SUMMARY
We investigated a gastroenteritis outbreak in Erzurum city, Turkey in December 2012 to identify its cause and mode of transmission. We defined a probable case as onset of diarrhoea (⩾3 episodes/day) or vomiting, plus fever or nausea or abdominal pain during 19–27 December, 2012 in an Erzurum city resident. In a case-control study we compared exposures of 95 randomly selected probable cases and 95 neighbourhood-matched controls. We conducted bacterial culture and real-time multiplex PCR for identification of pathogens. During the week before illness onset, 72% of cases and 15% of controls only drank water from antique neighbourhood fountains; conversely, 16% of cases and 65% of controls only drank bottled or tap water (adjusted odds ratio 20, 95% confidence interval 4·6–84, after controlling for age and sex using conditional logistic regression). Of eight stool specimens collected, two were positive for Shigella sonnei, one for astrovirus, one for astrovirus and norovirus, and one for astrovirus and rotavirus. Water samples from the fountains had elevated total coliform (38–300/100 ml) and Escherichia coli (22–198/100 ml) counts. In conclusion, drinking contaminated fountain water caused this multi-pathogen outbreak. Residents should stop drinking water from these fountains, and clean water from the water treatment plant should be connected to the fountains.
Key words: Case-control studies, gastroenteritis, outbreaks, waterborne infections
INTRODUCTION
An estimated 2·5 billion cases of diarrhoea occur annually worldwide, almost 90% of which are caused by inadequate water, sanitation, and hygiene. Diarrhoea is the second leading cause of childhood mortality worldwide, killing annually about 1·5 million children aged <5 years [1]. Worldwide, the burden from poor water, sanitation, and hygiene has been estimated to account for at least 4·0% of all deaths and 5·7% of the total disease burden; this burden is largely preventable [2].
In the Republic of Turkey, diarrhoeal disease outbreaks occur frequently throughout the country (Early Warning and Response Unit, Public Health Institution of Turkey, unpublished data). However, few are thoroughly investigated to identify the responsible agents and modes of transmission. On 21 December 2012, a clinician informed the Public Health Directorate in Erzurum Province in eastern Turkey of an apparent increase in diarrhoeal diseases. A subsequent case-finding effort identified hundreds of gastroenteritis patients. We investigated this outbreak in order to identify the responsible agents, cause, and mode of transmission, and to implement evidence-based control and prevention measures.
METHODS
We defined a suspected case as a diagnosis of gastroenteritis in a Yakutiye District resident during a visit between 19 and 27 December 2012 to the three public hospitals and one private hospital serving residents of the three central city districts, based on the following International Classification of Diseases-10 (ICD-10) codes: A09 (Infectious gastroenteritis), R11 (Nausea or vomiting), and K52 (Non-infectious gastroenteritis). A probable case was onset during 19–27 December 2012 in a Yakutiye District resident of vomiting or diarrhoea, plus at least one of the following clinical presentations: fever, nausea, or abdominal pain. We identified the cases by reviewing medical records at the four hospitals.
To generate hypotheses on the cause and mode of transmission for this outbreak, we interviewed 67 new gastroenteritis patients with diarrhoea and vomiting who sought emergency or infectious disease care at two hospitals during 27–28 December. We asked questions regarding their symptoms, demographics, type of water used, travel history, and whether there were any other cases in the family. We performed descriptive analysis of the data in the Enteric Disease Surveillance System for Erzurum Province to evaluate the distribution of cases by person, time, and place.
For hypothesis testing, we randomly selected 115 suspected cases from the 11 neighbourhoods in Yakutiye District that had the highest attack rates, using SPSS software (IBM Corp., USA). We identified the controls by visiting the houses next to the case-patient's house. Persons who had no gastroenteritis symptoms during the past month served as controls. For the final analysis we used the information of 95 probable cases and their neighbourhood-matched controls. We used conditional logistic regression to estimate odds ratios (OR) and 95% confidence intervals (CI), and to control for confounding.
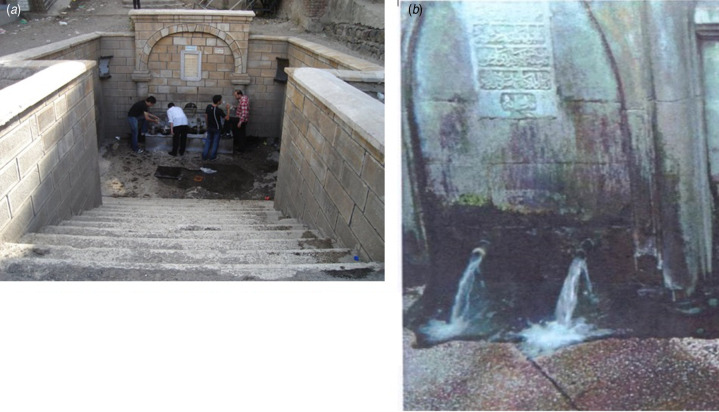
For laboratory investigation, we collected the stool specimens of patients who sought emergency medical care at the emergency departments of two of the four hospitals, using sterile containers. These specimens were transported to the National Reference Laboratory using standard courier packages. We conducted bacterial culture for Shigella spp., Salmonella spp., Campylobacter spp., verotoxigenic Escherichia coli, Vibrio cholerae O1, O139, and Aeromonas spp. We used multiplex real-time PCR to identify viral pathogens in the stool specimens, including norovirus (G1 and G2), rotavirus, adenovirus, and astrovirus. For the identification of protozoan parasites (including Giardia, Cryptosporidium, and Entamoeba histolytica), we used direct microscopy and real-time PCR; we also used the direct fluorescent antibody (DFA) testing to identify Giardia and Cryptosporidium, and the enzyme-linked immunosorbent assay (ELISA) to identify E. histolytica [3]. We visited the source of the tap-water and the water treatment plant; we also evaluated the water distribution system. We reviewed the routine chlorination records and microbiological testing results during November and December 2012 at the treatment plant. We collected water samples from the implicated antique neighbourhood fountains (Fig. 1) and used the membrane filtration method [4] to assess potential bacterial contamination.
Fig. 1.
Two examples of antique neighbourhood fountain implicated in this outbreak.
This investigation was part of the response to a public health emergency event; therefore, ethical review was not required.
RESULTS
On 20 December 2012, the Enteric Disease Surveillance System for Erzurum Province detected an increase in the number of patients with ICD-10 codes for gastroenteritis during hospital visits by residents who lived in the central city of the province (Fig. 2). The event was reported to the Early Warning and Response Unit at the Turkey Public Health Institution. In 2011, 635 patients were reported during 19–27 December; however, in 2012 the case count was 2096, an increase in cases of 1461 from 2011 to 2012.
Fig. 2.
Number of patients with ICD-10 codes for gastroenteritis (A09, K52, R11), Erzurum Province, Turkey, December 2011 and 2012.
When we examined the surveillance data for the central districts of this province, we found that gastroenteritis cases also peaked during early December. This peak was never reported. Metrological data showed that, in this province, the temperature in December is usually below 0°C; however, in 2012, immediately preceding the two peaks in gastroenteritis cases, the temperature was unseasonably warm (Fig. 2).
The attack rate of gastroenteritis for the central city was 5·6/1000. Of the three districts in the central city, Yakutiye District had the highest attack rate (8/1000). The neighbourhood-specific attack rates in this district ranged from 3·3 to 36/1000 (data not shown).
Of the 67 new gastroenteritis patients seeking emergency or infectious disease care due to vomiting or diarrhoea at the two local hospitals during 27–28 December 2012, 49% were males. Cases occurred in all age groups. Few persons (3%) had travel history. Patients mostly presented with non-specific gastroenteritis symptoms, including diarrhoea (99%), abdominal pain (94%), nausea (85%); 58% of the patients reportedly had watery diarrhoea; two (2%) had bloody diarrhoea. Regarding the source of their drinking water, 43% drank water from antique neighbourhood fountains, 7·5% drank water from both antique neighbourhood fountains and the municipal tap-water system.
The cases clustered around the antique neighbourhood fountains in the Yakutiye District of Erzurum city (Fig. 3). This district has 53 antique neighbourhood fountains, some of which date back to the Ottoman era (1299–1922) or pre-Ottoman era. The water coming out of these fountains is from unknown underground sources. We also learned from the Public Health Directorate of Erzurum Province that, on 20 December, sewage pipe work had been carried out in this area (Fig. 3). Based on the descriptive epidemiological analysis, we hypothesized that this outbreak was caused by drinking contaminated water from the antique neighbourhood fountains, or from the municipal water system contaminated during the sewage pipe work.
Fig. 3.
Location of cases in relation to antique neighbourhood fountains, Yakutiye District, Erzurum Province, Turkey, 19–27 December 2013.
Of the 115 suspected cases selected, 104 (90%) participated in our case-control study; the main reason for drop-out was absence from home. The final analysis dataset contained 95 probable cases and their matched controls. These probable cases had non-specific gastroenteritis symptoms, including diarrhoea, abdominal pain, vomiting, nausea, and fever; a substantial percentage of cases had either bloody or mucus diarrhoea (Table 1); 49% (47/95) of the probable cases had another case within the family.
Table 1.
Symptom distribution of the 95 cases in the case-control study of a gastroenteritis outbreak, Yakutiye District, Erzurum Province, Turkey, 19–27 December 2012
| Symptoms | Number | (%) |
|---|---|---|
| Diarrhoea | 87 | (92) |
| Bloody | 11 | (12) |
| Mucus | 30 | (32) |
| Abdominal pain | 82 | (86) |
| Vomiting | 81 | (85) |
| Nausea | 80 | (84) |
| Fever | 56 | (59) |
| Other | 6 | (6·4) |
The univariate analysis of the case-control study data showed that cases and controls differed by age and sex. When we investigated the source of drinking water of cases and controls, 76% of cases compared to 31% of controls drank water from antique neighbourhood fountains (OR 6·4, 95% CI 3·0–16). Conversely, 18% of cases compared to 50% of controls drank tap water (OR 0·14, 95% CI 0·044–0·37); 8·4% of the cases compared to 32% of controls drank bottled water (OR 0·15, 95% CI 0·039–0·44) (Table 2). Stratified analysis showed that 72% of cases compared to 15% of the controls drank water from the antique neighbourhood fountains only; conversely, 16% of cases compared to 65% of controls drank bottled or tap water only (OR 15, 95% CI 4·9–77; adjusted OR 20, 95% CI 4·6–84, adjusting for age and sex using conditional logistic regression) (Table 3).
Table 2.
Characteristics of 95 cases and 95 controls in the case-control study of a gastroenteritis outbreak, Erzurum Province, Turkey, 19–27 December 2012
| Characteristics | Cases, n (%) | Controls, n (%) | OR (95% CI) |
|---|---|---|---|
| Age (years) | |||
| 2–17 | 41 (43) | 6 (6·4) | 12 (3·3–42) |
| 18–39 | 28 (30) | 37 (39) | 1·3 (0·45–3·7) |
| 40–59 | 19 (20) | 39 (42) | 0·84 (0·28–2·5) |
| 60–82 | 7 (7·4) | 12 (13) | Ref. |
| Sex | |||
| Male | 35 (37) | 9 (9·5) | 5·6 (2·5–12) |
| Female | 60 (63) | 86 (91) | Ref. |
| Drinking water from antique neighbourhood fountains | |||
| Yes | 72 (76) | 29 (31) | 6·4 (3·0–16) |
| No | 23 (24) | 66 (69) | Ref. |
| Drinking tap water | |||
| Yes | 17 (18) | 47 (50) | 0·14 (0·044–0·37) |
| No | 78 (82) | 48 (50) | Ref. |
| Drinking bottled water | |||
| Yes | 8 (8·4) | 30 (32) | 0·15 (0·039–0·44) |
| No | 87 (92) | 65 (68) | Ref. |
| Drinking other water | |||
| Yes | 6 (6·3) | 7 (7·4) | 0·83 (0·20–3·3) |
| No | 89 (94) | 88 (93) | Ref. |
OR, Odds ratio; CI, confidence interval.
Table 3.
Association of drinking water with gastroenteritis onset during an outbreak: Erzurum Province, Turkey, 19–27 December, 2012
| What kind of water do you drink at home? | % cases (n = 95) | % controls (n = 95) | OR (95% CI) | aOR (95% CI)* |
|---|---|---|---|---|
| Water from antique neighbourhood fountains only | 72 | 15 | 15 (4·9–77) | 20 (4·6–84) |
| Mixed fountain and other water | 13 | 20 | 3·0 (0·54–30) | 2·1 (0·46–9·2) |
| Bottled or tap water only | 16 | 65 | Ref. |
OR, Odds ratio; aOR, adjusted odds ratio; CI, confidence interval.
Adjusted for age and sex using conditional logistic regression.
Stool specimens were collected from eight persons (six men and two women, average age 42 years, range 15–79 years). Laboratory investigation of the eight stool specimens at the reference laboratory at the Public Health Institution of Turkey identified various pathogens, including Shigella sonnei (two specimens), both astrovirus and norovirus (one specimen), both astrovirus and rotavirus (one specimen), and astrovirus (one specimen). None of the eight stool specimens yielded Giardia, Cryptosporidium, or E. histolytica.
Environmental investigation showed that the source of the tap water was a reservoir. This water was piped into a modern water-treatment plant, treated, and chlorinated using an automated system. However, the source of the groundwater flowing out of the antique fountains could not be determined because these antique fountains are protected by a Turkish law designed to protect cultural heritage. During November and December 2012, 68 peripheral water samples were taken for bacteriological analysis; 63 (93%) yielded no total coliforms or E. coli. Moreover, 252 peripheral water samples were taken during December 2012; 237 (94%) had a chlorine level ⩾0·2 ppm. On the other hand, water samples from nine antique neighbourhood fountains yielded highly elevated counts of total coliforms (range 38–300/100 ml) and E. coli (range 22–198/100 ml). Water from these antique fountains has been tested many times in the past and usually found to be microbiologically contaminated.
DISCUSSION
In this investigation of a gastroenteritis outbreak that affected more than 1000 people, illness was associated with drinking water from antique neighbourhood fountains. Laboratory investigation of clinical specimens indicated that multiple pathogens were involved in this outbreak. The fact that a high percentage of cases had bloody or mucus diarrhoea indicated that bacterial pathogens were significant causes during this outbreak. Water samples taken from the antique neighbourhood fountains showed heavy contamination.
In developed and developing countries alike, groundwater is routinely used, without treatment, as drinking water because it is considered safe [5, 6]. However, groundwater sources can be easily contaminated by agricultural run-off or improperly treated sewage, causing large community outbreaks [7–11]. In the USA, for example, the majority of waterborne disease outbreaks have been associated with contaminated groundwater, including large community outbreaks affecting thousands of people [12].
An outbreak of cryptosporidiosis and cyclosporiasis occurred in a village in western Turkey during September 2005. Subsequent investigation indicated that the outbreak was probably caused by contamination of the public drinking-water supply by sewage or animal waste after heavy precipitation [13]. Further, a waterborne acute diarrhoeal disease outbreak caused by group A rotavirus occurred during autumn 2005 in Malatya City, Turkey, affecting 9907 persons [14]. However, in general, such community outbreaks are rarely thoroughly investigated and documented. In Erzurum Province, the Public Health Directorate observed routine increases in gastroenteritis cases almost every spring and summer. This was the first time such a sharp increase in gastroenteritis cases had occurred in the winter, prompting this investigation. The fact that the two peaks in gastroenteritis cases occurred soon after the temperature reached above 0°C indicated that these outbreaks might have been due to the melting of underground ice, causing sewage contamination.
Research has repeatedly shown that water and sanitation improvements are cost-effective, especially in developing regions [15–17]. In developing countries, each US$1 invested in interventions to improve water and sanitation could result in a saving of US$5–46, depending on the type of intervention; the economic benefits of water improvement interventions include time saved due to easier access, increased productivity by the affected population, and savings in healthcare costs due to illnesses and deaths prevented [18]. In developed countries, improvement in water sanitation in the early to mid-20th century led to a sharp decline in the burden of many waterborne pathogens [19–21].
In Turkey, a sweeping statute on hygiene and sanitation was established in 1930. Among the many mandates of the statute was the requirement that all provinces should provide water meeting a sanitary standard to their residents [22]. As of 2013, residents in all urban centres have access to properly treated drinking water. However, waterborne outbreaks continue to occur [13, 14]. Part of the problem is that, in some cities in Turkey, there are antique neighbourhood fountains, some of which date hundreds of years back to the Ottoman or pre-Ottoman era. These fountains are antique structures, and legally protected by the Ministry of Culture and Tourism of Turkey. In the central city of Erzurum Province, 53 such antique neighbourhood fountains exist, all of which are located in the Yakutiye District, which is the oldest district of the central city. The water flowing out of these antique fountains comes from unknown underground sources; therefore, it is impossible for the municipal public health authority to treat the water. The local residents habitually drink water from these antique fountains in passing. They also drive up to these fountains, located in the old city's business district, to collect the water in large containers to carry home, which might explain the distribution of cases (see Fig. 3).
The main limitation of this study was that cases and controls were not closely matched by age and sex. To address this issue, we used conditional logistic regression to control for the potential confounding effects of these two factors. In addition, the use of next-door neighbours as controls could have biased the study findings since the water-drinking behaviours of these controls might be more similar to that of cases than to the well individuals in the general population.
In summary, this community-wide, multi-pathogen outbreak of gastroenteritis was caused by drinking water from contaminated antique neighbourhood fountains. After we submitted the investigation report, the city government convened a high-level meeting, and adopted a resolution to address the problem regarding the water from the antique neighbourhood fountains, to prevent such outbreaks in the future. Based on our recommendations, the provincial Public Health Directorate conducted a media campaign to warn residents against the use of water from the antique neighbourhood fountains. Subsequently, the provincial public health authority initiated a construction project to pipe in treated water from the municipal water-treatment plant to supply these antique neighbourhood fountains.
ACKNOWLEDGEMENTS
We thank the public health staff at the Erzurum Provincial Public Health Directorate for conducting the field study, data entry and cleaning.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.UNICEF/WHO. Diarrhoea: why children are still dying and what can be done. New York: United Nations Children's Fund, 2009.
- 2.Baker EL Jr., et al. Economic impact of a community-wide waterborne outbreak of gastrointestinal illness. American Journal of Public Health 1979; 69: 501–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dick J, Parrish NM. Microbiology tools for the epidemiologist. In: Nelson KE, Williams CM, eds. Infectious Disease Epidemiology Theory and Practice, 2nd edn. Boston: Jones and Bartlett Publishers, 2007, pp. 241–277. [Google Scholar]
- 4.Brock TD. Membrane Filtration: A User's Guide and Reference Manual. Madison, WI: Science Tech, 1983. [Google Scholar]
- 5.Gleick PH. The World's Water 2004–2005: The Biennial Report on Freshwater Resources. Washington, DC: Island Press, 2004. [Google Scholar]
- 6.Glennon RJ. Water Follies: Groundwater Pumping and the Fate of America's Fresh Waters. Washington, DC: Island Press, 2002. [Google Scholar]
- 7.Mac Kenzie WR, et al. A massive outbreak in Milwaukee of Cryptosporidium infection transmitted through the public water supply. New England Journal of Medicine 1994; 331: 161. [DOI] [PubMed] [Google Scholar]
- 8.Gallay A, et al. A large multi-pathogen waterborne community outbreak linked to faecal contamination of a groundwater system, France, 2000. Clinical Microbiology and Infection 2006; 12: 561–570. [DOI] [PubMed] [Google Scholar]
- 9.Mellou K, et al. A large waterborne gastroenteritis outbreak in central Greece, March 2012: challenges for the investigation and management. Epidemiology and Infection 2014; 142: 40–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laine J, et al. An extensive gastroenteritis outbreak after drinking-water contamination by sewage effluent, Finland. Epidemiology and Infection 2011; 139: 1105–1113. [DOI] [PubMed] [Google Scholar]
- 11.Fong T-T, et al. Massive microbiological groundwater contamination associated with a waterborne outbreak in Lake Erie, South Bass Island, Ohio. Environmental Health Perspectives 2007; 115: 856–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoder J, et al. Surveillance for waterborne disease and outbreaks associated with drinking water and water not intended for drinking – United States, 2005–2006. Morbidity and Mortality Weekly Report. Surveillance Summary 2008; 57: 39–62. [PubMed] [Google Scholar]
- 13.Aksoy U, et al. First reported waterborne outbreak of Cryptosporidiosis with cyclospora co-infection in Turkey. Eurosurveillance 2007; 12: 3142. [DOI] [PubMed] [Google Scholar]
- 14.Koroglu M, et al. A waterborne outbreak of epidemic diarrhea due to group A rotavirus in Malatya, Turkey. Microbiologica 2011; 34: 17. [PubMed] [Google Scholar]
- 15.Hutton G, Haller L. Evaluation of the costs and benefits of water and sanitation improvements at the global level. Geneva: World Health Organization, 2004. (http://wwwlive.who.int/entity/water_sanitation_health/wsh0404.pdf). Accessed 5 March 2014.
- 16.Clasen T, et al. Cost-effectiveness of water quality interventions for preventing diarrhoeal disease in developing countries. Journal of Water and Health 2007; 5: 599. [DOI] [PubMed] [Google Scholar]
- 17.Prüss-Üstün A, et al. Safer water, better health: costs, benefits and sustainability of interventions to protect and promote health. Geneva, Switzerland: World Health Organization, 2008, 60 pp (http://whqlibdoc.who.int/publications/2008/9789241596435_eng.pdf). Accessed 5 March 2014.
- 18.Hutton G, Haller L, Bartram J. Global cost-benefit analysis of water supply and sanitation interventions. Journal of Water and Health 2007; 5: 481. [DOI] [PubMed] [Google Scholar]
- 19.CDC. Achievements in Public Health, 1900–1999: control of infectious diseases. Morbidity and Mortality Weekly Report 1999; 48: 621–629. [PubMed] [Google Scholar]
- 20.CDC. Ten great public health achievements – worldwide, 2001–2010. Morbidity and Mortality Weekly Report 2011; 60: 814–818. [PubMed] [Google Scholar]
- 21.Wallace RB, Doebbeling BN, Last JM (eds). Maxcy-Rosenau-Last Public Health & Preventive Medicine, 14th edn. New York: McGraw-Hill Medical, 2008. [Google Scholar]
- 22.Republic of Turkey. Law on General Hygiene (No. 1489). Act No. 1593. 6 May 1930 (http://www.saglik.gov.tr/TR/belge/1-459/tarihi24041930--sayisi1593--rg-tarihi06051930--rg-sayis-.html). Accessed 5 March 2014.