Abstract
Background
The dynamic COVID-19 pandemic has been associated with mental strain. However, most studies focused primarily on the beginning of the pandemic and rarely took into account the long-term course. The aim of this prospective-longitudinal study was to investigate levels and changes of pandemic-related fears, unspecific anxiety, depressive symptoms, and psychosocial-behavioral factors over the first 1.5 years of the pandemic.
Methods
We conducted a nine-wave longitudinal online-survey from March 2020 to October 2021 with a total of 8148 participants of the adult general population in Germany. Descriptive examination and multilevel analysis were carried out to assess psychological burden, risk-bearing and protective psychosocial-behavioral factors, and associations with sociodemographics and the pandemic's duration and severity over the course of the pandemic.
Results
Symptoms of mental strain fluctuated across the pandemic and displayed a relative maximum at the pandemic's early beginning and during the second and third COVID-19 waves. Most participants (approximately 67.4 %–82.1 %) reported mild and transient symptoms, but a substantial portion (approximately 17.9 %–32.6 %) experienced pronounced mental health problems during the pandemic. Symptom severity was negatively associated with the duration of the pandemic and positively associated with the rate of new infections.
Limitations
The observational study design, non-probability-sampling methods, and online self-report assessments limit the generalizability of our results.
Conclusions
The fluctuating course of psychological burden during the pandemic emphasizes the relevance of continuous monitoring during this challenging time. Particularly individuals with pronounced subclinical symptoms or manifesting mental disorders should be targeted with adequate prevention and early intervention programs.
Keywords: Corona, SARS-CoV-2, Anxiety, Fear, Depression, Distress
1. Introduction
The ongoing pandemic of the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), respectively the coronavirus disease 19 (COVID-19), was paralleled by concerns regarding its short-, mid-, and long-term impacts on the mental health of populations worldwide (Robinson et al., 2022; Santomauro et al., 2021; Schafer et al., 2022). The striving for assessing and investigating pandemic-related psychopathological symptoms by researchers all over the world has led to a large but vastly heterogenous body of evidence (Rzymski et al., 2020; Schafer et al., 2022; Sousa et al., 2021).
At the beginning of the pandemic, most studies observed elevated levels of anxiety, depressive symptoms, distress, sleep issues, symptoms of eating disorders, and posttraumatic stress symptoms compared to actually measured or estimated pre-pandemic levels (Cénat et al., 2021; Necho et al., 2021; Schafer et al., 2022; Sheek-Hussein et al., 2021; Sousa et al., 2021). Findings on changes in the following months of the pandemic were highly heterogeneous and indicated either a symptom decrease, stagnation, or symptom increase (Robinson et al., 2022). Based on the existing research, conclusions about long-term symptom changes more than one year after the beginning of the COVID-19 pandemic are difficult to draw because most evidence stems from cross-sectional studies at the early beginning of the pandemic that do not take into account symptom trajectories over time and due to changes of the pandemic situation itself (e.g., due to fluctuating infection rates) (Sousa et al., 2021). Therefore, ongoing longitudinal monitoring of the further progress of anxiety, depressive, and other symptoms during the pandemic is of high relevance.
Several studies tried to extrapolate results from previous (health-related) crises as well as first results from the early COVID-19 pandemic to predict further changes of mental health burden (Fan et al., 2021; Santomauro et al., 2021). In this context, it was assumed that not only psychopathological symptoms would increase but also the prevalence rates of full-threshold mental disorders (Bohlken et al., 2021; Santomauro et al., 2021). For example, based on a systematic review, Santomauro et al. (2021) estimated a global increase in anxiety disorders of 76.2 million (25.6 % increase) and an increase in major depressive disorders of 53.2 million (27.6 % increase) due to the COVID-19 pandemic. Such predictions are prone to imprecision and uncertainty; nevertheless, they highlight the need for assessing psychopathological symptom changes as well as the incidence and persistence of mental disorders during this challenging time. It can be expected that potential changes in the incidence of full-threshold mental disorders only become evident in the longer run with a distinct delay (Bohlken et al., 2021), which again emphasizes the need for ongoing assessments.
Besides the importance of continuously assessing pandemic-related psychopathological symptoms, it is crucial to examine factors related to elevated symptoms (Bendau et al., 2020; Bueno-Notivol et al., 2021; Kunzler et al., 2021). Most research on risk-bearing and protective factors focused on sociodemographic variables (e.g., age, gender, and socioeconomic status) and was carried out during the first months of the pandemic (Dragioti et al., 2022; Kunzler et al., 2021; Rodríguez-Fernández et al., 2021). Only a few studies have investigated potentially modifiable variables, such as self-efficacy and health-related behaviors (Bendau et al., 2020; Bendau et al., 2021b; Pandey et al., 2021; Petzold et al., 2020a; Villadsen et al., 2021). Moreover, most research considered risk and resilience factors as relatively stable variables and there is scarce evidence regarding potential changes of those factors over the course of the pandemic.
Our nine-wave prospective-longitudinal study aims to close these research gaps by longitudinally examining the course of symptoms of mental strain (pandemic-related anxiety and fears, the cognitive preoccupation with the pandemic, the perceived risk of infection and broader parameters of unspecific generalized anxiety and depressive symptoms) over the first 1.5 years of the COVID-19 pandemic in Germany. Specifically, longitudinal changes of anxiety and depressive symptoms as a function of time and pandemic-related factors (e.g., fluctuating infection rates) are analyzed. In addition, changes in risk-bearing and protective factors are investigated.
2. Methods
2.1. Study design
Data was obtained by a nine-wave longitudinal community study from the beginning of the pandemic in March 2020 to 1.5 years later in October 2021 (Bendau, 2022; Bendau et al., 2021a; Petzold et al., 2020a). A non-probability convenience sample (N = 8148) of the adult general population in Germany took part in the online survey via the secured platform SoSci-Survey at up to nine assessments. Fig. 1 depicts the nine assessment periods and essential information about the dynamic pandemic situation in Germany during the time frame of this research project.
Fig. 1.
Overview of the nine periods of data collection, the daily SARS-CoV-2 infection rate and pandemic-related events in Germany (Bendau, 2022; Bendau et al., 2020; WHO, 2022).
Note. Number of participants at each assessment period: T1: 5114, T2: 2567, T3: 1641, T4: 1411, T5: 1405, T6: 2225, T7: 1752, T8: 1578, T9: 1336. Of the total sample of N = 8148 individuals, 60.2 % (n = 4903) participated in one, 10.8 % (n = 877) in two, 7.8 % (n = 639) in three, 5.3 % (n = 432) in four, 4.1 % (n = 333) in five, 3.6 % (n = 291) in six, 2.9 % (n = 238) in seven, 3.3 % (n = 265) in eight and 2.1 % (n = 170) in all nine waves of data collection.
Recruitment for first participation was done via news portals, social media channels (Twitter, Instagram, Facebook), and the homepage of the Charité – Universitätsmedizin Berlin (Bendau, 2022; Bendau et al., 2021a). After their first participation, participants who had given consent to be contacted for follow-ups received emails with invitations for the further assessment waves. They were free to choose which and how many measurement waves they participated in—therefore, the number of completed waves varies interpersonally (see Fig. 1). Data assessment was fully anonymous; data were stored separately from contact information (email addresses) and merged via anonymous codes on the participant level.
The research project was approved by the ethics committee of the Charité – Universitätsmedizin Berlin (EA1/071/20) and pre-registered at clinicaltrials.gov (NCT04331106). Before participation, all participants gave written informed consent. No financial or material incentives were given for the participation. Applied eligibility criteria were a minimum age of 18 years, current place of residence in Germany, and a sufficient level of German language proficiency.
2.2. Assessment
At all periods of data collection, the same self-report survey questionnaire was used (except that some additional items were added in the further progress of the pandemic and detailed sociodemographic information was only obtained at the first participation) (Bendau, 2022; Bendau et al., 2020; Bendau et al., 2021a; Petzold et al., 2020a).
Pandemic-related information was examined with binary (yes/no) items regarding quarantine, infections with SARS-CoV-2, vaccination status, etc. The subjective risk of an infection with SARS-CoV-2 within the next month was rated from 0 to 100 %.
Symptoms of anxiety related to the pandemic were assessed with the ten-item COVID-19-Anxiety Questionnaire (C-19-A; Petzold et al., 2020b). Its sum score ranges from 0 to 40 and higher values indicate stronger anxiety symptoms. Additionally, from the fifth assessment wave (T5) on, the retrospective rating of pandemic-related mental strain was obtained on a 10-point scale for every month of the pandemic. Nine self-created items (answered on a 6-point Likert-scale from 1 “not true at all” to 6 “totally true”) differentiated concerns and fears regarding the pandemic (e.g., targeting health-related, social, and economic fears) (Bendau et al., 2020; Petzold et al., 2020a). Using the same Likert-scale, eight items assessed potential protective variables and five items risk factors.
The dimensional presence of symptoms of unspecific/generalized anxiety (PHQ-2) and depression (GAD-2) were obtained by these two subscales of the validated Patient Health Questionnaire-4 (PHQ-4; Löwe et al., 2010). Each subscale consists of two items whose intensity is rated on a 4-point Likert-scale from 0 “not at all” to 3 “nearly every day”. A subscale sum score of ≥3, respectively a total score of ≥6, is classified as alarming symptom severity.
2.3. Data analysis
Descriptive analyses were carried out with IBM SPSS Version 26. Stata 15 was used to perform multilevel analyses with measurement occasions (Level 1) nested within persons (Level 2). We built a separate model for each symptom outcome (C-19-A, PHQ-4, PHQ-2, and GAD-2) and modelled the effects as fixed effects. The alpha level was set at 0.05.
Specifically, we regressed the standardized score of the respective symptom outcome (C-19-A, PHQ-4, PHQ-2, or GAD-2) on gender (Level 2; female (reference group), male, and diverse), age (Level 2; in years), a timing variable (Level 1), and a variable “number of infections” (Level 1) as multiple predictors.
The timing variable was used to test whether the respective symptom outcome increased or decreased gradually over time. It was coded with the number of days from the first day of the baseline assessment (T1) until the first day of the respective follow-up assessment (T2–T9) to indicate how the nine waves were temporally related. Specifically, it was coded with 0 at T1, 28 at T2, 49 at T3, 70 at T4, 182 at T5, 210 at T6, 280 at T7, 364 at T8, and 546 at T9.
The “number of infections” variable was used to test whether the respective symptom outcome varied by the COVID-19 infection rates at the respective time point. It was coded with the number of incident COVID-19 cases in Germany at the first day of the respective assessment wave as indicated by the official nowcast registers of the Robert-Koch-Institute (Robert Koch Institut, 2021). Specifically, it was coded with 4122 at T1, 1146 at T2, 678 at T3, 319 at T4, 2159 at T5, 15,853 at T6, 15,010 at T7, 16,349 at T8, and 7634 at T9.
To avoid the b-coefficients becoming too small to be displayed rounded to two decimal places, the timing variable was divided by 100 and the “number of infections” variable was divided by 1000 for the analyses.
3. Results
3.1. Sample characteristics
Of the total sample of 8148 participants, 71.7 % (n = 5845) identified as female, 27.6 % (n = 2245) as male, and 0.7 % (n = 58) as diverse. On average, participants were aged 37.47 years (SD = 12.00; range 18–99) when participating in the study for the first time. The majority had a university degree (52.7 %, n = 4295) or higher education entrance qualification (29.9 %, n = 2433). A secondary school degree or lower was reported by 16.3 % (n = 1333). A total of 18.9 % (n = 1541) was working in health care settings and 9.5 % (n = 776) reported having a severe physical illness.
3.2. Exposure to COVID-19
The proportion of participants knowing people who had been infected with SARS-CoV-2 grew continuously over the course of the study (from 26.8 % at T1 to 83.1 % at T9). In parallel, the small percentage of participants who experienced an infection themselves increased slightly (from 0.9 % at T1 to 5.6 % at T9). The percentage of individuals under quarantine ranged from 7.1 % at T1 to 0.9 % at T4 (T2: 2.8 %; T3: 1.7 %; T5: 1.4 %; T6: 3.2 %; T7: 2.5 %; T8: 2.1 %; T9: 1.1 %). At T8, approximately one quarter (24.3 %) had received at least one vaccination. At T9, this was true for nearly all participants (95.3 %).
3.3. Psychosocial-behavioral factors over the course of the pandemic
Table S1 shows the average expression of five potentially beneficial psychosocial-behavioral factors (self-efficacy; maintaining social contacts; acceptance/normalization of feelings; knowledge of where to get medical support; knowledge of where to get psychological support) and four factors of risk (suppression of negative feelings; reduced physical activity; unhealthy diet; increased substance use) at the nine measurement periods. All observed factors seem to be rather stable over time. On average, our sample scored rather high on the beneficial and low on the risk-bearing factors. Compared to the other risk factors, a reduced physical activity was the most frequently expressed risk factor.
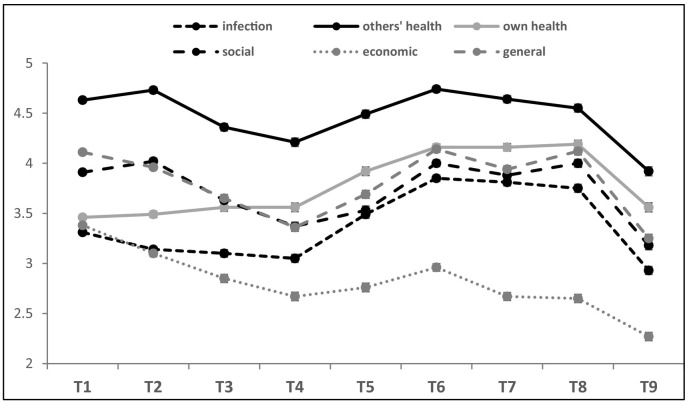
3.4. Pandemic-related fears
In terms of pandemic-related fears (Fig. 2), worries about the health of loved ones in case of an infection were most pronounced, followed by fears of negative consequences for one's own health and negative social consequences (e.g., less contact to family and friends). Changes in fears of social consequences and consequences in general corresponded to the intensity of restrictive measures in Germany. The fear of economic consequences (e.g., unemployment) was, on average, comparatively low in the study sample.
Fig. 2.
Different fears in the context of the COVID-19 pandemic.
Note. Scale ranges from 1 “no fear” to 6 “strong fear”; figure depicts means with standard errors.
3.5. Longitudinal changes of anxiety and depressive symptoms over the course of the pandemic
Fig. 3 and Table 1 present a descriptive overview of symptoms of mental strain during the COVID-19 pandemic. On average, pandemic-related anxiety (C-19-A), the cognitive preoccupation with the pandemic, the perceived risk of infection and the broader parameters of unspecific generalized anxiety (GAD-2) and depressive symptoms (PHQ-2) followed a similar course over the nine assessment points with peaks at the beginning of the pandemic and during the second and third COVID-19 waves. It is noticeable that the relative maximum of all of these parameters, except for depressive symptoms, lies at the first assessment, directly at the beginning of the pandemic. Divergently, depressive symptoms exhibited the maximum at T8 (spring 2021).
Fig. 3.
Descriptive analysis of symptoms of mental strain during the first 1.5 years of the COVID-19 pandemic.
Note. Means and standard errors are displayed. Sum score of the C-19-A ranges from 0 “no fear” to 40 “strong fear”; sum score of the GAD-2 respectively PHQ-2 ranges from 0 “no symptoms” to 6 “severe symptoms”.
Table 1.
Symptoms of mental strain during the first 1.5 years of the pandemic.
| n | T1 |
T2 |
T3 |
T4 |
T5 |
T6 |
T7 |
T8 |
T9 |
|
|---|---|---|---|---|---|---|---|---|---|---|
| 5114 | 2555 | 1610 | 1389 | 1386 | 2212 | 1727 | 1553 | 1311 | ||
| COVID-19-related fear (C-19-A) | 10. perc. | 2 | 1 | 1 | 0 | 0 | 2 | 1 | 1 | 0 |
| 25. perc. | 5 | 3 | 2 | 2 | 2 | 4 | 3 | 3 | 1 | |
| Median | 9 | 7 | 5 | 4 | 4 | 7 | 7 | 7 | 3 | |
| 75. perc. | 14 | 12 | 10 | 8 | 8 | 13 | 12 | 13 | 5 | |
| 90. perc. | 20 | 18 | 16 | 14 | 14 | 19 | 18 | 19 | 10 | |
| Anxiety and depressive symptoms (PHQ-4) | 10. perc. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 25. perc. | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | |
| Median | 4 | 3 | 3 | 3 | 3 | 3 | 3 | 4 | 3 | |
| 75. perc. | 6 | 5 | 5 | 5 | 5 | 6 | 5 | 6 | 4 | |
| 90. perc. | 9 | 9 | 8 | 8 | 8 | 9 | 9 | 9 | 8 | |
| ≥Cut-off | 28.3 % | 25.5 % | 22.0 % | 22.1 % | 21.2 % | 26.5 % | 24.1 % | 29.1 % | 17.9 % | |
| Anxiety symptoms (GAD-2) | 10. perc. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 25. perc. | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | |
| Median | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| 75. perc. | 3 | 3 | 2 | 2 | 2 | 3 | 2 | 3 | 2 | |
| 90. perc. | 5 | 5 | 4 | 4 | 4 | 5 | 4 | 5 | 4 | |
| ≥Cut-off | 32.6 % | 28.2 % | 24.4 % | 24.1 % | 23.2 % | 28.8 % | 24.1 % | 29.3 % | 20.8 % | |
| Depressive symptoms (PHQ-2) | 10. perc. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 25. perc. | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | |
| Median | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | |
| 75. perc. | 3 | 3 | 3 | 2 | 2 | 3 | 3 | 3 | 2 | |
| 90. perc. | 5 | 5 | 4 | 4 | 4 | 5 | 5 | 5 | 4 | |
| ≥Cut-off | 31.4 % | 29.6 % | 25.5 % | 24.8 % | 23.6 % | 29.3 % | 30.2 % | 35.0 % | 20.6 % |
Note. A PHQ-4 sum score ≥ the cut-off 6, respectively a GAD-2/PHQ-2 score ≥ 3, is classified as alarming symptom severity.
The average retrospective rating of one's pandemic-related mental strain at every month since the beginning of the pandemic (Fig. S1) exhibited a similar two-peak trend as the C-19-A values with a relative maximum at the beginning of the pandemic and a second maximum during winter 2020.
The results of the multilevel analysis are depicted in Table 2 . Compared to women, men experienced lower levels of pandemic-related fear, anxiety, and depressive symptoms over the course of the pandemic. Furthermore, anxiety and depressive symptoms decreased with age. As the duration of the pandemic lengthened, all analyzed symptoms decreased on average. Moreover, symptoms varied as a function of infection rates and tended to be higher in times of higher vs. lower COVID-19 cases.
Table 2.
Associations of gender, age, duration of the pandemic and the rate of new infections with fear, anxiety, and depressive symptoms over the first 1.5 years of the pandemic.
| COVID-19-related fear (C-19-A) | Depressive + anxiety symptoms (PHQ-4) | Anxiety symptoms (GAD-2) | Depressive symptoms (PHQ-2) | |
|---|---|---|---|---|
| Number of observations | 18,852 | 18,618 | 18,619 | 18,618 |
| Coefficient | b (SE) | b (SE) | b (SE) | b (SE) |
| Gender (male vs. female) | −0.196** (0.023) | −0.209** (0.023) | −0.273** (0.023) | −0.115** (0.023) |
| Gender (diverse vs. female) | 0.138 (0.124) | 0.506** (0.123) | 0.452** (0.123) | 0.479** (0.121) |
| Age (in years) | 0.002 (0.001) | −0.012** (0.001) | −0.008** (0.001) | −0.013** (0.001) |
| Time since the beginning of the pandemic (in days/100) | −0.170** (0.004) | −0.057** (0.004) | −0.061** (0.004) | −0.045** (0.004) |
| Rate of new infections (rate/1000) | 0.037** (0.001) | 0.014** (0.001) | 0.012** (0.001) | 0.014** (0.001) |
Note. b = coefficient from multilevel models. Standard errors are in parenthesis. Significance levels: **p < .01.
4. Discussion
4.1. Summary and interpretation of the results
We longitudinally investigated the course of symptoms of mental strain and risk and resilience factors across the first 1.5 years of the COVID-19 pandemic in an adult sample in Germany. We found that pandemic-related fears, unspecific anxiety, depressive symptoms, and the retrospective rating of mental distress followed, on average level, a similar trend with a first maximum at the beginning of the pandemic in spring 2020 and a second maximum in late fall 2020 until early spring 2021. This trend can be explained to a certain extent by a combination of the progressing duration of the pandemic (the longer the pandemic lasts, the less the symptoms occur) and the rate of infections (the higher the rate of new infections, the more severe the symptoms). The subjective risk of an infection with SARS-CoV-2 within the next month was, on average, the highest at the early beginning of the pandemic when objective infection rates were way lower than in the later progress of the pandemic. This suggests that during the early confrontation with an exceptional situation the overestimation of one's risk is particularly pronounced.
These observations, particularly with regard to pandemic-related anxiety during the early pandemic, are in line with findings from other longitudinal studies and meta-analyses (Manchia et al., 2021; Robinson et al., 2022). In a meta-analysis of 65 longitudinal cohort studies, Robinson et al. (2022) found, compared to pre-pandemic levels, significantly increased levels of psychopathological symptoms during the first two months of the pandemic, which then progressively decreased as the pandemic proceeded. The extent of anxiety symptoms was no longer significantly different from the pre-pandemic level by the (early) summer of 2020, while depressive symptoms showed somewhat stronger and longer-lasting increases. Several studies interpreted the overall declining trend of symptoms of mental distress during the first months of the pandemic as a hint of an evolving adaption to the exceptional pandemic situation (Bendau et al., 2020; Manchia et al., 2021; Robinson et al., 2022). Regarding the first months, our data supports this assumption. In the further progress of the pandemic, with the second increase of symptoms, our results suggest that besides adaption and habituation, the actual pandemic situation (e.g., rate of infections) plays an important role for the mental well-being.
In parallel to the infection dynamics, the extent of restrictive measures could be partly accountable for mental health burden (Henssler et al., 2021; Prati and Mancini, 2021). Furthermore, it can be assumed that vaccinations have a major impact on pandemic-related fears: At T9 (at the beginning of the fourth COVID-19 wave) a strong reduction in all of those fears was evident, notwithstanding a rising trend in infections; this might be explained by the high proportion of vaccinated individuals in our sample. It is noteworthy in this context that data collection took part before occurrence of the immune-escape virus variant Omicron and vaccination therefore seemed to provide an excellent protection not only to severe COVID-19-pathologies but also to transmission (Pandey et al., 2021). Furthermore, it should be considered that fears, in turn, also seem to be associated with vaccine acceptance (Bendau et al., 2021c).
In summary, our study sample seems to be rather resilient with mild symptom expressions, a rather high appearance of potentially protective factors and low variables of risk. On average, risk-bearing and protective factors remained relatively stable across the course of the pandemic (even if they presented a slight tendency toward a similar two-peak trend as stress-reactive symptoms). Despite these positive results on an average level, enhanced attention needs to be paid to those exhibiting low protective variables, pronounced risk factors, and/or maladaptive changes in these factors. Among the protective factors, the knowledge of where to get psychological support seems to have comparatively the greatest potential to be further improved. Reduced physical activity, on average, seems to be the most pronounced risk factor and should therefore get particular attention in preventive and therapeutic interventions (Villadsen et al., 2021). The extent of increased substance use was, on average rather low, but increments seem to persist slightly longer than changes in other risk-bearing factors. This is noteworthy because noxious changes in substance use may present a pronounced peril of persisting and aggravating over time and ought to be targeted accordingly (Manthey et al., 2021; Bendau et al., 2022).
Whereas our study focused on the dimensional assessment of (subclinical) mental strain, it is also important to consider the occurrence of incident full-threshold mental disorders caused or amplified by the pandemic. Bohlken et al. (2021) found, in German general practices during the pandemic in 2020, an increase in the incidence of anxiety disorders (+19 %) in the general population and depressive (+12 %) and stress-related disorders (+23 %) in the older population compared to previous years. However, the exact rates vary substantially between different studies—among other things due to specific study samples, methodological factors, and time frames (Bohlken et al., 2021; Gerdau-Heitmann et al., 2017). Alongside other factors, it can be expected that the majority of pandemic-caused disorders will become evident with a substantial time delay (Bohlken et al., 2021; Santomauro et al., 2021). During the first lockdown in 2020, for example, a drastic reduction in the utilization of psychiatric-psychotherapeutic services and in the diagnosed incidence of mental disorders was observed due to actual or subjectively perceived pandemic-related restrictions on services and concerns about an increased risk of infection in the event of utilization (Bohlken et al., 2021; Boldrini et al., 2021; Neelam et al., 2021).
To conclude, our sample showed rather mild levels of mental health issues that increased and decreased parallelly to the aggravating and relaxing pandemic situation, respectively. Future studies should complement these dimensional (primarily sub-clinical) observations with categorical assessment of the incidence of mental disorders during and after the COVID-19 pandemic. Individuals with high and persisting levels of mental burden as well as those actually developing or at greater risk for the incidence of manifest disorders deserve special consideration.
4.2. Limitations
Our study is characterized by several strengths: We longitudinally assessed a large sample of the adult general population in Germany in up to nine waves during the first 1.5 years of the COVID-19 pandemic. This wide time frame allows the collection of information beyond most existing studies. Further, we not only examined levels of symptoms of mental strain but also took into account changes in potentially risk-bearing and protective psychosocial-behavioral factors.
Nevertheless, the limitations of our study merit consideration. The correlative-observational design does not allow causal conclusions. Our sample was acquired by non-probability convenience sampling and, therefore, is not unconditionally representative of the general population in Germany (e.g., due to the overall higher female proportion, the younger average age, and the higher percentage of vaccinated individuals at the final assessment). The online-based recruitment and assessment of our study might amplify a sample/selection bias because individuals who frequently use (social) online media as well as those especially interested or affected by the topic may be more likely to participate, whereas those who do not regularly access social media and/or are affected by ‘digital poverty’ and ‘digital inequality’ (e.g., economically strongly disadvantaged and elderly people) are underrepresented. In the broader context, moreover, international comparisons are only possible to a limited extent because globally pandemic conditions varied highly (e.g., with regard to infection rates, restrictions, and supportive measures) (Bueno-Notivol et al., 2021; Cénat et al., 2021; Prati and Mancini, 2021; Robinson et al., 2022). This is further complicated by a high variance in operationalization and other aspects of methodology (Bueno-Notivol et al., 2021; Cénat et al., 2021). Particularly, the definition and assessment methods of specific psychopathological symptoms of distress, anxiety, and depression vary substantially and influence the results (Necho et al., 2021).
It should be further noted that our study data rely on anonymous self-report which is possibly vulnerable to answer biases. Thus, this information may be not entirely valid and reliable and should be complemented with objective epidemiological data from clinics, practices, etc. In addition, other sources of data (e.g., internet searches (Gianfredi et al., 2021)) to quantify psychological burden should be considered within an integrating approach.
5. Conclusion
In summary, our findings suggest that symptoms of mental strain tended to decrease over the course of the pandemic but were elevated in times of increased infection rates. While most individuals were only mildly affected by mental strain, some experienced pronounced anxiety and depressive symptoms at different stages of the pandemic. These should be targeted by adaptive preventive and therapeutic interventions during the pandemic as well as in its aftermath. The fluctuating symptom levels emphasize the relevance of continuous mental health monitoring over the course of the pandemic. Specifically, our results imply that support should be particularly provided at the beginning of extraordinary demanding situations and during phases of high infection rates and pronounced restrictive measures.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Role of the funding source
This work was supported by the Sonnenfeld Stiftung (grant for Antonia Bendau). The funding source had no involvement in the conceptualization and realization of the project or the manuscript.
Data availability
Data are available from the corresponding author on reasonable request.
CRediT authorship contribution statement
Antonia Bendau: Methodology, Formal analysis, Data curation, Visualization, Writing – original draft. Eva Asselmann: Methodology, Formal analysis, Writing – review & editing. Jens Plag: Methodology, Conceptualization, Writing – review & editing. Moritz Bruno Petzold: Methodology, Conceptualization, Writing – review & editing. Andreas Ströhle: Conceptualization, Supervision, Writing – review & editing.
Conflict of interest
The authors declare that there is no conflict of interest.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2022.09.105.
Appendix A. Supplementary data
Supplementary material (Table S1 and Figure S1)
References
- Bendau A. Charité – Universitätsmedizin Berlin. Refubium Freie Universität Berlin; 2022. Anxiety in Context of the COVID-19 Pandemic: Associations With Protective and Risk Factors, Mental Disorders and Vaccination Acceptance. Doctoral dissertation. [DOI] [Google Scholar]
- Bendau A., Kunas S.L., Wyka S., Petzold M.B., Plag J., Asselmann E., Ströhle A. Longitudinal changes of anxiety and depressive symptoms during the COVID-19 pandemic in Germany: the role of pre-existing anxiety, depressive, and other mental disorders. J. Anxiety Disord. 2021;102377 doi: 10.1016/j.janxdis.2021.102377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendau A., Petzold M.B., Wyka S., Pyrkosch L., Plag J., Ströhle A. Ängste in zeiten von COVID-19 und anderen gesundheitskrisen. Nervenarzt. 2021;92:417–425. doi: 10.1007/s00115-020-01030-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendau A., Plag J., Kunas S., Wyka S., Ströhle A., Petzold M.B. Longitudinal changes in anxiety and psychological distress, and associated risk and protective factors during the first three months of the COVID-19 pandemic in Germany. Brain Behav. 2020;e01964 doi: 10.1002/brb3.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendau A., Plag J., Petzold M.B., Ströhle A. COVID-19 vaccine hesitancy and related fears and anxiety. Int. Immunopharmacol. 2021;97 doi: 10.1016/j.intimp.2021.107724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendau A., Viohl L., Petzold M.B., Helbig J., Reiche S., Marek R., Romanello A., Moon D.U., Gross R.E., Gutwinski F., Masah D.J., Mick I., Montag C., Evens R., Majić T., Betzler F. No party, no drugs? Use of stimulants, dissociative drugs, and GHB/GBL during the early COVID-19 pandemic. Int. J. Drug Policy. 2022;102 doi: 10.1016/j.drugpo.2022.103582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohlken J., Kostev K., Riedel-Heller S., Hoffmann W., Michalowsky B. Effect of the COVID-19 pandemic on stress, anxiety, and depressive disorders in german primary care: a cross-sectional study. J. Psychiatr. Res. 2021;143:43–49. doi: 10.1016/j.jpsychires.2021.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boldrini T., Girardi P., Clerici M., Conca A., Creati C., Di Cicilia G., Ducci G., Durbano F., Maci C., Maone A., Nicolò G., Oasi O., Percudani M., Polselli G.M., Pompili M., Rossi A., Salcuni S., Tarallo F., Vita A., Lingiardi V. Consequences of the COVID-19 pandemic on admissions to general hospital psychiatric wards in Italy: reduced psychiatric hospitalizations and increased suicidality. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;110 doi: 10.1016/j.pnpbp.2021.110304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bueno-Notivol J., Gracia-García P., Olaya B., Lasheras I., López-Antón R., Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2021;21 doi: 10.1016/j.ijchp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cénat J.M., Blais-Rochette C., Kokou-Kpolou C.K., Noorishad P.-G., Mukunzi J.N., McIntee S.-E., Dalexis R.D., Goulet M.-A., Labelle P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragioti E., Li H., Tsitsas G., Lee K.H., Choi J., Kim J., Choi Y.J., Tsamakis K., Estradé A., Agorastos A. A large scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J. Med. Virol. 2022:1–15. doi: 10.1002/jmv.27549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan F.C., Zhang S.Y., Cheng Y. Incidence of psychological illness after coronavirus outbreak: a meta-analysis study. J. Epidemiol. Community Health. 2021;75:836–842. doi: 10.1136/jech-2020-215927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerdau-Heitmann C., Mümken S., Eberhard S., Koppelin F. Psychische Störungen im erwerbsalter : ermittlung der administrativen inzidenz und Prävalenz sowie regionaler unterschiede in Niedersachsen anhand von Sekundärdaten einer gesetzlichen krankenkasse. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2017;60:1346–1355. doi: 10.1007/s00103-017-2638-2. [DOI] [PubMed] [Google Scholar]
- Gianfredi V., Provenzano S., Santangelo O.E. What can internet users’ behaviours reveal about the mental health impacts of the COVID-19 pandemic? A systematic review. Public Health. 2021;198:44–52. doi: 10.1016/j.puhe.2021.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henssler J., Stock F., van Bohemen J., Walter H., Heinz A., Brandt L. Mental health effects of infection containment strategies: quarantine and isolation-a systematic review and meta-analysis. Eur. Arch. Psychiatry Clin. Neurosci. 2021:223–234. doi: 10.1007/s00406-020-01196-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunzler A.M., Röthke N., Günthner L., Stoffers-Winterling J., Tüscher O., Coenen M., Rehfuess E., Schwarzer G., Binder H., Schmucker C., Meerpohl J.J., Lieb K. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Glob. Health. 2021;17:34. doi: 10.1186/s12992-021-00670-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Wahl I., Rose M., Spitzer C., Glaesmer H., Wingenfeld K., Schneider A., Brähler E. A 4-item measure of depression and anxiety: validation and standardization of the patient health Questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 2010;122:86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- Manchia M., Gathier A.W., Yapici-Eser H., Schmidt M.V., de Quervain D., van Amelsvoort T., Bisson J.I., Cryan J.F., Howes O.D., Pinto L., van der Wee N.J., Domschke K., Branchi I., Vinkers C.H. The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: a critical review across waves. Eur. Neuropsychopharmacol. 2021;55:22–83. doi: 10.1016/j.euroneuro.2021.10.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manthey J., Kilian C., Carr S., Bartak M., Bloomfield K., Braddick F., Gual A., Neufeld M., O’Donnell A., Petruzelka B., Rogalewicz V., Rossow I., Schulte B., Rehm J. Use of alcohol, tobacco, cannabis, and other substances during the first wave of the SARS-CoV-2 pandemic in Europe: a survey on 36,000 european substance users. Subst. Abuse Treat. Prev. Policy. 2021;16:36. doi: 10.1186/s13011-021-00373-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Necho M., Tsehay M., Birkie M., Biset G., Tadesse E. Prevalence of anxiety, depression, and psychological distress among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Int. J. Soc. Psychiatry. 2021;67:892–906. doi: 10.1177/00207640211003121. [DOI] [PubMed] [Google Scholar]
- Neelam K., Duddu V., Anyim N., Neelam J., Lewis S. Pandemics and pre-existing mental illness: a systematic review and meta-analysis. Brain Behav. Immun. 2021;10 doi: 10.1016/j.bbih.2020.100177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey K., Thurman M., Johnson S.D., Acharya A., Johnston M., Klug E.A., Olwenyi O.A., Rajaiah R., Byrareddy S.N. Mental health issues during and after COVID-19 vaccine era. Brain Res. Bull. 2021;176:161–173. doi: 10.1016/j.brainresbull.2021.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petzold M.B., Bendau A., Plag J., Pyrkosch L., Mascarell Maricic L., Betzler F., Rogoll J., Große J., Ströhle A. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain and Behavior. 2020;10 doi: 10.1002/brb3.1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petzold M.B., Bendau A., Plag J., Pyrkosch L., Mascarell Maricic L., Rogoll J., Betzler F., Große J., Ströhle A. Development of the COVID-19-anxiety questionnaire and first psychometric testing. BJPsych Open. 2020;6 doi: 10.1192/bjo.2020.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati G., Mancini A.D. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021:1–11. doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institut Robert Koch. 2021. Nowcasting und R-Schätzung: Schätzung der aktuellen Entwicklung der SARS-CoV-2-Epidemie in Deutschland.https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Projekte_RKI/Nowcasting.html [Google Scholar]
- Robinson E., Sutin A.R., Daly M., Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022;296:567–576. doi: 10.1016/j.jad.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Fernández P., González-Santos J., Santamaría-Peláez M., Soto-Cámara R., Sánchez-González E., González-Bernal J.J. Psychological effects of home confinement and social distancing derived from COVID-19 in the general population-a systematic review. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18126528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rzymski P., Nowicki M., Mullin G.E., Abraham A., Rodríguez-Román E., Petzold M.B., Bendau A., Sahu K.K., Ather A., Naviaux A.-F., Janne P., Gourdin M., Delanghe J.R., Ochs H.D., Talmadge J.E., Garg M., Hamblin M.R., Rezaei N. Quantity does not equal quality: scientific principles cannot be sacrificed. Int. Immunopharmacol. 2020;86 doi: 10.1016/j.intimp.2020.106711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santomauro D.F., Mantilla Herrera A.M., Shadid J., Zheng P., Ashbaugh C., Pigott D.M., Abbafati C., Adolph C., Amlag J.O., Aravkin A.Y., Bang-Jensen B.L., Bertolacci G.J., Bloom S.S., Castellano R., Castro E., Chakrabarti S., Chattopadhyay J., Cogen R.M., Collins J.K., Dai X., Dangel W.J., Dapper C., Deen A., Erickson M., Ewald S.B., Flaxman A.D., Frostad J.J., Fullman N., Giles J.R., Giref A.Z., Guo G., He J., Helak M., Hulland E.N., Idrisov B., Lindstrom A., Linebarger E., Lotufo P.A., Lozano R., Magistro B., Malta D.C., Månsson J.C., Marinho F., Mokdad A.H., Monasta L., Naik P., Nomura S., O’Halloran J.K., Ostroff S.M., Pasovic M., Penberthy L., Reiner R.C., Jr., Reinke G., Ribeiro A.L.P., Sholokhov A., Sorensen R.J.D., Varavikova E., Vo A.T., Walcott R., Watson S., Wiysonge C.S., Zigler B., Hay S.I., Vos T., Murray C.J.L., Whiteford H.A., Ferrari A.J. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer K.M., Lieberman A., Sever A.C., Joiner T. Prevalence rates of anxiety, depressive, and eating pathology symptoms between the pre- and peri-COVID-19 eras: a meta-analysis. J. Affect. Disord. 2022;298:364–372. doi: 10.1016/j.jad.2021.10.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheek-Hussein M., Abu-Zidan F.M., Stip E. Disaster management of the psychological impact of the COVID-19 pandemic. Int J Emerg Med. 2021;14:19. doi: 10.1186/s12245-021-00342-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sousa G.M.de, Tavares V.D.D.O., Meiroz Grilo M.L.P.de, Coelho M.L.G., Lima-Araújo G.L.de, Schuch F.B., Galvão-Coelho N.L. Mental health in COVID-19 pandemic: a meta-review of prevalence meta-analyses. Front. Psychology. 2021;12 doi: 10.3389/fpsyg.2021.703838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villadsen A., Patalay P., Bann D. Mental health in relation to changes in sleep, exercise, alcohol and diet during the COVID-19 pandemic: examination of four UK cohort studies. Psychol. Med. 2021:1–10. doi: 10.1017/S0033291721004657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization WHO WHO Health Emergency Dashboard: Germany. 2022. https://covid19.who.int/region/euro/country/de Retrieved from.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material (Table S1 and Figure S1)
Data Availability Statement
Data are available from the corresponding author on reasonable request.