SUMMARY
We report on the follow-up and epidemiological study triggered by the isolation of the first vancomycin-resistant Staphylococcus aureus (VRSA) detected in Europe. The patient and 53 close contacts were screened for S. aureus colonization and all isolates recovered were characterized by multiple molecular typing methods. The VRSA remained confined to the infected foot of the patient and was not detected in any of the close contacts. Nasal colonization with S. aureus was detected in 20 subjects, of whom 15 carried methicilin-susceptible isolates with the remaining five harbouring methicilin-resistant S. aureus (MRSA). The majority of the isolates belonged to clones that have been previously shown to be prevalent in Portugal, both in the hospital setting and in the community. Only one isolate, an MRSA, was closely related to the VRSA. Like most of the characterized VRSA isolates from other countries, the VRSA isolated in Portugal belonged to clonal complex (CC) 5. Despite the absence of VRSA dissemination, the recent increase in the incidence of lineages belonging to CC5 in some European countries, including Portugal, may result in more frequent opportunities for the emergence of VRSA.
Key words: Antibiotic resistance, bacterial infections, bacterial typing, infectious disease epidemiology, methicillin-resistant, S. aureus (MRSA)
Vancomycin remains one of the first-line options for the treatment of infections with methicillin-resistant Staphylococcus aureus (MRSA), but concerns regarding the possible spread of vancomycin-resistant strains of S. aureus (VRSA) have increased since the identification of the first VRSA isolate in 2002 [1]. This concern is of particular relevance in countries with a high prevalence of MRSA and vancomycin-resistant enterococci (VRE), since the latter can act as donors of genetic elements conferring vancomycin resistance to the former.
In May 2013, a VRSA strain (vancomycin minimum inhibitory concentration of 1024 μg/ml, determined by the broth microdilution method according to the guidelines of the Clinical and Laboratory Standards Institute [2]), harbouring the vanA gene, was isolated in a hospital in Lisbon, Portugal, along with vanA-positive vancomycin-resistant Enterococcus faecalis and Pseudomonas aeruginosa. These bacteria were recovered from pus of the toe amputation wound of a female patient with diabetes mellitus, chronic renal failure requiring haemodialysis, and peripheral vascular disease [3]. At the time, the patient was being treated with vancomycin and amikacin due to isolation of P. aeruginosa and vancomycin-susceptible MRSA from previous cultures of the amputation site (March 2013). After the VRSA isolation, antimicrobial therapy was changed and daptomycin, rifampicin, and amikacin were administered for 6 weeks. The VRSA strain was no longer found in the wound after 3 weeks, while VRE and P. aeruginosa were still recovered. Four weeks after the initial VRSA isolation, the patient underwent a new amputation of the metatarsals due to evidence of osteomyelitis. VRE was no longer recovered from the infection site after 5 weeks of antimicrobial therapy. Given the persistence of P. aeruginosa, therapy was changed to piperacillin/tazobactam and colistin. In August, the patient was clinically stable and the cultures from the foot were negative. The patient was therefore discharged from the hospital, and antimicrobial therapy was stopped.
Following the identification of the VRSA strain, infection control precautions were reinforced and an epidemiological study was initiated, in order to monitor the possible dissemination of the VRSA strain. The patient was initially screened for colonization by culturing swabs obtained from the nares, axillae, perineum, and groin. Subsequently, she was screened weekly for nasal colonization until discharge from the hospital. Colonization of the patient with S. aureus was not detected at any time. Nasal swabs were cultured from a total of 53 close contacts of the patient, including: two household members, 47 healthcare workers, and four patients, whom were under haemodialysis in the same room as the index patient. VRSA was not identified in any of the screened individuals. Methicillin-susceptible S. aureus (MSSA) was recovered from 15 healthcare workers, and five MRSA isolates were recovered from three healthcare workers, one household contact, and one haemodialysis patient.
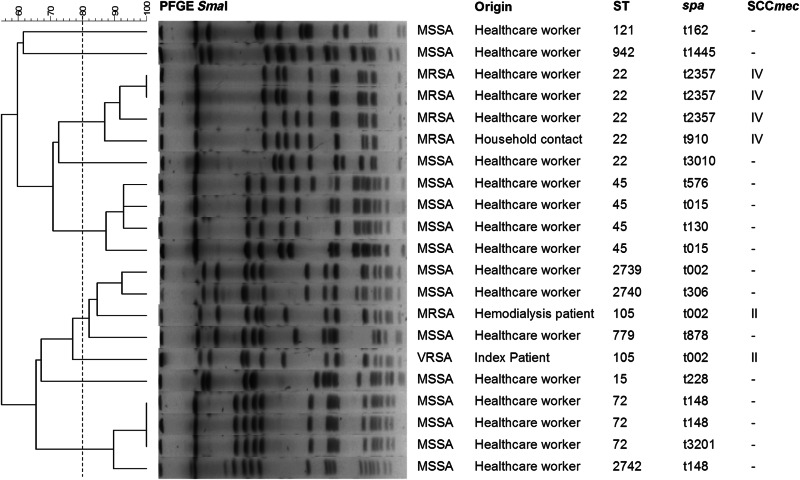
All MRSA and MSSA isolates recovered in this study, as well as the VRSA, were characterized by multilocus sequence typing (MLST), spa typing, and pulsed-field gel electrophoresis (PFGE) profiling of SmaI-digested DNA, as described previously [4]. The structure of the SCCmec element of all MRSA isolates (including the VRSA) was determined by multiplex PCR [4]. Of the five MRSA isolates, two different MLST sequence types (STs), three spa types and two SCCmec types were identified, while MSSA isolates presented 10 distinct STs (including three not previously described: ST2739, ST2740, and ST2742), and 11 spa types (Fig. 1). Only one colonizing MRSA strain, recovered from a patient treated in the same haemodialysis room as the index patient, presented the same ST, spa type, and SCCmec type as the VRSA isolate. However, clustering of the isolates based on a ⩾80% similarity of the PFGE profiles, which resulted in nine distinct clusters, placed the two strains in different clusters (Fig. 1). The MRSA isolate was grouped together with three MSSA isolates into the cluster closest to the VRSA isolate, which was not grouped with any other isolate.
Fig. 1.
Origin and molecular properties of the 21 Staphylococcus aureus isolates studied. The dendrogram was constructed based on the PFGE SmaI macrorestriction profiles of the isolates. The unweighted-pair group method using average linkages and the Dice coefficient (percentages, indicated in the scale above the dendrogram) were used in constructing the dendrogram. Clusters were defined as groups of isolates with a Dice coefficient of ⩾80% (indicated by a dashed vertical line).
In agreement with the results of the epidemiological studies conducted following isolation of VRSA strains in the USA [1, 5], transmission of the strain identified in Portugal to the patient's contacts at home, other patients, and healthcare workers was not detected. Moreover, colonization of the patient at sites other than the infected wound was also not detected, in contrast to the situation observed in two of the US patients [1].
The isolation of a vanA-positive strain of VRE from the patient's amputation wound [3] suggests that the VRSA identified in Portugal probably resulted from the transfer of the vanA-carrying genetic element into a putative recipient MRSA strain, during co-infection of the wound, in agreement with what has been proposed for other VRSA isolates [6]. This recipient MRSA may have been the one initially isolated from the amputation wound, for which the patient was receiving vancomycin treatment. However, this was not possible to confirm, since the MRSA isolate was no longer available for characterization.
Remarkably, all but one of the VRSA isolates found in the USA belong to clonal complex (CC) 5, which constitutes the most frequent lineage of hospital-associated MRSA infections in the USA [6, 7]. The VRSA isolated in Portugal is the first VRSA representing ST105. However, this is a single locus variant of ST5, supporting the hypothesis that strains of CC5 are more prone to acquire vanA-carrying genetic elements from VRE [6]. The properties of the VRSA, and of the MRSA colonizing another haemodialysis patient (ST105-t002-SCCmecII), match those of the second most frequent MRSA clone found in our hospital during 2010 (NY/Japan-related clone) [4]. The other MRSA isolates, which grouped into a different PFGE cluster, presented characteristics (ST22-t910/2357-SCCmecIV) consistent with the most frequent MRSA clone circulating both in hospitals and in the community in Portugal, namely EMRSA-15 [8].
Unsurprisingly, MSSA isolates were more frequently isolated from colonization and presented a high genetic diversity. Most of the isolates belonged to clones previously identified in Portugal, based on the spa type and MLST information, although some STs, spa types, and ST-spa combinations had not been previously reported in MSSA isolates in our country [9]. The three new STs identified in this study are all single-locus variants of highly prevalent STs in Portugal, namely ST5 and ST72.
The results of this study are consistent with the hypothesis that VRSA emerge following sporadic transfer of vanA from donor VRE into MRSA during polymicrobial infections, mostly in patients with underlying conditions and recent use of vancomycin [5]. The acquisition of genetic elements harbouring vanA by MRSA appears to be rare, with only a limited number of VRSA infections described worldwide [10, 11]. These VRSA strains seem to be at a disadvantage with respect to MRSA, since they rarely colonize the patient they infect and are not known to be transmitted to close contacts. The recent increase of CC5-associated clones observed in Portugal and other European countries [4] raises concerns that VRSA may arise more frequently in Europe in the near future, particularly in countries with a high prevalence of MRSA and VRE, highlighting the importance of continued surveillance and of establishing effective infection control measures.
DECLARATION OF INTEREST
Dr José Melo-Cristino has received research grants administered through his university and received honoraria for serving on the speakers’ bureaus of Pfizer, Novartis, and Gilead. Dr Mário Ramirez has received honoraria for serving on the speakers’ bureau of Pfizer and for consulting for GlaxoSmithKline. No company or financing body had any influence in the decision to publish.
REFERENCES
- 1.Sievert DM, et al. Vancomycin-resistant Staphylococcus aureus in the United States, 2002–2006. Clinical Infectious Diseases 2008; 46: 668–674. [DOI] [PubMed] [Google Scholar]
- 2.Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; twenty-third informational supplement. Wayne, PA, USA: Clinical and Laboratory Standards Institute, 2013, CLSI document M100-S23.
- 3.Melo-Cristino J, et al. First case of infection with vancomycin-resistant Staphylococcus aureus in Europe. Lancet 2013; 382: 205. [DOI] [PubMed] [Google Scholar]
- 4.Espadinha D, et al. Extensive dissemination of methicillin-resistant Staphylococcus aureus (MRSA) between the hospital and the community in a country with a high prevalence of nosocomial MRSA. PLoS One 2013; 8: e59960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finks J, et al. Vancomycin-resistant Staphylococcus aureus, Michigan, USA, 2007. Emerging Infectious Diseases 2009; 15: 943–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kos VN, et al. Comparative genomics of vancomycin-resistant Staphylococcus aureus strains and their positions within the clade most commonly associated with methicillin-resistant S. aureus hospital-acquired infection in the United States. mBio 2012; 3: e00112–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Limbago BM, et al. Report of the 13th vancomycin-resistant Staphylococcus aureus isolate from the United States. Journal of Clinical Microbiology 2014; 52: 998–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tavares A, et al. High prevalence of hospital-associated methicillin-resistant Staphylococcus aureus in the community in Portugal: evidence for the blurring of community-hospital boundaries. European Journal of Clinical Microbiology & Infectious Diseases 2013; 32: 1269–1283. [DOI] [PubMed] [Google Scholar]
- 9.Tavares A, et al. Population structure of methicillin-susceptible Staphylococcus aureus (MSSA) in Portugal over a 19-year period (1992–2011). European Journal of Clinical Microbiology & Infectious Diseases 2014; 33: 423–432. [DOI] [PubMed] [Google Scholar]
- 10.Askari E, et al. vanA-Positive vancomycin–resistant Staphylococcus aureus: systematic search and review of reported cases. Infectious Diseases in Clinical Practice 2013; 21: 91–93. [Google Scholar]
- 11.Rossi F, et al. Transferable vancomycin resistance in a community-associated MRSA lineage. New England Journal of Medicine 2014; 370: 1524–1531. [DOI] [PMC free article] [PubMed] [Google Scholar]