SUMMARY
Although contamination of food can occur at any point from farm to table, restaurant food workers are a common source of foodborne illness. We describe the characteristics of restaurant-associated foodborne disease outbreaks and explore the role of food workers by analysing outbreaks associated with restaurants from 1998 to 2013 reported to the Centers for Disease Control and Prevention's Foodborne Disease Outbreak Surveillance System. We identified 9788 restaurant-associated outbreaks. The median annual number of outbreaks was 620 (interquartile range 618–629). In 3072 outbreaks with a single confirmed aetiology reported, norovirus caused the largest number of outbreaks (1425, 46%). Of outbreaks with a single food reported and a confirmed aetiology, fish (254 outbreaks, 34%) was most commonly implicated, and these outbreaks were commonly caused by scombroid toxin (219 outbreaks, 86% of fish outbreaks). Most outbreaks (79%) occurred at sit-down establishments. The most commonly reported contributing factors were those related to food handling and preparation practices in the restaurant (2955 outbreaks, 61%). Food workers contributed to 2415 (25%) outbreaks. Knowledge of the foods, aetiologies, and contributing factors that result in foodborne disease restaurant outbreaks can help guide efforts to prevent foodborne illness.
Key words: Infectious disease epidemiology, outbreaks, public health
INTRODUCTION
Foodborne illness caused by a known pathogen causes an estimated 9·4 million illnesses, 56 000 hospitalizations, and over 1300 deaths annually in the United States [1]. Over 90% of these illnesses are caused by 15 major pathogens, including various viruses, bacteria, and parasites, but most commonly norovirus and Salmonella enterica [2, 3].
Annually, over 800 foodborne disease outbreaks are reported to the Centers for Disease Control and Prevention (CDC) and most commonly occur in a restaurant setting [2]. In 2013, 51% of single-setting foodborne disease outbreaks were caused by food prepared in a restaurant [4]. Americans eat at restaurants an average of five times weekly [5] and it is estimated that 47% of every dollar spent on food in 2015 was spent at a restaurant [6].
The U.S. Food and Drug Administration (FDA) provides guidelines designed to prevent foodborne disease in restaurant settings; states are responsible for adopting and enforcing restaurant food-safety regulations. These guidelines address the standards for personnel management and employee health, food-safety practices, equipment storage and cleanliness, waste disposal, physical facility optimization to avoid contamination with pathogens, and poisonous material handling and storage [7]. Contamination of food served in a restaurant can occur at any point from farm to table. The guidelines aim to minimize restaurants' role in foodborne illness.
The study objective was to describe the characteristics of restaurant-based foodborne disease outbreaks, identify outbreak contributing factors, and examine the role of food workers in these outbreaks. Results of this analysis can help guide efforts to prevent foodborne illness.
MATERIALS AND METHODS
CDC collects foodborne disease outbreak reports from state and local health departments through the Foodborne Disease Outbreak Surveillance System (FDOSS) [8]. The information collected for each outbreak includes year, month, state, number of illnesses, hospitalizations and deaths, confirmed aetiology, implicated food, settings where food was prepared, and contributing factors.
We reviewed foodborne disease outbreaks that occurred during 1998–2013 in which a restaurant was the only place where food was prepared. We analysed implicated food categories, aetiology, restaurant type, and factors contributing to outbreak occurrence.
Implicated foods were categorized using the Interagency Food Safety Analytics Collaboration's (IFSAC) scheme [9]. Implicated foods that contained ingredients belonging to more than one category were classified as ‘complex’ when the food category responsible for illness could not be determined. For most pathogens, an aetiology was defined as confirmed if the organism was detected in samples from two or more ill persons, or in an epidemiologically implicated food(s). For marine and other toxins, confirmation requires a clinically compatible illness in two or more ill persons who ate an implicated food (e.g. as with the distinct clinical syndromes of botulism, scrombroid toxin, or heavy metals) [10, 11]. Aetiologies not meeting the criteria were classified as suspect; these suspect aetiologies included toxin-mediated illness (e.g. Bacillus cereus, Clostridium perfringens, Staphylococcus aureus enterotoxin) and uncommon aetiologies (e.g. Trichinella, Cyclospora, pesticides) in which laboratory confirmation was only performed for a single ill person or illness was identified through clinical presentation and/or epidemiological risk factors without laboratory testing. Only confirmed aetiologies were included in aetiology analyses. The restaurant type (i.e. sit-down, fast-food, other) was reported starting in 2009. Contributing factors, or reasons for contamination, were grouped into one of four categories for analysis: food worker health and hygiene, food contamination before arrival at the restaurant, food handling and preparation practices in the restaurant, and other factors (Appendix A). Because more than one contributing factor could be reported for an outbreak, an outbreak could be included in more than one contributing factor category. Food workers were implicated if a contributing factor indicating lapses in food worker health and hygiene (e.g. bare-hand contact with food) was reported or if a food worker was explicitly implicated as the cause.
The Wilcoxon test was used to compare the median number of ill persons in outbreaks. All analysis was performed using SAS v. 9.3 (SAS Institute Inc., USA).
RESULTS
Of 17 445 outbreaks reported during 1998–2013, 9788 (56%) outbreaks involved food prepared in a restaurant (Appendix B), resulting in 124 608 illnesses, 4427 hospitalizations, and 32 deaths. There were a median of 620 outbreaks annually [interquartile range (IQR) 618–629], resulting in 3151 to 11 426 illnesses each year. The median outbreak size was five persons (IQR 3–12). The largest number of restaurant-associated outbreaks were reported from Florida (1742 outbreaks, 18%), California (1289 outbreaks, 13%), and Ohio (666 outbreaks, 7%). The annual number of restaurant-associated outbreaks and the percentage of all outbreaks linked to restaurants declined from 2000 (884, 63%) to 2013 (431, 52%) (Fig. 1).
Fig. 1.
Number of restaurant-associated foodborne disease outbreaks and percentage of all foodborne disease outbreaks, by year, Foodborne Disease Outbreak Surveillance System, 1998–2013.  , Number of foodworker-associated outbreaks;
, Number of foodworker-associated outbreaks;  , number of non-foodworker-associated outbreaks;
, number of non-foodworker-associated outbreaks;  , percentage of all foodborne disease outbreaks that were restaurant-associated.
, percentage of all foodborne disease outbreaks that were restaurant-associated.
Implicated foods
A food was implicated in 4102 (42%) outbreaks. Of these, 1775 (43%) had a food that could be assigned to a single category, most commonly fish (387 outbreaks, 33%), beef (314 outbreaks, 27%), chicken (239 outbreaks, 20%), and molluscs (147 outbreaks, 13%) (Table 1).
Table 1.
Foods implicated in restaurant-associated foodborne disease outbreaks, Foodborne Disease Outbreak Surveillance System, 1998–2013 (n = 1775)
| Food category | Outbreaks n (%) |
Illnesses n (%) |
Hospitalizations n (%) |
Deaths n (%) |
|---|---|---|---|---|
| Fish | 387 (22) | 1532 (7) | 79 (6) | 0 (0) |
| Beef | 314 (18) | 2831 (12) | 151 (11) | 3 (38) |
| Chicken | 239 (13) | 2274 (10) | 99 (7) | 1 (13) |
| Molluscs | 147 (8) | 786 (3) | 32 (2) | 0 (0) |
| Grains/beans | 108 (6) | 602 (3) | 11 (1) | 0 (0) |
| Vegetable row crops | 97 (6) | 3378 (15) | 236 (17) | 0 (0) |
| Pork | 94 (5) | 1173 (5) | 132 (10) | 1 (12) |
| Eggs | 85 (5) | 1770 (8) | 186 (13) | 0 (0) |
| Crustaceans | 64 (4) | 537 (2) | 7 (0·5) | 0 (0) |
| Fruits | 48 (3) | 2321 (10) | 46 (3) | 1 (12) |
| Seeded vegetables | 44 (2) | 2437 (11) | 190 (14) | 0 (0) |
| Root/underground | 38 (2) | 387 (2) | 7 (0·5) | 0 (0) |
| Dairy | 34 (2) | 662 (3) | 31 (2) | 0 (0) |
| Turkey | 33 (2) | 716 (3) | 99 (7) | 2 (25) |
| Other* | 43 (2) | 1456 (6) | 78 (6) | 0 (0) |
| Total | 1775 | 22 862 | 1384 | 8 |
Other outbreak food categories were fungi (n = 5), game (n = 2), herbs (n = 10), nuts/seeds (n = 1), oils/sugars (n = 2), other meat or poultry not otherwise specified (n = 10), and sprouts (n = 13).
Aetiology
A single confirmed aetiology was reported in 3072 (31%) outbreaks; norovirus caused the most outbreaks (1425, 46%) and outbreak-associated illnesses (52630, 42%) (Table 2). The median number of ill persons in norovirus outbreaks was 14 (IQR 7–26). Most deaths were due to Salmonella infections (5/23 deaths with a reported aetiology, 22%).
Table 2.
Aetiologies in restaurant-associated foodborne disease outbreaks, Foodborne Disease Outbreak Surveillance System, 1998–2013
| Aetiology | Confirmed n (%) |
Suspected n (%) |
Total n (%) |
Median outbreak size (IQR)* |
|---|---|---|---|---|
| Norovirus | 1425 (46) | 1178 (48) | 2603 (47) | 14 (7–26) |
| Salmonella enterica | 728 (24) | 93 (4) | 821 (15) | 9 (4–20) |
| Scombroid toxin | 238 (8) | 61 (3) | 299 (5) | 2 (2–3) |
| Clostridium perfringens | 123 (4) | 240 (10) | 363 (6) | 11 (6–24) |
| Shiga toxin-producing E. coli | 117 (4) | 2 (0) | 119 (2) | 8 (4–19) |
| Shigella spp. | 76 (2) | 9 (0) | 85 (2) | 10 (5–26) |
| Staphylococcus aureus enterotoxin | 74 (2) | 287 (12) | 361 (7) | 10 (4–20) |
| Campylobacter spp. | 65 (2) | 37 (2) | 102 (2) | 6 (3–11) |
| Hepatitis virus | 50 (2) | 1 (0) | 51 (1) | 9 (6–32) |
| Bacillus cereus | 47 (2) | 298 (12) | 345 (6) | 6 (3–11) |
| Vibrio spp. | 47 (2) | 36 (1) | 83 (2) | 4 (2–5) |
| Ciguatoxin | 26 (1) | 7 (0) | 33 (1) | 4 (2–6) |
| Other† | 47 (2) | 207 (8) | 254 (4) | n.a. |
| Total | 3072 | 2456 | 5528 |
n.a., Not applicable.
Interquartile range in outbreaks with confirmed aetiologies.
Other confirmed aetiologies were amnesic shellfish poisoning (n = 1), astrovirus (n = 1), Cyclospora (n = 9), Enterococcus (n = 1), Giardia (n = 6), heavy metals (n = 2), Listeria (n = 5), monosodium glutamate (n = 1), other chemicals and toxins not otherwise specified (n = 10), pesticides (n = 3), rotavirus (n = 1), sapovirus (n = 2), Trichinella (n = 1), and Yersinia (n = 2).
Other common confirmed aetiologies were Salmonella enterica (728 outbreaks, 24%), scombroid toxin (238 outbreaks, 8%), C. perfringens (123 outbreaks, 4%), Shiga toxin-producing Escherichia coli (117 outbreaks, 4%), and Shigella (76 outbreaks, 2%) (Table 2). The percentage of restaurant-associated outbreaks caused by norovirus increased during the study period, comprising 15% of outbreaks in 1998 and 40% of outbreaks in 2013. In contrast, the second most common confirmed aetiology, Salmonella, comprised 33% of outbreaks in 1998 and 31% in 2013 (Fig. 2).
Fig. 2.
Percentage of restaurant-associated outbreaks caused by the most common confirmed aetiologies, by year, Foodborne Disease Outbreak Surveillance System, 1998–2013.
Of the 750 outbreaks with a confirmed aetiology linked to a single food category, the most common pairs were scombroid toxin in fish (219 outbreaks, 29%), S. enterica in eggs (66 outbreaks, 9%), Vibrio spp. in molluscs (33 outbreaks, 4%), C. perfringens in beef (25 outbreaks, 3%), and norovirus in vegetable row crops (22 outbreaks, 3%).
Restaurant type
Of the 1859 single restaurant-associated outbreaks reported from 2009 to 2013, 1463 (79%) were at sit-down dining establishments and 246 (13%) were at fast-food establishments. Of the 804 outbreaks with both a restaurant type and a confirmed aetiology, norovirus outbreaks associated with sit-down restaurants were most common (321, 40%) (Table 3). Of the 278 outbreaks with both an implicated food category and information on restaurant type available, fish (57 outbreaks), molluscs (38 outbreaks), and chicken (26 outbreaks) were the most common foods associated with sit-down restaurants, and vegetable row crops and sprouts were most common in fast-food restaurants (five outbreaks each) (Table 3). Certain foods were more frequently implicated in sit-down than fast-food restaurants, including eggs (8% of outbreaks in sit-down dining restaurants vs. 0% in fast-food restaurants), pork (8% vs. 4%), molluscs (18% vs. 0%), chicken (12% vs. 4%), and fish (27% vs. 16%).
Table 3.
Number of restaurant-associated foodborne disease outbreaks by food, aetiology, and restaurant type, Foodborne Disease Outbreak Surveillance System, 2009–2013
| Restaurant type, n (%) | ||||
|---|---|---|---|---|
| Sit-down | Fast-food | Other* | Total | |
| Confirmed aetiology | ||||
| Norovirus | 321 (51) | 56 (51) | 41 (65) | 418 |
| Salmonella enterica | 151 (34) | 29 (27) | 14 (22) | 194 |
| Clostridium perfringens | 17 (3) | 1 (1) | 1 (2) | 19 |
| Scombroid toxin | 36 (6) | 4 (4) | 1 (2) | 41 |
| Shiga toxin-producing E. coli | 27 (4) | 9 (8) | 1 (2) | 37 |
| Campylobacter spp. | 20 (3) | 0 (0) | 1 (2) | 21 |
| Vibrio spp. | 16 (3) | 0 (0) | 1 (2) | 17 |
| Ciguatoxin | 10 (2) | 0 (0) | 1 (2) | 11 |
| Shigella spp. | 6 (1) | 4 (4) | 0 (0) | 10 |
| Bacillus cereus | 6 (1) | 2 (2) | 0 (0) | 8 |
| Staphylococcus enterotoxin | 4 (1) | 0 (0) | 1 (2) | 5 |
| Hepatitis | 2 (0) | 3 (3) | 0 (0) | 5 |
| Other† | 16 (3) | 1 (1) | 1 (2) | 18 |
| Total | 632 | 109 | 63 | 804 |
| Food category | ||||
| Fish | 57 (24) | 4 (16) | 3 (17) | 64 |
| Molluscs | 38 (16) | 0 (0) | 1 (6) | 39 |
| Chicken | 26 (11) | 1 (4) | 1 (6) | 28 |
| Vegetable row crops | 18 (8) | 5 (20) | 2 (11) | 25 |
| Beef | 21 (9) | 2 (8) | 0 (0) | 23 |
| Grains/beans | 20 (9) | 2 (8) | 0 (0) | 22 |
| Pork | 16 (7) | 1 (4) | 2 (11) | 19 |
| Eggs | 16 (7) | 0 (0) | 1 (6) | 17 |
| Sprouts | 1 (0) | 5 (20) | 1 (6) | 7 |
| Fruits | 5 (2) | 0 (0) | 1 (6) | 6 |
| Seeded vegetables | 2 (1) | 2 (8) | 1 (6) | 5 |
| Other‡ | 15 (6) | 3 (12) | 5 (28) | 23 |
| Total | 235 | 25 | 18 | 278 |
Other (e.g. mall food court, stand-alone deli, banquet) or unknown restaurant type.
Other confirmed etiologies were amnesic shellfish poisoning (n = 1), Cyclospora (n = 2), Enterococcus (n = 1), Giardia (n = 1), Listeria (n = 1), other chemicals and toxins not otherwise specified (n = 1), pesticides (n = 2), sapovirus (n = 2), and Trichinella (n = 1).
Other outbreak food categories were crustaceans (n = 3), dairy (n = 3), fungi (n = 1), herbs (n = 1), nuts/seeds (n = 1), other meat or poultry not otherwise specified (n = 6), root/underground (n = 4), and turkey (n = 4).
Outbreak contributing factors
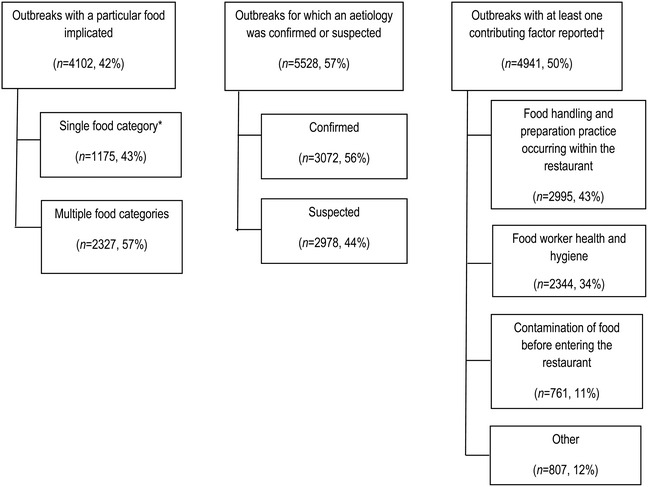
In the 9788 restaurant-associated outbreaks, 4941 (50%) outbreaks contained information on at least one contributing factor, with a total of 6907 contributing factors recorded (Appendix A). The most common were those related to food handling and preparation practices in the restaurant (2995 outbreaks, 61% of those with any contributing factor recorded) followed by those related to food worker health and hygiene (2344 outbreaks, 47%). Factors related to food contamination before reaching the restaurant (761 outbreaks, 15%) were less common.
The most common outbreak contributing factors related to food handling and preparation practices in the restaurant were improper adherence of an approved plan to use time as a public health control (962 outbreaks, 32%), inadequate or insufficient thawing of frozen products leading to the proliferation of pathogens (957 outbreaks, 32%), and cross-contamination by a non-food handler who was suspected of being infectious (954 outbreaks, 32%).
In the 1875 outbreaks with a confirmed aetiology and contributing factor information available, Salmonella was the most common confirmed aetiology in outbreaks in which food contamination before entering the restaurant was cited as a contributing factor [157 (33%) outbreaks of 481] and food handling and preparation practices in the restaurant was cited as a contributing factor [341 (40%) of 861 outbreaks]. Norovirus was the most common confirmed aetiology in outbreaks in which contamination related to food worker health and hygiene was cited as a contributing factor [706 (71%) of 997 outbreaks] and other contamination methods [68 (27%) of 253 outbreaks].
Scombroid toxin in fish was the most common food-aetiology pair in outbreaks with a confirmed aetiology related to contamination of food before reaching the restaurant (136 outbreaks), outbreaks related to food handling and preparation practices occurring within the restaurant (75 outbreaks), and outbreaks related to other contributing factors (33 outbreaks). Norovirus in vegetable row crops was the most common food-aetiology pair in outbreaks with a confirmed aetiology related to food worker health and hygiene (15 outbreaks).
Implication of food workers
Food workers were implicated as the source in 2344 (24%) of the 9788 outbreaks. The median size of outbreaks in which a food worker was implicated was eight ill persons (IQR 4–20), compared to a median of four (IQR 2–9) for all other outbreaks (P < 0·001).
A single food category was identified in 1372 (59%) of 2344 outbreaks involving a food worker, most commonly beef (62 outbreaks), chicken (45 outbreaks), and vegetable row crops (41 outbreaks). Most outbreaks where food workers were implicated occurred in sit-down restaurants [274 (82%) out of 336 outbreaks since 2009].
Information was available on a confirmed aetiology for 1131 of the 2344 outbreaks involving food workers. Norovirus was the most frequent cause (794 outbreaks, 70% of outbreaks involving a food worker), followed by S. enterica (191 outbreaks, 17%), and Staphylococcus aureus enterotoxin (35 outbreaks, 3%). The Salmonella serotypes most commonly implicated in food worker-associated outbreaks were Enteritidis (60 outbreaks), Typhimurium (26 outbreaks), Heidelberg (18 outbreaks), and Newport (14 outbreaks).
DISCUSSION
This study highlights the significant burden of foodborne disease outbreaks that occur in restaurants in the United States. Over half of all foodborne disease outbreaks reported to the CDC from 1998 to 2013 involved a restaurant setting.
We found that factors related to food handling and preparation practices in restaurants, including inadequate thawing resulting in pathogen proliferation and cross-contamination were the most frequent contributors to restaurant outbreaks. Food workers have reported that obstacles such as sink accessibility and clean cutting board availability, time demands, restaurant management and coworker influence, and lack of food-safety training and procedures, all negatively impact their ability to safely prepare foods in accordance with guidelines and regulations [12] and are likely reasons for food preparation lapses. Of these outbreaks with contributing factors related to food handling and preparation in the restaurant, Salmonella was the most common confirmed aetiology. This likely indicates that food enters the restaurant contaminated (i.e. poultry contaminated with Salmonella) and proper procedures are not followed to eliminate this organism once in the restaurant. Although the FDA Food Code was established to minimize five major risk factors in restaurant-associated foodborne illness, including improper holding temperatures, inadequate cooking, contaminated equipment, obtaining food from unsafe sources, and poor personal hygiene [7], obstacles to implementing and following these guidelines must be addressed.
We found that food workers contributed to a quarter of all restaurant-associated outbreaks, and outbreaks associated with food workers tended to be larger than others. This underscores the role of food worker health and hygiene and safe food preparation practices in restaurant settings in foodborne illness prevention. Food workers can contribute to food contamination by failing to adhere to safe food preparation time and temperature guidelines, directly introducing pathogens while preparing food when ill, or cross-contaminating ready-to-eat foods or cooked foods with raw food [12–14]. A recent survey of restaurant food workers found that most lacked knowledge about foodborne disease prevention, including correct handwashing technique, proper food storage, adequate meat temperatures, and how to tell if food has gone bad [14]. Food workers report not always wearing gloves while handling ready-to-eat foods and not changing gloves in between handling raw meat and ready-to-eat foods [15]. Inadequate handwashing is a well-established method for spreading illness [7]; food workers are less likely to practice appropriate handwashing when they are busy [14]. In an observational study assessing food workers' handwashing frequency, hands were washed only 39 (7%) of the 582 times they should have been washed. Hands were not washed after touching aprons, and rarely when changing tasks or handling different food products. Moreover, compliance with the FDA Food Code handwashing guideline was extremely low (5%) [16]. A survey from 2010 revealed that close to 88% of restaurant workers do not receive paid sick days and over 63% had cooked or served food while sick [17]. Moreover, one-third of restaurants do not have clear policies about when to allow a sick food worker to work and 20% of food workers went to work while ill at least once in the previous year [5, 17].
An implicated food was not reported in half of restaurant-associated outbreaks. This is in part because linking a food to an outbreak is often difficult, as it requires identifying a common food exposure. Ill persons may have many common exposures, making it difficult to distinguish which food item caused the outbreak. In outbreaks in which an implicated food was identified, half were linked to complex foods in which an ingredient in a single food category could not be identified. This is likely due to the inherent difficulty in determining the causative food category in a complex food consumed by many people. In some outbreaks, more than one food category may be responsible for illness (i.e. contamination of several food items by ill workers, or cross-contamination).
Overall, over 70% of outbreaks were due to animal-based foods (meat and seafood items). Animal-based foods were also more commonly implicated in sit-down restaurants (67% of outbreaks) than fast food restaurants (32% of outbreaks). Many animal-based food types are likely inherently contaminated before consumption and temperature abuse can lead to bacterial proliferation and toxin production. Appropriate cooking practices, including cooking to the appropriate internal temperature and limiting time at room temperature are imperative to decrease pathogen burden or toxin production before serving.
Nearly half of restaurant-associated outbreaks were caused by norovirus, including most food worker-associated outbreaks. Detection of norovirus outbreaks has increased since the 1990s, likely due in part to improved and more widely used molecular diagnostics, including real-time reverse transcription–polymerase chain reaction assays and sequence analysis [18, 19]. Norovirus outbreaks were also larger than those caused by other pathogens. This is likely due in part to norovirus' high infectivity and low infectious dose (as few as 18 viral particles may cause illness) [20]. Norovirus was the most common aetiology in outbreaks linked to vegetable row crops, foods that are commonly eaten raw and may not undergo a heat step to kill pathogens. Outbreaks due to food contaminated with norovirus during production (i.e. before arriving at the restaurant) are rarely identified [19, 21]. Consistently, our study found that most restaurant-associated norovirus outbreaks were associated with food worker health and hygiene lapses during food preparation or serving. A study reported that restaurants with certified kitchen managers have fewer food contamination events and fewer norovirus outbreaks [22], suggesting that this may be an important intervention.
Scombroid toxin (histamine) was the third most common aetiology identified and was most commonly associated with consumption of fish. Although the median outbreak size involving scombroid toxin was small, it is likely that illness from scombroid toxin is under-recognized since the clinical presentation is similar to an allergy [23]. Cooking contaminated foods does not destroy histamine [23], highlighting the importance of proper handling at the source. Over 85% of fish consumed in the United States is imported [24], and ensuring immediate freezing of raw fish after initial catch and proper storage during transport is crucial to prevent foodborne illness.
Norovirus, B. cereus, Staphylococcus aureus enterotoxin, and C. perfringens were the most common suspect aetiologies in restaurant-associated foodborne disease outbreaks. Since most outbreaks caused by these pathogens are short and illness is self-limited, it is often difficult to confirm the aetiology if ill persons do not seek care or if clinical specimens are not tested. In these instances, epidemiologists may assess the clinical syndrome, incubation period, food category, and outbreak setting and designate a suspect aetiology [25].
We found that more outbreaks occurred in sit-down restaurants than fast-food restaurants. There may be several explanations for this observation. First, different food types are prepared differently, for example, sit-down restaurants traditionally have a ‘cook-to-order’ option in comparison to standard cooking protocols in fast-food restaurants. ‘Cook-to-order’ food may be more prone to preparation errors, predisposing consumers to foodborne illness. Second, a customer may be more likely to consume raw or undercooked products at a sit-down restaurant, including raw fish, oysters, beef, or eggs. Third, outbreaks in sit-down restaurants might be more likely to be detected because food is usually consumed in group settings, thus more easily allowing ill persons to be identified and linked epidemiologically. Last, many fast-food restaurants have standardized cooking and supplier guidelines as a result of previous high-profile outbreaks; a decrease in the number of outbreaks in this setting may be a direct result of practice improvements.
In 2009, the surveillance system for foodborne disease outbreaks transitioned to a new electronic reporting platform and subsequently the total number of foodborne disease outbreaks decreased. A survey suggested that this overall decline in foodborne outbreaks was due to decreased resources available for outbreak detection during the influenza A(H1N1) epidemic and a surveillance artifact [26], given that the percentage of aetiologies and food categories did not change. In our study, the percentage of foodborne outbreaks that were restaurant-associated outbreaks declined annually since 2002, but has averaged 55% throughout the study period. Also, the percentage of illnesses associated with restaurant-associated foodborne outbreaks did not change dramatically over the study period (range 7–9%). The decrease in restaurant-associated outbreaks may be due to improved food handling practices and improved restaurant guidance to prevent foodborne illness or more outbreaks in multiple states are being identified as part of a single, multistate outbreak.
This study has a few limitations. The surveillance system relies on reporting and outbreak investigations by state, local, and territorial public health departments. Changes in the surveillance system, described above, may have contributed to the decrease in the number of outbreaks reported to CDC the health departments that year. Restaurant-related regulations and resources to perform outbreak investigations vary by state, and within a state can vary by jurisdiction. Results might have been influenced by states that receive more funding or resources or have larger populations. Restaurant-associated outbreaks may also be inherently more likely to be reported than other outbreaks.
Knowledge of the foods, aetiologies, and contributing factors that result in restaurant outbreaks can help guide efforts to prevent foodborne illness. Given that the majority of outbreaks were in sit-down restaurants and involved food preparation practices in the restaurant, more work needs to be done to address this issue. Emphasis must be placed on continued education, including refresher trainings for kitchen and serving staff including demonstrations of food-safety knowledge, effective management and appropriate restaurant practices oversight including having a trained manager on duty at all times, implementation of employee health controls including policies during illness and an emphasis on appropriate handwashing, and strict adherence to all food code guidelines.
ACKNOWLEDGEMENTS
We acknowledge the local, state, and territorial public health departments who report their outbreaks to CDC and the FDOSS surveillance team for their database management and expertise. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of CDC. This study received no financial support.
APPENDIX A
Categories used for analysis of contributing factors in restaurant-associated foodborne disease outbreaks, Foodborne Disease Outbreak Surveillance System, 1998–2013* (n = 6907 contributing factors)
| Category | Contributing factors 1998–2008 |
Contributing factors 2009–2012 |
No. of outbreaks (%) |
|---|---|---|---|
| Bare-handed contact by handler/worker/preparer (e.g. with ready-to-eat food) | Bare-hand contact by a food handler/worker/preparer who is suspected to be infectious | 1451 (62) | |
| Food worker health & hygiene | Handling by an infected person or carrier of pathogen (e.g. Staphylococcus, Salmonella, norovirus) | Other mode of contamination (excluding cross-contamination) by a food handler/worker/preparer who is suspected to be infectious | 1073 (46) |
| Glove-handed contact by handler/worker/preparer (e.g. with ready-to-eat food) | Glove-hand contact by a food handler/worker/preparer who is suspected to be infectious | 463 (20) | |
| Any of the above | 2344 (34) | ||
| Raw product/ingredient contaminated by pathogens from animal or environment (e.g. Salmonella Enteriditis in egg, norovirus in shellfish, E. coli in sprouts) | Contaminated raw product – food was intended to be consumed after a kill step | 396 (52) | |
| Contamination of food before reaching the restaurant | Toxic substance part of tissue (e.g. ciguatera) | Toxic substance part of the tissue | 220 (29) |
| Ingestion of contaminated raw products (e.g. raw shellfish, produce, eggs) | Contaminated raw product – food was intended to be served raw or undercooked/under processed | 187 (29) | |
| Obtaining foods from polluted sources (e.g. shellfish) | Foods originating from sources shown to be contaminated or polluted (such as a growing field or harvest area) | 22 (3) | |
| Any of the above | 761 (11) | ||
| Improper adherence of approved plan to use time as a public health control | 962 (32) | ||
| Inadequate thawing of frozen products (e.g. room thawing) | Food preparation practices that support proliferation of pathogens (during food preparation) | ||
| Insufficient thawing, followed by insufficient cooking (e.g. frozen turkey) | 957 (32) | ||
| Foods contaminated by a non-food handler/worker/preparer who is suspected to be infectious | 954 (32) | ||
| Cross-contamination from raw ingredient of animal origin (e.g. raw poultry on the cutting board) | Cross-contamination of ingredients (cross-contamination does not include ill food workers) | 710 (24) | |
| Preparing foods a half day or more before serving (e.g. banquet preparation a day in advance) | No attempt was made to control the temperature of implicated food or the length of time food was out of temperature control (during food service or display of food) | 566 (19) | |
| Insufficient time and/or temperature during hot holding (e.g. malfunctioning equipment, too large a mass of food) | Improper hot holding due to malfunctioning equipment | 426 (14) | |
| Insufficient time and/or temperature during initial cooking/heat processing (e.g. roasted meats/poultry, canned foods, pasteurization) | Insufficient time and/or temperature control during initial cooking/heat processing | 382 (13) | |
| Food handling and preparation practices in the restaurant | Inadequate cold-holding temperatures (e.g. refrigerator inadequate/not working, ice holding inadequate) | Improper cold holding due to malfunctioning refrigeration equipment | 311 (10) |
| Insufficient time and/or temperature during reheating (e.g. sauces, roasts) | Insufficient time and/or temperature during reheating | 303 (10) | |
| Storage in contaminated environment B leads to contamination of vehicle (e.g. store room, refrigerator) | Storage in contaminated environment | 268 (9) | |
| Improper cold holding due to an improper procedure or protocol | 110 (4) | ||
| Allowing foods to remain at room or warm outdoor temperature for several hours (e.g. during preparation or holding for service) | Improper hot holding due to improper procedure or protocol | 72 (2) | |
| Slow cooling (e.g. deep containers or large roasts) | Improper/slow cooling | 61 (2) | |
| Insufficient or improper use of chemical processes designed for pathogen destruction | 44 (1) | ||
| Prolonged cold storage for several weeks (e.g. permits slow growth of psychrophilic pathogens) | Prolonged cold storage | 35 (1) | |
| Anaerobic packaging/modified atmosphere (e.g. vacuum packed fish, salad in gas flushed bag) | Inadequate modified atmosphere packaging | 7 (0) | |
| Insufficient time and/or temperature control during freezing | 5 (0) | ||
| Inadequate acidification (e.g. mayonnaise, tomatoes canned) | Inadequate processing (acidification, water activity, fermentation) | ||
| Inadequate fermentation (e.g. processed meat, cheese) | 4 (0) | ||
| Insufficiently low water activity (e.g. smoked/salted fish) | |||
| Insufficient acidification (e.g. home canned foods) | |||
| Any of the above | 2995 (43) | ||
| Other source of contamination | Other source of contamination | 475 (59) | |
| Other process failures that permit the agent to survive | Other process failures that permit the agent to survive | 246 (30) | |
| Other | Other situations that promote or allow microbial growth or toxic production | Other situations that promote or allow microbial growth or toxic production | 130 (16) |
| Toxic container of pipelines (e.g. galvanized containers with acid food, copper pipe with carbonated beverages) | Toxic container | 15 (2) | |
| Poisonous substance intentionally added (e.g. cyanide or phenolphthalein added to cause illness) | Poisonous substance intentionally/deliberately added | 9 (1) | |
| Addition of excessive quantities of ingredients that are toxic under these situations (e.g. niacin poisoning in bread) | Addition of excessive quantities of ingredients that are toxic in large amounts | 4 (1) | |
| Poisonous or physical substance accidentally/incidentally added (e.g. sanitizer or cleaning compounds | Poisonous substance accidentally/inadvertently added | 2 (0) | |
| Any of the above | 807 (12) | ||
Contributing factor definitions were revised in 2009 and outbreaks may be listed under more than one factor.
APPENDIX B
Foodborne disease outbreaks associated with a restaurant setting, Foodborne Disease Outbreak Surveillance System, 1998–2013 (n = 9788)
 |
* Foods were classified according to the Interagency Food Safety Analytics Collaboration's (IFSAC) scheme and include the following categories: dairy, eggs, fish, fruits, fungi, game, grains-beans, herbs, meat (e.g. beef, pork), oils/sugars, nuts/seeds, poultry (e.g. chicken, turkey), shellfish (e.g. crustaceans, molluscs), sprouts, vegetables (e.g. root-underground, seeded, vegetable row crops), and other poultry or meat.
† More than one contributing factor categories may be reported.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Scallan E, et al. Foodborne illness acquired in the United States – major pathogens. Emerging Infectious Diseases 2011; 17: 7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Surveillance for foodborne disease outbreaks – United States, 1998–2008. Morbidity and Mortality Weekly Report 2013; 62: 1–34. [PubMed]
- 3.Hoffman S, Maculloch B, Batz M. Economic burden of major foodborne illnesses acquired in the United States, EIB-140, United States Department of Agriculture, Economic Research Service (http://www.ers.usda.gov/media/1837791/eib140.pdf). Accessed 15 September 2015.
- 4.Centers for Disease Control and Prevention. Surveillance for foodborne disease outbreaks, United States, 2013. (http://www.cdc.gov/foodsafety/pdfs/foodborne-disease-outbreaks-annual-report-2013-508c.pdf). Accessed 8 December 2015.
- 5.Sumner S, et al. factors associated with food workers working while experiencing vomiting or diarrhea. Journal of Food Protection 2011; 74: 215–220. [DOI] [PubMed] [Google Scholar]
- 6.National Restaurant Association. 2015. Restaurant industry pocket factbook (http://www.restaurant.org/Downloads/PDFs/News-Research/research/Factbook2015_LetterSize-FINAL.pdf). Accessed 15 September 2015.
- 7.U.S. Department of Health and Human Services. Food Code (http://www.fda.gov/downloads/Food/GuidanceRegulation/RetailFoodProtection/FoodCode/UCM374510.pdf). Accessed 15 September 2015.
- 8.Centers for Disease Control and Prevention. National Outbreak Reporting System (http://www.cdc.gov/nors/about.html). Accessed 10 September 2015.
- 9.Centers for Disease Control and Prevention. Interagency Food Safety Analystics Collaboration (IFSAC) (http://www.cdc.gov/foodsafety/ifsac/projects/food-categorization-scheme.html). Accessed 18 September 2015.
- 10.Centers for Disease Control and Prevention. Guide to confirming an etiology in a foodborne disease outbreak (http://www.cdc.gov/foodsafety/outbreaks/investigating-outbreaks/confirming_diagnosis.html). Accessed 21 June 2016.
- 11.Centers for Disease Control and Prevention. National outbreak reporting system guidance document (http://www.cdc.gov/outbreaknet/pdf/NORS_Guidance_5213_06232009(compliant).pdf). Accessed 27 September 2015.
- 12.Green L, Selman C. Factors impacting food workers’ and managers’ safe food preparation practices: a qualitative study. Food Protection Trends 2005; 25: 981–990. [Google Scholar]
- 13.DeBess EE, et al. Food handler assessment in Oregon. Foodborne Pathogenesis and Disease 2009; 6: 329–335. [DOI] [PubMed] [Google Scholar]
- 14.Green L, et al. Factors related to food workers hand hygiene practices. Journal of Food Protection 2007; 70: 661–666. [DOI] [PubMed] [Google Scholar]
- 15.Green L, et al. Food service workers self-reported food preparation practices: an EHS-Net study. International Journal of Hygiene and Environmental Health 2005; 208: 27–35. [DOI] [PubMed] [Google Scholar]
- 16.Strohbehn C, et al. Hand washing frequencies and procedures used in retail food services. Journal of Food Protection 2008; 71: 97–106. [DOI] [PubMed] [Google Scholar]
- 17.Norton DM, et al. Managerial practices regarding workers working while ill. Journal of Food Protection 2015; 78: 187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Diagnostic methods for norovirus (http://www.cdc.gov/norovirus/lab-testing/diagnostic.html) Accessed 22 December 2015.
- 19.Hall AJ, et al. Epidemiology of foodborne norovirus outbreaks, United States, 2001–2008. Emerging Infectious Diseases 2013; 18: 1566–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Teunis PF, et al. Norwalk virus: how infectious is it? Journal of Medical Virology 2008; 80: 1468–1476. [DOI] [PubMed] [Google Scholar]
- 21.Hall AJ, et al. Vital signs: foodborne norovirus outbreaks – United States, 2009–2012. Morbidity and Mortality Weekly Report 2014; 63: 491–495. [PMC free article] [PubMed] [Google Scholar]
- 22.Hedberg CW, et al. Systematic environmental evaluations to identify food safety differences between outbreak and nonoutbreak restaurants. Journal of Food Protection 2006; 69: 697–702. [DOI] [PubMed] [Google Scholar]
- 23.Food and Drug Administation. Scombrotoxin poisoning and decomposition (http://www.fda.gov/food/foodborneillnesscontaminants/buystoreservesafefood/ucm335658.htm).
- 24.National Oceanic and Atmospheric Administration. Commercial fisheries statistics (http://www.st.nmfs.noaa.gov/commercial-fisheries/fus/fus14/index). Accessed 31 August 2016.
- 25.Bennett SD, Walsh K, Gould LH. Foodborne Disease Outbreaks caused by Bacillus cereus, Clostridium perfringens, and Staphylococcus aureus, United States, 1998–2008. Clinical Infectious Diseases 2013; 57: 425–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Imanishi M, et al. Factors Contributing to Decline in Foodborne Disease Outbreak Reports, United States. Emerging Infectious Diseases 2014; 20: 1551–1553. [DOI] [PMC free article] [PubMed] [Google Scholar]




