SUMMARY
The incidence of respiratory syncytial virus (RSV) has been reported to exhibit seasonal variation. However, the impact of diurnal temperature range (DTR) on RSV has not been investigated. After acquiring data related to cases of RSV and weather parameters of DTR in Fukuoka, Japan, between 2006 and 2012, we used negative binomial generalized linear models and distributed lag nonlinear models to assess the possible relationship between DTR and RSV cases, adjusting for confounding factors. Our analysis revealed that the weekly number of RSV cases increased with a relative risk of 3·30 (95% confidence interval 1·65–6·60) for every 1°C increase in DTR. Our study provides quantitative evidence that the number of RSV cases increased significantly with increasing DTR. We suggest that preventive measures for limiting the spread of RSV should be considered during extended periods of high DTR.
Key words: Climatic change, diurnal temperature range, respiratory syncytial virus
INTRODUCTION
Respiratory syncytial virus (RSV) is the leading cause of lower respiratory tract infections and hospitalizations in infants and young children worldwide [1]. The incidence of RSV follows a seasonal pattern in temperate areas, with marked peaks in the winter season in the northern and southern hemispheres [2]. Despite this regular occurrence, differences exist in the region, duration, and magnitude of transmission periods [3]. New information regarding the regional dynamics of RSV epidemics would broaden our understanding of RSV transmission, thus helping to predict or prevent these epidemics.
The incidence of RSV has been reported to exhibit seasonal variation in a number of different areas. For example, ambient temperature was found to be inversely associated with RSV activity in China and Tunisia [4, 5]. In Malaysia, RSV cases were found to be directly correlated with rainy days and inversely correlated with temperature and humidity [6]. In the USA, it was found that RSV activity (1) peaked in summer and early autumn at sites with persistently warm temperatures and high humidity; (2) was maximal during winter, correlating with lower temperatures in temperate climates; and (3) was nearly continuous in areas where temperatures remained cold throughout the year [7]. In Germany and Italy, RSV infections were found to be correlated with decreasing temperature [8, 9]. In Mexico and Turkey, an increase in RSV activity was found to be significantly associated with lower temperature and higher humidity [10, 11]. In Hong Kong, RSV epidemics are more frequent during the rainy season when temperatures are high [12], while RSV cases in other studies showed a significant positive correlation with temperature and humidity [13]. In Singapore, the daily viral detection rates of RSV were found to be associated with higher temperatures, lower humidity, and higher diurnal temperature variation [14]. In Indonesia, it has been suggested that a significant increase in the risk of RSV is associated with an increase in temperature, humidity, and rainfall [15]. The observed seasonality of RSV both suggests that its incidence may be influenced by weather factors. Despite this speculation, the impact of diurnal temperature range (DTR) on the incidence of RSV, with adjustment for the mutual confounding between weather and other seasonal factors, has not been investigated in previous studies.
The present study examines the possible relationship between DTR and the incidence of RSV cases using surveillance data collected in Fukuoka, Japan, during the period of 2006–2012.
METHODS
Data sources
In Fukuoka Prefecture, which is located in the southwest of Japan, the number of RSV patients is reported to the Fukuoka Prefectural Government on a weekly basis from 120 sentinel medical institutions [16]. Cases are defined by clinical factors and laboratory tests. Clinical manifestations include a variety of respiratory illnesses, from cold-like symptoms to bronchitis, croup, and lower respiratory infections like bronchiolitis and pneumonia, according to the Act on Prevention of Infectious Diseases and Medical Care for Patients Suffering Infectious Diseases [17]. We obtained data that were reported by sentinel clinics and hospitals to the Fukuoka Institute of Health and Environmental Sciences, the municipal public health institute of the Fukuoka Prefectural Government. In addition, we also obtained data on daily minimum temperature, maximum temperature, average temperature, relative humidity and rainfall in Fukuoka Prefecture from the Japan Meteorological Agency. Weekly DTR was calculated as the weekly means for DTR. DTR was calculated as the daily maximum temperature minus the daily minimum temperature. Weekly means for temperature, relative humidity and rainfall were calculated from the daily records.
Statistical analysis
We used negative binomial generalized linear models with robust error variances to examine the relationship between the number of weekly RSV cases and DTR [18]. We also included mean temperature, humidity, and rainfall in the model to control for the effects of weather factors. To account for the seasonality of RSV cases that were not directly due to the weather, the model included Fourier terms up to the sixth harmonic. Fourier terms can be used to re-create any periodic signal, such as a consistent seasonal pattern, using a linear combination of sine and cosine waves of varying wavelengths [19]. The number of harmonics defines the lowest wavelength reproduced (i.e. the level of seasonal adjustment), with six harmonics corresponding to a wavelength of 9 weeks (i.e. one-sixth of a year). Indicator variables for the years under study were incorporated into the model to allow for long-term trends and inter-annual variations. To allow for autocorrelations, an autoregressive term of order 1 was incorporated into the models [20]. Plots of model residuals, predicted and observed time-series plots, and the partial autocorrelation function of the residuals (Supplementary online data, Fig. S1) suggested that this adjustment for seasonal trends was adequate.
Based on the results of exploratory analyses with the lowest deviance of the above-described models, we considered lags (delays in effect) of up to 16 weeks when analysing the influence of DTR on the number of RSV cases. In initial analyses designed to identify the broad shape of any association, we fitted a natural cubic spline (3 d.f.) [21] to the average DTR over lags of 0–16 weeks. We then fitted the data to linear models to quantify the change in disease risk associated with DTR. The choice of model (i.e. linear or threshold) [22] was based on our comparison of deviance in the models derived from likelihood ratio tests [23]; models with lower deviance are preferred. When the difference in the values of deviance between the linear and best-fit threshold models was <3·84 (χ2 value for 1 d.f. at the P = 0·05 level), the linear model was selected for simplicity. The observed values of deviances suggested that there was little change in the deviance between the linear and threshold models; thus, we assumed that linear models without a threshold were appropriate for assessing the associations between DTR and the incidence of RSV cases (the model is described in Protocol S1, online).
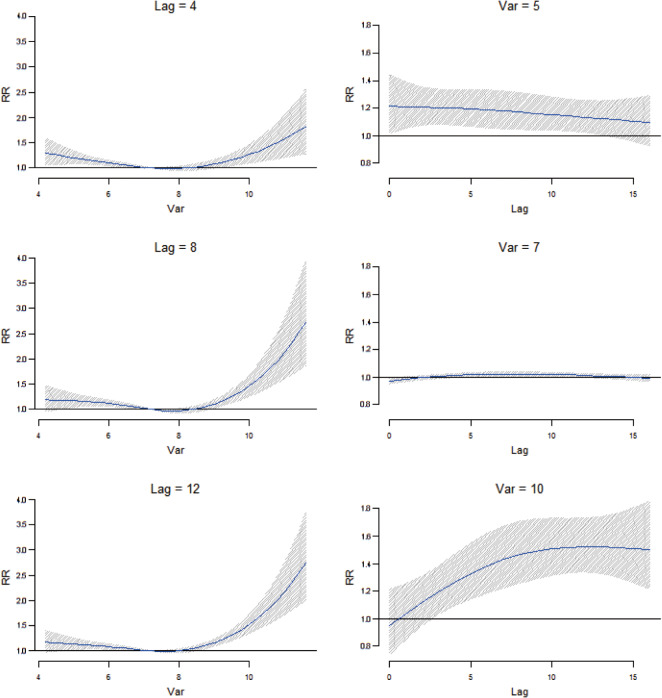
We also examined DTR–morbidity curves and lag effects in more detail using a quasi-likelihood Poisson regression model with distributed lag nonlinear model [24] adjusted for the confounding factors of temperature, humidity, rainfall, year, and seasonality. A distributed lag nonlinear model was developed on the basis of cross-basis function, which allows for the simultaneous estimation of possible nonlinear associations across lag periods [24]. Regarding the space of lags, we defined cubic spline with the natural constraint for the lag dimension of DTR. The knots for the spline for lags were placed at equally spaced values in the log scale of lags. Lag stratification was defined as 3 d.f. for the average DTR. We examined the possible nonlinear effect of DTR using a 3 d.f. natural cubic spline. As in the negative binomial generalized linear models, the maximum lag period of DTR was set at 16 weeks. Confounding factors of temperature, humidity, and rainfall using a 3 d.f. natural cubic spline with the maximum lag period of 16 weeks were also included in the model. Distributed lag nonlinear models are illustrated in Figure 3 (the model is described in Protocol S1, online).
Fig. 3.
Plot of relative risk (RR) by diurnal temperature range (DTR) for specific lag periods (left) and RR by lags for specific DTR (right).
As a sensitivity analysis, we also estimated DTR–morbidity relationships using different degrees of seasonal control (3rd and 12th harmonics). All statistical analyses were conducted using Stata v. 11.2 (Stata Corp., USA) and R statistical software (version 3.0.2) [25], using the dlnm package (version 2.0.6) [24].
Ethics approval
The ethics committee of the Fukuoka Prefectural Government Health and Environmental Research Advancement Committee approved this study on 27 December 2006 (reference no. 18-3515). Patients' records and other patients' information were anonymized and de-identified prior to analysis.
RESULTS
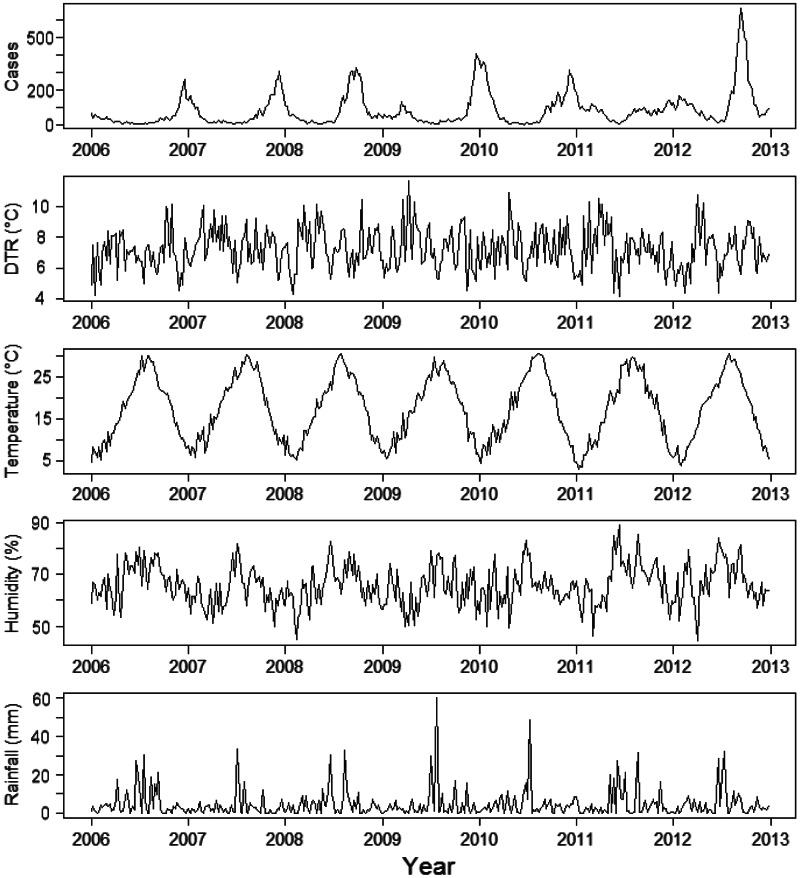
A total of 30 215 RSV cases from 2006 to 2012 were included in our analyses. Of these patients, 29 592(97·9%) were children aged 0–4 years, while the remaining 623 (2·1%) were aged ⩾5 years. Descriptive statistics for the number of patients based on age and weather variables are summarized in Table 1. In the analysis of the weekly reported number of RSV cases, the seasonal peak in cases was found to differ from year to year, although it typically occurred during the autumn or winter season (Fig. 1). The 7-year data were then analysed to identify relationships between the incidence of RSV and DTR.
Table 1.
Characteristics of the weekly number of respiratory syncytial virus (RSV) cases by age and meteorological data in Fukuoka, Japan, between 2006 and 2012
| Characteristics | Data |
|---|---|
| No. of weeks | 364 |
| No. of RSV cases | |
| No. (%) | |
| 0–4 years | 29592 (97·9) |
| >5 years | 623 (2·1) |
| Mean no. of cases per week | |
| Mean (5th to 95th percentile) | |
| 0–4 years | 81·3 (6–282) |
| >5 years | 1·7 (0–7) |
| Weekly mean diurnal temperature range (°C) | |
| Mean (5th to 95th percentile) | 7·2 (5·1–9·6) |
| Weekly mean temperature (°C) | |
| Mean (5th to 95th percentile) | 17·4 (5·9–29·5) |
| Weekly mean humidity (%) | |
| Mean (5th to 95th percentile) | 65·8 (52·8–79·1) |
| Weekly mean rainfall (mm) | |
| Mean (5th to 95th percentile) | 4·7 (0·0–19·2) |
Fig. 1.
Seasonal variation in the weekly number of respiratory syncytial virus cases by diurnal temperature range (DTR), temperature, relative humidity, and rainfall in Fukuoka, Japan, between 2006 and 2012.
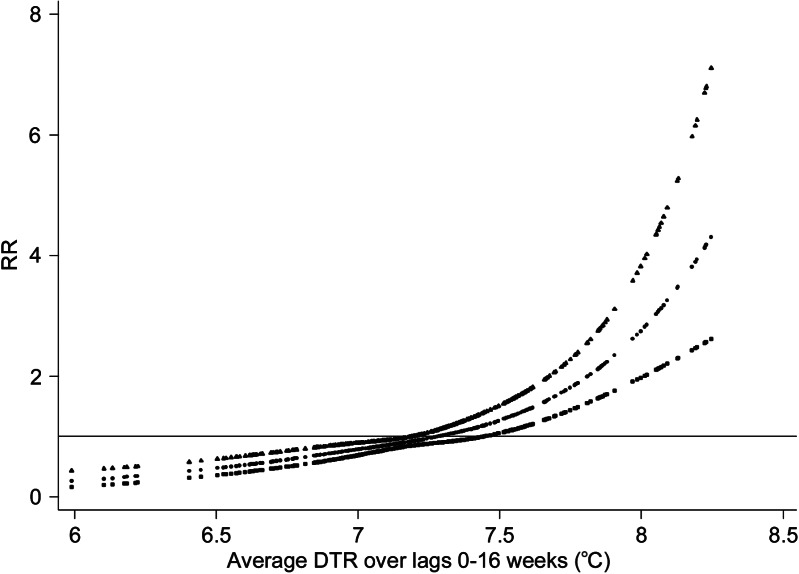
The relationship between the relative risk (RR) of RSV and DTR using negative binomial generalized linear models is shown in Figure 2. Analysis of the crude relationship showed no clear relationship between the risk of RSV and DTR (Supplementary data, Fig. S2). After adjusting for seasonal, inter-year, temperature, humidity and rainfall variations, it was confirmed that a significant increase in the risk of RSV was associated with an increase in DTR. Notably, the time between DTR increase and the occurrence of RSV involved lag periods of 0–16 weeks, as indicated by the positive linear slope with increasing temperature (Fig. 2). Our analysis revealed that an increase of 1°C in DTR resulted in a significant increase in the number of RSV cases, with a RR of 3·30 [95% confidence interval (CI) 1·65–6·60]. We also found evidence for an association with mean temperature and the number of cases of RSV (RR 0·51, 95% CI 0·39–0·68) (Supplementary data, Fig. S3); however, a substantially nonlinear relationship was indicated between the RR of RSV cases and mean temperatures during a lag of 0–16 weeks (Fig. S3).
Fig. 2.
Relationship between relative risk (RR) of respiratory syncytial virus scaled to mean weekly number of cases and diurnal temperature range (DTR) over lags of 0–16 weeks. The relationship was adjusted for temperature, relative humidity, rainfall, seasonal variations, and inter-year variations. The centre line in the graph shows the estimated spline curve, and the upper and lower lines represent the 95% confidence limits.
We also identified the RR of RSV by DTR using distributed lag nonlinear models at specific lag periods (4, 8, 12 weeks) and by lag at specific DTRs (5 °C, 7°C, 10°C), which corresponded to approximately the 5th, 50th, and 95th percentiles of DTR distribution, respectively (Fig. 3). The effects of high DTR were more prominent and persistent over longer lag periods.
To investigate whether the results were sensitive to the levels of control for seasonal patterns, the analyses were repeated using different degrees of seasonal control. Halving (three harmonics) or doubling (12 harmonics) the degree of seasonal control in sensitivity analyses only minimally changed the estimated effects of temperature and humidity. Specifically, the DTR model yielded a RR of 2·99 (95% CI 1·51–5·93) with three harmonics and 3·03 (95% CI 1·53–6·03) with 12 harmonics with respect to the incidence of RSV.
DISCUSSION
Our analysis of the effects of DTR on the incidence of RSV in Fukuoka, Japan, has yielded several notable findings. After adjustment for potential confounding by seasonal, inter-year, temperature, humidity and rainfall variations, we detected that the number of RSV cases increased with increasing DTR. This association appeared to have a major influence on the incidence of RSV infections. These findings indicate that these patterns should be considered when planning for early warnings of epidemics regarding the association between RSV cases and DTR.
Using negative binomial generalized linear models and distributed lag nonlinear models, we found that the number of RSV cases increased with higher DTR and was strongly positive at longer lag period lengths. The findings of the present study highlight the need to consider the weather effect of not only absolute temperature but also changes in DTR, particularly higher DTR. We speculate that this finding might be related to the failure of thermoregulation. The median incubation period of RSV is 4·4 days (95% CI 3·9–4·9) [26], and infected persons are most contagious for 3–8 days following signs of illness [27]; however, some infants, young children, and people with weakened immune systems could be contagious for as long as 4 weeks [27]. In addition, recent research has suggested that it might be possible to be a carrier of the virus for ⩾3 months, because parts of the virus have been found present in some people long after symptoms have disappeared [28]. This fact is of significance as asymptomatic carriers are capable of spreading the causative viruses. These characteristics of RSV infections also highlight the need for more precise modelling of lag effects of weather on disease risk.
The results of this study support the notion that there is a significant relationship between DTR and RSV infections. While the exact mechanism remains unclear, a previous study suggested that sudden changes in weather conditions may affect humoral or cellular immunity [29]. Very young children have a relatively immature immune system [30] and less self-care capacity [31], which might cause them to be more vulnerable to temperature change. Other studies have found that sudden changes in the temperature of inhaled air are associated with the release of inflammatory mediators by mast cells and thus cause more inflammatory nasal responses [32], which might also be related to higher RSV incidence. These findings might explain some of the mechanisms associated with the effect of DTR on RSV infections, and further study is needed to determine how the immune system is affected by DTR.
Although we did not have access to individual data of RSV cases in this study, a previous study suggested that the sharing of toys and other items in childcare centres or kindergartens might contribute to viral infections [33]. Another study found that parents do not dress children appropriately for weather and active play [34], which might be associated with the higher susceptibility of RSV infections. A recent study has also shown that children's opportunities for physical activities in childcare centres might often be curtailed because of inclement weather are often highly influenced by weather, outdoor play policies, and caregiver behaviours related to weather [35]. Further investigation into these factors in the spread of epidemic foci may have implications for the control of RSV infections.
A few limitations of this study should be mentioned. First, surveillance data for RSV do not capture all cases in the community. The under-reporting of infections can occur anywhere in the reporting chain, from the initial tendency of a patient to seek health care to the recording of the case in the disease registry. The degree of under-reporting may also vary between epidemic and non-epidemic periods. Second, the participating sentinel medical institutions were recruited on a voluntary basis; however, this is not expected to significantly influence the validity of the comparisons over time, which is the subject of this study. Third, we did not control for air pollution; however, a previous study on the potential role of air pollutants on the pattern of RSV-related illness in infancy was unable to identify a clear link between a variety of air pollutants and the timing of the RSV epidemic [36].
The present study suggests that DTR might have a potentially significant role in pediatric infectious diseases. Recent studies have suggested that DTR might be an independent risk factor for childhood asthma and diarrhoea [37, 38]. Infectious pathogens such as viruses, parasites and bacteria are devoid of thermostatic mechanisms, and reproduction and survival rates are strongly affected by fluctuations in temperature [39, 40]. Thus, clarification of the effects of weather variability on infectious disease epidemics is important for disease control and prevention by public health officials. In this study, the effects increased with higher DTR, highlighting that parents, medical staff, and public health officials would be made aware of the particularly high risk posed by high DTR and RSV-related morbidity in infants and young children. The results of this study may aid in the prediction of epidemics and in preparation for the effects of DTR on the epidemiology of RSV through implementation of preventive public health interventions, such as frequent hand washing, wiping of hard surfaces with soap and water or disinfectant, and the use of campaigns to encourage such preventative activities. It is expected that such activities might be practically useful for preventing or limiting the spread of RSV infections.
In conclusion, our study provides quantitative evidence that the number of RSV cases in Fukuoka, Japan, increased significantly with increased DTR over the study period. To our knowledge, this is the first report to quantify the impact of DTR on the number of RSV cases using time-series analysis. We therefore suggest that preventive measures for limiting the spread of RSV should be considered during extended periods of high DTR.
ACKNOWLEDGEMENTS
We thank the Fukuoka Prefectural Government, Department of Public Health and Medical Affairs, Division of Public Health for their painstaking efforts in infectious disease surveillance in Fukuoka, Japan. The study was supported in part by a Grant-in-Aid for Scientific Research from the Ministry of Health, Labour and Welfare, Japan. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S0950268814001575.
click here to view supplementary material
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Iwane MK, et al. Population-based surveillance for hospitalizations associated with respiratory syncytial virus, influenza virus, and parainfluenza viruses among young children. Pediatrics 2004; 113: 1758–1764. [DOI] [PubMed] [Google Scholar]
- 2.Hall CB, et al. Occurrence of groups A and B of respiratory syncytial virus over 15 years: associated epidemiologic and clinical characteristics in hospitalized and ambulatory children. Journal of Infectious Diseases 1990; 162: 1283–1290. [DOI] [PubMed] [Google Scholar]
- 3.Mullins JA, et al. Substantial variability in community respiratory syncytial virus season timing. Pediatric Infectious Disease Journal 2003; 22: 857–862. [DOI] [PubMed] [Google Scholar]
- 4.Li H, et al. Epidemiological analysis of respiratory viral etiology for influenza-like illness during 2010 in Zhuhai, China. Virology Journal 2013; 10: 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fodha I, et al. Epidemiological and antigenic analysis of respiratory syncytial virus in hospitalised Tunisian children, from 2000 to 2002. Journal of Medical Virology 2004; 72: 683–687. [DOI] [PubMed] [Google Scholar]
- 6.Khor CS, et al. Epidemiology and seasonality of respiratory viral infections in hospitalized children in Kuala Lumpur, Malaysia: a retrospective study of 27 years. BMC Pediatrics 2012; 12: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yusuf S, et al. The relationship of meteorological conditions to the epidemic activity of respiratory syncytial virus. Epidemiology and Infection 2007; 135: 1077–1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.du Prel JB, et al. Are meteorological parameters associated with acute respiratory tract infections? Clinical Infectious Diseases 2009; 49: 861–868. [DOI] [PubMed] [Google Scholar]
- 9.Vandini S, et al. Respiratory syncytial virus infection in infants and correlation with meteorological factors and air pollutants. Italian Journal of Pediatrics 2013; 39: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Noyola DE, Mandeville PB. Effect of climatological factors on respiratory syncytial virus epidemics. Epidemiology and Infection 2008; 136: 1328–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Turkish Neonatal Society. The seasonal variations of respiratory syncytial virus infections in Turkey: a 2-year epidemiological study. Turkish Journal of Pediatrics 2012; 54: 216–222. [PubMed] [Google Scholar]
- 12.Sung RY, et al. Seasonal patterns of respiratory syncytial virus infection in Hong Kong: a preliminary report. Journal of Infectious Diseases 1987; 156: 527–528. [DOI] [PubMed] [Google Scholar]
- 13.Chan PK, et al. Epidemiology of respiratory syncytial virus infection among paediatric patients in Hong Kong: seasonality and disease impact. Epidemiology and Infection 1999; 123: 257–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chew FT, et al. Seasonal trends of viral respiratory tract infections in the tropics. Epidemiology and Infection 1998; 121: 121–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Omer SB, et al. Climatic, temporal, and geographic characteristics of respiratory syncytial virus disease in a tropical island population. Epidemiology and Infection 2008; 136: 1319–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Onozuka D, Hashizume M, Hagihara A. Effects of weather variability on infectious gastroenteritis. Epidemiology and Infection 2010; 138: 236–243. [DOI] [PubMed] [Google Scholar]
- 17.Ministry of Health, Labour and Welfare. Act on Prevention of Infectious Diseases and Medical Care for Patients Suffering Infectious Diseases (http://www.mhlw.go.jp/bunya/kenkou/kekkaku-kansenshou11/01.html) Accessed 1 November 2013.
- 18.McCullagh P, Nelder J. Generalized Linear Models. London: Chapman and Hall, 1989. [Google Scholar]
- 19.Stolwijk AM, Straatman H, Zielhuis GA. Studying seasonality by using sine and cosine functions in regression analysis. Journal of Epidemiology and Community Health 1999; 53: 235–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brumback B, et al. Transitional regression models, with application to environmental time series. Journal of the American Statistical Association 2000; 95: 16–27. [Google Scholar]
- 21.Durrleman S, Simon R. Flexible regression models with cubic splines. Statistics in Medicine 1989; 8: 551–561. [DOI] [PubMed] [Google Scholar]
- 22.Armstrong B. Models for the relationship between ambient temperature and daily mortality. Epidemiology 2006; 17: 624–631. [DOI] [PubMed] [Google Scholar]
- 23.Daniels MJ, et al. Estimating particulate matter-mortality dose-response curves and threshold levels: an analysis of daily time-series for the 20 largest US cities. American Journal of Epidemiology 2000; 152: 397–406. [DOI] [PubMed] [Google Scholar]
- 24.Gasparrini A, Armstrong B, Kenward MG. Distributed lag non-linear models. Statistics in Medicine 2010; 29: 2224–2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria (http://www.R-project.org/).
- 26.Lessler J, et al. Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infectious Diseases 2009; 9: 291–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.CDC. Respiratory syncytial virus infection (RSV) (http://www.cdc.gov/rsv/). Accessed 1 October 2013.
- 28.Schwarze J, et al. Latency and persistence of respiratory syncytial virus despite T cell immunity. American Journal of Respiratory and Critical Care Medicine 2004; 169: 801–805. [DOI] [PubMed] [Google Scholar]
- 29.Bull GM. The weather and deaths from pneumonia. Lancet 1980; 1: 1405–1408. [DOI] [PubMed] [Google Scholar]
- 30.Gerba CP, Rose JB, Haas CN. Sensitive populations: who is at the greatest risk? International Journal of Food Microbiology 1996; 30: 113–123. [DOI] [PubMed] [Google Scholar]
- 31.Xu Z, et al. Impact of ambient temperature on children's health: a systematic review. Environmental Research 2012; 117: 120–131. [DOI] [PubMed] [Google Scholar]
- 32.Graudenz GS, et al. The role of allergic rhinitis in nasal responses to sudden temperature changes. Journal of Allergy and Clinical Immunology 2006; 118: 1126–1132. [DOI] [PubMed] [Google Scholar]
- 33.Ooi EE, et al. Seroepidemiology of human enterovirus 71, Singapore. Emerging Infectious Diseases 2002; 8: 995–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Copeland KA, et al. Flip flops, dress clothes, and no coat: clothing barriers to children's physical activity in child-care centers identified from a qualitative study. International Journal of Behavioral Nutrition and Physical Activity 2009; 6: 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Copeland KA, et al. Wide variability in physical activity environments and weather-related outdoor play policies in child care centers within a single county of Ohio. Archives of Pediatrics and Adolescent Medicine 2011; 165: 435–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bhatt JM, Everard ML. Do environmental pollutants influence the onset of respiratory syncytial virus epidemics or disease severity? Paediatric Respiratory Reviews 2004; 5: 333–338. [DOI] [PubMed] [Google Scholar]
- 37.Xu Z, et al. Diurnal temperature range and childhood asthma: a time-series study. Environmental Health 2013; 12: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xu Z, et al. Is diurnal temperature range a risk factor for childhood diarrhea? PLoS One 2013; 8: e64713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meerburg BG, Kijlstra A. Changing climate-changing pathogens: Toxoplasma gondii in North-Western Europe. Parasitology Research 2009; 105: 17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Patz JA, et al. Impact of regional climate change on human health. Nature 2005; 438: 310–317. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S0950268814001575.
click here to view supplementary material