SUMMARY
Many clinics in rural western Kenya lack access to safe water and hand-washing facilities. To address this problem, in 2005 a programme was initiated to install water stations for hand washing and drinking water in 109 health facilities, train health workers on water treatment and hygiene, and motivate clients to adopt these practices. In 2008, we evaluated this intervention's impact by conducting observations at facilities, and interviewing staff and clients about water treatment and hygiene. Of 30 randomly selected facilities, 97% had water stations in use. Chlorine residuals were detectable in at least one container at 59% of facilities. Of 164 interviewed staff, 79% knew the recommended water-treatment procedure. Of 298 clients, 45% had received training on water treatment at a facility; of these, 68% knew the recommended water-treatment procedure. Use of water stations, water treatment, and client training were sustained in some facilities for up to 3 years.
Key words: Hand hygiene, hospital-acquired (nosocomial) infections, water (safe)
INTRODUCTION
Healthcare-associated infections (HAIs) remain a problem worldwide. Data on HAIs in developing countries are scarce, but the risk of HAI is 2–20 times higher than in high-income countries [1]. Although the causes of HAIs are multifaceted, poor hand hygiene has been recognized as a contributing risk factor for over 160 years [2]. Despite widespread awareness of the importance of hand hygiene, many health facilities in the developing world lack access to facilities, soap, and safe water for hand washing. Additional barriers to improved hand hygiene include insufficient healthcare worker acceptance and limited patient participation and empowerment [3, 4].
A related problem in health facilities in the developing world is the lack of access to safe drinking water. In the absence of water, oral administration of some medications at the facilities, including directly observed therapy for tuberculosis, are not possible, while the use of contaminated water places patients who receive oral treatments, including oral rehydration solution, at risk of enteric infections and increases the risk of opportunistic infections in HIV-infected persons [5–7]. Furthermore, enteric infections can reduce the intestinal absorption of nutrients and presumably orally administered medicines [8].
To address these two problems, a pilot project to improve access to safe treated water for hand washing and drinking was carried out in 2004 at the Homa Bay District Hospital in Nyanza Province, Kenya. In this programme, CARE Kenya installed hand-washing and drinking-water stations consisting of safe water storage vessels, a limited supply of soap, and locally available water-treatment solution (WaterGuard) that had been socially marketed by Population Services International (PSI) since 2003, principally through radio advertising and stocking of small shops and pharmacies. The programme included training of healthcare workers in hand washing, water treatment and safe storage, and techniques for motivating clients to adopt these practices. An evaluation of this programme demonstrated an increase in confirmed water-treatment practices and knowledge of proper hand-washing procedures among facility clients [9].
In response to the promising outcome of the pilot project, similar interventions were implemented in 108 additional health facilities lacking a reliable source of water in western Kenya, between 2004 and 2008. The objectives of the programme were to improve hygienic conditions in health facilities by providing hand-washing and drinking-water infrastructure, training health providers in water treatment and hygiene, and using the new infrastructure as a platform for health providers to teach their colleagues and clients about water treatment and hygiene. In this programme, the intervention included the installation of hand-washing and drinking-water stations that consisted of 60-litre plastic vessels with a tap (Fig. 1), a metal stand (if necessary), and a basin; the provision of a 3-month starter supply of WaterGuard and soap; and a 4-h training-of-trainers session at a central location for two nurses per health facility with lectures and hands-on practice. During the training, health facility staff were instructed to train their colleagues and their clients in group and one-on-one (e.g. examination room) sessions, to treat water in all containers, and to replenish WaterGuard and soap from their clinic supply budget. Each water station costs approximately US$15, each bottle of WaterGuard costs US$0.26, and each bar of soap US$0.15. The average start-up cost per health facility for seven water stations and a 3-month supply of commodities was approximately US$130; commodity resupply costs were about US$20 per month. From October to December 2008, we evaluated the impact of this intervention on water treatment and hygiene knowledge and reported practices among health workers and their clients.
Fig. 1.

A hand-washing station with a lid and a spigot, and a bar of soap on the stand.
METHODS
Evaluation design
The evaluation was a cross-sectional survey of 30 randomly selected health facilities, including dispensaries (the lowest level and first line of contact with the healthcare system, providing mainly preventive and minor curative ambulatory services), health centres (which provide preventive and curative health services, usually with some capacity for inpatient care) and hospitals (which provide a wider range of inpatient and outpatient services). It consisted of three components: an assessment of the presence and use of drinking-water and hand-washing containers in health facilities, a survey of health facility staff, and exit interviews of clinic clients.
Sample selection
We selected a random sample of 30/109 facilities, stratifying proportionally by type of facility (hospital, health centre, dispensary). The 30 facilities were located in seven different districts in Nyanza Province. We attempted to interview all patient care staff present at each health facility on the day of the evaluation.
To determine the sample size for the client survey, we assumed reported WaterGuard utilization of 10%, a margin of error of ± 5%, and a design effect of 2, which resulted in an estimated 276 clients. We attempted to conduct exit interviews with 10 clients at each of the 30 health facilities.
Data collection
We made surprise visits to all of the selected health facilities. The charge nurses, who had worked with the implementing organization and were familiar with the project, gave permission for evaluation activities at the time of the visit and responded to questions about the facility and use of the intervention. At each health facility, a data collection form was completed that included observations of the hand-washing and drinking-water stations, the presence of WaterGuard and soap, and general sanitary conditions. A water station was defined as ‘in use’ if it was stationed in a location where staff or patients could use it; all stations were also examined to see if water was present. In addition, we tested water in hand-washing and drinking-water stations for free chlorine residuals using the N,N-diethyl-p-phenylene diamine (DPD) method (Hach Co., USA).
We interviewed all clinical staff available at dispensaries and health centres on the day of the visit. At hospitals, only outpatient Maternal and Child Health (MCH) staff were interviewed, as MCH clinics were the principal implementation site for the intervention. Staff were interviewed about their hand-washing and water-treatment knowledge and practices, and client teaching activities.
Due to the low number of clients visiting smaller facilities and the limited opening hours of most facilities, it was necessary to choose a convenience sample of clients in order to reach our target of 10 client interviews per facility. As mothers had been the main target of the intervention, we chose to interview women whenever possible. If the number of clients at the facility was low, we included men in our sample population, in order to reach the target. The clients were interviewed about their knowledge and practices of hand washing, water treatment and storage, and the content of the training they had received at the health facility, if any.
Informed consent
The Institutional Review Board (IRB) at CDC determined that this activity was an evaluation of proven public health practice and IRB regulations did not apply; the Kenyan Ministry of Health approved and supported the activity, which took place in its facilities. Oral informed consent was obtained from all participants and personal identifiers were permanently removed from databases.
Data analysis
Data from the evaluation were entered into EpiData v. 3.1 (EpiData Association, Denmark). Statistical analysis was performed using Epi Info v. 3.5.1 (CDC, USA). We calculated frequencies, median values and ranges, and stratified the interviews and observations according to type of facility.
RESULTS
Facility assessment
Facility and staff characteristics
A total of 30 facilities in seven different districts were visited. The sample consisted of 14 dispensaries, 10 health centres and six hospitals. A total of 164 staff members were interviewed; 57 at the dispensaries, 72 at the health centres and 35 at the hospitals. We interviewed all staff members present on the day of our visit (Table 1).
Table 1.
Facility and staff characteristics by health facility type, Nyanza Province, Kenya 2008
| Dispensaries | Health centres | Hospitals | Total | |
|---|---|---|---|---|
| Median number of staff employed (range) | 5 (2–12) | 8 (6–14) | 10 (4–31) | 8 (2–31) |
| Median number of patients seen per day (range) | 40 (17–190) | 58 (11–220) | 125 (20–300) | 58 (11–300) |
| Total number of staff interviewed | 57 | 72 | 35 | 164 |
| Median age of staff interviewed, years (range) | 35 (24–56) | 32 (21–55) | 39 (22–55) | 34 (21–56) |
| Median length of service (range) | 24 months (0–33 years) | 23 months (0–15 years) | 24 months (0–24 years) | 24 months (0–33 years) |
| Median number of staff trained by CARE Kenya (range) | 2 (0–2) | 2 (0–2) | 1 (0–3) | 1 (0–3) |
| Median number of months since implementation (range) | 18 months (6–40) | 12 months (4–36) | 36 months (9–40) | 18 months (4–40) |
Water storage and treatment practices
Of 30 facilities, 29 (97%) were observed to have at least one of the water stations in use (Table 2). Of 29 facilities using at least one container, 15 (52%) had been using safe water storage for >1 year (range 18 months to 4 years) and 14 (48%) had been using it for ⩽1 year (range 4–12 months). Of 94 water stations in use at the facilities, 90 (96%) contained water and all were covered by lids. It was not possible to distinguish whether water stations were used for hand washing or drinking. Soap was present within 1 m of at least one water station at 20 (67%) facilities. All 30 facilities reported treating their drinking water; of these, 29 (97%) reported using WaterGuard (Table 2). Free residual chlorine was detected in 30 (32%) of the 94 water stations, including at least one water station at 17 (57%) of the facilities. Detectable free chlorine residuals were found in at least one container at eight (53%) of the facilities with a programme duration of >1 year, and at nine (64%) facilities with a programme duration of ⩽1 year (P = 0·71).
Table 2.
Water sources, use of water stations, reported and observed water-treatment practices, and presence of soap, by health facility type, Nyanza Province, Kenya 2008
| Dispensaries (N = 14) n (%) | Health centres (N = 10) n (%) | Hospitals (N = 6) n (%) | Total (N = 30) n (%) | |
|---|---|---|---|---|
| Water source | ||||
| Improved | 14 (100) | 10 (100) | 6 (100) | 30 (100) |
| On-site | 13 (93) | 9 (90) | 5 (83) | 27 (90) |
| At least one water station in use | 14 (100) | 10 (100) | 5 (83) | 29 (97) |
| Reported treating their drinking water | 14 (100) | 10 (100) | 6 (100) | 30 (100) |
| Reported using WaterGuard | 14 (100) | 10 (100) | 5 (83) | 29 (97) |
| Chlorination products were observed | 14 (100) | 9 (90) | 5 (83) | 28 (93) |
| Stored water in at least one container testing positive for chlorine residuals | 8 (57) | 6 (60) | 3 (50) | 17 (57) |
| Soap within 1 m of at least one water station | 11 (79) | 7 (70) | 2 (33) | 20 (67) |
Chlorination products (WaterGuard, AquaGuard, Aquatabs, etc.) were observed at 28 (93%) of 30 facilities. The free supply that was initially provided had been depleted at six (43%) dispensaries, all of which had subsequently purchased their own products. Similarly, the free supply had been depleted at six (60%) health centres, of which five purchased their own products. All MCH departments at the hospitals were provided with chlorination products from a central unit of the hospital, and thus did not purchase products. In total, there were 40 containers at the dispensaries; 39 (98%) contained water and 15 (38%) tested positive for free chlorine residuals. At the health centres, 45 water stations were installed; 43 (96%) contained water and 12 (27%) tested positive for chlorine. In the hospitals there were nine containers, with eight (89%) containing water and three (33%) testing positive for chlorine. Detectable free chlorine residuals were found in at least one container at eight (73%) of the 11 facilities that reported purchasing their own chlorination products, and at nine (53%) of 17 facilities that still had them from the initial free distribution.
Staff
Demographics
We interviewed all 164 patient care staff members present on the day of our visit; 57 at the dispensaries, 72 at the health centres and 35 at the hospitals. The median age was 34 years (21–56 years) and the median length of service was 24 months (0 months to 33 years) (Table 1).
Knowledge and practices
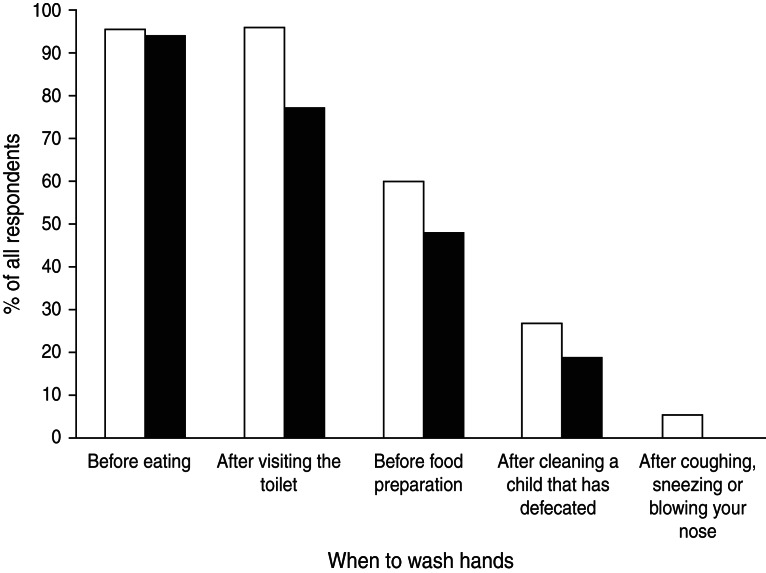
A total of 29 (18%) staff members reported having been trained on the water programme by CARE Kenya and 57 (36%) had received training from a colleague (Table 3). When asked to indicate when hand washing is important, respondents mentioned the following: after visiting the toilet (96%), before eating (95%), before food preparation (61%), after cleaning a child who has defecated (27%), after contact with a patient (26%) and after coughing, sneezing or blowing one's nose (4%) (Fig. 2). The response patterns were similar irrespective of facility type.
Table 3.
Percentage of health staff with knowledge of recommended water treatment and storage, by training received and health facility type, Nyanza Province, Kenya, 2008
| Dispensaries (N = 57) n (%) | Health centres (N = 72) n (%) | Hospitals (N = 35) n (%) | Total (N = 164) n (%) | |
|---|---|---|---|---|
| Reported receiving training from CARE Kenya | 15 (26) | 11 (15) | 3 (9) | 29 (18) |
| Reported receiving training from colleagues | 14 (25) | 32 (44) | 11 (31) | 57 (36) |
| Knew the recommended water-treatment procedure* | 42 (74) | 61 (85) | 27 (77) | 130 (79) |
| Knew the recommended water-treatment procedure* and had been trained | 26 (46) | 36 (50) | 11 (31) | 73 (45) |
| Knew the recommended water-treatment procedure* but had not been trained | 16 (28) | 25 (35) | 16 (46) | 57 (35) |
| Knew that all water sources should be treated | 40 (70) | 59 (82) | 31 (89) | 130 (79) |
| Knew that water should be treated during all seasons | 53 (93) | 67 (93) | 35 (100) | 155 (95) |
| Identified the recommended characteristics of safe storage containers† | 51 (90) | 55 (76) | 30 (86) | 136 (83) |
Recommended water-treatment procedure defined as knowledge of both recommended dose and recommended contact time of WaterGuard.
Containers with a narrow mouth, a lid and a spigot.
Fig. 2.
Percentage of health staff and clients indicating when hand washing is important, Nyanza Province, Kenya 2008. ■, Clients; □, staff.
Most staff knew the characteristics of safe water storage containers (83%), the recommended dose and contact time of WaterGuard (79%), and the importance of treating water from all sources (79%) in all seasons (95%) (Table 3). Knowledge of the recommended water-treatment procedure was described by 28 (97%) of 29 staff members trained by CARE Kenya and 57 (73%) of 78 who had not been trained.
Training of clients
A total of 150 (92%) staff reported teaching their clients about hand washing, and water treatment and safe storage. Specific hand-washing topics that staff reported teaching included the importance of hand washing (61%), when to wash hands (50%), and proper hand-washing technique (31%). Water handling topics included safe water storage (91%), recommended WaterGuard dosage (65%), proper WaterGuard contact time before consumption (48%), and WaterGuard as a diarrhoea prevention measure (45%).
Clients
Demographics
A total of 298 clients were interviewed; 276 (93%) were women. The median age of clients was 25 years (range 14–70 years). Less than 10% of all clients reported diarrhoea as the reason for their facility visit but 25% said that someone in their household had suffered from diarrhoea within the preceding 7 days.
Knowledge and practices
When clients were asked at what times hand washing is important, the two most common responses were ‘before eating’ (94%) and ‘after visiting the toilet’ (77%) while a lower percentage indicated before food preparation (47%), after cleaning a child that has defecated (18%), and after sneezing, coughing and blowing your nose (0·3%) (Fig. 2). Of 298 clients, 116 (39%) reported that they received training on hand washing at a health facility.
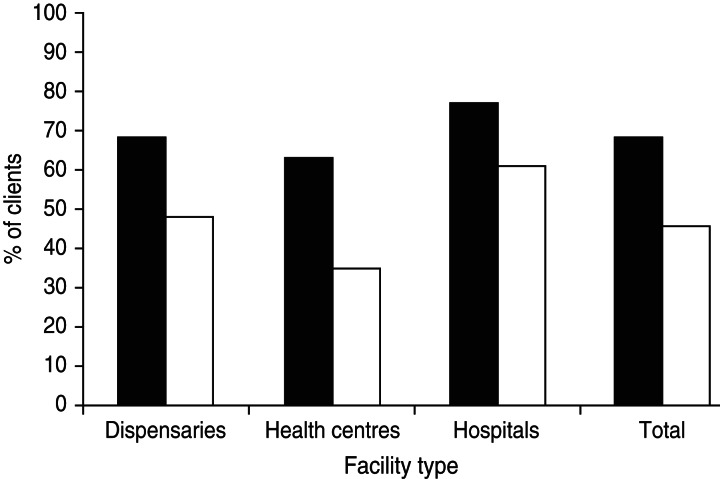
Of 298 clients, 291 (98%) had heard about WaterGuard (Table 4). The most commonly mentioned source of information was the radio (56%), followed by health facilities (45%). A total of 266 (89%) reported treating their water, of whom 200 (75%) used WaterGuard and 122 (46%) used boiling. Of 298 clients, 134 (45%) reported having received training at a health facility on WaterGuard and 76 (26%) reported having received training there on safe water storage. Of 134 clients who had been trained on WaterGuard, 91 (68%) had knowledge of the recommended water-treatment procedure, compared to 76 (46%) of 164 who had not received training on WaterGuard at a health facility (Fig. 3).
Table 4.
Sources of WaterGuard knowledge and reported water-treatment practices among clients, by health facility type, Nyanza Province, Kenya, 2008
| Dispensaries (N = 140) n (%) | Health centres (N = 98) n (%) | Hospitals (N = 60) n (%) | Total (N = 298) n (%) | |
|---|---|---|---|---|
| Heard about WaterGuard | ||||
| On the radio | 73 (52) | 58 (59) | 37 (62) | 168 (56) |
| At a health facility | 69 (49) | 43 (44) | 22 (37) | 134 (45) |
| Had not heard about WaterGuard | 4 (3) | 3 (3) | 0 (0) | 7 (2) |
| Reported treating household water | 125 (89) | 84 (86) | 57 (95) | 266 (89) |
| Reported having ever used WaterGuard | 109 (78) | 68 (69) | 50 (83) | 227 (76) |
| No. that had ever bought WaterGuard | 97 (69) | 58 (59) | 48 (80) | 203 (68) |
| No. that had ever been given WaterGuard | 48 (34) | 33 (34) | 14 (23) | 95 (32) |
| No. that had used WaterGuard within the last 3 days | 65 (46) | 43 (44) | 31 (52) | 139 (47) |
| Knew the recommended water-treatment procedure* | 81 (58) | 46 (47) | 40 (67) | 167 (56) |
Recommended water-treatment procedure defined as knowledge of both recommended dose and recommended contact time of WaterGuard.
Fig. 3.
Percentage of health facility clients with knowledge of proper use of WaterGuard, by training status, Nyanza Province, Kenya 2008. ■, Trained; □, untrained.
DISCUSSION
Results of this cross-sectional evaluation showed that hand washing and drinking-water stations appeared well maintained in a high percentage of health facilities where the stations had been installed between 4 and 40 months earlier. All health facilities but one had water stations that were actively being used at the time of the surprise visit, all reported treating their water, most had soap and water-treatment products present, and over half had at least one container with detectable free residual chlorine.
Our findings suggest that knowledge of hand washing and water treatment was transferred from staff to clients. Nearly 40% of the interviewed clients reported being taught about hygiene and over half about water treatment at a facility, and health facilities were the second most commonly mentioned source of information about WaterGuard. A higher proportion of clients that were taught about WaterGuard at a health facility knew the recommended water-treatment procedure in comparison with clients that had not received this training at a health facility. Our evaluation supports previous research in suggesting that health facilities are suitable venues for client education [9]. The use of health professionals, who have high credibility in local populations, in promoting water treatment and hand washing, can help motivate the adoption of this behaviour [9–11].
A low percentage of health facility staff and clients reported that it was important to wash hands after cleaning a child who had defecated. This finding was of concern because it suggested that both populations were placing themselves and their contacts at risk of pathogen transmission. Although a recent study found no association between cleaning a child's anus after defecation and child diarrhoea [12], this practice is recommended for diarrhoea prevention.
Similarly, a remarkably low percentage of both staff and clients reported washing hands after sneezing, coughing or blowing their nose, and only a small percentage of staff appeared to be aware of the importance of hand washing after physical contact with a patient, which indicated the need for improved training on the importance of hand washing. These findings may be the result of the intervention placing a particularly strong emphasis on the prevention of diarrhoeal disease. In light of growing concerns about pandemic influenza, future interventions should also stress the importance of hand washing in preventing respiratory infections [12, 13].
One risk to the sustained use of this type of an intervention is staff turnover. Although 36% of health providers reported that they were trained in this hygiene programme by their colleagues, continued turnover could reduce the use and impact of the intervention. To help mitigate this problem, a manual with programmatic information and implementation guidance has been produced and distributed to these and other health facilities.
Because of financial and logistical constraints, this evaluation had several important limitations. First, we did not have the resources to include a sample of comparison clinics which would have made the evaluation more robust. However, to our knowledge, no other organizations were distributing water stations at the time of this programme. In addition, all of the water stations, which had a design that was unique to our programme, were observed to be the ones that had been installed by the organization implementing this project. Second, we lacked the capacity to conduct household visits of interviewed clients to confirm by observation their reported practices. However, our findings were consistent with those of a previous study in western Kenya that included confirmation of household water treatment through visits to homes of clients who had received training at a health facility [9]. Third, financial constraints limited the length of the visit to each health facility to 1 day, which necessitated selecting a convenience sample of staff and clients that may not have been representative of the general health facility population. Fourth, because of limitations of time and money, we were unable to make structured observations of hand-washing behaviour, so reported hygiene improvements may have been overstated. However, by providing hand-washing infrastructure needed for hygiene in health facilities where none existed before, we believe the project improved hygiene. Fifth, budget limitations permitted the evaluation of only 30 health facilities. Finally, although this evaluation demonstrated that the clinic-based intervention was well-maintained, it was not possible to determine whether it was solely responsible for the transfer of hand-washing and water-treatment knowledge to untrained providers and clients because hygiene promotion and WaterGuard social marketing campaigns had taken place in Nyanza Province over the previous 5 years. However, social marketing on its own does not appear to result in high uptake of hand-washing and water-treatment practices [14, 15]. To further explore the impact of this clinic-based intervention, we suggest that future studies should include household visits to assess actual water-treatment behaviour and compare outcomes either between intervention and comparison facilities, or before and after implementation of the intervention at the same facility.
In conclusion, results of this evaluation suggest that health workers appear to be motivated to use and maintain the intervention even after 3 years; water stations were in use in many health facilities, soap and water-treatment products were present; and clients were being trained. Although the long-term goal remains the provision of 24-h access to piped, treated water, and adequate sanitary and hand-washing facilities in all dispensaries, clinics, and hospitals, this intervention offers a promising medium-term solution to reduce nosocomial infections and protect health. The availability of water-treatment social marketing programmes in at least 18 countries (http://www.psi.org/our-work/healthy-lives/diarrheal-disease) presents opportunities for the implementation of similar clinic-based programmes.
ACKNOWLEDGEMENTS
This evaluation could not have been performed without the help of the following staff: Beatrice Ohula, Raphael Ochieng, Dorkus Ngasi and David Omondi. We also thank the staff at the Nyando Integrated Child Health and Education Project for all their help and support. This paper is dedicated to the memory of Alfredo Obure (1976–2009). This evaluation was supported by the CARE-CDC Health Initiative (funded by the Woodruff Foundation), Danida and the Danish Council for Independent Research/Medical Sciences (reference numbers 271-07-0860 and 271-07-0861). The findings and conclusions in this report are those of the authors and do not necessarily represent those of the CDC.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Pittet D, et al. Infection control as a major World Health Organization priority for developing countries. Journal of Hospital Infection 2008; 68: 285–292. [DOI] [PubMed] [Google Scholar]
- 2.Wyklicky H, Skopec M. Ignaz Philipp Semmelweis, the prophet of bacteriology. Infection Control 1983; 4: 367–70. [DOI] [PubMed] [Google Scholar]
- 3.WHO. WHO guidelines on hand hygiene in health care, 2009.
- 4.WHO. Improved hand hygiene to prevent health care-associated infections, 2007.
- 5.Lule JR, et al. Effect of home-based water chlorination and safe storage on diarrhea among persons with human immunodeficiency virus in Uganda. American Journal of Tropical Medicine and Hygiene 2005; 73: 926–933. [PubMed] [Google Scholar]
- 6.Engelhart S, et al. Protecting vulnerable groups in the home: the interface between institutions and the domestic setting. Journal of Infection 2001; 43: 57–59; discussion 9–60. [DOI] [PubMed] [Google Scholar]
- 7.Daniels NA, et al. First do no harm: making oral rehydration solution safer in a cholera epidemic. American Journal of Tropical Medicine and Hygiene 1999; 60: 1051–1055. [DOI] [PubMed] [Google Scholar]
- 8.Petri WA Jr., et al. Enteric infections, diarrhea, and their impact on function and development. Journal of Clinical Investigation 2008; 118: 1277–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parker AA, et al. Sustained high levels of stored drinking water treatment and retention of hand-washing knowledge in rural Kenyan households following a clinic-based intervention. Epidemiology & Infection 2006; 134: 1029–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Reilly CE, et al. The impact of a school-based safe water and hygiene programme on knowledge and practices of students and their parents: Nyanza Province, western Kenya, 2006. Epidemiology & Infection 2008; 136: 80–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ulmer BC. The image of nursing. AORN Journal 2000; 71: 1124–1127. [DOI] [PubMed] [Google Scholar]
- 12.Suess T, et al. The role of facemasks and hand hygiene in the prevention of influenza transmission in households: results from a cluster randomised trial; Berlin, Germany, 2009–2011. BMC Infectious Diseases 2012; 12: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cowling BJ, et al. Facemasks and hand hygiene to prevent influenza transmission in households: a cluster randomized trial. Annals of Internal Medicine 2009; 151: 437–446. [DOI] [PubMed] [Google Scholar]
- 14.Stockman LJ, et al. Point-of-use water treatment and use among mothers in Malawi. Emerging Infectious Diseases 2007; 13: 1077–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thevos AK, et al. Adoption of safe water behaviors in Zambia: comparing educational and motivational approaches. Education for Health (Abingdon) 2000; 13: 366–376. [DOI] [PubMed] [Google Scholar]