12-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pineda C., Kaushik A., Kest H., Wickes B., Zauk A. Maternal Sepsis, Chorioamnionitis, and Congenital Candida kefyr Infection in Premature Twins. Pediatr. Infect. Dis. J. 2012;31:320–322. doi: 10.1097/INF.0b013e31823eee1a. [DOI] [PubMed] [Google Scholar]
- 41.Dietrichson E. Etude d’une collection norvégienne de levures (2e Partie) (suite et fin) Ann. Parasitol. Hum. Comp. 1954;29:460–498. doi: 10.1051/parasite/1954294460. [DOI] [PubMed] [Google Scholar]
- 42.Nielsen H., Stenderup J., Bruun B., Ladefoged J. Candida norvegensis peritonitis and invasive disease in a patient on continuous ambulatory peritoneal dialysis. J. Clin. Microbiol. 1990;28:1664–1665. doi: 10.1128/jcm.28.7.1664-1665.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hood S.V., Moore C.B., Denning D.W. Isolation of Candida norvegensis from Clinical Specimens: Four Case Reports. Clin. Infect. Dis. 1996;23:1185–1187. doi: 10.1093/clinids/23.5.1185. [DOI] [PubMed] [Google Scholar]
- 44.Kiraz N., Akay O.M., Sen Y., Aslan V., Akgun Y., Gulbas Z. Candida norvegensis fungaemia in a neutropenic patient with acute non-lymphoblastic leukaemia. Mycoses. 2010;53:460–462. doi: 10.1111/j.1439-0507.2009.01724.x. [DOI] [PubMed] [Google Scholar]
- 45.Sandven P., Nilsen K., Digranes A., Tjade T., Lassen J. Candida norvegensis: A fluconazole-resistant species. Antimicrob. Agents Chemother. 1997;41:1375–1376. doi: 10.1128/AAC.41.6.1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Krcmery V., Barnes A.J. Non-albicans Candida spp. causing fungaemia: Pathogenicity and antifungal resistance. J. Hosp. Infect. 2002;50:243–260. doi: 10.1053/jhin.2001.1151. [DOI] [PubMed] [Google Scholar]
- 47.Arikan S., Sancak B., Hascelik G. In vitroactivity of caspofungin compared to amphotericin B, fluconazole, and itraconazole againstCandidastrains isolated in a Turkish University Hospital. Med. Mycol. 2005;43:171–178. doi: 10.1080/13693780410001731565. [DOI] [PubMed] [Google Scholar]
- 48.Cuenca-Estrella M., Gomez-Lopez A., Mellado E., Monzon A., Buitrago M.J., Rodriguez-Tudela J.L. Activity Profile In Vitro of Micafungin against Spanish Clinical Isolates of Common and Emerging Species of Yeasts and Molds. Antimicrob. Agents Chemother. 2009;53:2192–2195. doi: 10.1128/AAC.01543-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sugita T., Takeo K., Ohkusu M., Virtudazo E., Takashima M., Asako E., Ohshima F., Harada S., Yanaka C., Nishikawa A., et al. Fluconazole-Resistant Pathogens Candida inconspicua and C. norvegensis: DNA Sequence Diversity of the rRNA Intergenic Spacer Region, Antifungal Drug Susceptibility, and Extracellular Enzyme Production. Microbiol. Immunol. 2004;48:761–766. doi: 10.1111/j.1348-0421.2004.tb03602.x. [DOI] [PubMed] [Google Scholar]
- 50.Stavrou A.A., Pérez-Hansen A., Lackner M., Lass-Flörl C., Boekhout T. Elevated Minimum Inhibitory Concentrations to Antifungal Drugs Prevail in 14 Rare Species of Candidemia-Causing Saccharomycotina Yeasts. Med. Mycol. 2020;58:987–995. doi: 10.1093/mmy/myaa005. [DOI] [PubMed] [Google Scholar]
- 51.Junqueira J.C., Fuchs B.B., Muhammed M., Coleman J.J., Suleiman J.M.A.H., Vilela S.F.G., Costa A.C.B.P., Rasteiro V.M.C., Jorge A.O.C., Mylonakis E. Oral Candida albicans isolates from HIV-positive individuals have similar in vitro biofilm-forming ability and pathogenicity as invasive Candida isolates. BMC Microbiol. 2011;11:247. doi: 10.1186/1471-2180-11-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li Y.-Y., Chen W.-Y., Li X., Li H.-B., Li H.-Q., Wang L., He L., Yang X.-P., Wang X.-C., Huang Y.-L., et al. Asymptomatic oral yeast carriage and antifungal susceptibility profile of HIV-infected patients in Kunming, Yunnan Province of China. BMC Infect. Dis. 2013;13:46. doi: 10.1186/1471-2334-13-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Agwu E., Ihongbe J.C., McManus B.A., Moran G.P., Coleman D.C., Sullivan D.J. Distribution of yeast species associated with oral lesions in HIV-infected patients in Southwest Uganda. Med. Mycol. 2012;50:276–280. doi: 10.3109/13693786.2011.604862. [DOI] [PubMed] [Google Scholar]
- 54.Guitard J., Angoulvant A., Letscher-Bru V., L’Ollivier C., Cornet M., Dalle F., Grenouillet F., Lacroix C., Vekhoff A., Maury E., et al. Invasive infections due toCandida norvegensisandCandida inconspicua: Report of 12 cases and review of the literature. Med. Mycol. 2013;51:795–799. doi: 10.3109/13693786.2013.807444. [DOI] [PubMed] [Google Scholar]
- 55.Musso M., Giannella M., Antonini M., Bordi E., Ettorre G.M., Tessitore L., Mariano A., Capone A. Invasive candidiasis due to Candida norvegensis in a liver transplant patient: Case report and literature review. Infect. Dis. Rep. 2014;6:28–30. doi: 10.4081/idr.2014.5374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sanclemente G., Marco F., Cervera C., Hoyo I., Colmenero J., Pitart C., Almela M., Navasa M., Moreno A. Candida norvegensis fungemia in a liver transplant recipient. Rev. Iberoam. Micol. 2015;32:115–117. doi: 10.1016/j.riam.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 57.Virgilio E., Mercantini P., Ferri M., Cavallini M., Teggi A., Ziparo V. Coexistence of Diffuse Malignant Peritoneal Mesothelioma andCandida norvegensisPeritonitis. Surg. Infect. 2014;15:660–661. doi: 10.1089/sur.2014.088. [DOI] [PubMed] [Google Scholar]
- 58.Mixão V., Hansen A.P., Saus E., Boekhout T., Lass-Florl C., Gabaldón T. Whole-Genome Sequencing of the Opportunistic Yeast Pathogen Candida inconspicua Uncovers Its Hybrid Origin. Front. Genet. 2019;10:383. doi: 10.3389/fgene.2019.00383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Egue L.A., N’Guessan F.K., Aka-Gbezo S., Bouatenin J.-P.K., Koussemon-Camara M. Candida species in tchapalo and bangui, two traditional alcoholic beverages from Côte d’Ivoire. Fungal Biol. 2018;122:283–292. doi: 10.1016/j.funbio.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 60.Kovács R., Gesztelyi R., Berényi R., Domán M., Kardos G., Juhász B., Majoros L. Killing rates exerted by caspofungin in 50 % serum and its correlation with in vivo efficacy in a neutropenic murine model against Candida krusei and Candida inconspicua. J. Med. Microbiol. 2014;63:186–194. doi: 10.1099/jmm.0.066381-0. [DOI] [PubMed] [Google Scholar]
- 61.Pérez-Hansen A., Lass-Flörl C., Lackner M. Antifungal Susceptibility Profiles of Rare Ascomycetous Yeasts. J. Antimicrob. Chemother. 2019;74:2649–2656. doi: 10.1093/jac/dkz231. [DOI] [PubMed] [Google Scholar]
- 62.Pfaller M.A., Diekema D.J. Epidemiology of Invasive Candidiasis: A Persistent Public Health Problem. Clin. Microbiol. Rev. 2007;20:133–163. doi: 10.1128/CMR.00029-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kurtzman C.P., Fell J.W., Boekhout T., editors. The Yeasts. 5th ed. Volume 1. Elsevier; Amsterdam, The Netherlands: 2011. CANDIDA | Yarrowia (Candida) lipolytica; p. xiii. [Google Scholar]
- 64.Walsh T.J., Salkin I.F., Dixon D.M., Hurd N.J. Clinical, microbiological, and experimental animal studies of Candida lipolytica. J. Clin. Microbiol. 1989;27:927–931. doi: 10.1128/jcm.27.5.927-931.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Trabelsi H., Chtara K., Khemakhem N., Néji S., Cheikhrouhou F., Sellami H., Guidara R., Makni F., Bouaziz M., Ayadi A. Fungemia Caused by Yarrowia lipolytica. Mycopathologia. 2015;179:437–445. doi: 10.1007/s11046-015-9859-4. [DOI] [PubMed] [Google Scholar]
- 66.Zinjarde S.S. Food-related applications of Yarrowia lipolytica. Food Chem. 2014;152:1–10. doi: 10.1016/j.foodchem.2013.11.117. [DOI] [PubMed] [Google Scholar]
- 67.Liu W.-C., Chan M.-C., Lin T.-Y., Hsu C.-H., Chiu S.-K. Candida lipolytica candidemia as a rare infectious complication of acute pancreatitis: A case report and literature review. J. Microbiol. Immunol. Infect. 2013;46:393–396. doi: 10.1016/j.jmii.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 68.Lai C.-C., Lee M.-R., Hsiao C.-H., Tan C.-K., Lin S.-H., Liao C.-H., Huang Y.-T., Hsueh P.-R. Infections caused by Candida lipolytica. J. Infect. 2012;65:372–374. doi: 10.1016/j.jinf.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 69.Zhao Y., Chan J.F.-W., Tsang C.-C., Wang H., Guo D., Pan Y., Xiao Y., Yue N., Chen J.H.-K., Lau S.K.-P., et al. Clinical Characteristics, Laboratory Identification, and In Vitro Antifungal Susceptibility of Yarrowia (Candida) lipolytica Isolates Causing Fungemia: A Multicenter, Prospective Surveillance Study. J. Clin. Microbiol. 2015;53:3639–3645. doi: 10.1128/JCM.01985-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Özdemir H., Karbuz A., Çiftçi E., Dinçaslan H.U., Ince E., Aysev D., Yavuz G., Doğru Ü. Successful treatment of central venous catheter infection due to Candida lipolytica by caspofungin-lock therapy. Mycoses. 2011;54:e647–e649. doi: 10.1111/j.1439-0507.2010.01964.x. [DOI] [PubMed] [Google Scholar]
- 71.Desnos-Ollivier M., Letscher-Bru V., Neuvéglise C., Dromer F. Yarrowia lipolytica causes sporadic cases and local outbreaks of infections and colonisation. Mycoses. 2020;63:737–745. doi: 10.1111/myc.13095. [DOI] [PubMed] [Google Scholar]
- 72.Diekema D.J., Messer S.A., Boyken L.B., Hollis R.J., Kroeger J., Tendolkar S., Pfaller M.A. In Vitro Activity of Seven Systemically Active Antifungal Agents against a Large Global Collection of Rare Candida Species as Determined by CLSI Broth Microdilution Methods. J. Clin. Microbiol. 2009;47:3170–3177. doi: 10.1128/JCM.00942-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Blanco M.T., Garcia-Martos P., García-Tapia A., Fernández C., Navarro J., Guerrero F. Fungemia por Candida lipolytica: A propósito de 2 casos. Rev. Iberoam. Micol. 2009;26:211–212. doi: 10.1016/j.riam.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 74.D’Antonio D., Romano F., Pontieri E., Fioritoni G., Caracciolo C., Bianchini S., Olioso P., Staniscia T., Sferra R., Boccia S., et al. Catheter-Related Candidemia Caused by Candida lipolytica in a Patient Receiving Allogeneic Bone Marrow Transplantation. J. Clin. Microbiol. 2002;40:1381–1386. doi: 10.1128/JCM.40.4.1381-1386.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Shin J.H., Kook H., Shin D.H., Hwang T.J., Kim M., Suh S.P., Ryang D.W. Nosocomial Cluster of Candida lipolytica Fungemia in Pediatric Patients. Eur. J. Clin. Microbiol. 2000;19:344–349. doi: 10.1007/s100960050491. [DOI] [PubMed] [Google Scholar]
- 76.Abbes S., Amouri I., Trabelsi H., Neji S., Sellami H., Rahmouni F., Makni F., Rebai T., Ayadi A. Analysis of virulence factors and in vivo biofilm-forming capacity of Yarrowia lipolytica isolated from patients with fungemia. Med. Mycol. 2016;55:193–202. doi: 10.1093/mmy/myw028. [DOI] [PubMed] [Google Scholar]
- 77.Bahloul M., Chtara K., Turki O., Bouaziz N.K., Regaieg K., Hammami M., Ben Amar W., Chabchoub I., Ammar R., Ben Hamida C., et al. Yarrowia lipolytica fungemia in patients with severe polytrauma requiring intensive care admission: Analysis of 32 cases. Intensiv. Care Med. 2017;43:1921–1923. doi: 10.1007/s00134-017-4900-3. [DOI] [PubMed] [Google Scholar]
- 78.Taj-Aldeen S.J., Abdulwahab A., Kolecka A., Deshmukh A., Meis J.F., Boekhout T. Uncommon opportunistic yeast bloodstream infections from Qatar. Med. Mycol. 2014;52:552–556. doi: 10.1093/mmycol/myu016. [DOI] [PubMed] [Google Scholar]
- 79.Viudes A., Pemán J., Cantón E., Úbeda P., Lopez-Ribot J.L., Gobernado M. Candidemia at a Tertiary-Care Hospital: Epidemiology, Treatment, Clinical Outcome and Risk Factors for Death. Eur. J. Clin. Microbiol. 2002;21:767–774. doi: 10.1007/s10096-002-0822-1. [DOI] [PubMed] [Google Scholar]
- 80.EUCAST Breakpoint Tables for Interpretation of MICs, Version 10.0, Valid from 4 February 2020. [(accessed on 18 August 2022)]. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/AFST/Clinical_breakpoints/AFST_BP_v10.0_200204_updatd_links_200924.pdf.
- 81.Pappagianis D., Collins M.S., Hector R., Remington J. Development of Resistance to Amphotericin B in Candida lusitaniae Infecting a Human. Antimicrob. Agents Chemother. 1979;16:123–126. doi: 10.1128/AAC.16.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Peyron F., Favel A., Michel-Nguyen A., Gilly M., Regli P., Bolmström A. Improved Detection of Amphotericin B-Resistant Isolates of Candida lusitaniae by Etest. J. Clin. Microbiol. 2001;39:339–342. doi: 10.1128/JCM.39.1.339-342.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Minari A., Hachem R., Raad I. Candida lusitaniae: A Cause of Breakthrough Fungemia in Cancer Patients. Clin. Infect. Dis. 2001;32:186–190. doi: 10.1086/318473. [DOI] [PubMed] [Google Scholar]
- 84.Merz W.G. Candida lusitaniae: Frequency of recovery, colonization, infection, and amphotericin B resistance. J. Clin. Microbiol. 1984;20:1194–1195. doi: 10.1128/jcm.20.6.1194-1195.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yoon S.A., Vazquez J.A., Steffan P.E., Sobel J.D., Akins R.A. High-Frequency, In Vitro Reversible Switching of Candida lusitaniae Clinical Isolates from Amphotericin B Susceptibility to Resistance. Antimicrob. Agents Chemother. 1999;43:836–845. doi: 10.1128/AAC.43.4.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rodrigues C.F., Henriques M. Liposomal and Deoxycholate Amphotericin B Formulations: Effectiveness against Biofilm Infections of Candida spp. Pathogens. 2017;6:62. doi: 10.3390/pathogens6040062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Viudes A., Pemán J., Cantón E., Salavert M., Úbeda P., Lopez-Ribot J., Gobernado M. Two Cases of Fungemia due to Candida lusitaniae and a Literature Review. Eur. J. Clin. Microbiol. 2002;21:294–299. doi: 10.1007/s10096-002-0713-5. [DOI] [PubMed] [Google Scholar]
- 88.Bariola J.R., Saccente M. Candida lusitaniae septic arthritis: Case report and review of the literature. Diagn. Microbiol. Infect. Dis. 2008;61:61–63. doi: 10.1016/j.diagmicrobio.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 89.Khan Z., Ahmad S., Al-Sweih N., Khan S., Joseph L. Candida lusitaniae in Kuwait: Prevalence, antifungal susceptibility and role in neonatal fungemia. PLoS ONE. 2019;14:e0213532. doi: 10.1371/journal.pone.0213532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pietrucha-Dilanchian P., Lewis R.E., Ahmad H., Lechin A.E. Candida Lusitaniae Catheter-Related Sepsis. Ann. Pharmacother. 2001;35:1570–1574. doi: 10.1345/aph.1A077. [DOI] [PubMed] [Google Scholar]
- 91.Hawkins J.L., Baddour L.M. Candida lusitaniae Infections in the Era of Fluconazole Availability. Clin. Infect. Dis. 2003;36:e14–e18. doi: 10.1086/344651. [DOI] [PubMed] [Google Scholar]
- 92.Blinkhorn R.J., Adelstein D., Spagnuolo P.J. Emergence of a new opportunistic pathogen, Candida lusitaniae. J. Clin. Microbiol. 1989;27:236–240. doi: 10.1128/jcm.27.2.236-240.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wawrysiuk S., Rechberger T., Futyma K., Miotła P. Candida lusitaniae—A case report of an intraperitoneal infection. Menopausal Rev. 2018;17:94–96. doi: 10.5114/pm.2018.77310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Elkamouni Y., Lmimouni B., Doghmi K., Elouenass M. Candida famata candidemia in immunosuppressed patient: Report of a case with literature review. Ann. Biol. Clin. 2011;69:609–611. doi: 10.1684/abc.2011.0622. [DOI] [PubMed] [Google Scholar]
- 95.Diba K., Makhdoomi K., Nasri E., Vaezi A., Javidnia J., Gharabagh D.J., Jazani N.H., Chavshin A.R., Badiee P., Badali H., et al. Emerging Candida species isolated from renal transplant recipients: Species distribution and susceptibility profiles. Microb. Pathog. 2018;125:240–245. doi: 10.1016/j.micpath.2018.09.026. [DOI] [PubMed] [Google Scholar]
- 96.Beyda N.D., Lewis R.E., Garey K.W. Echinocandin Resistance in Candida Species: Mechanisms of Reduced Susceptibility and Therapeutic Approaches. Ann. Pharmacother. 2012;46:1086–1096. doi: 10.1345/aph.1R020. [DOI] [PubMed] [Google Scholar]
- 97.Karapetsa M., Tsolaki V., Arabatzis M., Petinaki E., Velegraki A., Zakynthinos E. Septic shock due to Candida famata (Debaryomyces hansenii) candidemia in an ICU immunocompetent trauma-patient. J. Infect. Public Health. 2019;12:594–597. doi: 10.1016/j.jiph.2018.12.015. [DOI] [PubMed] [Google Scholar]
- 98.Marcos-Zambrano L.J., Puig-Asensio M., Pérez-García F., Escribano P., Sánchez-Carrillo C., Zaragoza O., Padilla B., Cuenca-Estrella M., Almirante B., Martín-Gómez M.T., et al. Candida guilliermondii Complex Is Characterized by High Antifungal Resistance but Low Mortality in 22 Cases of Candidemia. Antimicrob. Agents Chemother. 2017;61:e00099-17. doi: 10.1128/AAC.00099-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Dick J.D., Rosengard B.R., Merz W.G., Stuart R.K., Hutchins G.M., Saral R. Fatal Disseminated Candidiasis Due to Amphotericin-B-Resistant Candida guilliermondii. Ann. Intern. Med. 1985;102:67–68. doi: 10.7326/0003-4819-102-1-67. [DOI] [PubMed] [Google Scholar]
- 100.Chen C.-Y., Huang S.-Y., Tang J.-L., Tsay W., Yao M., Ko B.-S., Chou W.-C., Tien H.-F., Hsueh P.-R. Clinical features of patients with infections caused by Candida guilliermondii and Candida fermentati and antifungal susceptibility of the isolates at a medical centre in Taiwan, 2001–2010. J. Antimicrob. Chemother. 2013;68:2632–2635. doi: 10.1093/jac/dkt214. [DOI] [PubMed] [Google Scholar]
- 101.Nucci M., Marr K.A. Emerging Fungal Diseases. Clin. Infect. Dis. 2005;41:521–526. doi: 10.1086/432060. [DOI] [PubMed] [Google Scholar]
- 102.Pfaller M.A., Diekema D.J. Rare and Emerging Opportunistic Fungal Pathogens: Concern for Resistance beyond Candida albicans and Aspergillus fumigatus. J. Clin. Microbiol. 2004;42:4419. doi: 10.1128/JCM.42.10.4419-4431.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Reinhardt J.F., Ruane P.J., Walker L.J., George W.L. Intravenous catheter-associated fungemia due to Candida rugosa. J. Clin. Microbiol. 1985;22:1056–1057. doi: 10.1128/jcm.22.6.1056-1057.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sugar A., Stevens D.A. Candida rugosa in immunocompromised infection case reports, drug susceptibility, and review of the literature. Cancer. 1985;15:318–320. doi: 10.1002/1097-0142(19850715)56:2<318::AID-CNCR2820560219>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 105.Dubé M.P., Heseltine P.N.R., Rinaldi M.G., Evans S., Zawacki B. Fungemia and Colonization with Nystatin-Resistant Candida rugosa in a Burn Unit. Clin. Infect. Dis. 1994;18:77–82. doi: 10.1093/clinids/18.1.77. [DOI] [PubMed] [Google Scholar]
- 106.Colombo A.L., Azevedo Melo A.S., Crespo Rosas R.F., Salomão R., Briones M., Hollis R.J., Messer S.A., Pfaller M.A. Outbreak of Candida rugosa candidemia: An emerging pathogen that may be refractory to amphotericin B therapy. Diagn. Microbiol. Infect. Dis. 2003;46:253–257. doi: 10.1016/S0732-8893(03)00079-8. [DOI] [PubMed] [Google Scholar]
- 107.Rosas R., Nucci M., Castelo A., Colombo A.L. Predictive value of Candida spp. colonization in the diagnosis of candidemia in intensive care unit patients (abstract M-269); Proceedings of the 44th Interscience Conference on Antimicrobial Agents and Chemotherapy; Washington DC, USA. 30 October–2 November 2004. [Google Scholar]
- 108.Behera B., Singh R.I., Xess I., Mathur P., Hasan F., Misra M.C. Candida rugosa: A possible emerging cause of candidaemia in trauma patients. Infection. 2010;38:387–393. doi: 10.1007/s15010-010-0044-x. [DOI] [PubMed] [Google Scholar]
- 109.Colombo A.L., Guimarães T., Silva L.R.B.F., de Almeida Monfardini L.P., Cunha A.K.B., Rady P., Alves T., Rosas R.C. Prospective Observational Study of Candidemia in São Paulo, Brazil: Incidence Rate, Epidemiology, and Predictors of Mortality. Infect. Control Hosp. Epidemiol. 2007;28:570–576. doi: 10.1086/513615. [DOI] [PubMed] [Google Scholar]
- 110.da Matta D.A., de Almeida L.P., Machado A.M., Azevedo A.C., Kusano E.J.U., Travassos N.F., Salomão R., Colombo A.L. Antifungal susceptibility of 1000 Candida bloodstream isolates to 5 antifungal drugs: Results of a multicenter study conducted in São Paulo, Brazil, 1995–2003. Diagn. Microbiol. Infect. Dis. 2007;57:399–404. doi: 10.1016/j.diagmicrobio.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 111.Minces L.R., Ho K.S., Veldkamp P.J., Clancy C.J. Candida rugosa: A distinctive emerging cause of candidaemia. A case report and review of the literature. Scand. J. Infect. Dis. 2009;41:892–897. doi: 10.3109/00365540903161531. [DOI] [PubMed] [Google Scholar]
- 112.Piatti G., Feltrin S., Fellini E., Barbero V., Ballestrero A. Catheter-Related Sepsis by Candida Pararugosa in an Adult Patient under Chemotherapy Regimen. Case Rep. Infect. Dis. 2021;2021:8858157. doi: 10.1155/2021/8858157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.El Helou G., Palavecino E. Candida pararugosa: First Reported Bloodstream Infection in an Adult. Cureus. 2017;9:e1283. doi: 10.7759/cureus.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Noni M., Stathi A., Velegraki A., Malamati M., Kalampaliki A., Zachariadou L., Michos A. Rare Invasive Yeast Infections in Greek Neonates and Children, a Retrospective 12-Year Study. J. Fungi. 2020;6:194. doi: 10.3390/jof6040194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Arastehfar A., Shaban T., Zarrinfar H., Roudbary M., Ghazanfari M., Hedayati M.-T., Sedaghat A., Ilkit M., Najafzadeh M.J., Perlin D.S. Candidemia among Iranian Patients with Severe COVID-19 Admitted to ICUs. J. Fungi. 2021;7:280. doi: 10.3390/jof7040280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Oliveira V.K.P., Ruiz L.d.S., Oliveira N.A.J., Moreira D., Hahn R.C., de Azevedo Melo A.S., Nishikaku A.S., Paula C.R. Fun-gemia Caused by Candida Species in a Children’s Public Hospital in the City of São Paulo, Brazil: Study in the Period 2007-Revista do Instituto de Medicina Tropical de São Paulo. Rev. Inst. Med. Trop. São Paulo. 2014;56:301–305. doi: 10.1590/S0036-46652014000400006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Peremalo T., Madhavan P., Hamzah S., Than L., Wong E.H., Nasir M.D.M., Chong P.P., Ng K.P. Antifungal susceptibilities, biofilms, phospholipase and proteinase activities in the Candida rugosa complex and Candida pararugosa isolated from tertiary teaching hospitals. J. Med. Microbiol. 2019;68:346–354. doi: 10.1099/jmm.0.000940. [DOI] [PubMed] [Google Scholar]
- 118.Guarro J.W., Zhang J.P., Lawhon S., Fothergill S.D., Cano A.W., Sutton J., DA Paredes K. Molecular Identification and Antifungal Susceptibility Testing of Clinical Isolates of the Candida Rugosa Species Complex and Proposal of the New Spe-cies Candida Neorugosa. J. Clin. Microbiol. 2012;50:2397–2403. doi: 10.1128/JCM.00688-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Epis S., Capone A., Martin E., Paolucci M., Bazzocchi C., Valzano M., Bozic J., Novati S., Favia G., Ricci I. A rapid qPCR method to investigate the circulation of the yeast Wickerhamomyces anomalus in humans. New Microbiol. 2015;38:577–581. [PubMed] [Google Scholar]
- 120.Passoth V., Olstorpe M., Schnürer J. Past, present and future research directions with Pichia anomala. Antonie Leeuwenhoek. 2010;99:121–125. doi: 10.1007/s10482-010-9508-3. [DOI] [PubMed] [Google Scholar]
- 121.Medina I.R., Fuentes L.R., Arteaga M.B., Valcárcel F.R., Arbelo F.A., del Castillo D.P., Suárez S.D., Quintana O.F., Gutiérrez B.V., Sergent F.S., et al. Pigeons and their droppings as reservoirs of Candida and other zoonotic yeasts. Rev. Iberoam. Micol. 2017;34:211–214. doi: 10.1016/j.riam.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 122.Yılmaz-Semerci S., Demirel G., Tastekin A. Wickerhamomyces anomalus blood stream infection in a term newborn with pneumonia. Turk. J. Pediatr. 2017;59:349–351. doi: 10.24953/turkjped.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 123.Jung J., Moon Y.S., Yoo J.A., Lim J.-H., Jeong J., Jun J.-B. Investigation of a nosocomial outbreak of fungemia caused by Candida pelliculosa (Pichia anomala) in a Korean tertiary care center. J. Microbiol. Immunol. Infect. 2018;51:794–801. doi: 10.1016/j.jmii.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 124.Suhr M.J., Gomes-Neto J.C., Banjara N., Florescu D.F., Mercer D.F., Iwen P.C., Hallen-Adams H.E. Epidemiological In-vestigation of Candida Species Causing Bloodstream Infection in Paediatric Small Bowel Transplant Recipients. Mycoses. 2017;60:366–374. doi: 10.1111/myc.12603. [DOI] [PubMed] [Google Scholar]
- 125.Lin H.-C., Lin H.-Y., Su B.-H., Ho M.-W., Ho C.-M., Lee C.-Y., Lin M.-H., Hsieh H.-Y., Lin H.-C., Li T.-C., et al. Reporting an outbreak of Candida pelliculosa fungemia in a neonatal intensive care unit. J. Microbiol. Immunol. Infect. 2013;46:456–462. doi: 10.1016/j.jmii.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 126.Zhang Z., Cao Y., Li Y., Chen X., Ding C., Liu Y. Risk Factors and Biofilm Formation Analyses of Hospital-Acquired In-fection of Candida Pelliculosa in a Neonatal Intensive Care Unit. BMC Infect. Dis. 2021;21:620. doi: 10.1186/s12879-021-06295-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Yang Y., Wu W., Ding L., Yang L., Su J., Wu B. Two different clones of Candida pelliculosa bloodstream infection in a tertiary neonatal intensive care unit. J. Infect. Dev. Ctries. 2021;15:870–876. doi: 10.3855/jidc.12103. [DOI] [PubMed] [Google Scholar]
- 128.Svobodova L., Bednářová D., Hamal P. The Prevalence of Candida Pelliculosa, Candida Utilis, and Candida Fabianii in the Olomouc University Hospital: Epidemiological Study. Epidemiol. Mikrobiol. Imunol. Cas. Spol. Pro. Epidemiologii A Mikrobiol. Ceske Lek. Spol. JE Purkyne. 2016;65:34–38. [PubMed] [Google Scholar]
- 129.Cecarini V., Cuccioloni M., Bonfili L., Ricciutelli M., Valzano M., Cappelli A., Amantini C., Favia G., Eleuteri A.M., Angeletti M., et al. Identification of a Killer Toxin from Wickerhamomyces anomalus with β-Glucanase Activity. Toxins. 2019;11:568. doi: 10.3390/toxins11100568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Parafati L., Cirvilleri G., Restuccia C., Wisniewski M. Potential Role of Exoglucanase Genes (WaEXG1 and WaEXG2) in the Biocontrol Activity of Wickerhamomyces anomalus. Microb. Ecol. 2016;73:876–884. doi: 10.1007/s00248-016-0887-5. [DOI] [PubMed] [Google Scholar]
- 131.Harit T., Bellaouchi R., Rokni Y., Riahi A., Malek F., Asehraou A. Synthesis, Characterization, Antimicrobial Activity, and Docking Studies of New Triazolic Tripodal Ligands. Chem. Biodivers. 2017;14:e1700351. doi: 10.1002/cbdv.201700351. [DOI] [PubMed] [Google Scholar]
- 132.Paris A.P., Persel C., Serafin C.F., Simão R.d.C.G., Gandra R.F. Susceptibility of Candida albicans Isolated from Blood to Wickerhamomyces anomalous Mycocins. Curr. Microbiol. 2016;73:878–884. doi: 10.1007/s00284-016-1135-4. [DOI] [PubMed] [Google Scholar]
- 133.Tay S.-T., Lim S.-L., Tan H.-W. Growth inhibition of Candida species by Wickerhamomyces anomalus mycocin and a lactone compound of Aureobasidium pullulans. BMC Complement. Altern. Med. 2014;14:439. doi: 10.1186/1472-6882-14-439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Vasconcelos N.M., Fontes J.M., Lins M., Bernardo G.R.B., Araújo J.M., Lima G.M.S. Streptomyces ansochromogenes Tur-10 produces a substance with antifungal bioactivity. Genet. Mol. Res. 2015;14:5435–5444. doi: 10.4238/2015.May.22.13. [DOI] [PubMed] [Google Scholar]
- 135.Esgin H., Bulut E., Örüm Ç. Candida pelliculosa endophthalmitis after cataract surgery: A case report. BMC Res. Notes. 2014;7:169. doi: 10.1186/1756-0500-7-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hanada K., Miyokawa N., Sano A., Igarashi S., Yoshida A. Fungal Dacryocystitis with Cacosmia after Penetrating Kera-toplasty—Taxonomy and Identification of Pathogenic Fungi Based on DNA Sequence Analysis. Nippon Ganka Gakkai Zasshi. 2012;116:1144–1149. [PubMed] [Google Scholar]
- 137.Dutra V.R., Silva L.F., Oliveira A.N.M., Beirigo E.F., Arthur V.M., Da Silva R.B., Ferreira T.B., Andrade-Silva L., Silva M.V., Fonseca F.M., et al. Fatal Case of Fungemia by Wickerhamomyces anomalus in a Pediatric Patient Diagnosed in a Teaching Hospital from Brazil. J. Fungi. 2020;6:147. doi: 10.3390/jof6030147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Kamoshita M., Matsumoto Y., Nishimura K., Katono Y., Murata M., Ozawa Y., Shimmura S., Tsubota K. Wickerhamo-myces Anomalus Fungal Keratitis Responds to Topical Treatment with Antifungal Micafungin. J. Infect. Chemother. 2015;21:141–143. doi: 10.1016/j.jiac.2014.08.019. [DOI] [PubMed] [Google Scholar]
- 139.Ratcliffe L., Davies J., Anson J., Hales S., Beeching N.J., Beadsworth M.B.J. Candida Pelliculosa Meningitis as an Oppor-tunistic Infection in HIV: The First Reported Case. Int. J. STD AIDS. 2011;22:54–56. doi: 10.1258/ijsa.2010.010113. [DOI] [PubMed] [Google Scholar]
- 140.Cartier N., Chesnay A., N’Diaye D., Thorey C., Ferreira M., Haillot O., Bailly É., Desoubeaux G. Candida nivariensis: Identification strategy in mycological laboratories. J. Mycol. Médicale. 2020;30:101042. doi: 10.1016/j.mycmed.2020.101042. [DOI] [PubMed] [Google Scholar]
- 141.Tay S.T., Lotfalikhani A., Sabet N.S., Ponnampalavanar S., Sulaiman S., Na S.L., Ng K.P. Occurrence and Characteriza-tion of Candida Nivariensis from a Culture Collection of Candida Glabrata Clinical Isolates in Malaysia. Mycopathologia. 2014;178:307–314. doi: 10.1007/s11046-014-9778-9. [DOI] [PubMed] [Google Scholar]
- 142.Borman A.M., Muller J., Walsh-Quantick J., Szekely A., Patterson Z., Palmer M.D., Fraser M., Johnson E.M. Fluconazole Resistance in Isolates of Uncommon Pathogenic Yeast Species from the United Kingdom. Antimicrob. Agents Chemother. 2019;63:e00211-19. doi: 10.1128/AAC.00211-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Arastehfar A., Daneshnia F., Salehi M.-R., Zarrinfar H., Khodavaisy S., Haas P.-J., Roudbary M., Najafzadeh M.-J., Zomorodian K., Charsizadeh A. Corrigendum: Molecular Characterization and Antifungal Susceptibility Testing of Can-dida Nivariensis from Blood Samples-an Iranian Multicentre Study and a Review of the Literature. J. Med. Microbiol. 2019;68:1695. doi: 10.1099/jmm.0.001075. [DOI] [PubMed] [Google Scholar]
- 144.Enache-Angoulvant A., Guitard J., Grenouillet F., Martin T., Durrens P., Fairhead C., Hennequin C. Rapid Discrimination between Candida glabrata, Candida nivariensis, and Candida bracarensis by Use of a Singleplex PCR. J. Clin. Microbiol. 2011;49:3375–3379. doi: 10.1128/JCM.00688-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Decat E., Van Mechelen E., Saerens B., Vermeulen S.J.T., Boekhout T., De Blaiser S., Vaneechoutte M., Deschaght P. Rapid and Accurate Identification of Isolates of Candida Species by Melting Peak and Melting Curve Analysis of the Inter-nally Transcribed Spacer Region 2 Fragment (ITS2-MCA) Res. Microbiol. 2013;164:110–117. doi: 10.1016/j.resmic.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 146.Cai S., Xu J., Shao Y., Gong J., Zhao F., He L., Shan X. Rapid identification of the Candida glabrata species complex by high-resolution melting curve analysis. J. Clin. Lab. Anal. 2020;34:e23226. doi: 10.1002/jcla.23226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Shi Y., Zhu Y., Fan S., Vitagliano A., Liu X., Liao y., Liang Y., Vitale S.G. Clinical Characteristics and Antifungal Susceptibility of Candida nivariensis from Vulvovaginal Candidiasis. Gynecol. Obstet. Investig. 2020;85:88–93. doi: 10.1159/000504095. [DOI] [PubMed] [Google Scholar]
- 148.Hernando-Ortiz A., Mateo E., Ortega-Riveros M., De-La-Pinta I., Quindós G., Eraso E. Caenorhabditis elegans as a Model System To Assess Candida glabrata, Candida nivariensis, and Candida bracarensis Virulence and Antifungal Efficacy. Antimicrob. Agents Chemother. 2020;64:e00824-20. doi: 10.1128/AAC.00824-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Gupta B., Gupta S., Chaudhary M., Raj A.T., Awan K.H., Patil S. Oral candida prevalence and species specificity in leprosy. Disease-a-Month. 2020;66:100920. doi: 10.1016/j.disamonth.2019.100920. [DOI] [PubMed] [Google Scholar]
- 150.López-Soria L.M., Bereciartua E., Santamaría M., Soria L.M., Hernández-Almaraz J.L., Mularoni A., Nieto J., Montejo M. First Case Report of Catheter-Related Fungemia by Candida Nivariensis in the Iberian Peninsula. Rev. Iberoam. Micol. 2012;30:69–71. doi: 10.1016/j.riam.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 151.Sikora M., Kuthan R., Piskorska-Malolepsza K., Golas-Pradzynska M., Domański D., Augustynowicz-Kopeć E., Swoboda-Kopec E. Prevalence and Antifungal Susceptibility of the Emerging Fungal Species, Candida nivariensis, Isolated in a Teaching Hospital in Poland. Pol. J. Microbiol. 2019;68:303–308. doi: 10.33073/pjm-2019-032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Li J., Shan Y., Fan S., Liu X. Prevalence of Candida nivariensis and Candida bracarensis in Vulvovaginal Candidiasis. Mycopathologia. 2014;178:279–283. doi: 10.1007/s11046-014-9800-2. [DOI] [PubMed] [Google Scholar]
- 153.Morales-López S., Dudiuk C., Vivot W., Szusz W., Córdoba S.B., Garcia-Effron G. Phenotypic and Molecular Evaluation of Echinocandin Susceptibility of Candida glabrata, Candida bracarensis, and Candida nivariensis Strains Isolated during 30 Years in Argentina. Antimicrob. Agents Chemother. 2017;61:e00170-17. doi: 10.1128/AAC.00170-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Treviño-Rangel R.D.J., Espinosa-Pérez J.F., Villanueva-Lozano H., Montoya A.M., Andrade A., Bonifaz A., González G.M. First report of Candida bracarensis in Mexico: Hydrolytic enzymes and antifungal susceptibility pattern. Folia Microbiol. 2018;63:517–523. doi: 10.1007/s12223-018-0592-5. [DOI] [PubMed] [Google Scholar]
- 155.Correia A., Sampaio P., James S., Pais C. Candida bracarensis sp. nov., a novel anamorphic yeast species phenotypically similar to Candida glabrata. Int. J. Syst. Evol. Microbiol. 2006;56:313–317. doi: 10.1099/ijs.0.64076-0. [DOI] [PubMed] [Google Scholar]
- 156.Moreira A., Silva S., Botelho C., Sampaio P., Pais C., Henriques M. Candida bracarensis: Evaluation of Virulence Factors and its Tolerance to Amphotericin B and Fluconazole. Mycopathologia. 2015;180:305–315. doi: 10.1007/s11046-015-9925-y. [DOI] [PubMed] [Google Scholar]
- 157.Lotfali E., Fattahi A., Sayyahfar S., Ghasemi R., Rabiei M.M., Fathi M., Vakili K., Deravi N., Soheili A., Toreyhi H., et al. A Review on Molecular Mechanisms of Antifungal Resistance in Candida glabrata: Update and Recent Advances. Microb. Drug Resist. 2021;27:1371–1388. doi: 10.1089/mdr.2020.0235. [DOI] [PubMed] [Google Scholar]
- 158.Telleria O., Ezpeleta G., Herrero O., Miranda-Zapico I., Quindós G., Cisterna R. Validation of the PCR–dHPLC method for rapid identification of Candida glabrata phylogenetically related species in different biological matrices. J. Chromatogr. B. 2012;893–894:150–156. doi: 10.1016/j.jchromb.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 159.Miranda-Zapico I., Eraso E., Hernández-Almaraz J.L., López-Soria L.M., Carrillo-Muñoz A.J., Hernández-Molina J.M., Quindós G. Prevalence and antifungal susceptibility patterns of new cryptic species inside the species complexes Candida parapsilosis and Candida glabrata among blood isolates from a Spanish tertiary hospital. J. Antimicrob. Chemother. 2011;66:2315–2322. doi: 10.1093/jac/dkr298. [DOI] [PubMed] [Google Scholar]
- 160.Swoboda-Kopeć E., Sikora M., Golas M., Piskorska K., Gozdowski D., Netsvyetayeva I. Candida nivariensis in comparison to different phenotypes of Candida glabrata. Mycoses. 2014;57:747–753. doi: 10.1111/myc.12264. [DOI] [PubMed] [Google Scholar]
- 161.Małek M., Mrowiec P., Klesiewicz K., Skiba-Kurek I., Szczepański A., Białecka J., Żak I., Bogusz B., Kędzierska J., Budak A., et al. Prevalence of human pathogens of the clade Nakaseomyces in a culture collection—the first report on Candida bracarensis in Poland. Folia Microbiol. 2018;64:307–312. doi: 10.1007/s12223-018-0655-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Asadzadeh M., Alanazi A.F., Ahmad S., Al-Sweih N., Khan Z. Lack of detection of Candida nivariensis and Candida bracarensis among 440 clinical Candida glabrata sensu lato isolates in Kuwait. PLoS ONE. 2019;14:e0223920. doi: 10.1371/journal.pone.0223920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Hou X., Xiao M., Chen S.C., Kong F., Wang H., Fan X., Zhao Y.-P., Xu Y.-C. Identification of Candida glabrata complex species: Use of Vitek MS® RUO & Bruker ClinproTools®. Future Microbiol. 2018;13:645–657. doi: 10.2217/fmb-2017-0241. [DOI] [PubMed] [Google Scholar]
- 164.Morales-lópez S., Dudiuk C., Vivot W., Szusz W. Crossm Phenotypic and Molecular Evaluation of Echinocandin Suscepti-bility of Candida. Antimicrob. Agents Chemother. 2017;61:7–10. doi: 10.1128/AAC.00170-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Hasejima N., Kamei K., Matsubayashi M., Kawabe R., Shimura C., Hijikata N., Oda T., Matsushima H. The first case of bloodstream infection by Candida intermedia in Japan: The importance of molecular identification. J. Infect. Chemother. 2011;17:555–558. doi: 10.1007/s10156-011-0215-4. [DOI] [PubMed] [Google Scholar]
- 166.Charsizadeh A., Mirhendi H., Nikmanesh B., Eshaghi H., Makimura K. Microbial epidemiology of candidaemia in neonatal and paediatric intensive care units at the Children’s Medical Center, Tehran. Mycoses. 2017;61:22–29. doi: 10.1111/myc.12698. [DOI] [PubMed] [Google Scholar]
- 167.Shirkhani S., Sepahvand A., Mirzaee M., Anbari K. Phospholipase and proteinase activities of Candida spp. isolates from vulvovaginitis in Iran. J. Mycol. Médicale. 2016;26:255–260. doi: 10.1016/j.mycmed.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 168.Hesham A.E.-L., Gupta V.K., Singh B. Use of PCR-denaturing gradient gel electrophoresis for the discrimination of Candida species isolated from natural habitats. Microb. Pathog. 2018;120:19–22. doi: 10.1016/j.micpath.2018.04.027. [DOI] [PubMed] [Google Scholar]
- 169.Tietz H.J., Küssner A., Thanos M., de Andrade M.P., Presber W., Schönian G. Phenotypic and genotypic characterization of unusual vaginal isolates of Candida albicans from Africa. J. Clin. Microbiol. 1995;33:2462–2465. doi: 10.1128/jcm.33.9.2462-2465.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Al-Hedaithy S.S.A., Fotedar R. Recovery and studies on chlamydospore-negativeCandida albicansisolated from clinical specimens. Med. Mycol. 2002;40:301–306. doi: 10.1080/mmy.40.3.301.306. [DOI] [PubMed] [Google Scholar]
- 171.Romeo O., Criseo G. Molecular Epidemiology of Candida albicans and Its Closely Related Yeasts Candida dubliniensis and Candida africana. J. Clin. Microbiol. 2009;47:212–214. doi: 10.1128/JCM.01540-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Romeo O., Criseo G. Morphological, biochemical and molecular characterisation of the first ItalianCandida africanaisolate. Mycoses. 2009;52:454–457. doi: 10.1111/j.1439-0507.2008.01630.x. [DOI] [PubMed] [Google Scholar]
- 173.Alonso-Vargas R., Elorduy L., Eraso E., Cano J.F., Guarro J., Pontón J., Quindós G. Isolation of Candida Africana, Proba-ble Atypical Strains of Candida Albicans, from a Patient with Vaginitis. Med. Mycol. 2008;46:167–170. doi: 10.1080/13693780701633101. [DOI] [PubMed] [Google Scholar]
- 174.Odds F.C., Bougnoux M.-E., Shaw D.J., Bain J.M., Davidson A.D., Diogo D., Jacobsen M.D., Lecomte M., Li S.-Y., Tavanti A., et al. Molecular Phylogenetics of Candida albicans. Eukaryot. Cell. 2007;6:1041–1052. doi: 10.1128/EC.00041-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Tietz H.-J., Hopp M., Schmalreck A., Sterry W., Czaika V. Candida africana sp. nov., a new human pathogen or a variant of Candida albicans? Mycoses. 2001;44:437–445. doi: 10.1046/j.1439-0507.2001.00707.x. [DOI] [PubMed] [Google Scholar]
- 176.Forche A., Schönianb G., Gräserb Y., Vilgalys R., Mitchell T.G. Genetic Structure of Typical and Atypical Populations of Candida albicans from Africa. Fungal Genet. Biol. 1999;28:107–125. doi: 10.1006/fgbi.1999.1164. [DOI] [PubMed] [Google Scholar]
- 177.Sharma C., Muralidhar S., Xu J., Meis J.F., Chowdhary A. Multilocus sequence typing of Candida Africana from patients with vulvovaginal candidiasis in New Delhi, India. Mycoses. 2014;57:544–552. doi: 10.1111/myc.12193. [DOI] [PubMed] [Google Scholar]
- 178.Hazirolan G., Altun H.U., Gumral R., Gursoy N.C., Otlu B., Sancak B. Prevalence of Candida africana and Candida dubliniensis, in vulvovaginal candidiasis: First Turkish Candida africana isolates from vulvovaginal candidiasis. J. Mycol. Med. 2017;27:376–381. doi: 10.1016/j.mycmed.2017.04.106. [DOI] [PubMed] [Google Scholar]
- 179.Yazdanparast S.A., Khodavaisy S., Fakhim H., Shokohi T., Haghani I., Nabili M., Gholami H., Ahmadi I., Badali H. Molecular Characterization of Highly Susceptible Candida africana from Vulvovaginal Candidiasis. Mycopathologia. 2015;180:317–323. doi: 10.1007/s11046-015-9924-z. [DOI] [PubMed] [Google Scholar]
- 180.Majdabadi N., Falahati M., Heidarie-Kohan F., Farahyar S., Rahimi-Moghaddam P., Ashrafi-Khozani M., Razavi T., Mohammadnejad S. Effect of 2-Phenylethanol as Antifungal Agent and Common Antifungals (Amphotericin B, Fluconazole, and Itraconazole) on Candida Species Isolated from Chronic and Recurrent Cases of Candidal Vulvovaginitis. ASSAY Drug Dev. Technol. 2018;16:141–149. doi: 10.1089/adt.2017.837. [DOI] [PubMed] [Google Scholar]
- 181.Naeimi B., Mirhendi H., Khamisipour G., Sadeghzadeh F., Ahmadi B. Candida Africana in Recurrent Vulvovaginal Can-didiasis (RVVC) Patients: Frequency and Phenotypic and Genotypic Characteristics. J. Med. Microbiol. 2018;67:1601–1607. doi: 10.1099/jmm.0.000834. [DOI] [PubMed] [Google Scholar]
- 182.Hu Y., Yu A., Chen X., Wang G., Feng X. Molecular Characterization ofCandida africanain Genital Specimens in Shanghai, China. BioMed Res. Int. 2015;2015:185387. doi: 10.1155/2015/185387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Borman A.M., Szekely A., Linton C.J., Palmer M.D., Brown P., Johnson E.M. Epidemiology, Antifungal Susceptibility, and Pathogenicity of Candida Africana Isolates from the United Kingdom. J. Clin. Microbiol. 2013;51:967–972. doi: 10.1128/JCM.02816-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Romeo O., Criseo G. Candida africana and its closest relatives. Mycoses. 2010;54:475–486. doi: 10.1111/j.1439-0507.2010.01939.x. [DOI] [PubMed] [Google Scholar]
- 185.Ngouana T.K., Krasteva D., Drakulovski P., Toghueo R.K., Kouanfack C., Ambe A., Reynes J., Delaporte E., Boyom F.F., Mallié M., et al. Investigation of minor species Candida africana, Candida stellatoidea and Candida dubliniensis in the Candida albicans complex among Yaoundé (Cameroon) HIV-infected patients. Mycoses. 2015;58:33–39. doi: 10.1111/myc.12266. [DOI] [PubMed] [Google Scholar]
- 186.Theill L., Dudiuk C., Morano S., Gamarra S., Nardin M.E., Méndez E., Garcia-Effron G. Prevalence and antifungal susceptibility of Candida albicans and its related species Candida dubliniensis and Candida africana isolated from vulvovaginal samples in a hospital of Argentina. Rev. Argent. Microbiol. 2016;48:43–49. doi: 10.1016/j.ram.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 187.Shan Y., Fan S., Liu X., Li J. Prevalence of Candida albicans-closely related yeasts, Candida africana and Candida dubliniensis, in vulvovaginal candidiasis. Med. Mycol. 2014;52:636–640. doi: 10.1093/mmy/myu003. [DOI] [PubMed] [Google Scholar]
- 188.Nnadi E., Ayanbimpe G., Scordino F., Okolo M.O., Enweani I.B., Criseo G., Romeo O. Isolation and molecular characterization ofCandida africanafrom Jos, Nigeria. Med. Mycol. 2012;50:765–767. doi: 10.3109/13693786.2012.662598. [DOI] [PubMed] [Google Scholar]
- 189.Buckley H.R., van Uden N. Five new Candida species. Mycopathologia. 1968;36:257–266. doi: 10.1007/BF02050372. [DOI] [PubMed] [Google Scholar]
- 190.De Almeida J.N., Campos S.V., Thomaz D.Y., Thomaz L., de Almeida R.K.G., del Negro G.M.B., Gimenes V.F., Grenfell R.C., Motta A.L., Rossi F., et al. Candida Blankii: An Emergent Opportunistic Yeast with Reduced Susceptibility to Antifungals Correspondence. Emerg. Microbes Infect. 2018;7:1–3. doi: 10.1038/s41426-017-0015-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Chowdhary A., Stielow J.B., Upadhyaya G., Singh P.K., Singh A., Meis J.F. Candida blankii: An emerging yeast in an outbreak of fungaemia in neonates in Delhi, India. Clin. Microbiol. Infect. 2020;26:648.e5–648.e8. doi: 10.1016/j.cmi.2020.01.001. [DOI] [PubMed] [Google Scholar]
- 192.Al-Haqqan A., Al-Sweih N., Ahmad S., Khan S., Joseph L., Varghese S., Khan Z. Azole-resistant Candida blankii as a newly recognized cause of bloodstream infection. New Microbes. New Infect. 2018;26:25–29. doi: 10.1016/j.nmni.2018.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Kollu V.S., Kalagara P.K., Islam S., Gupte A. A Report of Candida blankii Fungemia and Possible Endocarditis in an Immunocompetent Individual and the Review of Literature. Cureus. 2021;13:e14945. doi: 10.7759/cureus.14945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Pham T.T., Dinh K.V., Nguyen V.D. Biodiversity and Enzyme Activity of Marine Fungi with 28 New Records from the Tropical Coastal Ecosystems in Vietnam. Mycobiology. 2021;49:559–581. doi: 10.1080/12298093.2021.2008103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Bereczki L., Bartha N., Kocsube S., Soki J., Lengyel G., Tálosi G., Mader K., Deák J., Doczi I. Fungaemia caused by Candida pulcherrima. Med. Mycol. 2012;50:522–524. doi: 10.3109/13693786.2011.644590. [DOI] [PubMed] [Google Scholar]
- 196.Mpakosi A., Siopi M., Falaina V., Siafakas N., Roilides E., Kimouli M., Theodoraki M., Karle P., Meletiadis J. Successful therapy of Candida pulcherrima fungemia in a premature newborn with liposomal amphotericin B and micafungin. Med. Mycol. Case Rep. 2016;12:24–27. doi: 10.1016/j.mmcr.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Deconinck L., Meybeck A., Pradier M., Patoz P., Melliez H., Senneville E. Community acquired fungemia caused by Candida pulcherrima: Diagnostic contribution of MALDI-TOF mass spectrometry. Ann. Clin. Microbiol. Antimicrob. 2016;15:14. doi: 10.1186/s12941-016-0129-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Önal U., Metin D.Y., Karaca C., Polat S.H., Ersin S., Taşbakan M.I. Retrospective evaluation of candidemic patients among general surgery department in a tertiary care university hospital. Turk. J. Surg. 2019;35:210–213. doi: 10.5578/turkjsurg.4252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Marín Martínez E.M., Aller García A.I., Martín-Mazuelos E. Epidemiología, factores de riesgo y sensibilidad in vitro en candidemias por especies diferentes de Candida albicans. Rev. Iberoam. Micol. 2016;33:248–252. doi: 10.1016/j.riam.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 200.Türkel S., Ener B. Isolation and Characterization of New Metschnikowia Pulcherrima Strains as Producers of the Antimicrobial Pigment Pulcherrimin. 2009. [(accessed on 6 July 2022)]. Available online: http://uu245-211.uludag.edu.tr/handle/11452/22813. [DOI] [PubMed]
- 201.Cuenca-Estrella M., Gomez-Lopez A., Isla G., Rodriguez D., Almirante B., Pahissa A., Rodriguez-Tudela J.L., Group B.C.P.S. Prevalence of Candida Bracarensis and Candida Nivariensis in a Spanish Collection of Yeasts: Comparison of Re-sults from a Reference Centre and from a Population-Based Surveillance Study of Candidemia. Med. Mycol. 2011;49:525–529. doi: 10.3109/13693786.2010.546373. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.