Abstract
The prevalence of mental health disorders has increased during the COVID-19 pandemic. Patients with chronic diseases, such as diabetes, are a particularly vulnerable risk group. This study aims to assess the levels and prevalence of anxiety, distress, and stress in patients with diabetes during the COVID-19 pandemic. A systematic review was conducted in CINAHL, Cochrane, LILACS, Medline, SciELO, and Scopus in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. Thirty-seven articles with a total of 13,932 diabetic patients were included. Five meta-analyses were performed. The prevalence of anxiety was 23% (95% CI = 19–28) in T1DM and 20% (95% CI = 6–40) in T2DM patients. For diabetes distress it was 41% (95% CI = 24–60) for T1DM and 36% in T2DM patients (95% CI = 2–84). For stress, the prevalence was 79% (95% CI = 49–98) in T1DM patients. People with diabetes have significant psychiatric comorbidity as well as psychological factors that negatively affect disease management, increasing their vulnerability in an emergency situation. To establish comprehensive care in diabetic patients addressing mental health is essential, as well as including specific policy interventions to reduce the potential psychological harm of the COVID-19 pandemic.
Keywords: anxiety, COVID-19, diabetes, distress, meta-analysis, stress
1. Introduction
The coronavirus infection (COVID-19) has become a global health problem since the beginning of 2020 [1]. The lockdown as well as the restrictions in the different waves of contagion have caused a negative impact on the health of the general population and especially on people who suffer from chronic diseases such as people with diabetes [2]. People with diabetes mellitus (DM) are a risk group, with high hospitalization and mortality rate, and this risk increases when there is COVID-19 infection [3].
The prevalence of mental health disturbances has increased at an alarming rate during the COVID-19 pandemic [4]. Patients with DM present multiple psychosocial factors, which together with the psychological stressors of a pandemic, such as quarantine, social distance, and fear of contagion, make this group even more vulnerable [5]. Mental disorders in DM patients reach figures of up to 50%, which predisposes to an increase in mental health disorders in the face of a pandemic situation that leads to difficulties in adapting psychologically [6]. Some reports show that up to 87% of DM type 2 patients indicate being “psychologically affected” [7].
Among the possible issues in psychological health, we can find a greater susceptibility to severe symptoms of depression and a feeling of loneliness, anxiety, stress, or diabetes stress, referring to negative emotions related to the disease such as feeling frustrated, desperate, or angry [8,9,10]. These comorbidities in DM patients can reduce self-care, adherence to treatment and engagement with health professionals, with a negative impact on disease management [11,12]. Several studies indicate that up to 50% of DM patients were afraid of possible contagion [7]. This situation, together with medical distrust, and frustration due to the difficulties in DM management, is related to a reduction in control visits and even more in the demand for assistance in non-emergencies problems, especially those related to mental health [13,14].
The lockdown and successive waves of restrictions have disrupted healthy lifestyle patterns and the ability to self-care [14]. Some studies report that up to 54% of chronic patients claim to have problems related to their usual treatment [15], and data from a survey conducted in 155 countries by the World Health Organization showed that diabetes treatment was partially or completely interrupted in 49% of the countries surveyed [16]. Unhealthy behaviours in DM patients with higher consumption of sugary drinks as well as a reduction in physical activity have also been reported [7]. Other studies report a reduction in self-monitoring of blood glucose; only 28% of patients regularly monitored glucose levels during the COVID-19 lockdown [17]. Given these data, some authors show a clear relationship between self-care deficit and an increase in the number of mental disorders [18].
Although there are several studies that analyse mental health in the general population, data about chronic disease patients and more specifically in patients with DM are still limited. There are studies focused on the treatment of diabetes and associated complications during the COVID-19 pandemic [5,19,20]; however, no systematic review and meta-analysis address psychological disturbances.
An analysis of levels of these variables, looking at the definition by the Medical Subject Headings, anxiety (“feelings or emotions of dread, apprehension and impending disaster”), distress (“negative emotional state with emotional and/or physical discomfort”), and stress (with emotional factors predominating) in the population with DM is necessary, since the number of DM patients affected by these problems before the COVID-19 pandemic was important [21] and these levels may have increased. This review analyses the data currently available in the pandemic scenario, in order to establish intervention strategies and address a psychosocial approach in people with DM during COVID-19. Therefore, the objective of this systematic review and meta-analysis was to analyse the levels and prevalence of anxiety, distress, and stress during the COVID-19 pandemic in diabetic patients.
2. Methods
2.1. Design
The review and meta-analysis were reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [22] (see Supplementary Materials Table S1 for further information). The protocol was registered in PROSPERO (International Prospective Register of Systematic Reviews) with the registration number CRD42022325197.
2.2. Search Strategy
A search was performed in the following databases: the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO), the Cochrane Central Register of Controlled Trials (CENTRAL), LILACS (BIREME), Medline (Ovid), SciELO (BIREME), and Scopus (Elsevier). The search was done in July 2022 without restriction by language or publication date. The search terms used were: “(anxiety OR psychological distress OR stress) AND (diabetes OR chronic illness OR chronically ill OR non-communicable diseases) AND (SARS-CoV-2 OR coronavirus OR COVID-19)”.
2.3. Eligibility Criteria
Studies conducted during the COVID-19 pandemic were included with the following inclusion criteria: (1) original studies, (2) type 1 diabetes mellitus (T1DM) or type 2 diabetes mellitus (T2DM), (3) assessing anxiety, distress, or stress symptoms (percentages, means, or median levels), (4) use of anxiety, distress, and stress validated measurement tool. There was no restriction by language or publication date.
Studies were excluded if they were: (1) letters to editors, conference paper review articles, and case reports, (2) articles with other types of diabetes (gestational, MODY, LADA), (3) articles including different chronic pathologies without indicating a number of participants with diabetes, (4) sample of patients with serious cognitive/neurological impairment or mental/physical disability.
2.4. Study Selection and Data Collection
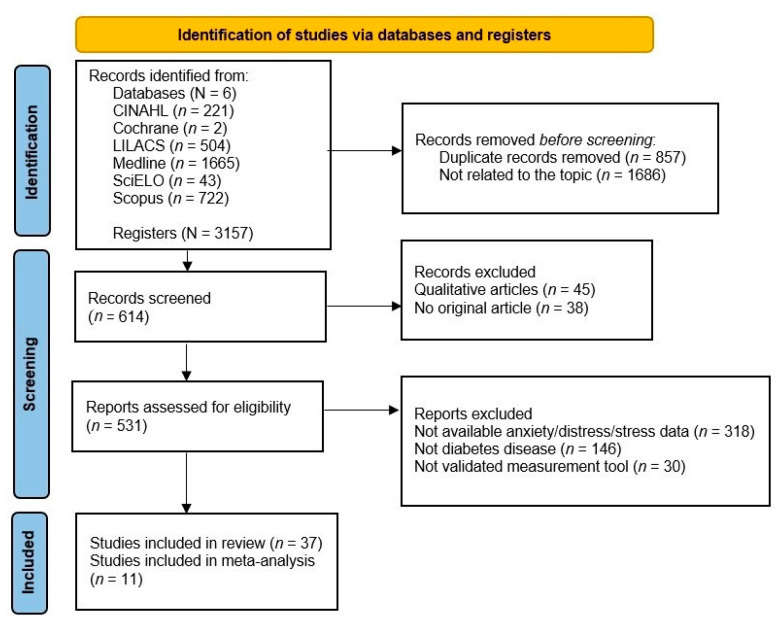
First, two independent reviewers analysed titles and abstracts and then the full texts according to the inclusion criteria (Figure 1). A third author was consulted in case of disagreement.
Figure 1.
Flow diagram of the selection process.
Two authors extracted data from selected studies into an Excel spreadsheet, consulting with a third author in case of discrepancies. The following information was extracted from each study: (1) author, year of publication, country, (2) study design and period, (3) sample, (4) setting, (5) measuring instrument, (6) type of diabetes, (7) levels of anxiety, distress, or stress (percentage, mean, median) (Table 1).
Table 1.
Characteristics of the included studies (n = 37).
| Author, Year, Country | Study /Period |
Sample | Setting | Scale | Type of Diabetes | Anxiety/Distress/Stress M(SD)/M (IQR) |
EL/RG |
|---|---|---|---|---|---|---|---|
| Abdelghani et al., [26], 2021, Egypt | Cross-sectional June–September 2020 |
N = 200 Mean age 48.4 (13.7) Female 63 % Mean duration of DM 6.2 (5.3) years |
Endocrinology outpatient clinic | HADS-Anxiety | T1DM T2DM |
Anxiety 8.8 (4.4) |
2b/B |
| Abdoli et al. [27], 2021, US, Brazil, and Iran | Cross-sectional April–June 2020 |
N = 1788 US (n = 1099) Brazil (n = 477) Iran (n = 212) Age >18 years Female 78.28% |
Online survey | DDS | T1DM |
Distress No/little/moderate US 86.6% Brazil 69.2% Iran 42.9% High US 13.40% Brazil 30.8% Iran 57.1% |
2b/B |
| Agarwal et al. [28], 2020, India | Cross-sectional April–May 2020 |
N = 89 Mean age 19.61 (3.8) Female 48.3% Mean duration of DM 8.4 (5) years |
Online survey | PSS | T1DM |
Stress Low 42.7% Moderate 51.7% Severe 5.6% |
2b/B |
| Ajele et al., [29], 2022, Nigeria | Cross-sectional April–July 2021 |
N = 223 Mean age 53.26 (11.05) Female 26% |
Outpatient clinic | PAID-DDS | T1DM T2DM |
Distress 60.61 (29.51) |
2b/B |
| Alkhormi et al., [30], 2022, Saudi Arabia | Cross-sectional August–-February 2022 |
N = 375 Female 51.7% |
Diabetic center + primary healthcare centers | GAD-7 | T2DM |
Anxiety Normal 52.8% Moderate-Severe 47.2% |
2b/B |
| Alshareef et al. [31], 2020, Saudi Arabia | Cross-sectional May 2020 |
N = 394 Female 42.9% |
Phone survey | K10 | T2DM |
Distress 9.78 (4.14) |
2b/B |
| Alzubaidi et al. [32], 2022, United Arab Emirates | Cross-sectional February–July 2021 |
N = 206 Female 42.2% Mean age 58.7 (11.2) Mean duration of DM 15.7 (8) years |
Phone survey | DDS | T2DM |
Distress Low 85.9% Moderate 10.7% High 3.4% |
2b/B |
| Bao [33], 2021, China | Cross-sectional January 2019–December 2020 |
N = 256 Range age 25-78 years Female 57.4% |
Department of Endocrinology | PAID-DDS | T2DM |
Distress 32.16 (12.13) Moderate 37.89% Severe 20.31% |
2b/B |
| Barchetta et al. [34], 2020, Italy | Observational retrospective study March–April 2020 |
N = 50 Mean age of 40.7 (13.5) Female 38% |
Diabetes outpatient clinics | PSS | T1DM |
Stress Low 26% Moderate 60% Severe 14% |
2b/B |
| Büyükbayram et al. [35], 2022, Turkey | Cross-sectional January–July 2021 |
N = 184 Mean age of 51.77 (15.07) Female 52.2% |
Internal medicine clinic | PSS | T2DM |
Stress 23.82 (8.34) |
2b/B |
| Caruso et al. [36], 2021, Italy | Cross-sectional study February–March 2020 |
N = 48 Mean age 42.4 (15.9) Female 47.9% |
Endocrinology unit | GHQ-12 | T1DM |
Anxiety 4.5 Mild 50% |
2b/B |
| Chao et al. [37], 2021, US | Observational prospective study July–December 2020 |
N = 2829 Mean age 75.6 (6) Female 63.2% |
Health center | GAD-7 | T2DM |
Anxiety 2.4 (3.5) Moderate/Severe 5% |
2b/B |
| Cusinato et al. [38], 2021, Italy | Observational retrospective study March–April 2020 |
N = 117 Mean age 15.9 (2.3) Female 44% Mean duration of DM 7.9 (4.6) years |
Pediatric Diabetes Unit | TAD-Anxiety | T1DM |
Anxiety 7% |
2b/B |
| Cyranka et al., [39], 2021, Poland | Cross-sectional March–May 2020 |
N = 49 Mean age 29.8 (8.9) Female 75.5% Mean duration of DM 16.2 (7.3) years |
Outpatient clinic | STAI PSS |
T1DM |
Anxiety STAI 39.7 (11) Stress PSS 21 (4.1) |
2b/B |
| Di Dalmazi et al. [40], Italy | Observational retrospective study February–March 2020 | N = 76 Mean age 45 years Female 48.7% Mean duration of DM 22 years |
Endocrinology and diabetes unit | PSS | T1DM |
Stress 14.5 (9.8–20) |
2b/B |
| Di Riso et al. [41], 2021, Italy | Cross-sectional May–June 2020 |
N = 71 Mean age 11 (2.26) year Female 46.6% |
Pediatric Diabetes Unit | SCAS-Anxiety | T1DM |
Anxiety 16.7% |
2b/B |
| Elhenawy & Eltonbary, [42], 2021, Egypt | Cross-sectional March 2020 |
N = 115 Female 53.9% |
Online survey | PSS | T1DM |
Stress Low 0% Moderate 66.6% Severe 33.4% |
2b/B |
| Hosomi et al. [43], 2022, Japan | Observational retrospective study April–May 2020 |
N = 34 Mean age 59.1 (16) Female 67.6% Diabetes duration 14.5 (16) |
Department of Endocrinology | VAS-Stress | T1DM |
Stress 6.7 (2.1) |
2b/B |
| Huang et al. [44], 2022, China | Cross-sectional study July–September 2020 |
N = 286 | Clinics | VAS- Anxiety | T2DM |
Anxiety 5.3 (2.8) |
2b/B |
| Kim et al. [45], 2022, US | Cross-sectional June–December 2020 |
N = 84 Mean age 68.46 (5.41) Female 54.76% Mean duration of DM 13.89 (7.53) years |
Online survey | DDS | T2DM |
Distress 1.35 (1.55) 0.63% |
2b/B |
| Khari et al. [46], 2021, Iran | Cross-sectional September–December 2020 |
N = 427 Female 66% |
Online survey | PSS | T1DM T2DM |
Stress 31.69 (5.88) |
2b/B |
| Madsen et al., [47], 2021, Denmark | Observational prospective study March 2020 |
N = 1366 Mean age 61.7 (12.8) Female 44.5% |
Online survey | DDS SCL-ANX4 |
T1DM T2DM |
Distress DDS 1.8 (1.00) Low 75.4% Moderate-High 24.6% Anxiety SCL-ANX4 0.5 (0.66) <10% risk of anxiety 80.5% 20% risk of anxiety 14.6% 30% risk of anxiety 3.6% 40% risk of anxiety 1.1% 45% risk of anxiety 0.2% |
2b/B |
| Magliah et al. [48], 2021, Saudi Arabia | Cross-sectional June 2020 |
N = 65 Mean age 30 (7.88) Female 70.8% Mean duration of DM 17.67 (6.89) years |
Online survey | GAD-7 | T1DM |
Anxiety None/minimal 56.9% Mild 24.6% Moderate 10.8% Severe 7.7% |
2b/B |
| Munekawa et al. [49], 2021, Japan | Cross-sectional April–May 2020 |
N = 203 Mean age 67.4 (11.3) Female 37.9% Mean duration of DM 14.4 (10.1) year |
Department of Endocrinology a | VAS-Stress | T2DM |
Stress 6.0 (1.7) |
2b/B |
| Miller et al. [50], 2022, US | Observational prospective study March 2020 |
N = 41 Range age 10.3–19.1 years |
Online survey | GAD-7 PSS |
T1DM |
Anxiety GAD-7 4.43 (4.63) Stress PSS 2.51 (0.71) |
2b/B |
| Musche et al., [51], 2021, Germany | Cross-sectional April–June 2020 |
N = 240 Age > 18 years Female 74.3% |
Online survey | GAD-7 | T1DM T2DM |
Anxiety T1DM (n = 169) None/minimal 46.2% Mild 30.8% Moderate 17.2% Severe 5.9% T2DM (n = 74) None/minimal 45.9% Mild 27% Moderate 14.9% Severe 9% |
2b/B |
| Myers et al., [52], 2021, US | Observational prospective study May–June 2020 |
N = 404 Mean age 51.46 years Mean duration of DM 40.21 (17.70) years |
Online survey | GAD-7 DDS PSS |
T1DM T2DM |
Anxiety GAD-7 T1DM (n = 100) 6.81 (4.96) Low-Mild 74% Moderate-Severe 26% T2DM (n = 304) 5.68 (5.50) Low-Mild 75.99% Moderate-Severe 24.01% Distress DDS T1DM (n = 95) 2.61 (0.85) Low 30.53% Moderate 35.79% High 33.68% T2DM (n = 293) 2.43 (0.95) Low 37.88% Moderate 32.08% High 30.03% Stress PSS T1DM (n = 100) 17.59 (6.99) Low 32% Moderate 59% High 9% T2DM (n = 304) 15.82 (8.33) Low 43.09% Moderate 46.05% High 10.86% |
2b/B |
| Olickal et al. [53], 2020, India | Cross-sectional July–August 2020 |
N = 350 Female 22% |
Phone survey | K10 | T2DM |
Distress Low 67.4% Moderate 30% High 2.6% |
2b/B |
| Naous et al. [54], 2022, Lebanon | Cross-sectional January–June 2021 |
N = 461 Median age 59 years Female 47.4% Median duration of DM 10 years |
Hospitals and private clinics | K10 | T2DM |
Distress 26 (18-35) Well 27.4% Mild 19.1% Moderate 15.1% Severe 38.4% |
2b/B |
| Nassar & Salameh, [55], 2021, Lebanon | Case-control study April–May 2020 |
N = 72 Mean age 65.5 (10.5) Female 48.6% |
Phone survey | BDS22-Anxiety | T2DM |
Anxiety 0.5 (1.1) |
2b/B |
| Regeer et al. [56], 2021, Netherlands | Cross-sectional May 2020 |
N = 536 Mean age 65.9 (7.9) Female 46% Mean duration of DM 13.3 (8) years |
Online survey | PSS VAS-Anxiety |
T2DM |
Stress PSS 12.98 (6.61) Anxiety VAS 4.2 (2.5) |
2b/B |
| Ruissen et al. [57], 2021, Netherlands | Observational prospective study March–June 2020 |
N = 435 Female 42% |
Online survey | PSS | T1DM T2DM |
Stress 13.25 (6.45) Elevated 34.1% |
2b/B |
| Sacre et al. [58], 2021, Australia | Observational prospective study April–May 2020 |
N = 450 Mean age 66 (9) Female 31% Mean duration of DM 12 years |
Phone/Online survey | GAD-7 PAID-DDS |
T2DM |
Anxiety GAD-7 2 (1.7–2.3) Mild 16.4% Moderate-Severe 8.4% Distress PAID 9 (8–10) Severe 7.8% |
2b/B |
| Shin et al. [59], 2021, Korea | Cross-sectional April–July 2020 |
N = 246 Mean age 73.8 (5.7) Female 59.3% Mean duration of DM 17.7 (8.8) years |
Outpatient clinic | IES-R-Stress | T2DM |
Stress 6.4 (6.6) Minimal 97.2% Mild 1.2% Moderate 1.2% Severe 0.4% |
2b/B |
| Silveira et al. [60], 2021, Brazil | Cross-sectional May–July 2020 |
N = 436 North, Northeast, Central-West (n =118) Southeast (n = 273) South (n = 45) Mean age 30.52 (9.22) Female 83% Mean duration of DM 15.29 (9.79) years |
Online survey | DDS | T1DM |
Distress Brazilian regions North, Northeast, Central-West 2.72 (0.99) No/Little 64.6% Moderate/High 35.4% Southeast 2.38 (1) No/Little 70.8% Moderate/High 29.2% South 2.76 (1.13) No/Little 68.8% Moderate/High 31.2% |
2b/B |
| Sisman et al. [61], 2021, Turkey | Cross-sectional | N = 304 Mean age 42.1 (15.5) Female 56% Mean duration of DM 10.3 (8.5) years |
Online survey | HADS-Anxiety | T1DM T2DM |
Anxiety T1DM 7.1 (3.6) 44.7% T2DM 7.5 (4.3) 46.6% |
2b/B |
| Utli & Vural Doğru [62], 2021, Turkey | Cross-sectional December 2020–April 2021 |
N = 378 Mean age 52.37 (11.37) Female 37.3% |
Endocrinology clinic + outpatients’ department | VAS-Anxiety VAS-Stress |
T2DM |
Anxiety VAS-Anxiety 7.32 (1.56) Stress VAS-Stress 7.06 (1.62) |
2b/B |
2b = evidence level from the OCEBM, B = recommendation grade from the OCEBM, BDS22 = Beirut Distress Scale, DDS = Diabetes Distress Scale, DM = Diabetes Mellitus, EL = Evidence level, GAD-7 = General Anxiety Disorder-7, GHQ-12 = General Health Questionnaire-12 items, HADS = Hospital Anxiety and Depression Scale, IES-R = Impact of Event Scale Revised, IQR = Interquartile range, K10 = Kessler Psychological Distress Scale, PAID = Problem Areas in Diabetes-Distress item, PSS = Perceived Stress Scale, RG = Recommendation grade, T1DM = Type 1 diabetes, T2DM = Type 2 diabetes, TAD = Test of Depression and Anxiety Scale, SCAS = Spence Children Anxiety Scale, SCL-ANX4 = Symptom Check List-revised anxiety subscale, SD = Standard deviation, STAI = State-Trait Anxiety Inventory, VAS = Visual Analog Scale.
2.5. Quality Assessment, Evidence Level and Grade of Recommendation
A quality assessment and bias analysis were carried out by two reviewers independently with a third reviewer consulted in case of disagreement.
The National Heart, Lung and Blood Institute quality assessment scale was used for bias assessment of observational studies [23] (Appendix A). The recommendations of the OCEBM were also used (Oxford Centre for Evidence-Based Medicine) to analyse the levels of evidence and grades of recommendation [24] (Table 1).
2.6. Data Analyses
A descriptive analysis was performed for the systematic review, extracting the variables in a data table.
For the meta-analysis, all the studies that presented data on the percentage of anxiety, diabetes distress, or stress measured through the same tool were used. Heterogeneity was assessed using the I2 index. Random effects meta-analysis were performed [25]. Sensitivity analysis and Egger’s regression test were used to assess bias in the studies.
Five meta-analyses were performed to estimate the prevalence of anxiety, diabetes distress or stress, and the corresponding confidence interval. StatsDirect software (StatsDirect Ltd., Cambridge, UK) was used for all statistical calculations.
3. Results
3.1. Characteristics of the Studies Included
The initial search found 3157 results. After deleting duplicates and reading the title and abstract, a total of 614 articles were selected. Finally, after reading the full text and analysing the inclusion criteria, 37 articles were included. The study search and selection process are shown in Figure 1.
All the studies found were observational (cross-sectional, retrospective, or prospective) and one was a case-control study. The total sample population consisted of 13,932 type 1 and type 2 diabetic patients. Most studies were conducted in Italy (n = 5), US (n = 5), followed by Saudi Arabia (n = 3), and Turkey (n = 3) (Table 1).
To measure anxiety, the most used questionnaires were the General Anxiety Disorder-7 (GAD-7) (n =7) and the Visual Analog Scale (VAS) for anxiety (n = 3). The remaining questionnaires used for anxiety were the Hospital Anxiety and Depression Scale (HADS), the Test of Depression and Anxiety Scale (TAD), Spence Children Anxiety Scale (SCAS), the Symptom Check List-revised anxiety subscale (SCL-ANX4), the General Health Questionnaire-12 items (GHQ-12), and the State-Trait Anxiety Inventory (STAI) (see Table 1).
The scales used to measure distress were the Diabetes Distress Scale (DDS) (n = 6), the Kessler Psychological Distress Scale (K10) (n = 3), the questionnaire Problem Areas in Diabetes-Distress item (PAID) (n = 3), and the Beirut Distress Scale (BDS22) (Table 1).
Finally, the stress measurement tools used were the Perceived Stress Scale (PSS) (n = 11), the Visual Analog Scale (VAS) for stress (n = 3), and the Impact of Event Scale Revised (IES-R) (Table 1).
The data were collected in different settings that included the collection of information through telephone surveys, online forms or through face-to-face at outpatient clinics, hospitals, or primary care centres. Most of the studies (n = 21) collected data during the first phase of the pandemic (January–June 2020).
The studies included had an adequate level of quality; according to the measurement tools applied there were no exclusions. The assessment and characteristics of the studies are represented in Table 1.
3.2. Mean Levels of Anxiety, Distress and Stress
The average anxiety levels varied from minimal [37,44,47,50,56,58,61], to mild [26,36,52], to moderate [62], to severe [39]. For diabetes distress, the mean levels were low [31,45,47,55,58], moderate [33,52,60], and high [29,54]. The mean stress levels found ranged from minimal [50,56,57,59], moderate [35,39,40,43,49,52,62], and high [46].
3.3. Meta-Analysis
Five random effects meta-analyses were performed with a total of 1024 T1DM patients and 4238 T2DM patients.
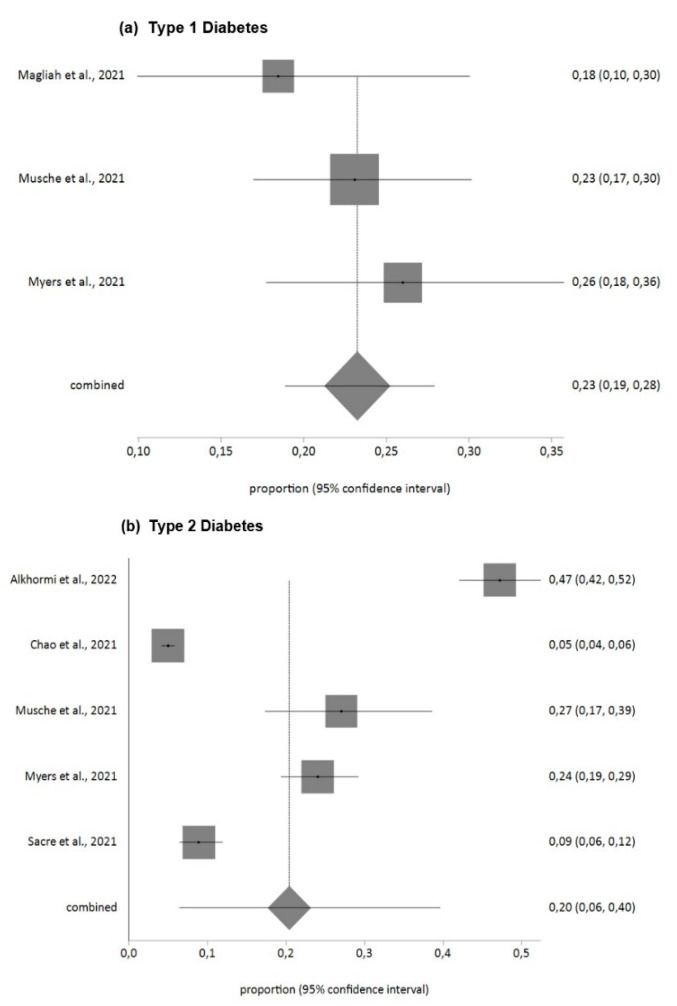
For anxiety according to the GAD-7 tool, the prevalence found in T1DM patients for moderate and severe levels (GAD-7 ≥ 10 score) was 23% (95% CI = 19–28) with low heterogeneity (I2 = 0%). For T2DM patients, it was 20% (95% CI = 6–40) with high heterogeneity (I2 = 99%).
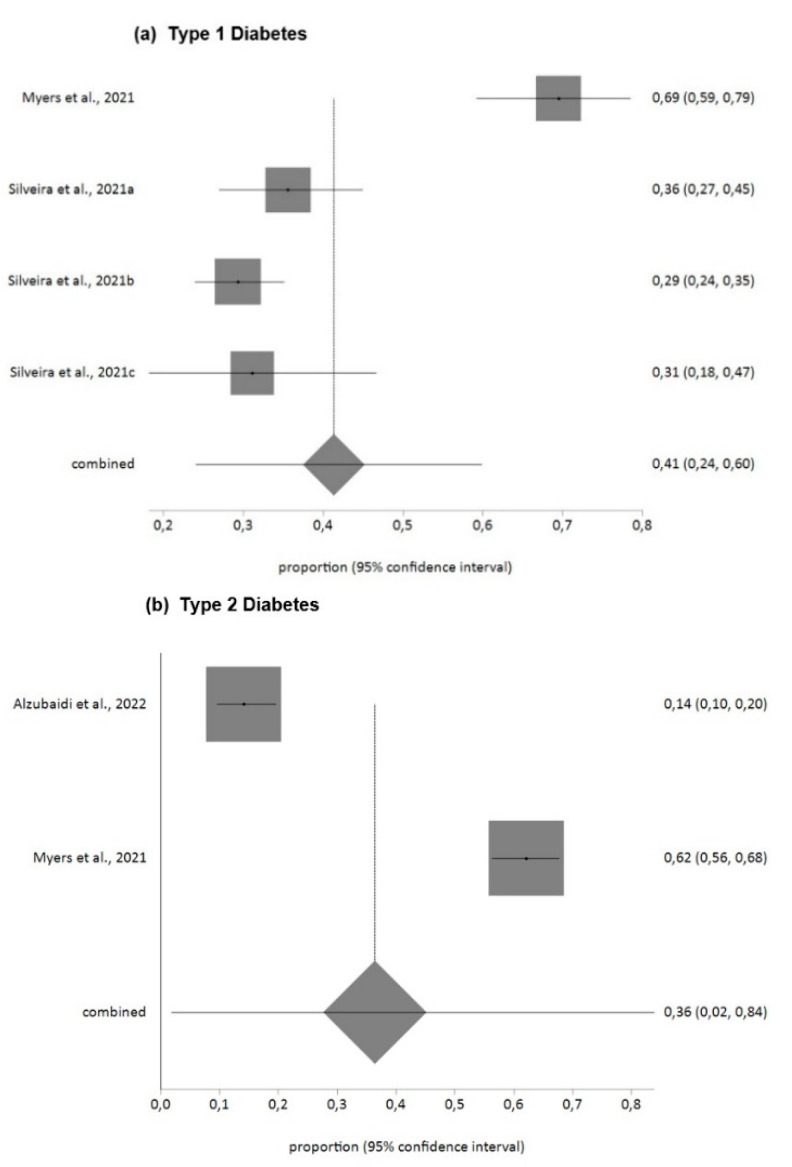
For diabetes distress measured with the DDS questionnaire, the prevalence found in T1DM patients for moderate and high levels (DDS > 2) was 41% (95% CI = 24–60) with high heterogeneity (I2 = 93%), and for T2DM patients 36% (95% CI = 2–84) with high heterogeneity (I2 = 99%).
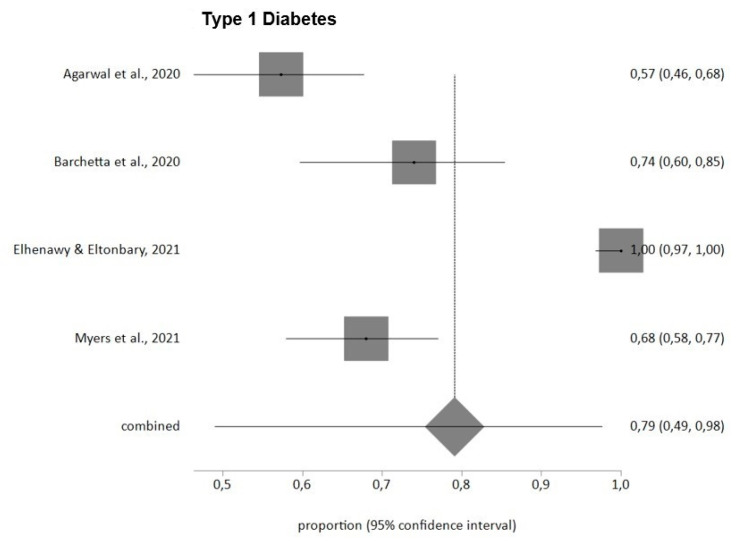
Finally, stress levels measured with the PSS questionnaire showed a prevalence in T1DM patients for moderate and high levels (PSS ≥ 14) of 79% (95% CI = 49–98) with high heterogeneity (I2 = 97%). Egger’s test showed no publication bias, and no study was removed after sensitivity analysis.
Figure 2, Figure 3 and Figure 4 summarize the findings in relation to anxiety, distress and stress prevalence.
Figure 2.
Prevalence of anxiety in DM patients during COVID-19 pandemic (GAD-7). (a) Type 1 Diabetes [48,51,52], (b) Type 2 Diabetes [30,37,51,52,58].
Figure 3.
Prevalence of distress in DM patients during COVID-19 pandemic (DDS). (a) Type 1 Diabetes [52,60], (b) Type 2 Diabetes [32,52].
Figure 4.
Prevalence of stress in DM patients during COVID-19 pandemic (PSS) [28,34,42,52].
4. Discussion
This study suggests relevant data about psychological disorders in the diabetic population during the pandemic, with a meta-analytical prevalence estimation of anxiety of 23% in T1DM patients and 20% in T2DM patients, diabetes distress of 41% in T1DM and 36% in T2DM, and stress of 79% in T1DM.
Studies before the pandemic reported a prevalence of anxiety symptoms of 17.7% for T1DM patients [63], and of 18% for T2DM [64] being for diabetes distress of 42.1% in T1DM [65] and 29.4% in T2DM [66], and for the stress of 50% in T1DM [67]. These data suggest a significant increase in symptoms.
In addition, the prevalence of anxiety found in DM patients was higher than that of studies performed in other groups during the pandemic. In the elderly population, the prevalence of anxiety symptoms found ranged from 10.10% [68] to 21.6% of moderate/severe anxiety in general population [69,70]. Other studies in the general population stated DM as one of the main psychosocial problems with a prevalence of up to 40% [71]. Even a recent meta-analysis in the general population showed that the mean prevalence of anxiety and psychological stress was 38.1% and 37.5%, respectively [72].
More than half of the population with chronic pathology wished to have received additional information about the risks associated with their medical condition during the pandemic [15]. Several authors indicate that the provision of diabetes care was significantly disrupted during the pandemic [73], as corroborated by studies conducted in chronic patients where 52% of adults and 38% of children worsened their health condition during confinement [74].
During the pandemic, the psychological disorders of diabetic patients are often not recognized or underestimated, which can impair the quality of life and self-management of the disease [75]. Greater support for self-care is related to higher adherence to the expected regimen and life changes [12]; however, psychological stressors can have an adverse effect, for example in the loss of good glycaemic control [76].
This study suggests a higher prevalence of anxiety and stress diabetes in T1DM patients, as corroborated by other studies that found several factors related to worse mental health such as T1DM or the female gender [70,77]. Other factors such as age remain controversial; some studies reported worse data in younger patients [70,77,78,79,80], while for others the levels were higher in older age groups [81].
Regarding the negative results of the pandemic involving mental health, other related factors were the fear of contagion by COVID-19 [82,83] and COVID-19 anxiety syndrome [84]. Studies reported that up to 27.3% of people with DM experienced stress due to the spread of the COVID-19 pandemic and 20% experienced stress due to fear of drug shortages [85]. Even in hospitalized patients, stress levels reached up to 39.3% [75], being lower than those found in our meta-analysis.
Several studies highlight these facts as a reason for greater concern and related them to a reduced capacity in the provision of psychological support to this group [73]. Therefore, finding strategies to identify and reduce anxiety, distress, and stress, as well as multiple other possible disorders such as depression or loneliness should be a priority for diabetes services [86]. In this sense, several studies support the routine implementation of telemedicine [87], as well as increasing the capacity of primary care to provide telehealth services for diseases related to COVID-19 and for several other chronic medical conditions [88]. Studies that have used the telemedicine care model have found positive benefits, for example in a higher mean reduction in the HbA1c level compared with traditional care model [89], so it could also have positive results in the treatment of mental health disorders.
Although a large number of protocols have been developed to identify and recover people with DM infected by COVID-19, there is still a large gap in mental health care. Managing DM in the midst of the COVID-19 pandemic has proven to be a real challenge. To date little is known about how pandemics globally affect the psychosocial health of people with DM. This study is the first meta-analysis to provide an assessment of current levels of anxiety, distress, and stress since the onset of COVID-19 exclusively in patients with DM. It is necessary to clarify the current situation of mental health disorders in these patients in order to establish intervention strategies.
4.1. Limitations
This study has several limitations. First, the inclusion of T21DM and T2DM patients from different countries could increase the heterogeneity given the differences in the conditions of the health system, the management and follow-up of the disease, and also clinical variability in the percentage of female, type of diabetes, or measurement instrument. The heterogeneity in the meta-analyses were also high. However, the results of this study may allow understanding the impact of the pandemic on these patients as a start for future research. Another limitation is the inclusion of all the data since the start of the pandemic (different restrictions and waves of contagion), which could increase the heterogeneity. Finally, the different methods of data collection (by telephone, online, or face-to-face interviews) could lead to bias. This review has shown that there are important levels of anxiety, distress, and stress in people with diabetes during the COVID-19 pandemic. Future research should analyse which factors are related with these problems and how those levels can be reduced.
4.2. Implication for Practice and Research
The COVID-19 infection and confinement have a diverse impact on access to health services, psychosocial well-being, and self-management of people with diabetes, which must be contextualized to the responses and preparation of each country. Diabetes significantly increases the risk of emotional and behavioural disorders, especially in times of social crisis such as the one experienced with the COVID-19 pandemic [90]. Improving effective self-care behaviours that include healthy coping (healthy eating, being active, blood glucose control) are essential components to establishing optimal behaviour goals, which in turn will improve mental health outcomes [5]. Future research is needed to analyse the monitoring of levels as the pandemic progresses, as well as large multicentre longitudinal studies to avoid the above-mentioned limitations.
5. Conclusions
The prevalence found during the COVID-19 pandemic for anxiety ranged between 23% and 20%, for diabetes distress between 41% and 36%, and for stress it was 79%. People with diabetes have significant psychiatric comorbidity as well as psychological factors that negatively affect disease management, increasing their vulnerability in an emergency situation. To establish comprehensive care in diabetic patients addressing mental health is essential, as well as including specific policy interventions to reduce the potential psychological harm of the COVID-19 pandemic. Moreover, assessing the variables that can prevent or reduce the development of anxiety, distress, and stress in this population would be important.
Acknowledgments
This study forms part of the Doctoral Thesis of the first-named author within the Health Sciences Doctoral Program from the University of Murcia (Spain).
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jpm12091412/s1, Supplementary Material Table S1: PRISMA 2020 checklist.
Appendix A
Table A1.
Observational studies quality assessment with National Heart, Lung, and Blood Institute.
| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abdelghani et al., [26], 2021, Egypt | Y | Y | Y | Y | Y | NA | NA | NA | Y | NA | Y | NA | Y | Y |
| Abdoli et al. [27], 2021, US, Brazil, and Iran | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Agarwal et al. [28], 2020, India | Y | Y | NR | Y | N | NA | NA | NA | N | NA | Y | NA | NA | Y |
| Ajele et al., [29], 2022, Nigeria | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | N |
| Alkhormi et al., [30], 2022, Saudi Arabia | Y | Y | Y | Y | Y | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Alshareef et al. [31], 2020, Saudi Arabia | Y | Y | NR | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Alzubaidi et al. [32], 2022, United Arab Emirates | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | N |
| Bao [33], 2021, China | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Barchetta et al. [34], 2020, Italy | Y | Y | NR | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Büyükbayram et al. [35], 2022, Turkey | Y | Y | NR | Y | Y | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Caruso et al. [36], 2021, Italy | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | N |
| Chao et al. [37], 2021, US | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Cusinato et al. [38], 2021, Italy | Y | Y | NR | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | N |
| Cyranka et al., [39], 2021, Poland | Y | Y | NR | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | N |
| Di Dalmazi et al. [40], Italy | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Di Riso et al. [41], 2021, Italy | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Elhenawy and Eltonbary, [42], 2021, Egypt | Y | Y | NR | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Hosomi et al. [43], 2022, Japan | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Huang et al. [44], 2022, China | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | N |
| Kim et al. [45], 2022, US | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Khari et al. [46], 2021, Iran | Y | Y | NR | Y | Y | NA | NA | NA | Y | NA | Y | NA | NA | N |
| Madsen et al., [47], 2021, Denmark | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | N |
| Magliah et al. [48], 2021, Saudi Arabia | Y | Y | NR | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Munekawa et al. [49], 2021, Japan | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Miller et al. [50], 2022, US | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Musche et al., [51], 2021, Germany | Y | Y | NR | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Myers et al., [52], 2021, US | Y | Y | NR | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | N |
| Olickal et al. [53], 2020, India | Y | Y | Y | Y | Y | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Naous et al. [54], 2022, Lebanon | Y | Y | NR | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | N |
| Nassar and Salameh, [55], 2021, Lebanon | Y | Y | N | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | N |
| Regeer et al. [56], 2021, Netherlands | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Ruissen et al. [57], 2021, Netherlands | Y | Y | NR | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Sacre et al. [58], 2021, Australia | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Shin et al. [59], 2021, Korea | Y | Y | Y | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Silveira et al. [60], 2021, Brazil | Y | Y | NR | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Sisman et al. [61], 2021, Turkey | Y | Y | NR | Y | N | NA | NA | NA | Y | NA | Y | NA | NA | Y |
| Utli and Vural Doğru [62], 2021, Turkey | Y | Y | Y | Y | Y | NA | NA | NA | Y | NA | Y | NA | NA | Y |
N = No, Q = Question, Y = Yes.
Author Contributions
Conceptualization, R.A.G.-L. and N.S.-M.; methodology, R.A.G.-L. and J.L.G.-U.; software, A.V.-S.; validation, N.S.-M. and J.L.R.-B.; formal analysis, J.L.R.-B.; resources, M.J.M.-J. and M.E.G.-B.; data curation, R.A.G.-L. and M.E.G.-B.; writing—original draft preparation, R.A.G.-L. and N.S.-M.; writing—review and editing, J.L.G.-U. and N.S.-M.; visualization, J.L.G.-U. and N.S.-M.; supervision, J.L.G.-U. and N.S.-M.; project administration J.L.G.-U. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pandey D., Bansal S., Goyal S., Garg A., Sethi N., Pothiyill D.I., Sreelakshmi E.S., Sayyad M.G., Sethi R. Psychological Impact of Mass Quarantine on Population during Pandemics—The COVID-19 Lock-Down (COLD) Study. PLoS ONE. 2020;15:e0240501. doi: 10.1371/journal.pone.0240501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu H., Chen S., Liu M., Nie H., Lu H. Comorbid Chronic Diseases Are Strongly Correlated with Disease Severity among COVID-19 Patients: A Systematic Review and Meta-Analysis. Aging Dis. 2020;11:668. doi: 10.14336/AD.2020.0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shafiee A., Teymouri Athar M.M., Nassar M., Seighali N., Aminzade D., Fattahi P., Rahmannia M., Ahmadi Z. Comparison of COVID-19 Outcomes in Patients with Type 1 and Type 2 Diabetes: A Systematic Review and Meta-Analysis. Diabetes Metab. Syndr. 2022;16:102512. doi: 10.1016/j.dsx.2022.102512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fauci A.S., Lane H.C., Redfield R.R. COVID-19—Navigating the Uncharted. N. Engl. J. Med. 2020;382:1268–1269. doi: 10.1056/NEJMe2002387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singhai K., Swami M.K., Nebhinani N., Rastogi A., Jude E. Psychological Adaptive Difficulties and Their Management during COVID-19 Pandemic in People with Diabetes Mellitus. Diabetes Metab. Syndr. 2020;14:1603–1605. doi: 10.1016/j.dsx.2020.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Balhara Y.P.S. Diabetes and Psychiatric Disorders. Indian J. Endocrinol. Metab. 2011;15:274. doi: 10.4103/2230-8210.85579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghosh A., Arora B., Gupta R., Anoop S., Misra A. Effects of Nationwide Lockdown during COVID-19 Epidemic on Lifestyle and Other Medical Issues of Patients with Type 2 Diabetes in North India. Diabetes Metab. Syndr. Clin. Res. Rev. 2020;14:917–920. doi: 10.1016/j.dsx.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C., Ho R. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hossain M.M., Sultana A., Purohit N. Mental Health Outcomes of Quarantine and Isolation for Infection Prevention: A Systematic Umbrella Review of the Global Evidence. Epidemiol. Health. 2020;42:e2020038. doi: 10.4178/EPIH.E2020038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meng H., Xu Y., Dai J., Zhang Y., Liu B., Yang H. Analyze the Psychological Impact of COVID-19 among the Elderly Population in China and Make Corresponding Suggestions. Psychiatry Res. 2020;289:112983. doi: 10.1016/j.psychres.2020.112983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holaday L.W., Oladele C.R., Miller S.M., Dueñas M.I., Roy B., Ross J.S. Loneliness, Sadness, and Feelings of Social Disconnection in Older Adults during the COVID-19 Pandemic. J. Am. Geriatr. Soc. 2021 doi: 10.1111/jgs.17599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dziedzic B., Idzik A., Kobos E., Sienkiewicz Z., Kryczka T., Fidecki W., Wysokiński M. Loneliness and Mental Health among the Elderly in Poland during the COVID-19 Pandemic. BMC Public Health. 2021;21:1976. doi: 10.1186/s12889-021-12029-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Basit K.A., Zafar A.B., Fawwad A., Waris N., Shaheen F., Basit A. Psychometric Analysis for Fear of COVID-19 Scale (FCV-19S) and Its Association with Depression in Patients with Diabetes: A Cross Sectional Study from a Tertiary Care Centre in Karachi, Pakistan. Diabetes Metab. Syndr. 2021;15:733–737. doi: 10.1016/j.dsx.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al-Sofiani M.E., Albunyan S., Alguwaihes A.M., Kalyani R.R., Golden S.H., Alfadda A. Determinants of Mental Health Outcomes among People with and without Diabetes during the COVID-19 Outbreak in the Arab Gulf Region. J. Diabetes. 2021;13:339–352. doi: 10.1111/1753-0407.13149. [DOI] [PubMed] [Google Scholar]
- 15.Pécout C., Pain E., Chekroun M., Champeix C., Kulak C., Prieto R., Vugt J., Gilchrist K., Lainé-Pellet A.-F. Impact of the COVID -19 Pandemic on Patients Affected by Non-Communicable Diseases in Europe and in the USA. Int. J. Environ. Res. Public Health. 2021;18:6697. doi: 10.3390/ijerph18136697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dyer O. COVID-19: Pandemic Is Having “Severe” Impact on Non-Communicable Disease Care, WHO Survey Finds. BMJ. 2020;369:m2210. doi: 10.1136/BMJ.M2210. [DOI] [PubMed] [Google Scholar]
- 17.Nachimuthu S., Vijayalakshmi R., Sudha M., Viswanathan V. Coping with Diabetes during the COVID-19 Lockdown in India: Results of an Online Pilot Survey. Diabetes Metab. Syndr. Clin. Res. Rev. 2020;14:579–582. doi: 10.1016/J.DSX.2020.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Co M.A., Tan L.S.M., Tai E.S., Griva K., Amir M., Chong K.J., Lee Y.S., Lee J., Khoo E.Y.H., Wee H.L. Factors Associated with Psychological Distress, Behavioral Impact and Health-Related Quality of Life among Patients with Type 2 Diabetes Mellitus. J. Diabetes Complicat. 2015;29:378–383. doi: 10.1016/J.JDIACOMP.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 19.Kowall B., Kostev K., Landgraf R., Hauner H., Bierwirth R., Rathmann W. Effects of the COVID-19 Pandemic on Clinically Diagnosed Psychiatric Disorders in Persons with Type 2 Diabetes. Diabetes Med. 2022;39:e14852. doi: 10.1111/DME.14852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moradian S., Teufel M., Jahre L., Musche V., Fink M., Dinse H., Schweda A., Weismüller B., Dörrie N., Tan S., et al. Mental Health Burden of Patients with Diabetes before and after the Initial Outbreak of COVID-19: Predictors of Mental Health Impairment. BMC Public Health. 2021;21:2068. doi: 10.1186/s12889-021-12101-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Westley K.V., August K.J., Alger M.R., Markey C.H. Main and interactive effects of diabetes distress and stress from life events on overall psychological distress. J. Health Psychol. 2021;26:312–318. doi: 10.1177/1359105318804865. [DOI] [PubMed] [Google Scholar]
- 22.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Heart, Lung and Blood Institute Study Quality Assessment Tools for Observational Cohort and Cross-Sectional Studies. [(accessed on 1 June 2022)]; Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- 24.Howick J., Chalmers I., Glasziou P., Greenhalg T., Heneghan C., Liberati A., Moschetti I., Phillips B., Thornton H. The Oxford 2011 Levels of Evidence. [(accessed on 10 July 2022)]. Available online: https://www.cebm.net/2016/05/ocebm-levels-of-evidence.
- 25.Higgins J.P.T., Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. The Cochrane Collaboration. [(accessed on 7 July 2022)]. Available online: www.cochrane-handbook.org.
- 26.Abdelghani M., Hamed M.G., Said A., Fouad E. Evaluation of Perceived Fears of COVID-19 Virus Infection and Its Relationship to Health-Related Quality of Life among Patients with Diabetes Mellitus in Egypt during Pandemic: A Developing Country Single-Center Study. Diabetol. Int. 2021;13:108–116. doi: 10.1007/s13340-021-00511-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abdoli S., Silveira M.S.V.M., Doosti-Irani M., Fanti P., Miller-Bains K., Pavin E.J., Cardoso E.B., Vardanjani L.R., Noorian K., Hessler D. Cross-National Comparison of Psychosocial Well-Being and Diabetes Outcomes in Adults with Type 1 Diabetes during the COVID-19 Pandemic in US, Brazil, and Iran. Diabetol. Metab. Syndr. 2021;13:63. doi: 10.1186/s13098-021-00681-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Agarwal N., Harikar M., Shukla R., Bajpai A. COVID-19 Pandemic: A Double Trouble for Indian Adolescents and Young Adults Living with Type 1 Diabetes. Int. J. Diabetes Dev. Ctries. 2020;40:346–352. doi: 10.1007/s13410-020-00869-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ajele W.K., Babalola O.B., Idehen E.E., Oladejo T.A. Relationship between Depression and Psychological Well-Being among Persons with Diabetes during COVID-19 Pandemic: Diabetes Distress as a Mediator. J. Diabetes Metab. Disord. 2022;21:631–635. doi: 10.1007/S40200-022-01025-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alkhormi A.H., Mahfouz M.S., Alshahrani N.Z., Hummadi A., Hakami W.A., Alattas D.H., Alhafaf H.Q., Kardly L.E., Mashhoor M.A. Psychological Health and Diabetes Self-Management among Patients with Type 2 Diabetes during COVID-19 in the Southwest of Saudi Arabia. Medicina. 2022;58:675. doi: 10.3390/medicina58050675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alshareef R., Al Zahrani A., Alzahrani A., Ghandoura L. Impact of the COVID-19 Lockdown on Diabetes Patients in Jeddah, Saudi Arabia. Diabetes Metab. Syndr. Clin. Res. Rev. 2020;14:1583–1587. doi: 10.1016/j.dsx.2020.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alzubaidi H., Hafidh K., Saidawi W., Othman A.M., Khakpour M.M., Zoghbor M.M., Abu-Gharbieh E., Alzoubi K.H., Shaw J.E. Behavioral, Psychological, and Clinical Outcomes of Arabic-Speaking People with Type 2 Diabetes during COVID-19 Pandemic. Prim. Care Diabetes. 2022;16:355–360. doi: 10.1016/j.pcd.2022.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bao H. Relationship among Family Support, Mental Resilience and Diabetic Distress in Patients with Type 2 Diabetic Mellitus during COVID-19. Iran. J. Public Health. 2021;50:1648–1657. doi: 10.18502/ijph.v50i8.6811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barchetta I., Cimini F.A., Bertoccini L., Ceccarelli V., Spaccarotella M., Baroni M.G., Cavallo M.G. Effects of Work Status Changes and Perceived Stress on Glycaemic Control in Individuals with Type 1 Diabetes during COVID-19 Lockdown in Italy. Diabetes Res. Clin. Pract. 2020;170:108513. doi: 10.1016/j.diabres.2020.108513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Büyükbayram Z., Aksoy M., Güngör A. Investigation of the Perceived Stress Levels and Adherence to Treatment of Individuals with Type 2 Diabetes During the COVID-19 Pandemic. Arch. Health Sci. Res. 2022;9:61–69. doi: 10.5152/ArcHealthSciRes.2022.21088. [DOI] [Google Scholar]
- 36.Caruso I., Di Molfetta S., Guarini F., Giordano F., Cignarelli A., Natalicchio A., Perrini S., Leonardini A., Giorgino F., Laviola L. Reduction of Hypoglycaemia, Lifestyle Modifications and Psychological Distress during Lockdown Following SARS-CoV-2 Outbreak in Type 1 Diabetes. Diabetes Metab. Res. Rev. 2021;37:e3404. doi: 10.1002/DMRR.3404. [DOI] [PubMed] [Google Scholar]
- 37.Chao A.M., Wadden T.A., Clark J.M., Hayden K.M., Howard M.J., Johnson K.C., Laferrère B., McCaffery J.M., Wing R.R., Yanovski S.Z., et al. Changes in the Prevalence of Symptoms of Depression, Loneliness, and Insomnia in U.S. Older Adults with Type 2 Diabetes during the COVID-19 Pandemic: The Look AHEAD Study. Diabetes Care. 2021;45:74–82. doi: 10.2337/dc21-1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cusinato M., Martino M., Sartori A., Gabrielli C., Tassara L., Debertolis G., Righetto E., Moretti C. Anxiety, Depression, and Glycemic Control during COVID-19 Pandemic in Youths with Type 1 Diabetes. J. Pediatr. Endocrinol. Metab. 2021;34:1089–1093. doi: 10.1515/jpem-2021-0153. [DOI] [PubMed] [Google Scholar]
- 39.Cyranka K., Matejko B., Klupa T., Małecki M.T., Kieć-Wilk B., Cyganek K., Dudek D. Type 1 Diabetes and COVID-19: The Level of Anxiety, Stress and the General Mental Health in Comparison to Healthy Control. Psychiatr. Pol. 2021;55:511. doi: 10.12740/PP/ONLINEFIRST/133356. [DOI] [PubMed] [Google Scholar]
- 40.Di Dalmazi G., Maltoni G., Bongiorno C., Tucci L., DI Natale V., Moscatiello S., Laffi G., Pession A., Zucchini S., Pagotto U. Comparison of the Effects of Lockdown Due to COVID-19 on Glucose Patterns among Children, Adolescents, and Adults with Type 1 Diabetes: CGM Study. BMJ Open Diabetes Res. Care. 2020;8:e001664. doi: 10.1136/bmjdrc-2020-001664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Di Riso D., Bertini S., Spaggiari S., Olivieri F., Zaffani S., Comerlati L., Marigliano M., Piona C., Maffeis C. Short-Term Effects of COVID-19 Lockdown in Italian Children and Adolescents with Type 1 Diabetes Mellitus: The Role of Separation Anxiety. Int. J. Environ. Res. Public Health. 2021;18:5549. doi: 10.3390/IJERPH18115549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Elhenawy Y.I., Eltonbary K.Y. Glycemic Control among Children and Adolescents with Type 1 Diabetes during COVID-19 Pandemic in Egypt: A Pilot Study. Int. J. Diabetes Dev. Ctries. 2021;41:389–395. doi: 10.1007/s13410-021-00968-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hosomi Y., Munekawa C., Hashimoto Y., Okamura T., Takahashi F., Kawano R., Nakajima H., Majima S., Senmaru T., Nakanishi N., et al. The Effect of COVID-19 Pandemic on the Lifestyle and Glycemic Control in Patients with Type 1 Diabetes: A Retrospective Cohort Study. Diabetol. Int. 2022;13:85–90. doi: 10.1007/s13340-021-00507-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Huang L., Zhang L., Jiang S., Liang B., Xu N., Li J., Zhang X., Zhang Z. Association of the Coronavirus Disease 2019 Outbreak on the Diabetes Self-Management in Chinese Patients: An Analytical Cross-Sectional Study. Diabetes. Metab. Syndr. Obes. 2022;15:1413–1422. doi: 10.2147/DMSO.S351823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kim M.J., Park C., Sharp L.K., Quinn L., Bronas U.G., Gruss V., Fritschi C. Impact of Worries Associated with COVID-19 on Diabetes-Related Psychological Symptoms in Older Adults with Type 2 Diabetes. Geriatr. Nurs. 2022;43:58–63. doi: 10.1016/j.gerinurse.2021.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Khari S., Pazokian M., Zarmehrparirouy M. Perceived Stress and Preventive Behaviors in Patients with Diabetes during the Outbreak of Coronavirus Disease 2019. Evid. Based Care J. 2021;11:53–59. doi: 10.22038/EBCJ.2021.60878.2587. [DOI] [Google Scholar]
- 47.Madsen K.P., Willaing I., Rod N.H., Varga T.V., Joensen L.E. Psychosocial Health in People with Diabetes during the First Three Months of the COVID-19 Pandemic in Denmark. J. Diabetes Complicat. 2021;35:107858. doi: 10.1016/j.jdiacomp.2021.107858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Magliah S.F., Zarif H.A., Althubaiti A., Sabban M.F. Managing Type 1 Diabetes among Saudi Adults on Insulin Pump Therapy during the COVID-19 Lockdown. Diabetes Metab. Syndr. 2021;15:63–68. doi: 10.1016/J.DSX.2020.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Munekawa C., Hosomi Y., Hashimoto Y., Okamura T., Takahashi F., Kawano R., Nakajima H., Osaka T., Okada H., Majima S., et al. Effect of Coronavirus Disease 2019 Pandemic on the Lifestyle and Glycemic Control in Patients with Type 2 Diabetes: A Cross-Section and Retrospective Cohort Study. Endocr. J. 2021;68:201–210. doi: 10.1507/endocrj.EJ20-0426. [DOI] [PubMed] [Google Scholar]
- 50.Miller A.L., Albright D., Bauer K.W., Riley H.O., Hilliard M.E., Sturza J., Kaciroti N., Lo S.L., Clark K.M., Lee J.M., et al. Self-Regulation as a Protective Factor for Diabetes Distress and Adherence in Youth with Type 1 Diabetes During the COVID-19 Pandemic. J. Pediatr. Psychol. 2022;47:873–882. doi: 10.1093/jpepsy/jsac045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Musche V., Kohler H., Bäuerle A., Schweda A., Weismüller B., Fink M., Schadendorf T., Robitzsch A., Dörrie N., Tan S., et al. COVID-19-Related Fear, Risk Perception, and Safety Behavior in Individuals with Diabetes. Healthcare. 2021;9:480. doi: 10.3390/healthcare9040480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Myers B.A., Klingensmith R., de Groot M. Emotional Correlates of the COVID-19 Pandemic in Individuals with and without Diabetes. Diabetes Care. 2021;45:42–58. doi: 10.2337/dc21-0769. [DOI] [PubMed] [Google Scholar]
- 53.Olickal J.J., Chinnakali P., Suryanarayana B.S., Ulaganeethi R., Kumar S.S., Saya G.K. Effect of COVID19 Pandemic and National Lockdown on Persons with Diabetes from Rural Areas Availing Care in a Tertiary Care Center, Southern India. Diabetes Metab. Syndr. Clin. Res. Rev. 2020;14:1967–1972. doi: 10.1016/j.dsx.2020.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Naous E., Boulos M., Sleilaty G., Achkar A.A., Gannagé-Yared M.-H. Quality of Life and Other Patient-Reported Outcomes in Adult Lebanese Patients with Type 2 Diabetes during COVID-19 Pandemic. J. Endocrinol. Investig. 2022;45:763–772. doi: 10.1007/s40618-021-01701-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nassar C.M., Salameh P. Association between Type 2 Diabetes Mellitus and Health Literacy, Behavioral and Environmental Risk Factors in Lebanon: A Case-Control Study. J. Health Soc. Sci. 2021;6:103–114. [Google Scholar]
- 56.Regeer H., Nieuwenhuijse E.A., Vos R.C., Kiefte-de Jong J.C., van Empelen P., de Koning E.J.P., Bilo H.J.G., Huisman S.D. Psychological Factors Associated with Changes in Physical Activity in Dutch People with Type 2 Diabetes under Societal Lockdown: A Cross-Sectional Study. Endocrinol. Diabetes Metab. 2021;4:e00249. doi: 10.1002/edm2.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ruissen M.M., Regeer H., Landstra C.P., Schroijen M., Jazet I., Nijhoff M.F., Pijl H., Ballieux B.E.P.B., Dekkers O., Huisman S.D., et al. Increased Stress, Weight Gain and Less Exercise in Relation to Glycemic Control in People with Type 1 and Type 2 Diabetes during the COVID-19 Pandemic. BMJ Open Diabetes Res. Care. 2021;9:e002035. doi: 10.1136/bmjdrc-2020-002035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sacre J.W., Holmes-Truscott E., Salim A., Anstey K.J., Drummond G.R., Huxley R.R., Magliano D.J., van Wijngaarden P., Zimmet P.Z., Speight J., et al. Impact of the COVID-19 Pandemic and Lockdown Restrictions on Psychosocial and Behavioural Outcomes among Australian Adults with Type 2 Diabetes: Findings from the PREDICT Cohort Study. Diabet. Med. 2021;38:e14611. doi: 10.1111/dme.14611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shin S.M., Oh T.J., Choi S.H., Jang H.C. Effects of Social Distancing on Diabetes Management in Older Adults during COVID-19 Pandemic. Diabetes Metab. J. 2021;45:765–772. doi: 10.4093/DMJ.2021.0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Silveira M.S.V.M., Pavin E.J., Cardoso E.B., Fanti P., Abdoli S. Emotional Burden and Care of Adults with Type 1 Diabetes during the COVID-19 Pandemic in Brazilian Regions. J. Diabetes Complicat. 2021;35:108053. doi: 10.1016/j.jdiacomp.2021.108053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sisman P., Polat I., Aydemir E., Karsi R., Gul O.O., Cander S., Ersoy C., Erturk E. How the COVID-19 Outbreak Affected Patients with Diabetes Mellitus? Int. J. Diabetes Dev. Ctries. 2022;42:53–61. doi: 10.1007/s13410-021-00992-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Utli H., Vural Doğru B. The Effect of the COVID-19 Pandemic on Self-Management in Patients with Type 2 Diabetics. Prim. Care Diabetes. 2021;15:799–805. doi: 10.1016/j.pcd.2021.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Akbarizadeh M., Far M.N., Ghaljaei F. Prevalence of Depression and Anxiety among Children with Type 1 and Type 2 Diabetes: A Systematic Review and Meta-Analysis. World J. Pediatr. 2022;18:16–26. doi: 10.1007/S12519-021-00485-2/FIGURES/5. [DOI] [PubMed] [Google Scholar]
- 64.Chaturvedi S.K., Manche Gowda S., Ahmed H.U., Alosaimi F.D., Andreone N., Bobrov A., Bulgari V., Carrà G., Castelnuovo G., De Girolamo G., et al. More Anxious than Depressed: Prevalence and Correlates in a 15-Nation Study of Anxiety Disorders in People with Type 2 Diabetes Mellitus. Gen. Psychiatry. 2019;32:15. doi: 10.1136/GPSYCH-2019-100076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fisher L., Hessler D., Polonsky W., Strycker L., Masharani U., Peters A. Diabetes Distress In Adults With Type 1 Diabetes: Prevalence, Incidence and Change Over Time. J. Diabetes Complicat. 2016;30:1123. doi: 10.1016/J.JDIACOMP.2016.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Huynh G., Tran T.T., Do T.H.T., Truong T.T.D., Ong P.T., Nguyen T.N.H., Pham L.A. Diabetes-Related Distress Among People with Type 2 Diabetes in Ho Chi Minh City, Vietnam: Prevalence and Associated Factors. Diabetes Metab. Syndr. Obes. Targets Ther. 2021;14:683–690. doi: 10.2147/DMSO.S297315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rechenberg K., Whittemore R., Holland M., Grey M. General and Diabetes-Specific Stress in Adolescents with Type 1 Diabetes. Diabetes Res. Clin. Pract. 2017;130:1–8. doi: 10.1016/J.DIABRES.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang Z.H., Qi S.G., Zhang H., Mao P.X., He Y.L., Li J., Xiao S.Y., Peng H.M., Sun W.W., Guo H.Y., et al. Impact of the COVID-19 epidemic on anxiety among the elderly in community. Zhonghua Yi Xue Za Zhi. 2020;100:3179–3185. doi: 10.3760/cma.j.cn112137-20200720-02167. [DOI] [PubMed] [Google Scholar]
- 69.Shevlin M., McBride O., Murphy J., Miller J.G., Hartman T.K., Levita L., Mason L., Martinez A.P., McKay R., Stocks T.V.A., et al. Anxiety, Depression, Traumatic Stress and COVID-19-Related Anxiety in the UK General Population during the COVID-19 Pandemic. BJPsych Open. 2020;6:E125. doi: 10.1192/BJO.2020.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dawel A., Shou Y., Smithson M., Cherbuin N., Banfield M., Calear A.L., Farrer L.M., Gray D., Gulliver A., Housen T., et al. The Effect of COVID-19 on Mental Health and Wellbeing in a Representative Sample of Australian Adults. Front. Psychiatry. 2020;11:1026. doi: 10.3389/FPSYT.2020.579985/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Young-Hyman D., De Groot M., Hill-Briggs F., Gonzalez J.S., Hood K., Peyrot M. Psychosocial Care for People With Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care. 2016;39:2126–2140. doi: 10.2337/DC16-2053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Necho M., Tsehay M., Birkie M., Biset G., Tadesse E. Prevalence of Anxiety, Depression, and Psychological Distress among the General Population during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Int. J. Soc. Psychiatry. 2021;67:892–906. doi: 10.1177/00207640211003121. [DOI] [PubMed] [Google Scholar]
- 73.Forde R., Arente L., Ausili D., De Backer K., Due-Christensen M., Epps A., Fitzpatrick A., Grixti M., Groen S., Halkoaho A., et al. The Impact of the COVID-19 Pandemic on People with Diabetes and Diabetes Services: A Pan-European Survey of Diabetes Specialist Nurses Undertaken by the Foundation of European Nurses in Diabetes Survey Consortium. Diabet. Med. 2021;38:e14498. doi: 10.1111/DME.14498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.De Groef A., Hallemans A., Gebruers N., Meirte J., Saeys W., Truijen S., Haenen V., Johnson C., Meert L., Peeters L., et al. The Impact of COVID-19 Lockdown on the General Health Status of People with Chronic Health Conditions in Belgium: A Cross-Sectional Survey Study. Physiother. Theory Pract. 2022:1–16. doi: 10.1080/09593985.2022.2036278. [DOI] [PubMed] [Google Scholar]
- 75.Somma A., Krueger R.F., Markon K.E., Gialdi G., Colanino M., Ferlito D., Liotta C., Frau C., Fossati A. A Longitudinal Study on Clinically Relevant Self-Reported Depression, Anxiety and Acute Stress Features among Italian Community-Dwelling Adults during the COVID-19 Related Lockdown: Evidence of a Predictive Role for Baseline Dysfunctional Personality Dimensions. J. Affect. Disord. 2021;282:364–371. doi: 10.1016/J.JAD.2020.12.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yang A., Wang X., Wei J., Zhao G., Zhang L., Jing X., Wang K., Gao B. Analysis of Influencing Factors of Blood Glucose Levels in Diabetic Patients during Epidemic of COVID-19. Chin. J. Diabetes Mellit. 2020;12:500–503. doi: 10.3760/cma.j.cn115791-20200310-00139. [DOI] [Google Scholar]
- 77.Solomou I., Constantinidou F. Prevalence and Predictors of Anxiety and Depression Symptoms during the COVID-19 Pandemic and Compliance with Precautionary Measures: Age and Sex Matter. Int. J. Environ. Res. Public Health. 2020;17:4924. doi: 10.3390/IJERPH17144924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer-Childs E.R., Barger L.K., et al. Mental Health, Substance Use, and Suicidal Ideation during the COVID-19 Pandemic. MMWR Morb. Mortal. Wkly. Rep. 2020;69:1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.González-Sanguino C., Ausín B., Castellanos M.Á., Saiz J., López-Gómez A., Ugidos C., Muñoz M. Mental Health Consequences during the Initial Stage of the 2020 Coronavirus Pandemic (COVID-19) in Spain. Brain. Behav. Immun. 2020;87:172–176. doi: 10.1016/J.BBI.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bidzan-Bluma I., Bidzan M., Jurek P., Bidzan L., Knietzsch J., Stueck M., Bidzan M. A Polish and German Population Study of Quality of Life, Well-Being, and Life Satisfaction in Older Adults during the COVID-19 Pandemic. Front. Psychiatry. 2020;11:585813. doi: 10.3389/FPSYT.2020.585813/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Parlapani E., Holeva V., Nikopoulou V.A., Sereslis K., Athanasiadou M., Godosidis A., Stephanou T., Diakogiannis I. Intolerance of Uncertainty and Loneliness in Older Adults during the COVID-19 Pandemic. Front. Psychiatry. 2020;11:842. doi: 10.3389/FPSYT.2020.00842/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Joensen L.E., Madsen K.P., Holm L., Nielsen K.A., Rod M.H., Petersen A.A., Rod N.H., Willaing I. Diabetes and COVID-19: Psychosocial Consequences of the COVID-19 Pandemic in People with Diabetes in Denmark-What Characterizes People with High Levels of COVID-19-Related Worries? Diabet. Med. 2020;37:1146–1154. doi: 10.1111/DME.14319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pettinicchio D., Maroto M., Chai L., Lukk M. Findings from an Online Survey on the Mental Health Effects of COVID-19 on Canadians with Disabilities and Chronic Health Conditions. Disabil. Health J. 2021;14:101085. doi: 10.1016/j.dhjo.2021.101085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Distaso W., Malik M., Semere B.S., Alhakami B.A., Alexander E.C., Hirani D., Shah R.J., Kinga Suba M.D., Mckechnie V., Nikčević A., et al. Diabetes Self-Management during the COVID-19 Pandemic and Its Associations with COVID-19 Anxiety Syndrome, Depression, and Health Anxiety. Diabet. Med. 2022;00:e14911. doi: 10.1111/dme.14911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sankar P., Ahmed W.N., Mariam Koshy V., Jacob R., Sasidharan S. Effects of COVID-19 Lockdown on Type 2 Diabetes, Lifestyle and Psychosocial Health: A Hospital-Based Cross-Sectional Survey from South India. Diabetes Metab. Syndr. 2020;14:1815–1819. doi: 10.1016/j.dsx.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of Depression Symptoms in US Adults before and during the COVID-19 Pandemic. JAMA Netw. Open. 2020;3:e2019686. doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tchero H., Kangambega P., Briatte C., Brunet-Houdard S., Retali G.R., Rusch E. Clinical Effectiveness of Telemedicine in Diabetes Mellitus: A Meta-Analysis of 42 Randomized Controlled Trials. Telemed. J. E Health. 2019;25:569–583. doi: 10.1089/tmj.2018.0128. [DOI] [PubMed] [Google Scholar]
- 88.Jetty A., Jabbarpour Y., Westfall M., Kamerow D.B., Petterson S., Westfall J.M. Capacity of Primary Care to Deliver Telehealth in the United States. J. Am. Board Fam. Med. 2021;34:S48–S54. doi: 10.3122/jabfm.2021.S1.200202. [DOI] [PubMed] [Google Scholar]
- 89.Faleh AlMutairi M., Tourkmani A.M., Alrasheedy A.A., ALHarbi T.J., Bin Rsheed A.M., ALjehani M., AlRuthia Y. Cost-Effectiveness of Telemedicine Care for Patients with Uncontrolled Type 2 Diabetes Mellitus during the COVID-19 Pandemic in Saudi Arabia. Ther. Adv. Chronic Dis. 2021;12:20406223211042544. doi: 10.1177/20406223211042542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Alessi J., de Oliveira G.B., Franco D.W., Brino do Amaral B., Becker A.S., Knijnik C.P., Kobe G.L., de Carvalho T.R., Telo G.H., Schaan B.D., et al. Mental Health in the Era of COVID-19: Prevalence of Psychiatric Disorders in a Cohort of Patients with Type 1 and Type 2 Diabetes during the Social Distancing. Diabetol. Metab. Syndr. 2020;12:76. doi: 10.1186/s13098-020-00584-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.