SUMMARY
Human anthrax cases reported in the country of Georgia increased 75% from 2011 (n = 81) to 2012 (n = 142). This increase prompted a case-control investigation using 67 culture- or PCR-confirmed cases and 134 controls matched by residence and gender to investigate risk factor(s) for infection during the month before case onset. Independent predictors most strongly associated with disease in the multivariable modelling were slaughtering animals [odds ratio (OR) 7·3, 95% confidence interval (CI) 2·9–18·1, P < 0·001] and disposing of dead animals (OR 13·6, 95% CI 1·5–119·8, P = 0·02). Participants owning or working with livestock (n = 131) were additionally interviewed about livestock management practices during the previous 6 months: 53 (44%) of 121 respondents vaccinated livestock against anthrax; 19 (16%) of 116 moved livestock >1 km; 15 (12%) of 125 had sick livestock; and 11 (9%) of 128 respondents reported finding dead livestock. We recommend joint public health and veterinary anthrax case investigations to identify areas of increased risk for livestock anthrax outbreaks, annual anthrax vaccination of livestock in those areas, and public awareness education.
Key words: Anthrax, bacterial infections, control, epidemiology, zoonoses
INTRODUCTION
Anthrax is a zoonosis caused by the Gram-positive spore-forming bacteria Bacillus anthracis. The spores can remain viable in soil for decades, contributing to disease persistence [1]. Anthrax primarily occurs in herbivorous wildlife and livestock that ingest B. anthracis spores while grazing [2]. Biting flies and blowflies may serve as mechanical vectors [3, 4]. Human anthrax is primarily dependent on exposure to infected animals, their carcasses, or to products from infected animals (e.g. meat, wool, hides) [5]. Three primary forms of anthrax are recognized in humans: cutaneous, gastrointestinal, and inhalation. Of these, cutaneous anthrax is the most common, comprising 95–99% [5, 6] of an estimated 2000–20 000 human anthrax cases occurring annually worldwide [7]. Anthrax is endemic in Central and Southwestern Asia, Southern and Eastern Europe, and West Africa [8]. Outbreaks frequently occur during hot, dry conditions following heavy rains and flooding, or following rains ending a period of drought [2, 9, 10]. Control of anthrax primarily depends on vaccination of susceptible livestock; surveillance, rapid identification, and treatment of affected animals; quarantine of impacted premises; prevention of animal access to contaminated pastures or feed; and appropriate disposal of infected carcasses and decontamination [2, 10].
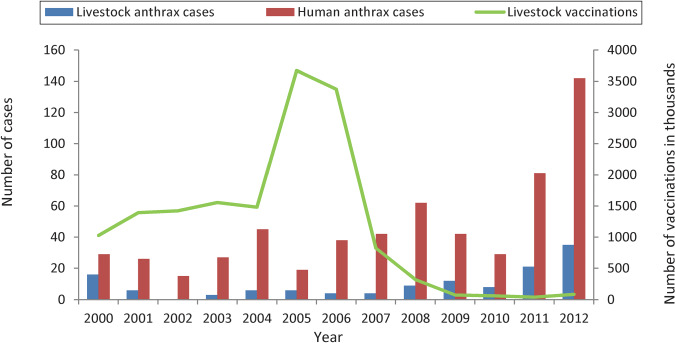
Anthrax is considered endemic in Georgia. A 1995 law required the prevention of epizootic diseases in Georgia, which included mandatory livestock anthrax vaccinations; in 2007, responsibility shifted from Georgia National Food Agency (NFA) veterinarians vaccinating livestock annually to livestock owners contracting private veterinarians to provide anthrax vaccinations. Between 2000 and 2012, the NFA reported 120 livestock anthrax cases; the number of livestock cases increased threefold between 2010 and 2012 (Fig. 1). However, it is assumed that livestock cases are greatly underreported. Of those livestock cases reported in the OIE WAHID database [11] from 2007 to 2012, 65% were from Kvemo Kartli and Kakheti, two adjoining regions in Eastern Georgia; in 2012, according to the Geostat database [12], Kvemo Kartli and Kakheti had 40% of all livestock in Georgia.
Fig. 1.
Number of human and anthrax livestock cases, and number of livestock anthrax vaccinations by year, Georgia, 2000–2012. (Source: Georgia National Center for Disease Control and Public Health and Georgia National Food Agency.)
Between 2000 and 2012, 597 human cases were reported to the Georgia National Center for Disease Control and Public Health (NCDC); of these, 86% were reported from Kvemo Kartli and Kakheti. From 2000 to 2010, the annual number of human cases in Georgia ranged from 15 to 62. The number of cases increased from 28 in 2010 to 81 in 2011, and increased again by 75% to 142 in 2012. Seventy-seven cases reported in 2012 (up to July) prompted an epidemiological investigation of anthrax in Georgia in order to characterize the outbreak.
METHODS
Descriptive epidemiology and control strategies
At the start of the investigation in August 2012, a line listing of cases by region, district, settlement, and date was used for planning. At the end of 2012, all NCDC confirmed and probable human anthrax cases for the year were enumerated, demographic data were extracted, and an epidemic curve was plotted. Cases meeting the following case definitions were identified in the electronic integrated disease surveillance system (EIDSS):
Confirmed case: clinically compatible illness with culture and identification of B. anthracis from clinical specimens, or by evidence of B. anthracis DNA by PCR in clinical specimens collected from a normally sterile site (e.g. blood or cerebral spinal fluid) or from a lesion (skin, pulmonary, reticuloendothelial, or gastrointestinal).
Probable case: clinically compatible illness that does not meet the confirmed case definition, but is epidemiologically linked to a documented anthrax environmental exposure.
Livestock anthrax cases reported to the OIE WAHID database [11] were added to the epidemic curve. A one-sample t test was used to compare 2012 case counts to counts from previous years. Interviews were conducted with NCDC and NFA personnel to determine medical and veterinary outbreak response measures.
Case-control investigation
In order to provide data on exposures and risks associated with human anthrax, a case-control investigation was planned for the locations with the highest human anthrax incidence. The activity was conducted as a 1:2 matched case-control investigation, specifically investigating exposure and risk factors during the 1-month period prior to the onset date for the case associated with each case-control triplet. Cases and controls were limited to persons aged ⩾18 years. Controls were matched by place of residence (within 250 m of the case's residence) and gender, and were recruited by random selection from the closest households to the case's household in which potential subjects were present. In the instance of a refusal, the next household or potential subject was selected until a control was recruited. Gender matching was used due to the possibility of over-selecting females because most males were away from home during working hours.
The case-control investigation questionnaire addressed human, livestock, and environmental risk factors that may have contributed to the occurrence of human anthrax. Concerns were raised by various ministry staff regarding perceived risk from soil exposure, so soil-specific exposure questions were added. Occupational exposures assessed included livestock-related occupations (herder/shepherd, farmer/rancher, livestock worker, veterinarian, slaughterhouse worker, or butcher); other occupations assessed were housewife and student. Slaughter of livestock was considered a risk factor if respondents participated in slaughter of any livestock, whether or not their own.
Cross-sectional assessment
Following completion of the case-control questionnaire, respondents identified as owning or working with livestock were asked to participate in the cross-sectional survey. The objectives were to identify animal management practices or exposures associated with the occurrence of anthrax in livestock and to assess the history of anthrax in the respondent and possible livestock illness or losses which were not previously identified as due to anthrax. All questions addressed the 6 months prior to the interview date.
Questionnaire/interview procedures
The questionnaires were translated into the major languages used in the regions (Georgian, Azeri, Russian). Interview teams were trained on the investigation protocol, informed consent procedures, and questionnaire, and were provided colour pictures of cutaneous anthrax lesions to assist with interviews. Teams included native Azeri language speakers for interviews in villages with primarily Azeri-speaking populations.
Anthrax cases occurring in Kvemo Kartli and Kakheti from April to October 2012 were considered for recruitment. For case-patients not at home at the time of the interview visit, we either arranged meetings or conducted phone interviews. Potential controls were limited to those who were at home during the time of the interview visit; demographic data and addresses of the cases were known and controls could be recruited in the associated neighbourhoods.
Data management and analysis
Epi Info v. 7.1 (CDC, USA) was used for data management. Data were independently double-entered and validated. All data collection instruments were identified in NCDC and CDC records by unique project ID numbers only. SAS v. 9.3 (SAS Institute Inc., USA) was used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) to compare risk factors of cases and controls using conditional logistic regression. Multivariable model selection utilized backward selection on all combinations of the most significant variables from univariate analysis, accounting for multicollinearity and minimizing missing strata to < 10%.
Ethical review
The investigation protocol was reviewed by the NCDC and CDC National Center for Emerging and Zoonotic Infectious Diseases, in accordance with institutional review policies. The protocol was determined to be non-research under 45 CFR 46·102(d), and therefore did not require IRB review.
RESULTS
Descriptive epidemiology and control strategies
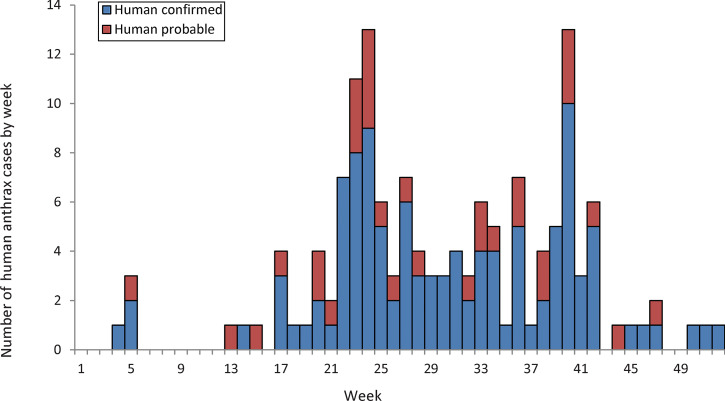
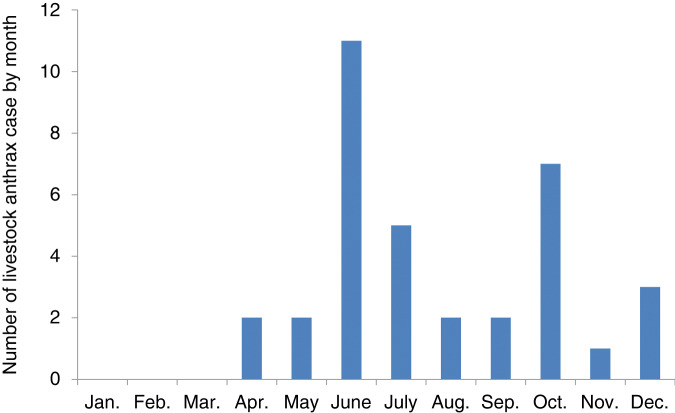
In 2012, 110 confirmed and 32 probable human cutaneous anthrax cases were reported (Table 1). The majority of cases occurred in Kvemo Kartli and Kakheti and corresponded to incidences of 17·8 and 7·6 cases/100 000, respectively (Fig. 2). The case count in Kvemo Kartli and Kakheti was significantly greater than the average count seen in the previous 12 years in both regions (17·1 and 4·4, respectively; P < 0·001). Most cases were male and aged between 20 and 59 years. The median age for all cases was 41 years (range 5–75 years). Cases started to increase in April, peaking in June and again in October (Fig. 3). Thirty-five livestock anthrax cases – including 31 cattle, three sheep or goats, and one horse – were reported to the OIE WAHID database [11] in 2012, with cases also peaking in June and October (Fig. 4).
Table 1.
Demographic characteristics of human anthrax cases reported in 2012 in Georgia
| Characteristic | n | % |
|---|---|---|
| Sex | ||
| Male | 119 | 84 |
| Female | 23 | 16 |
| Region | ||
| Kvemo Kartli | 91 | 64 |
| Kakheti | 31 | 22 |
| Tbilisi | 9 | 6 |
| Samegrelo Zemo Svaneti | 4 | 3 |
| Imereti | 3 | 2 |
| Ajara | 2 | 1 |
| Guria | 1 | 1 |
| Mtskheta Mtianeti | 1 | 1 |
| Age group, years | ||
| <20 | 7 | 5 |
| 20–29 | 29 | 20 |
| 30–39 | 26 | 18 |
| 40–49 | 33 | 23 |
| 50–59 | 32 | 23 |
| >59 | 15 | 11 |
| Total | 142 | 100 |
Fig. 2.
Human anthrax incidence (per 100 000 population) by region, Georgia, 2012 (http://www.geostat.ge/).
Fig. 3.
Human anthrax case numbers (confirmed and probable) by week (n = 142), Georgia, 2012. (Source: data reported in the electronic integrated disease surveillance system to Georgia National Center for Disease Control and Public Health.)
Fig. 4.
Confirmed livestock cases by month, Georgia, 2012. (Source: data reported in OIE WAHID database [11].)
Interviews with NCDC and NFA personnel revealed that initial livestock investigation and control strategies were constrained by lack of resources. NCDC, NFA, and the laboratory of the Ministry of Agriculture reported surveillance data to a common electronic system; however, data were not actively shared between human and livestock health authorities. Initial focus on soil exposures as a potential cause for human cases limited the implementation of livestock anthrax control programmes during the initial outbreak response. An ongoing national cattle identification and foot-and-mouth disease vaccination campaign delayed the start of a national cattle anthrax vaccination response programme until November 2012. During our investigation, awareness literature including prevention recommendations was distributed to neighbours around each case. Television alerts commenced in September 2012 and continued into 2013.
Case-control investigation
A total of 67 case-patients and 134 controls were enrolled in the case-control investigation; 82% (n = 55) of cases were confirmed, and 18% (n = 12) probable. The mean age of cases was 42 years (range 18–72 years), and that of controls 46 years (range 18–75 years). Cases and controls were matched on gender and region, and similar in nationality and age groups (Table 2). The majority were male and from Kvemo Kartli. Most participants were Azerbaijani or Georgian.
Table 2.
Characteristics of 2012 anthrax case-control investigation participants, Georgia
| Characteristic | Cases | Controls | OR (95% CI) | P value | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Sex* | – | |||||
| Male | 57 | 85 | 114 | 85 | – | |
| Female | 10 | 15 | 20 | 15 | – | |
| Region* | – | |||||
| Kvemo Kartli | 55 | 82 | 110 | 82 | – | |
| Kakheti | 11 | 16 | 22 | 16 | – | |
| Tbilisi | 1 | 1 | 2 | 1 | – | |
| Nationality | 0·6 | |||||
| Azeri | 42 | 63 | 79 | 59 | 3·2 (0·3–36·6) | |
| Georgian | 24 | 36 | 50 | 37 | Reference | |
| Other† | 1 | 1 | 5 | 4 | Undefined | |
| Age group, years | 0·3 | |||||
| 18–34 | 23 | 34 | 36 | 27 | Reference | |
| 35–49 | 23 | 34 | 42 | 31 | 0·8 (0·4–1·6) | |
| ⩾50 | 21 | 31 | 56 | 42 | 0·5 (0·2–1·2) | |
| Total | 67 | 100 | 134 | 100 | ||
OR, Odds ratio; CI, confidence interval.
Cases and controls matched on sex and region; therefore, odds ratios are not reported.
Other nationalities included Greek and Ukrainian.
Individually analysed risk factors for developing anthrax are given in Table 3. The risk factors most strongly associated with case-patients were caring for sick livestock (OR 24·6, 95% CI 3·2–188·1, P = 0·002) and disposing of dead livestock (OR 18·1, 95% CI 2·3–142·0, P = 0·006). Being part of households that owned animals; slaughtering or skinning livestock; having livestock-related occupations; or participation in livestock care, including herding and removal of animal waste or dirty bedding, were associated with disease. Participation in livestock slaughter included five subcategorized activities, of which none individually were significantly associated with disease. Cases were more likely to slaughter their own livestock. Cases were also more likely to have owned cattle, horses, goats, or dogs than controls, and were less likely to report insect bites (Table 3).
Table 3.
Evaluation of potential risk factors for anthrax in case-control investigation participants in the 1 month prior to case onset date, Georgia, 2012
| Risk factor | Cases | Controls | OR*† | 95% CI | P value | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Livestock-related occupations‡ | 26 | 48 | 24 | 25 | 4·0 | 1·5–10·0 | 0·005 |
| Household animals | 53 | 79 | 67 | 51 | 7·2 | 2·7–19·1 | <0·001 |
| Cattle | 49 | 74 | 60 | 45 | 5·5 | 2·4–12·9 | <0·001 |
| Horse | 15 | 26 | 9 | 7 | 6·0 | 2·0–18·5 | 0·002 |
| Sheep | 17 | 28 | 20 | 16 | 2·2 | 1·0–5·2 | 0·06 |
| Goat | 9 | 16 | 7 | 6 | 3·3 | 1·1–10·0 | 0·03 |
| Dog | 35 | 59 | 39 | 31 | 4·6 | 2·0–10·4 | <0·001 |
| Livestock care | 47 | 70 | 61 | 47 | 3·8 | 1·8–8·2 | <0·001 |
| Herding | 31 | 48 | 43 | 34 | 3·2 | 1·4–7·2 | 0·004 |
| Cleaning§ | 37 | 61 | 54 | 43 | 3·0 | 1·4–6·4 | 0·005 |
| Milking | 15 | 25 | 29 | 23 | 1·5 | 0·6–3·8 | 0·4 |
| Shearing | 10 | 17 | 14 | 11 | 1·9 | 0·8–4·7 | 0·2 |
| Care for sick livestock | 16 | 25 | 6 | 5 | 24·6 | 3·2–188·1 | 0·002 |
| Sell sick livestock | 5 | 11 | 5 | 6 | 5·8 | 0·6–53·6 | 0·1 |
| Kill/dispose of carcass | 6 | 14 | 8 | 11 | 0·9 | 0·2–3·9 | 0·9 |
| Slaughter or skin livestock | 28 | 44 | 16 | 13 | 7·0 | 2·9–17·2 | <0·001 |
| Dispose of dead livestock | 11 | 17 | 3 | 2 | 18·1 | 2·3–142·0 | 0·006 |
| Exposed to livestock with suspected anthrax | 59 | 92 | 127 | 97 | 0·3 | 0·1–1·5 | 0·1 |
| How owner would treat sick livestock | |||||||
| Owner treated | 10 | 22 | 19 | 23 | 1·2 | 0·5–3·4 | 0·7 |
| Veterinarian treated | 29 | 63 | 54 | 66 | 0·9 | 0·4–2·2 | 0·9 |
| Slaughter own livestock | 27 | 42 | 29 | 25 | 2·9 | 1·3–6·6 | 0·01 |
| Activities during livestock slaughter | |||||||
| Holding animal down | 21 | 81 | 26 | 93 | 0·2 | 0·03–2·2 | 0·2 |
| Gutting | 24 | 96 | 25 | 89 | 2·6 | 0·3–25·2 | 0·4 |
| Killing | 23 | 88 | 27 | 96 | 1·0 | 0·06–16·0 | 1·0 |
| Skinning | 24 | 92 | 24 | 92 | 2·0 | 0·2–22·1 | 0·6 |
| Witnessing within a 10 m radius | 7 | 33 | 9 | 33 | 0·3 | 0·03–2·7 | 0·3 |
| Wear overalls or apron | 3 | 60 | 6 | 46 | Undefined | 1·0 | |
| Reason no protective equipment used | |||||||
| Not aware protective equipment needed | 13 | 76 | 22 | 81 | 0·7 | 0·1–5·2 | 0·7 |
| Normally does not use protective equipment | 15 | 65 | 10 | 38 | 0·3 | 0·03–2·5 | 0·3 |
| Meat handling activities | |||||||
| Cutting | 32 | 49 | 49 | 40 | 1·6 | 0·8–3·2 | 0·2 |
| Preparing for cooking | 21 | 34 | 45 | 37 | 0·8 | 0·4–1·7 | 0·6 |
| Moving | 29 | 45 | 40 | 33 | 2·1 | 1·0–4·2 | 0·05 |
| Cooking | 17 | 27 | 45 | 36 | 0·6 | 0·3–1·2 | 0·2 |
| Drying | 6 | 10 | 14 | 12 | 0·8 | 0·3–2·3 | 0·7 |
| Eating | 44 | 69 | 94 | 76 | 0·6 | 0·3–1·2 | 0·2 |
| Covered injury handling meat | 3 | 7 | 17 | 28 | 0·2 | 0·05–1·1 | 0·06 |
| Meat sources | |||||||
| Own farm | 21 | 36 | 24 | 21 | 3·5 | 1·3–9·4 | 0·01 |
| Butcher's shop | 31 | 52 | 82 | 67 | 0·4 | 0·2–0·9 | 0·03 |
| Grocery | 10 | 20 | 22 | 19 | 0·7 | 0·2–2·3 | 0·6 |
| Meat market | 25 | 47 | 61 | 52 | 0·8 | 0·4–1·7 | 0·5 |
| Neighbour | 13 | 28 | 18 | 17 | 2·5 | 0·7–8·4 | 0·2 |
| Mobile meat seller | 8 | 16 | 18 | 16 | 0·7 | 0·2–2·3 | 0·6 |
| Consumed raw or undercooked meat | |||||||
| Source of meat | |||||||
| Consumed cattle (beef) | 13 | 87 | 22 | 67 | 2·4 | 0·4–13·2 | 0·3 |
| Consumed sheep (mutton or lamb) | 5 | 33 | 15 | 47 | 0·3 | 0·03–2·6 | 0·3 |
| Where meat was consumed | |||||||
| At home | 12 | 67 | 21 | 75 | 0·3 | 0·03–3·2 | 0·3 |
| At restaurant | 4 | 25 | 9 | 32 | 0·9 | 0·2–4·6 | 0·9 |
| How meat was prepared | |||||||
| Pink in middle | 5 | 8 | 5 | 4 | 2·7 | 0·5–15·0 | 0·2 |
| Boiled | 48 | 76 | 84 | 67 | 1·8 | 0·8–4·0 | 0·2 |
| Grilled | 9 | 15 | 12 | 10 | 1·3 | 0·4–3·8 | 0·6 |
| Roasted | 17 | 28 | 46 | 38 | 0·6 | 0·3–1·2 | 0·1 |
| Kinkali (dumplings) | 29 | 47 | 69 | 54 | 0·7 | 0·4–1·5 | 0·4 |
| Shashlik (grilled barbecue) | 23 | 36 | 58 | 46 | 0·6 | 0·3–1·3 | 0·2 |
| Would eat meat from sick livestock | 59 | 92 | 113 | 88 | 2·0 | 0·6–7·3 | 0·3 |
| Would eat meat from livestock found dead | 60 | 95 | 112 | 88 | 5·0 | 1·0–24·8 | 0·05 |
| Travel|| | 13 | 20 | 17 | 13 | 1·7 | 0·7–4·1 | 0·3 |
| Handled livestock products | 33 | 51 | 27 | 22 | 4·0 | 1·9–8·4 | <0·001 |
| Bones/horn | 9 | 41 | 4 | 18 | 1·4 | 0·08–23·6 | 0·8 |
| Skin/hide | 16 | 62 | 4 | 17 | 3·0 | 0·3–28·8 | 0·3 |
| Leather | 12 | 55 | 7 | 30 | 2·6 | 0·3–25·2 | 0·4 |
| Insect bite | 53 | 88 | 127 | 97 | 0·2 | 0·03–0·8 | 0·02 |
| Work with soil | |||||||
| Near sick or dead livestock | 61 | 97 | 118 | 95 | 1·6 | 0·2–10·1 | 0·6 |
| Near livestock burial site | 15 | 94 | 36 | 95 | 0·7 | 0·04–11·8 | 0·8 |
| Near other earthworks | 42 | 65 | 75 | 58 | 1·5 | 0·6–3·4 | 0·4 |
| While gardening | 9 | 64 | 27 | 59 | 0·6 | 0·1–4·2 | 0·6 |
| Covered injury while working soil | 2 | 11 | 13 | 34 | 0·2 | 0·02–2·0 | 0·2 |
| Total | 67 | 100 | 134 | 100 | − | − | − |
OR, Odds ratio; CI, confidence interval.
All values shown in bold indicate a significant difference (P < 0·05).
All ORs and corresponding 95% CIs are calculated comparing cases to controls.
Livestock-related occupations included herder/shepherd, farmer/rancher, livestock worker, and veterinarian.
Cleaning defined as removing animal waste and/or dirty bedding.
Participant travelled outside place of residence/village.
Having contact with or helping to prepare livestock products (e.g. meat, skin, leather, bones) was associated with disease; however, no individual type of livestock origin product was significantly associated with disease. Eating meat from one's own farm was associated with disease while buying meat from a butcher's shop was protective. No prepared meat dish or cooking preference was associated with disease and no meat handling activities were significantly associated. Consuming raw or undercooked meat was not associated with disease, nor was the source of meat or location the meat was consumed.
Despite original concerns raised that disease was due to contact with contaminated soil, work with soil near livestock burial sites or work with soil at other locations including agricultural farm work were not associated with disease.
The independent predictors that remained most strongly associated with disease in the multivariable model were slaughtering animals (OR 7·3, 95% CI 2·9–18·1, P < 0·001) and disposing of dead animals within the month prior to case onset (OR 13·6, 95% CI 1·5–119·8, P = 0·02).
Cross-sectional assessment
From the pool of 201 case-control participants, 131 (65%) were eligible for enrolment in the cross-sectional assessment and all elected to participate (Table 4). Less than half of respondents reported vaccinating their livestock for anthrax in the previous 6 months. Of those who reported not vaccinating their animals for anthrax, one-third stated that they did not know about anthrax vaccination for their animals, and one-quarter stated they could not afford the vaccine; the response rates for these questions were low (22% and 24%, respectively). Other findings indicated that few of the respondents moved livestock >1 km from where they were pastured the day of the interview. Those respondents reporting sick animals also mostly reported anthrax-related symptoms, such as acute illness and/or head or neck swelling and subsequent animal deaths; two of 10 reported sick animals were sold or slaughtered for consumption. Sudden death in animals was also reported, some of which were processed for meat.
Table 4.
Participants’ responses to animal management questions, 2012 anthrax cross-sectional assessment in Georgia (n = 131)
| Variable | Yes | No | ||
|---|---|---|---|---|
| n | % | n | % | |
| Livestock anthrax vaccination | 53 | 44 | 68 | 56 |
| Did not know about vaccine | 10 | 67 | 5 | 33 |
| Unable to afford vaccine | 12 | 75 | 4 | 25 |
| Move livestock >1 km | 19 | 16 | 97 | 84 |
| Had sick livestock | 15 | 12 | 110 | 88 |
| Sick livestock had anthrax symptoms | 9 | 64 | 5 | 36 |
| Sick livestock died | 8 | 80 | 2 | 20 |
| Sell or slaughtered sick livestock for consumption | 2 | 20 | 8 | 80 |
| Had livestock die suddenly | 11 | 9 | 117 | 91 |
| Processed for consumption | 2 | 25 | 6 | 75 |
DISCUSSION
Descriptive epidemiology and control strategies
According to the GIDEON database [13], human cutaneous anthrax in Georgia increased after funding for control programmes began to decline in 1989. In 2007, responsibility for providing livestock anthrax vaccinations shifted to individual farmers which probably led to a decrease in vaccinations administered and a resulting increase in livestock cases. The bimodal peaks in the 2012 anthrax outbreak of both livestock and human cases were unusual. The June peak was preceded by heavy rainfall in May, which was three times greater than the rainfall observed in June, which itself was 1·5 times less than the previous 30-year average. Additionally, the October peak in Kvemo Kartli occurred after July where rainfall was twofold higher and August rainfall was twofold less than the previous 30-year average. No significant changes in average temperatures were recorded by the Georgia National Environmental Agency. This pattern of outbreak peaks occurring in dry or normal precipitation months following months where heavy rains occurred has been reported elsewhere for previous livestock anthrax outbreaks [14, 15]. Two suggested mechanisms include: (1) new grass growth and loosened soil, due to rain, increasing the likelihood of spore ingestion by livestock on contaminated pastures and (2) emergence of excess biting flies implicated in mechanical transmission [16]. Further investigation of the ecological relationships in Georgia between weather patterns and outbreaks of anthrax is warranted.
The significant increase in human anthrax cases in 2012 indicated an even larger outbreak exceeding the already increasing trend in cases. The high proportion of human cases in Kvemo Kartli and Kakheti could be related to those regions containing 40% of Georgia's susceptible livestock. However, a parallel increase in livestock anthrax was not identified, in part because livestock deaths are often not reported. Additionally, human cases were not commonly linked to specific livestock case exposures, due partially to a lack of coordinated anthrax case investigation between medical and veterinary authorities. Only two of the human cases investigated in this outbreak were linked to the same exposure source, the slaughter of an infected sheep; otherwise, households or clusters of households with more than one case were not noted.
Interestingly, no gastrointestinal cases were reported in this outbreak. Mild cases with non-specific gastroenteritis symptoms either may not seek medical care or anthrax may not be suspected [2]. Moreover, hyperacute cases may avoid diagnosis as they die before receiving medical attention [2]. Additionally, there is a high background level of diarrhoeal disease in Georgia including hemorrhagic diarrhoea [17], which could reduce the index of suspicion for anthrax as an aetiological cause. There are also existing cultural preferences in Georgia against consuming raw or under-cooked meat, which may limit the occurrence of gastrointestinal anthrax.
Case-control investigation
Most human anthrax outbreaks are generally related to livestock anthrax cases or outbreaks [5, 6]. In this investigation, all risk factors significantly associated with disease were related to exposure to livestock or their products. After multivariable analysis, dead livestock disposal and animal slaughter were the independent predictors most strongly associated with disease; this was especially true for those slaughtering their own livestock. Slaughtering sick livestock has been reported in other countries as a routine practice in an attempt to recover some of their investment [18]; this investigation provides evidence that meat from sick livestock and livestock found dead was processed for sale or consumption, probably to minimize economic loss. There is no policy in Georgia for compensation of livestock losses, which may prompt residents to resort to this activity. In addition, persons may not be aware of the risks of anthrax associated with butchering, handling, or consuming meat from infected animals [18]; in this investigation, most cases (92%) and controls (88%) reported that they would consume livestock that were found to be sick, or dead (95% and 88%, respectively).
The strongest association found among individual potential risk factors was caring for sick livestock. Contact with sick or dying anthrax-infected livestock has previously been demonstrated to be the principal source of human agricultural exposures [2, 5, 6]. Cutaneous anthrax can occur when agricultural and veterinary workers handle, slaughter, perform necropsy on, or dispose of affected and dead animals [19]. Those who owned livestock, especially cattle and goats, had higher odds of becoming infected than controls. Dog ownership and horse ownership were also significantly associated. However, this is probably the result of close correlation between dog and horse ownership and cattle ownership, as 91% and 92% of dog and horse owners, respectively, also owned cattle. Horse meat is not commonly consumed in Georgia, limiting human exposures to equine carcasses. Furthermore, equine anthrax has been reported rarely in Georgia, and without any associated human cases reported. Canines are considered relatively resistant to infection [3, 20], and no canine cases have been reported in the OIE WAHID database [11].
Another strong association was seen with those who handled livestock products such as meat, skin, leather, or bones. No specific livestock species or product type was found to have higher odds for infection; however, handling and bringing meat from diseased animals into the household was found to be associated with disease in an investigation of anthrax in Haiti [21]. In our investigation, eating meat from one's own farm was a risk, as was slaughtering one's own livestock and slaughtering livestock that were found sick; however, buying meat from a butcher's shop was protective. It is likely that human anthrax exposures and cases occurred when people slaughtered and butchered their own potentially infected animals, whereas regulations requiring meat sold in markets and butcher's shops to originate from inspected slaughterhouses potentially reduced the risk of meat from infected animals being sold there.
As expected, those who worked in livestock-related occupations were at higher risk of developing anthrax; however, no single occupation classification was significantly associated. Both herding and cleaning animal waste or dirty bedding were identified as higher-risk farm activities. Each involves working closely with livestock or their environment. Agricultural field work was not associated with disease in this investigation; however, it was previously identified as a self-reported source of exposure in Georgia [22]. It was noted that this exposure source is not well documented and the reports may result from recall bias or an unwillingness to disclose slaughtering of infected animals [22].
Three species of blood-feeding insects were able to mechanically transmit anthrax to guinea pigs and mice in one study [4]; however, we found bites from blood-feeding insects were more frequently reported by controls compared to cases. We did not determine the species of biting insects; therefore, different species may have been involved with controls and cases based on their locations relative to animal carcasses, which may explain this finding. Additionally, biting flies are more frequently associated with livestock outbreaks than with human cases since they only occasionally bite humans [16].
We found slaughter and disposing of dead animals to remain strong independent predictors of human disease in multivariable analysis. We also emphasize the univariate analysis results demonstrating that increased risk is primarily related generally to occupational contact with livestock and meat for consumption due to the level of multicollinearity between individual characteristics and behaviours elicited in the questionnaire.
Cross-sectional assessment
Most cross-sectional assessment participants did not vaccinate their livestock. Given the cessation of national anthrax vaccination campaigns in Georgia in 2007 and subsequent decrease in anthrax vaccine administration, reinstitution of annual government-sponsored vaccination programmes may be necessary, particularly in endemic regions. Livestock vaccination remains a mainstay of control, reducing animal disease incidence, sometimes to the point of elimination, thereby reducing human exposures to infected livestock and animal products and consequent illness [10, 23].
Only a few respondents reported moving livestock >1 km from where they were pastured on the day of interview; however, both free-roaming and shepherded livestock were observed within and near many communities. This question was important to determine any role of animal movement in exposure, such as exposing animals to areas containing anthrax carcass burial sites. Regardless, livestock anthrax appeared to be localized and not resulting from exposures in other regions, such as may arise in animals migrating from pastures in other regions of the country.
The cross-sectional assessment explored health outcomes in livestock, with two-thirds of respondents reporting acute illness and/or head or neck swelling, clinical signs associated with anthrax infections. These findings suggest there were livestock anthrax cases not being identified and reported. After finding dead livestock, approximately one-fifth of respondents processed the carcasses for human consumption; again this salvage practice most likely occurred to minimize economic loss, but potentially resulted in human exposures and illness. Public health and animal health messaging can help inform livestock owners to recognize anthrax, of the value of veterinary examinations, and of the human health risks from slaughtering and consuming sick livestock or carcasses. The introduction of compensation for livestock losses that are properly notified to authorities, with subsequent investigation, response and appropriate decontamination may help reduce the occurrence of salvage slaughter and butchering of anthrax-infected animals. Alternatively, the introduction of insurance for livestock, whereby compensation is provided if anthrax occurs in animals that are appropriately vaccinated, can help promote vaccination as a preventive practice and mitigate economic loss, thus reducing the likelihood that anthrax-affected meat will enter the food chain.
Limitations
Survey participants were similar demographically except for specific occupations related to livestock. Since controls were those who were at home at the time of the interview visit, control participants were possibly biased towards those who did not participate in fieldwork or have livestock-associated occupations, which could increase the value of the odds ratio. Our results were also potentially influenced by differential recall bias and false reporting. Persons without anthrax may not remember exposure history during the time period of risk for the matched cases. This may lead to differential under-reporting of exposure by controls, and increase the value of the odds ratio. By contrast, cases may not admit their participation in slaughter of sick livestock or sale of meat from a sick animal; this was identified by NCDC investigators as a practice with origins during the Soviet period, when such activities would result in punitive measures from the government [24, 25]. This under-reporting of exposure by cases could lower the value of the odds ratio.
Other limitations were related to the questions regarding livestock anthrax vaccination. The timing of vaccination relative to the occurrence of anthrax in any animal in the interviewee's or a neighbouring herd was not ascertained by the questionnaire, so we were unable to assess a temporal relationship between livestock vaccination and either human or animal anthrax cases. It was therefore possible that a respondent would report that they had vaccinated their livestock for anthrax, but only after the disease had appeared in either their herd or a neighbouring herd; one case reported vaccinating his animals only after he had developed anthrax himself.
We were unable to obtain responses to follow-up questions related to knowledge of anthrax prevention practices in livestock and the ability to afford vaccinations from over three-quarters of participants who did not vaccinate, so these results should be interpreted with caution. These topics may potentially be sensitive resulting in participants’ reluctance to respond or to provide factual responses. Regardless, we think that both vaccine knowledge and affordability are important factors to explore with regard to intervention recommendations.
Recommendations
It was evident that handling carcasses, sick livestock, or associated livestock products were significant risk factors for human disease; people should be discouraged from handling possible anthrax-infected livestock or products in any form, unless properly trained and wearing appropriate personal protective equipment. The combination of compensation programmes to prevent the slaughter and sale of meat from infected animals and nationally sponsored anthrax vaccination campaigns in livestock may reduce the burden of human and animal disease; such programmes could be initially focused in areas with recent reports of animal or human cases. The NFA started prophylactic anthrax vaccination of cattle in the predominantly affected regions of Kvemo Kartli and Kakheti at the end of 2012 and in 2013. Finally, we encourage collaboration between relevant partners to develop and distribute health messaging on control and recognition of anthrax in humans and animals, integration of disease surveillance, and collaborative investigation of anthrax cases. According to the ProMED database [26], such an investigation occurred in August 2013, where a joint human and animal health investigation of a human anthrax case in Tbilisi, Georgia identified the exposure source as meat sold in a market, ultimately traced back to an illegal, uninspected source. The response included decontamination and cessation of further sale of suspect meat at the market, with no subsequent human cases reported.
ACKNOWLEDGEMENTS
The authors thank Arianne Folkema (Region of Waterloo Public Health) for statistical contributions on investigation methodology and analysis.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
APPENDIX. The anthrax investigation team
Z. Asanishvili1, T. Napetvaridze1, S. Guramishvili2, M. Lashkarashvili2, N. Mamuchishvili2, S. Huseynova3, M. Shikhiyev3, M. Abdullayev3, E. Zeynalov3
1 Georgia National Food Agency, Georgia Ministry of Agriculture, Tbilisi, Georgia
2 Georgia National Center for Disease Control and Public Health, Georgia Ministry of Health, Tbilisi, Georgia
3 South Caucasus Field Epidemiology and Laboratory Training Program, Tbilisi, Georgia
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Manchee RJ, et al. Bacillus anthracis on Gruinard Island. Nature 1981; 294: 254–255. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Anthrax in Humans and Animals, 4th edn. Geneva: WHO Press, 2008, pp. 1–208. [PubMed] [Google Scholar]
- 3.Hugh-Jones ME, de Vos V. Anthrax and wildlife. Revue Scientifique et Technique (International Office of Epizootics) 2002; 21: 359–383. [DOI] [PubMed] [Google Scholar]
- 4.Turell MJ, Knudson GB. Mechanical transmission of Bacillus anthracis by stable flies (Stomaxys calcitrans) and mosquitoes (Aedes aegypti and Aedes taeniorhynchus). Infection and Immunity 1987; 55: 1859–1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pile JC, et al. Anthrax as a potential biological warfare agent. Archives of Internal Medicine 1998; 158: 429–434. [DOI] [PubMed] [Google Scholar]
- 6.Quinn CP, Turnbull PCB. Anthrax. In: Hausler WJ, Sussman M (eds). Topley and Wilson's Microbiology and Microbial Infection, 9th edn. London: Edward Arnold, 1998, pp. 799–818. [Google Scholar]
- 7.Martin GJ, Friedlander AM. Bacillus anthracis (anthrax). In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, 7th edn. Philadelphia: Churchill Livingstone, 2010, pp. 2715–2725. [Google Scholar]
- 8.Hugh-Jones M. 1996–97 global anthrax report. Journal of Applied Microbiology 1999; 87: 189–191. [DOI] [PubMed] [Google Scholar]
- 9.Dragon DC, Rennie RP. The ecology of anthrax spores: tough but not invincible. Canadian Veterinary Journal 1995; 36: 295–301. [PMC free article] [PubMed] [Google Scholar]
- 10.Shadomy SV, Smith TL. Zoonosis update: anthrax. Journal of the American Veterinary Medical Association 2008; 233: 63–72. [DOI] [PubMed] [Google Scholar]
- 11.OIE WAHID Interface database. (http://www.oie.int/wahis_2/public/wahid.php/Wahidhome/Home). Accessed 26 September 2014.
- 12.Geostat database. (http://www.geostat.ge/index.php?action=page&p_id=428&lang=eng). Accessed 26 June 2014.
- 13.GIDEON database. (http://web.gideononline.com/web/epidemiology/#). Accessed 27 February 2012.
- 14.Vas Ness GB, et al. The Oklahoma-Kansas anthrax epizootic of 1957. Journal of the American Veterinary Medical Association 1959; 134: 125–129. [PubMed] [Google Scholar]
- 15.Mongoh MN, et al. Risk factors associated with anthrax outbreak in animals in North Dakota, 2005: a retrospective case-control study. Public Health Reports 2008; 123: 352–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hugh-Jones M, Blackburn J. The ecology of Bacillus anthracis. Molecular Aspects of Medicine 2009; 30: 356–367. [DOI] [PubMed] [Google Scholar]
- 17.Chokoshvili O, et al. Investigation of an outbreak of bloody diarrhea complicated with hemolytic uremic syndrome. Journal of Epidemiology and Global Health 2014; 4: 249–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chakraborty A, et al. Anthrax outbreaks in Bangladesh, 2009–2010. American Journal of Tropical Medicine and Hygiene 2012; 86: 703–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bales ME, et al. Epidemiologic response to anthrax outbreaks: field investigations, 1950–2001. Emerging Infectious Diseases 2002; 8: 1163–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Langston C. Postexposure management and treatment of anthrax in dogs – executive councils of the American academy of veterinary pharmacology and therapeutics and the American college of veterinary clinical pharmacology. AAPS Journal 2005; 7: E272–E273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peck RN, Fitzgerald DW. Cutaneous anthrax in the Artibonite Valley of Haiti: 1992–2002. American Journal of Tropical Medicine and Hygiene 2007; 77: 806–811. [PubMed] [Google Scholar]
- 22.Kracalik I, et al. Human cutaneous anthrax, Georgia 2010–2012. Emerging Infectious Diseases 2014; 20: 261–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Turnbull PCB. Anthrax vaccines: past, present and future. Vaccine 1991; 9: 533–539. [DOI] [PubMed] [Google Scholar]
- 24.Guillemin J. Anthrax: The Investigation of a Deadly Outbreak. Berkeley: University of California Press, 1999, pp. 22–24. [Google Scholar]
- 25.Balayev IP. Strict observance of veterinary regulations. Chelovek I Zakon [Man and the Law] 1980; 9: 70–72. [Google Scholar]
- 26.ProMED database. (http://www.promedmail.org/). Archive number: 20130826·1901988.