SUMMARY
Between December 2010 and July 2011, 252 cases of STEC O157 PT8 stx1 + 2 infection were reported in England, Scotland and Wales. This was the largest outbreak of STEC reported in England and the second largest in the UK to date. Eighty cases were hospitalized, with two cases of haemolytic uraemic syndrome and one death reported. Routine investigative data were used to generate a hypothesis but the subsequent case-control study was inconclusive. A second, more detailed, hypothesis generation exercise identified consumption or handling of vegetables as a potential mode of transmission. A second case-control study demonstrated that cases were more likely than controls to live in households whose members handled or prepared leeks bought unwrapped [odds ratio (OR) 40, 95% confidence interval (CI) 2·08-769·4], and potatoes bought in sacks (OR 13·13, 95% CI 1·19-145·3). This appears to be the first outbreak of STEC O157 infection linked to the handling of leeks.
Key words: Epidemiology, foodborne infections, food safety, outbreaks, Shiga-like toxin-producing E. coli
INTRODUCTION
Shiga toxin-producing Escherichia coli (STEC) infections are foodborne zoonoses. STEC infections cause symptoms ranging from mild gastroenteritis to bloody diarrhoea to haemolytic uraemic syndrome (HUS) [1]. In the UK, STEC O157 is the most commonly reported serogroup. From 2006 to 2010, an average of 921 cases of STEC O157 infection was reported annually in England and Wales (E&W) [2]. STEC O157 phage type 8 (PT8) is one of the most common phage types reported in E&W, accounting for 27% of cases in 2010.
Although most cases of STEC O157 infection in the UK are sporadic, outbreaks do occur [3–11]. Most outbreaks reported in the UK are small and nationally distributed outbreaks are rare. In 2005, a national outbreak of STEC O157 PT8 infection carrying the Shiga toxin 1 + 2 genes (stx1 + 2) was associated with handling raw beef, or consuming beef products at home [4].
Foodborne and non-foodborne outbreaks of STEC infection have been reported [3–11]. The low infectious dose of STEC [11] means that secondary spread is common within outbreaks [12–14]. A wide range of foodstuffs have been implicated in outbreaks. Outbreaks associated with beef or dairy products are more common than those linked to contaminated fruits or vegetables [5, 15–17].
In February 2011, an increase in the detection of STEC O157 PT8 stx1 + 2 infections in England was identified by the Health Protection Agency (HPA) [18]. A single molecular profile accounted for the observed excess. Increased reporting was subsequently seen in Scotland and Wales. The outbreak strain was previously uncommon and distinct from the 2005 outbreak strain [19]. Therefore, an epidemiological investigation was initiated to find the cause of the outbreak.
METHODS
Microbiological methods
In the UK, faecal samples from cases of suspected STEC infection or haemolytic uraemic syndrome (HUS) are sent to local laboratories and cultured for the presence of E. coli O157 (http://www.hpa-standardmethods.org.uk/). Presumptive isolates are referred to the HPA Laboratory of Gastrointestinal Pathogens (LGP) or the Scottish E. coli Reference Laboratory (SERL) for confirmation and typing. Where no faecal sample is available, serum samples may be referred for detection of antibodies to E. coli O157 [20]. Strains confirmed as E. coli O157 are phage-typed. The presence of genes encoding stx1 and/or stx2 genes, and in E&W intimin, are determined through real-time PCR [21].
The outbreak strain was STEC O157 PT8 and possessed the genes for stx1, stx2 and intimin. Multi-locus variable number tandem repeat analysis (MLVA) typing was used to differentiate the outbreak strain for cases in E&W [19]. In Scotland the outbreak strain was defined by pulsed-field gel electrophoresis (PFGE). PFGE was performed on a subset of isolates referred to LGP which confirmed that the outbreak strains from Scotland, England and Wales were indistinguishable.
Case ascertainment and descriptive epidemiology
Outbreak cases were defined as UK residents with domestically acquired (i.e. no foreign travel in the 7 days before illness) STEC O157 PT8 stx1 + 2 infection of the outbreak MLVA or PFGE profile with onset of symptoms on or after 1 December 2010 if symptomatic. For asymptomatic cases, the date of confirmation of STEC infection was used in place of the date of onset.
Isolates of the outbreak profile were reported by LGP and SERL to epidemiologists at HPA. Descriptive data for cases in England were collected using the National Enhanced Surveillance System for STEC (NESSS). NESSS combines clinical and epidemiological data collected through the enhanced surveillance questionnaire with microbiological results. Local laboratories report presumptive isolates of STEC to HPA teams, who then arrange for the questionnaire to be administered. Symptomatic contacts of cases and contacts that are deemed to pose a risk of onward transmission are screened, and the case status, i.e. primary, co-primary, secondary or asymptomatic is based on standard definitions (http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/EscherichiaColiO157/Surveillance/).
Exposure questionnaires for Welsh outbreak cases and aggregate data for Scottish outbreak cases were sent to the HPA for collation and analysis to inform the descriptive epidemiology of the outbreak.
Standard case definition for analytical studies
For all analytical studies, cases were defined as domestically acquired (no foreign travel in the 10 days prior to illness) primary symptomatic cases resident in the UK and infected with STEC O157 PT8 stx1 + 2 of the outbreak MLVA or PFGE profile. Cases were limited to domestic, primary symptomatic cases to ensure that the cases had been exposed to the vehicle of transmission. The onset date was also limited to include only recent infections to minimize recall bias. A more rigorous definition of domestically acquired infection was used in the analytical studies than in the descriptive analysis (10 days compared to 7 days).
First hypothesis generation
A case-case analysis of data collected through NESSS was performed to generate hypotheses. Cases were defined according to the analytical studies case definition, although limited to England residents as exposure data was obtained through NESSS, limited to adults because few childhood cases were reported at that time, and expanded to include cases where MLVA profiles were not yet available (probable cases) with onsets in December 2010 or January 2011. Cases meeting the case definition were compared to primary domestic cases of STEC O157 of other phage types with illness onset in the same period. Any confounding effects of age and gender were adjusted for in the analysis.
Twenty-nine cases of STEC PT8 stx1 + 2 infection were compared to 17 cases of infection with other STEC subtypes. There were associations between STEC PT8 stx1 + 2 infection and the consumption of beef [odds ratio (OR) 5·74, 95% confidence interval (CI) 1·35–24·38, P = 0·02] and yoghurt (OR 3·93, 95% CI 1·09–14·2, P = 0·04), plus purchasing products from one particular supermarket chain (OR 4·00, 95% CI 1·05–15·25, P = 0·04). There were no associations between STEC PT8 stx1 + 2 and the consumption of particular branded foods.
First case-control study
In February 2011, an unmatched case-control study was undertaken to examine associations between infection and the consumption of cooked beef, yoghurt or fromage-frais. Fromage-frais was included due to potential misclassification of fromage-frais and yoghurt. Cases and controls were frequency-matched based on residential postcode. Cases were defined according to the analytical studies case definition although limited to adults with onset of symptoms on or after 1 January 2011. Controls were identified through sequential telephone number dialling, starting from each case's number and adding five, allowing frequency-matching of cases and controls based on telephone number area code. Controls aged ⩾18 years, who had not had symptoms of gastrointestinal illness or travelled abroad in the 10 days prior to interview, and who had not had close contact with another individual with gastrointestinal illness were eligible for inclusion in the study. Cases and controls were interviewed by trained HPA or Health Protection Scotland (HPS) specialists using a standardized questionnaire.
Second hypothesis generation
Cases meeting the analytical studies case definition with onset of symptoms on or after 1 December 2010 were selected as part of a trawl. Selected cases were interviewed in their homes by experienced interviewers using a detailed questionnaire. Exposure histories for a wide range of foods, behaviours, and other factors were collected through the use of multi-tiered closed-option questions and open-ended history taking (see Supplementary material).
Thirteen cases were interviewed. The following generic foods were commonly consumed: milk (92%), cheese (85%), and biscuits (77%). However, no common products, brands or outlets were identified. The frequency of handling and preparing raw potatoes (77%), raw carrots (69%), raw onions (62%) and other raw vegetables (69%) in domestic kitchens was considered higher than expected, based on review of data from other national outbreak investigations and expert opinion.
Second case-control study
In May 2011, a case-control study was undertaken to examine associations between infection and the consumption and/or handling of potentially soil-bearing vegetables. Questions on exposures associated with infection in the first study were included as were questions on beef consumption. Cases and controls were defined according to the analytical studies case definition with onset dates on or after 1 April 2011. Controls were defined according to the first case-control study and were frequency-matched to cases on region of residence. Controls were selected from volunteers in local or national health protection offices, and their relatives.
Statistical analysis
The occupation and deprivation status of cases was classified using national data sources [22–25]. The case-case study in the first hypothesis generation was analysed using logistic regression in Stata v. 12 (StataCorp., USA). Stata was used to analyse both case-control studies. Logistic regression was used to estimate crude odds ratios, only adjusting for age and gender. Exact logistic regression was used where cells contained zero values. In the first case-control study, exposures with an estimated OR >1 and P ⩽ 0·3 were included in multivariable logistic regression analyses. In the second case-control study a cut-off value of P = 0·2 was used. In multivariable analyses, exposures that provided no evidence of any association with infection, or provided evidence suggesting a protective effect, were excluded sequentially until all exposures in the regression models provided evidence of a positive association. Age group (<21, 10-year age groups up to 60, and >60 years) and sex were retained in the final multivariable models. In the first case-control study, two exposures pertaining to the hypothesized causal exposure to beef were also always retained in the regression model.
RESULTS
Descriptive epidemiology
The outbreak began in December 2010 and was declared over on 2 August 2011. During this period, 252 domestic cases infected with the outbreak strain of STEC O157 PT8 stx1 + 2 were confirmed. A further six cases with the outbreak strain were excluded from the outbreak analysis because of their travel/residence histories. An alert was sent to other countries through the European Centre for Disease Control and Prevention Epidemic Intelligence Information System (EPIS) in February 2011. No cases of the outbreak strain were reported outside the UK.
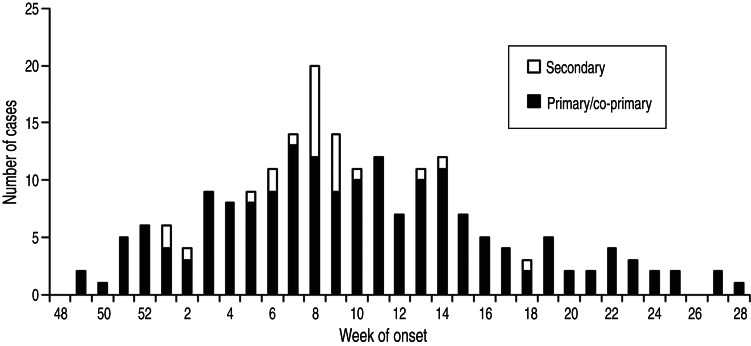
The last known onset of an outbreak case was on 4 July 2011. The epidemic curves for cases in all countries showed the weekly incidence peaking during week 8 of 2011 (Fig. 1). The majority of cases were primary (n = 192), 25 were secondary and 14 were asymptomatic. The status of 21 cases remains uncertain. Eighty cases were hospitalized, and there were two reported HUS cases. One death was reported, an elderly male with underlying illness but not HUS.
Fig. 1.
Epidemic curve – primary and secondary domestic cases of STEC O157 PT8 stx1 + 2 with the outbreak profile reported (n = 204).
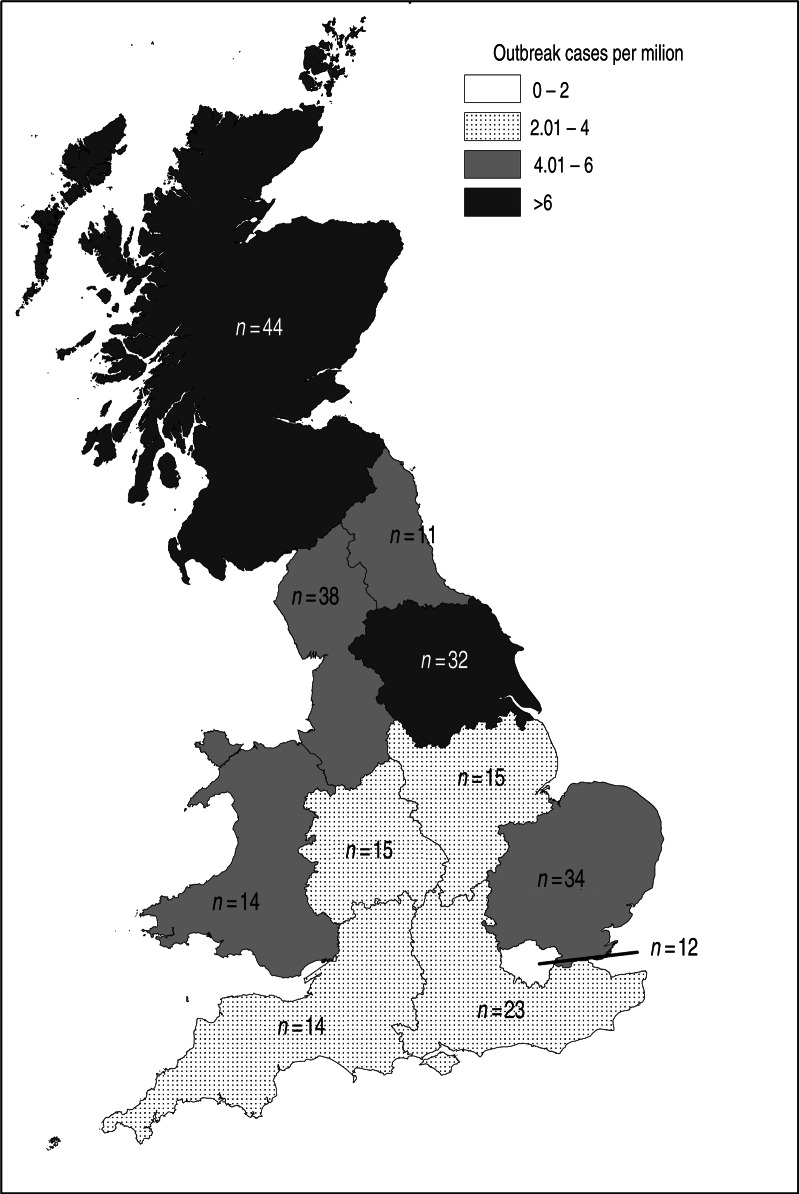
The highest rates of infection were reported from Scotland (8·47 cases/million) and Yorkshire & Humberside (6·09 cases/million). No cases were reported in Northern Ireland (Fig. 2).
Fig. 2.
Map of outbreak cases per million residents for the regions of England, Scotland and Wales.
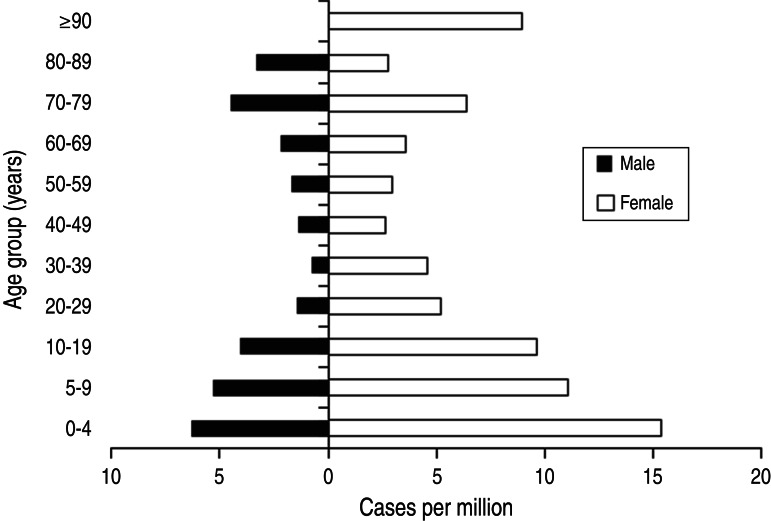
Seventy percent of cases were female and 60% were aged >16 years (Fig. 3). A higher proportion of cases of the outbreak profile were female (70% vs. 55%, χ2 test, P < 0·001), and fewer were children aged <5 years (15% vs. 24%, χ2 test, P = 0·008) compared to non-outbreak cases reported to NESSS in the same period. Of the 195 cases for which a surveillance questionnaire was completed, only six (3%) reported belonging to ethnic minorities. There was no statistically significant association between deprivation and illness.
Fig. 3.
Age and gender distribution per million population.
First case-control study
Twenty-five cases and 49 controls were included in the first case-control study. Females predominated in both cases (68%) and controls (69%, χ2 test, P = 0·9). Controls were older than cases (Fisher's exact test, P = 0·02); the median age of cases was 43 years, compared to 63 years in controls. Cases included in the case-control study had a similar gender (χ2 test, P = 0·83) and age (Fisher's exact test, P = 0·08) profile as outbreak cases not included in the case-control study, although children were not included in the analysis.
Following single variable analysis, 18 exposures met the inclusion criteria for multivariable analysis. No associations between infection and consumption of beef (P = 0·45) or burgers (P = 0·78) were identified (Table 1). An association between infection and purchasing food from one particular supermarket (OR 91·77, P = 0·007) accounted for only 12% of cases and involved a different supermarket chain from that identified during hypothesis generation. Consumption of both cream (OR 93·14, P = 0·002) and fromage-frais (OR 152·29, P = 0·008) in the home were associated with infection. Cases reported consuming various brands and types of cream and fromage-frais, purchased from many retailers. Further investigations found that the reported brands were manufactured at different processing plants using ingredients sourced from different locations. All had received sufficient heat treatment to destroy STEC O157.
Table 1.
First case-control study results: exposures in the final multivariable logistic regression analysis, adjusted for age group and gender
| Exposure | % cases exposed | % controls exposed | OR | 95% CI | P value |
|---|---|---|---|---|---|
| Cat (contact with) | 24 | 6 | 14·26 | 1·33–152·2 | 0·03 |
| Other venue | 20 | 10 | 23·96 | 1·93–297·5 | 0·01 |
| Beef (outside home) | 28 | 12 | 2·45 | 0·24–24·89 | 0·45 |
| Burgers (outside home) | 12 | 2 | 4·41 | 0·00–136 600 | 0·78 |
| Fromage-frais (home) | 8 | 2 | 152·29 | 3·81–6092 | 0·008 |
| Cream (home) | 28 | 6 | 93·14 | 5·29–1640 | 0·002 |
| Supermarket 1 | 40 | 14 | 8·33 | 0·83–83·74 | 0·07 |
| Supermarket 2 | 12 | 4 | 91·77 | 3·35–2511 | 0·007 |
OR, Odds ratio; CI, confidence interval.
Twenty-five cases and 49 controls were included in the model.
Second analytical study
The second case-control study included 30 cases and 62 controls. Cases and controls had similar age distributions (Fisher's exact test, P = 0·6); the median age was 41·5 years in cases, and 43·5 years in controls. Gender distribution was similar in cases and controls (63% of cases female, 61% of controls; χ2 test, P = 0·8). No difference in occupation (χ2 test for trends, P = 0·08) or deprivation status (χ2 test for trends, P = 0·6) was found between cases and controls. Those included in the case-control study had a similar age (Fisher's exact test, P = 0·13) and gender (χ2 test, P = 0·4) profile as other outbreak cases.
Single variable analysis showed no associations between infection and the consumption of cream, yoghurt or fromage-frais. A total of 31 exposures met the criteria for inclusion in the multivariable analysis; however, many of these variables pertained to exposure to the same food in different situations. These exposures were grouped and a total of 14 exposures were considered in multivariable analysis (Table 2). The ‘bagged vegetables' (OR 3·37, P = 0·08) and ‘other beef’ (OR 2·29, P = 0·2) variables were excluded as these variables included many products.
Table 2.
Second case-control study results: exposures with an odds ratio >1 and a P value <0·2 in single variable analysis, adjusted for age group and gender
| Exposure | Case | Control | OR | 95% CI | P value | Considered in MVA | ||
|---|---|---|---|---|---|---|---|---|
| Exposed | Unexposed | Exposed | Unexposed | |||||
| Food preparation (handled or cooked within household) | ||||||||
| Burger | 7 | 23 | 7 | 55 | 3·57 | 1·01–12·67 | 0·05 | Y |
| Other beef | 6 | 24 | 6 | 56 | 2·29 | 0·62–8·48 | 0·2 | N |
| Chicken outside the home | 5 | 25 | 3 | 59 | 3·91 | 0·81–18·81 | 0·09 | Y |
| Potatoes bought in sacks* | 6 | 3 | 8·36 | 0·97–71·82 | 0·05 | Y | ||
| Raw celery | 11 | 19 | 13 | 49 | 1·95 | 0·72–5·31 | 0·19 | Y |
| Celery bagged* | 10 | 11 | 2·15 | 0·76–6·09 | 0·15 | N | ||
| Raw leeks | 9 | 21 | 4 | 58 | 7·44 | 1·90–29·11 | 0·004 | N |
| Organic leeks*† | 2 | 0 | 6·18 | 0·47–∞ | 0·16 | N | ||
| Leeks bagged* | 4 | 3 | 3·15 | 0·59–16·87 | 0·18 | N | ||
| Leeks unwrapped* | 5 | 1 | 33·16 | 2·35–467·5 | 0·009 | Y | ||
| Handle raw leeks* | 6 | 1 | 35·34 | 2·63–475·0 | 0·007 | N | ||
| Handle leek packaging* | 4 | 4 | 2·89 | 0·61–13·73 | 0·18 | N | ||
| Swedes | 6 | 24 | 4 | 56 | 3·08 | 0·73–13·01 | 0·13 | N |
| Turnips | 6 | 24 | 3 | 57 | 4·55 | 0·95–21·86 | 0·06 | N |
| Bagged other vegetables* | 7 | 5 | 3·37 | 0·86–13·21 | 0·08 | N | ||
| Eat sponge cake | 9 | 21 | 9 | 53 | 2·93 | 0·90–9·52 | 0·07 | Y |
| Eat raw cake mixture* | 4 | 4 | 2·97 | 0·57–15·46 | 0·20 | N | ||
| Eaten in the last 5 days | ||||||||
| Potato cooked in oven | 12 | 17 | 15 | 35 | 2·00 | 0·68–5·86 | 0·2 | N |
| Cooked leeks (any) | 8 | 22 | 3 | 59 | 9·11 | 1·98–41·80 | 0·004 | N |
| Cooked leeks (home) | 8 | 22 | 3 | 59 | 9·11 | 1·98–41·80 | 0·004 | N |
| Cooked turnip (any) | 7 | 23 | 4 | 58 | 4·87 | 1·13–20·99 | 0·03 | N |
| Cooked turnip (home) | 7 | 23 | 4 | 58 | 4·87 | 1·13–20·99 | 0·03 | N |
| Cream (home) | 9 | 21 | 11 | 51 | 1·97 | 0·67–5·76 | 0·2 | Y |
| Shops | ||||||||
| Butcher's shop | 12 | 18 | 14 | 48 | 2·76 | 0·99–7·67 | 0·05 | Y |
| Corner shop | 7 | 23 | 9 | 53 | 2·23 | 0·69–7·17 | 0·18 | Y |
| Other shop | 7 | 23 | 7 | 55 | 3·89 | 1·02–14·76 | 0·05 | Y |
| Vegetable box† | 2 | 28 | 0 | 62 | 4·95 | 0·38–∞ | 0·2 | Y |
| Combined exposures | ||||||||
| Beef cooked at home | 23 | 7 | 42 | 20 | 1·86 | 0·65–5·34 | 0·2 | N |
| Exposure to raw leek | 10 | 20 | 4 | 58 | 7·88 | 2·08–29·90 | 0·002 | Y |
| Exposure to raw swede | 8 | 22 | 5 | 57 | 4·11 | 1·05–16·09 | 0·04 | Y |
| Exposure to raw turnip | 8 | 22 | 4 | 58 | 5·79 | 1·42–23·54 | 0·01 | Y |
OR, Odds ratio; CI, confidence interval; MVA, multivariable analysis.
Estimates obtained using exact logistic regression due to zero cells.
Compared to no exposure to that food item.
The multivariable logistic regression model (Table 3) showed an association between illness and chicken consumed outside the home (OR 13·07, P = 0·01). This exposure was reported by five cases (16·7%). There was a weak association between infection and exposure to raw turnips in the home (OR 5·1, P = 0·07) which was reported by eight cases (26·7%).
Table 3.
Second case-control study results: exposures in the final multivariable logistic regression analysis, adjusted for age group and gender
| Exposure | OR | 95% CI | P value |
|---|---|---|---|
| Chicken outside the home | 13·07 | 1·68–101·5 | 0·01 |
| No potatoes | Ref. | ||
| Not bought in sack | 0·90 | 0·16–5·26 | 0·9 |
| Bought in sack | 13·13 | 1·19–145·3 | 0·04 |
| Any raw leek at home | 6·25 | 1·33–29·28 | 0·02 |
| Any raw turnip at home | 5·10 | 0·86–30·24 | 0·07 |
Twenty-eight cases and 59 controls were included in the model.
Potatoes bought in sacks (OR 13·13, P = 0·04) and exposure to any raw leeks in the home (OR 6·25, P = 0·02) were both associated with infection. When exposure to any raw leeks was replaced in the regression model by exposure to leeks bought unwrapped (unwrapped leeks) the estimated odds ratios of the other exposures in the model remained similar, but the estimated odds ratio for unwrapped leeks rose to 40 (P = 0·01) (Table 4). Ten cases (33%) were exposed to raw leeks in the home, of which half were unwrapped. Twenty-eight cases (93%) were exposed to raw potatoes, six of whom bought potatoes in sacks. In total, 14 cases (47%) were directly exposed to either any leeks or potatoes bought in sacks.
Table 4.
Second case-control study results: exposures in the final multivariable logistic regression analysis including leeks bought unwrapped in place of any raw leeks, adjusted for age group and gender
| Exposure | OR | 95% CI | P value |
|---|---|---|---|
| Chicken (outside home) | 16·02 | 1·98–129·3 | 0·009 |
| No potatoes | Ref | ||
| Not bought in sack | 0·79 | 0·13–4·77 | 0·8 |
| Bought in sack | 11·98 | 1·02–140·9 | 0·05 |
| No leeks | Ref. | ||
| Leeks not bought unwrapped | 1·04 | 0·11–9·51 | >0·9 |
| Leeks bought unwrapped | 40·00 | 2·08–769·4 | 0·01 |
| Any raw turnip in home | 5·43 | 0·87–33·75 | 0·07 |
OR, Odds ratio; CI, confidence interval.
Twenty-eight cases and 59 controls were included in the model.
DISCUSSION
This outbreak of STEC O157 PT8 stx1 + 2 infection was the largest reported in England to date, and the second largest in the UK. The outbreak had a major impact. Eighty people were admitted to hospital, two with HUS and one person died. However, the proportion of cases that went on to develop HUS or other extra-intestinal symptoms was low compared to previous large outbreaks of STEC O157 infection where 6–22% of cases reported HUS [17, 26–29]. An epidemiological study of childhood HUS in the UK and Republic of Ireland [1] found that STEC O157 PT8 infection was less likely to be associated with HUS than PT21/28 or PT2.
Two hypothesis-generating, and two analytical investigations were required before we could identify a robust association between infection with the outbreak STEC strain, and exposure to any vehicle. The second case-control study demonstrated associations between infection and living in a household where leeks (particularly unwrapped) and/or potatoes purchased in sacks were handled or prepared in the domestic kitchen in the 5 days before the onset of symptoms. These findings are consistent with the unfolding epidemiology of the outbreak, the natural history of STEC O157 and the growing and consumption of leeks and potatoes.
Soil contamination as a potential source of infection
Both leeks and potatoes were implicated in this outbreak. While leeks and potatoes purchased in supermarkets are often packaged and washed before purchase, they often carry residual soil. Previous investigations of outbreaks of STEC [15] and Salmonella enterica [16, 30] infection have shown that growing crops can be exposed to pathogens from environmental sources and that apparently clean washed produce can transmit infection. Previous investigations have shown that standing fruit, vegetables (including potatoes) and soil can become contaminated with STEC O157 through the application of contaminated irrigation/run-off water or manure, or wildlife gaining access to crops [15, 30–32]. STEC O157 can survive in soil or crops for periods of months [33] if they became contaminated in the field, or during processing, storage or distribution.
The second case-control study identified unwrapped leeks and potatoes bought in sacks as the strongest risk factors for infection with the outbreak STEC strain. These vegetables may have more soil contamination than those bought wrapped. As they are handled directly without packaging from the point of purchase onwards, there is an increased risk of exposure for anyone handling them.
The role of the domestic food handler
The second case-control study found that the handling rather than consumption of leeks and potatoes was associated with illness. A 2010 survey of 3163 adults in the UK found that women did more food shopping than men (87% vs. 59%), and more food preparation for themselves (71% vs. 42%) and other people (56% vs. 17%) [34]. This might explain the excess of female cases affected in this outbreak.
If leeks or potatoes are contaminated with STEC, there is risk of exposure when handling these vegetables either at point of purchase or in domestic settings. The low infectious dose of STEC O157 [11] exacerbates risk from environmental transmission [35] and cross-contamination [36], increasing the likelihood that those handling food will be infected through contact with contaminated leeks or potatoes, or with other foods or surfaces that had been cross-contaminated. Those consuming leeks and potatoes, but not handling them raw are likely to be at lower risk of infection as these vegetables are seldom eaten raw and cooking should eliminate STEC. Ready-to-eat foods stored in the home can be directly or indirectly cross-contaminated with STEC from contaminated leeks or potatoes. Consumption of such foods presents a risk to all household members.
Spatial and temporal distribution of cases
The absence of cases outside the UK suggests the vehicle may have been a domestic product which was not exported. Approximately 70–75% of leeks, and most potatoes sold in the UK, are grown domestically [Food Standards Agency (FSA), 2011, written communication]. Cases of the outbreak profile were reported from Scotland, England and Wales. Most leeks and potatoes on sale in Northern Ireland are produced locally, perhaps explaining the absence of cases in this part of the UK (FSA, 2011, written communication).
While leeks and potatoes produced in the UK are distributed nationally, individual producers often supply to a relatively well defined geographical zone. A distinct regional distribution of cases was observed, with cases concentrated in Northern England and Scotland, suggesting that the source of contaminated vegetables was a producer or several producers supplying these areas. The outbreak profile (MLVA and PFGE) was not circulating widely in humans in the UK prior to the outbreak [19], suggesting that contamination is likely to have originated from a single location.
The rate at which cases emerged when taken alongside the geographical distribution suggests that the outbreak was likely to be associated with a vehicle of infection with low-level intermittent contamination. The prolonged nature of the outbreak suggests a continuing source of contamination, e.g. contaminated soil. Case numbers reduced markedly from mid-May 2011, coinciding with the end of the UK growing season for leeks. Leeks are harvested, distributed and sold without extended storage (FSA, 2011, written communication).
Methodological considerations
In the first study, fromage-frais and cream were significantly associated with illness. However, the number of cases reporting exposure was small and products were produced by a range of manufacturers and retailers. Since further investigation showed these products did not share ingredients, or distribution channels, these were not considered plausible vehicles of infection. It is thought the demonstrated association was due to confounding.
The hypothesis generation performed in the first study was based on data collected through NESSS in England. While routine surveillance data have been used successfully in the past to identify vehicles of infection in foodborne outbreaks [37], in this study it proved unsuccessful. Enhanced surveillance questionnaires cannot be used to collect complete exposure histories. Questionnaire length must be balanced against work-load constraints. While enhanced surveillance systems offer an efficient method of generating hypotheses in some situations, they are unlikely to identify unusual exposures. The NESSS questionnaire does not include questions on exposure to leeks or potatoes because these are unusual vehicles of infection for STEC. Therefore neither vegetable was identified as a potential vehicle during the initial hypothesis generation.
The second hypothesis-generation phase sought a more detailed food exposure history and was successful in identifying the exposures that potentially explained how the outbreak strain was transmitted. We designed, to our knowledge, the most comprehensive trawling questionnaire ever used in England for a national foodborne outbreak investigation (see Supplementary material). The subsequent case-control study utilized members of staff and their family members as controls. This novel technique reduced the number of non-responders and increased the speed at which the investigation could be completed. However, there are limitations to this approach. While the HPA is a large and diverse organization, and cases and controls were similar in respect to age, gender, occupational status and deprivation, the staff might not be representative of the general population and this might introduce bias. Using staff of the investigating agency also risks the control population being aware of the hypothesis. However, no members of the investigating team, departments involved in the outbreak or senior management were used as controls and details of the hypothesis or findings of the first case-control study were not known across the HPA.
While only one third of cases reported handling or consuming leeks in the second case-control study, this was significantly higher than controls. The case-control questionnaire collected data on exposures in the 5 days prior to illness; however, both leeks and potatoes can be stored in the home for longer than this period. Given the low infectious dose of STEC [11], and the ability for it to remain viable in kitchen settings for much longer than 5 days [38, 39], it may be that cross-contamination to other foods or food contact surfaces in the home, and the presence of residual contamination after the leeks or potatoes had been used, accounted for the low number of cases reporting handling leeks in the 5 days prior to illness.
The significance of potatoes as a vehicle of infection is hard to determine, as this product is eaten by most of the British public (FSA, 2011, written communication). However, the significant association with potatoes bought in sacks does lend strength to the hypothesis that soil contamination on vegetables was the source of the outbreak. An association was also identified with chicken consumed outside the home, although no commonality of exposures could be identified.
Data from the epidemiological investigations were supplied in full to the appropriate regulatory agencies. Discussions were held with growers' associations and retailers. The outbreak control team was subsequently advised that production data were commercially sensitive and could not be shared or promulgated. As such it was not possible to conduct environmental investigations which might have provided supportive microbiological evidence. Discussions have since been held between stakeholder organizations to identify improvements which would allow root cause investigations to be conducted effectively. As a consequence improvements in trace-back investigations have since been implemented. These have been used successfully in more recent investigations [40–42].
CONCLUSIONS
Our investigations were successful in demonstrating an association between STEC O157 PT8 stx1 + 2 infection and handling leeks and potatoes. While potatoes have been implicated in an outbreak previously [31], as far as we know this is the first time that an outbreak of STEC O157 infection has been linked to handling leeks. Although there are unanswered questions in terms of the exact point of contamination of both leeks and potatoes, from our investigations leeks and potatoes appear to be biologically plausible vehicles of infection in this outbreak with a strong epidemiological link to illness in cases.
Our ultimate findings demonstrate the wisdom of adopting an open-minded approach to the investigation of outbreaks of STEC infection. As was highlighted by the large outbreak of STEC O104 infection in Germany linked to sprouted fenugreek seeds [17], novel vehicles of transmission continue to emerge and will probably do so in the future. In light of this we need to recognize that the safest approach to take is to obtain wide-ranging detailed histories from selected cases to generate hypotheses around which the development of analytical epidemiological, microbiological or trace-back investigations can be designed. It is also essential to take a step-wise approach to investigation and to continuously review findings. It is always worthwhile considering how to identify indirect transmission of pathogens and vehicles of transmission that might be less visible to cases.
ACKNOWLEDGEMENTS
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
SUPPLEMENTARY MATERIAL
For supplementary material accompanying this paper visit http://doi.org/10.1017/S0950268815001016.
click here to view supplementary material
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Lynn RM, et al. Childhood hemolytic uremic syndrome, United Kingdom and Ireland. Emerging Infectious Diseases 2005; 11: 590–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Health Protection Agency. E. coli O157 annual totals, May 2012 (http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1249113624846).
- 3.Ihekweazu C, et al. Large outbreak of verocytotoxin-producing Escherichia coli O157 infection in visitors to a petting farm in South East England, 2009. Epidemiology & Infection 2012; 140: 1400–1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Health Protection Agency. National increase in Vero-cytotoxin-producing Escherichia coli O157 (VTEC O157) PT8 – case control study. Communicable Disease Report. CDR Weekly 2006; 16.
- 5.Whittaker PJ, et al. A national outbreak of verotoxin-producing Escherichia coli O157 associated with consumption of lemon-and-coriander chicken wraps from a supermarket chain. Epidemiology & Infection 2009; 137: 375–382. [DOI] [PubMed] [Google Scholar]
- 6.Stirling A, et al. An outbreak of Escherichia coli O157 phage type 2 infection in Paisley, Scotland. Eurosurveillance 2007; 12: E070823. [DOI] [PubMed] [Google Scholar]
- 7.Verma A, et al. An outbreak of E. coli O157 associated with a swimming pool: an unusual vehicle of transmission. Epidemiology & Infection 2007; 135: 989–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salmon R. Outbreak of verotoxin producing E. coli O157 infections involving over forty schools in south Wales, September 2005. Eurosurveillance 2005; 10: E051006. [DOI] [PubMed] [Google Scholar]
- 9.Health Protection Agency. Foodborne outbreaks epidemiological data, May 2011 (http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/FoodborneOutbreakSurveillanceAndRiskAssessment/FoodborneOutbreaks/).
- 10.Health Protection Agency. Non-foodborne outbreaks epidemiological data, May 2011 (http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1249113624846).
- 11.Willshaw GA, et al. Vero cytotoxin-producing Escherichia coli O157 in beefburgers linked to an outbreak of diarrhoea, haemorrhagic colitis and haemolytic uraemic syndrome in Britain. Letters in Applied Microbiology 1994; 19: 304–307. [DOI] [PubMed] [Google Scholar]
- 12.Snedeker KG, et al. Primary and secondary cases in Escherichia coli O157 outbreaks: a statistical analysis. BMC Infectious Diseases 2009; 9: 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parry SM, Salmon RL. Sporadic STEC O157 infection: secondary household transmission in Wales. Emerging Infectious Diseases 1998; 4: 657–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Werber D, et al. Preventing household transmission of Shiga toxin-producing Escherichia coli O157 infection: promptly separating siblings might be the key. Clinical Infectious Diseases 2008; 46: 1189–1196. [DOI] [PubMed] [Google Scholar]
- 15.Wendel AM, et al. Multistate outbreak of Escherichia coli O157:H7 infection associated with consumption of packaged spinach, August-September 2006: the Wisconsin investigation. Clinical Infectious Diseases 2009; 48: 1079–1086. [DOI] [PubMed] [Google Scholar]
- 16.Berger CN, et al. Fresh fruit and vegetables as vehicles for the transmission of human pathogens. Environmental Microbiology 2010; 12: 2385–2397. [DOI] [PubMed] [Google Scholar]
- 17.Frank C, et al. Epidemic profile of Shiga-toxin-producing Escherichia coli O104:H4 outbreak in Germany. New England Journal of Medicine 2011; 365: 1771–1780. [DOI] [PubMed] [Google Scholar]
- 18.Farrington CP, et al. A statistical algorithm for the early detection of outbreaks of infectious disease. Journal of the Royal Statistical Society, Series A 1996; 159: 547–563. [Google Scholar]
- 19.Perry N, et al. Application of multilocus variable number tandem repeat analysis to monitor Verocytotoxin-producing Escherichia coli O157 phage type 8 in England and Wales: emergence of a profile associated with a national outbreak. Journal of Applied Microbiology 2013; 115: 1052–1058. [DOI] [PubMed] [Google Scholar]
- 20.Chart H, et al. Analysis of saliva for antibodies to the LPS of Escherichia coli O157 in patients with serum antibodies to E. coli O157 LPS. Journal of Medical Microbiology 2003; 52: 569–572. [DOI] [PubMed] [Google Scholar]
- 21.Jenkins C, et al. Assessment of a real-time PCR for the detection and characterization of verocytotoxigenic Escherichia coli. Journal of Medical Microbiology 2012; 61: 1082–1085. [DOI] [PubMed] [Google Scholar]
- 22.Office for National Statistics. The National Statistics Socio-economic classification. 2010.
- 23.Scottish Government National Statistics. Scottish index of multiple deprivation. 2009.
- 24.Department of Communities and Local Government. English indices of deprivation 2010. Department of Communities and Local Government 2010 (https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/6871/1871208.pdf).
- 25.Welsh Government Statistical Directorate. Welsh index of multiple deprivation. 2011.
- 26.Cowden JM, et al. Epidemiological investigation of the central Scotland outbreak of Escherichia coli O157 infection, November to December 1996. Epidemiology & Infection 2001; 126: 335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Welsh Assembly Government. The public inquiry into the September 2005 outbreak of E. coli O157 in South Wales. Queen's Printer and Controller of HMSO, 2009.
- 28.Health Protection Agency Independent Investigation Committee. Review of the major outbreak of E. coli O157 in Surrey, 2009. Health Protection Agency, 2010.
- 29.Dundas S, et al. The central Scotland Escherichia coli O157:H7 outbreak: risk factors for the hemolytic uremic syndrome and death among hospitalized patients. Clinical Infectious Diseases 2001; 33: 923–931. [DOI] [PubMed] [Google Scholar]
- 30.Horby PW, et al. A national outbreak of multi-resistant Salmonella enterica serovar Typhimurium definitive phage type (DT) 104 associated with consumption of lettuce. Epidemiology & Infection 2003; 130: 169–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morgan GM, et al. First recognized community outbreak of haemorrhagic colitis due to verotoxin-producing Escherichia coli O157.H7 in the UK. Epidemiology & Infection 1988; 101: 83–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laidler MR, et al. Escherichia coli O157:H7 infections associated with consumption of locally grown strawberries contaminated by deer. Clinical Infectious Diseases 2013; 57: 1129–1134. [DOI] [PubMed] [Google Scholar]
- 33.Fremaux B, Prigent-Combaret C, Vernozy-Rozand C. Long-term survival of Shiga toxin-producing Escherichia coli in cattle effluents and environment: an updated review. Veterinary Microbiology 2008; 132: 1–18. [DOI] [PubMed] [Google Scholar]
- 34.Food Standards Agency. Exploring food attitudes and behaviours in the UK: findings from the Food and You Survey, 2010. 2011.
- 35.Strachan NJ, et al. Escherichia coli O157: burger bug or environmental pathogen? International Journal of Food Microbiology 2006; 112: 129–137. [DOI] [PubMed] [Google Scholar]
- 36.Pennington TH. Report on the circumstances leading to the 1996 outbreak of infection with E. coli O157 in Central Scotland, the implications for food safety and the lessons learned. The Stationery Office, 1997.
- 37.CDC. Multistate outbreak of listeriosis associated with Jensen Farms cantaloupe – United States, August–September 2011. Morbidity and Mortality Weekly Report 2011; 60: 1357–1358. [PubMed] [Google Scholar]
- 38.Maule A. Survival of verocytotoxigenic Escherichia coli O157 in soil, water and on surfaces. Symposium Series. Society for Applied Microbiology 2000; 71: 78S. [DOI] [PubMed] [Google Scholar]
- 39.Chauret C. Survival and control of Escherichia coli O157:H7 in foods, beverages, soil and water. Virulence 2011; 2: 593–601. [DOI] [PubMed] [Google Scholar]
- 40.Inns T, et al. Outbreak of Salmonella enterica Goldcoast infection associated with whelk consumption, England, June to October 2013. Eurosurveillance 2013; 18. [DOI] [PubMed] [Google Scholar]
- 41.Launders N, et al. Outbreak of Shiga toxin-producing E. coli O157 associated with consumption of watercress, United Kingdom, August to September 2013. Eurosurveillance 2013; 18. [DOI] [PubMed] [Google Scholar]
- 42.Byrne L. A multi-country outbreak of Salmonella Newport gastroenteritis in Europe associated with watermelon from Brazil, confirmed by whole genome sequencing: October 2011–January 2012. Eurosurveillance 2014; [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://doi.org/10.1017/S0950268815001016.
click here to view supplementary material