Abstract
Critical illness is common throughout the world and is associated with high costs of care and resource intensity. The Corona virus disease 2019 (COVID-19) pandemic created a sudden surge of critically ill patients, which in turn led to devastating effects on health care systems worldwide and more so in Africa. This narrative report describes how an attempt was made at bridging the existing gaps in quality of care for critically ill patients at national and regional levels for COVID and the postpandemic era in a low income country.
Keywords: Intensive care units, Capacity building, Low-income country, Uganda, COVID
Key points
-
•
Uganda, like many other other low income countries, has very limited critical care capacity.
-
•
The COVID 19 pandemic spurred governtments efforts to improve critical care capacity not just for COVID but also for the post pandemic era.
-
•
This paper describes the process of building a low income country's critical care capacity in the pandemic era.
Introduction
Among people with COVID-19 about 5% have critical disease with complications such as respiratory failure, acute respiratory distress syndrome (ARDS), severe sepsis and septic shock, thromboembolism, and/or multiorgan failure, including acute kidney injury and cardiac injury.1 , 2 All these people required critical care, including admission to intensive care units (ICU), use of equipment to continuously monitor vital signs and support organs, as well as administration of specialized treatments. Similar to the rest of sub-Saharan Africa,1 Uganda’s limited ICU capacity was already well documented,3 and the COVID-19 pandemic had already required numerous countries to expand their surge capacity to meet the needs of patients with severe and critical illness.4, 5, 6 In anticipation of increased ICU admissions, understanding that medical oxygen was a critical need for the management of cases of COVID-19, the government of Uganda decided to strengthen critical care health care services at regional referral hospitals by establishing numerous ICU around the nation, to avoid overwhelming the new ICU at national referral hospital at Mulago. It was also recognized that the national medical oxygen scale-up implementation plans needed updating.
General Response
In anticipation of the COVID-19 pandemic, the Ugandan Ministry of Health activated the Incident Management System through the National Task Force (NTF) and District Task Forces for coordination of the COVID-19 response and preparedness.7 The NTF is multisectoral and multidisciplinary in nature, comprising of key ministries, agencies, and departments as well as partners and relevant stakeholders, and works through its subcommittees. The NTF assigned an Incident Management Commander as the overall team lead of the response that had 9 pillars: Surveillance, Case management, Laboratory, Risk Communication, Logistics, SIRI (Strategic Information Research and Innovations), Community Engagement, Vaccination, and Continuity of Essential Health Services.
Critical Care Planning Committee
In April 2020, the national critical care subcommittee was drawn from ICU clinicians, Ministry of Health senior management, biomedical engineers, and development partners under the Continuation of Essential health services pillar.
Conceptual Framework Underpinning This Exercise
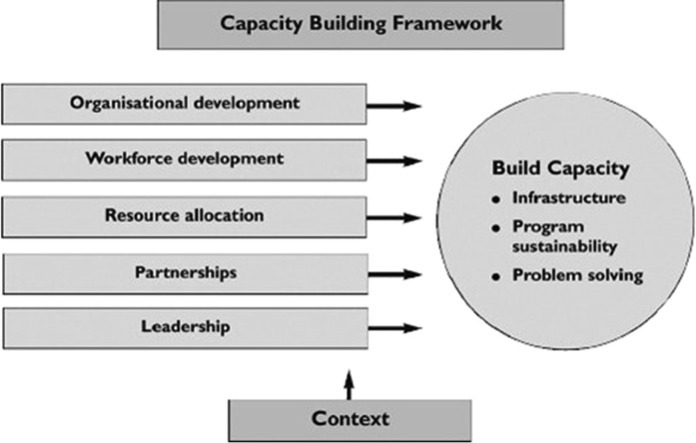
We modified the approach used by Arabi and colleagues,8 which drew on concepts from a capacity building model by Hawe and colleagues.9 This model has within its framework key strategies we considered important to guide our exercise. These strategies were organizational development, workforce development, resource allocation, leadership, and partnership. We initially focused on building the capacity around 3 domains: infrastructure, human resources, and sustainability (instead of problem solving) (Fig. 1 ).
Fig. 1.
Conceptual framework underpinning this exercise.
Therefore, the response was divided into 2 assignments: (1) needs assessment, (2) interventions.
Summary of Uganda’s Healthcare System
According to the ministry of health,10 the number of health facilities (public, private, and private not for profit) in Uganda now totals 6937. The data also show that 45.16% (3133) of health facilities are government owned, 14.44% (1002) are private and not for profit (PNFP), whereas the remaining 40.29% (2795) are private for profit and 0.10% (7) community-owned facilities.
The government and PNFPs are mostly higher levels of health facilities, whereas the private for profit facilities majorly consists of lower levels (Health Center II [HC IIs] and clinics).
Uganda’s health facilities are stratified into 7 levels based on the services they provide and the catchment area they are intended to serve. The lowest level health facilities are designated as HC I followed by HC II to HC IV as level 2 to level 4 health facilities with ability to provide more health services: General Hospital (GH), Regional Referral Hospital, and National Referral Hospitals as the topmost level facilities in this structure.
Referrals for patient care follow this level of stratification. In addition, the country now has 5 Specialized Hospitals, which include Mulago National Specialized Hospital, Mulago Specialized Women and Neonatal Hospital, Regional Pediatric Surgical Hospital in Entebbe, Uganda Heart Institute, and Uganda Cancer Institute.
The country also has 4 National Referral Hospitals, namely Mulago National Referral Hospital, Kawempe National Referral Hospital, Kiruddu National Referral Hospital, and Butabika National Referral Hospital. There are 16 Regional Referral Hospitals and 62 GHs in the country.
Intensive care services start at the regional referral hospital level, where the scheme of service for the anesthesiologist begins.
Assessment of Human Resource for Critical Care Provision
The assessment was carried out using telephonic surveys as well as site visits. A structured questionnaire was used to determine the number of acute care providers.
As many African countries, physician-anaesthesia providers play a leading role in management of critical illness11; however, this health workforce is still a key bottleneck for the appropriate provision of critical care health services, with key challenges such as inadequate numbers of anesthesiologists, limited skills, retention, motivation, and service delivery.12 According to the Ministry of Health, only one-quarter of the anesthesia human resource required in Uganda as of 2020 had been met to match the Health Sector Development Plan 2020 (eg, Uganda has less than 30 registered public sector anesthesiologists compared with the 359 required).13 Likewise in the nursing sector, there were 171 ICU nurses, of whom only13 had formal training in critical care nursing (and yet the country needed about 2400 ICU/ high dependency unit [HDU] nurses).3 At the national referral hospital ICU, there is a modular critical care training initiative, leading to a World Federation of Critical Care Nurses–accredited competency certificate.
Several reasons leading to the critical shortage of this cadre were highlighted in this assessment: production of critical care professionals does not adequately match health service needs and demands. The number of physician and nonphysician anesthetists graduating each year is meager and cannot fill the ever-widening gaps. There was only one critical care nurses’ program at the time, and it graduated a handful of nurses per year.
As a means of temporarily closing the gap (task shifting), the government developed the anesthetic officer training program. However, their training focused on perioperative medicine and not critical care.
Later an improved program, the Bachelor of Science (BSc) in anesthesia, was developed and launched. However, the program is still in its nascent stages and is slowly picking momentum.
We noted low staff retention and motivation mainly stemming from a lack of paths for career development as well as low pay. Inadequate remuneration further undermines efforts at recruitment, retention, and effective service provision.
It was also noted that in the current staffing structure, there is no unifying body or cadre to provide the much-needed visionary leadership, setting, and monitoring of standards, co-ordination with regulatory bodies, health policy formulation and analysis, and creation of a sense of mission in critical care services in Uganda.
Assessment of Infrastructure for Critical Care Services
Data from a recent (2019) study of the country’s ICU capacity revealed only 12 functional ICUs, most of which were in the central region. There were 55 ICU beds making up a ratio of 1.3 ICU beds per million population.3 The ICU beds comprised 1.5% of the total bed capacity of the studied hospitals. Most of the ICUs were mixed (paediatric-adults), anaesthesia-led were 9 and 5 operated in a closed model. An additional assignment to update this information was proposed, to inform planning.
The assignment was split into 2 components. (1) the national survey and (2) the quantification exercise. Because this was a public health emergency response with no patients involved, there was no need for ethical approvals required from regulatory bodies.
The national survey was conducted by teams of biomedical engineers and technicians based at 16 regional referral hospitals. Each health subdistrict is served by the regional referral hospital. Data were gathered by site inspections and through researcher administered questionnaires. The findings confirmed the study findings.
Assessment of Oxygen Capacity
A previous quantification for the national oxygen plan had assumed that at least 124,348 m3 per month would be needed as of to fulfill the oxygen need of all public facilities from HC IV, GH, regional referral hospitals, and the national referral hospitals. Admittedly, this was made on the back of inadequate data and best estimates.
We assessed 16 referral hospitals around the country. The national referral hospital at Mulago was assessed in 2 sections, that is Upper Mulago National Referral Hospital and Lower Mulago National Referral Hospital because the 2 have had independent oxygen supplies for some years now.
The study team conducted this assessment during physical visits to the hospitals over a period of 3 months/weeks. We obtained information on sources of oxygen, functionality of the oxygen sources, backup sources of power, human resource attending to hospital oxygen needs, and presence of a HDU or ICUs within the facility.
The sources of oxygen identified at the various hospitals included Pressure Swing Adsorption oxygen plants, oxygen concentrators, and oxygen cylinders.
Of the 16 regional referral hospitals assessed, all used oxygen cylinders and oxygen concentrators in different parts of the hospitals, and 17 hospitals had oxygen plants.
All hospitals reported unstable power supply for their oxygen service, with black outs occurring every week. Only one hospital had a back-up power source specifically for their oxygen plant. All hospitals reported having generators for backup power supply for GH activities.
All hospitals had staff assigned to the oxygen plants/supply. However, 2 hospitals had 1 staff to run these activities for the entire week, 3 had 2 staff, and the rest had 3 or more staff. Moroto and Fort portal had the highest number of staff (7) for this purpose.
We determined that the regional referral hospitals’ pressure swing adsorption plants could only produce 120,000 L of oxygen in an 8-hour work shift; this is equivalent to 17 cylinders of the J size, which were the most common cylinders available.
Interventions
Human resources
A multidisciplinary team that included ICU-based anaesthesiologists and physicians, biomedical engineers, and human resources administrative staff was set up to develop a human resource for critical care plan. Continuous stakeholder engagements were made, and a strategy evolved. This strategy had short-, medium-, and long-term goals. Short-term goals included short courses in critical care nursing, oxygen therapy, and infection prevention for patient management during the COVID-19 pandemic; this was done by in-service training of existing health workers. The association of Anaesthesiologists of Uganda with support from development partners and in conjunction with the ministry did this by training dedicated ICU staff at the regional referral hospitals; this was supplemented by recruitment of health workers on short-term contracts for the pandemic response. The medium- and long-term goals focus on identifying and increasing the presence of critical care specialists at the regional referral hospitals; this is being done by development of a 4-year collegiate training program (based on the College of Anaesthesiologists of East, Central, and Southern Africa (CANECSA) anaesthesiology and critical care curriculum) that would target and retain medical officers at the regional referral hospitals; this is intended to supplement the current Master of Medicine Specialist programs at the 2 national universities (Makerere and Mbarara) that are inadequate to cater for national needs.13 In addition, the Ministry of Health through its existing collaboration with National Health Service Health Education England has developed a government-to-government program to develop specialty training in key areas of the health sector including Critical Care. The Strengthening Workforce Capacity through global Learning in Critical Care (SCALE-Critical Care) is expected to develop human resource capacity to deliver intensive care at facility level as well as drive health system improvement. The program will further create opportunities for virtual learning and global placements to UK professionals and trainees to learn from a clinically rich environment in Uganda. The overall goal of the program is to increase critical care capacity through workforce development between Uganda and the UK by developing distant learning in critical care between training institutions in Uganda and the UK; enabling Ugandan Health workers benefit from the Medical Training Initiative Scheme and other training and scholarship pathways in the UK for critical care; and increasing Global Placement of UK professionals to support Critical Care training, practice, and research in Uganda. In addition, a pulmonary critical care fellowship is in the later stages of development.
Regarding critical care nursing, capacity building began with the Ministry of Health’s recognition of critical care nursing as a nursing subspecialty, followed by inclusion of dedicated salaried posts in critical care nursing in the health service commission at the regional and national referral hospital levels. Before the COVID-19 pandemic, the only recognized critical care nursing training program was a master’s in nursing (Critical Care Nursing) offered at one university in the country. The Ministry of Health further provided 25 scholarships for Masters in Critical Care Nursing and 400 slots for an In-service Certificate in Intensive Care Nursing taught at Mbarara University of Science and Technology. In addition, 2 other universities are now offering postgraduate studies in critical care nursing. There is also continuous engagement at a multisectoral level, to retain and remunerate the various cadres that have successfully completed these courses/programs.
Infrastructure
The quantification exercise was conducted through a series of meetings in which clinical data from the regional referral hospitals were used to determine ICU bed capacity per hospital and in line with human resources as well as budgetary allocations.
Clinical scenarios were created to aid in planning. In all scenarios COVID-19 and non-COVID-19 care was considered. In addition, the costing exercise took into consideration all supplies and consumables expended during treatment of a critically ill patient, regardless of age.
Reference was made to the national oxygen plan National Scale up of Medical Oxygen Implementation Plan (2018–2022)14 to enable the team to leverage the exercise on existing infrastructure.
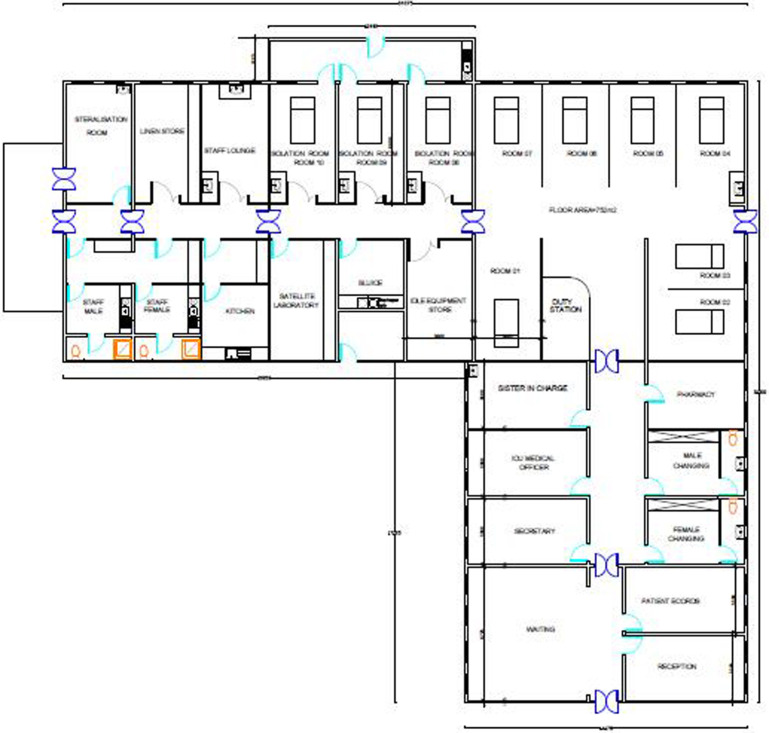
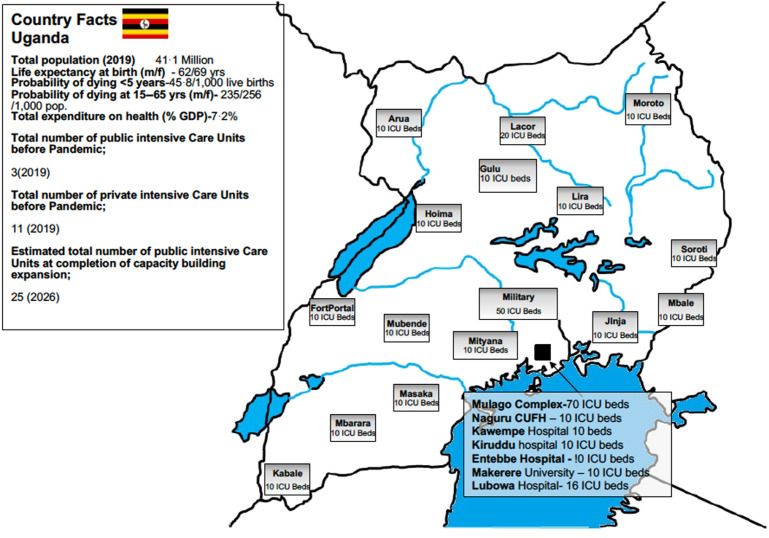
As a result, the decision was to construct/renovate and equip 10-bed ICUs at all regional referral hospitals. To provide guidance and recommendations for the planning or renovation of intensive care units, the committee of the health infrastructure division was composed of biomedical engineers, and critical care clinicians used various evidence-based resources with context in consideration.15, 16, 17 The planned units were to be open semipartitioned general ICUs staffed by a mix of both critical care– and noncritical care–trained nurses. The highest form of organ support therapy to be provided was cardiorespiratory in terms of mechanical ventilation and use of vasopressors. Specifications for major ICU equipment (such as mechanical ventilators, high-flow oxygen devices, fluid infusion, medical furniture, patient monitors) were designed according to the National Equipment Guidelines,18 and in addition, local biomedical limitations were put into consideration. For example, the lack of medical air meant that ventilators had to have their own source of driving gas (turbine or other electronically driven pneumatics). Floor plans for the units considered patient flow/monitoring as well as possible future poor staffing ratios. Later, some ICUs had isolation units (± negative pressure), added as extensions (Fig. 2 ). In addition, an update of planned ICUs from other public sectors was created (Fig. 3 ).
Fig. 2.
ICU design for regional referral hospitals.
Fig. 3.
Distribution of planned and built public intensive care units across the country.
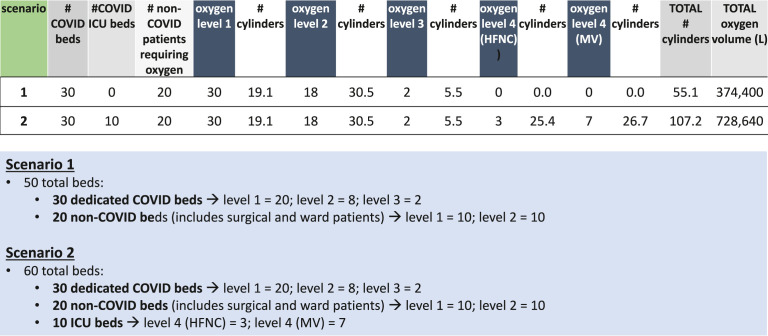
Oxygen Quantification
The committee came up with 2 clinical scenarios borne out of the national response plan (Fig. 4 ); this was based on assumptions modeled by the scientific advisory committee that at worst case scenario ∼180,000 total cases to be registered up to the period 20th August of 2020 with the proportion of cases needing oxygen at 15% severe (27,000) and 5% critical (9000). We assumed the ratio of adults to pediatric cases would be 9:1 and each of the 16 treatment centers to manage 2250 severe and critical care cases.
Fig. 4.
Oxygen demand for 2 different COVID-19 scenarios with and without dedicated ICU beds (6800L).
Firstly, illness severity was graded according to oxygen demand (determined by the average flow rate) on a scale 1 to 4 as follows: 1 = 3 L/min by nasal prongs; 2 = 8 L/min by simple Hudson or venturi face mask; 3 = 12 to 15 L/min by nonrebreather mask; 4 = 20 to 60 L/min by CPAP/NIV/IMV/HFNC.
Being that at the time there were no functional ICUs at most hospitals, demand was expected from the repurposed 30-bed COVID isolation wards and from ongoing hospital care (operating theaters, labor wards, emergency department); this created the basis for the first scenario (see Fig. 4).
The second scenario took into consideration the new 10-bed ICU infrastructure that was being planned and added this to all aspects of scenario 1 (see Fig. 4).
It was therefore predicted that at surge, in scenario 1, the 30 dedicated COVID beds would have 20 level one patients; 8 level two; and 2 level three patients. The 20 non-COVID beds (includes surgical and ward patients) 10 level one patients and 10 level two patients.
In scenario 2, the 30 dedicated COVID beds would have 20 level one patients, 8 level two, and 2 level three patients. The 20 non-COVID beds (includes surgical and ward patients) 10 level one patients and 10 level two patients. In addition, there would be 10 ICU patients, 7 on mechanical ventilation and 3 on high-flow nasal cannula, all at level four status.
Following the aforementioned process, it was calculated that each regional referral would need to generate 374,400 L of oxygen per day for scenario 1 and 728,640 L of oxygen per day for scenario 2 (see Fig. 4).
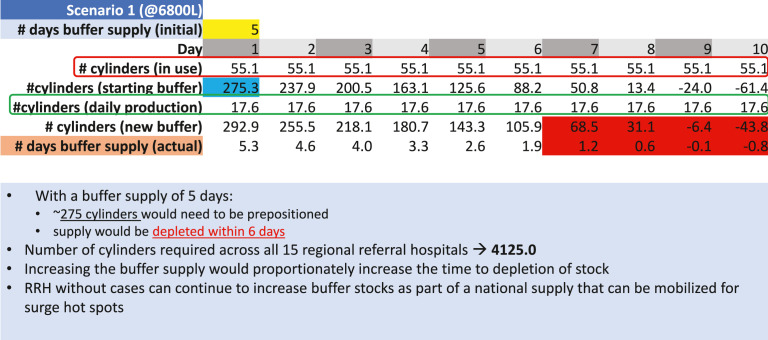
In addition, it was determined that prepositioning a buffer supply of 275 cylinders was needed to ensure sufficient oxygen buffer supply of 5 days for scenario 1. It was also determined that these 275 cylinders would be depleted within 6 days, and therefore, the number of cylinders required across all 15 regional referral hospitals to be 4125 (Fig. 5 ).
Fig. 5.
Prepositioning a buffer supply of cylinders to ensure sufficient oxygen supply for a finite period (Scenario 1).
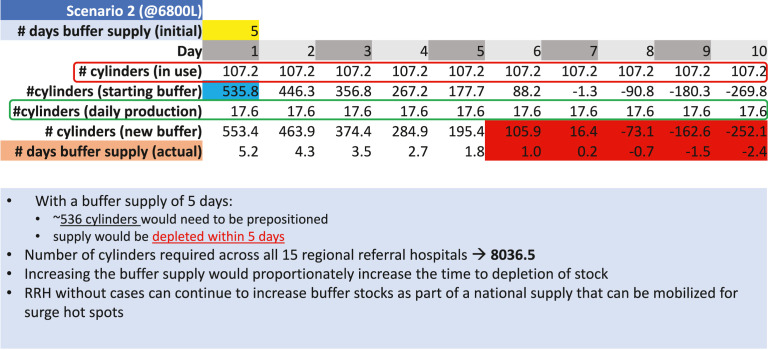
For scenario 2, it was determined that prepositioning a buffer supply of 536 cylinders was needed to ensure sufficient oxygen buffer supply of 5 days for scenario 1. It was also determined that these cylinders would be depleted within 6 days, and therefore, the number of cylinders required across all 15 regional referral hospitals to be 8036 (Fig. 6 ).
Fig. 6.
Prepositioning a buffer supply of cylinders to ensure sufficient oxygen supply for a finite period (Scenario 2).
Challenges
Introduction or scale-up of a relatively new specialty in a low-resource setting is conflicted by competition with limited resources. Making significant additions to the national drug/consumables’ procurement process required frequent engagement with key stakeholders; this was quite difficult to do in the middle of a budget cycle and a pandemic.
Global consensus on appropriate nurse-to-patient ratio in resource-limited ICUs has not yet been achieved.4 , 16 Some HIC data were used to inform some of the planning for recruitment and retention, although ultimately the number of nurses who received training was decided by whichever resources were available.
We have experienced underutilization of procured equipment because of the continued of lack of human resources. In addition, the demand for critical capacity still far outstrips the pace of training. For example, technicians were expected to carry out their day jobs (maintaining hospital equipment) while also running the plants. There is no night shift, so the plants were run at half capacity. There were no backup generators, and power cuts shut off the supply.
There was frequent burnout among key people in this process. The already few critical care human resources also participated in COVID case management, as well as other sector responses. Many fell ill and had to isolate themselves, with a few needing hospitalization; this had a significant impact on the capacity building process and has been observed globally.19
There is a lack of contextual evidence to drive practice guideline development, and this has limited the development process to “best practice” protocols or using guidelines that have taken into consideration diversity of resources. In addition, we also noted that there was poor or no implementation of recommendations from locally conducted done research.
Future Considerations
Building up a national ICU system from scratch is a laborious and expensive undertaking, more so when done in a resource-limited setting. This is an ongoing project, which is likely to undergo significant evolution, as lessons are learned and there is an improvement in resource allocation for critical care. The most important hurdle will be improving the quality and quantity of the human resource.
The care for the critically ill patient in Africa places significant strain on an already constrained health care system, which means that significant focus should go to capacity building in recognition and treatment of life-threatening acute illness. Early interventions reduce organ dysfunction progression and lessen the strain on limited resources20; this is what the bulk of our short-term training courses are focused on.
By using the “chain of survival” model enables the concept of “task sharing” to be appropriately adopted, with every cadre having an important role from “bystander” recognition of critical illness to the intensivist in the ICU along a referral continuum. Other acute care professions with relatively similar skillsets can be positioned along this continuum. This brings in the importance of strengthening prehospital care and emergency unit professionals’ capacity to fill the gaps in this continuum. One such program that seems to embrace this is the Essential Emergency and Critical Care (EECC).21 EECC is defined as the care that should be provided to all critically ill patients of all ages in all hospitals in the world. It is distinguished by 3 principles: first, priority to those with the most urgent clinical need, including both early identification and timely care; second, provision of the life-saving treatments that support and stabilize failing vital organ functions; and third, a focus on effective care of low cost and low complexity. We are considering a clinical trial in our setting for this.
One such example is one where a staffing model allows accredited critical care personnel (critical care trained anesthesiologists, emergency, and internal medicine physicians) to oversee nonaccredited staff and for outside specialists to contribute to areas in which they excel, such as nonphysician anesthesiologists and emergency care physicians managing airways; this has been alluded to in a white paper.16 Uganda has already laid the foundation for this framework. And the next steps would be to harmonize this process.
Embracing point of care medicine in the “chain of survival” would minimize delays, reduce cost of care, and prevent congestion at diagnostic departments. The COVID pandemic highlighted the importance of lung ultrasound in helping improve management while maintaining infection control and prevention, and this is one of many ways in which critical care will never be the same.5
Conducting critical care research in low- and middle-income countries (LMICs) is hampered by lack of skills and funding. The lack of context-specific research impairs treatment guideline development. Even when research is done, data collected during clinical studies are based on specific research questions of a time-limited value.
In high-income countries ongoing patient registries provide a continual evaluation of service provision, epidemiology, and quality of care by providing real-time access to data.22 In Uganda we are establishing a national perioperative and ICU registry, which is hoped to provide a platform for shared learning as well as embed clinical research. It will strengthen our understanding of the burden of surgical and critically ill patients in Uganda and allow us to continually improve the quality of patient care in the country.
Evidence suggests that treatment by trained critical care providers improves survival in critically ill patients.23 In LMICs, many critically ill patients lack access to this cadre. A telemedicine technology–based approach where experienced critical care–trained providers can monitor and treat patients from a centralized location can help address this issue. This has the potential improving the overall quality of care. Although published studies of ICU telemedicine show mixed results,24 studies that consider context are associated with improvements in adherence to simple evidence-based daily care processes and survival outcomes.25 , 26
As in some LMICs, Ugandan ICU patients’ treatment costs are often not fully covered by the health/insurance systems; this implies that patients and their families incur high out-of-pocket expenses. Indeed, this was the experience at the height of the COVID pandemic. The possible solution to ensuring a minimum critical package lies in the ongoing setup of the national health insurance and ministry of health cost-sharing schemes and regional and national referral hospitals. An intentional and well-thought-out stand-alone critical care financing policy/package would ensure equitable access for most of the people who would otherwise find the costs prohibitive.
Summary
This paper highlights a systematic, multisectoral approach to build ICU (critical care) capacity in a low-income, low-resource setting for COVID and beyond. We share on-going challenges, important lessons learned so far, and perspectives for the future.
Clinics care points
-
•
The critical care or intensive care unit is an important place in the healthcare system for supportive management of patients with acute organ dysfunction.
-
•
Availability of well-resourced critical care facilities is associated with a reduction in all cause morbidity and mortality.
-
•
Low-income countries have severely limited and under resourced critical care capacity. The COVID pandemic left many countries severely exposed.
-
•
Building national critical care capacity in a low-income country is a continuous resource consuming multidisciplinary process.
Author contributions
A. Kwizera conceptualized the article. All authors made substantial contributions to the writing of the manuscript article as well as to the process described in the article.
Funding sources: no funding was used for this effort.
Acknowledgments
The authors would like to thank the ministry of health and all stakeholder in the government of Uganda for their role in this effort.
Disclosure
The authors have no conflicts of interest to declare with regard to this article.
References
- 1.African C-CCOSI Patient care and clinical outcomes for patients with COVID-19 infection admitted to African high-care or intensive care units (ACCCOS): a multicentre, prospective, observational cohort study. Lancet. 2021;397(10288):1885–1894. doi: 10.1016/S0140-6736(21)00441-4. [published Online First: 2021/05/24] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Estenssoro E., Loudet C.I., Rios F.G., et al. Clinical characteristics and outcomes of invasively ventilated patients with COVID-19 in Argentina (SATICOVID): a prospective, multicentre cohort study. Lancet Respir Med. 2021;9(9):989–998. doi: 10.1016/S2213-2600(21)00229-0. [published Online First: 2021/07/06] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Atumanya P., Sendagire C., Wabule A., et al. Assessment of the current capacity of intensive care units in Uganda; A descriptive study. J Crit Care. 2020;55:95–99. doi: 10.1016/j.jcrc.2019.10.019. [published Online First: 2019/11/13] [DOI] [PubMed] [Google Scholar]
- 4.Kodama C., Kuniyoshi G., Abubakar A. Lessons learned during COVID-19: building critical care/ICU capacity for resource limited countries with complex emergencies in the World Health Organization Eastern Mediterranean Region. J Glob Health. 2021;11:03088. doi: 10.7189/jogh.11.03088. [published Online First: 2021/07/31] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arabi Y.M., Azoulay E., Al-Dorzi H.M., et al. How the COVID-19 pandemic will change the future of critical care. Intensive Care Med. 2021;47(3):282–291. doi: 10.1007/s00134-021-06352-y. [published Online First: 2021/02/23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caresia C.E. Management of critically ill COVID-19 patients: challenges and affordable solutions. Pan Afr Med J. 2021;38:270. doi: 10.11604/pamj.2021.38.270.28689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ministry of Health U. Uganda COVID19 Response and preparedness plan. 2020.
- 8.Arabi Y.M., Taher S., Berenholtz S.M., et al. Building capacity for quality and safety in critical care: a roundtable discussion from the second international patient safety conference in April 9-11, 2013, Riyadh, Saudi Arabia. Ann Thorac Med. 2013;8(4):183–185. doi: 10.4103/1817-1737.118480. [published Online First: 2013/11/20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hawe P., Lloyd B., King L., et al. NSW Health Department; 2000. Indicators to help with capacity building in health promotion. [Google Scholar]
- 10.Ministry of Health U. Uganda’s healthcare provider network. 2021.
- 11.Metogo J.A.M., Tochie J.N., Etoundi P.O., et al. Anaesthesiologist-intensivist phycisians at the core of the management of critically ill COVID-19 patients in Africa: persistent challenges, some resolved dilemma and future perspective. Pan Afr Med J. 2020;37(Suppl 1):44. doi: 10.11604/pamj.supp.2020.37.44.25234. [published Online First: 2021/02/09] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lipnick M.S., Bulamba F., Ttendo S., et al. The need for a global perspective on task-sharing in anesthesia. Anesth Analg. 2017;125(3):1049–1052. doi: 10.1213/ANE.0000000000001988. [published Online First: 2017/04/30] [DOI] [PubMed] [Google Scholar]
- 13.F Bulamba R.B., Kimbugwe J., Ochieng J.P., et al. Development of the anaesthesia workforce and organisation of the speciality in Uganda: a mixed-methods case study. South Afr J Anaesth Analg. 2022 doi: 10.36303/SAJAA.2022.28.3.2646. [DOI] [Google Scholar]
- 14.Ministry of Health U. National Scale up of Medical Oxygen Implementation Plan. 2018-2022. 2018.
- 15.Papali A., Adhikari N.K.J., Diaz J.V., et al. In: Sepsis management in resource-limited settings. Dondorp A.M., Dunser M.W., Schultz M.J., editors. CH); Cham: 2019. Infrastructure and organization of adult intensive care units in resource-limited settings; pp. 31–68. [PubMed] [Google Scholar]
- 16.Losonczy L.I., Papali A., Kivlehan S., et al. White paper on early critical care services in low resource settings. Ann Glob Health. 2021;87(1):105. doi: 10.5334/aogh.3377. [published Online First: 2021/11/18] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Valentin A., Ferdinande P., Improvement EWGoQ. Recommendations on basic requirements for intensive care units: structural and organizational aspects. Intensive Care Med. 2011;37(10):1575–1587. doi: 10.1007/s00134-011-2300-7. [published Online First: 2011/09/16] [DOI] [PubMed] [Google Scholar]
- 18.Ministry of Health U. National Medical Equipment Policy. 2009.
- 19.Mehta S., Machado F., Kwizera A., et al. COVID-19: a heavy toll on health-care workers. Lancet Respir Med. 2021;9(3):226–228. doi: 10.1016/S2213-2600(21)00068-0. [published Online First: 2021/02/09] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turner H.C., Hao N.V., Yacoub S., et al. Achieving affordable critical care in low-income and middle-income countries. BMJ Glob Health. 2019;4(3):e001675. doi: 10.1136/bmjgh-2019-001675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schell C.O., Khalid K., Wharton-Smith A., et al. Essential Emergency and Critical Care: a consensus among global clinical experts. BMJ Glob Health. 2021;6(9) doi: 10.1136/bmjgh-2021-006585. [published Online First: 2021/09/23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haniffa R. Linking of global intensive care c. Future perspectives for clinical quality registries in critical care. J Crit Care. 2021;63:279. doi: 10.1016/j.jcrc.2020.12.004. [published Online First: 2020/12/15] [DOI] [PubMed] [Google Scholar]
- 23.Diaz J.V., Riviello E.D., Papali A., et al. Global critical care: moving forward in resource-limited settings. Ann Glob Health. 2019;85(1):3. doi: 10.5334/aogh.2413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kahn J.M., Rak K.J., Kuza C.C., et al. Determinants of intensive care unit telemedicine effectiveness. An ethnographic study. Am J Respir Crit Care Med. 2019;199(8):970–979. doi: 10.1164/rccm.201802-0259OC. [published Online First: 2018/10/24] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kovacevic P., Dragic S., Kovacevic T., et al. Impact of weekly case-based tele-education on quality of care in a limited resource medical intensive care unit. Crit Care. 2019;23(1):220. doi: 10.1186/s13054-019-2494-6. [published Online First: 2019/06/16] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Flurin L., Tekin A., Bogojevic M., et al. International virtual simulation education in critical care during COVID-19 pandemic: preliminary description of the virtual checklist for early recognition and treatment of acute illness and iNjury program. Simul Healthc. 2022;17(3):205–207. doi: 10.1097/SIH.0000000000000656. [published Online First: 2022/04/20] [DOI] [PMC free article] [PubMed] [Google Scholar]