SUMMARY
We describe two cases of infant botulism due to Clostridium butyricum producing botulinum type E neurotoxin (BoNT/E) and a previously unreported environmental source. The infants presented at age 11 days with poor feeding and lethargy, hypotonia, dilated pupils and absent reflexes. Faecal samples were positive for C. butyricum BoNT/E. The infants recovered after treatment including botulism immune globulin intravenous (BIG-IV). C. butyricum BoNT/E was isolated from water from tanks housing pet ‘yellow-bellied’ terrapins (Trachemys scripta scripta): in case A the terrapins were in the infant's home; in case B a relative fed the terrapin prior to holding and feeding the infant when both visited another relative. C. butyricum isolates from the infants and the respective terrapin tank waters were indistinguishable by molecular typing. Review of a case of C. butyricum BoNT/E botulism in the UK found that there was a pet terrapin where the infant was living. It is concluded that the C. butyricum-producing BoNT type E in these cases of infant botulism most likely originated from pet terrapins. These findings reinforce public health advice that reptiles, including terrapins, are not suitable pets for children aged <5 years, and highlight the importance of hand washing after handling these pets.
Key words: Botulism, Clostridium, public health, toxins, zoonoses
INTRODUCTION
Infant botulism may occur in the first year of life due to infection by neurotoxin-producing clostridial organisms which colonize the gastrointestinal tract [1]. Most cases are caused by Clostridium botulinum but C. butyricum and C. baratii have been identified as the causative agent in a small proportion of cases. The potent neurotoxin (eight serological types, A–H) blocks cholinergic synapses, resulting in symptoms ranging from mild hypotonia to severe, flaccid paralysis [1, 2]. Around 100 cases of infant botulism are reported annually in the USA, almost all caused by either type A or type B neurotoxin [3]. Some European countries have reported no cases and others very few [4]. C. butryicum-producing type E toxin is a rare cause of infant botulism. Six cases have been reported worldwide since it was first described in 1984 [5]; additional information is provided below on a seventh case which occurred in the UK [6].
Living in a rural area and having a parent who works with soil have been identified as risk factors [1]. Spores of neurotoxigenic clostridia are present in dust and soil, as documented in about 20% of soil samples in the USA. In general, the type of neurotoxin detected from clostridial organisms in soil matches that which predominates in infant cases in that area [7]. Honey has been identified as a source of C. botulinum spores, including honey which had been ingested by infants who developed botulism [1, 3, 5]. We describe the clinical, laboratory, public health and environmental investigation and management of two cases of infant botulism due to C. butyricum-producing botulinum type E neurotoxin (BoNT/E) in which there was evidence of environmental contamination with an indistinguishable C. butyricum originating from pet terrapins.
CLINICAL HISTORIES
Case A
An 11-day-old boy was admitted to hospital in December 2010. He had a 24-h history of poor feeding and lethargy but no history of fever, vomiting or diarrhoea. His Apgar scores were normal at birth and he was exclusively breast-fed. On admission he had a poor suck and a weak cry, with bilateral ptosis, intermittent roving eye movements and dilated pupils which reacted sluggishly to light. He had an absent gag reflex, was markedly hypotonic, lacked spontaneous limb movements and deep tendon reflexes were absent. He was transferred to the intensive care unit for mechanical ventilation with a working diagnosis of acute encephalitis.
The differential diagnosis included infant botulism and on the infant's third day in hospital a stool sample was sent to the Gastrointestinal Bacteria Reference Laboratory, Public Health England (PHE), at Colindale in London. His clinical condition continuously improved and he was normal on neurological examination when discharged home on day 9. The presence of type E neurotoxigenic clostridia in his stool sample was reported on the day of discharge but as he appeared to have made a full recovery, anti-botulinum treatment was not initiated at this time.
The infant was readmitted 2 days later with a recurrence of symptoms and again required mechanical ventilation. He was treated with trivalent equine botulinum antitoxin ABE and made a full recovery over the next 10 days. Following consultation with the California Department of Public Health Infant Botulism Treatment and Prevention Program (IBTPP), botulism immune globulin intravenous (human) (BIG-IV) was administered to protect against further relapse and he was discharged home well the following day.
Subsequent identification of the isolate from the infant's faeces confirmed the presence of C. butyricum BoNT/E (see sections on Laboratory Methods, Laboratory Results and Table 1 for further information). C. butyricum containing bontE continued to be identified from serial faecal specimens up to 42 days after the first specimen was taken but was not isolated from specimens taken after 47 days.
Table 1.
Results of microbiological investigations of clinical, medicinal and environmental samples for neurotoxigenic clostridia
| Sample | Real-time PCR detection of bont A/B/E/F genes | Culture result |
|---|---|---|
| Case A | ||
| Infant faeces | bontE detected | C. butyricum BoNT/E |
| Mother's faeces | bontE detected | C. butyricum BoNT/E |
| Vitamin drops | Not detected | Neurotoxigenic clostridia not isolated |
| Nipple cream | Not detected | Neurotoxigenic clostridia not isolated |
| Bio-oil | Not detected | Neurotoxigenic clostridia not isolated |
| Tank water | bontE detected | C. butyricum BoNT/E |
| Tank sediment | bontE detected | C. butyricum BoNT/E |
| Turtle food, family home | bontE detected | C. butyricum BoNT/E |
| Turtle food same batch x5, pet store | Not detected | Neurotoxigenic clostridia not isolated |
| Case B | ||
| Infant faeces | bontE detected | C. butyricum BoNT/E |
| Mother's faeces | Not detected | Neurotoxigenic clostridia not isolated |
| Father's faeces | Not detected | Neurotoxigenic clostridia not isolated |
| Infant formula | Not detected | Neurotoxigenic clostridia not isolated |
| Brown sugar | Not detected | Neurotoxigenic clostridia not isolated |
| Goldfish food (opened) | Not detected | Neurotoxigenic clostridia not isolated |
| Goldfish food (unopened) | Not detected | Neurotoxigenic clostridia not isolated |
| Large fish tank: water | Not detected | Neurotoxigenic clostridia not isolated |
| Large fish tank: stones | Not detected | Neurotoxigenic clostridia not isolated |
| Goldfish tank: water | Not detected | Neurotoxigenic clostridia not isolated |
| Goldfish tank: stones | Not detected | Neurotoxigenic clostridia not isolated |
| Terrapin tank: water | bontE detected | C. butyricum BoNT/E |
Case B
Case B had normal Apgar scores after delivery in March 2013 but had three bilious vomits on day 2. An upper gastrointestinal study showed no abnormality and he was discharged on day 3. Breast-fed, he was well until day 10.
He was admitted to the maternity hospital with a 10-h history of poor feeding, constipation and increasing lethargy. He was pale, pupil reactions were sluggish, he had generalized hypotonia but his anterior fontanelle was soft. His breathing became laboured and he started grunting. He was commenced on continuous positive airway pressure (CPAP) ventilation but did not require sedation which was unusual.
When transferred to a paediatric intensive care unit he continued to be hypotonic and had absent reflexes. His pupils were poorly reactive and ophthalmology showed no papilloedema. His chest X-ray showed some lung collapse and there were dilated loops of bowel on plain abdominal X-ray. He was commenced on antibiotics. Lumbar puncture was normal as was a brain MRI and he remained apyrexial throughout.
A diagnosis of botulism was considered and some apnoeic episodes were noted while on CPAP. Electromyography studies were organized on day 2 that were consistent with botulism. Following discussion of the clinical scenario with the IBTPP, equine antitoxin was administered. He was extubated the following day. He became more alert and active, and his tone improved. His pupils however remained dilated and poorly reactive, and although present, his reflexes were difficult to elicit.
On his 6th day in hospital the PHE Reference Laboratory in London reported the presence of type E neurotoxigenic clostridia in his stool sample. BIG-IV was administered on day 9 in view of his ongoing clinical signs and to prevent relapse. He continued to improve and was discharged on day 14. The laboratory confirmed the identity of the clostridial species as C. butyricum by 16S sequencing. On follow-up his development was age appropriate. Stool samples remained positive for C. butyricum BoNT/E for 196 days after initial detection but were negative after collection at 217 days.
In both cases clinicians liaised with public health and environmental health staff, communicating with the family to assess and manage any risks of transmission.
Laboratory methods
Faecal specimens referred to the PHE Reference Laboratory were inoculated into cooked meat broth (CMB). On the day of reception the broths were examined for C. botulinum by real-time PCR detection of bontA/B/E/F genes and subcultured to two pre-reduced cooked meat medium (CMM) enrichment broths with added glucose and starch, one of which was then heat-shocked at 60 °C for 30 min. Enrichment cultures were incubated at either 30 °C or 35 °C for up to 5 days and subcultured onto solid medium with or without antibiotics after incubation for 1, 3 and 5 days [8]. Plates were incubated in an anaerobic cabinet (Don Whitley Scientific, UK) at either 30 °C or 35 °C in an atmosphere of 80% N2, 10% H2 and 10% CO2 for 1–5 days.
Medicinal and environmental products were examined for C. botulinum by enrichment culture as described above. Tests for the presence of C. botulinum bontA/B/E/F genes were performed on day 1 for human faecal specimens inoculated into CMB broth and on days 1, 3 and 5 for samples inoculated into CMM broth. DNA was extracted from broth cultures using InstaGene™ matrix (Bio-Rad, USA) and from individual bacterial colonies using microLYSIS® reagent (Microzone, UK). Real-time PCR assays were set up with fluorescent probes that were 3′-labelled with Black Hole Quencher™ (Eurogentec, Belgium) and dephosphorylated at the 3′ end to prevent extension. The assays utilized Taqman® Fast universal PCR mastermix (Applied Biosystems®, Life Technologies, Thermo Fisher Scientific, USA) and were run on an Applied Biosystems 7500 Fast Real-time PCR system under the following default conditions: an initial holding stage of 20 s at 95 °C, followed by 40 cycles of 3 s at 95 °C and 30 s at 60 °C. Positive, negative and internal amplification controls were included [9]. Colonies that tested positive by PCR for bontE were purified and identified by 16S DNA sequencing.
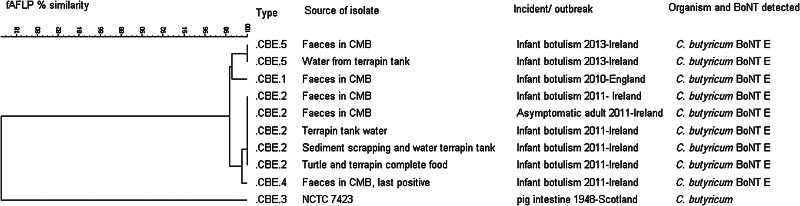
C. butyricum isolates containing bontE genes from faecal, medicinal and environmental specimens were subtyped by fluorescent amplified fragment length polymorphism (fAFLP) analysis using a modification of the standardized fAFLP protocol described by Desai et al. 2001 [10]. This typing technique using both enzymes HhaI and HindIII is faster and less labour intensive than PFGE and has been used in the UK to discriminate clostridial strains since 2007. fAFLP profiles of the two cases were compared with those from a previous case of C. butyricum type E infant botulism in England and to the non-neurotoxigenic type strain C. butyricum (NCTC 7423).
Laboratory results
Case A
After incubation for 1 day bontE genes were detected by PCR in enrichment cultures set up from faecal samples from both the infant and the mother, samples of water and sediment from a tank housing pet terrapins and a sample of opened terrapin feed from the infant's home (Table 1). Lipase-negative, lecithinase-negative, bontE gene-positive colonies were purified from PCR-positive enrichment broths and identified by 16S sequencing as C. butyricum. Five samples of unopened terrapin feed of the same batch and other medicinal samples tested negative.
Case B
Using the above methods, bontE genes were detected by PCR in the infant's faeces and in water from a tank which housed terrapins in the home of a relative who had held and fed the infant (Table 1). Again, lipase-negative, lecithinase-negative, bontE gene-positive colonies were purified from PCR-positive enrichment broths and identified by 16S sequencing as C. butyricum. Samples of water and stones from tanks which housed ornamental fish and goldfish in another relative's home were negative as were samples of fish food and goldfish food, and infant formula and sugar which the infant had consumed.
The fAFLP profiles obtained from chromatographs showing fluorescing fragments or peaks (Peak Scanner™, Applied Biosystems®) of C. butyricum BoNT/E isolates from case A, mother's faeces, terrapin tank water and sediment and terrapin fish food were indistinguishable except for one isolate from the infant which differed by a single fluorescent peak out of an approximate total of 95 (Fig. 1). In case B the fAFLP profiles of C. butyricum BoNT/E isolates from faeces and the terrapin tank water from the relative's home were indistinguishable. fAFLP profiles of isolates from cases A and B differed by only three peaks.
Fig. 1.
Comparison of C. butyricum BoNT/E isolates from cases of infant botulism, associated environmental samples and the type of C. butyricum strain.
The fAFLP profiles were compared with that from a C. butyricum type E isolate from a previous case of infant botulism in England [6]. The profiles from cases A and B type E infant botulism shared many similarities with the C. butyricum BoNT/E isolate from the type E infant botulism case in England but were distinguishable by four and three fluorescent peaks, respectively (Fig. 1). The fAFLP profiles of C. butyricum type E isolates from the infants clustered together at >98% similarity but separately from the non-toxigenic C. butyricum NCTC type strain.
Public health and environmental health investigation and management
On both occasions, the laboratory identification of C. butyricum BoNT type E was reported to the Department of Public Health, Health Service Executive, Dublin. The Incident Control Team comprised public health, environmental health, microbiology and clinical personnel, and staff from the national Health Protection Surveillance Centre. There was discussion with experts in the Gastrointestinal Bacteria Reference Laboratory, Public Health England and the IBTPP in California.
In case A, interviews with the infant's parents confirmed that he had been exclusively breast-fed prior to the onset of illness; he had not been fed honey. The family had pets – a dog and ‘yellow-bellied’ terrapins (Trachemys scripta scripta). A stool sample was obtained from his mother and samples were taken of products ingested or potentially ingested by him, including vitamin drops and moisturising creams. Samples of water and sediment from the terrapin tank and of the terrapin feed were prioritized for testing in view of the known association between BoNT type E and aquatic environments.
The terrapins and the water tank were removed from the infant's home prior to his second discharge from hospital. Soft furnishings in the bedroom in which the terrapins had been housed were deep cleaned and the carpet on which the terrapins exercised was destroyed. The family was instructed in the use of scrupulous hand hygiene to minimize any risk of transmission of clostridial spores and were advised that the infant should not be in contact with other infants until his stool samples were consistently negative for C. butyricum.
C. butyricum BoNT/E was isolated from the opened container of terrapin feed. Manufactured in the UK, it included dried shrimps, krill and gammarus imported from Belgium (originally sourced in China), Germany and the USA, as well as three types of food ‘sticks’ including one imported from The Netherlands. After the ingredients are mixed, the food is placed into sealed bags and stored in a dedicated freezer, before being weighed into pots, sealed and lidded.
Local pet food outlets were requested to suspend sales of the suspect batch. Five samples from unopened containers of that batch were tested. When negative results were obtained from all of those samples, the stores were informed that the batch of feed could be replaced on the shelves.
The Irish Department of Agriculture, Fisheries and Food (now the Department of Agriculture, Food & the Marine) informed their counterparts in the Department of Food and Rural Affairs in the UK of the identification of C. butyricum in the terrapin tank water and sediment, and in the open container of terrapin feed. The manufacturer was informed of the laboratory results. On the basis of the findings in case A, a case of C. butyricum BoNT/E infant botulism in the UK in May 2010 was reviewed. Honey had been considered the most likely vehicle of transmission but on further investigation it was found that this infant's family also kept yellow-bellied terrapins as pets and used the same brand of feed as in the Irish case. Unfortunately, samples were not available for testing.
In case B the parents could not initially recall the infant having had contact with terrapins but on repeat questioning, 8 days post-diagnosis the mother remembered that the child had visited a house with a fish tank and a goldfish tank. One day later, the father recalled that another family visiting that day owned a pet terrapin. The infant had been held by members of that family, one of whom had fed the infant and had soothed him by putting a finger in his mouth. That family did not use proprietary terrapin food. Samples from the fish tank, terrapin tank and fish foods were sent for testing to the Reference Laboratory in the UK. Neurotoxigenic clostridia were not detected in stool samples from the infant's parents but water from the terrapin tank in the relatives' home tested positive for the same organism as the infant. On both occasions, an alert was sent through EPIS to alert European colleagues that turtles needed to be considered in the list of potential exposures in a case of infant botulism. Information on the Health Protection Surveillance Centre website was updated.
Local pet shops reported that the terrapins and related goods had been supplied by a company in Northern Ireland. The Irish Department of Agriculture, Food and the Marine informed their counterparts in the Department of Food and Development in Northern Ireland of the identification of C. butyricum BoNT/E in the terrapin tank water. The suppliers identified the pet shops to which they were sending terrapins or supplies such as terrapin food in the Republic of Ireland.
After each case information was sent to all pet shops about the infectious disease risks, such as salmonellosis, associated with reptiles. A press release issued by public health authorities and media interviews aimed to raise awareness of the risks and the public health advice that children aged <5 years should not be in contact with reptiles.
Following the second case, public health colleagues reviewed infant deaths in Northern Ireland but did not find any where botulism might have been the underlying cause of death.
DISCUSSION
These are the first cases of infant botulism notified in Ireland. The Gastrointestinal Reference Laboratory in Colindale, London, has reported a total of 17 cases in the UK from the first report in 1978 until January 2014. Infant botulism caused by neurotoxigenic C. butyricum type E is particularly rare; seven other cases have been reported worldwide: four in Italy and one each in Japan, the USA and the UK [5, 6].
These cases are also notable for the young age of presentation, at 11 days. The mean age at onset of infant botulism is 13·8 weeks in the USA and 14·3 weeks in cases reported outside the USA [11]. CDC reported that the US infant with neurotoxigenic C. butyricum type E botulism presented when 1-week-old [12, 13] but the case reported from Japan was aged 9 months [14]. Other cases of infant botulism reported at a very young age include a case of C. baratii-producing type F toxin with onset 38 h after birth, with four other cases having an age of onset of 3, 9, 14 and 90 days [15]. The first reported case of C. botulinum-producing type E toxin presented at 9 days old [16].
Constipation may be a predisposing factor as well as one of the most frequent clinical manifestations of infant botulism [5, 17]. Difficulties obtaining a passed stool sample for laboratory testing are attributed to decreased colonic motility caused by the neurotoxin. The PHE laboratory recommends obtaining rectal washout specimens as described on the IBTPP website.
The cases we report were treated with the trivalent equine botulinum antitoxin (A, B and E) which contains antitoxin to neurotoxin type E [18]. As equine antitoxin has a short duration of action (2–3 weeks) [19], human BIG-IV with duration of action up to 6 months was also administered [3].
BIG-IV is produced by the California Department of Public Health (IBTPP; www.infantbotulism.org) from hyperimmune plasma donated by volunteers immunized with pantavalent botulinum toxoid A–E (i.e. toxoids of toxins A–E). For this reason BIG-IV contains botulinum-toxin-neutralizing antibody against the five botulinum toxins types A–E. However, BIG-IV is approved by the U.S. Food and Drug Administration only for the treatment of infant botulism types A and B. We believe case A was the second report of an infant botulism type E case treated with BIG-IV [16]. Despite faecal excretion of C. butyricum BoNT/E up to 42 and 196 days after it was first detected, the infants remained well following treatment with BIG-IV, which may have reflected on-going benefit from BIG-IV until stool clearance of C. butyricum BoNT/E excretion was achieved.
A case of C. botulinum type A toxin was recently reported as having positive stools for a similar 7-month period [20]. The introduction of treatment with BIG-IV allows infants to be discharged from hospital sooner than previously [3]. However continuing faecal excretion of toxic clostridia can pose a risk if healthy infants are exposed to recuperating infants [5]. Ongoing testing is required until stool clearance has been demonstrated, and parents and caregivers should be informed about the importance of hygiene and the potential risk to other healthy infants.
The source of spores causing infant botulism is rarely determined. In addition to honey being a well documented source of C. botulinum, a chamomile and fennel infusion was the suspected source in two cases of C. botulinum BoNT/B in Spain [21]. A case of sudden infant death in Finland was attributed to infant botulism after isolation of C. botulinum BoNT/B from post-mortem samples of the infant's intestinal contents and from vacuum cleaner dust from the infant's household but the source of the spores was not identified [22]. Peanut butter was found to be the source of C. botulinum BoNT/A spores in an adult with intestinal toxaemia botulism [23]. Investigation of cases of C. butyricum BoNT/E in Italy included extensive testing of environmental and food samples but no potential source was identified [5].
Investigation of case A lead to the hypothesis that the infant botulism most likely reflected environmental exposure to C. butyricum originating from pet terrapins or the terrapin feed in the family home. A faecal specimen from the baby's mother was positive for C. butyricum-producing BoNT type E but this intestinal carriage was asymptomatic. Given that the infant was born by caesarean section and that the age of onset was 11 days, perinatal transmission was considered unlikely.
Environmental samples associated with pet terrapins were prioritized for testing in case A because C. botulinum BoNT/E is particularly associated with marine and aquatic environments and C. butyricum, while widespread in the environment, has also been found in marine sediments [24]. The C. butyricum from this case of infant botulism was distinguishable from a strain of C. butyricum isolated from the first infant botulism type E case in the UK. However, the majority of peaks were indistinguishable, indicating that the two strains are related. Both families had exposure to pet terrapins and associated care equipment and supplies. A UK survey of a range of food and environmental samples found evidence of C. butyricum in 31% of samples but none of the representative subset tested carried the type E botulinum gene [25].
The indistinguishable fAFLP profiles of C. butyricum type E isolates from case A, the mother and terrapin tank water, sediment and feed provided evidence of a common source, most likely either the terrapins or the terrapin feed, giving rise to contamination of the tank water and sediment. The terrapin feed sample which tested positive for C. butyricum type E was from an opened container. While the organism was not detected in five unopened samples from the same batch, at this stage the terrapin feed could not be ruled out as a source. If spores originated in the feed, they could potentially germinate within the terrapin gastrointestinal system. The feed is formulated to float, so the terrapins' heads are visible above the water when feeding; this would increase the potential for any contaminants to be dispersed to the environment regardless of the original source of the C. butyricum. Terrapins are amphibious and were occasionally removed from the tank to walk on the bedroom floor, further increasing the potential for environmental contamination.
In case B the terrapins were not in the infant's home. Rather the infant was brought to visit a relative. While there, another visitor who cared for terrapins, held the infant for a couple of hours. In this instance, the terrapins were not exposed to the proprietary brand of food but shared the household food. This strengthened the evidence that it was the terrapins and not the terrapin food which was the source of infection in case A and in the UK case. It was also notable that in case B the infant was not directly exposed to the environment inhabited by the terrapins. It is hypothesized that the person who cared for the terrapins and who held the infant transmitted the spores which resulted in the infection. This is not surprising in view of the capacity for anaerobic spores to multiply in the newborn gut and that a very small dose of botulinum neurotoxin may have potentially lethal consequences.
The association between type E toxin and aquatic environments has received attention in recent years due to outbreaks of avian botulism in the Great Lakes area of North America, attributed to C. botulinum [26]. This has been associated with accumulations of algal mats which facilitate the growth of anaerobic bacteria, such as clostridia. Studies of the macroalga Cladophora in Lake Michigan detected C. botulinum present as vegetative cells rather than dormant spores. It is of interest that the first reported case of botulism due to C. botulinum-producing BoNT/E in a 9-day-old infant was reported from a hospital in Winfield, Illinois, close to Lake Michigan [16]. A study which compared type E toxin between C. botulinum and C. butyricum found they were very similar, and concluded that neurotoxigenic C. butyricum could arise when a wild-type strain acquires the toxin gene of a C. botulinum type E strain [27]. C. butyricum has been found in marine sediments [24] and where C. botulinum type E toxin is also present there is potential for C. butyricum to acquire the E toxin gene. Following this, it is possible that algal mats and the associated anaerobic conditions facilitate the growth of C. butyricum producing BoNT/E which are ingested by terrapins in their native habitats.
During the course of these investigations it emerged that there is no system in place in Ireland to register importers of exotic pets or pet feed. In addition, there is no licensing or inspection system in place to regulate pet shops. A report on these issues was submitted to the three national government departments with responsibility for health, agriculture and the environment. Forthcoming European and Irish legislation, enactment and enforcement are expected to address some of these issues.
This is the first report of infant botulism linked to terrapins kept as household pets. It highlights the importance of public health investigation and infection control in cases of infant botulism. Adherence to advice that reptiles, including terrapins, should not be kept as pets in homes where there are children aged <5 years, primarily to prevent salmonellosis, would also prevent cases of infant botulism associated with terrapins. The importance of hand washing after handling these pets also needs to be stressed, especially while visiting families with small children.
ACKNOWLEDGEMENTS
We are grateful to the infants' parents for their cooperation with the investigations into these cases. Thanks are also due to Dr Stephen Arnon and colleagues, Infant Botulism Center, California; Infant Botulism Treatment and Prevention Program, California Department of Public Health, 850 Marina Bay Parkway, Room E-361 Richmond, California 94 804, USA for their support in managing these cases. Dr Anthony Bouldin, Paediatric Neurologist, Our Lady's Children's Hospital, Crumlin, Dublin Hospital reviewed case B with Dr Richard Johnson of the Infant Botulism Center, California. The diagnosis, treatment and management of cases A and B were funded by the participating institutions.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Fox CK, Keet CA, Strober JB. Recent advances in infant botulism. Pediatric Neurology 2005; 32: 149–154. [DOI] [PubMed] [Google Scholar]
- 2.Barash JR, Arnon SS. A novel strain of Clostridium botulinum that produces type B and type H botulinum toxins. Journal of Infectious Diseases 2014; 209: 183–191. [DOI] [PubMed] [Google Scholar]
- 3.Arnon SS, et al. Human botulism immune globulin for the treatment of infant botulism. New England Journal of Medicine 2006; 354: 462–471. [DOI] [PubMed] [Google Scholar]
- 4.King LA, et al. Infant botulism in France, 1991–2009. Archives of Pediatrics and Adolescent Medicine 2010; 17: 1288–1292. [DOI] [PubMed] [Google Scholar]
- 5.Fenicia L, Anniballi F. Infant botulism. Annali dell'Istituto Superiore di Sanita 2009; 45: 134–146. [PubMed] [Google Scholar]
- 6.Grant KA, McLauchlin J, Amar C. Infant botulism: advice on avoiding feeding honey to babies and other possible risk factors. Community Practitioner 2013; 86: 44–46. [PubMed] [Google Scholar]
- 7.Arnon SS. Infant botulism. In: Feigen RD, et al. , eds. Textbook of Pediatric Infectious Diseases, 5th edn. Philadelphia: Saunders, 2004, pp. 1758–1766. [Google Scholar]
- 8.Dezfulian M, et al. Selective medium for isolation of Clostridium botulinum from human feces. Journal of Clinical Microbiology 1981; 13: 526–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grant KA, et al. Report of two unlinked cases of infant botulism in the UK in October 2007. Journal of Medical Microbiology 2009; 58: 1601–1606. [DOI] [PubMed] [Google Scholar]
- 10.Desai M, et al. Genome sequence-based fluorescent amplified fragment length polymorphism of Campylobacter jejuni, its relationship to serotyping, and its implications for epidemiological analysis. Journal of Clinical Microbiology 2001; 39: 3823–3829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koepke R, Sobel J, Arnon SS. Global occurrence of infant botulism 1976–2006. Pediatrics 2008; 122: e73–e82. [DOI] [PubMed] [Google Scholar]
- 12.Dykes JK, et al. Laboratory investigation of the first case of Clostridium butyricum type E infant botulism in the United States. In Proceedings, 45th Interagency Botulism Research Coordinating Committee Meeting, Philadelphia, 2008; abstract P–45.
- 13.CDC. (http://www.cdc.gov/nationalsurveillance/PDFs/Botulism_CSTE_2006_website.pdf). Accessed 12 September 2014.
- 14.Abe YT, et al. Infantile botulism caused by Clostridium butyricum type E toxin. Pediatric Neurology 2008; 38: 55–57. [DOI] [PubMed] [Google Scholar]
- 15.Barash JR, Tang TWH, Arnon SS. First case of infant botulism caused by Clostridium baratii type F in California. Journal of Clinical Microbiology 2005; 43: 4280–4282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lúquez C, et al. First report worldwide of an infant botulism case due to Clostridium botulinum type E. Journal of Clinical Microbiology 2010; 48: 326–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spika JS, et al. Risk factors for infant botulism in the United States. American Journal of Diseases of Children 1989; 143: 828–832. [Erratum in American Journal of Diseases of Children 1990; 144: 60.] [DOI] [PubMed] [Google Scholar]
- 18.Novartis Vaccines and Diagnostics. (http://www.immunisation.ie/en/Downloads/pdffile_15706_en.pdf). Accessed 12 September 2014.
- 19.Horowitz BZ. Type E botulism. Clinical Toxicology 2010; 48: 880–895. [DOI] [PubMed] [Google Scholar]
- 20.Derman Y, et al. Infant botulism with prolonged faecal excretion of botulinum neurotoxin and Clostridium botulinum for 7 months. Epidemiology and Infection 2014; 142: 335–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.López Laso E, et al. Infant botulism. Anales de Pediatría 2008; 68: 499–502. [DOI] [PubMed] [Google Scholar]
- 22.Nevas M, et al. Infant botulism acquired from household dust presenting as sudden infant death syndrome. Journal of Clinical Microbiology 2005; 43: 511–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sheppard YD, et al. Intestinal toxaemia botulism in 3 adults, Ontario, Canada, 2006–2008. Emerging Infectious Diseases 2012; 18: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tsukamoto K, et al. Characterization of Clostridium butyricum neurotoxin associated with food-borne botulism. Microbial Pathogenesis 2002; 33: 177–184. [PubMed] [Google Scholar]
- 25.Ghoddusi HB, Sherburn R. International Journal of Food Microbiology Preliminary study on the isolation of Clostridium butyricum strains from natural sources in the UK and screening the isolates for presence of the type E botulinal toxin gene. International Journal of Food Microbiology 2010; 142: 202–206. [DOI] [PubMed] [Google Scholar]
- 26.Chun CL, et al. Association of toxin-producing Clostridium botulinum with the macroalga Cladophora in the Great Lakes. Environmental Science and Technology 2013; 47: 2587–94. [DOI] [PubMed] [Google Scholar]
- 27.Giménez JA, Sugiyama H. Comparison of toxins of Clostridium butyricum and Clostridium botulinum Type E. Infection and Immunity 1988; 56: 926–929. [DOI] [PMC free article] [PubMed] [Google Scholar]