Abstract
Introduction: As the number of elderly patients requiring surgical intervention rises, it is believed that frailty syndrome has a greater impact on perioperative course than on chronological age. The aim of this study was to evaluate the efficacy of various imaging features for frailty assessment in patients undergoing emergency laparotomy. Methods: The study included all patients that qualified for emergency surgery with preoperative CT scans between 2016 and 2020 in the Second Department of General Surgery. Multiple trauma patients were excluded from the analysis. The modified frailty index and brief geriatric assessment were used in the analysis. CT images were reviewed for the assessment of osteopenia, sarcopenia, sarcopenic obesity, renal volume and abdominal aorta calcification rate. Results: A total of 261 patients were included in the analysis. Multivariate logistic regression identified every next ASA class (OR: 4.161, 95%CI: 1.672–10.355, p = 0.002), intraoperative adverse events (OR: 12.397, 95%CI: 2.166–70.969, p = 0.005) and osteopenia (OR: 4.213, 95%CI: 1.235–14.367, p = 0.022) as a risk factor for 30-day mortality. Our study showed that every next ASA class (OR: 1.952, 95%Cl: 1.171–3.256, p = 0.010) and every point of the BGA score (OR: 1.496, 95%Cl: 1.110–2.016, p = 0.008) are risk factors for major complications. Conclusions: Osteopenia was the best parameter for perioperative mortality risk stratification in patients undergoing emergency surgical intervention. Sarcopenia (measured as psoas muscle area), sarcopenic obesity, aortic calcifications and mean kidney volume do not predict poor outcomes in those patients. None of the radiological markers appeared to be useful for the prediction of perioperative morbidity.
Keywords: frailty, emergency surgery, emergency laparotomy, elderly, osteopenia, sarcopenia, sarcopenic obesity, abdominal aorta calcification rate, renal volume, BGA score, mFI, modified frailty index, brief geriatric assessment
1. Introduction
As life expectancy around the world is increasing, the number of elderly patients requiring surgical intervention rises. Geriatric patients usually have more comorbidities, which increases the risk of perioperative complications [1,2]. Having said that, metrical age itself does not seem to be an independent risk factor for morbidity [3]. Thus, research on risk assessment is shifting its focus to patient frailty evaluation [4]. There are several methods to estimate frailty, including scales that score patients based on the occurrence of different concomitant diseases [5,6]. This approach assumes full access to a patient’s medical records, which creates a serious limitation in emergency surgery situations [7]. Inability to properly communicate with the patient and missing information about their coexisting conditions makes comorbidity scoring ineligible. This is the reason why alternative methods of frailty assessment might be useful in such cases [8].
Several new approaches for frailty assessment using computed tomography (CT) measurements were proposed. For instance, assessment of sarcopenia by measuring psoas muscle area has been proven to be efficient [9,10,11,12,13]. Other imaging features, such as sarcopenic obesity, aortic calcifications, osteopenia, and mean kidney pixel value, are mentioned as options for frailty assessment [8]. However, an optimal radiological parameter for frailty assessment has still not been selected. Therefore, our study aimed to evaluate the efficacy of various imaging features for frailty assessment in patients undergoing emergency laparotomy.
2. Materials and Methods
This study was approved by the local research ethics committee following the guidelines of the Declaration of Helsinki of 1975, with its later amendments. The study obtained the approval of the Ethics Committee of the Jagiellonian University no. 1072.6120.14.2020. Every patient has given informed consent to be included in the study.
A retrospective database of patients who have undergone emergency surgical intervention between January 2016 and December 2020 was developed. A dataset was created in a tertiary referral university hospital, with an annual volume of around 1500 emergency surgeries. Patients that qualified for emergency surgery with preoperative CT scans were included in the study. We excluded patients submitted to the surgery with different imaging modalities used (X-ray, ultrasound) or with no preoperative imaging. Due to the unit profile, only patients above 18 years old were included in the study. Multiple trauma patients were excluded from the analysis. Additionally, every patient had their frailty assessed with the frailty index (mFI) and brief geriatric assessment (BGA) scales [5]. Complications were reported following the Clavien–Dindo classification [14].
All CT studies were acquired on a 64-slice GE Optima CT660 scanner (GE Healthcare, Boston, MA, USA) and included series before and after administering contrast agents. Venous phase series were extracted for further analysis. All volumes had a maximum of 1.3 mm layer height.
The exported images were reviewed using the RadiAnt DICOM viewer (Medixant, Poznań, Poland) and Mimics (Materialise NV, Leuven, Belgium) for the assessment of osteopenia, sarcopenia, sarcopenic obesity, renal volume, and abdominal aorta calcification rate. CT scan measurements were carried out by trained evaluators and reviewed by a board-certified radiologist with 15 years of experience in abdominal and emergency imaging.
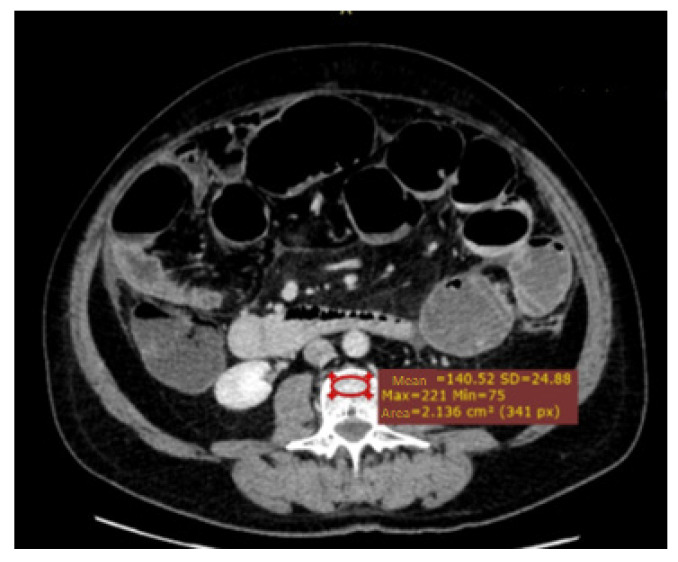
As described previously, measurement of the attenuation in Hounsfield units (HU) within the region of interest (ROI) is the preferred way to assess osteopenia [15]. A 2D ROI was placed in the anterior trabecular area of the vertebrae on an axial projection at the L3 level (Figure 1).
Figure 1.
Osteopenia assessment—ROI (region of interest)—anterior trabecular area of the vertebrae on an axial projection at the L3 level.
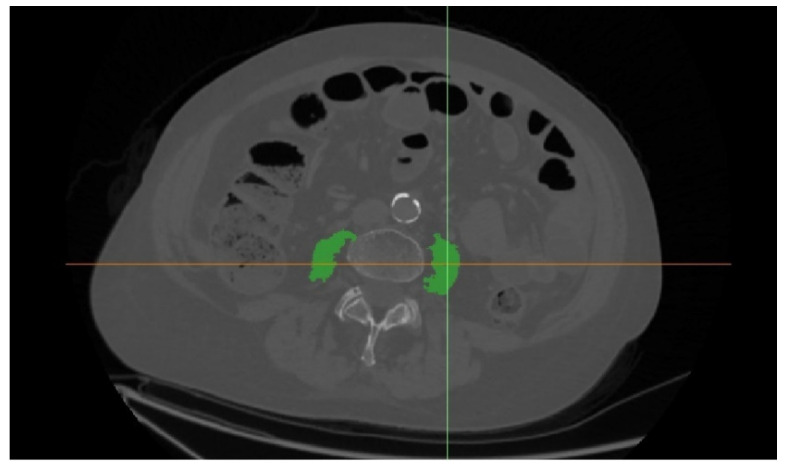
Sarcopenia assessment was defined as the bilateral psoas muscles area normalized for the patient’s height (cm2/m2) at the level of L3. The area was contoured semi-automatically with region growth algorithms and (−29,150 HU) limits. The segmented areas were manually corrected if necessary (Figure 2).
Figure 2.
Bilateral psoas muscles area.
The sarcopenic obesity parameter was defined as the total cross-sectional visceral and subcutaneous fat tissue area divided by the total cross-sectional muscle tissue area on a single axial slice at L3 (Figure 3). Following the approach from other studies, region growth algorithms were used with the (−150, 50 HU) range for visceral fat and (−190, 30 HU) for subcutaneous fat [16].
Figure 3.
Sarcopenic obesity assessment.
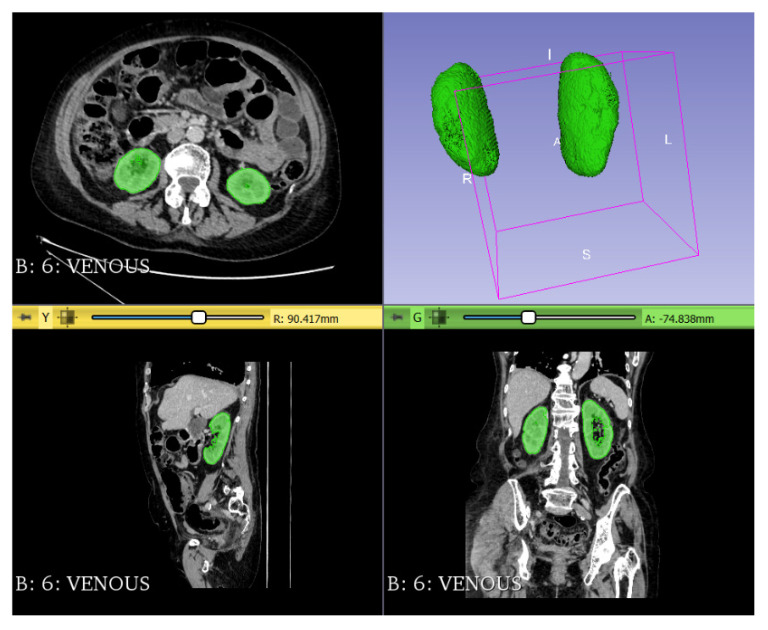
Kidneys were segmented semi-automatically and bilateral renal volume was normalized for the patient’s height (Figure 4). All artifacts, kidney vessels, renal calyces and pelvises, and renal cysts were manually excluded from the volume calculations.
Figure 4.
Renal volume measurement.
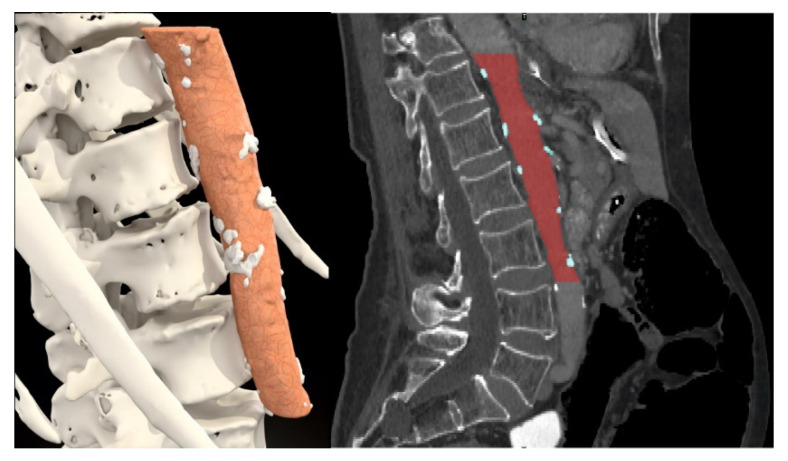
The abdominal aorta calcification rate was calculated as a percentage of calcification volume divided by the total aorta volume. The aorta was segmented from Th12 to the bottom edge of L3 (Figure 5).
Figure 5.
Calcification plaque measurement in aorta.
Statistical Analysis
The primary outcome was the mortality rate. The secondary outcomes were the following perioperative features: complication rate, surgery duration, intensive care unit (ICU) admission, and readmission rate. All data were analyzed with Statistica version 13.0 PL (StatSoft Inc., Tulsa, OK, USA). Continuous results are presented as the median and interquartile range (IQR). Categorical variables were compared by the chi-square test. The Shapiro–Wilk test was used to check for the normal distribution of data, and Student’s t-test was used for normally distributed quantitative data. For non-normally distributed quantitative variables, the Mann–Whitney U test was used. A p-value < 0.05 was considered statistically significant. All considerable patient and treatment-related factors were analyzed with univariate logistic regression models in search of risk factors for mortality and morbidity. Receiver operating curves (ROC) were used to set cut-off points for frailty regarding psoas muscle area/height (PMA), sarcopenic obesity (SO), aortic calcification (AC), osteopenia and kidney volume (KV).
3. Results
A total of 261 patients were included in the analysis. The demographic characteristics of the study group are included in Table 1.
Table 1.
Baseline characteristics of study groups.
| Parameter | Total | Group 1 (30-Day Mortality—0) | Group 2 (30-Day Mortality—1) | p Value |
|---|---|---|---|---|
| Patients, n (%) | 261 | 215 (82.4%) | 46 (17.6%) | - |
| Females, n (%) | 128 (49%) | 105 (48.8%) | 23 (50%) | 0.886 |
| Median age (IQR) (years) | 65 (52–76) | 63 (47–74) | 77 (63–83) | <0.001 |
| Median BMI (IQR) (kg/m2) | 25.33 (22.86–28.22) | 24.91 (22.67–28.08) | 25.83 (23.00–29.29) | 0.172 |
| ASA class: I, n (%) II, n (%) III, n (%) IV, n (%) V, n (%) |
25 (9.6%) 88 (33.7%) 92 (35.2%) 52 (19.9%) 4 (1.5%) |
25 (11.6%) 87 (40.5%) 76 (35.3%) 27 (12.6%) 0 (0%) |
0 (0%) 1 (2.2%) 16 (34.8%) 25 (54.3%) 4 (8.7%) |
<0.001 |
| Comorbidities: Hypertension, n (%) Diabetes, n (%) Heart failure, n (%) COPD or recent pneumonia, n (%) End stage renal failure, n (%) |
107 (41.0%) 47 (18.0%) 54 (20.7%) 21 (8.0%) 7 (2.7%) |
80 (37.2%) 30 (14.0%) 32 (14.9%) 14 (6.5%) 2 (0.9%) |
27 (58.7%) 17 (37.0%) 22 (47.8%) 7 (15.2%) 5 (10.7%) |
0.007 <0.001 <0.001 0.049 <0.001 |
| mFI scale: Low risk, n (%) Intermediate risk, n (%) High risk, n (%) Unable to assess, n (%) |
114 (43.7%) 61 (23.4%) 80 (30.7%) 6 (2.3%) |
107 (49.8%) 54 (25.15%) 51 (23.7%) 3 (1.4%) |
7 (15.2%) 7 (15.2%) 29 (63.0%) 3 (6.5%) |
<0.001 |
| BGA scale: Low risk, n (%) Intermediate risk, n (%) High risk, n (%) Unable to assess, n (%) |
214 (82.0%) 13 (5.0%) 10 (3.8%) 24 (9.2%) |
203 (94.4%) 7 (3.3%) 5 (2.3%) 0 (0%) |
11 (23.9%) 6 (13.0%) 5 (10.9%) 24 (52.2%) |
<0.001 |
| Type of surgery: Appendectomy, n (%) Cholecystectomy, n (%) Colon resection, n (%) Small bowel resection, n (%) Laparotomy without resection, n (%) Ulcer perforation surgery, n (%) Other, n (%) |
33 (12.64%) 15 (5.75%) 91 (34.87%) 40 (15.33%) 41 (15.7%) 25 (9.58%) 16 (6.13%) |
33 (15.34%) 15 (6.98%) 65 (30.23%) 32 (14.88%) 37 (17.21%) 20 (9.31%) 13 (6.05%) |
0 (0%) 0 (0%) 26 (56.52%) 8 (17.39%) 4 (8.7%) 5 (10.87%) 3 (6.52%) |
<0.001 |
IQR: interquartile range; ASA: physical status classification system; COPD: chronic obstructive pulmonary disease; mFI: modified frailty index; BGA: brief geriatric assessment
A total of 46 patients (17.6%) died within 30 days of surgical intervention and formed group 2. The remaining 215 patients survived and formed group 1. Patients in group 2 were significantly older (77 (63-83 IQR) vs. 63 (47-74 IQR), p < 0.001). Moreover, CD III-V complications were significantly more common in group 2 (22.8% vs. 100%, p < 0.001), and they were more often admitted to the ICU (17.2% vs. 71.1%, p < 0.001). Both mFI and BGA scales identified more high-risk patients in group 2 (p < 0.001). The most common operation in both groups was colon resection (30.23% in group 1 and 56.52% in group 2). Numerical values for perioperative outcomes in both groups are presented in Table 2.
Table 2.
Perioperative outcomes of study groups.
| Parameter | Total | Group 1 (30-Day Mortality—0) | Group 2 (30-Day Mortality—1) | p Value |
|---|---|---|---|---|
| Laparoscopy vs. laparotomy, n | 37 (14.2%) vs. 224 (85.8%) | 36 (16.7%) vs. 179 (83.3%) | 1 (2.2%) vs. 45 (97.8%) | 0.019 |
| Surgeon attending vs. surgery resident operating, n | 145 (55.6%) vs. 116 (44.4%) | 119 (55.3%) vs. 96 (44.7%) | 26 (56.5%) vs. 20 (43.5%) | 0.959 |
| Median surgery duration (IQR) (minutes) | 120 (85–165) | 120 (80–165) | 135 (90–228) | 0.057 |
| Intraoperative adverse events, n | 18 (6.9%) | 7 (3.3%) | 11 (23.9%) | <0.001 |
| Median length of hospital stay (IQR) (days) | 7 (4–11) | 7 (5–11) | 4.5 (1–10) | <0.001 |
| Number of patients with admission to ICU | 70 (26.8%) | 37 (17.2%) | 33 (71.1%) | <0.001 |
| Median ICU stay if occurred (IQR) (days) | 9 (0–21) | 10 (0–28) | 7 (2–14) | 0.568 |
| Major postoperative complication (Clavien–Dindo scale > 2) | 95 (36.4%) | 49 (22.8%) | 46 (100%) | <0.001 |
The area under the ROC (AUROC) for mortality was the largest for calcification plaques (AUC = 0.736, cut-off point = 0.019, p < 0.001). AUROC for osteopenia was 0.725, cut-off point = 100.85, p < 0.001. AUROC for the psoas muscle area (PMA) was 0.693, cut-off point = 5.768, p < 0.001. AUROC for kidney volume/height was 0.679, cut-off point = 72.158, p < 0.001. AUROC for sarcopenic obesity was 0.580, cut-off point = 3.836, p = 0.095 (Table 3).
Table 3.
ROC curves for 30-day mortality.
| Parameter/Medical Condition | AUROC | 95%CI AUROC | p Value |
|---|---|---|---|
| Calcification plaques | 0.736 | 0.659–0.813 | <0.001 |
| Osteopenia (ROI at L3) | 0.725 | 0.647–0.804 | <0.001 |
| Psoas muscle area/height | 0.693 | 0.610–0.777 | <0.001 |
| Kidney volume/height | 0.679 | 0.585–0.773 | <0.001 |
| Sarcopenic obesity | 0.580 | 0.486-0.673 | 0.095 |
ROC: receiver operating curves; AUROC: the area under the ROC; ROI: the region of interest
Patients in group 2 had lower median PMA than patients in group 1 (5.19 (4.06–7.39 IQR) vs. 7.16 (5.01–9.41), p < 0.001). They also had higher median sarcopenic obesity levels (2.50 (1.62–3.84 IQR) vs. 2.29 (1.23–3.10 IQR), p = 0.093). Patients in group 2 had a much higher median percent of atherosclerotic plaques in the aorta volume than patients in group 1 (3.69% (1.87–8.24 IQR) vs. 0.60% (0.0–2.91 IQR), p < 0.001). Mean kidney volume/height was higher in group 1 than in group 2 (89.1 vs. 66.7, p < 0.001) (Table 4).
Table 4.
Radiological frailty parameters in study groups.
| Parameter | Total | Group 1 (30-Day Mortality—0) | Group 2 (30-Day Mortality—1) | p Value |
|---|---|---|---|---|
| Median psoas muscle area/height (IQR) (cm2/m) | 7.16 (5.01–9.41) | 7.61 (5.38–9.70) | 5.19 (4.06–7.39) | <0.001 |
| Number of patients with psoas area/height under cut-off point | 94 (36.0%) | 65 (30.2%) | 29 (63.0%) | <0.001 |
| Median sarcopenic obesity (IQR) (cm2/cm2) | 2.30 (1.33–3.19) | 2.29 (1.23–3.10) | 2.50 (1.62–3.84) | 0.093 |
| Number of patients with sarcopenic obesity under cut-off point | 31 (11.9%) | 20 (9.3%) | 11 (24.4%) | 0.004 |
| Median osteopenia in ROI at L3 (IQR) (HU) | 138.1 (102.1–181.0) | 144.0 (109.6–193.8) | 100.6 (74.6–142.5) | <0.001 |
| Number of patients with osteopenia under cut-off point | 61 (23.4%) | 38 (17.7%) | 23 (50.0%) | <0.001 |
| Median percent of atherosclerotic plaques in aorta volume (IQR) (%) | 0.86 (0–3.81) | 0.60 (0–2.91) | 3.69 (1.87–8.24) | <0.001 |
| Number of patients with percent of calcification plaques in aorta volume under cut-off point | 100 (38.3%) | 66 (30.7%) | 34 (73.9%) | <0.001 |
| Mean kidney volume/height ± SD (cm3/m) | 85.7 (69.7–104.5) | 89.1 (73.6–105.7) | 66.7 (53.6–93.6) | <0.001 |
| Number of patients with kidney volume/height under cut-off point | 79 (30.27) | 49 (22.8%) | 30 (65.2%) | <0.001 |
HU: Hounsfield units.
Univariate logistic regression revealed the following risk factors for 30-day mortality: every 10 years of age (OR: 1.763, 95%CI: 1.369–2.270, p < 0.001), every next ASA class (OR: 6.529, 95%CI: 3.461–12.318, p < 0.001), intraoperative adverse events (OR: 9.294, 95%CI: 3.375–25.596, p < 0.001), every point of mFI-5 score (OR: 2.485, 95%CI: 1.839–3.357, p < 0.001), every point of BGA score (OR: 1.449, 95%CI: 1.219–1.721, p < 0.001), PMA (OR: 3.937, 95%CI: 2.023–7.660, p < 0.001), sarcopenic obesity (OR: 3.154, 95%CI: 1.388–7.169, p = 0.006), osteopenia (OR: 4.658, 95%CI: 2.369–9.157, p < 0.001), calcification volume rate in aorta (OR: 6.352, 95%CI: 3.116–13.129, p < 0.001) and kidney volume/height (OR: 6.352, 95%CI: 3.201–12.605, p < 0.001).
Multivariate logistic regression identified the following risk factors for 30-day mortality: every next ASA class (OR: 4.161, 95%CI: 1.672–10.355, p = 0.002), intraoperative adverse events (OR: 12.397, 95%CI: 2.166–70.969, p = 0.005) and osteopenia (OR: 4.213, 95%CI: 1.235–14.367, p = 0.022) (Table 5).
Table 5.
Risk factors for 30-day mortality.
| Parameter | OR | 95%CI | p Value |
|---|---|---|---|
| Univariate analysis: | |||
| Male sex | 0.955 | 0.505–1.805 | 0.886 |
| Every 10 years of age | 1.763 | 1.369–2.270 | <0.001 |
| Every next ASA class | 6.529 | 3.461–12.318 | <0.001 |
| Body mass index (every 1 kg/m2) | 1.060 | 0.993–1.130 | 0.079 |
| Laparotomy vs. laparoscopy (laparotomy-1) | 9.050 | 1.208–67.798 | 0.032 |
| Surgeon specialist vs. surgeon resident operating (surgeon resident-1) | 1.017 | 0.533–1.942 | 0.959 |
| Intraoperative adverse events | 9.294 | 3.375–25.596 | <0.001 |
| Every point of mFI-5 score | 2.485 | 1.839–3.357 | <0.001 |
| Every point of BGA score | 1.449 | 1.219–1.721 | <0.001 |
| Psoas muscle area/height under cut-off point | 3.937 | 2.023–7.660 | <0.001 |
| Sarcopenic obesity under cut-off point | 3.154 | 1.388–7.169 | 0.006 |
| Osteopenia under cut-off point | 4.658 | 2.369–9.157 | <0.001 |
| Calcification volume rate in aorta under cut-off point | 6.396 | 3.116–13.129 | <0.001 |
| Kidney volume/height under cut-off point | 6.352 | 3.201–12.605 | <0.001 |
| Multivariate analysis: | |||
| Every 10 years of age | 1.098 | 0.659–1.827 | 0.720 |
| Every next ASA class | 4.161 | 1.672–10.355 | 0.002 |
| Intraoperative adverse events | 12.397 | 2.166–70.969 | 0.005 |
| Every point of mFI-5 score | 1.447 | 0.864–2.424 | 0.160 |
| Every point of BGA score | 1.161 | 0.905–1.488 | 0.241 |
| Psoas muscle area/height under cut-off point | 2.485 | 0.781–7.906 | 0.123 |
| Sarcopenic obesity under cut-off point | 1.812 | 0.469–6.993 | 0.389 |
| Osteopenia under cut-off point | 4.213 | 1.235–14.367 | 0.022 |
| Atherosclerosis in aorta under cut-off point | 1.241 | 0.342–4.506 | 0.743 |
| Kidney volume/height under cut-off point | 1.012 | 0.296–3.464 | 0.984 |
AUROC for major complications was the largest for aortic calcifications (AUC = 0.688, cut-off point = 2.78, p < 0.001). AUROC for major complications for kidney volume/height was 0.629, cut-off point = 75.18, p = 0.001. AUROC for major complications for osteopenia was 0.621, cut-off point = 115.34, p = 0.001. AUROC for major complications for PMA was 0.617, cut-off point = 10.873, p = 0.002. AUROC for major complications for sarcopenic obesity was 0.559, cut-off point = 0.72, p = 0.120 (Table 6).
Table 6.
ROC curves for major complications.
| Parameter/Medical Condition | AUROC | 95%CI AUROC | p Value |
|---|---|---|---|
| Calcification plaques | 0.688 | 0.619–0.757 | <0.001 |
| Osteopenia | 0.621 | 0.551–0.691 | 0.001 |
| Psoas muscle area/height | 0.617 | 0.545–0.689 | 0.002 |
| Kidney volume/height | 0.629 | 0.553–0.704 | 0.001 |
| Sarcopenic obesity | 0.559 | 0.485–0.632 | 0.120 |
Univariate logistic regression revealed the following risk factors for major complications: every 10 years of age (OR: 1.466, 95%CI: 1.242–1.729, p < 0.001), every next ASA class (OR: 3.546, 95%Cl: 2.335–5.387, p < 0.001), laparotomy vs. laparoscopy (OR: 3.343, 95%CI: 1.340–8.342, p = 0.010), every point of mFI-5 score (OR: 2.107, 95%Cl: 1.644–2.699, p < 0.001), every point of BGA score (OR: 1.812, 95%Cl: 1.431–2.281, p < 0.001), PMA (OR: 2.408, 95%CI: 1.431–4.053, p = 0.001), sarcopenic obesity (OR: 2.843, 95%Cl: 1.323–6.109, p = 0.007), osteopenia (OR: 2.813, 95%Cl: 1.568–5.048, p = 0.001), calcification volume rate in aorta (OR: 3.805, 95%Cl: 2.222–6.517, p < 0.001) and kidney volume/height (OR: 4.594, 95%Cl: 2.627–8.033, p < 0.001).
Multivariate logistic regression identified the following risk factors for major complications: every next ASA class (OR: 1.952, 95%Cl: 1.171–3.256, p = 0.010) and every point of BGA score (OR: 1.496, 95%Cl: 1.110–2.016, p = 0.008) (Table 7).
Table 7.
Risk factors for major complications.
| Parameter | OR | 95%CI | p Value |
|---|---|---|---|
| Univariate analysis: | |||
| Male sex | 1.007 | 0.607–1.669 | 0.980 |
| Every 10 years of age | 1.466 | 1.242–1.729 | <0.001 |
| Every next ASA class | 3.546 | 2.335–5.387 | <0.001 |
| Body mass index (every 1 kg/m2) | 1.039 | 0.985–1.095 | 0.163 |
| Laparotomy vs. laparoscopy (laparotomy-1) | 3.343 | 1.340–8.342 | 0.010 |
| Surgeon specialist vs. surgeon resident operating (surgeon resident-1) | 0.827 | 0.496–1.378 | 0.466 |
| Intraoperative adverse events | 3.902 | 1.414–10.774 | 0.009 |
| Every point of the mFI-5 score | 2.107 | 1.644–2.699 | <0.001 |
| Every point of the BGA score | 1.812 | 1.439–2.281 | <0.001 |
| Psoas muscle area/height under cut-off point | 2.408 | 1.431–4.053 | 0.001 |
| Sarcopenic obesity under cut-off point | 2.843 | 1.323–6.109 | 0.007 |
| Osteopenia under cut-off point | 2.813 | 1.568–5.048 | 0.001 |
| Calcification volume rate in aorta under cut-off point | 3.805 | 2.222–6.517 | <0.001 |
| Kidney volume/height under cut-off point | 4.594 | 2.627–8.033 | <0.001 |
| Multivariate analysis: | |||
| Every 10 years of age | 0.997 | 0.741–1.342 | 0.987 |
| Every next ASA class | 1.952 | 1.171–3.256 | 0.010 |
| Every point of the mFI-5 score | 1.129 | 0.748–1.703 | 0.563 |
| Every point of the BGA score | 1.496 | 1.110–2.016 | 0.008 |
| Psoas muscle area/height under cut-off point | 1.341 | 0.561–3.207 | 0.509 |
| Sarcopenic obesity under cut-off point | 2.603 | 0.780–8.691 | 0.120 |
| Osteopenia under cut-off point | 1.262 | 0.473–3.371 | 0.642 |
| Atherosclerosis in aorta under cut-off point | 1.504 | 0.606–3.734 | 0.379 |
| Kidney volume/height under cut-off point | 1.963 | 0.843–4.572 | 0.118 |
4. Discussion
Our study revealed that osteopenia is the most useful radiological feature for 30-day mortality prediction in patients requiring emergency laparotomy. None of the evaluated imaging markers of frailty proved to be efficient in the prediction of major complication occurrence.
As the number of frail patients requiring surgical interventions increases, methods of its assessment emerge. The modified frailty index was identified as an independent risk factor of postoperative morbidity in patients undergoing common general surgery interventions [4]. Furthermore, as a study by Lee points out, frailty is not only a risk factor for perioperative complications, but also for a negative 1-year prognosis [17]. In our study, we also used mFI and BGA scales for frailty assessment; however, only BGA was useful for the stratification of risk for perioperative complications.
Traditional scoring systems require knowledge of multiple patient-dependent factors. It makes this approach very limited in emergency situations, and quick imaging analysis could help overcome this. Radiological features of frailty are recognized as a predictor of a negative outcome in cardiothoracic procedures [10,18]. Richards et al. drew the same conclusion regarding colorectal cancer surgery, where a CT scan is performed routinely as a part of preoperative staging [9]. Not every patient requiring emergency surgery has a CT scan performed preoperatively. Having said that, patients without CT scans are usually undergoing less complex procedures and are not that susceptible to frailty.
Among the radiological markers of frailty, the most recognizable is the area of psoas major muscle, used to assess sarcopenia. Shinohara et al. noticed a relation between sarcopenia and poor prognosis in patients treated for non-small cell lung carcinoma [11]. In addition, Okamura pointed out its importance in the outcomes of aortic valve replacement [10]. Yamashita et al. identified sarcopenic obesity as a risk factor for poor muscle function, and therefore poor prognosis after cardiovascular surgery [19]. However, most studies concentrate on elective cases [9,10,18]. Gomibuchi used it as a part of the assessment of patients with type A aortic dissection, pointing out the importance of frailty in this procedure [20]. Simpson et al. compared PMA to the P-POSSUM scale in patients over 80 years old undergoing emergency laparotomy and found PMA as a worthy indicator of postoperative mortality [12].
In our study, we tried to find this correlation in emergency cases, broadening the patients’ spectrum to a whole population; however, as was the case for Mccusker et al., who did not find this relation in geriatric trauma patients, we were also unable to indicate it [21]. Anastácio et al. point out that volumetric measurements, in addition to the composition of the body, might represent the signs of frailty that underline the meaning of sarcopenic obesity [13]. Data regarding the impact of sarcopenic obesity on abdominal surgery are limited and mostly focused on pancreatic and gastric cancer [22,23,24,25]. On the other hand, Kaplan et al. indicated that both osteopenia and sarcopenia were independently associated with increased 1-year mortality in 65-year-old and older patients admitted to ICU after traumatic injury [15].
Aortic calcifications and kidney volume were not identified as risk factors either for 30-day mortality or for morbidity. However, only a few papers assessed these factors. There is strong evidence that they might be useful for frailty assessments.
Our study has some limitations. Firstly, our analysis is retrospective and requires investigation in a larger, prospective scenario. Moreover, due to the nature of the study, we included only patients with available CT scans obtained preoperatively. This caused the exclusion of patients with a better overall condition and milder diseases, such as appendicitis. As no CT is required in these cases, one might suspect that patients in that group would be less prone to frailty. Furthermore, a CT scan is time-consuming, which limits the utilization of radiological frailty assessment in unstable, trauma patients. Finally, although our approach overcomes the problem of lacking patient’s medical information, this method is time-consuming and requires a radiologist or a skilled evaluator to perform measurements. This, however, will be automatized in the future with advances in medical image processing.
5. Conclusions
Osteopenia was the best parameter for perioperative mortality risk stratification in patients undergoing emergency surgical intervention. Sarcopenia (measured as psoas muscle area), sarcopenic obesity, aortic calcifications and mean kidney volume do not predict poor outcomes in those patients. None of the radiological markers appeared to be useful in the prediction of perioperative morbidity.
Author Contributions
Conceptualization, M.R., K.K. and A.G.; Data curation, K.K., J.W., P.T., N.P. and M.L.; Formal analysis, K.K., J.W., P.T. and M.P.; Investigation, M.R. and P.T.; Methodology, M.R., K.K. and J.W.; Supervision, M.R.; Validation, A.G.; Writing—original draft, M.R. and K.K.; Writing—review and editing, M.R., K.K. and M.P. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was approved by the local research ethics committee, following the guidelines of the Declaration of Helsinki of 1975 with its later amendments. The study obtained approval from the Ethics Committee of the Jagiellonian University no. 1072.6120.14.2020.
Informed Consent Statement
Every patient has given informed consent to be included in the study.
Data Availability Statement
The data used for this study are available on demand after contact with the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Saripella A., Wasef S., Nagappa M., Riazi S., Englesakis M., Wong J., Chung F. Effects of comprehensive geriatric care models on postoperative outcomes in geriatric surgical patients: A systematic review and meta-analysis. BMC Anesthesiol. 2021;21:127. doi: 10.1186/s12871-021-01337-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Merani S., Payne J., Padwal R.S., Hudson D., Widder S.L., Khadaroo R.G. Predictors of in-hospital mortality and complications in very elderly patients undergoing emergency surgery. World J. Emerg. Surg. 2014;9:43. doi: 10.1186/1749-7922-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moore T., Tubman I., Levy G., Brooke G. Age as a Risk Factor for Perioperative Complications in Women Undergoing Pelvic Reconstructive Surgery. Female Pelvic Med. Reconstr. Surg. 2010;16:290–295. doi: 10.1097/SPV.0b013e3181e128b6. [DOI] [PubMed] [Google Scholar]
- 4.Seib C.D., Rochefort H., Chomsky-Higgins K., Gosnell J.E., Suh I., Shen W.T., Duh Q.-Y., Finlayson E. Association of Patient Frailty With Increased Morbidity After Common Ambulatory General Surgery Operations. JAMA Surg. 2018;153:160–168. doi: 10.1001/jamasurg.2017.4007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy P.B., Savage S.A., Zarzaur B.L. Impact of Patient Frailty on Morbidity and Mortality after Common Emergency General Surgery Operations. J. Surg. Res. 2019;247:95–102. doi: 10.1016/j.jss.2019.10.038. [DOI] [PubMed] [Google Scholar]
- 6.Tan H.L., Chia S.T.X., Nadkarni N.V., Ang S.Y., Seow D.C.C., Wong T.H. Frailty and functional decline after emergency abdominal surgery in the elderly: A prospective cohort study. World J. Emerg. Surg. 2019;14:62. doi: 10.1186/s13017-019-0280-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Curtis E., Romanowski K., Sen S., Hill A., Cocanour C. Frailty score on admission predicts mortality and discharge disposition in elderly trauma patients over the age of 65 y. J. Surg. Res. 2018;230:13–19. doi: 10.1016/j.jss.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 8.Lauerman M.H., Raithel M., Kufera J., Shanmuganathan K., Bruns B.R., Scalea T.M., Stein D.M. Comparison of individual and composite radiographic markers of frailty in trauma. Injury. 2019;50:149–155. doi: 10.1016/j.injury.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 9.Richards S.J., Senadeera S.C., Frizelle F.A. Sarcopenia, as Assessed by Psoas Cross-Sectional Area, Is Predictive of Adverse Postoperative Outcomes in Patients Undergoing Colorectal Cancer Surgery. Dis. Colon Rectum. 2020;63:807–815. doi: 10.1097/DCR.0000000000001633. [DOI] [PubMed] [Google Scholar]
- 10.Okamura H., Kimura N., Tanno K., Mieno M., Matsumoto H., Yamaguchi A., Adachi H. The impact of preoperative sarcopenia, defined based on psoas muscle area, on long-term outcomes of heart valve surgery. J. Thorac. Cardiovasc. Surg. 2019;157:1071–1079.e3. doi: 10.1016/j.jtcvs.2018.06.098. [DOI] [PubMed] [Google Scholar]
- 11.Shinohara S., Otsuki R., Kobayashi K., Sugaya M., Matsuo M., Nakagawa M. Impact of Sarcopenia on Surgical Outcomes in Non-small Cell Lung Cancer. Ann. Surg. Oncol. 2020;27:2427–2435. doi: 10.1245/s10434-020-08224-z. [DOI] [PubMed] [Google Scholar]
- 12.Simpson G., Parker A., Hopley P., Wilson J., Magee C. Pre-operative psoas major measurement compared to P-POSSUM as a prognostic indicator in over-80s undergoing emergency laparotomy. Eur. J. Trauma Emerg. Surg. 2020;46:215–220. doi: 10.1007/s00068-018-1025-5. [DOI] [PubMed] [Google Scholar]
- 13.Anastácio L.R., Ferreira L.G., Ribeiro H.S., Diniz K.G.D., Lima A.S., Correia M.I.T., Vilela E.G. Sarcopenia, obesity and sarcopenic obesity in liver transplantation: A body composition prospective study. Arq. Bras. De Cir. Dig. 2019;32:e1434. doi: 10.1590/0102-672020190001e1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clavien P.A., Barkun J., de Oliveira M.L., Vauthey J.N., Dindo D., Schulick R.D., de Santibañes E., Pekolj J., Slankamenac K., Bassi C., et al. The Clavien-Dindo Classification of Surgical Complications: Five-year experience. Ann. Surg. 2009;250:187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 15.Kaplan S., Pham T.N., Arbabi S., Gross J.A., Damodarasamy M., Bentov I., Taitsman L.A., Mitchell S.H., Reed M.J. Association of Radiologic Indicators of Frailty With 1-Year Mortality in Older Trauma Patients. JAMA Surg. 2017;152:e164604. doi: 10.1001/jamasurg.2016.4604. [DOI] [PubMed] [Google Scholar]
- 16.Pędziwiatr M., Pisarska M., Major P., Grochowska A., Matłok M., Przęczek K., Stefura T., Budzyński A., Kłęk S. Laparoscopic colorectal cancer surgery combined with enhanced recovery after surgery protocol (ERAS) reduces the negative impact of sarcopenia on short-term outcomes. Eur. J. Surg. Oncol. 2016;42:779–787. doi: 10.1016/j.ejso.2016.03.037. [DOI] [PubMed] [Google Scholar]
- 17.Lee K.C., Bs J.S., Sturgeon D., Lipsitz S., Weissman J.S., Rosenthal R.A., Kim D.H., Mitchell S.L., Cooper Z. The Impact of Frailty on Long-Term Patient-Oriented Outcomes after Emergency General Surgery: A Retrospective Cohort Study. J. Am. Geriatr. Soc. 2020;68:1037–1043. doi: 10.1111/jgs.16334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Mourik M.S., Janmaat Y.C., Van Kesteren F., Vendrik J., Planken R.N., Henstra M.J., Velu J.F., Vlastra W., Zwinderman A.H., Koch K.T., et al. CT determined psoas muscle area predicts mortality in women undergoing transcatheter aortic valve implantation. Catheter. Cardiovasc. Interv. 2019;93:E248–E254. doi: 10.1002/ccd.27823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yamashita M., Kamiya K., Matsunaga A., Kitamura T., Hamazaki N., Matsuzawa R., Nozaki K., Tanaka S., Nakamura T., Maekawa E., et al. Prognostic value of sarcopenic obesity estimated by computed tomography in patients with cardiovascular disease and undergoing surgery. J. Cardiol. 2019;74:273–278. doi: 10.1016/j.jjcc.2019.02.010. [DOI] [PubMed] [Google Scholar]
- 20.Gomibuchi T., Seto T., Komatsu M., Tanaka H., Ichimura H., Yamamoto T., Ohashi N., Wada Y., Okada K. Impact of Frailty on Outcomes in Acute Type A Aortic Dissection. Ann. Thorac. Surg. 2018;106:1349–1355. doi: 10.1016/j.athoracsur.2018.06.055. [DOI] [PubMed] [Google Scholar]
- 21.Mccusker A., Khan M., Kulvatunyou N., Zeeshan M., Sakran J.V., Hayek H., O’Keeffe T., Hamidi M., Tang A., Joseph B. Sarcopenia defined by a computed tomography estimate of the psoas muscle area does not predict frailty in geriatric trauma patients. Am. J. Surg. 2019;218:261–265. doi: 10.1016/j.amjsurg.2018.07.024. [DOI] [PubMed] [Google Scholar]
- 22.Mintziras I., Miligkos M., Wächter S., Manoharan J., Maurer E., Bartsch D.K. Sarcopenia and sarcopenic obesity are significantly associated with poorer overall survival in patients with pancreatic cancer: Systematic review and meta-analysis. Int. J. Surg. 2018;59:19–26. doi: 10.1016/j.ijsu.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 23.Pecorelli N., Capretti G., Sandini M., Damascelli A., Cristel G., DE Cobelli F., Gianotti L., Zerbi A., Braga M. Impact of Sarcopenic Obesity on Failure to Rescue from Major Complications Following Pancreaticoduodenectomy for Cancer: Results from a Multicenter Study. Ann. Surg. Oncol. 2018;25:308–317. doi: 10.1245/s10434-017-6216-5. [DOI] [PubMed] [Google Scholar]
- 24.Ratnayake C.B.B., Wells C., Olsson M., Windsor J.A., Pandanaboyana S. Sarcopenic obesity and post-operative morbidity after pancreatic surgery: A cohort study. ANZ J. Surg. 2019;89:1587–1592. doi: 10.1111/ans.15431. [DOI] [PubMed] [Google Scholar]
- 25.Zhang W.-T., Lin J., Chen W.-S., Huang Y.-S., Wu R.-S., Chen X.-D., Lou N., Chi C.-H., Hu C.-Y., Shen X. Sarcopenic Obesity Is Associated with Severe Postoperative Complications in Gastric Cancer Patients Undergoing Gastrectomy: A Prospective Study. J. Gastrointest. Surg. 2018;22:1861–1869. doi: 10.1007/s11605-018-3835-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used for this study are available on demand after contact with the corresponding author.