Abstract
OBJECTIVE:
Investigate the association between maternal homelessness at the time of delivery and perinatal outcomes, with a focus on neonatal health outcomes.
STUDY DESIGN:
Population-based cohort using California’s statewide database included 1,520,253 women with linked birth and maternal discharge data, 2008–2012. Multivariable analysis assessed homelessness at time of delivery on perinatal outcomes, preterm delivery, and neonatal intensive care unit admission.
RESULT:
A total of 672 women (0.05%) were homeless at the time of delivery. Homelessness was associated with premature delivery at multiple gestational age cutoffs (34w0d–36w6d; 32w0d–33w6d; 28w0d–31w6d; <28w0d) (range of aORs:1.62–2.19), and neonatal intensive care unit admission (aOR = 1.66, 95% CI:1.31–2.09). Among term infants, homelessness remained associated with increased odds of neonatal intensive care unit admission (aOR = 1.84, 95% CI:1.34–2.53), low birthweight (aOR = 1.99, 95% CI:1.36–2.90), neonatal abstinence syndrome (aOR = 2.13, 95% CI:1.35–2.53), hypoxic-ischemic encephalopathy (aOR = 14.38, 95% CI:3.90–53.01), and necrotizing enterocolitis (aOR = 14.94, 95% CI:2.68–83.20).
CONCLUSION:
Homelessness in pregnancy was associated with adverse perinatal outcomes including increased odds of preterm delivery across all gestational ages, and increased risk of neonatal intensive care unit admission and low birth weight independent of preterm delivery.
INTRODUCTION
Social determinants have been well-recognized to contribute to health inequities. People experiencing homelessness are affected by multiple social and structural determinants of health, including social exclusion, unemployment or poor working conditions, and access to safe food [1–5]. As of 2018 in the United States, women account for 28% of the people experiencing homelessness [6]. In obstetrics, social determinants of health have been shown to affect key metrics of maternal and neonatal health, including severe maternal morbidity and mortality, preterm birth, and small for gestational age (SGA) infants [7–10].
Prior studies have examined health disparities in the homeless population [11]. Pregnant women experiencing homelessness tend to have higher prevalence of medical co-morbidities, including mental disorders, chronic health problems, and substance use disorders [12–14]. One recent study from Clark et al. showed increased risks of hypertension in pregnancy and hemorrhage during pregnancy among women experiencing homelessness in Massachusetts [15]. Another recent study from Pantell et al. using approximately the same dataset examined here focused on maternal outcomes, and found that women with unstable housing had higher odds of preterm birth, longer length of stay, and higher frequency of readmission within 12 months post-partum [14].
Although, several studies have attempted to evaluate outcomes in neonates born to women experiencing homelessness including prematurity and birthweight, these studies were challenged by small sample size, and did not have consistency with the definition of homeless [15–20]. A population level study investigating women experiencing homelessness in pregnancy and prematurity across different gestational ages (<28 and 32 weeks) or a broader spectrum of neonatal complications including mortality has not been conducted. California accounts for one in every 8 births in the United States and has the largest share (31%) of people experiencing homelessness in the country [6, 21].
The objective of our study was to investigate the potential association between homelessness in pregnancy and perinatal outcomes, particularly neonatal birthweight, prematurity, mortality and selected neonatal health conditions in the homeless population in California.
MATERIAL/SUBJECTS AND METHODS
Study population and data source
We performed a retrospective cohort study using linked birth certificate and hospital discharge diagnosis data from California’s Office of Statewide Health Planning and Development (OSHPD) for the years 2008–2012. This dataset is the most current, linked OSHPD dataset available and includes information on a range of maternal, pregnancy, and infant characteristics from birth certificates combined with clinical details from prenatal and delivery hospitalization [22]. Over this time period, nearly all maternal and infant hospitalization (98%) are captured in this database. The Stanford University Institutional Review Board and California State Committee for the Protection of Human Subjects reviewed and approved this study before its initiation.
Women experiencing homelessness were defined using the ICD-9 code “lack of housing” (v60.0) at the time of delivery hospitalization. Those without this code served as the housed, referent population. Figure 1 depicts the inclusion criteria of the study population. The study excluded women with unlinked delivery records, subsequent deliveries of women with multiple births, and women with deliveries at hospitals without at least one identified pregnancy of a woman experiencing homelessness in order to account for differences in coding practices across hospitals. In addition, we excluded missing and implausible covariates included in analytical models, including gestational duration <20 weeks or >42 weeks. After excluding patients from hospitals that did not meet these criteria, the total number of women in the analytic cohort was 1,466,398 (Fig. 1).
Fig. 1. Inclusion criteria for study population.
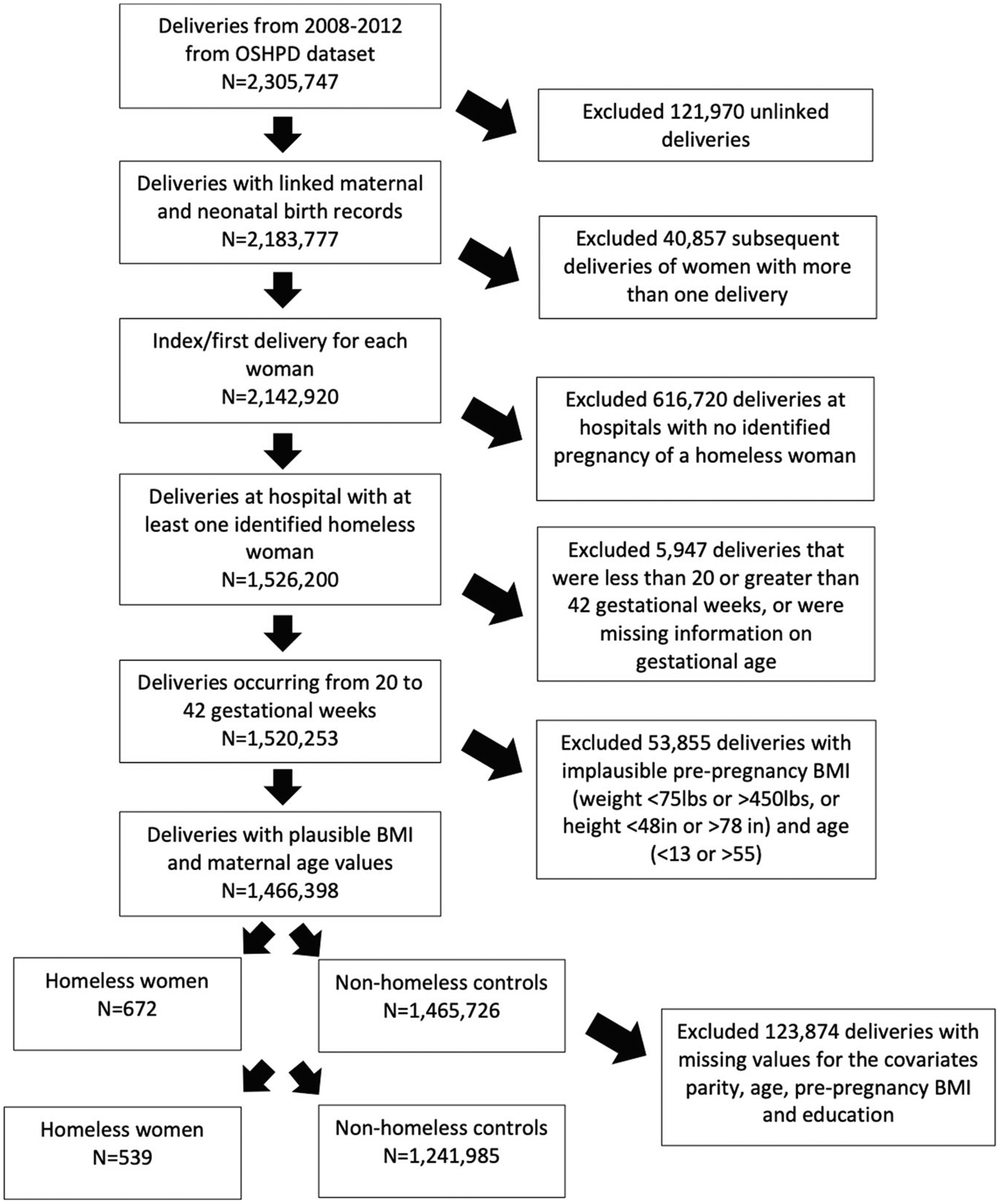
Flow diagram depicting the inclusion/exclusion criteria of the study population.
Variables
Maternal demographic and clinical characteristics, including education, health insurance status, age, race/ethnicity, parity, data on timing of initiation of prenatal care, and prior cesarean section, were derived from the birth certificate. Information on cigarette use and substance use during pregnancy was derived from OSHPD and birth certificate data. Maternal comorbidities including mental illness, pre-existing hypertension, pre-existing diabetes, and asthma were identified using a ICD-9 codes and/or birth certificate data.
Data from both birth certificate information and ICD-9 code(s) during the delivery admission were used to determine maternal pregnancy outcomes. These outcomes include gestational diabetes, preeclampsia, placental abruption, chorioamnionitis, preterm premature rupture of membranes (PPROM), mode of delivery, and postpartum hemorrhage. Severe maternal morbidity (SMM) was also evaluated, defined using the 21 diagnosis and procedure ICD-9 codes recommended by the Centers of Disease Control and Prevention [23].
Neonatal outcomes were obtained using the information on the birth certificate which included: low birthweight (LBW; <2500 g), and gestational age at birth; and also ICD-9 codes in the hospital discharge summary: hypoxic ischemic encephalopathy, intraventricular hemorrhage, neonatal enterocolitis, respiratory distress syndrome, neonatal seizure, and neonatal abstinence syndrome. In-hospital neonatal death (within one month of birth) and infant death (within nine months of birth) were based on the death certificates and neonatal intensive care unit (NICU) admission for >24 h was based on data recorded on birth certificate. Data on infant death were only available for years 2008–2011. In addition, we evaluated preterm delivery defined as <28 (extremely preterm), 28 weeks to 31 weeks 6 days (very preterm), 32 weeks to 33 weeks 6 days, and 34 weeks to 36 weeks 6 days, respectively, based upon birth certificate data. In adherence with our IRB protocol, frequencies of rare events with <15 individuals were denoted as such.
Statistical analysis
For all analyses conducted, we used a two-sided alpha of 0.05 to evaluate significance. We compared sociodemographic, clinical, and obstetric characteristics, as well as maternal and neonatal pregnancy outcomes by homelessness status using Chi-squared or Fisher’s exact tests. Associations between homelessness and outcome (maternal and neonatal) measures were estimated with odds ratios computed using Firth’s penalized likelihood approach to logistic regression to address the issue of small-sample bias for all comparisons [24]. Variables considered for adjustment in multivariable models were based on univariate analyses and prior literature and included: parity, age, smoking, substance use disorder, race/ethnicity, pre-pregnancy BMI, and education. Only individuals with complete data were included in regression analyses (Fig. 1). Analyses stratified on term and preterm delivery were conducted to examine whether association between homelessness and neonatal morbidity was solely attributed to preterm delivery. Adjusted p values were calculated using the Benjamini-Hochberg test to assess for potential multiple comparison bias in the calculated odds ratios, with a false discovery rate q < 0.05. Data were analyzed using SAS version 9.4 (SAS institute, Cary, NC, USA).
RESULTS
Among 1,466,398 women included in descriptive analysis, 672 women (0.05%) met the definition of experiencing homelessness at the time of delivery hospitalization (Fig. 1). Compared to women who were not homeless, women experiencing homelessness had differences in age, education, race/ethnicity, insurance status, parity, and in the initiation of prenatal care in the second trimester or later (Table 1). In addition, women experiencing homelessness had higher frequencies of smoking, substance use disorders, and were more likely to have hypertension, diabetes, mental illness, and asthma (Table 1). Table 2 shows women experiencing homelessness suffered several obstetrical comorbidities at higher frequency in the index pregnancy, including greater than two times the incidence of PPROM (4.8% vs 1.9%; p < 0.001), placental abruption (3.0% vs 1.1%; p < 0.001), and severe maternal morbidity (3.9% vs. 1.6%; p < 0.001) at delivery.
Table 1.
Baseline maternal sociodemographic, clinical, and obstetric characteristics of women who were and were not homeless and giving birth in California hospitals between 2008 and 2012.
| Characteristics | Homeless (n = 672) N (%) | Non- homeless (n = 1,465,726)N (%) | P value |
|---|---|---|---|
| Maternal age, years | |||
| <25 | 226 (32.6) | 441,442 (30.2) | 0.012 |
| 25–34 | 308 (45.8) | 755,934 (51.6) | |
| ≥35 | 138 (20.3) | 277,178 (18.2) | |
| Missing | 0 | 20 | |
| Race/ethnicity | |||
| White, non- Hispanic | 324 (48.2) | 434,192 (29.6) | <0.001 |
| Hispanic | 143 (21.2) | 707,346 (48.3) | |
| Black, non- Hispanic | 140 (20.8) | 89,434 (6.1) | |
| Asian/Pacific Islander, non- Hispanic | 25 (3.7) | 163,480 (11.2) | |
| Other | 17 (2.5) | 48,737 (3.3) | |
| Unknown | 23 (3.4) | 22,537 (1.5) | |
| Education | |||
| No high school degree | 212 (35.1) | 356,207 (25.3) | <0.001 |
| High school degree | 222 (37.7) | 361,535 (25.6) | |
| Some college | 160 (26.5) | 335,850 (23.8) | |
| College | <15 | 365,800 (25.0) | |
| Missing | 68 | 54,873 | |
| Health insurance | |||
| Private insurance | 56 (8.3) | 666,083 (45.4) | <0.001 |
| Public insurance | 601 (89.4) | 797,306 (54.4) | |
| Unknown/missing | 15 (2.2) | 2337 (0.2) | |
| Pre-pregnancy BMI | |||
| <18.5 | 35 (5.7) | 57,408 (4.1) | 0.007 |
| 18.5–24.99 | 272 (44.2) | 705,140 (49.8) | |
| ≥25 | 309 (50.2) | 653,807 (43.2) | |
| Missing | 56 | 49,371 | |
| Parity | |||
| 1 | 220 (32.9) | 679,781 (46.4) | <0.001 |
| 2–3 | 286 (42.8) | 630,726 (43.0) | |
| 4 or more | 162 (24.3) | 154,913 (10.6) | |
| Missing | 4 | 306 | |
| Initiation of prenatal care | |||
| No prenatal care | 100 (15.9) | 5369 (0.4) | <0.001 |
| 1st trimester | 290 (46.2) | 1,250,812 (83.6) | |
| 2nd trimester | 167 (26.6) | 199,769 (13.4) | |
| 3rd trimester | 71 (11.3) | 38,081 (2.6) | |
| Missing | 44 | 23,699 | |
| Prior cesarean birth | 151 (22.5) | 224,023 (15.3) | <0.001 |
| Smoked cigarettes during pregnancy | 304 (45.4) | 54,843 (3.7) | <0.001 |
| Substance use disorder during pregnancy | 358 (53.3) | 35,703 (2.4) | <0.001 |
| Alcohol | 64 (9.5) | 5102 (0.4) | <0.001 |
| Opioid | 44 (6.6) | 3646 (0.3) | <0.001 |
| Amphetamine | 166 (24.7) | 8041 (0.6) | <0.001 |
| Cocaine | 63 (9.4) | 1907 (0.1) | <0.001 |
| Comorbidities | |||
| Asthma | 103 (15.3) | 56,675 (3.9) | <0.001 |
| Pre-existing hypertension | 56 (8.3) | 38,749 (2.6) | <0.001 |
| Pre-existing diabetes | 21 (3.1) | 19,800 (1.4) | <0.001 |
| Mental condition during pregnancy | 437 (65.0) | 76,522 (5.2) | <0.001 |
Table 2.
Maternal pregnancy and neonatal birth outcomes of homeless and non-homeless women in California between 2008 and 2012.
| Characteristics | Homeless (n = 672) N (%) | Non- homeless (n = 1,465,726) N (%) | P value |
|---|---|---|---|
| Maternal outcomes | |||
| Pregnancy complications | |||
| Gestational diabetes | 77 (11.5) | 143,039 (9.8) | 0.139 |
| Preterm premature rupture of the membranes (PPROM) | 32 (4.8) | 28,043 (1.9) | <0.001 |
| Preeclampsia and eclampsia | 55 (8.2) | 74,545 (5.1) | <0.001 |
| Chorioamnionitis | 22 (3.3) | 51,535 (3.5) | 0.733 |
| Placental abruption | 21 (3.1) | 15,825 (1.1) | <0.001 |
| Severe maternal morbidity (SMM) | 26 (3.9) | 23,361 (1.6) | <0.001 |
| Postpartum hemorrhage (PPH) | 22 (3.3) | 43,722 (3.0) | 0.658 |
| Mode of delivery | |||
| Vaginal | 437 (65.0) | 993,413 (67.8) | 0.072 |
| CS- Primary | 93 (13.8) | 218,788 (14.9) | |
| CS - Repeat or failed trial of labor | 142 (21.1) | 253,524 (17.3) | |
| Neonatal outcomes | |||
| Birthweight | |||
| Low (<2500 g) | 107 (16.0) | 93,041 (6.4) | <0.001 |
| Missing | <15 | 702 | |
| Gestational age at birth (weeks) | |||
| Gestational age < 28wk | <15 | 7436 (0.5) | <0.001 |
| Gestational age 28w–31w6d | 16 (2.4) | 11,010 (0.8) | <0.001 |
| Gestational age 32w–33w6d | 21 (3.1) | 14,133 (1.0) | <0.001 |
| Gestational age 34w–36w6d | 91 (13.5) | 87,093 (5.9) | <0.001 |
| Gestational age ≥ 37w | 534 (79.5) | 1,346,054 (91.8) | <0.001 |
| Hypoxic-ischemic encephalopathy (HIE) | <15 | 561 (0.0) | 0.028 |
| Intraventricular hemorrhage (IVH) | <15 | 5150 (0.4) | <0.001 |
| Necrotizing enterocolitis (NEC) | <15 | 1789 (0.1) | 0.050 |
| Respiratory distress syndrome (RDS) | 30 (4.5) | 24,476 (1.7) | <0.001 |
| Neonatal abstinence syndrome (NAS) | 29 (4.3) | 4171 (0.3) | <0.001 |
| Neonatal seizure | <15 | 5253 (0.4) | 0.003 |
| NICU admission > 24 h | 119 (17.7) | 94,160 (6.4) | <0.001 |
| In-hospital death | |||
| Neonatal (birth to 1 month)* | <15 | 3611 (0.3) | 0.004 |
| Infant (birth to 9 months)* | <15 | 5322 (0.4) | <0.001 |
| Missing | 162 | 241,958 | |
Data are only available for 2008–2011.
Table 2 shows that 16.0% of neonates born to women experiencing homelessness were low birthweight compared to 6.4% among controls (p < 0.001). In addition, intraventricular hemorrhage, respiratory distress syndrome, and neonatal abstinence syndrome were all rare outcomes, but occurred at higher frequency among neonates born to women experiencing homelessness.
Table 3 depicts crude and multivariable analyses investigating associations between experiencing homelessness in pregnancy with select maternal as well as neonatal outcomes. After adjustment, higher odds of PPROM (aOR = 1.70, 95% CI:1.15–2.52) and placental abruption (aOR = 1.69, 95% CI:1.03–2.76) were observed among women experiencing homelessness. After adjustment, the odds ratio of NICU admission >24 h (aOR = 1.69, 95% CI:1.35–2.12) remained increased in women experiencing homelessness. When assessing risk of preterm delivery among multiple gestational age cutoffs compared to term deliveries (>37 weeks), preterm deliveries remained increased in women experiencing homelessness across all ages <28 weeks (aOR = 2.19, 95% CI:1.14–4.18), 28 weeks to 31 weeks 6 days (aOR = 1.91, 95% CI:1.08–3.37), 32 weeks to 33 weeks 6 days (aOR = 1.88, 95% CI:1.11–3.18), and 34 weeks to 36 weeks 6 days (aOR = 1.62, 95% CI:1.25–2.09). There were a few outcomes showing significant increased odds associated with homelessness in crude analyses, but were no longer statistically significant after adjustment. These included an increased odds of neonatal outcomes such as neonatal death (OR = 3.19, 95% CI:1.11–7.81), and infant death (OR = 3.36, 95% CI:1.45–7.81), as well as maternal baseline comorbidities and outcomes such as preexisting hypertension (OR = 3.03, 95% CI: 2.20–4.17), pre-existing diabetes (OR = 2.18, 95% CI:1.32–3.62), and maternal outcome of preeclampsia and eclampsia (OR = 1.62, 95% CI:1.19–2.22).
Table 3.
Unadjusted and adjusted odds ratios for maternal baseline characteristics and perinatal outcomes in homeless compared to non-homeless women at time of delivery.
| Characteristics | Unadjusted OR OR (95% CI) |
Adjusted OR▼ OR (95% CI) |
|---|---|---|
| Maternal baseline | ||
| Asthma | 4.37 (3.45–5.54)** | 1.34 (1.05–1.72) |
| Pre-existing hypertension | 3.03 (2.20–4.17)** | 1.27 (0.91–1.77) |
| Mental disorders | 31.07 (26.09–37.01)** | 7.28 (5.44–9.75)** |
| Pre-existing diabetes | 2.18 (1.32–3.62)** | 1.18 (0.70–1.96) |
| Maternal outcomes | ||
| Severe maternal morbidity | 2.60 (1.69–4.00)** | 1.25 (0.81–1.93) |
| PPH | 1.12 (0.70–1.80) | 1.07 (0.67–1.73) |
| Gestational diabetes | 1.16 (0.89–1.52) | 1.13 (0.86–1.49) |
| Preeclampsia and eclampsia | 1.62 (1.19–2.22)** | 1.35 (0.99–1.86) |
| PPROM | 2.70 (1.82–3.99)** | 1.70 (1.15–2.52)** |
| Chorioamnionitis | 0.88 (0.54–1.44) | 1.09 (0.67–1.78) |
| Placental abruption | 2.95 (1.80–4.81)** | 1.69 (1.03–2.76) |
| Neonatal outcomes | ||
| NICU admission for >24h | 2.89 (2.30–3.63)** | 1.66 (1.31–2.09)** |
| Neonatal in-hospital death (birth to 1 month)* | 3.19 (1.11–9.14)** | 1.85 (0.64–5.32) |
| Infant in-hospital death (birth to 9 months)* | 3.36 (1.45–7.81)** | 1.75 (0.75–4.08) |
| Prematurity | ||
| Gestational age<28w | 4.06 (2.13–7.72)** | 2.19 (1.14–4.18) |
| Gestational age 28w–31w6d | 3.81 (2.22–6.55)** | 1.91 (1.08–3.37) |
| Gestational age 32w–33w6d | 3.15 (1.87–5.32)** | 1.88 (1.11–3.18) |
| Gestational age 34w–36w6d | 2.53 (1.97–3.24)** | 1.62 (1.25–2.09)** |
| Gestational age ≥ 37w | Reference | Reference |
Adjusted for parity (1, 2–3, 4 or more), age (continuous), cigarette use (Y/N), substance use disorder (Y/N), race-ethinicity (Asian/PI, Black, Hispanic, White, other, unknown), pre-pregnancy BMI (continuous), and education.
Data are only available for 2008–2011.
q < 0.05 after false discovery rate calculation using the Benjamini-Hochberg procedure.
Given that many neonatal outcomes are associated with being preterm, we explored whether higher odds of adverse neonatal outcomes among women experiencing homelessness could be accounted for solely by being born preterm. Table 4 shows the odds of neonatal outcomes among women experiencing homelessness stratified by preterm delivery. Within term infants born to women experiencing homelessness, there were increased odds of low birthweight, hypoxic-ischemic encephalopathy, neonatal abstinence syndrome, necrotizing enterocolitis, and NICU admission in both crude and adjusted analyses. Of note, term infants born to women experiencing homelessness had a 1.84 (95% CI:1.34–2.53) times greater adjusted odds of requiring NICU admission >24 h compared to their counterparts.
Table 4.
Unadjusted and adjusted logistic regression analysis of neonatal outcomes in homeless compared to non-homeless women stratified by premature birth (<37 weeks)*.
| Outcomes | Unadjusted | Adjusted | ||
| Preterm infantsOR (95% CI) | Term infantsOR (95% CI) | Preterm infantsOR (95% CI) | Term infantsOR (95% CI) | |
| Low birthweight (<2500 g) | 1.11 (0.75, 1.64) | 3.40 (2.34, 4.94)** | 0.89 (0.61, 1.31) | 1.99 (1.36, 2.90)** |
| Hypoxic-ischemic encephalopathy (HIE) | 5.80 (0.35, 95.12) | 17.70 (5.08, 61.65)** | 4.65 (0.27, 81.55) | 14.38 (3.90, 53.01)** |
| Intraventricular hemorrhage (IVH) | 2.05 (0.97, 4.33) | 2.53 (0.16, 40.71) | 1.86 (0.89, 3.89) | 1.28 (0.08, 21.88) |
| Necrotizing enterocolitis (NEC) | 1.16 (0.23, 5.84) | 18.94 (3.79, 94.77)** | 1.00 (0.20, 4.89) | 14.94 (2.68, 83.2)** |
| Respiratory distress syndrome (RDS) | 1.29 (0.79, 2.09) | 3.60 (1.55, 8.33)** | 1.14 (0.71, 1.83) | 2.29 (0.98, 5.34) |
| Neonatal abstinence syndrome (NAS) | 8.12 (3.13, 21.05)** | 19.34 (12.39, 30.18)** | 0.83 (0.32, 2.14) | 2.13 (1.35, 3.38)** |
| Neonatal seizure | 4.13 (1.41, 12.06)** | 2.57 (0.90, 7.36) | 3.39 (1.17, 9.86) | 1.66 (0.58, 4.77) |
| NICU admission | 1.21 (0.82, 1.79) | 3.03 (2.21, 4.16)** | 0.96 (0.65, 1.4) | 1.84 (1.34, 2.53)** |
| Neonatal death (birth to 1 month) | 1.85 (0.63, 5.46) | 2.23 (0.14, 35.77) | 1.56 (0.55, 4.45) | 1.66 (0.10, 27.3) |
| Infant death (birth to 9 months) | 1.60 (0.54, 4.69) | 4.66 (1.34, 16.22)** | 1.21 (0.43, 3.44) | 2.41 (0.69, 8.46) |
Adjusted for parity (1, 2–3, 4 or more), age (continuous), smoking (Y/N), substance use disorder (Y/N), race (white, black, Asian/PI, Hispanic, other, unknown), pre-pregnancy BMI (continuous), and education.
q < 0.05 after false discovery rate calculation using the Benjamini-Hochberg procedure.
Given the number of women excluded owing to no identified pregnancies of homeless women at the delivery hospital (Fig. 1), we compared that excluded population to the housed population used throughout this analysis. The excluded population had similar demographics, maternal and neonatal outcomes to the housed population (analysis not shown).
DISCUSSION
This study observed that women experiencing homelessness at the time of delivery were at elevated risk of delivering prematurely, as well as delivering infants who required a NICU stay and had other adverse perinatal outcomes. Higher odds of adverse perinatal outcomes and NICU admission were observed among both term and preterm births.
Previous studies have evaluated the potential association between homelessness or housing stability and prematurity, although findings have been mixed. In 2019, Clark et al. noted that mothers with housing instability in Massachusetts had a 1.9 times greater risk of early or threatened delivery. In addition, studies in Canada and England showed significant increases in preterm delivery in homeless women. However, a cross-sectional study across multiple US cities by Cutts et al. in 2014 did not observe a significant difference in prematurity in those experiencing homelessness. A recent study that used a propensity scoring matching to assess “unstable housing” during pregnancy and/or the following year, noted significant increases in prematurity >32 weeks, but not at <32 weeks [15, 17, 18]. Our data allowed us to investigate prematurity across multiple gestational ages. We demonstrated significant differences across all gestational ages, including a 2.19 times greater odds of delivery before 28 weeks of gestation after adjusting for potential confounding variables. Possible differences in risk by gestational age, i.e., increased risk in very preterm (28 weeks to 31 weeks 6 days) and extremely preterm (<28 weeks) delivery, are important to investigate given that such deliveries increase neonatal risks for infant death and various long-term sequalae [25, 26].
There has been a paucity of research assessing perinatal outcomes and NICU admission for women experiencing homelessness. A study by Richards et al. in 2011 showed that non-homeless women were 0.8 times likely to have an infant in the NICU compared to homeless women. However, prematurity was not assessed in this study, and thus it is unclear whether their observed risk was dependent on prematurity [14, 16]. Our study found that infants of women experiencing homelessness had higher odds of other poor neonatal outcomes, even after stratifying by being born preterm. In term infants born to women experiencing homelessness, we observed an increased odds of NICU admission. In addition, these term infants also had increased odds of hypoxic-ischemic encephalopathy, neonatal abstinence syndrome, necrotizing enterocolitis, and low birthweight (<2500 g). Prior studies have not examined the previously discussed infant health issues that result from women experiencing homelessness during pregnancy. These findings indicate that the association of neonatal morbidity with maternal homelessness is not only dependent on premature delivery.
Women experiencing homelessness at birth showed significant increases in high-risk behaviors, baseline comorbidities, and peripartum complications. These results align with others who have shown similar results, including in the Pantell et al. study that was conducted on pregnant women with unstable housing in California [14] and among other studies within the United States [15, 27–30]. Delayed entry into prenatal care, as seen in this population of women experiencing homelessness, may exacerbate the risk of adverse pregnancy outcomes.
A strength of our study is the use of the OSHPD dataset, which allowed for a large sample size. This was a population-based study that included almost complete coverage of all maternal-neonatal hospitalizations in California. We were able to comprehensively examine the association between maternal housing status and the birth and neonatal outcomes, many of which have not been previously described, Given the transient nature of homelessness and challenges for people experiencing homelessness to establish and maintain care [31–33], this population-based database allowed us to include in analyses those women who may have otherwise been lost to follow-up or changed providers multiple times.
The main limitation of this study is that we relied on medical billing codes to determine housing status at the time of delivery, as well as other variables. Such a reliance on codes may underestimate the proportion of women who experienced homelessness and may have attenuated estimated odds toward the null. Certain outcomes were very rare, such as necrotizing enterocolitis and hypoxic-ischemic encephalopathy, limiting the ability to assess differences. In addition, since we only looked at housing status at birth, we cannot evaluate the effects of unstable housing or homelessness at various points during pregnancy.
In conclusion, results of our study show that pregnant women experiencing homelessness at the time of delivery are at increased risk for their infants having neonatal complications beyond what would be expected from prematurity alone. Creative and ambitious interventions are needed to address the overarching factors that contribute to homelessness in pregnancy in order examine the effects on adverse neonatal outcomes. Access to safe and long-term housing of expectant mothers may alleviate some of this associated neonatal morbidity and risk of preterm delivery.
Footnotes
Supplementary information The online version contains supplementary material available at https://doi.org/10.1038/s41372-021-01187-3.
COMPETING INTERESTS
The authors declare no competing interests.
REFERENCES
- 1.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep 2014;129:19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marmot M Social determinants of health inequalities. Lancet. 2005;365:1099–104. [DOI] [PubMed] [Google Scholar]
- 3.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–98. [DOI] [PubMed] [Google Scholar]
- 4.Wilkinson RG, Marmot M. Social determinants of health: the solid facts: World Health Organization; 2003. [Google Scholar]
- 5.Bassuk EL, Weinreb LF, Buckner JC, Browne A, Salomon A, Bassuk SS. The characteristics and needs of sheltered homeless and low-income housed mothers. JAMA. 1996;276:640–6. [PubMed] [Google Scholar]
- 6.Henry M, Mahathey A, Morrill T, Robinson A, Shivji A, Watt R, et al. The 2018 Annual Homeless Assessment Report (AHAR) to Congress: Part 1: Point-in-time estimates of homelessness. Washington D.C.: Department of Housing and Urban Development, Office of Community Planning and Development; 2018. p. 100. [Google Scholar]
- 7.Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Race, ethnicity, and nativity differentials in pregnancy-related mortality in the United States: 1993–2006. Obstet Gynecol 2012;120:261–8. [DOI] [PubMed] [Google Scholar]
- 8.Luo Z-C, Wilkins R, Kramer MS. Effect of neighbourhood income and maternal education on birth outcomes: a population-based study. Cmaj 2006;174:1415–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim D, Saada A. The social determinants of infant mortality and birth outcomes in Western developed nations: a cross-country systematic review. Int J Environ Res Public Health. 2013;10:2296–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nkansah-Amankra S, Dhawain A, Hussey JR, Luchok KJ. Maternal social support and neighborhood income inequality as predictors of low birth weight and preterm birth outcome disparities: analysis of South Carolina Pregnancy Risk Assessment and Monitoring System survey, 2000–2003. Matern Child Health J 2010;14:774–85. [DOI] [PubMed] [Google Scholar]
- 11.Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384:1529–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wagner JD, Menke EM. Substance use by homeless pregnant mothers. J Health Care Poor Underserved. 1992;3:161–72. [DOI] [PubMed] [Google Scholar]
- 13.Weinreb L, Goldberg R, Perloff J. Health characteristics and medical service use patterns of sheltered homeless and low-income housed mothers. J Gen Intern Med 1998;13:389–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pantell MS, Baer RJ, Torres JM, Felder JN, Gomez AM, Chambers BD, et al. Associations between unstable housing, obstetric outcomes, and perinatal health care utilization. Am J Obstet Gynecol MFM. 2019;1:100053. 10.1016/j.ajobmf.2019.100053. [DOI] [PubMed] [Google Scholar]
- 15.Clark RE, Weinreb L, Flahive JM, Seifert RW. Homelessness contributes to pregnancy complications. Health Aff (Millwood). 2019;38:139–46. [DOI] [PubMed] [Google Scholar]
- 16.Richards R, Merrill RM, Baksh L. Health behaviors and infant health outcomes in homeless pregnant women in the United States. Pediatrics. 2011;128:438–46. [DOI] [PubMed] [Google Scholar]
- 17.Cutts DB, Coleman S, Black MM, Chilton MM, Cook JT, de Cuba SE, et al. Homelessness during pregnancy: a unique, time-dependent risk factor of birth outcomes. Matern Child Health J 2015;19:1276–83. [DOI] [PubMed] [Google Scholar]
- 18.Little M, Shah R, Vermeulen MJ, Gorman A, Dzendoletas D, Ray JG. Adverse perinatal outcomes associated with homelessness and substance use in pregnancy. CMAJ. 2005;173:615–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paterson CM, Roderick P. Obstetric outcome in homeless women. BMJ. 1990;301:263–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stein JA, Lu MC, Gelberg L. Severity of homelessness and adverse birth outcomes. Health Psychol. 2000;19:524–34. [PubMed] [Google Scholar]
- 21.Martin JA, Hamilton BE, Osterman MJK. Births in the United States, 2017. NCHS Data Brief 2018;318:1–8. [PubMed] [Google Scholar]
- 22.Herrchen B, Gould JB, Nesbitt TS. Vital statistics linked birth/infant death and hospital discharge record linkage for epidemiological studies. Comput Biomed Res 1997;30:290–305. [DOI] [PubMed] [Google Scholar]
- 23.Severe Maternal Morbidity Indicators and Corresponding ICD Codes during Delivery Hospitalizations.Center for Disease Control; 2018. [updatedDecember 13, 2018. Available from: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/smm/severe-morbidity-ICD.htm. [Google Scholar]
- 24.Firth S Bias reduction of maximum likelihood estimates. Biometrika. 1993;80:27–38. [Google Scholar]
- 25.Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller A-B, et al. Born too soon: the global epidemiology of 15 million preterm births. Reprod health. 2013; 10:S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clark RE, Weinreb L, Flahive JM, Seifert RW. Infants exposed to homelessness: health, health care use, and health spending from birth to age six. Health Aff (Millwood). 2019;38:721–8. [DOI] [PubMed] [Google Scholar]
- 27.Crawford DM, Trotter EC, Hartshorn KJ, Whitbeck LB. Pregnancy and mental health of young homeless women. Am J Orthopsychiatry. 2011;81:173–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bassuk EL, Buckner JC, Perloff JN, Bassuk SS. Prevalence of mental health and substance use disorders among homeless and low-income housed mothers. Am J Psychiatry. 1998;155:1561–4. [DOI] [PubMed] [Google Scholar]
- 29.Robertson MJ, Winkleby MA. Mental health problems of homeless women and differences across subgroups. Annu Rev Public Health. 1996;17:311–36. [DOI] [PubMed] [Google Scholar]
- 30.Zlotnick C, Zerger S. Survey findings on characteristics and health status of clients treated by the federally funded (US) Health Care for the Homeless Programs. Health Soc Care Community. 2009;17:18–26. [DOI] [PubMed] [Google Scholar]
- 31.Riley AJ, Harding G, Underwood MR, Carter YH. Homelessness: a problem for primary care? Br J Gen Pract 2003;53:473–9. [PMC free article] [PubMed] [Google Scholar]
- 32.Skosireva A, O’Campo P, Zerger S, Chambers C, Gapka S, Stergiopoulos V. Different faces of discrimination: perceived discrimination among homeless adults with mental illness in healthcare settings. BMC Health Serv Res 2014;14:376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bloom KC, Bednarzyk MS, Devitt DL, Renault RA, Teaman V, Van Loock DM. Barriers to prenatal care for homeless pregnant women. J Obstet, Gynecologic, Neonatal Nurs 2004;33:428–35. [DOI] [PubMed] [Google Scholar]


