SUMMARY
Active symptom surveillance was applied to three selected communities ( 160 147 persons) in Tianjin from 2010 to 2012. We examined 1089 individuals showing pertussis-like symptoms, of which 1022 nasopharyngeal specimens were tested for pertussis by polymerase chain reaction and 802 sera for anti-pertussis toxin antibodies. Of the total cases tested, 113 were confirmed, and their demographic, clinical, and vaccination-related data were collected. The annual incidence was 23·52 cases/100 000 persons among communities, which was 16·22 times that obtained via hospital reports for the same period (P < 0·001). The actual incidence in the 15–69 years age group was most significantly underestimated by hospitals, given that it was 43·08 times that of the reported hospital rate. Among the cases aged <15 years, 84·5% were individuals who had been fully vaccinated. The misdiagnosis rate was as high as 94·69%, and only 5·31% of the confirmed pertussis cases were properly diagnosed as pertussis at their first medical visit. Pertussis incidence in China has been severely underestimated and this was in part due to a high misdiagnosis rate. Adolescents and adults have become new high-risk populations. Future work should focus on reinforcing immunization programmes, especially among adolescents and adults.
Key words: Community populations, epidemiological features, high immunization coverage, pertussis resurgence, symptom surveillance
INTRODUCTION
Pertussis (whooping cough) is a highly contagious and potentially life-threatening disease that posed a substantial public health burden in the pre-vaccine era [1]. Since the initiation of the Expanded Programme on Immunization by the World Health Organization (WHO) in 1974, the morbidity and mortality caused by pertussis infection have been largely ameliorated worldwide [2]. In China, the incidence based on hospital reports was maintained under 0·2 cases/100 000 persons between 2006 and 2010, as recorded in the China National Infectious Diseases Surveillance System [3]. In Tianjin, the incidence of pertussis had decreased from 540·10 cases/100 000 persons in 1963 to 0·18 cases/100 000 persons in 2009 [4, 5]. The diphtheria, tetanus toxoid, whole-cell pertussis (DTwP) vaccine was introduced into the national childhood immunization schedule in 1973, which was replaced by a diphtheria, tetanus toxoid, acellular pertussis (DTaP) vaccine in May 2007. Both DTwP and DTaP vaccines are administered in the 3rd, 4th, and 5th months of life, followed by one booster dose given at age 18 months [6]. Since 2000, vaccination coverage in target populations has always been above 95%.
Despite a significant improvement in pertussis control and prevention, the disease is far from being eradicated. Over the last two decades, there was pertussis resurgence in a number of developed countries with high vaccination coverage such as the USA, Japan, Australia and South Korea [7–10]. It was estimated by the WHO that globally around 50 million people have been infected with pertussis, 90% of whom reside in developing countries [11]. China, as part of the developing world, also faces the challenge of combating the rising incidence. Given that pertussis is usually identified via passive hospital reports and lack of laboratory diagnosis in China, patients who did not voluntarily seek medical care may have been missed [3]. Chinese scholars estimated the infection rate of pertussis was 7000–9395/100 000 persons [12, 13]. However, those studies were using too low cut-off values for anti-pertussis toxin (PT) IgG at 30 and 40 IU/ml, respectively, and lacked clinical diagnosis and laboratory test support.
With the aim of determining the true pertussis incidence in regions with high vaccination coverage in China, we adopted a novel approach called active symptom surveillance based on community population. This study involved three selected communities in Tianjin, China, and was conducted between January 2010 and December 2012. In addition, we also investigated the epidemiological features of all subjects, which included clinical symptoms, medical history, and vaccination status.
SUBJECTS, MATERIALS AND METHODS
Community selection and case identification
Each community health service centre was selected from Hongqiao, Beichen and Hangu districts, which represented urban, suburban, and ex-urban areas in Tianjin, China. These centres were 8·2, 29·8 and 63·4 km, respectively, from Tianjin centre. Hongqiao, Beichen and Hangu district centres have populations of 62 798, 60 280 and 37 046 people, respectively. The total population served was an average of 160 147 persons annually. Individuals showing one of the following four symptoms were enrolled in the study: (1) paroxysmal coughing; (2) post-tussive vomiting without other apparent cause; (3) paroxysmal cyanosis or asphyxia in newborns or infants for unidentifiable reasons; (4) a cough lasting at least 2 weeks without other apparent cause [14], when the individual visited a community health service centre and sought medical care, regardless if the first diagnosis was pertussis or another respiratory disease. Specimens were collected and tested, and if the result was positive by culture, polymerase chain reaction (PCR) and serology, the case was diagnosed as a pertussis case. A confirmed pertussis case was defined as the presence of: (1) positive culture; (2) positive PCR test; (3) positive paired serology [fourfold increase in levels of IgG antibodies against pertussis toxin (anti-PT IgG) between the acute and recovery phase blood samples]; or (4) a single serum anti-PT IgG level ⩾80 IU/ml (if the subject had not been vaccinated during the last 3 years) [14]. Verbal informed consent was obtained from subjects or their guardians, as authorized by the Tianjin Centers for Disease Control and Prevention Ethics Committee.
Specimen and information collection
Demographical and clinical information of the subjects were collected and recorded on a daily basis. Two nasopharyngeal (NP) swabs and 2 ml of venous blood were also collected from each subject at the same time. Blood sera was separated by centrifugation at 3000 rpm at 25 °C for 5 min. Specimens to be analysed using PCR or enzyme-linked immunosorbent assays (ELISA) were stored at −20 °C.
Culture
One NP swab was inoculated onto charcoal-cephalexin blood agar (CCBA) followed by incubation at 37 °C for 3–7 days. Potential Bordetella pertussis colonies were picked for Gram staining, catalase and slide agglutination tests as described previously [15].
PCR analysis
The second NP swab was used for PCR detection. Nucleic acids were extracted from NP swabs using the NucliSens easy MAG automated system (bioMérieux, France). Five microlitres of each nucleic acid sample were used as the template to amplify both the IS481 region and pertussis toxin encoding gene (PT gene) in the presence of 1 × PCR buffer, 2 mm MgCl2, 0·2 mm dNTP, 0·2 μm of each gene specific primer, 0·06 U Taq DNA polymerase (Takara, Japan) in a 25 μl reaction. The reactions were conducted in a GeneAmp® PCR System 9700 (Applied Biosystems, USA) and the cycling conditions used were: 94 °C for 10 min, 94 °C for 20 s, 60 °C for 20 s (annealing), 72 °C for 30 s (extension), 72 °C for 5 min. Steps 2–4 were repeated for 40 cycles. The oligonucleotide sequences of the primers were as follows – IS481 forward [IS2 (nt 28–53)]: 5′-GCATGGTTCATCCGAACAACCGGATTTG-3′; IS481 reverse [IS3 (nt 164–138)]: 5′-AATTGCTGGACCATTTCGAGTCGACG-A3′ CGAGTCGACG; PT gene forward: 5′-CCAACGCGCATGCGTGCAGATTCGTC-3’; PT gene reverse: 5′-CCCTCTGCGTTTTGATGGTGCCTATTTTA-3′. All PCR products were resolved in a 1% agarose gel to check for the presence of the IS481 (137 bp) and PT gene (191 bp) specific fragments. The PCR-positive results were considered B. pertussis, when both IS481 (137 bp) and PT gene (191 bp) tested positive at the same time [16].
Serological test
Anti-PT IgG levels in serum samples were determined using ELISA B. pertussis Toxin IgG kits (quantitative) (Institut Virion-Serion GmbH, Germany) according to the manufacturer's instructions. All sera samples were diluted 100-fold before being loaded into microtitre plates. Absorbance at both 405 nm and 630 nm was measured on a spectrophotometer (Sunrise, Tecan, Switzerland). Based on the standards provided with the kits, anti-PT IgG levels ⩾80 IU/ml were regarded as positive [17].
Statistical analysis
Data were analysed using the SPSS v. 19·0 (SPSS Inc., USA) and Microsoft Excel 2003 (Microsoft Corp., USA). Statistical comparisons were performed using Pearson's χ2 test or Fisher's exact test as appropriate. Significance was determined at α = 0·05.
RESULTS
Overall pertussis incidence in community populations
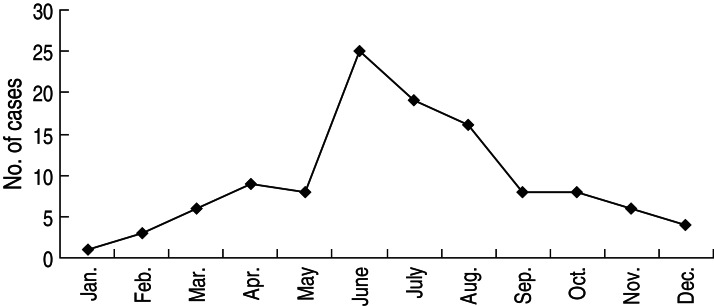
A total of 1089 individuals showing pertussis-like symptoms were examined between January 2010 and December 2012, of whom 10·38% (113/1089) cases were confirmed to have been infected by B. pertussis (Table 1). According to our observations, the annual incidence of each year far exceeded the reported hospital rates (Table 2), resulting in an average of 23·52 cases/100 000 persons (P < 0·001). This number was 16·22 times the annual incidence (1·45 cases/100 000 persons) as documented via passive hospital reports for the same period of time. This strongly suggested a severe underestimation of pertussis incidence in regions with high vaccination coverage in China. Seasonal distribution was higher in summer, although there were cases in every month. There were 25 cases in June, 19 cases in July and 16 cases in August, respectively. The proportion of confirmed cases was 53·10% in summer (Fig. 1).
Table 1.
Overall positive rates of pertussis infection
| Year | No. of cases examined | Samples collected | No. of cases confirmed | Positive rate, % (95% CI) | |
|---|---|---|---|---|---|
| Blood serum | NP swabs | ||||
| 2010 | 312 | 215 | 305 | 36 | 11·54 (7·99–15·09) |
| 2011 | 391 | 306 | 356 | 37 | 9·46 (6·56–12·63) |
| 2012 | 386 | 281 | 361 | 40 | 10·36 (7·32–13·40) |
| Total | 1089 | 802 | 1022 | 113 | 10·38 (8·57–12·19) |
CI, confidence interval; NP, nasopharyngeal.
Table 2.
Comparison of pertussis incidence obtained via symptom surveillance and hospital report
| No. of cases confirmed | Incidence (per 100 000) | |||
|---|---|---|---|---|
| Year | Symptom surveillance | Hospital screening | Fold difference | |
| 2010 | 36 | 22·15 | 1·85 | 11·97 |
| 2011 | 37 | 22·77 | 1·23 | 18·51 |
| 2012 | 40 | 25·36 | 1·27 | 19·97 |
| Total | 113 | 23·52 | 1·45 | 16·22 |
Fig. 1.
Seasonal distribution of confirmed pertussis cases based on community population.
Demographic and geographical characteristics of confirmed cases
As pertussis infections were found to be more prevalent than we had expected, we set out to characterize the confirmed cases. Of the 113 cases, 58 were males and 55 were females, indicating there were no gender-specific differences. In terms of occupation, most of the confirmed patients were students (25·81%) and children (21·77%) attending school or child care on a regular basis. There were also three cases involving medical professionals. Of the three regions examined, the highest incidence (45 cases/100 000 persons) was observed in Hangu district, which was 25-fold of the reported hospital numbers, and represented the most marked difference between active symptom surveillance and passive hospital screening (Table 3). In terms of age distribution, the youngest and the oldest cases were aged 1 month and 69 years, respectively. The majority of the infected cases fell in the 1–6 and 15–69 years age groups accounting for 35·40% (40/113) and 37·19% (42/113) of all confirmed cases, respectively (Table 4). By comparing the reported surveillance and hospital incidences for various age groups, it was found that infants aged <1 year showed the most subtle discrepancy between the two scenarios, with the surveillance-identified incidence being merely 2·24-fold that of the reported hospital results. By contrast, the 15–69 years age group was found to be the most underestimated group. In this group, the actual incidence was 43·08 times that of the reported hospital numbers. Most markedly, it appears to be a trend that the difference in results reported by active symptom surveillance and passive hospital reports increased with age (r = 0·971, P = 0·001).
Table 3.
Pertussis incidence in different regions
| No. of cases | Incidence (per 100 000) | |||
|---|---|---|---|---|
| Region | Symptom surveillance | Hospital screening | Fold difference | |
| Hongqiao | 45 | 23·89 | 0 | — |
| Beichen | 18 | 9·95 | 2·89 | 3·44 |
| Hangu | 50 | 45 | 1·8 | 25 |
| Total | 113 | 23·52 | 1·45 | 16·22 |
Table 4.
Pertussis incidence of different age groups via symptom surveillance and hospital report
| Age group (years) | No. of cases | Incidence (per 100 000) | ||
|---|---|---|---|---|
| Symptom surveillance | Hospital screening | Fold difference | ||
| 0 | 6 | 110·13 | 49·06 | 2·24 |
| 1–6 | 40 | 108·23 | 5·85 | 18·50 |
| 7–14 | 25 | 64·76 | 2·69 | 24·07 |
| 15–69 | 42 | 10·58 | 0·24 | 43·08 |
| Total | 113 | 23·52 | 1·45 | 16·22 |
Test results of confirmed pertussis cases
A single blood of pertussis sample collection rate was 97·34% (110/113). Twenty-three cases that had been vaccinated within 3 years were excluded from the reported findings. The positive rate of anti-PT IgG determined by ELISA was 60·92% (53/87), and the disease course median of confirmed cases was 22 days [interquartile range (IQR) 17–35 days]. The rate of the paired serology sample collection and positive findings were 8·84% (10/113) and 90% (9/10), respectively. NP swab sampling rate and positive rate of PCR were 100% (113/113) and 50·44% (57/113), respectively, and the disease course median of confirmed cases was 10 days (IQR 7–18 days). There was no significant difference in positive detection rates between the anti-PT IgG (60·92%) and NP swab PCR (50·44%) (P = 0·14). Six cases yielded positive results by both PCR and anti-PT IgG. NP swab sampling rate and positive culture rate were just 20·35% (23/113) and 0·00% (0/113), respectively.
Immunization history distribution of confirmed pertussis cases
According to our data, 42 patients aged ⩾15 years had no immunization record, and 2/71 patients (2·82%) aged <15 years had never been vaccinated. Among the latter group, 12·68% (9/71) got the disease before reaching the vaccination age or before the entire vaccination schedule was completed. Markedly, 84·5% (60/71) of the <15 years age group had been fully vaccinated and were still infected. The age distribution of confirmed cases in vaccinated subjects was 1–13 years, of which 30% (18/60) were in the 5–6 years age group, and 25% (15/60) in the 3–4 years age group. The other age distributions were 13·33% (15/60) in the 1–2 years age group, 13·33% (15/60) in the 11–13 years age group, 10% (6/60) in the 7–8 years age group, and 8·33% (5/60) in the 9–10 years age group. The findings indicate that routine vaccination may not be sufficient to protect children from pertussis infection in China.
High misdiagnosis rate at the first doctor's visit
In addition to the above-mentioned higher than expected number of pertussis cases in vaccinated individuals, a high misdiagnosis rate also attracted our attention. Only 5·31% (6/113) of confirmed cases were properly diagnosed with pertussis at their first doctor's visit, while the remainder were misdiagnosed, resulting in an overall misdiagnosis rate of 94·69% (107/113) (Table 5). About half of the misdiagnosed cases (51·32%, 58/113) were mistaken as pneumonia, while cold (18·58%) and tracheitis (15·04%) ranked as the second and the third most frequently diagnosed conditions. With respect to age distribution, around 50% of infants aged <1 year were misdiagnosed and this was relatively low compared to those in the other age groups (92–100%) (P < 0·001), particularly in the ⩾15 years age group where 100% of cases were misdiagnosed. The high misdiagnosis rate could be attributed to atypical symptoms, particularly in the ⩾15 years age group, whose positive rates of typical symptoms (such as paroxysmal coughing, post-tussive vomiting and asphyxia) were only 0–22·64%. The median duration of coughing for the ⩾15 years age group was 25 days (IQR 17–40 days), which was longer than that of the <15 years age group, whose median duration of coughing was 10 days (IQR 7–18 days). This should be of concern to Chinese physicians.
Table 5.
Age distribution of misdiagnosed cases
| Primary diagnosis | Misdiagnosis | ||||||
|---|---|---|---|---|---|---|---|
| Age group (years) | Pneumonia | Bronchitis | Tracheitis | Cold | Pertussis | No. of cases | Percentage (%) |
| 0 | 2 | 0 | 1 | 0 | 3 | 6 | 50·00 |
| 1–6 | 26 | 6 | 4 | 3 | 1 | 40 | 97·50 |
| 7–14 | 15 | 3 | 3 | 2 | 2 | 25 | 92·00 |
| 15–69 | 15 | 2 | 9 | 16 | 0 | 42 | 100·00 |
| Total | 58 | 11 | 17 | 21 | 6 | 113 | 94·69 |
DISCUSSION
In the post-vaccination era, pertussis still remains a major challenge for public health [18]. It was reported that 13–20% of adolescents and adults who had a prolonged cough were found to have been infected with pertussis [19]. This study found that 10·38% of subjects were infected by B. pertussis and the average incidence was 23·52 cases/100 000 persons. This is the first long-term study of pertussis resurgence in community populations with high vaccination coverage in China.
Upon thorough examination, it turned out that the incidence of pertussis was greatly underestimated given the marked disparity between the incidence reported via active symptom surveillance and passive hospital reports. This was reminiscent of what happened in Valencia, Spain, where the surveyed pertussis incidence in a group aged <15 years (46 cases/100 000 persons) substantially exceeded the reported hospital rate (5·1 cases/100 000 persons) [20]. Pertussis surveillance is invariably incomplete and can be affected by enhanced awareness or improved diagnostic methods, leading to perceived changes in epidemiology [21]. The major reason for the high reported incidence of pertussis was that we have established highly sensitive serological and PCR assays to establish the confirmation of pertussis infection.
As pertussis incidence rises in the population, its epidemiological features have also undergone some changes. In terms of age distribution, adolescent and adult cases accounted for 37·17% of all cases. In addition, surveillance-identified incidence in the 15–69 years age group was 43·08 times the reported hospital incidence, displaying the most significant difference between the two study populations in all age groups. More importantly, there appeared to be a trend that the actual incidence of pertussis became more seriously neglected as age increased. Consistent with our findings, some high immunization coverage countries such as the USA and Canada have also experienced a shift of higher pertussis incidence from young children to adolescents and adults [22, 23]. In South Korea, 29·00% of pertussis infection occurred in people aged ⩾15 years [10]. The underlying reasons may include the level of surveillance or natural booster-induced population immunity, and a demographic transition or shift [24, 25].
Children in the 1–6 years age group (35·40%) showed the second highest incidence of pertussis at 108·23/100 000 persons, which was 18·50 times the incidence reported by hospitals. Of the children aged <15 years, 84·5% had been fully immunized with all four scheduled doses of pertussis vaccine. Based on a pertussis immunity level surveillance in Tianjin, the positive immunity rate was even lower for the 1–6 years age group [6]. Therefore the major reason for the high incidence in the 1–6 years age group is that levels of immunity following vaccination decrease rapidly. In addition, adult cases, particularly those where the disease is not prominently manifested, have become an important source of infection for children [26, 27].
It was striking that only six (5·31%) confirmed cases were properly diagnosed as pertussis at their first doctor's visit. Although the <1 year age group showed a relatively low rate of misdiagnosis at 50%, the rates of misdiagnosis in all other age groups were above 92%. In particular, all cases in the adolescent and adult groups were misdiagnosed. This may be due to the fact that pertussis symptoms in adolescents and adults is becoming increasingly less typical [10, 28]. This should be of concern to Chinese physicians.
Some cases exhibiting atypical symptoms are not serious enough to warrant medical assistance, so a larger number of cases were not monitored in this study. As a result there remains a large gap between our results and the true incidence rate of pertussis disease. Another limitation of our study is that the rate of paired serum specimens collected was low, because the cases had improved or were resolved in the recovery stage.
Pertussis re-emergence has posed a big challenge on disease prevention and control in China. Apart from identifying adolescent and adult cases in a timely fashion, it is also necessary to reinforce immunization in adolescents and adults, especially in those who are in close contact with infants (e.g. family members and paediatricians), in order to effectively control the spread of pertussis infection. The Global Pertussis Initiative (GPI) recommended ‘cocoon’ vaccination of all close contacts of infants too young to be vaccinated. This practice was implemented in the USA in 2006 [29–31]. At the same time, many countries have revised their original pertussis vaccination programmes, to consider administering TDaP vaccines to adolescents. For example, in Australia, Canada, Germany, Switzerland, and USA, the final dose of the DTaP vaccine series is administered to young children at age 4–6 years and the TDaP vaccines at age 9–15 years [32]. Considering the current immunization schedule used in China, we suggest using the DTaP vaccine instead of the DT vaccine in children aged 6 years, and that the pertussis immunization schedule should be formulated for adolescents and adults, in order to control pertussis resurgence in China.
ACKNOWLEDGEMENTS
We thank Mingzhu Liu, Hongqiao Community Health Service Center, Shouzhu Li, Tianmu Community Health Service Center, and Ying Zhang, Zhaishang Community Health Service Center. This work was supported by the Research Fund for the Control of Infectious Diseases Study, Tianjin Center for Disease Control and Prevention (TJCDC-2010-CK-01).
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Healy CM, et al. Prevalence of pertussis antibodies in maternal delivery, cord, and infant serum. Journal of Infectious Diseases 2004; 190: 335–340. [DOI] [PubMed] [Google Scholar]
- 2.Meng CY, et al. Current status and perspective of worldwide disease burden of pertussis. Chinese Journal of Vaccines and Immunization 2006; 12: 318–321. [Google Scholar]
- 3.Wang HB, et al. Epidemiological analysis on pertussis in China during 2006–2010. Chinese Journal of Vaccines and Immunization 2012; 18: 207–210. [Google Scholar]
- 4.Huang HT, et al. Analysis on epidemiological characteristic and antibody level of pertussis in Tianjin during 2005–2007. Modern Preventive Medicine 2009; 16: 536–540. [Google Scholar]
- 5.Gao ZG, et al. Analysis on influence factors about resurgence and changing epidemiological characteristic of pertussis in Tianjin municipal. Chinese Journal of Vaccines and Immunization 2011; 17: 212–215. [Google Scholar]
- 6.Huang HT, et al. Surveillance and analysis the immunity status and risk factors of pertussis in Tianjin municipal in 2009. Chinese Journal of Vaccines and Immunization 2010; 16: 536–540. [Google Scholar]
- 7.Schmidtke AJ, et al. Population diversity among Bordetella pertussis isolates, United States, 1935–2009. Emerging Infectious Diseases 2012; 18: 1248–1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kamiya H, et al. Transmission of Bordetella holmesii during pertussis outbreak, Japan. Emerging Infectious Diseases 2012; 18: 1166–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Octavia S, et al. Newly emerging clones of Bordetella pertussis carrying prn2 and ptxP3 alleles implicated in Australian pertussis epidemic in 2008–2010. Journal of Infectious Diseases 2012; 205: 1220–1224. [DOI] [PubMed] [Google Scholar]
- 10.Choe YJ, et al. National pertussis surveillance in South Korea 1955–2011: epidemiological and clinical trends. International Journal of Infectious Diseases 2012; 16: e850–854. [DOI] [PubMed] [Google Scholar]
- 11.Zarei S, et al. Immunogenicity of a triple diphtheria-tetanus-whole cell pertussis vaccine in Iranian preschool children. Iranian Journal of Immunology 2007; 4: 101–109. [DOI] [PubMed] [Google Scholar]
- 12.Wang CQ, et al. Seroprevalence of Bordetella pertussis antibody in children and Adolescents in China. Pediatric Infectious Disease Journal 2011; 30: 593–596. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Q, et al. The seroepidemiology of immunoglobulin G antibodies against pertussis toxin in China: a cross sectional study. BMC Infectious Diseases 2012; 12: 138–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang Y, et al. Incidence surveillance of pertussis based on community and analysis of its transmitted features in Tianjin. Chinese Journal of Vaccines and Immunization 2011; 17: 209–211. [Google Scholar]
- 15.He Q, et al. Comparison of polymerase chain reaction with culture and enzyme immunoassay for diagnosis of pertussis. Journal of Clinical Microbiology 1993; 31: 642–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu Y, et al. Molecular epidemiologic analysis on confirmed pertussis cases. Chinese Journal of Public Health 2011; 27: 987–989. [Google Scholar]
- 17.World Health Organization. Vaccines and Biologicals. Laboratory Manual for the Diagnosis of Whooping Cough Caused by Bordetella pertussis/Bordetella parapertussis. Geneva: Switzerland, revised March 2007.
- 18.Sheridan SL, et al. Unexpectedly limited durability of immunity following acellular pertussis vaccination in preadolescents in a North American outbreak. Clinical Infectious Diseases 2012; 55: 1435–1436. [DOI] [PubMed] [Google Scholar]
- 19.Cherry JD. The epidemiology of pertussis: a comparison of the epidemiology of the disease pertussis with the epidemiology of Bordetella pertussis infection. Pediatrics 2005; 115: 1422–1427. [DOI] [PubMed] [Google Scholar]
- 20.Diez-Domingo J, et al. Incidence of pertussis in persons < or=15 years of age in Valencia, Spain: seroprevalence of antibodies to pertussis toxin (PT) in children, adolescents and adults. Journal of Infection 2004; 49: 242–247. [DOI] [PubMed] [Google Scholar]
- 21.Cherry JD 1, et al. Clinical definitions of pertussis: summary of a Global Pertussis Initiative Roundtable Meeting, February 2011. Clinical Infectious Diseases 2012; 54: 1756–1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tanaka M, et al. Trends in pertussis among infants in the United States, 1980–1999. Journal of the American Medical Association 2003; 290: 2968–2975. [DOI] [PubMed] [Google Scholar]
- 23.Bettinger JA, et al. The effect of changing from whole-cell to acellular pertussis vaccine on the epidemiology of hospitalized children with pertussis in Canada. Pediatric Infectious Disease Journal 2007; 26: 31–35. [DOI] [PubMed] [Google Scholar]
- 24.Rohani P, et al. The decline and resurgence of pertussis in the US. Epidemics 2011; 3: 183–188. [DOI] [PubMed] [Google Scholar]
- 25.Pichichero ME. Booster vaccinations: can immunologic memory outpace disease pathogenesis? Pediatrics 2009; 124: 1633–1641. [DOI] [PubMed] [Google Scholar]
- 26.Baptista PN, et al. Source of infection in household transmission of culture-confirmed pertussis in Brazil. Pediatric Infectious Disease Journal 2005; 24: 1027–1028. [DOI] [PubMed] [Google Scholar]
- 27.Wendelboe AM, et al. Transmission of Bordetella pertussis to young infants. Pediatric Infectious Disease Journal 2007; 26: 293–299. [DOI] [PubMed] [Google Scholar]
- 28.Tozzi AE, et al. Diagnosis and management of pertussis. Canadian Medical Association Journal 2005; 172: 509–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Forsyth KD, et al. New pertussis vaccination strategies beyond infancy: recommendations by the global pertussis initiative. Clinical Infectious Diseases 2004; 39: 1802–1809. [DOI] [PubMed] [Google Scholar]
- 30.Schellekens J, et al. Pertussis sources of infection and routes of transmission in the vaccination era. Pediatric Infectious Disease Journal 2005; 24: S19–24. [DOI] [PubMed] [Google Scholar]
- 31.Coudeville L, et al. Adult pertussis vaccination strategies and their impact on pertussis in the United States: evaluation of routine and targeted (cocoon) strategies. Epidemiology and Infection 2008; 136: 604–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang J. Pertussis and pertussis vaccine. Chinese Journal of Applied Clinical Pediatrics 2013; 28: 1530–1535. [Google Scholar]