Abstract
Background and Objectives:
Congenital syphilis (CS) is increasing in the United States and is associated with intersecting social and structural determinants of health. This study aimed to delineate birthing parent characteristics associated with CS in an adjusted model.
Methods (n = 720):
People diagnosed with syphilis during pregnancy from 2017 to 2018 who were interviewed and linked to infants in the California state surveillance system were included (herein, “birthing parents”). Sociodemographic and clinical CS risk factors informed a stepwise multivariable logistic regression model in which the outcome of interest was infants born with CS. CS prevention continuums delineated the proportion of pregnant people with syphilis who completed steps (e.g., prenatal care entry, syphilis testing, treatment) needed to prevent CS; the outcome was delivering an infant without CS. We stratified continuums by homelessness and methamphetamine use to explore differences in CS outcomes.
Results:
Of 720 birthing parents, 245 (34%) delivered an infant with CS. Although CS was initially associated with homelessness (odds ratio [OR] = 2.5, 95% confidence interval [CI]: 1.6, 4.0) and methamphetamine use (OR = 2.1, 95% CI: 1.4, 3.1), the addition of prenatal care into a final adjusted model attenuated these associations to not significant. In CS prevention continuums, delivering an infant without CS was less likely for people who reported methamphetamine use (p < .001) and/or homelessness (p < .001). However, when examining only those who received prenatal care, statistical differences for these predictors no longer existed. In the final adjusted model the following were associated with CS: no prenatal care (OR = 16.7, 95% CI: 9.2, 30.3) or late prenatal care (OR = 2.9, 95% CI: 1.9, 4.2); early stage of syphilis (OR = 2.6, 95% CI: 1.8, 3.7); living in Central California (OR = 2.1, 95% CI: 1.1, 4.2).
Conclusions and Scientific Significance:
This is the first analysis to explore birthing parent characteristics associated with delivering an infant with CS in an adjusted model. We demonstrate that prenatal care, when accessed, can result in effective CS prevention among people who are unhoused and/or using methamphetamine equally well compared to counterparts without these risk factors.
INTRODUCTION
Congenital syphilis (CS)—vertical transmission of syphilis to a fetus in utero—is increasing in the United States, driven by escalating rates in the West and South.1,2 Untreated, CS sequelae include stillbirth, preterm birth, and physical and neurologic deficits. Once approaching elimination, the number of CS cases rose 460% nationally—from 334 to 1870 cases—between 2012 and 20192; preliminary 2020 case counts are reported to be 2022.3 Over the same time period, CS cases in California rose 1251%, from 33 to 446 cases.4
Early detection and treatment of syphilis before and during pregnancy are the mainstays of CS prevention, with treatment efficacy approaching 100% when administered according to the stage of disease and initiated 30 days or more before delivery.5 Vertical transmission is associated with early stage of disease in pregnancy, high titers, and delayed prenatal treatment.5–9
In 2020, the Centers for Disease Control and Prevention (CDC) described regional differences around the United States in CS characteristics using 2018 data of CS cases inclusive of live and stillborn infants. Lack of timely prenatal care was the most common missed opportunity in the West, lack of adequate treatment in the South, late identification of seroconversion during pregnancy in the Northeast, and a combination of factors in the Midwest. Acknowledging these uniquely local aspects of CS trends, the CDC recommended state-specific inquiry to understand local opportunities for public health intervention.10
In California, demographic differences in CS cases echo higher rates of syphilis among reproductive-age females, particularly with regard to the geographic region of birth and race/ethnicity of the birthing parent (i.e., pregnant parents who birth their infant). Known racial/ethnic inequities in syphilis rates are caused by structural determinants including racism increased case numbers and rates of prenatal syphilis and CS.11 In 2018, the statewide rate of syphilis among Black females was 30.2 per 100,000 persons compared with 9.9 and 11.4 per 100,000 persons for White/non-Hispanic and Hispanic females, respectively.12 Geographic region shows similar patterns. For instance, in 2018 the rate of early syphilis among females 15–44 years old in Central California was more than double the statewide rate (56 vs. 25 per 100,000 people).13,14
In 2018 in California, 57% of birthing parents of CS infants (inclusive of liveborn and syphilitic stillbirths) reported delayed or no prenatal care; 51% reported methamphetamine use within the past 12 months; 26% reported incarceration within the past 12 months; and 22% reported experiencing homelessness.15 Comparatively, of all live births in California in 2018, only 3.7% were born to birthing parents who received late or no prenatal care.16 This discrepancy alludes to available prenatal care for the state’s general population, which may not be accessed by the majority of birthing parents of infants with CS. Studies of community-specific syphilis increases among pregnant people also identify features of structural racism and other health determinants including poverty, homelessness, substance use, and incarceration history as contributors to gaps in prenatal screening and treatment, resulting in increased CS cases.17–24 To date, these intersecting characteristics have not been analyzed in an adjusted model to develop an improved understanding of their relationship to CS.
Here, we performed regression modeling to identify birthing parent characteristics associated with delivering an infant with CS. We then used a CS prevention continuum23,25 to identify specific prenatal missed opportunities for birthing parents who are homeless and those who use methamphetamine.
MATERIALS AND METHODS
Study design and population
Data on pregnant people with syphilis and their infants were collected via routine sexually transmitted diseases (STD) surveillance activities within the California Project Area, including all of California except Los Angeles and San Francisco counties (due to separate federal funding streams and surveillance data management systems). Data were entered into the state surveillance system by local public health staff and reviewed by California Department of Public Health (CDPH) staff for quality assurance.
The study population included birthing parents diagnosed with syphilis during pregnancy or at delivery between January 1, 2017, and December 31, 2018, who were linked to an infant with a documented CS outcome26 (either CS or non-CS) and were interviewed and medical records reviewed, both of which are part of routine disease intervention for syphilis cases diagnosed during pregnancy or at delivery. Pregnant people with syphilis who did not link to an infant CS outcome within nine months of diagnosis or who were not interviewed were excluded. This project was reviewed by the California Health and Human Services Agency’s Committee for the Protection of Human Subjects and deemed exempt.
Data measures
CS was per the 2018 CDC surveillance case definition and included syphilitic stillbirths. This case definition encompasses laboratory-confirmed CS cases, cases where CS is probable based on infant clinical criteria, and cases where CS is probable due to inadequately treated or untreated prenatal syphilis. Birthing parent demographic variables included age, race/ethnicity (Black, white, Hispanic, other), and geographic region (Northern, Bay Area, Central, Southern). Socio-behavioral characteristics present in the past 12 months included methamphetamine use, injection drug use, incarceration, and partner methamphetamine use and incarceration. Self-reported housing status around the time of diagnosis was included. Homelessness was defined as either residence type noted as “homeless” during the interview, or documentation of a predefined term associated with unstable housing (e.g., “homeless,” “unstable housing,” “couch surfing,” “SRO” (single room occupancy hotel), “living on street”) in the medical record or investigation notes. Incarceration, methamphetamine use, and injection drug use were identified by self-report during interviews or documentation in the medical record or investigation notes. Partner methamphetamine use and/or incarceration in the past 12 months were per self-report. Interview questions in which an answer was either “refused” or blank were counted as null. The syphilis stage and timing of prenatal care initiation were extracted from the surveillance case report form.
Clinical CS risk factors included disease stage and timing of prenatal care initiation. The stage was dichotomized as early—including primary, secondary, and early non-primary non-secondary (also known as early latent) stages—and late-latent/unknown duration. Prenatal care initiation was defined as before 20 weeks’ gestation, at/beyond 20 weeks’ gestation, or none.
Statistical analysis
Descriptive statistics were calculated to characterize birthing parents of infants with CS and without CS. In addition, sensitivity comparisons of birthing parents linked versus not linked to an infant (thus excluded from further analysis), and those interviewed versus not interviewed (also excluded from further analysis), were performed for age, stage of disease, geographic region, and race/ethnicity. Statistical significance was assessed using chi-square tests, p-value < .05 considered significant.
Univariate logistic regression identified variables associated with CS. All significant variables in univariate analyses were included in a multivariable logistic regression. The regression was performed in a stepwise fashion beginning with demographic, staging and socio-behavioral variables to create Model 1, to determine which variables significantly associated with CS might be mediated or modified by prenatal care. Prenatal care was then incorporated to create the final Model 2. All analyses were performed using SAS version 9.4 (SAS Institute, Inc.).
Congenital syphilis prevention continuums (CSPC)—modeled after HIV care cascades23,25—were created to identify specific prenatal opportunities for CS prevention. Surveillance records of birthing parents were reviewed for the following, occurring at least 30 days before delivery: (1) first prenatal care visit; (2) first syphilis test; (3) syphilis treatment initiation. Cases were assessed for appropriate treatment according to disease stage.27 Data for each sequential continuum bar included cases counted in the preceding bar(s). The final bar in the CSPC, the CS Prevention Ratio (CSPR), reflects the proportion of CS cases averted (i.e., the number of non-CS infants divided by the number of birthing parents). Twins were counted as a single birth.
Model 2 identified subpopulations in which the association with CS was diminished when adjusting for prenatal care. We, therefore, stratified the CSPC by these variables to explore specific points of difference in prenatal care. Finally, additional stratified continuums considered only birthing parents with documented prenatal care.
RESULTS
Descriptive, univariate, and multivariable analyses
Between January 1, 2017, and December 31, 2018, 7189 females with syphilis were identified, 1391 (19%) of whom were pregnant. Of those, 1084 (78%) were linked to an infant with a CS outcome in the surveillance system, and 720 (66%) were interviewed and included in analyses (Figure 1). Among them, 245 (34%) delivered an infant with CS.
FIGURE 1.
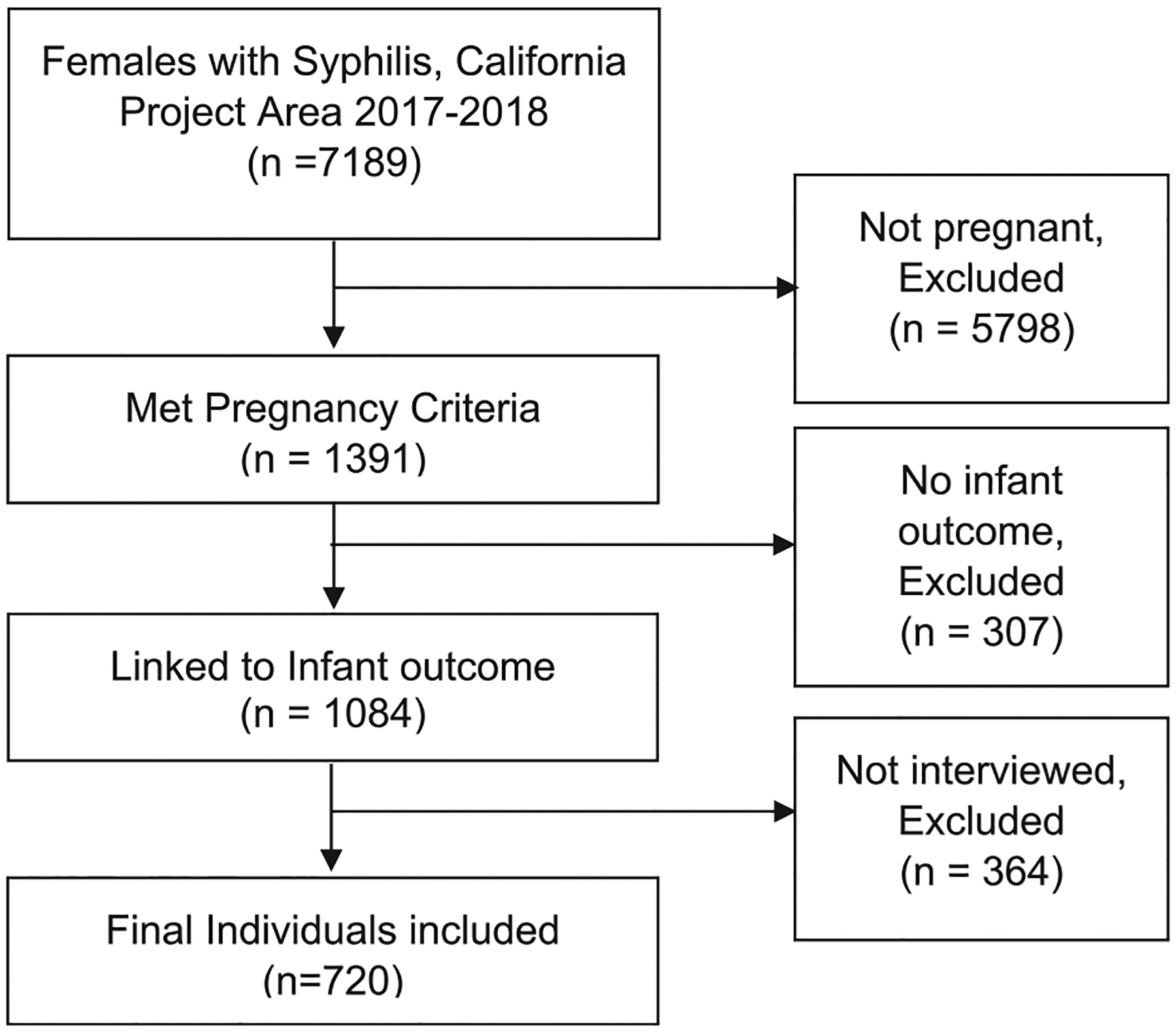
Inclusion and exclusion criteria
Among those included in analyses, there were no significant differences in age or race/ethnicity between birthing parents of infants with CS compared with those who delivered non-CS infants (Table 1). Compared with non-CS infants, infants with CS were more likely to be born to birthing parents who used methamphetamine, (46% vs. 27%, p < .001), experienced homelessness (23% vs. 10%, p < .001), or whose partner used methamphetamine (33% vs. 25%, p = .01) within the prior 12 months.
TABLE 1.
Characteristics of birthing parent by CS outcome, CA Project Area 2017–2018
| Overall (n = 720) | CS (n = 245) | Non-CS (n = 475) | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | N | % | p value | |
| Age group | .77 | ||||||
| 13–19 | 67 | 9.3 | 19 | 7.8 | 48 | 10.1 | |
| 20–24 | 178 | 24.7 | 57 | 23.3 | 121 | 25.5 | |
| 25–29 | 218 | 30.3 | 77 | 31.4 | 141 | 29.7 | |
| 30–34 | 149 | 20.7 | 53 | 21.6 | 96 | 20.2 | |
| 35+ | 108 | 15.0 | 39 | 15.9 | 69 | 14.5 | |
| Race/ethnicitya | .20 | ||||||
| Black | 82 | 11.8 | 31 | 12.9 | 51 | 11.2 | |
| Hispanic | 366 | 52.7 | 117 | 48.6 | 249 | 54.9 | |
| White | 207 | 29.8 | 82 | 34.0 | 125 | 27.5 | |
| Otherb | 40 | 5.8 | 11 | 4.6 | 29 | 6.4 | |
| Regionc | .06 | ||||||
| North/Sac | 70 | 9.7 | 16 | 6.5 | 54 | 11.4 | |
| Bay Area | 57 | 7.9 | 15 | 6.1 | 42 | 8.8 | |
| Central | 426 | 59.2 | 159 | 64.9 | 267 | 56.2 | |
| South | 167 | 23.2 | 55 | 22.5 | 112 | 23.6 | |
| Ever diagnosed with STDd | .22 | ||||||
| Yes | 257 | 35.7 | 95 | 38.8 | 162 | 34.1 | |
| Methamphetamine usee | <.001 | ||||||
| Yes | 240 | 33.3 | 112 | 45.7 | 128 | 27.0 | |
| Incarceratione | .13 | ||||||
| Yes | 120 | 16.7 | 48 | 19.6 | 72 | 15.2 | |
| Homelessness | <.001 | ||||||
| Yes | 101 | 14.0 | 55 | 22.5 | 46 | 9.7 | |
| IDUe | .49 | ||||||
| Yes | 41 | 5.7 | 16 | 6.5 | 25 | 5.3 | |
| Partner methamphetamine usee | .01 | ||||||
| Yes | 193 | 26.8 | 81 | 33.1 | 112 | 23.6 | |
| Partner incarceratione | .42 | ||||||
| Yes | 155 | 21.5 | 57 | 23.3 | 98 | 20.6 | |
| Stage | <.001 | ||||||
| Early | 287 | 39.9 | 128 | 52.2 | 159 | 33.5 | |
| Late | 433 | 60.1 | 117 | 47.8 | 316 | 66.5 | |
| Gestational age at first Prenatal Care | <.001 | ||||||
| At or before 20 weeks | 307 | 42.6 | 51 | 20.8 | 256 | 53.9 | |
| After 20 weeks | 310 | 43.1 | 113 | 46.1 | 197 | 41.5 | |
| None | 103 | 14.3 | 81 | 33.1 | 22 | 4.6 | |
Note: Compared with non-CS infants, infants with CS were more likely to be born to birthing parents who used methamphetamine, experienced homelessness, or whose partner used methamphetamine within the prior 12 months. Significant differences were seen with regard to the syphilis stage and timing of prenatal care. Bold values are statistically significant.
Abbreviations: CA, California; CS, congenital syphilis; STD, sexually transmitted diseases.
Race/ethnicity missing for 25 females.
Other includes American Indian/Alaska Native, Asian/Pacific Islander, Multirace, Other.
San Francisco and Los Angeles are excluded.
Ever diagnosed with an STD includes diagnosis with chlamydia, gonorrhea, or syphilis.
Within the last 12 month.
Significant differences were seen with regard to syphilis stage (p < .001) and timing of prenatal care (p < .001) (Table 1). Approximately half (52%) of those who delivered an infant with CS had early-stage syphilis in contrast to 32% of those who delivered non-CS infants. 79% of those who delivered infants with CS had not received prenatal care by 20 weeks’ gestation, compared to 47% of those who delivered of non-CS infants. Importantly, 33% of those who delivered infants with CS reported no prenatal care, versus 5% of those who delivered non-CS infants.
In univariate analyses (Table 2), the following variables were significantly associated with delivering an infant with CS: having received no prenatal care (OR = 18.5, 95% CI: 10.6, 32.3) or late prenatal care (OR = 2.9, 95% CI: 2.0, 4.2); homelessness (OR = 2.7, 95% CI: 1.8, 4.1); methamphetamine use (OR = 2.3, 95% CI: 1.7, 3.2); living in the Central region (OR = 2.0, 95% CI: 1.1, 3.6); early stage (OR = 2.2, 95% CI: 1.6, 3.0); and partner methamphetamine use (OR = 1.6, 95% CI: 1.1, 2.2). All variables in the first adjusted analysis (Model 1) remained associated with CS, with the exceptions of partner methamphetamine use. Southern region became significantly associated with CS in Model 1 as well (OR = 2.3 95% CI: 1.2, 4.5). After the addition of prenatal care to create the final Model 2, the following were significantly associated with CS: having received no prenatal care (OR = 16.7, 95% CI: 9.2, 30.3) or late prenatal care (OR = 2.9, 95% CI: 1.9, 4.2); early stage of syphilis (OR = 2.6, 95% CI: 1.8, 3.7); living in the Central region (OR = 2.1, 95% CI: 1.1, 4.2). Birthing parents with homelessness or methamphetamine use were not more likely to have infants with CS compared with birthing parents without these characteristics, after adjusting for the variables above.
TABLE 2.
Univariate and adjusted logistic regression: birthing parent characteristics and CS outcome, without (Model 1) and with (Model 2) prenatal care
| Univariate Crude OR (95% CI) | Model 1: aOR (95% CI) | Model 2: aOR (95% CI) | |
|---|---|---|---|
| Age group | Not significant | - | - |
| Race/ethnicitya | Not significant | - | - |
| Regionb | |||
| North/Sac | Ref | Ref | Ref |
| Bay Area | 1.2 (0.5–2.7) | 1.6 (0.7–3.7) | 1.8 (0.7–4.7) |
| Central | 2.0 (1.1–3.6) | 2.4 (1.3–4.4) | 2.1 (1.1–4.2) |
| South | 1.7 (0.9–3.2) | 2.3 (1.2–4.5) | 2.1 (0.99–4.3) |
| Ever diagnosed STDc | Not significant | - | - |
| Meth use5 | |||
| Yes | 2.3 (1.7–3.2) | 2.1 (1.4–3.1) | 1.5 (0.96–2.4) |
| No | Ref | Ref | Ref |
| Incarcerationd | Not significant | - | - |
| Homelessness | |||
| Yes | 2.7 (1.8–4.1) | 2.5 (1.6–4.0) | 1.7 (0.99–2.9) |
| No | Ref | Ref | Ref |
| IDUd | Not significant | - | - |
| Partner methd | - | ||
| Yes | 1.6 (1.1–2.2) | 0.8 (0.5–1.2) | 0.7 (0.4–1.2) |
| No | Ref | Ref | Ref |
| Partner incarceratedd | Not significant | - | - |
| Stage | |||
| Early | 2.2 (1.6–3.0) | 2.2 (1.6–3.1) | 2.6 (1.8–3.7) |
| Late | Ref | Ref | Ref |
| Gest. age first PNC | |||
| At or before 20 weeks | Ref | - | Ref |
| After 20 weeks | 2.9 (2.0–4.2) | - | 2.9 (1.9–4.2) |
| None | 18.5 (10.6–32.3) | - | 16.7 (9.2–30.3) |
Note: In univariate analyses, the following were significantly associated with delivering an infant with CS: having received no or late prenatal care; homelessness; methamphetamine use; living in the Central region; early stage; and partner methamphetamine use. In the final Model 2, having received late or no prenatal care; early stage of syphilis; living in the Central region remained associated with CS. However, birthing parents experiencing homelessness or methamphetamine use were not more likely to have infants with CS compared with birthing parents without these characteristics. Bold values are statistically significant.
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; CS, congenital syphilis; STD, sexually transmitted diseases.
Race/ethnicity missing for 25 females.
San Francisco and Los Angeles local health jurisdictions are excluded.
Ever diagnosed with an STD includes diagnosis with chlamydia, gonorrhea, or syphilis.
Timing is within the last 12 months.
CS prevention continuums stratified for methamphetamine use and homelessness
CSPCs shown in Table 3 present differences in prenatal prevention steps stratified by methamphetamine use and homelessness. Although the region of birth and early stage of syphilis were also significantly associated with CS outcome, the addition of prenatal care did not weaken the association, and thus neither region nor stage was explored with a unique CSPC.
TABLE 3.
Congenital syphilis (CS) prevention continuums: Prenatal syphilis prevention among total population versus prenatal care recipients, by methamphetamine use and housing status
| Prenatal visita (%) | Tested for syphilisa (%) | Initiateda treatment(%) | Treated correctly (%) | CS cases prevented (%) | p value (CSPR) | |
|---|---|---|---|---|---|---|
| Metham-phetamine use | ||||||
| Total study population (n = 720) | ||||||
| No meth. use (n = 480) | 91 | 84 | 77 | 76 | 72 | <.001 |
| Meth. use (n = 240) | 74 | 67 | 60 | 57 | 53 | |
| Prenatal care recipients (n = 614) | ||||||
| No meth. use (n = 437) | - | 93 | 84 | 83 | 79 | .06 |
| Meth. use (n = 177) | - | 90 | 81 | 77 | 72 | |
| Housing status | ||||||
| Total study population (n = 720) | ||||||
| Not homeless (n = 619) | 89 | 81 | 74 | 73 | 69 | <.001 |
| Homeless (n = 101) | 65 | 60 | 52 | 50 | 46 | |
| Prenatal care recipients (n = 614) | ||||||
| Not homeless (n = 548) | - | 92 | 84 | 82 | 78 | .12 |
| Homeless (n = 66) | - | 92 | 80 | 77 | 70 |
Note: Among all people with syphilis in pregnancy, both methamphetamine use, and unstable housing status were significantly associated with failure to prevent CS compared to those who did not have these characteristics. However, when including only people with documented prenatal care, there were no statistical differences with regard to methamphetamine groups or housing status. Bold values are statistically significant.
Abbreviation: CSPR, CS prevention ratio.
Occurred at least 30 days before delivery.
When stratifying by methamphetamine use, the largest drop in the continuum was prenatal care entry (91% and 74% for non-methamphetamine use vs. methamphetamine use, respectively [p < .001]); CSPRs—the proportion of CS cases prevented—were 72% and 53% respectively (p < .001). However, when including only people with documented prenatal care, there were no statistical differences with regard to methamphetamine groups.
The CSPC stratified by homelessness similarly showed the largest gap was at the time of prenatal care entry (89% vs. 65% for non-homelessness and homelessness respectively [p < .001]); CSPRs were 69% and 46%, respectively (p < .001). When considering only those who received prenatal care, there were no significant differences between groups (Table 3).
Sensitivity analyses
When comparing those interviewed to those not interviewed (and thus excluded from analysis), fewer interviewees were Black (p = .032), and lived in the Southern region (p < .001); more interviewees lived in the Central region (p < .001) and had early-stage syphilis (p < .001).
When comparing those linked to an infant to those not linked (thus excluded from analysis), fewer linkages were listed as “other” with regard to race/ethnicity (0.004). There were also regional differences for infant linkage, with fewer linkages occurring for those living in the Southern region compared to other regions (p = .024).
DISCUSSION
Principle findings
In adjusted models of CS in California, the following was statistically significantly associated with CS outcomes: receiving late or no prenatal care, early stage of syphilis, and living in the Central region. Prenatal care significantly attenuated associations between CS and homelessness, and CS and methamphetamine use. For birthing parents who use methamphetamine and those experiencing homelessness, population-specific CSPCs showed a significant drop-off at prenatal care entry. Yet, among birthing parents engaged in care, methamphetamine use and housing status did not impact the likelihood of CS prevention. Meanwhile, associations between region and CS, as well as stage of disease and CS, were not strongly affected by the presence or absence of prenatal care in adjusted analysis.
Although our descriptive findings were consistent with previously known associations with CS,5–8,23 our adjusted analysis identified missed opportunities for subpopulations affected by methamphetamine use or homelessness, which impacted the majority of infants with CS in California. Stratified CSPCs showed that while lower proportions of those who used methamphetamine and/or experienced homelessness entered prenatal care—and thus missed opportunities for CS prevention—when considering solely those with documented prenatal care, differences with regard to these variables ceased to be significant.
From a clinical perspective, entry into prenatal care is a crucial step for syphilis screening and treatment. Yet, screening and treatment may also be done wherever pregnant individuals present—an emergency room or urgent care, substance use treatment facility, jail, or STD clinic. Notably, individuals with risk factors for syphilis (e.g., substance use disorders, homelessness) may face significant barriers to entering traditional prenatal care settings.28–30 Improved access to services could be achieved by recognizing that prenatal care—inclusive of syphilis screening and treatment—may be initiated wherever pregnant people seek care. However, those who enter prenatal care, regardless of substance use or housing status, may have important characteristics that facilitate retention in care, and thus treatment completion and CS prevention. Furthermore, this finding suggests providers and public health staff who assist in coordinating syphilis treatment for pregnant people may deliver adequate care across these subpopulations. Conversely, to achieve elimination of CS, creative strategies may be needed to reach individuals who are not sufficiently accommodated by existing prenatal care systems, particularly those affected by homelessness or methamphetamine use, in light of well-documented stigma and discrimination experienced in healthcare settings by both of these groups.
With regard to demographics, both poverty and limited access to health care may contribute to higher rates of syphilis and subsequent CS in the Central region.31 Furthermore, Central California is the heart of the state’s agricultural industry; limited insurance provision, inadequate services for people with limited English proficiency, and hesitancy to seek medical care in light of immigration status may all pose barriers to syphilis diagnosis and treatment. Unlike methamphetamine use and housing status, the inclusion of prenatal care in the model did not impact the association between Central region and CS in adjusted analyses, suggesting other factors not routinely surveilled, as those mentioned above, maybe particularly powerful.
With regard to race and ethnicity, when considering only pregnant people with syphilis as in this analysis, there were no differences in CS outcome. Prenatal care did not affect inequities, as there was no widening of the gap across racial groups. However, from an equity perspective, because of the underlying unequal prevalence of syphilis among females in California who are not pregnant, Black females and their infants are disproportionately affected by CS. Prenatal care did not narrow gaps that exist before pregnancy. These data highlight the importance of focusing prevention and treatment efforts not only during pregnancy but outside of pregnancy to combat structural racism and long-standing racial inequities.
Strengths and limitations
Our paper was strengthened by multiple aspects of the study’s design and analysis. First, our study included a large public health surveillance data set from the majority of California counties. Our study is strengthened by its academic-government partnership, which afforded both epidemiologic and clinical perspectives to be incorporated into design, analyses, and interpretation. Finally, our analyses expanded upon an adjusted model, and used novel stratified CSPCs to identify points of intervention for subpopulations most affected by CS.
There are several limitations to our study. First, surveillance data is limited to individuals tested for syphilis and reported to the public health department; data collection and entry are subject to human error and inconsistency across counties. As such, underestimates of the number of syphilis may exist, and there is potential for the inaccuracy of the data. Second, our data does not include San Francisco and Los Angeles local health jurisdictions. While San Francisco had just 1 CS case during the study period, the city of Los Angeles reported 98 cases from 2017 to 2018 which was lacking in this data set. Also, the nuances of CS prevention in the context of homelessness and methamphetamine for California’s two major urban areas were able to be not explored in this study. Third, persons not interviewed were excluded, which may disproportionately exclude certain groups, particularly those experiencing homelessness and/or substance use and those with limited English proficiency. Therefore, these variables may be underestimated. Sensitivity comparisons showed a significant difference in clinical-stage between interviewed versus not interviewed. Although all pregnant people with syphilis are prioritized for disease investigation (including interviews), this difference is likely due to the public health’s prioritization to locate people with transmissible early-stage disease. Thus, people with the early-stage disease were overrepresented. Race/ethnicity and regional differences in both infant-linked and interviewed comparisons were also appreciated, suggesting our sample might not be generalizable to not linked/non-interviewed birthing parents with regard to these variables. In addition, the counting of “refused” or blank interview answers as null may further underestimate stigmatizing characteristics. The use of a keyword search for identifying homelessness may miss people who were experiencing homelessness if all keywords were absent and may misidentify someone as homeless if a keyword was present. Moreover, experiencing homelessness may change over time, and types of homelessness (e.g., unsheltered, staying in a shelter, or couch surfing) may variably affect health outcomes including CS.32 Finally, variables in our analyses did not account for other factors that might influence prenatal care entry: transportation barriers, immigration status, concerns around loss of parental rights, or perceived stigma or discrimination by providers—all of which have been reported by frontline clinicians and public health staff in CS case reviews but are not routinely collected in surveillance data.33,35 Research is needed to evaluate alternative care models designed to expand prenatal care access to populations most affected by CS. In addition, further work is needed to explore factors driving local geographic differences in CS prevention. Lastly, interventions to address structural racism contributing to racial inequities in female syphilis before pregnancy are urgently needed.
CONCLUSION
This analysis demonstrates the importance of early prenatal care initiation in preventing CS. Programs that support prenatal care engagement in populations facing significant barriers to care—particularly those experiencing homelessness, or who use methamphetamine—are essential to successfully prevent CS cases. This may be particularly important to providers in substance use treatment programs, who have an opportunity to detect and treat syphilis during or before pregnancy among people at increased risk of infection. More broadly, efforts to detect and treat syphilis in pregnancy outside of traditional prenatal care settings (e.g., emergency departments, urgent care, harm reduction programs, public health outreach, homeless service agencies, correctional facilities) may afford additional CS prevention opportunities.
ACKNOWLEDGMENTS
We are very grateful for the tireless work of the California Department of Public Health and local health jurisdiction disease investigation staff who contribute to the surveillance of people with syphilis and other STDs. We particularly thank Ashley Dockter, MPH; Lupe Espain; Jessica Frasure-Williams, MPH; Denise Gilson; Jennifer Harmon, MPH; Kimberly Hernandez, MPH, CPH; Lydia Lizardo; Alira Medel, BA; Romni Neiman; Kelly Nguyen, MPH; Raquel Paz; Meghan Polich, MPH; Melissa Reyna, MPH; Leila Yasmin Saadat, MPH; Denise Smith, PHN, MPA. This manuscript was developed as an activity of the California Department of Public Health STD Control Branch, funded by the Centers for Disease Control and Prevention CDC-RFA-PS19-1901: Strengthening STD Prevention and Control for Health Departments (STD PCHD); Grant no. NH25PS005127.
Funding information
Centers for Disease Control and Prevention, Grant/Award Number: CDC-RFA-PS19-1901; Strengthening STD Prevention and Control for Health Departments (STDPCHD), Grant/Award Number: NH25PS005127
Footnotes
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests. The authors alone are responsible for the content and writing of this paper.
REFERENCES
- 1.Trivedi S, Williams C, Torrone E, Kidd S. National trends and reported risk factors among pregnant women with syphilis in the United States, 2012–2016. Obstet Gynecol. 2019;133(1):27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2019. US Department of Health and Human Services; 2019. [Google Scholar]
- 3.Bowen VB, McDonald R, Grey JA, Kimball A, Torrone EA. High congenital syphilis case counts among US infants born in 2020. N Engl J Med. 2021;385(12):1144–1145. [DOI] [PubMed] [Google Scholar]
- 4.California Department of Public Health. Sexually Transmitted Diseases Control Branch Data 2019. 2020, 2021.
- 5.Alexander JM, Sheffield JS, Sanchez PJ, Mayfield J, Wendel GD. Efficacy of treatment for syphilis in pregnancy. Obstet Gynecol. 1999;93(1):5–8. [DOI] [PubMed] [Google Scholar]
- 6.Cheng JQ, Zhou H, Hong FC, et al. Syphilis screening and intervention in 500 000 pregnant women in Shenzhen, the People’s Republic of China. Sex Transm Infect. 2007;83(5):347–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qin J-B, Feng T-J, Yang T-B, et al. Risk factors for congenital syphilis and adverse pregnancy outcomes in offspring of women with syphilis in Shenzhen, China: a prospective nested case-control study. Sex Transm Dis. 2014;41(1):13–23. [DOI] [PubMed] [Google Scholar]
- 8.Zhu L, Qin M, Du L, Xie R-h Wong T, Wen SW. Maternal and congenital syphilis in Shanghai, China, 2002 to 2006. Int J Infect Dis. 2010;14:e45–e48. [DOI] [PubMed] [Google Scholar]
- 9.Hong F-C, Wu X-B, Yang F, et al. Risk of congenital syphilis (cs) following treatment of maternal syphilis: results of a CS control program in China. Clin Infect Dis. 2017;65:588–594. [DOI] [PubMed] [Google Scholar]
- 10.Kimball A, Torrone E, Miele K, et al. Missed opportunities for prevention of congenital syphilis—United States, 2018. Morb Mortal Wkly Rep. 2020;69(22):661–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McLemore MR, Altman MR, Cooper N, Williams S, Rand L, Franck L. Health care experiences of pregnant, birthing and postnatal women of color at risk for preterm birth. Soc Sci Med. 2018;201:127–135. [DOI] [PubMed] [Google Scholar]
- 12.California Department of Public Health. Sexually Transmitted Diseases Control Branch. Syphilis Tables California, 2019. Accessed March 30, 2020.
- 13.California Department of Public Health. Sexually Transmitted Diseases Control Branch. Congenital Syphilis. 2020. Accessed March 30, 2020. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/CongenitalSyphilis.aspx
- 14.Plotzker RE, Murphy RD, Stoltey JE. Congenital syphilis prevention: strategies, evidence, and future directions. Sex Transm Dis. 2018;45: S29–S37. [DOI] [PubMed] [Google Scholar]
- 15.Burghardt NO, Dockter A, Murphy RD. Stratification of the California Project Area (CPA) congenital syphilis (CS) prevention cascade by methamphetamine use to explore points of intervention for priority populations. National Coalition of STD Directors Engage Conference; November 20, 2019. [Google Scholar]
- 16.March of Dimes Peristats: California. Quick Facts Prenatal Care. Accessed April 7, 2020. 2020; https://www.marchofdimes.org/peristats/ViewTopic.aspx?reg=06%26top=5%26lev=0%26slev=4
- 17.Patel SJ, Klinger EJ, O’Toole D, Schillinger JA. Missed opportunities for preventing congenital syphilis infection in New York City. Obstet Gynecol. 2012;120(4):882–888. [DOI] [PubMed] [Google Scholar]
- 18.Taylor MM, Mickey T, Browne K, Kenney K, England B, Blasini-Alcivar L. Opportunities for the prevention of congenital syphilis in Maricopa County, Arizona. Sex Transm Dis. 2008;35(4): 341–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Trepka MJ, Bloom SA, Zhang G, Kim S, Nobles RE. Inadequate syphilis screening among women with prenatal care in a community with a high syphilis incidence. Sex Transm Dis. 2006;33(11):670–674. [DOI] [PubMed] [Google Scholar]
- 20.Paz-Bailey G, Teran S, Levine W, Markowitz LE. Syphilis outbreak among Hispanic immigrants in Decatur, Alabama: association with commercial sex. Sex Transm Dis. 2004;31(1):20–25. [DOI] [PubMed] [Google Scholar]
- 21.DiOrio D, Kroeger K, Ross A. Social vulnerability in congenital syphilis case mothers: qualitative assessment of cases in Indiana, 2014–2016. Sex Transm Dis. 2018;45(7):447–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blank S, McDONNELL DD, Rubin SR, et al. New approaches to syphilis control: finding opportunities for syphilis treatment and congenital syphilis prevention in a women’s correctional setting. Sex Transm Dis. 1997;24(4):218–226. [DOI] [PubMed] [Google Scholar]
- 23.Biswas HH, Chew Ng RA, Murray EL, et al. Characteristics associated with delivery of an infant with congenital syphilis and missed opportunities for prevention—California, 2012 to 2014. Sex Transm Dis. 2018;45(7):435–441. [DOI] [PubMed] [Google Scholar]
- 24.Wagman JAHE, Smith D, Buekens P, et al. Research brief. Addressing the rise of congenital syphilis in California and Louisiana: Working toward setting-specific solutions among high-risk pregnant women. May 2019.
- 25.Gardner EM, McLees MP, Steiner JF, del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011; 52(6):793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Case Definitions in Effect During 2019 (Syphilis, Congenital). 2019. Accessed December 20, 2021. https://www.cdc.gov/std/statistics/2019/case-definitions.htm
- 27.Workowski KABG. Sexually transmitted diseases treatment guidelines, 2015. MMWR. 2015;64:34–48. [PMC free article] [PubMed] [Google Scholar]
- 28.Smid M, Bourgois P, Auerswald CL. The challenge of pregnancy among homeless youth: Reclaiming a lost opportunity. J Health Care Poor Underserved. 2010;21(2 suppl):140–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Richards R, Merrill RM, Baksh L. Health behaviors and infant health outcomes in homeless pregnant women in the United States. Pediatrics. 2011;128(3):438–446. [DOI] [PubMed] [Google Scholar]
- 30.Roberts SC, Pies C. Complex calculations: how drug use during pregnancy becomes a barrier to prenatal care. Matern Child Health J. 2011;15(3):333–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cuffe KM, Kang JDY, Dorji T, et al. Identification of US counties at elevated risk for congenital syphilis using predictive modeling and a risk scoring system. Sex Transm Dis. 2020;47(5):290–295. [DOI] [PubMed] [Google Scholar]
- 32.Clemenzi-Allen A, Geng E, Christopoulos K, et al. Degree of housing instability shows independent “dose-response” with virologic suppression rates among people living with human immunodeficiency virus. Paper presented at: Open forum infectious diseases; 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harville EW, Giarratano GP, Buekens P, Lang E, Wagman J. Congenital syphilis in East Baton Rouge parish, Louisiana: providers’ and women’s perspectives. BMC Infect Dis. 2021;21(1):64. doi: 10.1186/s12879-020-05753-6 [DOI] [PMC free article] [PubMed] [Google Scholar]


