Abstract
Background
Accurate restoration of alignment is vital to the success of a total knee arthroplasty (TKA) procedure. Deformities, whether these are intra-articular and/or extra-articular AND/OR whether these are uniplanar/multiplanar/complex, can impose varying technical challenges in surgical planning and execution. Literature on performing TKA in presence of limb deformity is limited, especially for extra-articular deformities.
Objectives
The objectives of this narrative review are twofold. Firstly, we analyse the existing English literature for studies focussed on TKA and deformity correction and summarise the important points about deformity pathomechanics, clinical and radiological assessment, pre-operative planning and surgical techniques. The second objective is to provide the readers with a simplistic and wholistic management algorithm to assist surgeons in meticulous planning to tackle the technical challenges imposed by lower limb deformities while performing a TKA.
Discussion
Approach to each patient must be holistic and customised on an individual basis according to patient characteristics, deformity characteristics and surgeon experience. The three main options available are: (1) Primary TKA (symmetric cuts/asymmetric cuts with/without computer navigation assistance) (2) Single stage corrective osteotomy and TKA and (3) Two-staged deformity correction and TKA. A multi-disciplinary team approach is required and a knee surgeon well-versed in revision arthroplasty and a limb reconstruction surgeon specialising in deformity correction, should be involved from the outset. The use of computer navigation technology, particularly for deformity correction and TKA, has increased over the last couple of decades and is recommended by the authors for these challenging cases.
Keywords: Knee, Arthroplasty, Deformity, Navigation, Biomechanics, Osteotomy
1. Introduction
Total knee arthroplasty (TKA) offers significant quality of life benefits (in terms of pain, function and knee outcome scores).1 Restoration of mechanical alignment of the limb by judicious soft tissue balancing, accurate bone resection and implant positioning is important for satisfactory outcomes.2,3 The presence of intra-articular or extra-articular deformities (either in the femur or the tibia) poses technical challenges.4, 5, 6 These deformities can be uniplanar or multiplanar. Uniplanar deformities in either coronal (varus or valgus) or in the sagittal (procurvatum or recurvatum) plane are relatively easier to manage; however, the same cannot be said about multiplanar deformities. Complex multiplanar deformities, especially if associated with translation, are even harder to manage. Detailed evaluation of deformities is critical, as the direction of angular and translational deformities can differ.6,7
Single-stage extended intra-articular bone resection and soft tissue release can be used to manage deformities < 100 in the coronal and < 200 in the sagittal plane; however, more complex deformities require corrective osteotomy with TKA (either concomitant or as a two-stage procedure).6, 7, 8, 9
A single-stage procedure, involving intra-articular bone resection and soft tissue release, can jeopardise the insertion of collateral ligaments and lead to instability.8 A staged osteotomy followed by arthroplasty, or a concomitant osteotomy plus TKA is beneficial in severe cases requiring extensive bony cuts or where cuts would interfere with collateral ligament attachments and soft tissue balancing; this approach is also useful in cases where the deformity is associated with leg-length discrepancy (LLD).
The purpose of this article is to review the literature and identify challenges involved in undertaking TKA in the presence of these deformities. Each case must be assessed and treated on an individual basis. We aim to outline a simplified approach and a useful treatment algorithm for the management of these uncommon scenarios.
2. Effect of malalignment on the knee
The mechanical axis of the limb is represented by a line connecting centres of femoral head and ankle joint. This line should normally pass 8 mm medial, ± 7 mm, to the centre of the knee.10, 11, 12, 13 Deviation outside this range is termed mechanical axis deviation (MAD). MAD causes increased loading of either the medial or lateral compartment.
The femoral mechanical axis is from the centre of the hip to the centre of the knee joint. The femoral anatomical axis represents the mid-diaphyseal line of the femur. The femoral mechanical and anatomical axes normally subtend an angle of 6° ±2°.14,15 The mechanical axis of the tibia passes from the centre of the knee to centre of the ankle joint and is same as the anatomical axis. The knee joint line, however, is parallel to the ground during normal gait, with the mechanical axis in 3° of varus in relation to the vertical axis.13,15,16
Even with a normal mechanical axis, weightbearing across the lateral and medial compartments is unequal. During single leg stance, 60% to 70% of body weight passes through the medial compartment, which increases up to 90% with 4°–6° varus deformity.14 Although valgus alignment increases the lateral compartment peak pressure and hence the chances of lateral compartment OA, the medial compartment of the knee continues to bear more load until more severe valgus deformity is present.17,18 Khan et al.19 observed that for every 10 increase in the valgus malalignment, there is approximately 55% increase in the chances of lateral compartment OA and a 19% increase in the chance of severe OA.20
3. Assessment and planning
-
•
Patient personality – history; examination; functional demands/expectations.
-
•
Deformity personality – intra or extra-articular; level; magnitude; direction; uni or multi apical; associated soft tissue contractures.
-
•
Surgeon experience – unless the surgeon is familiar with both deformity planning and TKA, a two-surgeon MDT approach is recommended.
3.1. History
A detailed history to identify the cause of the deformity, previous interventions21 and infection is important. Fracture malunion of the femur and/or tibia, is the most common cause of extra-articular deformity around knee.22
Age and functional requirements of the patient are important factors to consider. For example, a simple single-stage procedure, with some compromise to the overall alignment of the limb, may be appropriate in an elderly patient with lower functional demands; however, in a younger patient with high functional demands, a more complex procedure to restore mechanical alignment accurately is more appropriate. Simultaneous involvement of spine, hip and ankle joints should also be explored.
3.2. Clinical examination
This should include a thorough assessment of the spine, hip, knee, foot, and ankle joints, including range-of-motion, muscle strength and secondary compensatory deformities. Often deformities are compensated at distant joints to improve mechanical axis and gait. These compensatory deformities can be mobile, party mobile or fixed. Partly mobile and fixed deformities, unlike mobile deformities, may result in secondary deformities if they are not addressed. Leg length discrepancy, rotational profile and ligament laxity should also be part of assessment.
3.3. Radiographic evaluation
Long leg weight-bearing (WB) radiographs with the patellae facing anterior (with a calibration ball to correct magnification errors), extending from pelvis to ankle joints, is the workhorse of radiographic evaluation. Non-weight bearing CT scanograms do not represent the true magnitude of the deformity and therefore should not be utilized for planning.
Although conventional deformity planning method is popular, in many cases peri-articular and subtle multiapical deformities may be missed. The authors, therefore, suggest Paley's method23,10,13 with the following steps:
Coronal plane: use either mechanical axis or anatomical axis but the same method must be used consistently during the entire planning (Fig. 1A and B).
-
•
Measure mechanical axis deviation (MAD) – to assess overall limb alignment.
-
•
MAD angle is the angle between mechanical axis of femur and mechanical axis of tibia.
-
•
Draw anatomical or mechanical lateral distal femoral angle (aLDFA, mLDFA respectively)
-
•
Draw medial proximal tibial angle (MPTA)
-
•
Draw joint line convergence angle (JLCA) – to identify any intraarticular deformities
-
•
Draw medial or lateral proximal femoral angle (MPFA or LPFA respectively)
-
•
Draw lateral distal tibial angle (LDTA)
Fig. 1.
Normal angles in the coronal plane - a - Mechanical axis b - Anatomical axis c - Sagittal plane axis.
Sagittal plane (Fig. 1C):
-
•
Draw anatomical posterior distal femoral angle (aPDFA)
-
•
Draw anatomical posterior proximal tibial angle (aPPTA)
-
•
Draw anatomical anterior distal tibial angle (aADTA)
The intersection of the proximal and distal axes of the deformed bone is called the Centre of Rotation of Angulation (CORA). Correcting the deformity at the CORA will result in a well-aligned limb. Complex interaction of osteotomy level, CORA, and angulation correction axis (ACA) will result in different amounts of secondary translation and final position of bone. Surgeons should be familiar with deformity planning and osteotomy rules to avoid iatrogenic deformity resulting from correction of the primary deformity.
Rotational deformities are best analysed clinically, although a CT scan is also frequently utilized to quantify the deformity.24 Detailed deformity planning is beyond the scope of this article.
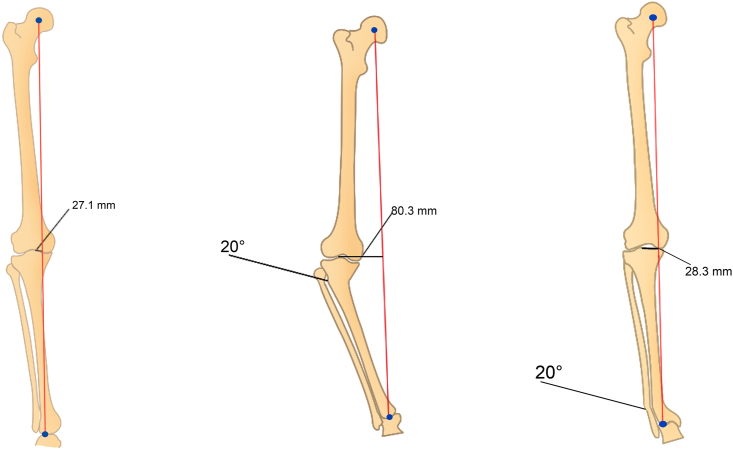
4. Effect of site of deformity (Fig. 2)
Fig. 2.
Effect of level of deformity on MADa - Medial compartment OA with increased Mechanical Axis Deviation (MAD) to 27.1 mm (Normal MAD 0 -10 mm medial) double check that we have said 10 mm in our text otherwise change it to match the text.b - 20 degrees deformity at the knee shifts the MAD to 80.3 mmc - 20 degrees deformity at ankle only shifts the MAD only slightly to 28.3 mm.
Both the magnitude and the level of the deformity must be considered. A 200 (Fig. 2B, C) deformity at the level of knee will significantly affect the mechanical axis; however, the same deformity nearer to the ankle or hip joint will have a more subtle effect. Geometry dictates that midshaft deformities will have 50% effect on overall mechanical axis of the limb. Effect of the deformity on the limb is more important than actual angulation of deformity.
5. Principles and pre-operative planning
The three main options are:
-
(1)Primary TKA
-
a.Standard TKA with conventional, symmetric bone resection cuts
-
b.Asymmetric resection and non-navigated TKA
-
c.Asymmetric resection and navigation assisted TKA
-
a.
-
(2)
Single stage procedure: Simultaneous corrective osteotomy and TKA
-
(3)
2 stage procedure: Corrective osteotomy followed by delayed TKA.
The objective is to ensure optimal implant survival, to restore the mechanical alignment of the limb with minimum soft tissue release (Table 1) (see Table 2).
Table 1.
Summary of studies reviewing the various studies in the literature for the different management methods.
| Intervention | Authors | Year | N | No of Stages | Follow Up(mo) | Average Deformity Corrected | Outcomes Assessed |
|---|---|---|---|---|---|---|---|
| TKR - Asymmetric Resection, Conventional | Wang & Wang | 2002 | 15 | Single | 38 | Coronal (15.1) & Sagittal (8.1) | Final Alignment (0.3), ROM (103), KSS (91.7) |
| Ritter et al. | 2004 | 82 | Single | 78 | Coronal Only (≥20 Varus-Valgus) | Final Alignment (4.9 Valgus ± 3), KSS (87.8) | |
| Kubiak et al. | 2008 | 111 | Single | 144 | Coronal Only (≥20 Valgus - 10 Varus) | ROM (100), KSS (92.2) | |
| Xiao-Gang et al. | 2012 | 7 | Single | 29 | Coronal (15) & Sagittal (10.5) | Final Alignment (1), HSS (89.8) | |
| Rajgopal et al.(7) | 2013 | 36 | Single | 85 | Coronal (16.2) & sagittal (10.1) | Final alignment (12), Knee society knee score (85), ROM (60) | |
| TKR + Distal Femoral Osteotomy - Conventional | Deschamps et al. | 2010 | 16 | Single | 48 | Coronal Only (21 Valgus - 24 Varus) | ROM (94) |
| 2 | Two-stage | Coronal Only (21 Valgus - 24 Varus) | ROM (94) | ||||
| Xiao-Gang et al. | 2012 | 2 | Single | 29 | Coronal (15) & Sagittal (10.5) | Final Alignment (1), HSS (89.8) | |
| Veltman et al. | 2015 | 21 | Single | 64 | Coronal (Femoral - Varus (12), Valgus (15), Tibial - Varus (17),Valgus (11)) Sagittal (n = 3, Angulation (N/A)) | ROM (97), OKS (38.5) | |
| TKR - Asymmetric Resection, Conventional with preoperative CT Planning | Marczak et al. | 2014 | 35 | Single | 57 | Coronal Only (18.6 Valgus - 21.4 Varus) | Final Alignment (5.5), ROM (90.1), KSS (80.5) |
| TKR - Asymmetric Resection, Navigated | Klein et al. | 2006 | 5 | Single | N/A | Coronal Only (16.2 Valgus - 13.3 Varus) | Final Alignment (1.1) |
| Bottros et al. | 2008 | 9 | Single | 18.9 | Coronal Only (2 Valgus - 14 Varus) | Final Alignment (1.3), ROM (98), KSS (92) | |
| Kim et al. | 2010 | 4 | Single | 14 | Coronal Only (15.1 Valgus) | Final Alignment (0.3), ROM (110), KSS (95) | |
| Liu et al. | 2011 | 8 | Single | 24 | Coronal Only (13.2 Valgus - 8.4 Varus) | Final Alignment (1.2), ROM (106.2), KSS (84) | |
| Tigani et al. | 2012 | 9 | Single | 28 | Coronal Only (≥10 Varus-Valgus) | Final Alignment (0), ROM (81), KSS (72) | |
| Rhee et al. | 2013 | 13 | Single | 37 | Coronal (7.5) & Sagittal (22) | Final Alignment (0.23 Valgus), ROM (118.46), KSS (89.62) |
Table 2.
Simplified flowchart for managing complex knee deformities with total knee arthroplasty.
| Surgical plan | Indications |
|---|---|
| Primary TKA- Standard TKA with conventional, symmetric bone resection cuts with navigation |
|
| Primary TKA - Standard navigated TKA with asymmetric bone resection |
|
| Single-stage procedure: Simultaneous corrective osteotomy and TKA |
|
| 2-stage procedure: Corrective osteotomy followed by delayed TKA |
|
Generally, it is accepted that deformity <10°-200 in the coronal plane or <20°-300 in the sagittal plane may be treated with an intra-articular correction using asymmetric cuts.7,25 Patients where pre-operative planning with asymmetric cuts shows compromise of the collateral ligament origins or patellar tendon attachment should undergo an osteotomy prior to TKA.
Wang and Wang25 described a radiographic templating method, using line drawings of a full-length AP weight-bearing radiograph of the limb, to decide between intra-articular versus extra-articular deformity correction. A line is drawn perpendicular to the mechanical axis of the femur at the level of the femoral condyles. If this line passes distal to the origin of the collateral ligament (approximately 25 mm from the joint line) intra-articular bone resection can be performed to correct the extra-articular deformity. For extra-articular deformity of the tibia a line is drawn along the medullary canal of the tibia distal to the angular deformity and if this passed within the tibial condyles, then intra-articular correction is possible.
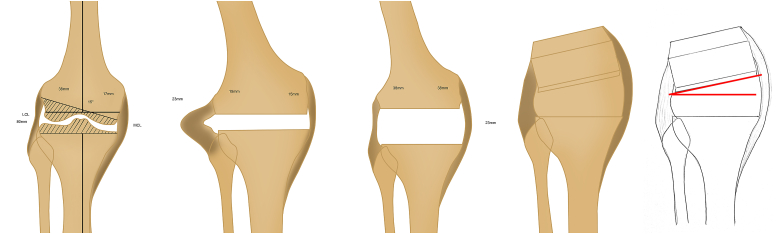
5.1. Primary TKA
Tibial resection affects both flexion and extension gap equally. Although single-stage, intra-articular resection does not require simultaneous osteotomy, it will require soft tissue release. Intra-articular correction of an extra-articular varus deformity requires removal of more lateral than medial femoral condyle and conversely a valgus deformity will require greater medial resection.9 In both situations, this asymmetric resection will result in imbalance of the soft tissues (Fig. 3a–d). More specifically, pre-operative femoral or tibial varus deformity will, post-resection, result in laxity of the lateral soft tissue structures and therefore will require medial soft tissue release, which may in turn alter the joint line, potentially causing patella-femoral problems.
Fig. 3.
Hypothetical case - Images Courtesy Kevin Tetsworth, Brisbane, Australia3a – 15 degrees extra articular femoral shaft deformity – Femoral asymmetric cut and tibia neutral cut3b – lateral ligament laxity due to asymmetric cut3c – MCL release – extension gap balanced3d – Flexion gap not balanced with MCL laxity.
Femoral or tibial valgus deformity post-resection will result in laxity of the medial structures requiring release of the lateral structures. Lateral collateral laxity is better tolerated than medial collateral laxity and therefore the surgeon can perhaps correct slightly more varus than valgus. Similarly, the superficial medial collateral tibial attachment is further removed from the joint line compared with its femoral attachment and therefore, the surgeon can perhaps correct slightly more deformity on the tibia than on the femur.
Femoral asymmetric cuts affect extension and flexion unequally, creating a more challenging problem; there may be difficulty in achieving satisfactory patella-femoral alignment and tracking and there can be difficulty in achieving varus-valgus stability in mid-flexion. The joint line may be raised, increasing the patella-femoral joint load; this may not show up in early outcome measures, but may then present as later symptoms (Fig. 3a–d).
It is possible that despite some increase in patella-femoral joint loading, correction of deformity that involves a few millimetres of additional excision medially or laterally on the distal femoral cut, appropriately accommodated in flexion by slight rotation of the femoral component, may give acceptable functional outcomes.
It is suggested therefore that the asymmetric cuts method may be useful for minor malalignments but in view of the potential long-term effects, the authors recommend avoidance of this method in severe deformities .
5.1.1. Primary TKA with standard cuts (symmetric resection)
If the deformity is small or the deformity is near the ankle or hip joints, then it will result in little effect on MAD; a TKA with standard cuts can then be undertaken (Fig. 4a and b).
Fig. 4.
Effect of level of deformity on MADa - Proximal femoral deformity, well away from knee and consequently have little affect on MADb - Standard cuts and standard TKA.
5.1.2. TKA with asymmetric cuts using conventional methods, no osteotomy
Deformity correction by intra-articular bone resection with standard TKR can be challenging. Despite detailed planning, the amount of bone resection remains approximate, and the risk of malalignment is high. We, therefore, recommend computer-navigated knee replacements for all single-stage procedures with asymmetric bone resection (Fig. 5).
Fig. 5.
Asymmetric cuts and mechanically aligned TKA with computer navigationa - Tibia and Femoral deformity with significant medial MADb - Asymmetric cuts and TKA with computer navigation with normal MAD.
5.1.3. TKA with computer navigation
We suggest navigated TKA for all patients with lower limb deformity; in conventional surgery the bone cuts are based on intra or extra-medullary alignment guides or jigs, which in the presence of extra-articular deformity, retained implants and if the CORA of the deformity is very close to the knee joint line, may not be feasible or accurate.26,27, 28, 29
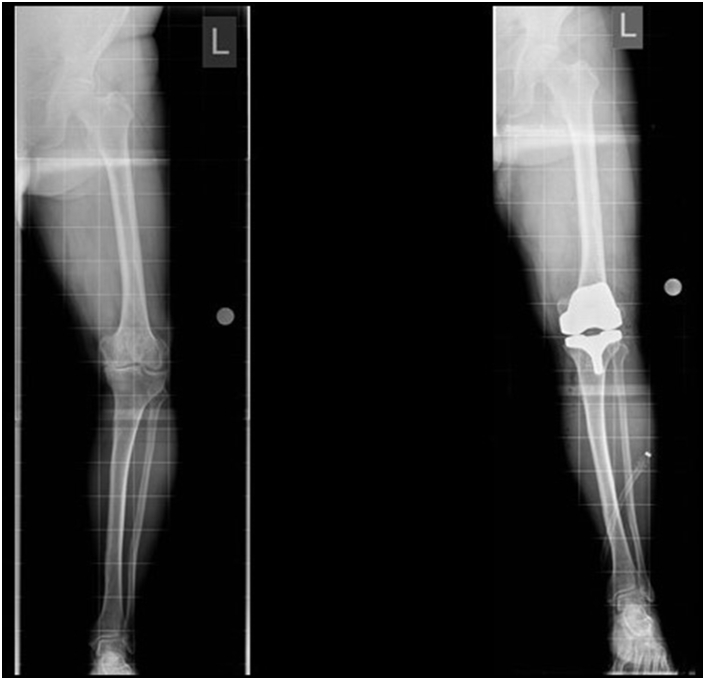
5.2. Single stage deformity correction & TKA
In this approach a corrective osteotomy is performed concomitantly with TKA as a single-stage procedure.30 In a malunited femur or tibia, corrective osteotomy is performed before TKA and fixed with an internal implant or a long stem prosthesis (Fig. 6A and B). Navigation assistance is recommended to achieve greater accuracy and because the metalwork may hinder the use of conventional TKA instrumentation.31
Fig. 6.
Single stage TKA with osteotomya - significant Valgus tibial deformity with Valgus OAb - single stage correction, osteotomy with long stem TKR.
The patient is spared multiple operations although recovery may be longer and more difficult compared with staged procedures.9 Blood loss and cement extrusion through the osteotomy site during implantation of TKA, with consequent non-union, can occur.
Lonner et al.5 reported 11 knees with extra-articular deformity treated by femoral osteotomy followed by TKA in a single setting. Although they reported significant improvements in the Knee Society Score, the complication rate was 45%. Madelaine et al.32 reported 4 major post-operative complications and 4 intra-operative tibial plateau fractures in their series of 15 knees of single-stage HTO and TKA. Although evidence is limited to small case series, the complication rate of this complex procedure appears to be high.
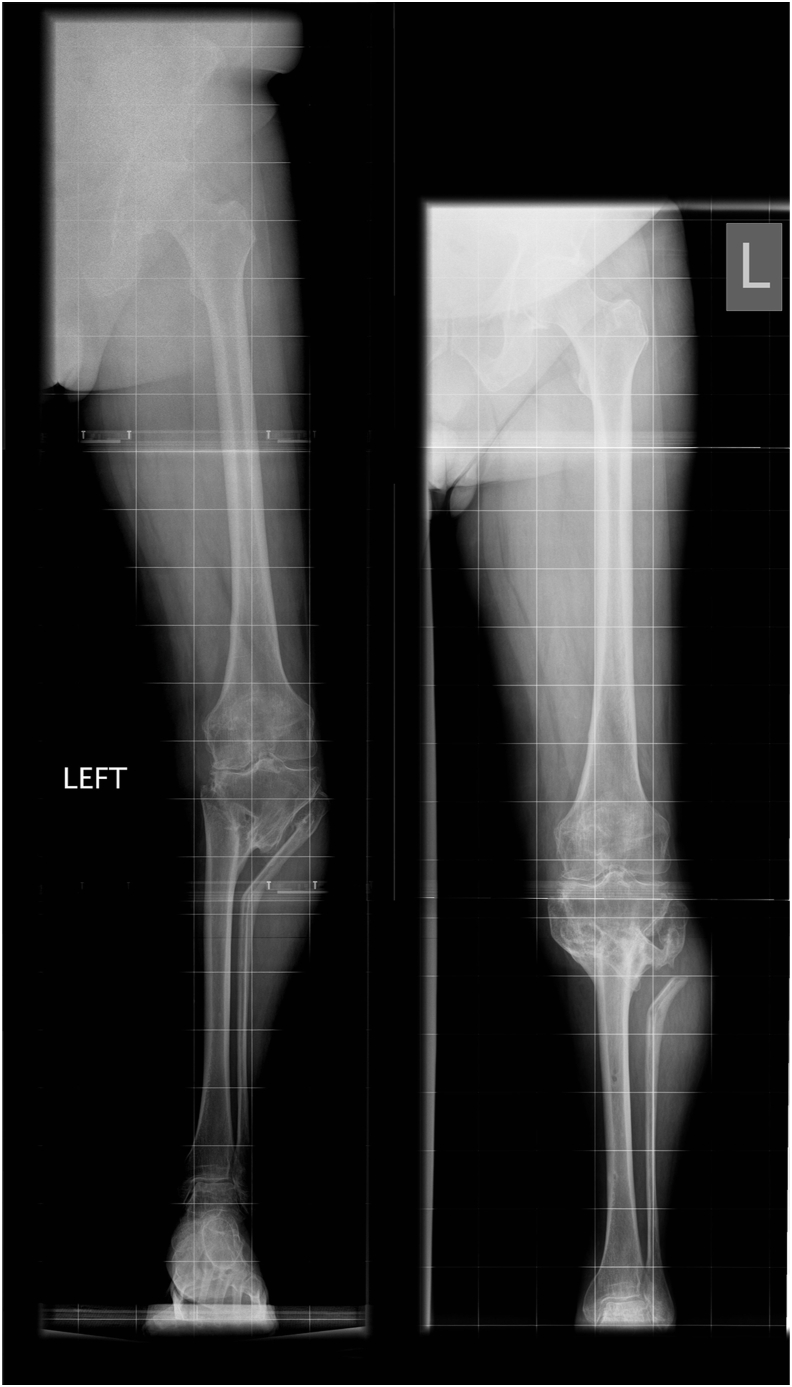
5.3. Staged deformity correction & TKA
Two-stage procedures allow for recovery between osteotomy and arthroplasty. In some cases, osteotomy and correction of malalignment delays the need for TKA due to alleviation of symptoms (Fig. 7a and b). In selected young patients with deformity, osteotomy can be converted to HTO, thereby offloading the medial compartment and deferring the TKA, thus benefitting from the decreased life-time risk of revision with increasing age.33
Fig. 7.
Planned for 2 stage TKA - Deformity correction alleviated symptoms and consequently need for TKA7a – pre op Translation deformity, significant medial MAD and medial compartment grade 4 OA7b – Post correction, neutral alignment. At 13 years FU patient with minimal symptoms and does not require TKA.
Various techniques are available for fixation of deformity correction osteotomies.8,34 Internal fixation, although less cumbersome for the patient than external fixation, relies on the accuracy of deformity correction achieved, with no option of fine tuning the deformity correction post-operatively, and often does not address the dynamic component of the deformity. It is usually used for correction of femoral deformities due to convenience. In the recent past, external fixator assisted internal fixation has been utilized to improve accuracy (Fig. 8a–d). Antegrade nails, possibly inserted with navigation or patient-specific instrumentation (PSI) have an advantage over retrograde femoral nails as they can potentially be left in-situ.
Fig. 8.
2 stage surgery - Stage 1 Osteotomy, Stage 2 TKA8a – pre op multi apical deformity8b – Fixator assisted 2 level osteotomy and internal fixation to correct the deformity. Osteotomies healed8c & d – Post TKR with long stem tibia to support the osteotomy site.
Gradual correction with circular frame is preferred when soft tissue quality is poor, in complex deformities, when patients have had multiple procedures in the past or to minimise the risk to peroneal nerve when correcting severe valgus deformity.35 Circular external fixation, although relatively more cumbersome, provides the most accurate deformity correction whilst addressing both static and dynamic components of the deformity simultaneously.
6. Conclusions
TKA in the presence of deformity is complex and requires MDT approach. Ideally, a knee surgeon well-versed in revision arthroplasty and a limb reconstruction surgeon specialising in deformity correction, should be involved from the outset. Functional, realistic goals should be set taking into consideration the patient's wishes. Single-stage osteotomy and TKA should ideally be performed by a two-surgeon team.
The role of navigation in managing complex lower limb deformities is increasing and its use is recommended. Relative merits of using the mechanical axis, the anatomical axis or the kinematic axis for aligning femoral and tibial components lies beyond the scope of this paper; these alternative philosophies each have their proponents.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent to publish
Yes.
Authors contributions
RJ: Data assimilation and manuscript preparation.
KS: Editing.
HS: Planning, figures and tables, editing.
Funding
None.
Institutional ethical committee approval (for all human studies)
Not applicable.
Availability of data and materials
Available.
Declaration of competing interest
None.
Acknowledgements
None.
Contributor Information
Rakesh John, Email: rakeshjohn23@gmail.com.
Kevin Sherman, Email: kps31@cam.ac.uk.
Hemant Sharma, Email: hksorth@yahoo.co.uk.
References
- 1.Shan L., Shan B., Suzuki A., Nouh F., Saxena A. Intermediate and long-term quality of life after total knee replacement: a systematic review and meta-analysis. J Bone Joint Surg. 2015;97(2):156–168. doi: 10.2106/JBJS.M.00372. [DOI] [PubMed] [Google Scholar]
- 2.Wasielewski R.C., Galante J.O., Leighty R.M., Natarajan R.N., Rosenberg A.G. Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res. 1994;299:31–43. [PubMed] [Google Scholar]
- 3.Oswald M.H., Jakob R.P., Schneider E., Hoogewoud H.M. Radiological analysis of normal axial alignment of femur and tibia in view of total knee arthroplasty. J Arthroplasty. 1993;8(4):419–426. doi: 10.1016/s0883-5403(06)80042-2. [DOI] [PubMed] [Google Scholar]
- 4.Roffi R.P., Merritt P.O. Total knee replacement after fractures about the knee. Orthop Rev. 1990;19(7):614–620. [PubMed] [Google Scholar]
- 5.Lonner J.H., Siliski J.M., Lotke P.A. Simultaneous femoral osteotomy and total knee arthroplasty for treatment of osteoarthritis associated with severe extra-articular deformity. J Bone Joint Surg Am. 2000;82(3):342–348. doi: 10.2106/00004623-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Sculco P.K., Kahlenberg C.A., Fragomen A.T., Rozbruch S.R. Management of extra-articular deformity in the setting of total knee arthroplasty. J Am Acad Orthop Surg. 2019;27(18):819–830. doi: 10.5435/JAAOS-D-18-00361. [DOI] [PubMed] [Google Scholar]
- 7.Rajgopal A., Vasdev A., Dahiya V., Tyagi V.C., Gupta H. Total knee arthroplasty in extra articular deformities: a series of 36 knees. Indian J Orthop. 2013;47(1):35–39. doi: 10.4103/0019-5413.106893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hungerford D.S. Extra-articular deformity is always correctable intra-articularly: To the Contrary. Orthopedics. 2009;32(9):677–679. doi: 10.3928/01477447-20090728-23. [DOI] [PubMed] [Google Scholar]
- 9.Koenig J.H., Maheshwari A.V., Ranawat A.S., Ranawat C.S. Extra-articular deformity is always correctable intra-articularly: in the affirmative. Orthopedics. 2009;32(9):676–678. doi: 10.3928/01477447-20090728-22. [DOI] [PubMed] [Google Scholar]
- 10.Paley D., Tetsworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of uniapical angular deformities of the tibia or femur. Clin Orthop Relat Res. 1992;280:48–64. [PubMed] [Google Scholar]
- 11.Cicuttini F., Wluka A., Hankin J., Wang Y. Longitudinal study of the relationship between knee angle and tibiofemoral cartilage volume in subjects with knee osteoarthritis. Rheumatology. 2004;43(3):321–324. doi: 10.1093/rheumatology/keh017. [DOI] [PubMed] [Google Scholar]
- 12.Brouwer G.M., Tol A.W.V., Bergink A.P., et al. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee Arthritis. Rheum. 2007;56(4):1204–1211. doi: 10.1002/art.22515. [DOI] [PubMed] [Google Scholar]
- 13.Paley D. Springer Berlin Heidelberg; 2002. Principles of Deformity Correction [Internet] [Google Scholar]
- 14.Hsu R.W., Himeno S., Coventry M.B., Chao E.Y. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–227. [PubMed] [Google Scholar]
- 15.Cherian J.J., Kapadia B.H., Banerjee S., Jauregui J.J., Issa K., Mont M.A. Mechanical, anatomical, and kinematic Axis in TKA: concepts and practical applications. Curr Rev Musculoskelet Med. 2014;7(2):89–95. doi: 10.1007/s12178-014-9218-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krackow K.A. Approaches to planning lower extremity alignment for total knee arthroplasty and osteotomy about the knee. Adv Orthop Surg. 1983;7:69–88. [Google Scholar]
- 17.Johnson F., Leitl S., Waugh W. The distribution of load across the knee. A comparison of static and dynamic measurements. J Bone Joint Surg Br. 1980;62(3):346–349. doi: 10.1302/0301-620X.62B3.7410467. [DOI] [PubMed] [Google Scholar]
- 18.Harrington I.J. Static and dynamic loading patterns in knee joints with deformities. J Bone Joint Surg. 1983;65(2):247–259. doi: 10.2106/00004623-198365020-00016. [DOI] [PubMed] [Google Scholar]
- 19.Khan F.A., Koff M.F., Noiseux N.O., et al. Effect of local alignment on compartmental patterns of knee osteoarthritis. J Bone Joint Surg Am. 2008;90(9):1961–1969. doi: 10.2106/JBJS.G.00633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scott C.E.H., Nutton R.W., Biant L.C. Lateral compartment osteoarthritis of the knee: biomechanics and surgical management of end-stage disease. The Bone & Joint Journal. 2013;95-B(4):436–444. doi: 10.1302/0301-620X.95B4.30536. [DOI] [PubMed] [Google Scholar]
- 21.Khanna V., Sambandam S.N., Ashraf M., Mounasamy V. Extra-articular deformities in arthritic knees-a grueling challenge for arthroplasty surgeons: an evidence-based update. Orthop Rev. 2018;26(4):9. doi: 10.4081/or.2017.7374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wolff A.M., Hungerford D.S., Pepe C.L. The effect of extraarticular varus and valgus deformity on total knee arthroplasty. Clin Orthop Relat Res. 1991;271:35–51. [PubMed] [Google Scholar]
- 23.Paley D., Tetsworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of multiapical frontal plane angular and bowing deformities of the femur and tibia. Clin Orthop Relat Res. 1992;280:65–71. [PubMed] [Google Scholar]
- 24.Staheli L.T., Corbett M., Wyss C., King H. Lower-extremity rotational problems in children. Normal values to guide management. J Bone Joint Surg Am. 1985;67(1):39–47. [PubMed] [Google Scholar]
- 25.Wang J.-W., Wang C.-J. Total knee arthroplasty for arthritis of the knee with extra-articular deformity. J Bone Joint Surg Am. 2002;84(10):1769–1774. doi: 10.2106/00004623-200210000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Shao J., Zhang W., Jiang Y., et al. Computer-navigated TKA for the treatment of osteoarthritis associated with extra-articular femoral deformity. Orthopedics. 2012;35(6):794–799. doi: 10.3928/01477447-20120525-15. [DOI] [PubMed] [Google Scholar]
- 27.Rhee S.J., Seo C.H., Suh J.T. Navigation-assisted total knee arthroplasty for patients with extra-articular deformity. Knee Surg Relat Res. 2013;25(4):194–201. doi: 10.5792/ksrr.2013.25.4.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu Z., Pan X., Zhang X. Total knee arthroplasty using navigation system for severe osteoarthritis with extra-articular deformity. Eur J Orthop Surg Traumatol. 2013;23(1):93–96. doi: 10.1007/s00590-011-0912-9. [DOI] [PubMed] [Google Scholar]
- 29.Bottros J., Klika A.K., Lee H.H., Polousky J., Barsoum W.K. The use of navigation in total knee arthroplasty for patients with extra-articular deformity. J Arthroplasty. 2008;23(1):74–78. doi: 10.1016/j.arth.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 30.Mullaji A., Shetty G.M. Computer-assisted total knee arthroplasty for arthritis with extra-articular deformity. J Arthroplasty. 2009;24(8):1164–1169. doi: 10.1016/j.arth.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 31.Mullaji A., Shetty G.M. Correction of severe deformity in total knee arthroplasty: decision making and key technical considerations. Semin Arthroplasty. 2012;23(1):27–30. [Google Scholar]
- 32.Madelaine A., Villa V., Yela C., et al. Results and complications of single-stage total knee arthroplasty and high tibial osteotomy. Int Orthop. 2014;38(10):2091–2098. doi: 10.1007/s00264-014-2420-0. [DOI] [PubMed] [Google Scholar]
- 33.Bayliss L.E., Culliford D., Monk A.P., et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet. 2017;389(10077):1424–1430. doi: 10.1016/S0140-6736(17)30059-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seah K.T.M., Shafi R., Fragomen A.T., Rozbruch S.R. Distal femoral osteotomy: is internal fixation better than external? Clin Orthop Relat Res. 2011;469(7):2003–2011. doi: 10.1007/s11999-010-1755-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim R.H., Scuderi G.R., Dennis D.A., Nakano S.W. Technical challenges of total knee arthroplasty in skeletal dysplasia. Clin Orthop Relat Res. 2009;469(1):69–75. doi: 10.1007/s11999-010-1516-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 36.Sharma L., Lou C., Cahue S., Dunlop D.D. The mechanism of the effect of obesity in knee osteoarthritis: the mediating role of malalignment. Arthritis Rheum. 2000;43(3):568–575. doi: 10.1002/1529-0131(200003)43:3<568::AID-ANR13>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 37.Veltman E.S., van Wensen R.J.A., Defoort K.C., van Hellemondt G.G., Wymenga A.B. Single-stage total knee arthroplasty and osteotomy as treatment of secondary osteoarthritis with severe coronal deviation of joint surface due to extra-articular deformity. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2835–2840. doi: 10.1007/s00167-015-3889-9. [DOI] [PubMed] [Google Scholar]
- 38.Rozbruch S.R., Kazmers N.H., Fragomen A.T. Prevention of pin site infection in external fixation: a review of the literature. Strategies Trauma Limb Recon. 2016;11(2):75–85. doi: 10.1007/s11751-016-0256-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Available.