Abstract
Increasing prevalence of A. baumannii was found in the faecal samples of inpatients without infection caused by A. baumannii (0.15%; 55/7806). The aim of the study was to determine whether there is a relationship between the clinical strains and the increased faecal occurrence. Characteristics of faecal and clinical isolates were compared between 2017 and 2019, and the direction of causality was assessed by Granger causality tests. In the case of the antibiotic resistance, faecal carriage of carbapenem-resistant Acinetobacter baumannii (CRAb) was Granger-caused by prevalence of CRAb in inpatients (F = 15.84, p < 0.001), but inpatient prevalence was not Granger-caused by CRAb faecal carriage (F = 0.03, p = 0.855). Whole genomes of 16 faecal isolates were sequenced by Illumina MiSeq; cgMLST types were determined. In faecal isolates, the occurrence of carbapenem resistance was lower than among the clinical isolates from the same period; only blaOXA-72 harbouring ST636 and ST492 were detected, and the blaOXA-23 harbouring ST2 and ST49 strains previously dominant in clinical isolates were absent. Carriage of blaOXA-72 was linked to pMAL-1-like and pA105-2-like plasmids in ST636 and ST492 isolates, respectively, both in clinical and faecal isolates. The new ST636 and ST492 strains may colonise the gut microbiota of the patients, which thus may play a role as a reservoir.
Keywords: asymptomatic carriage, resistance reservoir, microbiota, class D carbapenemase
1. Introduction
Healthcare-associated infections (HCAI) are among the most important emerging threats worldwide [1,2,3]. It is estimated that the number of deaths associated with multidrug-resistant (MDR) pathogens could reach 10 million by 2050, and the cost for control of resistance can reach USD 2.9 billion in the United States [1,4,5]. Moreover, the HCAIs caused by MDR bacteria are a major burden on the health care system; for example, ventilator-associated pneumonia lengthened the hospital stay by 9.1 and 38.7 bed-days in adult and neonatal intensive-care units (ICUs), respectively [6]. One of the major sources of HCAIs is the patient’s own microbiota; the intestinal microbiome is considered an important reservoir for these drug-resistant microorganisms and plays a crucial role not solely in the spread of antimicrobial-resistant strains but also acts as a hidden reservoir for genes conferring antibiotic resistance [7,8,9]. The rate of asymptomatic colonization of the gastrointestinal tract by extended-spectrum β-lactamase- (ESBL-) producing bacteria can reach 14% globally [10,11,12,13]; The colonisation with carbapenem-resistant Enterobacterales occurs less frequently (<10%) than with ESBL producers but shows an increasing rate [13].
Epidemiological studies indicate that MDR A. baumannii carriage rates are significantly lower compared to that of MDR Enterobacterales or enterococci as the latter are often part of the normal microbiota of healthy individuals, while A. baumannii is mainly environmental and rarely found in the intestinal tract of persons without prior hospital admission. However, intestinal colonisation, when present, may serve as an infectious source for the colonised or other patients. As carbapenem-resistant A. baumannii (CRAb) is a major agent in HCAI, faecal carriage of CRAb and its role in the strain dynamics of CRAb are worthy of attention [14].
Our working group has been following up the molecular epidemiology of CRAb clinical isolates since 2010 in the university [15,16]; the (ST2; ST49) dominant in the first part of the study period were replaced by blaOXA-72 producers (ST636, ST492) in 2016–2017. The present study investigates the prevalence and antibiotic resistance of the faecal A. baumannii isolates collected between January 2017 and April 2019 in order to characterise the role of faecal CRAb carriage in their molecular epidemiology in comparison with contemporary clinical isolates from 2017.
2. Results
2.1. Prevalence, Susceptibility Testing and Resistance Genes
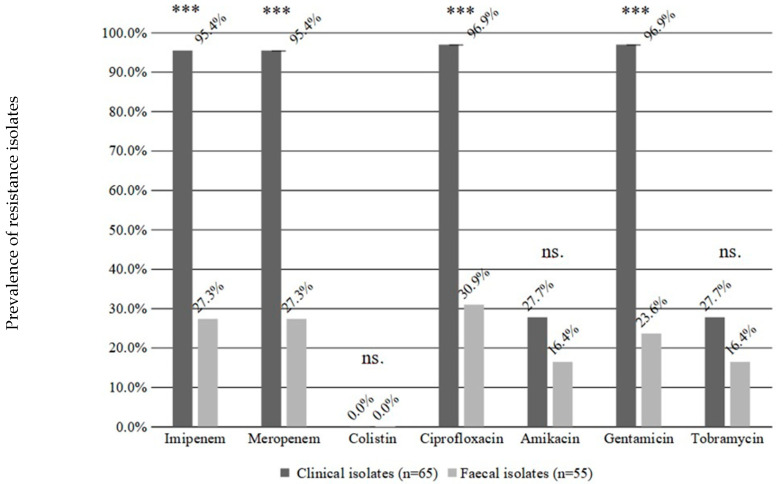
In an earlier study period (2011–2013) of faecal carriage only one A. baumannii isolate was found in 5862 faecal samples (0.02%), while between January 2017 and April 2019, 7806 faecal samples were investigated, and 55 A. baumannii isolates (0.15%) were found in the faecal samples of inpatients, which is an order of magnitude higher than detected earlier. Other samples available from these carriers were negative for A. baumannii. Out of these 55 isolates, 30 originated from paediatric, 15 from internal medicine and 10 isolates from other wards; 15 of these 55 were resistant to imipenem and meropenem (CRAb), 17 to ciprofloxacin, 9 to amikacin and tobramycin and 13 to gentamicin. (Figure 1). None of the CRAb isolates originated from the faecal samples of paediatric patients. The blaOXA-40-like carbapenemase was found in 19 isolates, curiously, four carbapenem-susceptible isolates harboured a blaOXA-40-like gene. The earlier frequent blaOXA-23-like carbapenemases were absent, except for two isolates co-carrying blaOXA-23-like together with a blaOXA-40-like genes.
Figure 1.
Comparison of resistance phenotypes between faecal and clinical isolates for different antibiotics. The percentages show the prevalence of resistant isolates (Y axis). Significance levels: *** p < 0.001; ns. not significant. Result of the clinical isolates from our previous work [16].
2.2. Whole Genome Sequencing (WGS)
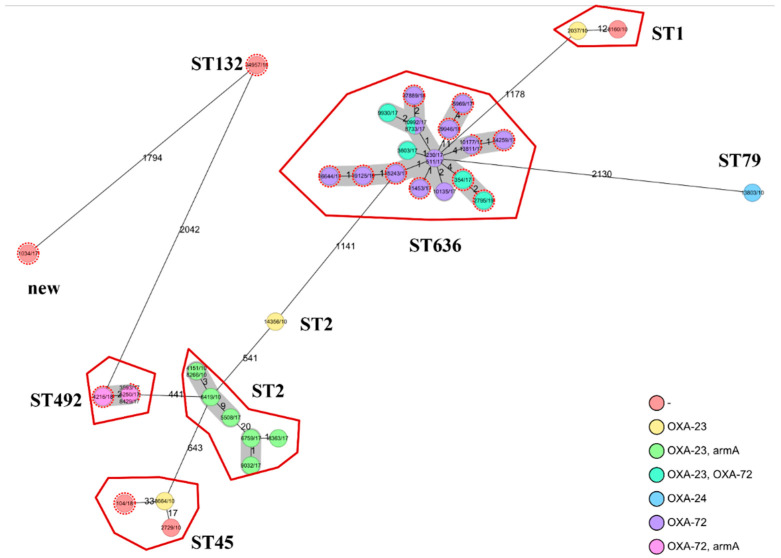
Among the sequenced 16 faecal isolates, only blaOXA-72 harbouring ST636 (n = 11) and ST492 (n = 2) were detected; two ST636 isolates carried blaOXA-72 and blaOXA-23 simultaneously (Table 1). Further investigation of the environment of the blaOXA-72 gene revealed that the ST636 and ST492 isolates carry pMAL-1-like and pA105-2-like plasmids, respectively. Only three isolates belonged to other STs; the aac(6′)-Ib-cr and blaOXA-120 (blaOXA-51-like) carrier ST132, the blaOXA-20 (blaOXA-51-like) carrier ST45 isolate and the blaOXA-106 (blaOXA-51-like) carrier isolate belonging to a novel sequence type (Table 1.). The WGS confirmed that both faecal and clinical ST636 isolates are genetically very close to each other, with only <= 4 alleles distance detected (Figure 2).
Table 1.
The findings of whole genome sequencing antibiotic susceptibility testing of selected isolates and the relation between Acinetobacter baumannii sequence types and acquired carbapenemases.
| Isolate | Year | ST | Acquired CHDLs |
Resistance Phenotype | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| IMP | MEM | COL | CIP | AMN | GMN | TMN | ||||
| ab61 Ac.No.: SRX14056986 |
2017 | new | None | S | S | S | R | S | S | S |
| ab64 Ac.No.: SRX14056995 |
2017 | 492 | blaOXA-72 | R | R | S | R | R | R | R |
| ab65 Ac.No.: SRX14056996 |
2017 | 636 | blaOXA-72 | R | R | S | R | S | R | S |
| ab66 Ac. No.: SRX14056997 |
2017 | 636 | blaOXA-72 | S | S | S | R | R | S | R |
| ab67 Ac.No.: SRX14056998 |
2017 | 636 | blaOXA-72 | R | R | S | R | S | R | S |
| ab68 Ac.No.: SRX14056999 |
2017 | 636 | blaOXA-72 | R | R | S | R | S | S | S |
| ab69 Ac.No.: SRX14057000 |
2017 | 636 | blaOXA-72 | R | R | S | S | S | S | S |
| ab71 Ac.No.: SRX14056988 |
2017 | 636 | blaOXA-72 | R | R | S | R | S | R | S |
| ab72 Ac.No.: SRX14056989 |
2017 | 636 | blaOXA-23 blaOXA-72 |
R | R | S | R | R | R | R |
| ab73 Ac.No.: SRX14056990 |
2017 | 636 | blaOXA-72 | R | R | S | R | S | R | S |
| ab74 Ac.No.: SRX14056991 |
2017 | 636 | blaOXA-72 | R | R | S | R | R | R | R |
| ab75 Ac.No.: SRX14056992 |
2017 | 636 | blaOXA-72 | R | R | S | R | S | R | S |
| ab60 Ac.No.: SRX14056985 |
2018 | 45 | None | S | S | S | R | R | S | R |
| ab63 Ac.No.: SRX14056994 |
2018 | 492 | blaOXA-72 | R | R | S | R | R | R | R |
| ab70 Ac.No.: SRX14056987 |
2018 | 132 | None | S | S | S | S | S | S | S |
| ab62 Ac.No.: SRX14056993 |
2019 | 636 | blaOXA-23 blaOXA-72 |
R | R | S | R | R | R | R |
IMP = imipenem; MEM = meropenem; COL = colistin; CIP = ciprofloxacin; AMN = amikacin; GMN = gentamicin; TMN = tobramycin; R = resistant; S = susceptible Ac.No. = accession number; ST = sequence type; CHDLs = carbapenem hydrolysing class D β-lactamase.
Figure 2.
Minimum spanning tree based on cgMLST allelic profiles of A. baumannii isolates. Each circle represents an allelic profile based on sequence analysis of 2390 cgMLST target genes. Circles with dashed lines represent the faecal isolates, while the solid-contoured circles show the clinical isolates, colour-grouped by genotype. The numbers on the connecting lines illustrate the number of allelic differences. Closely related genotypes (<10 allelic differences based on presence-absence) are shaded. The cgMLST data of the clinical isolates were derived from our previous study [16].
2.3. Comparison of Faecal and Clinical Isolates
The resistance rate among clinical isolates from 2017 were significantly higher to imipenem (95.4% vs. 27.3%; p < 0.001), meropenem (95.4% vs. 27.3%; p < 0.001), ciprofloxacin (96.9% vs. 30.9%; p < 0.001) and gentamicin (96.9% vs. 23.6%; p < 0.001) (Figure 1). This difference was not significant in the case of amikacin and tobramycin, but the resistance rates to these antibiotics were also higher in clinical isolates (Figure 1).
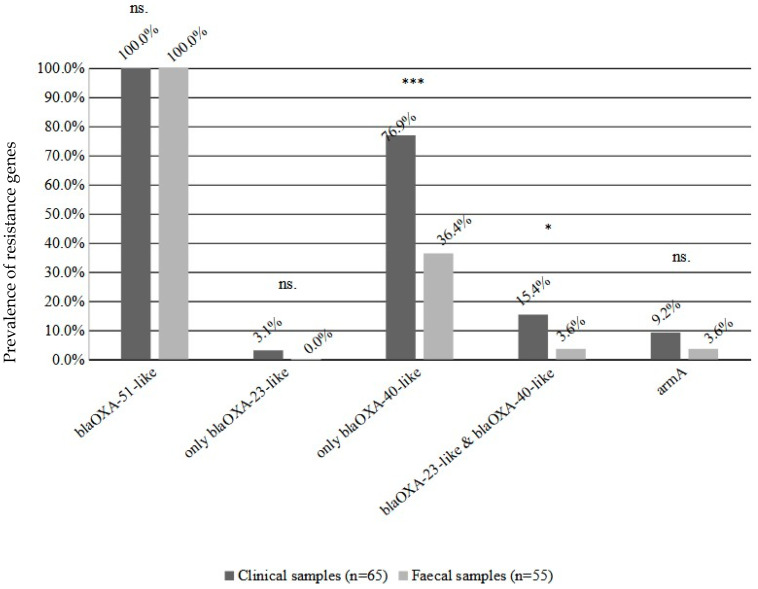
Prevalence of the blaOXA-40-like carbapenemase genes were significantly higher in clinical A. baumannii isolates (76.9% vs. 36.4; p < 0.001), two isolates carried only the blaOXA-23-like gene, while in the faecal isolates there were no strains carrying only the blaOXA-23-like carbapenemase. The proportion of isolates carrying two carbapenemases was also significantly higher among clinical isolates (15.4% vs. 3.6%; p < 0.05) (Figure 3). There was no significant difference for the aminoglycoside resistance armA gene (9.2% vs. 3.6%) (Figure 3).
Figure 3.
The prevalence of resistance genes among the clinical and faecal A. baumannii isolates. The percentages show the prevalence rate among the isolates (Y axis). Significance levels: * p < 0.05; *** p < 0.001; ns not-significant. The results of clinical isolates from our previous work [16].
The minimum inhibitory concentrations (MICs) of imipenem and meropenem were uniformly >32 mg/L in case of CRAb isolates. The time-kill analysis showed that there is no difference between the faecal and clinical strains in growth dynamics in the presence of carbapenems (data not shown). Meropenem was bactericidal at 128 mg/L in the case of ST492 isolates, but a bactericidal effect was never found against ST636, neither against isolates carrying blaOXA-72 nor against isolates with both blaOXA-72 and blaOXA-23. Imipenem was bactericidal at 256 mg/L against all investigated isolates.
The blaOXA-72 carriage was linked to pMAL-1-like and pa105-2-like plasmids in ST636 and to ST492 isolates both in clinical and faecal isolates, and in one clinical isolate we found a complete pMAL-1 plasmid (GeneBank ID: KX230793.1) as a single contig with 99.99% identity. The blaOXA-23 gene was linked to Tn2008 (GeneBank ID: LN877214.1) transposon in all cases.
Faecal carriage of CRAb was Granger-caused by prevalence of CRAb in inpatients (F = 15.84, p < 0.001), but inpatient prevalence was not Granger-caused by CRAb faecal carriage (F = 0.03, p = 0.855). In contrast, neither faecal carriage of carbapenem-susceptible A. baumannii was Granger-caused by prevalence of carbapenem-susceptible A. baumannii in inpatients (F = 2.15, p = 0.155) nor vice versa (F = 0.13, p = 0.726).
3. Discussion
The study was inspired by the observation that the prevalence of CRAb in faecal samples increased significantly in the study period 2017–1019 compared to 2011–2013 (0.02% vs. 0.15%, p < 0.05; unpublished data). CRAb isolates originated from asymptomatic carriers, inpatients who did not show signs of A. baumannii infection, and it was not detected in any of their other samples. In comparison to the clinical isolates, the in vitro resistance was lower in the faecal A. baumannii isolates than in the clinical isolates in the case of all investigated antibiotics. The results of the WGS showed that only the newly appeared STs (ST636, ST492) could be found among the faecal CRAb isolates.
Several studies report the gut colonisation by CRAb in infected ICU patients, and prevalence rates were usually between 4.8% to 18.3%, but according to Corbella et al. (1996), the colonisation may reach 72.2%, and notably, a relationship was found between colonisation and nosocomial infections in ICUs, increased mortality rate and longer hospitalisation [17,18]. Our results are in concordance with the findings of Dijkshoorn et al., who reported 0.8% and 1.0% prevalence of A. baumannii in healthy individuals [19]. However, data is scant on the occurrence of CRAb among faecal samples of patients not infected by CRAb. Li et al. [20] reported a comparable faecal prevalence of 1.48% (74/5000) in an active surveillance of hospitalised patients using meropenem-containing selective medium, but in this report, it is unclear whether these had infection with A. baumannii or were colonised asymptomatically. The distribution of carbapenemase genes was markedly different between isolates from infectious sites and faecal isolates [20]. Eight, five, two and two A. baumannii isolates out of the sixteen were positive for blaOXA-23-like, blaOXA-40-like, blaVIM and blaNDM genes, respectively, though lack of the blaOXA-51-like gene in three isolates raises the possibility of misidentification in these cases [20].
In our setting, not only the incidence of faecal carriage of A. baumannii increased, but CRAb strains also appeared in the faeces of asymptomatic adult, but not paediatric, carriers. Faecal colonisation by CRAb, but not by carbapenem-susceptible A. baumannii, seems to be consequent to the prevalence of CRAb infections as indicated by Granger causality analysis. Similarly, colonisation of patients with ESBL-producing bacteria was shown to be consequent to the prevalence of infections earlier in this setting [21]. Accordingly, colonisation of the faecal microbiota seems to occur during hospital stay, which then becomes a risk factor for colonising healthcare personnel, roommates or future room occupants [22].
Furthermore, only the sequence types ST636 and ST492 harbouring blaOXA-72 carbapenemase gene were found, while the previously dominant ST2 isolates carrying blaOXA-23 were absent. This suggests that colonisation ability may be strain-specific, which, besides their higher resistance against meropenem [16], may have contributed to the epidemic success of blaOXA-72 carrying strains [23,24,25], as their worldwide emergence seems to be contemporary to that of ST492 and ST636 [26].
Faecal carriage of multiresistant pathogens is an increasingly recognised problem, which is aggravated by lack of effective methods for eradication from colonised patients. Consequently, screening and isolation of positives patients remain most effective countermeasure against spread [27], necessitating increased infection control activities and allocation of time and resources.
The non-fermenting nosocomial Gram negatives A. baumannii and P. aeruginosa are generally accepted to persist mainly in abiotic reservoirs, such as water pipes or fomites, which is easier to contain using appropriate infection control practices [28,29]. Colonised individuals are thought to play only a minor or negligible role. As evidenced from the example of carbapenem-resistant Enterobacterales (CRE), faecal carriage may seriously hamper the eradication efforts of MDR pathogens from hospitals [30]. Therefore, appearance of CRAb strains with an increased ability to colonise the human gastrointestinal tract is alarming, since such a case will necessitate testing and infection control management of faecal carriage and not only the environmental contamination.
4. Materials and Methods
4.1. Isolates
Faecal samples of inpatients (n = 7806) sent for routine faecal culture between January 2017 and April 2019 at the Clinical Centre of the University of Debrecen were investigated for carriage of multiresistant Gram-negative bacteria. Samples were cultured on eosin-methylene blue agar (Neogen, Lansing, MI, USA) supplemented with 2 mg/L cefotaxime. After identification by matrix-assisted laser desorption/ionisation time-of-flight mass spectrometry (MALDI-TOF-MS) using a Microflex Biotyper (Bruker Daltonics, Billerica, MA, USA), A. baumannii isolates were investigated further. The susceptibility to amikacin, tobramycin, gentamicin, imipenem, meropenem and ciprofloxacin were determined by Kirby–Bauer method according to the European Committee on Antimicrobial Susceptibility Testing (EUCAST) guidelines (v 11.0) [31]; colistin susceptibility testing was performed by microdilution test (Merlin Diagnostics, Bornheim, Germany). Faecal isolates were compared to 65 clinical CRAb isolates (mainly from bronchial, wound and blood samples) collected in 2017 in our previous research [16].
The direction of causality between faecal carriage and isolations from clinical disease was analysed by Granger causality tests. Granger causality test is based on comparing forecast quality of one time-series alone and when including another time series. If the forecast quality is better in the latter case, then the first time-series is Granger caused by the other, indicating a potential causality [32]. We collected the monthly incidence of carbapenem susceptible A. baumannii and CRAb in faecal samples from inpatients and the monthly incidence densities of inpatients infected by carbapenem-susceptible A. baumannii and by CRAb per 100 occupied bed-days between 2017 and 2019. The Granger causality was tested between the respective pairs of time series [33]. Difference in susceptibility and resistance genes prevalence was analysed by chi-square test. The difference in imipenem and meropenem resistance between the clinical and faecal A. baumannii isolates was investigated by time-kill analysis [16].
4.2. Resistance Genes
Based on previous experience, carbapenemases blaOXA-23-like, blaOXA-24/40-like, blaOXA-51-like and the armA aminoglycoside resistance gene were sought by polymerase chain reaction (PCR), as described earlier [16,34,35].
4.3. Whole Genome Sequencing
Based on resistance gene carriage, representative CRAb (n = 13) as well as carbapenem-susceptible (n = 3) isolates were chosen for whole genome sequencing (WGS). The primary consideration for the selection criteria was the resistance gene profile, previously determined by PCR, and we also took into account phenotypic resistance. For isolates with the same resistance profile (genotype and phenotype), the origin of the faecal samples (hospital department) served as an additional criterion. Libraries were prepared with the Nextera DNA Flex library preparation kit (Illumina, San Diego, CA, USA) and sequenced with the MiSeq Reagent Kit v2 (300 cycles, Illumina) on the MiSeq platform (Illumina). The resulting FASTQ files were quality-trimmed before being de novo assembled with the Velvet assembler included in the Ridom SeqSphere+ software (Ridom GmbH, Münster, Germany). The cgMLST analysis was carried out using the Ridom SeqSphere+ software based on the ‘A. baumannii cgMLST’ version 1.0 scheme. The generated raw sequence reads uploaded to NCBI BioProject database (BioProject ID: PRJNA671692). The sequenced faecal isolates were compared to clinical isolates from our previous study (BioProject ID: PRJNA671692). The accession numbers of the faecal isolates are shown in Table 1. The antibiotic resistance genes were sought for in the genomes by ResFinder (v3.9; 90% ID threshold, 60% minimum length) and Comprehensive Antibiotic Resistance Database (CARD, v3.1.4).
Acknowledgments
The isolates and antibiotic susceptibility testing were kindly provided by the Department of Medical Microbiology, Clinical Centre, University of Debrecen.
Author Contributions
Conceptualisation B.B., Á.T. and G.K.; methodology B.B., Z.T. and L.M.; software, B.B., Z.T. and G.K.; validation, Á.T.; formal analysis B.B., Á.T. and G.K.; investigation, B.B., Z.T. and J.B.N.; writing—original draft preparation, B.B. and G.K.; writing—review and editing, B.B., Á.T. and G.K.; supervision G.K.; project administration B.B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The sequences of the bacterial strains were uploaded to the National Center for Biotechnology Information (NCBI) BioProject and BioSample databases. BioProject ID: PRJNA671692.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
The study itself did not receive funding. Zoltán Tóth, and Bence Balázs supported by the EFOP-3.6.3-VEKOP-16-2017-00009 project co-financed by EU and the European Social Fund and supported by the ÚNKP-21-4-I New National Excellence Program of the Ministry for Innovation and Technology from the source of The National Research, Development and Innovation Fund.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ma Y.X., Wang C.Y., Li Y.Y., Li J., Wan Q.Q., Chen J.H., Tay F.R., Niu L.N. Considerations and caveats in combating ESKAPE pathogens against nosocomial infections. Adv. Sci. 2020;7:1901872. doi: 10.1002/advs.201901872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cassini A., Högberg L.D., Plachouras D., Quattrocchi A., Hoxha A., Simonsen G.S., Colomb-Cotinat M., Kretzschmar M.E., Devleesschauwer B., Cecchini M., et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019;19:56–66. doi: 10.1016/S1473-3099(18)30605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rice L.B. Federal funding for the study of antimicrobial resistance in nosocomial pathogens: No ESKAPE. J. Infect. Dis. 2008;197:1079–1081. doi: 10.1086/533452. [DOI] [PubMed] [Google Scholar]
- 4.O’Neill J. Tackling a Crisis for the Health and Wealth of Nations. [(accessed on 24 March 2019)]. Available online: https://amr-review.org/sites/default/files/AMR%20Review%20Paper%20-%20Tackling%20a%20crsis%20for%20the%20health%20and%20wealth%20of%20nations_1.pdf.
- 5.Shrestha P., Cooper B.S., Coast J., Oppong R., Do Thi Thuy N., Phodha T., Celhay O., Guerin P.J., Wertheim H., Lubell Y. Enumerating the economic cost of antimicrobial resistance per antibiotic consumed to inform the evaluation of interventions affecting their use. Antimicrob. Resist. Infect. Control. 2018;7:98. doi: 10.1186/s13756-018-0384-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mehta Y., Jaggi N., Rosenthal V.D., Kavathekar M., Sakle A., Munshi N., Chakravarthy M., Todi S.K., Saini N., Rodrigues C., et al. Device-Associated Infection Rates in 20 Cities of India, Data Summary for 2004–2013: Findings of the International Nosocomial Infection Control Consortium. Infect. Control. Hosp. Epidemiol. 2016;37:172–181. doi: 10.1017/ice.2015.276. [DOI] [PubMed] [Google Scholar]
- 7.Lin M.Y., Lyles-Banks R.D., Lolans K., Hines D.W., Spear J.B., Petrak R., Trick W.E., Weinstein R.A., Hayden M.K., Centers for Disease Control and Prevention Epicenters Program The importance of long-term acute care hospitals in the regional epidemiology of Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2013;57:1246–1252. doi: 10.1093/cid/cit500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hayden M.K., Lin M.Y., Lolans K., Weiner S., Blom D., Moore N.M., Fogg L., Henry D., Lyles R., Thurlow C., et al. Prevention of colonization and infection by Klebsiella pneumoniae carbapenemase-producing enterobacteriaceae in long-term acute-care hospitals. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2015;60:1153–1161. doi: 10.1093/cid/ciu1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shimasaki T., Seekatz A., Bassis C., Rhee Y., Yelin R.D., Fogg L., Dangana T., Cisneros E.C., Weinstein R.A., Okamoto K., et al. Increased Relative Abundance of Klebsiella pneumoniae Carbapenemase-producing Klebsiella pneumoniae Within the Gut Microbiota Is Associated With Risk of Bloodstream Infection in Long-term Acute Care Hospital Patients. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2019;68:2053–2059. doi: 10.1093/cid/ciy796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Juhász J., Ligeti B., Gajdács M., Makra N., Ostorházi E., Farkas F.B., Stercz B., Tóth Á., Domokos J., Pongor S., et al. Colonization Dynamics of Multidrug-Resistant Klebsiella pneumoniae Are Dictated by Microbiota-Cluster Group Behavior over Individual Antibiotic Susceptibility: A Metataxonomic Analysis. Antibiotics. 2021;10:268. doi: 10.3390/antibiotics10030268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lob S.H., Biedenbach D.J., Badal R.E., Kazmierczak K.M., Sahm D.F. Antimicrobial resistance and resistance mechanisms of Enterobacteriaceae in ICU and non-ICU wards in Europe and North America: SMART 2011–2013. J. Glob. Antimicrob. Resist. 2015;3:190–197. doi: 10.1016/j.jgar.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 12.Karanika S., Karantanos T., Arvanitis M., Grigoras C., Mylonakis E. Fecal Colonization With Extended-spectrum Beta-lactamase-Producing Enterobacteriaceae and Risk Factors Among Healthy Individuals: A Systematic Review and Metaanalysis. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2016;63:310–318. doi: 10.1093/cid/ciw283. [DOI] [PubMed] [Google Scholar]
- 13.Qin X., Wu S., Hao M., Zhu J., Ding B., Yang Y., Xu X., Wang M., Yang F., Hu F. The Colonization of Carbapenem-Resistant Klebsiella pneumoniae: Epidemiology, Resistance Mechanisms, and Risk Factors in Patients Admitted to Intensive Care Units in China. J. Infect. Dis. 2020;221:S206–S214. doi: 10.1093/infdis/jiz622. [DOI] [PubMed] [Google Scholar]
- 14.Aljindan R., Bukharie H., Alomar A., Abdalhamid B. Prevalence of digestive tract colonization of carbapenem-resistant Acinetobacter baumannii in hospitals in Saudi Arabia. Pt 4J. Med. Microbiol. 2015;64:400–406. doi: 10.1099/jmm.0.000033. [DOI] [PubMed] [Google Scholar]
- 15.Mózes J., Ebrahimi F., Gorácz O., Miszti C., Kardos G. Effect of carbapenem consumption patterns on the molecular epidemiology and carbapenem resistance of Acinetobacter baumannii. J. Med. Microbiol. 2014;63:1654–1662. doi: 10.1099/jmm.0.082818-0. [DOI] [PubMed] [Google Scholar]
- 16.Balázs B., Tóth Z., Nagy F., Kovács R., Tóth H., Nagy J.B., Tóth Á., Szarka K., Majoros L., Kardos G. The Role of Uniform Meropenem Usage in Acinetobacter baumannii Clone Replacement. Antibiotics. 2021;10:127. doi: 10.3390/antibiotics10020127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Corbella X., Pujol M., Ayats J., Sendra M., Ardanuy C., Dominguez M.A., Linares J., Ariza J., Gudiol F. Relevance of digestive tract colonization in the epidemiology of nosocomial infections due to multiresistant Acinetobacter baumannii. Clin. Infect. Dis. 1996;23:329–334. doi: 10.1093/clinids/23.2.329. [DOI] [PubMed] [Google Scholar]
- 18.Maamar E., Alonso C.A., Ferjani S., Jendoubi A., Hamzaoui Z., Jebri A., Saisani M., Ghedira S., Torres C., Boubaker I.B.B. NDM-1-and OXA-23-producing Acinetobacter baumannii isolated from intensive care unit patients in Tunisia. Int. J. Antimicrob. Agents. 2018;52:910–915. doi: 10.1016/j.ijantimicag.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 19.Dijkshoorn L., Van Aken E., Shunburne L., Van Der Reijden T.J.K., Bernards A.T., Nemec A., Towner K.J. Prevalence of Acinetobacter baumannii and other Acinetobacter spp. in faecal samples from non-hospitalised individuals. Clin. Microbiol. Infect. 2005;11:329–332. doi: 10.1111/j.1469-0691.2005.01093.x. [DOI] [PubMed] [Google Scholar]
- 20.Li S., Duan X., Peng Y., Rui Y. Molecular characteristics of carbapenem-resistant Acinetobacter spp. from clinical infection samples and fecal survey samples in Southern China. BMC Infect. Dis. 2019;19:900. doi: 10.1186/s12879-019-4423-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ebrahimi F., Mózes J., Monostori J., Gorácz O., Fésűs A., Majoros L., Szarka K., Kardos G. Comparison of rates of fecal colonization with extended-spectrum beta-lactamase-producing enterobacteria among patients in different wards, outpatients and medical students. Microbiol. Immunol. 2016;60:285–294. doi: 10.1111/1348-0421.12373. [DOI] [PubMed] [Google Scholar]
- 22.Wohrley J.D., Bartlett A.H. The Role of the Environment and Colonization in Healthcare-Associated Infections. Healthc.-Assoc. Infect. Child. 2018;16:17–36. [Google Scholar]
- 23.Petrović T., Uzunović S., Barišić I., Luxner J., Grisold A., Zarfel G., Ibrahimagić A., Jakovac S., Slaćanac D., Bedenić B. Arrival of carbapenem-hydrolyzing-oxacillinases in Acinetobacter baumannii in Bosnia and Herzegovina. Infect. Genet. Evol. 2018;58:192–198. doi: 10.1016/j.meegid.2017.12.021. [DOI] [PubMed] [Google Scholar]
- 24.Nemec A., Krizova L., Maixnerova M., Musilek M. Multidrug-resistant epidemic clones among bloodstream isolates of Pseudomonas aeruginosa in the Czech Republic. Res. Microbiol. 2010;161:234–242. doi: 10.1016/j.resmic.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 25.Villalón P., Ortega M., Sáez-Nieto J.A., Carrasco G., Medina-Pascual M.J., Garrido N., Valdezate S. Dynamics of a sporadic nosocomial Acinetobacter calcoaceticus–Acinetobacter baumannii complex population. Front. Microbiol. 2019;10:593. doi: 10.3389/fmicb.2019.00593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gheorghe I., Barbu I.C., Surleac M., Sârbu I., Popa L.I., Paraschiv S., Feng Y., Lazar V., Chifiriuc M.C., Oţelea D., et al. Subtypes, resistance and virulence platforms in extended-drug resistant Acinetobacter baumannii Romanian isolates. Sci. Rep. 2021;11:13288. doi: 10.1038/s41598-021-92590-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gniadek T.J., Carroll K.C., Simner P.J. Carbapenem-resistant non-glucose-fermenting Gram-negative bacilli: The missing piece to the puzzle. J. Clin. Microbiol. 2016;54:1700–1710. doi: 10.1128/JCM.03264-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weinberg S.E., Villedieu A., Bagdasarian N., Karah N., Teare L., Elamin W.F. Control and management of multidrug resistant Acinetobacter baumannii: A review of the evidence and proposal of novel approaches. Infect. Prev. Pract. 2020;2:100077. doi: 10.1016/j.infpip.2020.100077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pachori P., Gothalwal R., Gandhi P. Emergence of antibiotic resistance Pseudomonas aeruginosa in intensive care unit; a critical review. Genes Dis. 2019;6:109–119. doi: 10.1016/j.gendis.2019.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gijón D., Curiao T., Baquero F., Coque T.M., Cantón R. Fecal carriage of carbapenemase-producing Enterobacteriaceae: A hidden reservoir in hospitalized and nonhospitalized patients. J. Clin. Microbiol. 2012;50:1558–1563. doi: 10.1128/JCM.00020-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. [(accessed on 1 January 2018)]. Available online: https://www.eucast.org/ast_of_bacteria/previous_versions_of_documents/
- 32.Anil S. Granger causality. Scholarpedia. 2007;2:1667. [Google Scholar]
- 33.Wessa P. Bivariate Granger Causality (v1.0.4) in Free Statistics Software (v1.2.1), Office for Research Development and Education. 2016. [(accessed on 1 January 2022)]. Available online: http://www.wessa.net/rwasp_grangercausality.wasp/
- 34.Naas T., Levy M., Hirschauer C., Marchandin H., Nordmann P. Outbreak of carbapenem-resistant Acinetobacter baumannii producing the carbapenemase OXA-23 in a tertiary care hospital of Papeete, French Polynesia. J. Clin. Microbiol. 2005;43:4826–4829. doi: 10.1128/JCM.43.9.4826-4829.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bogaerts P., Galimand M., Bauraing C., Deplano A., Vanhoof R., De Mendonca R., Rodriguez-Villalobos H., Struelens M., Glupczynski Y. Emergence of ArmA and RmtB aminoglycoside resistance 16S rRNA methylases in Belgium. J. Antimicrob. Chemother. 2007;59:459–464. doi: 10.1093/jac/dkl527. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The sequences of the bacterial strains were uploaded to the National Center for Biotechnology Information (NCBI) BioProject and BioSample databases. BioProject ID: PRJNA671692.