Abstract
Background and Objectives: Empathy is an important attribute of a healthy doctor–patient relationship. Although multiple studies have assessed empathy in different countries, little is known about its levels among Saudi residents and its association with perceived stress. Objectives: To assess the levels of empathy and to identify if there is an association with stress in general and across the demographic and training characteristics of residents. Materials and Methods: A cross-sectional questionnaire-based study was carried out from December 2020 to March 2021 among residents training at a tertiary academic center in Riyadh, Saudi Arabia. Empathy and perceived stress were measured using the Jefferson Scale of Empathy (JSE) and the Perceived Stress Scale (PSS). Results: A total of 229 residents participated. The mean JSE score was 105.25 ± 15.35. The mean JSE scores were significantly higher among residents training in pediatrics (mean difference (MD) = 17.35, p < 0.001), family medicine (MD = 12.24, p = 0.007), and medical specialties (MD = 11.11, p = 0.012) when compared with surgical specialties and anesthesia. In addition, residents who worked 1–4 on-calls per month had a higher mean JSE score (MD = 11.23, p = 0.028) compared with those who worked 7 or more on-calls. Lastly, no correlation between empathy and perceived stress was detected in the whole sample (r = −0.007, p = 0.913); however, there was a correlation among residents training in medical specialties (r = −0.245, p = 0.025). Conclusion: Residents in our study had empathy levels comparable with Asian but lower than Western residents. We recommend qualitative studies that explore potential factors that might affect empathy among residents and studying the association between empathy and perceived stress among medical residents. Postgraduate curricula should incorporate interventions that foster a more empathetic doctor–patient relationship.
Keywords: empathy, psychological stress, residency, COVID-19, Saudi Arabia
1. Introduction
Empathy is defined as “a predominantly cognitive (rather than an affective or emotional) attribute that involves an understanding (rather than feeling) of experiences, concerns and perspectives of the patient, combined with a capacity to communicate this understanding, and an intention to help” [1]. Physicians’ empathy has been linked with multiple benefits, such as increased patient satisfaction, better clinical outcomes, and lower rates of complications [2,3]. Residents were found to have lower levels of empathy when they were compared with both first- and second-year medical students and specialists [4,5]. A systematic review that included longitudinal studies conducted on residents in the USA showed a progressive decline in empathy throughout residency years [6]. A later cross-sectional study from the USA showed lower empathy scores among second- and fourth-year residents compared with first-year residents [7]. However, a study conducted in Singapore did not find a difference in empathy levels between residency years [8], and a study from South Korea found higher empathy among fourth-year residents compared with first-year residents [9]. Previous research showed that medical students who had higher empathy were more likely to choose the following specialties for residency training: internal medicine, family medicine, obstetrics and gynecology (ob/gyn), pediatrics, and psychiatry [10]. This finding was replicated in studies measuring empathy levels among physicians including residents in training [1,9]. Generally, previous research on medical students and physicians showed higher empathy scores among females [1]. Considering the studies conducted only on residents, some found higher levels of empathy among females [9,11]; however, other studies did not find any difference between genders [4,7,12,13].
Perceived stress is a common mental health issue among residents in training [14,15]. Residents can face different types of stressors: training-related, work-related, social, and financial [14]. Furthermore, the burden of the COVID-19 pandemic might have exaggerated the effect of previous stressors and be a stressor itself with the concern of acquiring the infection or transmitting it to family members [16]. The association between stress and empathy has previously been studied mainly in medical students and pediatric residents, with conflicting results between positive, negative, or no correlations [17,18,19,20,21]. Authors attributed positive correlations to the fact that students suffering from stress might become more empathetic with others who were suffering, such as patients [18]. Interestingly, Michalec et al. suggested that students might adapt to stress during medical school by becoming less empathetic to decrease their vulnerability to stress [17]. Studies that incorporated interventions to decrease stress among residents reported improvement in empathy levels [22,23,24,25,26,27,28]. Notably, when constructs of empathy were considered, mindfulness-based stress reduction (MBSR) resulted in a significant improvement in perspective taking among residents [24].
Perceived stress, especially occupational stress, has been associated with burnout in general and with the emotional exhaustion and depersonalization constructs of burnout in medical residents [20,29,30,31,32]. On the other hand, multiple studies have been conducted on residents to study the association between empathy and burnout [5,8,9,30,31,33,34,35,36,37]. Some of the studies reported an association between higher empathy and lower overall burnout [5,30,32,37]. Conversely, other studies did not find a similar association [33,35,36]. Looking more closely at the associations between empathy and the constructs of burnout [5,8,9,31,33,34,35], most studies reported a negative correlation between empathy and depersonalization [5,8,9,31]. However, Olson et al. did not find a correlation between empathy and depersonalization [33], and, interestingly, Lafreniere et al. found a positive association between residents’ depersonalization and patients’ ratings of their empathy [34]. Nevertheless, when the association between the emotional exhaustion construct of burnout and empathy in residents was studied, mixed results were reported. For instance, Park et al. and Lee et al. reported a negative correlation [8,9], while Olson et al. and Huang et al. did not find any correlation [31,33].
When empathy levels among medical students from Kingdom of Saudi Arabia (KSA) and Kuwait were assessed, they were found to be lower than their counterparts in Western countries yet similar to medical students from Asian countries [18,38,39]. Abdulkader et al. studied empathy among a small sample (n = 30) of physicians from a single center in Riyadh, KSA; however, they did not report whether they included residents in training or not [40]. Meanwhile, studies that describe levels of empathy among residents in KSA are lacking. In addition, there are few studies that investigated the association between perceived stress and empathy among residents. Therefore, we sought to assess empathy levels among trainees enrolled at residency programs in an academic tertiary medical center in KSA. Furthermore, we aimed to determine if there were associations between empathy levels and perceived stress, stressors, and concern about COVID-19 infection or transmission to residents’ families.
2. Methods
2.1. Study Design and Setting
This was a cross-sectional, online survey that included residents training at King Saud University Medical City (KSUMC), Riyadh, KSA, during the period from December 2020 to March 2021. The KSUMC is a tertiary academic medical city that comprises three hospitals (King Khalid University Hospital, King Abdulaziz University Hospital, and Dental University Hospital).
2.2. Eligibility Criteria and Classification of Specialties
In the present study, eligible participants included residents training in any academic year at KSUMC. Residents were allowed to participate if they were enrolled in clinical specialties that require physical contact with patients. Therefore, residents enrolled in the following residency programs were excluded: anatomical histopathology, hematopathology, medical microbiology, medical biochemistry, pathology, and preventive medicine. Furthermore, interns (i.e., last-year medical students in KSA), dental and pharmacy residents, and fellows were excluded from participation. Ultimately, we obtained a complete list of 597 residents who were eligible for participation from the Postgraduate Medical Education Center at King Saud University. Residents were classified by specialty based on the curricula of their training rotations. Internal medicine and its subspecialties (dermatology, neurology, and psychiatry) were classified as one category (medical), general surgery, anesthesia, and surgical subspecialties (cardiac surgery, neurosurgery, ophthalmology, orthopedics, otorhinolaryngology, pediatric surgery, plastic surgery, urology) as one category (surgical and anesthesia), and emergency medicine and critical care as one category. Lastly, family medicine, ob/gyn, pediatrics, and radiology were kept as they were.
2.3. Research Instruments and Data Collection
We developed a self-administered questionnaire in English using the SurveyMonkey® (Momentive, San Mateo, CA, USA) online platform. The questionnaire comprised 6 parts and 40 items: (1) sociodemographic and residency-related characteristics (five items), including gender, marital status, residency year, specialty, and the specialty in which the resident is currently working; (2) workload characteristics (three items), including the number of on-calls or shifts during the past month and the perceived difference between current workload (during the COVID-19 pandemic) and usual workload before the pandemic; (3) a multiple-response item on the possible stressors (work-related, financial, or social); (4) two Likert-scale items on concern about acquiring COVID-19 and transmitting the infection to family members; (5) the 10-item Perceived Stress Scale (PSS-10) [41]; (6) and the 20-item Jefferson Scale of Empathy (JSE) health professions version [1]. A pilot study was initially conducted with 17 residents (who were not included in the final analysis) to calculate the mean JSE score and to obtain feedback from participants specifically about the ease of access, comprehension, and length of the questionnaire. There were no issues with access or comprehension; however, participants reported that the questionnaire was lengthy; thus, we opted to use the 4-item PSS instead of the 10-item questionnaire [42]. JSE-Health Professions consists of 20 items answered on a 7-point Likert scale. The JSE measures 3 main constructs of empathy, including perspective taking (10 items), compassionate care (8 items), and standing in the patient’s shoes (2 items). The responses were coded from 1 (strongly disagree) to 7 (strongly agree). Ten items were positively worded, and the remaining items were negatively worded. The coding of the negatively worded items was reversed, and a total JSE score was calculated for each participant (ranging from 20 to 140), where higher JSE scores indicated greater empathy [1]. On the other hand, PSS-4 consists of 4 items that measure perceived stress in the past month on a 5-point Likert scale. Responses to items 1 and 4 were coded from 0 (never) to 4 (very often), while items 2 and 3 were reverse-coded. The total score ranged between 0 and 16, and higher scores indicated higher stress levels [41,42].
2.4. Sample Size and Participants’ Recruitment
We calculated the sample size required to detect a significant difference from the results of Lee et al. (mean JSE score 104.9 ± 13.2) utilizing G*Power software version 3.1 (Faul et al., Düsseldorf, Germany). We considered an expected mean JSE score of 101.5 (calculated from our pilot study), a power of 95%, and an α of 0.05 to detect a significant difference. The result was a sample size of 198 participants.
We prepared a message that contained the study rationale and objectives as well as a direct link to the consent form and study questionnaire. This message was shared with residents through their chief resident in their social media groups used for training-related announcements. Lastly, they were reminded of participation twice on a monthly basis.
2.5. Ethical Considerations
Permission to use the JSE-Health Professions was obtained from Thomas Jefferson University (Philadelphia, PA, USA), which allows up to 3 out of the 20 items to be illustrated. PSS 4 and 10 do not require permission to use. Ethical approval was obtained from the institutional review board (IRB) of the College of Medicine at King Saud University (project number: E-20–4998). The objectives of the study were explained to all respondents, and they provided consent prior to their participation. Participation was voluntary, and no self-identifying information was mentioned in the list obtained nor collected in the questionnaire, including name, identification number, phone number, and email. Data were only collected for research purposes and stored on the password-protected computer of the principal investigator.
2.6. Statistical Analysis
Statistical analysis was carried out using the Statistical Package for Social Sciences version 26.0 (IBM Corporation, Armonk, NY, USA). Questionnaires with missing responses to PSS-4 or JSE were excluded. Categorical variables were expressed as frequencies and percentages, whereas means, medians, interquartile ranges (IQR), and standard deviations (SDs) were used to present continuous variables. Cronbach’s alpha was used to measure the internal consistency of PSS-4 and JSE. The differences in PSS-4 and JSE scores across sociodemographic and residency-related characteristics were assessed using a t-test for two independent groups (gender and the marital status) and one-way analysis of variance (ANOVA) for variables with three or more groups. Tukey or Games–Howell post hoc tests were performed on all pairwise multiple comparisons for significantly different groups. Correlations between PSS-4 and JSE scores and continuous or ordinal variables were tested using Pearson’s or Spearman’s correlation tests, respectively. Statistical significance was considered at p < 0.05.
3. Results
3.1. Sociodemographic, Residency-Related, and Workload Characteristics
The number of respondents was 252 residents, which comprises 127.3% of the sample size calculated and 42.2% of the total target population. However, we excluded one participant because his specialty was pathology and 22 participants due to missing primary outcomes (responses to the PSS-4 or JSE scales). Therefore, 229 questionnaires were analyzed. The highest response rate was among family medicine residents (91.5%), followed by medical (50%), pediatrics (45.3%), emergency medicine and critical care (35.9%), ob/gyn (31.6%), surgical (15.3%), and radiology (11.4%). The sample comprised 115 males (50.2%) and 162 single participants (70.7%). Most respondents were enrolled in the following residency programs: medical (32.8%), family medicine (23.6%), and pediatrics (14.8%). During the preceding month, 73.0% of respondents were working on-calls, with 45% working 1–4 on-calls per month. Approximately one-third of the participants (29.7%) indicated that their workload in the preceding month was higher than their usual pre-COVID-19 pandemic workload. The distribution of the sociodemographic, residency-related, and workload characteristics of participating residents is shown in Table 1.
Table 1.
Sociodemographic, residency-related, and workload characteristics of participating residents (n = 229).
| Variable | Category | Frequency | Percentage |
|---|---|---|---|
| Gender | Female | 114 | 49.8 |
| Male | 115 | 50.2 | |
| Marital status | Married | 67 | 29.3 |
| Single | 162 | 70.7 | |
| Specialty | Emergency and critical care | 23 | 10 |
| Family medicine | 54 | 23.6 | |
| Medical | 75 | 32.8 | |
| Obstetrics and gynecology (ob/gyn) | 12 | 5.2 | |
| Pediatrics | 34 | 14.8 | |
| Radiology | 4 | 1.7 | |
| Surgical and anesthesia | 27 | 11.8 | |
| Current rotation | Emergency and critical care | 30 | 13.1 |
| Family medicine | 20 | 8.7 | |
| Medical | 83 | 36.2 | |
| Pediatrics | 17 | 7.4 | |
| Ob/Gyn | 33 | 14.4 | |
| Radiology | 8 | 3.5 | |
| Surgical and anesthesia | 37 | 16.2 | |
| Research | 1 | 0.4 | |
| Residency Year | R1 | 58 | 25.3 |
| R2 | 66 | 28.8 | |
| R3 | 43 | 18.8 | |
| R4 | 57 | 24.9 | |
| R5 | 5 | 2.2 | |
| Number of on-calls in the previous month | No on-calls | 41 | 17.9 |
| 1–4 | 103 | 45.0 | |
| 5–6 | 48 | 21.0 | |
| 7 or more | 16 | 7.0 | |
| Shift work | Yes | 21 | 9.2 |
| No | 208 | 90.8 | |
| Workload during COVID-19 pandemic compared to usual workload | Less than usual | 78 | 34.1 |
| Unaffected | 83 | 36.2 | |
| More than usual | 68 | 29.7 |
3.2. Sources of Stress
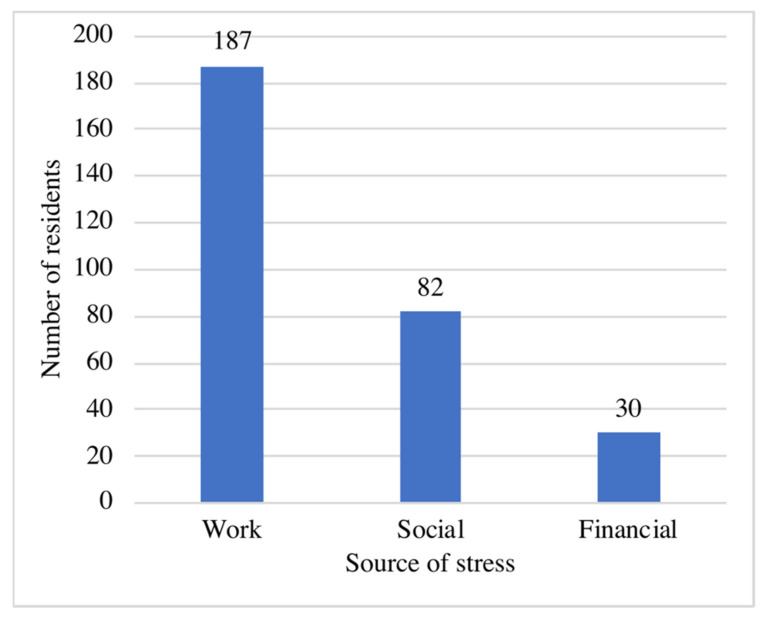
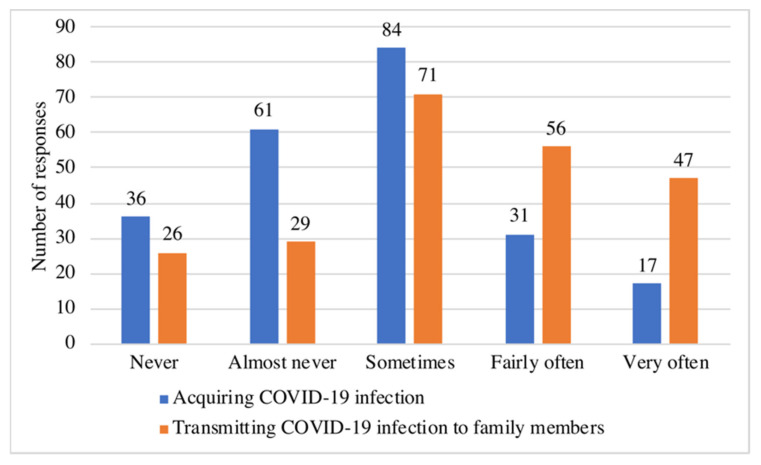
In general, 29 (12.7%) residents reported that they did not have any particular source of stress. On the other hand, the remaining 200 participants selected 296 multiple responses from the available 3 sources of stress. The highest reported source of stress was work-related stress, which was reported by 187 residents (81.7%). Figure 1 illustrates the frequency of sources of stress reported by the residents. Regarding the risk of COVID-19 infection, residents were more concerned about the possibility of transmitting the infection (responding “very often” or “fairly often”) to their families (45.0%) than about acquiring the infection themselves (21%). Figure 2 displays residents’ responses regarding their concerns about COVID-19 infection.
Figure 1.
Frequency of sources of stress reported by the residents (n = 200).
Figure 2.
Residents’ responses regarding their concerns about COVID-19 infection (n = 229).
3.3. Perceived Stress Scale
The Cronbach’s alpha for the PSS-4 was 0.652. The median (IQR) PSS-4 score of all the residents was 7.0 (5.0–9.0). Females and residents who reported having work or social sources of stress had significantly higher mean PSS-4 scores. Moreover, there were medium and small positive correlations between the PSS-4 score and the number of sources of stress reported by the resident and the concerns about both acquiring COVID-19 and transmitting it to family members, respectively. The mean PSS-4 scores and correlation coefficients across the sociodemographic, residency-related, and workload characteristics of residents are shown in Table 2.
Table 2.
Mean scores and correlation coefficients of PSS-4 and JSE scores across the sociodemographic, residency-related, and workload characteristics of residents (n = 229).
| Variable | Category | PSS-4 | JSE | ||
|---|---|---|---|---|---|
| Mean ± SD | p Value † | Mean ± SD | p Value † | ||
| Scores | Whole sample | 7.37 ± 2.72 | NA | 105.25 ± 15.35 | NA |
| Gender | Female | 8.13 ± 2.7 | <0.001 | 107.20 ± 14.83 | 0.055 |
| Male | 6.61 ± 2.53 | 103.31 ± 15.67 | |||
| Marital status | Married | 7.06 ± 2.7 | 0.272 | 106.40 ± 16.05 | 0.466 |
| Single | 7.49 ± 2.72 | 104.77 ± 15.08 | |||
| Specialty | Emergency and critical care | 7.09 ± 3.16 | 0.501 | 97.83 ± 10.38 | <0.001 |
| Family medicine | 7.07 ± 2.49 | 108.09 ± 13.18 | |||
| Medical | 7.2 ± 2.64 | 106.96 ± 14.37 | |||
| Ob/Gyn | 8.17 ± 3.35 | 100.58 ± 19.41 | |||
| Pediatrics | 8.18 ± 2.53 | 113.21 ± 14.09 | |||
| Radiology | 7.75 ± 2.22 | 87.25 ± 7.18 | |||
| Surgical and anesthesia | 7.22 ± 2.97 | 95.85 ± 17.54 | |||
| Current rotation | Emergency and critical care | 6.70 ± 2.97 | 0.154 | 102.93 ± 14.58 | 0.002 |
| Family medicine | 7.15 ± 2.58 | 107.70 ± 12.97 | |||
| Medical | 7.20 ± 2.54 | 105.96 ± 14.05 | |||
| Ob/Gyn | 8.18 ± 3.03 | 99.47 ± 16.96 | |||
| Pediatrics | 8.45 ± 2.56 | 114.15 ± 13.27 | |||
| Radiology | 7.25 ± 2.19 | 100.75 ± 18.11 | |||
| Surgical and anesthesia | 7.11 ± 2.93 | 99.92 ± 17.40 | |||
| Residency year | R1 | 7.69 ± 2.72 | 0.743 | 103.62 ± 14.17 | 0.032 |
| R2 | 7.5 ± 2.79 | 105.7 ± 15.80 | |||
| R3 | 7.14 ± 2.24 | 104.79 ± 13.67 | |||
| R4 | 7.07 ± 2.88 | 108.37 ± 15.72 | |||
| R5 | 7.2 ± 4.02 | 80.6 ± 21.7 | |||
|
Spearman’s
Correlation |
p value |
Spearman’s
Correlation |
p value | ||
| −0.088 | 0.185 | 0.087 | 0.189 | ||
| Number of on-calls in the previous month | No on-calls | 6.88 ± 2.54 | 0.065 | 104.68 ± 13.62 | 0.042 |
| 1–4 | 7.1 ± 2.72 | 107.8 ± 14.47 | |||
| 5–6 | 8.17 ± 2.75 | 105.1 ± 16.56 | |||
| 7 or more | 7.88 ± 2.31 | 96.56 ± 15.23 | |||
| Shift work in the previous month | Yes | 7.43 ± 3 | 0.913 | 100.81 ± 17.71 | 0.165 |
| No | 7.36 ± 2.7 | 105.7 ± 15.07 | |||
| Workload during the past month compared to pre-pandemic workload | Less than usual | 7.15 ± 2.6 | 0.5 | 102.72 ± 17.61 | 0.2 |
| Unaffected | 7.31 ± 3.1 | 106.64 ± 14.08 | |||
| More than usual | 7.67 ± 2.29 | 106.46 ± 13.83 | |||
| Source of stress | |||||
| Work | Yes | 7.78 ± 2.65 | <0.001 | 104.84 ± 15.6 | 0.396 |
| No | 5.55 ± 2.25 | 107.07 ± 14.22 | |||
| Social | Yes | 8.37 ± 2.66 | <0.001 | 107.41 ± 13.62 | 0.111 |
| No | 6.81 ± 2.6 | 104.04 ± 16.15 | |||
| Financial | Yes | 7.67 ± 2.77 | 0.518 | 105.23 ± 12.35 | 0.995 |
| No | 7.32 ± 2.71 | 105.25 ± 15.78 | |||
| Number of sources of stress | 0 | 4.86 ± 2.01 | <0.001 | 106.48 ± 13.94 | 0.419 |
| 1 | 7.29 ± 2.51 | 103.73 ± 16.84 | |||
| 2 | 8.43 ± 2.49 | 107.57 ± 13.89 | |||
| 3 | 8.12 ± 3.24 | 104.82 ± 11.44 | |||
|
Spearman’s
Correlation |
p value |
Spearman’s
Correlation |
p value | ||
| 0.343 | <0.001 | 0.023 | 0.733 | ||
| The concern of acquiring COVID-19 infection | Never | 6.39 ± 2.36 | 109.14 ± 15.12 | 0.371 | |
| Almost never | 7.56 ± 3.07 | 0.02 | 104.34 ± 15.27 | ||
| Sometimes | 7.12 ± 2.64 | 103.43 ± 15.53 | |||
| Fairly often | 8.45 ± 2.41 | 106 ±12.77 | |||
| Very often | 8 ± 2.35 | 107.88 ± 19.04 | |||
|
Spearman’s
Correlation |
p value |
Spearman’s
Correlation |
p value | ||
| 0.165 | 0.012 | −0.01 | 0.879 | ||
| The concern of transmitting COVID-19 to family members | Never | 5.96 ± 2.13 | 0.024 | 105.23 ± 15.79 | 0.986 |
| Almost never | 7.52 ± 2.73 | 104.97 ± 16.31 | |||
| Sometimes | 7.11 ± 2.79 | 104.62 ± 14.88 | |||
| Fairly often | 7.77 ± 3.07 | 105.30 ± 15.11 | |||
| Very often | 7.96 ± 2.17 | 106.32 ± 16.08 | |||
|
Spearman’s
Correlation |
p value |
Spearman’s
Correlation |
p value | ||
| 0.191 | 0.004 | 0.054 | 0.417 | ||
†t test or one-way analysis of variance (ANOVA).
3.4. Jefferson Scale of Empathy
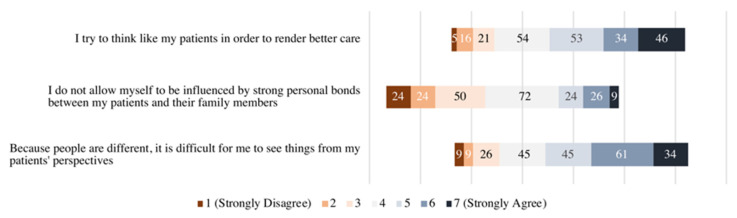
The Cronbach’s alpha for the JSE scale was 0.839. The median (IQR) JSE score of the whole sample was 106.0 (95.0–117.0). The mean scores for the perspective taking, compassionate care, and standing in the patient’s shoes constructs of the JSE were 53.78 ± 10.08, 41.37 ± 7.02, and 10.09 ± 2.48, respectively. The lowest mean scores for an item from the standing in patient’s shoes, perspective taking, and compassionate care constructs were for items 6 (4.86, out of 7), 17 (4.83), and 18 (3.71), respectively. Figure 3 shows a stacked bar chart of residents’ responses to the aforementioned items. The mean JSE score was higher among females compared with males, but the difference was not statistically significant. However, empathy mean scores differed significantly within the categories of residents’ specialty, residency level, and residents’ number of on-calls in the preceding month. Mean scores and correlation coefficients of JSE across the sociodemographic, residency-related, and workload characteristics of residents are shown in Table 2. Subsequently, a post hoc multiple-comparisons test revealed a significant mean JSE score difference between medical and surgical and anesthesia residents, family medicine and surgical and anesthesia, pediatrics and emergency and critical care, radiology, and surgical and anesthesia residents. In addition, fourth-year residents had significantly higher mean JSE scores than fifth-year residents, and residents working one to four on-calls per month had higher JSE score than residents who worked seven or more on-calls. The results of significant post hoc analyses are summarized in Table 3, and the detailed post hoc analyses are supplemented in Appendix A (Table A1, Table A2, Table A3 and Table A4).
Figure 3.
Stacked bar chart of residents’ responses to items 6, 17, and 18 of the JSE (n = 229).
Table 3.
Pairwise comparisons with significant differences in means between categories based on post hoc analysis.*
| Variable | Group 1 | Group 2 | Difference between Groups’ Means | Std. Error | p Value † |
|---|---|---|---|---|---|
| Specialty | Medical | Surgical and anesthesia | 11.11 | 3.22 | 0.012 |
| Family medicine | Surgical and anesthesia | 12.24 | 3.38 | 0.007 | |
| Pediatrics | Emergency and critical care | 15.38 | 3.87 | 0.002 | |
| Radiology | 25.96 | 7.58 | 0.013 | ||
| Surgical and anesthesia | 17.35 | 3.70 | <0.001 | ||
| Current rotation | Pediatrics | Emergency and critical care | 11.22 | 3.76 | 0.048 |
| Ob/Gyn | 14.68 | 4.44 | 0.019 | ||
| Surgical and anesthesia | 14.23 | 3.56 | 0.002 | ||
| Residency year | R4 | R5 | 21.77 | 7.05 | 0.019 |
| Number of on-calls in the past month | 1–4 | 7 or more | 11.23 | 4 | 0.028 |
* Detailed post hoc analyses are supplemented in Appendix A. † Tukey’s multiple-comparisons test.
3.5. Correlation between Empathy and Stress
In the whole sample, PSS-4 score did not correlate with the JSE score (r = −0.007, p = 0.913) or with its constructs: perspective taking (r = −0.003, p = 0.96), compassionate care (r = −0.037, p = 0.568), and standing in patient’s shoes (r = 0.076, p = 0.248). There was a small, nonsignificant, negative correlation (r = −0.146, p = 0.119) between JSE and PSS-4 scores among male residents. There was a small, significant, negative correlation (r = −0.245, p = 0.025) between JSE and PSS-4 scores among residents training in a medical specialty at the time of participation. In addition, there were nonsignificant, moderate positive (r = 0.386, p = 0.126) and negative (r = −0.366, p = 0.373) correlations among residents rotating in ob/gyn and radiology, respectively. Table 4 shows the correlation coefficients across the sociodemographic, residency-related, and workload characteristics of residents.
Table 4.
Correlations between PSS-4 and JSE scores for the whole sample and across sociodemographic and training characteristics (n = 229).
| Variable | Category | PSS-4 and JSE | |
|---|---|---|---|
| Pearson’s Correlation | p Value | ||
| Whole sample | −0.007 | 0.913 | |
| Gender | Male | −0.146 | 0.119 |
| Female | 0.055 | 0.556 | |
| Marital status | Single | −0.06 | 0.446 |
| Married | 0.127 | 0.305 | |
| Specialty | Emergency and critical care | 0.044 | 0.839 |
| Family medicine | 0.019 | 0.893 | |
| Medical | −0.18 | 0.121 | |
| Ob/Gyn | 0.448 | 0.144 | |
| Pediatrics | 0.037 | 0.834 | |
| Radiology | 0.256 | 0.744 | |
| Surgical and anesthesia | −0.125 | 0.534 | |
| Current rotation | Emergency and critical care | −0.018 | 0.925 |
| Family medicine | 0.140 | 0.557 | |
| Medical | −0.245 | 0.025 | |
| Ob/Gyn | 0.386 | 0.126 | |
| Pediatrics | 0.062 | 0.731 | |
| Radiology | −0.366 | 0.373 | |
| Surgical and anesthesia | −0.012 | 0.942 | |
| Residency level | R1 | 0.030 | 0.826 |
| R2 | −0.048 | 0.703 | |
| R3 | −0.079 | 0.613 | |
| R4 | −0.042 | 0.754 | |
| R5 | 0.158 | 0.800 | |
| Number of on-calls in the past month | No on-calls | 0.015 | 0.927 |
| 1–4 | −0.012 | 0.903 | |
| 5–6 | 0.189 | 0.197 | |
| 7 or more | −0.184 | 0.495 | |
| Shift work | Yes | −0.194 | 0.398 |
| Workload during the past month compared to usual workload | Less than usual | −0.013 | 0.910 |
| Unaffected | −0.007 | 0.951 | |
| More than usual | −0.028 | 0.819 | |
4. Discussion
The mean empathy score among residents in our study (105.25) was similar to scores previously reported among medical students (106.55 and 105.18) but lower than that among physicians (111) in KSA [38,39,40]. On the other hand, we did not find a difference in empathy scores between residency years. The only exception was between fourth-year and fifth-year residents, which can be explained by the fact that we had a few (n = 5) fifth-year residents from specialties with low empathy scores, such as surgical and ob/gyn. When taking together, the fact that empathy scores were similar between our study and previous studies of medical students in KSA and that there were no differences between residency years in empathy levels suggests that empathy does not decline in the transition following medical school or throughout the residency years. Although a systematic review of longitudinal studies and a cross-sectional study from the USA suggest a decline in empathy during clinical training [6,7], this was not the case in cross-sectional Singaporean and South Korean studies [8,9]. Therefore, there is a need for a longitudinal study to investigate the changes in empathy among Saudi residents.
When compared with studies conducted among residents in different parts of the world, the mean empathy scores in our study were higher than that for Iranian residents (100.6) [43], generated mixed results compared with Asian countries (104.6, similar to Singapore; higher than South Korea, 93.59; and lower than Japan, 114.46) [8,9,36] and lower than residents in European countries, the USA, and Latin America (111.8–119.1) [5,11,12,13,44,45,46]. Previous research indicated multiple contributors to these differences in empathy levels: first, medical education factors such as the selection of residents and nature of training [47]; second, cultural and social influences on the doctor–patient relationship [1,9]; third, work-related factors such as working hours and on-calls [8,29]; and fourth, study-related factors such as the sampling and timing of data collection. We believe that qualitative studies on residents in KSA will be useful for exploring the factors that negatively affect residents’ empathy.
Females in our study had higher levels of empathy; however, and similar to previous studies [4,7,12,13], the difference was small and did not reach statistical significance. It is not surprising that residents from pediatrics, family medicine, and other medical specialties obtained the highest empathy scores [1,9,10]. On the other hand, and also consistent with the literature, residents from surgical specialties, anesthesia, and radiology achieved the lowest scores [9,10,44]. Interestingly, residents training in emergency medicine and critical care had low scores for empathy. This is inconsistent with previous research [1,9]. Residents in these specialties usually work in shifts, which might partially contribute to their low scores since residents who worked in shifts in our study had lower empathy scores, although these were not statically significant given the small number of shiftwork groups (n = 21). Another potential explanation is that the doctor–patient relationship in emergency medicine and critical care lacks continuity compared with other specialties [4]. Lastly, Passalacqua et al. reported lower empathy levels among residents at the end of the on-calls compared with the start [29]. This might explain why residents who worked seven or more on-calls per month had significantly lower empathy levels than their counterparts with one to four on-calls per month.
We did not find a significant correlation between perceived stress and empathy or its three constructs, including perspective taking. This is similar to previous studies conducted with medical students and pediatric residents that found no associations [17,20,21]. It is possible that the conflicting results of correlation between empathy and stress in different specialties might explain why we did not find a correlation between empathy and stress in the sample as a whole. For instance, the correlation between empathy and stress was negative among residents from medical specialties, while it was positive among ob/gyn residents. Furthermore, these conflicting results between specialties calls for further studies on each individual specialty. The only exception was among residents who were training in medical specialties at the time of participation in this study. Medical rotation is characterized by providing care to adult patients with advanced illness and multiple comorbidities in addition to demanding on-calls that provide little time to sleep or rest [48,49]. There were multiple subgroups with small-to-moderate correlations between stress and empathy that did not reach statistical significance due to relatively small group numbers, such as male residents and residents from the ob/gyn specialty. Those subgroups could be targets of further research investigating the association between perceived stress and empathy. Other items on stress in our study—such as having a work-related or social source of stress, number of stress sources, and COVID-19-related concerns—showed significant associations with PSS-4. However, they did not show any association with empathy.
The present study utilized validated questionnaires for the assessment of stress and empathy. This is the first study that investigated the levels of empathy specifically among Saudi residents in training programs. In addition, it adds to the literature on the association between empathy and perceived stress. This study was conducted during the second wave of the COVID-19 pandemic (Winter 2021), and it reflects the levels of empathy shown during those circumstances.
5. Limitations
This study was carried out in a single training center and used convenience sampling, which might limit the generalizability of the results. The use of a short scale (PSS-4) might have affected the measurement of perceived stress. Due to its cross-sectional design, the study collected data at a single point in time, which might have limited the ability to establish temporal relationships. Lastly, participants from certain specialties (for example radiology) were underrepresented due to low response rates.
6. Conclusions
Residents in our study had empathy levels comparable with those of residents from Asian countries but lower than those of residents from Western countries. We did not find a difference between residency years with regard to empathy levels. Subgroups with lower empathy included residents training in surgical specialties and anesthesia, emergency and critical care, and radiology and residents who worked seven or more on-calls in the past month. There was no correlation between empathy and perceived stress as a whole, but there were correlations within certain subgroups. We recommend the following for further research: longitudinal studies to investigate if there are changes in empathy during training; qualitative studies to explore potential factors that might affect empathy among residents, including on-calls; and studies on the association between empathy and perceived stress among male physicians; and residents training in medical and ob/gyn specialties. Lastly, postgraduate medical education curricula should incorporate interventions that foster a more empathetic doctor–patient relationship.
Acknowledgments
The authors thank the College of Medicine Research Center, Deanship of Scientific Research, King Saud University, Saudi Arabia for their support. Additionally, we thank the participating residents, the Deanship of Scientific Research, and the Researcher Support and Services Unit at King Saud University for their technical support and the Postgraduate Medical Education Center at King Saud University for providing residents lists.
Appendix A. Post Hoc Analyses for Groups with Significant ANOVA Test
Table A1.
Post hoc analysis of the differences in JSE means between residents’ specialties.
| Group 1 | Group 2 | Difference between Groups’ Means | Std. Error | p Value † |
|---|---|---|---|---|
| Medical | Emergency medicine and critical care | 9.13 | 3.42 | 0.111 |
| Family medicine | −1.13 | 2.56 | 0.999 | |
| Ob/Gyn | 6.38 | 4.46 | 0.785 | |
| Pediatrics | −6.25 | 2.97 | 0.353 | |
| Radiology | 19.71 | 7.36 | 0.109 | |
| Surgical and anesthesia | 11.11 | 3.22 | 0.012 | |
| Family medicine | Emergency and critical care | 10.27 | 3.57 | 0.066 |
| Ob/Gyn | 7.51 | 4.58 | 0.657 | |
| Pediatrics | −5.11 | 3.14 | 0.664 | |
| Radiology | 20.84 | 7.43 | 0.079 | |
| Surgical and anesthesia | 12.24 | 3.38 | 0.007 | |
| Pediatrics | Emergency and critical care | 15.38 | 3.87 | 0.002 |
| Ob/Gyn | 12.62 | 4.82 | 0.125 | |
| Radiology | 25.96 | 7.58 | 0.013 | |
| Surgical and anesthesia | 17.35 | 3.70 | <0.001 | |
| Surgical and anesthesia | Emergency and critical care | −1.97 | 4.07 | 0.999 |
| Ob/Gyn | −4.73 | 4.98 | 0.964 | |
| Pediatrics | 8.60 | 7.69 | 0.922 | |
| Emergency and critical care | Ob/Gyn | −2.76 | 5.11 | 0.998 |
| Radiology | 10.58 | 7.77 | 0.822 | |
| Ob/Gyn | Radiology | 13.33 | 8.28 | 0.676 |
† Tukey’s multiple-comparisons test.
Table A2.
Post hoc analysis of the differences in mean JSE scores between residents’ current rotations.
| Group 1 | Group 2 | Difference between Groups’ Means | Std. Error | p Value † |
|---|---|---|---|---|
| Medical | Emergency medicine and critical care | 3.03 | 3.17 | 0.963 |
| Family medicine | −1.74 | 3.71 | 0.999 | |
| Ob/Gyn | 6.49 | 3.96 | 0.658 | |
| Pediatrics | −8.19 | 3.06 | 0.110 | |
| Radiology | 5.21 | 5.51 | 0.965 | |
| Surgical and anesthesia | 6.04 | 2.94 | 0.384 | |
| Family medicine | Emergency and critical care | 4.77 | 4.30 | 0.925 |
| Ob/Gyn | 8.23 | 4.91 | 0.633 | |
| Pediatrics | −6.45 | 4.22 | 0.727 | |
| Radiology | 6.95 | 6.23 | 0.923 | |
| Surgical and anesthesia | 7.78 | 4.13 | 0.494 | |
| Pediatrics | Emergency and critical care | 11.22 | 3.76 | 0.048 |
| Ob/Gyn | 14.68 | 4.44 | 0.019 | |
| Radiology | 13.40 | 5.87 | 0.256 | |
| Surgical and anesthesia | 14.23 | 3.56 | 0.002 | |
| Surgical and anesthesia | Emergency and critical care | −3.01 | 3.66 | 0.982 |
| Ob/Gyn | 0.45 | 4.36 | 1.000 | |
| Pediatrics | −0.83 | 5.81 | 1.000 | |
| Emergency and critical care | Ob/Gyn | 3.46 | 4.52 | 0.988 |
| Radiology | 2.18 | 5.92 | 1.000 | |
| Ob/Gyne | Radiology | −1.28 | 6.38 | 1.000 |
† Tukey’s multiple-comparisons test.
Table A3.
Post hoc analysis of differences in JSE means between different residency levels.
| Group 1 | Group 2 | Difference between Groups’ Means |
Std. Error | p Value † |
|---|---|---|---|---|
| R2 | R1 | 2.08 | 2.72 | 0.941 |
| R3 | 0.91 | 2.96 | 0.998 | |
| R4 | −2.67 | 2.73 | 0.865 | |
| R5 | 19.1 | 7.02 | 0.054 | |
| R1 | R3 | −1.17 | 3.04 | 0.995 |
| R4 | −4.75 | 2.82 | 0.447 | |
| R5 | 17.02 | 7.05 | 0.115 | |
| R4 | R3 | 3.58 | 3.06 | 0.768 |
| R5 | 21.77 | 7.05 | 0.019 | |
| R3 | R5 | 18.19 | 7.15 | 0.084 |
† Tukey’s multiple-comparisons test.
Table A4.
Post hoc analysis of differences in mean JSE score by number of on-calls.
| Group 1 | Group 2 | Difference between Groups’ Means |
Std. Error | p Value † |
|---|---|---|---|---|
| 1–4 on-calls | No on-calls | 3.11 | 2.75 | 0.669 |
| 5–6 on-calls | 2.69195 | 2.59948 | 0.729 | |
| 7 or more on-calls | 11.23 | 4 | 0.028 | |
| 5–6 on-calls | No on-calls | 0.42 | 3.16315 | 0.999 |
| 7 or more on-calls | 8.54 | 4.29384 | 0.195 | |
| No on-calls | 7 or more on-calls | 8.12043 | 4.38452 | 0.252 |
† Tukey’s multiple comparisons test.
Author Contributions
Conceptualization, H.I.A. and M.N.A.; methodology, H.I.A., M.N.A. and M.A.; resources, H.I.A. and M.N.A.; investigation, H.I.A., M.N.A. and M.A.; data curation, H.I.A. and M.N.A.; formal analysis, H.I.A., M.N.A., M.A. and K.O.A.; writing—original draft preparation, H.I.A., M.N.A., M.A., K.O.A., A.A.A. and S.M.A.; writing—review and editing, H.I.A., A.A.A., S.M.A. and M.A.B.; visualization, H.I.A. and M.N.A.; supervision, H.I.A.; funding acquisition, H.I.A. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of the College of Medicine at King Saud University, Riyadh, Saudi Arabia (Project number: E-20–4998, 1 December 2020).
Informed Consent Statement
Informed consent was obtained from all the subjects involved in the study.
Data Availability Statement
Data can be requested from the principal investigator.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by the College of Medicine Research Center, Deanship of Scientific Research, King Saud University, Saudi Arabia.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hojat M. Empathy in Health Professions Education and Patient Care. 1st ed. Springer International Publishing; Cham, Switzerland: 2016. [Google Scholar]
- 2.Han J.L., Pappas T.N. A Review of Empathy, Its Importance, and Its Teaching in Surgical Training. J. Surg. Educ. 2018;75:88–94. doi: 10.1016/j.jsurg.2017.06.035. [DOI] [PubMed] [Google Scholar]
- 3.Walsh S., O’Neill A., Hannigan A., Harmon D. Patient-Rated Physician Empathy and Patient Satisfaction during Pain Clinic Consultations. Ir. J. Med. Sci. 1971. 2019;188:1379–1384. doi: 10.1007/s11845-019-01999-5. [DOI] [PubMed] [Google Scholar]
- 4.DiLalla L.F., Hull S.K., Dorsey J.K. Effect of Gender, Age, and Relevant Course Work on Attitudes Toward Empathy, Patient Spirituality, and Physician Wellness. Teach. Learn. Med. 2004;16:165–170. doi: 10.1207/s15328015tlm1602_8. [DOI] [PubMed] [Google Scholar]
- 5.Ferreira S., Afonso P., Ramos M.d.R. Empathy and Burnout: A Multicentre Comparative Study between Residents and Specialists. J. Eval. Clin. Pract. 2020;26:216–222. doi: 10.1111/jep.13147. [DOI] [PubMed] [Google Scholar]
- 6.Neumann M., Edelhäuser F., Tauschel D., Fischer M.R., Wirtz M., Woopen C., Haramati A., Scheffer C. Empathy Decline and Its Reasons: A Systematic Review of Studies With Medical Students and Residents. Acad. Med. 2011;86:996–1009. doi: 10.1097/ACM.0b013e318221e615. [DOI] [PubMed] [Google Scholar]
- 7.Hamm B., Karafa M., Yu P.C., Rose S., Neuendorf K. Comparison of Burnout and Empathy Among Millennial and Generation X Residents and Fellows: Associations with Training Level and Race but Not Generation Affiliation. Acad. Psychiatry. 2020;44:388–393. doi: 10.1007/s40596-020-01226-9. [DOI] [PubMed] [Google Scholar]
- 8.Lee P., Loh J., Sng G., Tung J., Yeo K. Empathy and Burnout: A Study on Residents from a Singapore Institution. Singap. Med. J. 2018;59:50–54. doi: 10.11622/smedj.2017096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park C., Lee Y.J., Hong M., Jung C.-H., Synn Y., Kwack Y.-S., Ryu J.-S., Park T.W., Lee S.A., Bahn G.H. A Multicenter Study Investigating Empathy and Burnout Characteristics in Medical Residents with Various Specialties. J. Korean Med. Sci. 2016;31:590. doi: 10.3346/jkms.2016.31.4.590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Newton B.W., Barber L., Clardy J., Cleveland E., O’Sullivan P. Is There Hardening of the Heart During Medical School? Acad. Med. 2008;83:244–249. doi: 10.1097/ACM.0b013e3181637837. [DOI] [PubMed] [Google Scholar]
- 11.Voinescu B.J., Szentagotai A., Coogan A. Residents’ Clinical Empathy: Gender and Specialty Comparisons—A Romanian Study. Acta Med. Acad. 2009;38:11–15. [Google Scholar]
- 12.Grosseman S., Novack D.H., Duke P., Mennin S., Rosenzweig S., Davis T.J., Hojat M. Residents’ and Standardized Patients’ Perspectives on Empathy: Issues of Agreement. Patient Educ. Couns. 2014;96:22–28. doi: 10.1016/j.pec.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 13.Delgado-Bolton R., San-Martín M., Alcorta-Garza A., Vivanco L. Empatía médica en médicos que realizan el programa de formación médica especializada. Estudio comparativo intercultural en España. Aten. Primaria. 2016;48:565–571. doi: 10.1016/j.aprim.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alosaimi F.D., Kazim S.N., Almufleh A.S., Aladwani B.S., Alsubaie A.S. Prevalence of Stress and Its Determinants among Residents in Saudi Arabia. Saudi Med. J. 2015;36:605–612. doi: 10.15537/smj.2015.5.10814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soares D.S., Chan L. Stress and Wellbeing of Junior Doctors in Australia: A Comparison with American Doctors and Population Norms. BMC Med. Educ. 2016;16:183. doi: 10.1186/s12909-016-0693-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Temsah M.-H., Al-Sohime F., Alamro N., Al-Eyadhy A., Al-Hasan K., Jamal A., Al-Maglouth I., Aljamaan F., Al Amri M., Barry M., et al. The Psychological Impact of COVID-19 Pandemic on Health Care Workers in a MERS-CoV Endemic Country. J. Infect. Public Health. 2020;13:877–882. doi: 10.1016/j.jiph.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Michalec B. An Assessment of Medical School Stressors on Preclinical Students’ Levels of Clinical Empathy. Curr. Psychol. 2010;29:210–221. doi: 10.1007/s12144-010-9081-y. [DOI] [Google Scholar]
- 18.Hasan S., Al-Sharqawi N., Dashti F., AbdulAziz M., Abdullah A., Shukkur M., Bouhaimed M., Thalib L. Level of Empathy among Medical Students in Kuwait University, Kuwait. Med. Princ. Pract. 2013;22:385–389. doi: 10.1159/000348300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park K.H., Kim D., Kim S.K., Yi Y.H., Jeong J.H., Chae J., Hwang J., Roh H. The Relationships between Empathy, Stress and Social Support among Medical Students. Int. J. Med. Educ. 2015;6:103–108. doi: 10.5116/ijme.55e6.0d44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reed S., Kemper K.J., Schwartz A., Batra M., Staples B.B., Serwint J.R., McClafferty H., Schubert C.J., Wilson P.M., Rakowsky A., et al. Variability of Burnout and Stress Measures in Pediatric Residents: An Exploratory Single-Center Study From the Pediatric Resident Burnout–Resilience Study Consortium. J. Evid.-Based Integr. Med. 2018;23:2515690X1880477. doi: 10.1177/2515690X18804779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wahjudi J.W., Findyartini A., Kaligis F. The Relationship between Empathy and Stress: A Cross-Sectional Study among Undergraduate Medical Students. Korean J. Med. Educ. 2019;31:215–226. doi: 10.3946/kjme.2019.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoenders H.J.R., Booij S.H., Knegtering H., van den Brink H. Mindfulness training for psychiatrists in residency: A pilot study. Tijdschr. Voor Psychiatr. 2016;58:809–813. [PubMed] [Google Scholar]
- 23.Runyan C., Savageau J.A., Potts S., Weinreb L. Impact of a Family Medicine Resident Wellness Curriculum: A Feasibility Study. Med. Educ. Online. 2016;21:30648. doi: 10.3402/meo.v21.30648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Verweij H., van Ravesteijn H., van Hooff M.L.M., Lagro-Janssen A.L.M., Speckens A.E.M. Mindfulness-Based Stress Reduction for Residents: A Randomized Controlled Trial. J. Gen. Intern. Med. 2018;33:429–436. doi: 10.1007/s11606-017-4249-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bentley P.G., Kaplan S.G., Mokonogho J. Relational Mindfulness for Psychiatry Residents: A Pilot Course in Empathy Development and Burnout Prevention. Acad. Psychiatry. 2018;42:668–673. doi: 10.1007/s40596-018-0914-6. [DOI] [PubMed] [Google Scholar]
- 26.Speckens A., Verweij H., van Ravesteijn H., Lagro-Janssen T. Mindfulness for medical, surgical and psychiatric residents. Tijdschr. Voor Psychiatr. 2019;61:188–193. [PubMed] [Google Scholar]
- 27.Quinn M.A., Grant L.M., Sampene E., Zelenski A.B. A Curriculum to Increase Empathy and Reduce Burnout. WMJ Off. Publ. State Med. Soc. Wis. 2020;119:258–262. [PubMed] [Google Scholar]
- 28.Fendel J.C., Aeschbach V.M., Schmidt S., Göritz A.S. The Impact of a Tailored Mindfulness-based Program for Resident Physicians on Distress and the Quality of Care: A Randomised Controlled Trial. J. Intern. Med. 2021;290:1233–1248. doi: 10.1111/joim.13374. [DOI] [PubMed] [Google Scholar]
- 29.Passalacqua S.A., Segrin C. The Effect of Resident Physician Stress, Burnout, and Empathy on Patient-Centered Communication During the Long-Call Shift. Health Commun. 2012;27:449–456. doi: 10.1080/10410236.2011.606527. [DOI] [PubMed] [Google Scholar]
- 30.McClafferty H., Brooks A., Chen M.-K., Brenner M., Brown M., Esparham A., Gerstbacher D., Golianu B., Mark J., Weydert J., et al. Pediatric Integrative Medicine in Residency Program: Relationship between Lifestyle Behaviors and Burnout and Wellbeing Measures in First-Year Residents. Children. 2018;5:54. doi: 10.3390/children5040054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang L., Caspari J.H., Sun X., Thai J., Li Y., Chen F., Zhao X. Risk and Protective Factors for Burnout among Physicians from Standardized Residency Training Programs in Shanghai: A Cross-Sectional Study. BMC Health Serv. Res. 2020;20:965. doi: 10.1186/s12913-020-05816-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kemper K.J., Schwartz A., Wilson P.M., Mahan J.D., Schubert C.J., Staples B.B., McClafferty H., Serwint J.R., Batra M. Pediatric Resident Burnout-Resilience Study Consortium Burnout in Pediatric Residents: Three Years of National Survey Data. Pediatrics. 2020;145:e20191030. doi: 10.1542/peds.2019-1030. [DOI] [PubMed] [Google Scholar]
- 33.Olson K., Kemper K.J., Mahan J.D. What Factors Promote Resilience and Protect Against Burnout in First-Year Pediatric and Medicine-Pediatric Residents? J. Evid.-Based Complement. Altern. Med. 2015;20:192–198. doi: 10.1177/2156587214568894. [DOI] [PubMed] [Google Scholar]
- 34.Lafreniere J.P., Rios R., Packer H., Ghazarian S., Wright S.M., Levine R.B. Burned Out at the Bedside: Patient Perceptions of Physician Burnout in an Internal Medicine Resident Continuity Clinic. J. Gen. Intern. Med. 2016;31:203–208. doi: 10.1007/s11606-015-3503-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chaukos D., Chad-Friedman E., Mehta D.H., Byerly L., Celik A., McCoy T.H., Denninger J.W. Risk and Resilience Factors Associated with Resident Burnout. Acad. Psychiatry. 2017;41:189–194. doi: 10.1007/s40596-016-0628-6. [DOI] [PubMed] [Google Scholar]
- 36.Nishimura Y., Miyoshi T., Obika M., Ogawa H., Kataoka H., Otsuka F. Factors Related to Burnout in Resident Physicians in Japan. Int. J. Med. Educ. 2019;10:129–135. doi: 10.5116/ijme.5caf.53ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wolfshohl J.A., Bradley K., Bell C., Bell S., Hodges C., Knowles H., Chaudhari B.R., Kirby R., Kline J.A., Wang H. Association between Empathy and Burnout among Emergency Medicine Physicians. J. Clin. Med. Res. 2019;11:532–538. doi: 10.14740/jocmr3878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ayuob N., AlHarthi M., Alahmadi G., Bokhary D., Deek B. Is the Empathy Level of Medical Students at KAU Changeable along Their Study Years? What Is behind This Change? Med. Sci. Int. Med. J. 2016;5:484. doi: 10.5455/medscience.2016.05.8402. [DOI] [Google Scholar]
- 39.Iqbal M.Z., Riyadh AlBuraikan A., Abdullah AlQarni A., Abdulaziz AlQahtani H., Mohammad AlOhali A., Mohammed AlMusaileem M. Measuring Empathy in Medical Students: A Cross-Sectional Study. J. Pak. Med. Assoc. 2022;72:1101–1105. doi: 10.47391/JPMA.3226. [DOI] [PubMed] [Google Scholar]
- 40.Abdulkader R.S., Venugopal D., Jeyashree K., Al Zayer Z., Senthamarai Kannan K., Jebitha R. The Intricate Relationship Between Client Perceptions of Physician Empathy and Physician Self-Assessment: Lessons for Reforming Clinical Practice. J. Patient Exp. 2022;9:237437352210775. doi: 10.1177/23743735221077537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cohen S., Kamarck T., Mermelstein R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983;24:385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 42.Cohen S. The Social Psychology of Health. The Claremont Symposium on Applied Social Psychology; Sage Publications, Inc; Thousand Oaks, CA, USA: 1988. Perceived Stress in a Probability Sample of the United States; pp. 31–67. [Google Scholar]
- 43.Shariat S.V., Kaykhavoni A. Empathy in Medical Residents at Iran University of Medical Sciences. Iran. J. Psychiatry Clin. Psychol. 2010;16:248–256. [Google Scholar]
- 44.Hojat M., Mangione S., Nasca T.J., Cohen M.J.M., Gonnella J.S., Erdmann J.B., Veloski J., Magee M. The Jefferson Scale of Physician Empathy: Development and Preliminary Psychometric Data. Educ. Psychol. Meas. 2001;61:349–365. doi: 10.1177/00131640121971158. [DOI] [Google Scholar]
- 45.Glaser K.M., Markham F.W., Adler H.M., McManus R.P., Hojat M. Relationships between Scores on the Jefferson Scale of Physician Empathy, Patient Perceptions of Physician Empathy, and Humanistic Approaches to Patient Care: A Validity Study. Med. Sci. Monit. 2007;13:CR291–CR294. [PubMed] [Google Scholar]
- 46.Fernández-Olano C., Montoya-Fernández J., Salinas-Sánchez A.S. Impact of Clinical Interview Training on the Empathy Level of Medical Students and Medical Residents. Med. Teach. 2008;30:322–324. doi: 10.1080/01421590701802299. [DOI] [PubMed] [Google Scholar]
- 47.Kataoka H.U., Koide N., Ochi K., Hojat M., Gonnella J.S. Measurement of Empathy among Japanese Medical Students: Psychometrics and Score Differences by Gender and Level of Medical Education. Acad. Med. 2009;84:1192–1197. doi: 10.1097/ACM.0b013e3181b180d4. [DOI] [PubMed] [Google Scholar]
- 48.Bellini L.M., Shea J.A. Mood Change and Empathy Decline Persist during Three Years of Internal Medicine Training. Acad. Med. 2005;80:164–167. doi: 10.1097/00001888-200502000-00013. [DOI] [PubMed] [Google Scholar]
- 49.McFarland D.C., Malone A.K., Roth A. Acute Empathy Decline among Resident Physician Trainees on a Hematology-Oncology Ward: An Exploratory Analysis of House Staff Empathy, Distress, and Patient Death Exposure: Acute Empathy Decline. Psychooncology. 2017;26:698–703. doi: 10.1002/pon.4069. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data can be requested from the principal investigator.