Abstract
Introduction
The inferior alveolar nerve (IAN) can occasionally be observed in the extraction socket of the mandibular third molar (M3M) intraoperatively. Exposure of inferior alveolar neurovascular bundle during surgery primarily depends upon the absence of bony cortex between the canal and root of impacted third molar or either by existence of a very thin cortical lining between two which gets broken during luxation of tooth. Accurate anatomical relationship of inferior alveolar canal with root apex of impacted (M3M) and the location of canal can be determined by Cone beam computed tomography (CBCT).
Material and methods
Initially 200 patients evaluated by Orthopantomogram (OPG) for anatomical relationship of IAN with impacted (M3M) and various radiographic risk factors for nerve injury. Among these 200, 75 showed the presence of two or more than two risk factors for IAN injury which then were further evaluated by using CBCT for presence or absence of cortex of canal and location of canal on buccal, lingual, inferior, and interradicular position.
Conclusion
Cortex of canal is an important barrier between the root apex and inferior alveolar neurovascular bundle. Interruption of cortex on CBCT, the interradicularly and lingually positioned neurovascular bundle become a strong affirmation for intra operative nerve exposure during (M3M) surgery. Although its exposure is affected by various factors such as bone density, sex and age of patient, surgeon's expertise, operative tissue damage, post operative edema, surgical procedure, but neurosensory deficit do not occur simply after the exposure of neurovascular bundle.
Keywords: Impacted mandibular third molar, Orthopantomography, Cone beam computed, Tomography, Cortex of inferior alveolar canal, Nerve exposure, Paresthesia
Abbreviations: Mandibular third molar, M3M; Orthopantomography, Panoramic radiography, OPG; Cone beam computed tomography, CBCT
1. Introduction
The surgical extraction of the impacted mandibular third molar (M3M) is a routine procedure that is done on radiographic basis.1 Prophylactic removal of mandibular third molars always taken into consideration to prevent the pathologies associated with it.2 The standard imaging technique used in the preoperative evaluation of M3Ms is Panoramic radiography (OPG).3 3D and cross sectional image analysis has been made possible to understand with the use of third party software and advances in radiographic imaging modalities like CBCT.4 It enables the 3D visualization of the relationship between M3M roots and the IAC when patients are at increased risk of injury to the IAN based on OPG findings.5 Like all surgical procedures, removal of mandibular third molar is also associated with various complications like pain, swelling, trismus, dry socket, wound dehiscence and altered lip, tongue sensation. Previous studies have suggested post operative paresthesia as the third most common complication.6 The incidence of this complication is influenced by the surgeon's expertise, anatomical structures, operative tissue damage, postoperative oedema, surgical procedure, bone density, sex and the age of the patient.7,8 The incidence of injury to Inferior alveolar nerve (IAN) varies from 0.4% to 8.0% and permanent injury has been reported in less than 1% of patients.9 The purpose of study was to search: Is there any correlation exists between the OPG risk factors and the cortex of Inferior alveolar canal on CBCT and does this association has any influence on nerve exposure during impacted mandibular third molar surgery and post operative neurosensory deficit?
2. Material and methods
2.1. Study design and sample
A prospective study was designed to find out the research question. Patient consent was obtained from all the patients for any human participants in this study, including publication of any patient images. Inclusion criteria for patient selection was all types { mesioangular, vertical, distoangular, horizontal, inverted} of symptomatic impacted lower third molars (pain, pericoronitis, swelling, trismus), age range between 20 -50 years. Patients who were previously treated for fracture of jaw in third molar region, impacted third molars associated with any pathological condition & any systemic disorders were excluded. This prospective study was approved by local institution under IRB (Institutional review board) standards. All the patients approximately 200 presenting to Department of Oral & Maxillofacial Surgery from December 2018 to November 2020 were evaluated by using orthopantomogram for relationship of root apex of impacted third molar with the inferior alveolar canal and following risk signs noted:
-
1.
Interruption of white line (IWL).
-
2.
Diversion of mandibular canal.
-
3.
Narrowing of mandibular canal.
-
4.
Darkening of root.
-
5.
Deflection of root.
-
6.
Dark and bifid root apex.
-
7.
Narrowing of root.
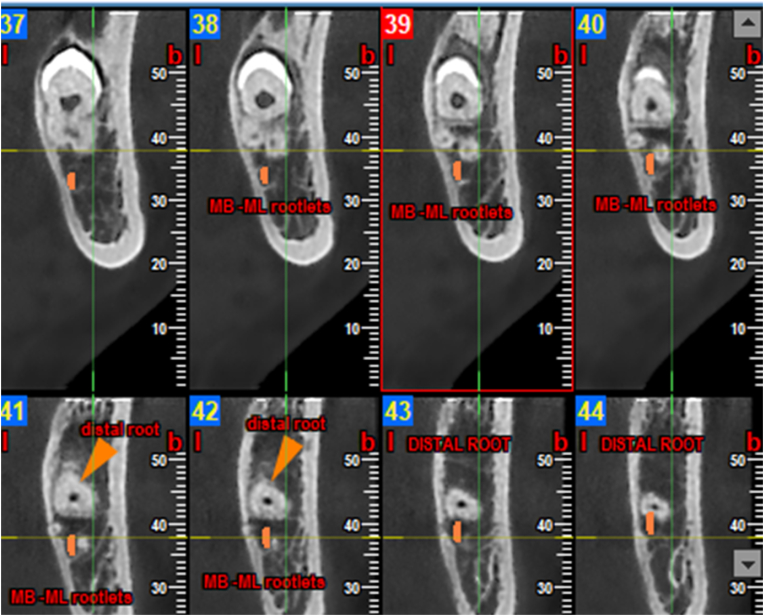
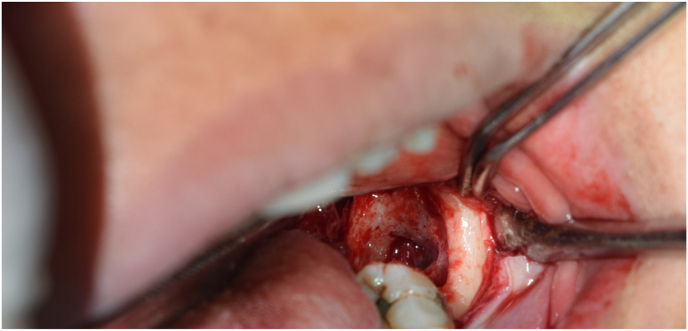
A total of 75 patients among these 200 showed the presence of two or more than two risk factors for inferior alveolar nerve injury which then were selected and further evaluated by using CBCT for Following factors: presence or absence of cortex of canal and location of canal on buccal, lingual, inferior, and interradicular position (Fig. 1). Neurovascular bundle exposed intraoperatively when the canal was located interradicularly (Fig. 2). Both the OPG and CBCT findings were analyzed compared and standard surgical technique i.e. Lingual split technique) was used by a single surgeon of at least 10 year of clinical experience.
Fig. 1.
Coronal section of CBCT depicting three roots and inter-radicular positioning of canal in relation to mesio-buccal and mesiolingual roots, (Orange colour marking shows the positioning of inferior alveolar canal. (41,42).
Fig. 2.
Intraoperative neurovascular bundle exposure in interradicularly located canal.
3. Results and observations
A total of 75 patients were included in the study. The teeth were classified according to Pell and Gregory's classification. The OPG findings of these impacted teeth were categorized as per description of 7 radiographic signs given by J.P Rood.12 On OPG Interruption of white line was recorded in 45 patients, Narrowing of canal was recorded in 12 patients, Divergence of mandibular canal was recorded in nine patients, Darkening of root was recorded in 63 patients, Deflection of root was recorded in 18 patients, Narrowing of root was recorded in 30 patients. All these patients were subjected to CBCT and following findings were noted:
-
1.
Cortex of inferior alveolar canal: Usually two radio opaque white lines which outline the canal are seen along the root apices of mandibular molars. Coronal section in CBCT provides the cortication status of inferior alveolar canal in relation to roots of mandibular third molar. Of the 75 patients assessed Interruption of cortex was reported in 51 patients.
-
2.
Comparison of OPG and CBCT findings: All the radiographic risk factors noted on OPG compared with interruption of cortex of inferior alveolar canal on CBCT. On OPG 45 patients were having interruption of white line while 51 patients showed the interruption of cortex of canal on CBCT (Table 1). Narrowing of canal on OPG noted in 12 patients while on CBCT only 6 patients revealed the narrowing of canal. Divergence of inferior alveolar canal on OPG noted in 9 patients while CBCT showed divergence of inferior alveolar canal in only 6 patients. 63 patients showed darkening of root on OPG while only 45 patients among these 63 showed interrupted cortex on CBCT. 18 patients showed deflection of root on OPG while only 9 patients among these 18 have interrupted cortex on CBCT. 30 patients showed narrowing of root on OPG while only 21 among these 30 have interrupted cortex on CBCT.
-
3.
Co-relation of interruption of cortex of inferior alveolar canal with the intra operative neurovascular bundle exposure (Table 2). 51 patients showed interruption of cortex on CBCT and nerve exposure was encountered in all these patients intraoperatively which was confirmed by clinical inspection of extraction socket after copious irrigation with the saline. The clinical diagnosis of neurovascular bundle was made on palpation with a suction tip followed by this if patient felt abnormal sensation to cold and pain.
-
4.
Co-relation of intra-operative nerve exposure with the location of inferior alveolar neurovascular bundle: The canal was located lingually in 36 cases and among these 36 patients only 18 were having intraoperative nerve exposure. Out of 75 patients 30 cases were having canal in inter-radicular position and all have nerve exposure intraoperatively. 6 patients out of 75 have canal in inferior position and only 3 have nerve exposure intraoperatively. While no nerve exposure was observed in buccaly located canal. Nerve exposure was observed in the following sequence: interradicular > lingual > inferior (Table 3).
-
5.
Exposure of Neurovascular bundle and neurosensory deficit: These two factor were considered as outcome variable of impacted mandibular third molar surgery. Patient was planned to evaluate the neurosensory deficit following the surgical procedure using three assesment methods that were light touch, pin prick, two point discrimination test on first, third and seventh post operative day. The testing was not repeated for the successive days if sensory perception was unaffected on first post operative day. The interesting part of this prospective study was the absence of neurosensory deficit even after the exposure of inferior alveolar neurovascular bundle.
Table 1.
Co-relation of Interruption of white line (IWL) on OPG with Interrupted cortex on CBCT.
| CBCT (Interrupted cortex) |
Total | Chi-Square value = 52.941 |
||||
|---|---|---|---|---|---|---|
| Absent | Present | |||||
| OPG (IWL) | Absent | Count | 24 | 6 | 30 | |
| % within OPG (IWL) | 80.0% | 20.0% | 100.0% | |||
| Present | Count | 0 | 45 | 45 | P value = 0.001 S |
|
| % within OPG (IWL) | 0.0% | 100.0% | 100.0% | |||
| Total | Count | 24 | 51 | 75 | ||
| % within OPG (IWL) | 32.0% | 68.0% | 100.0% | |||
Table 1 showing relation between Interruption of white line on OPG with interruption of cortex on CBCT. Among 75 patients interruption of white line was noted in 45 patients on OPG and was absent on 30 patients, where as on CBCT interruption of cortex was noted in 51 patients and was absent in 24 patients. On Chi-Square statistical analysis the p-value was found to be 0.001 significant, which shows that there is a correlation between interruption of white line on OPG with interruption of cortex on CBCT.
Table 2.
Intraoperative Nerve Exposure with CBCT Interrupted cortex.
| CBCT (Interrupted cortex) |
Total | Chi square value – 75.000 | ||||
|---|---|---|---|---|---|---|
| Absent | Present | |||||
| NERVE EXPOSURE | Absent | Count | 24 | 00 | 24 | |
| % within NERVE EXPOSURE | 100.0% | 0.0% | 100.0% | |||
| Present | Count | 0 | 51 | 51 | P value – 0.001 | |
| % within NERVE EXPOSURE | 0.0% | 100.0% | 100.0% | |||
| Total | Count | 24 | 51 | 75 | ||
| % within NERVE EXPOSURE | 32.0% | 68.0% | 100.0% | |||
Table 2 showing corelation between intraoperative nerve exposure with interruption of cortex on CBCT. Among 75 patients 51 patients were having interruption of cortex on CBCT and nerve exposure was encountered in all these patients intraoperatively. On statistical analysis the p value found to be 0.001 Significant, Which shows that there is a significant correlation between interruption of cortex with the intraoperative nerve exposure.
Table 3.
Intraoperative nerve exposure with location of canal on CBCT.
| CBCT FINDING (location of canal) |
Total | ||||||
|---|---|---|---|---|---|---|---|
| Buccal | Lingual | Interradicular | Inferior | ||||
| NERVE EXPOSURE | Absent | Count | 3 | 18 | 0 | 3 | 24 |
| % within NERVE EXPOSURE | 12.5% | 75.0% | 0.0% | 12.5% | 100.0% | ||
| Present | Count | 0 | 18 | 30 | 3 | 51 | |
| % within NERVE EXPOSURE | 0.0% | 35.3% | 58.8% | 5.9% | 100.0% | ||
| Total | Count | 3 | 36 | 30 | 6 | 75 | |
| % within NERVE EXPOSURE | 4.0% | 48.0% | 40.0% | 8.0% | 100.0% | ||
Table 3. Depicting the distribution of subjects according to location of canal and their relation with intraoperative nerve exposure. The canal was located lingually in 36 cases and among these 36 patients only 18 were having intraoperative nerve exposure. Out of 75 patients 30 cases were having canal in inter-radicular position and all have nerve exposure intraoperatively. 6 patients out of 75 have canal in inferior position and only 3 have nerve exposure intraoperatively. While no nerve exposure was observed in buccaly located canal.
3.1. Statistical analysis
Data was entered in a microsoft excel sheet and was analyzed using SSPS software version 26 and chi square test. On Comparison of all OPG radiographic risk signs with interruption of cortex the p value was found to be significant (0.001) between the interruption of white line on OPG with the interruption of cortex on CBCT (Table 1). All other OPG radiographic risk signs on comparison with interrupted cortex on CBCT showed a p value (>0.05) which made these radiographic risk signs insignificant. A significant p value (0.001) was found while correlating the interruption of cortex on CBCT with intraoperative nerve exposure (Table 2).
4. Discussion
Trigeminal and facial nerves are the nerves of Maxillofacial region that mostly get involved in various facial pathologies, facial injuries, Orthognathic surgeries and other surgical procedures. Among all the causes of nerve injuries, 52.1% nerve injuries occur due to surgical removal of third molar.2 Various factors responsible for nerve exposure and neurosensory deficit can be categorized into clinical, radiographic and operative procedures. Clinical features like teeth fully impacted in bone, horizontal impactions7,8 and older patients9, 10, 11 may suggest a higher risk of IAN injury. The completely formed roots, more mineralized bone and hypovascularity with increasing age, affecting the healing may be the reasons for this.12 Prophylactic removal of impacted mandibular third molar should be avoided in patients aged 24 years or older because of a high possibility of complications, such as permanent neurosensory deficits, infection, and alveolitis.13 Rood and Shehab12 has reported 5 types of signs on orthopantomogram, significantly related with IAN injury i.e. darkening of root, deflection of root, narrowing of the roots, interruption of the canal's white line and diversion of the canal. It has also been found that three of these signs i.e. interruption of the border of the white line of the canal, darkening of third molar roots, and change in course of the canal, are more valid predictors of a close relationship between the roots of the tooth and the IAN.14,15 Presence of cortex of canal is an important barrier between the root apex and inferior alveolar neurovascular bundle. Nerve exposure is likely in cases of close approximation of roots of the tooth and the IAN.8 Exposure of inferior alveolar neurovascular bundle if not treated carefully may lead to neurosensory deficit.9 Nerve compression and/or traction rather that severing the nerve during surgery, as a consequence of root movement during tooth luxation with an elevator has been accepted the most common reason of postoperative neurosensory deficit.8 The incidence of IAN injury is influenced by the surgeon's expertise, anatomical and radio-graphic factors, operative tissue damage, postoperative edema, surgical procedures, bone density, sex and the age of the patient. Iatrogenic origin of neurosensory dysfunction may be direct trauma to the nerve caused by the compression of IAN by elevators or indirectly by the elevated roots.9 Clinical observation of the neurovascular bundle and excessive haemorrhage into the socket may be the few possible causes of trauma to the IAN during third molar surgery. In the present study the significance of various risk factors in determining the nerve exposure and neurosensory deficit was assessed. Specifically it is hypothesized that interruption of white line on orthopantamogram is truly associated with the interruption of cortex on CBCT and it is an important risk sign for possible intraoperative nerve exposure during impacted third molar removal.
Tay A B G and Go W S11 found that beside various clinical, radiographical, anatomical risk factors, one important parameter is just exposure of intact inferior alveolar neurovascular bundle intraoperatively and hence they interpreted that in such cases there is 20% risk of postoperative paresthesia with a 70% chance of recovery within 1 year if it is exposed and observed during third molar surgery. Studies according to D. Gülicher, K. L. Gerlach,16 Sedaghatfar M, August M. A, Dodson T. B,17 which are also in agreement with the statement that intra operative opening of the inferior alveolar canal is also a cause for its deficit. This is contrary to our study in which, cases with intra operative inferior alveolar vascular bundle exposure and its clinical observation has not lead to any neurosensory deficit. The reason for this could be anatomical position of inferior alveolar nerve as it runs in inferior alveolar canal (IAC) and is supported by the alveolus and the neurovascular bundle. Moreover if we describe the structure of neurovascular bundle then the inferior alveolar vein is the most superior structure followed by inferior alveolar artery which lies underneath the vein followed by inferior alveolar nerve which is inferiorly placed in the canal. Thus superficial injuries to neurovascular bundle may only be limited to vein and artery leading to haematoma which compresses the inferior alveolar nerve and could be the cause for transient neurosensory deficit. Permanent paresthesia occurs only when the roots of impacted third molar are hooked around neurovascular bundle, that can lead to severing of nerve while doing surgical intervention. Present study showed a significant relationship between interruption of white line on OPG with the interruption of cortex on CBCT which is highly suggestive of intraoperative nerve exposure. This is in accordance with the study done by Rood J.P, Shehab Nooraldeen B.A.A12 and Matzen et al.18 who proposed that three signs i.e. diversion of mandibular canal, darkening of the root, interruption of white line are significantly associated with the nerve exposure and IAN injury.
We may also hypothesize that lingually and interadicularly positioned mandibular canal is more likely to be in contact with the mandibular third molar due to insufficient space. This is in accordance with the studies done by Liqun Gu, Chao Zhu, Kejia Chen, Xianchu Liu, Zhangui Tang2 who proposed the position of mandibular canal with the roots of the mandibular third molar. It was (88.1%) on the apical side, (7.9%) buccal side, (3.5%) on lingual side (3.5%) between the roots (0.5%) and the prevalence of nerve injury is significant on the interradicular and lingual position of the canal during surgery. Various studies have evaluated OPG/CBCT features in relation to mandibular third molar with the inferior alveolar canal but very few studies have compared all the OPG features with the cortex of canal in CBCT. Hence the outcome of present prospective study is that there is a significant association between interruption of white line on OPG with interruption of cortex on CBCT which along with the interradicularly and lingually positioned inferior alveolar neurovascular bundle becomes a strong affirmation for intra operative nerve exposure during third molar surgery.
5. Conclusion
Thus it can be concluded that exposure of intact inferioralveolar neurovascular bundle during impacted mandibular third molar surgery is not responsible for neurosensory deficit until and unless it is damaged during the procedure. Cortex of canal is an important barrier between the root apex and inferior alveolar neurovascular bundle and its existence can be precisely determined with the help of advanced investigatory protocol such as CBCT. Three dimensional image produced by using CBCT along with Surgeon's expertise and skills will be useful for adequate surgical planning in avoiding or reducing the nerve damage and preventing the possible complication of neurosensory deficit.
References
- 1.Su N., Wijk A.V., Berkhout E., et al. Predictive value of panoramic radiography for injury of inferior alveolar nerve after mandibular third molar surgery. J Oral Maxillofac Surg. 2017 Apr;75(4):663–679. doi: 10.1016/j.joms.2016.12.013. [DOI] [PubMed] [Google Scholar]
- 2.Gu L., Zhu C., Chen K., Liu X., Tang Z. Anatomic study of the position of the mandibular canal and corresponding mandibular third molar on cone-beam computed tomography images. Surg Radiol Anat. 2018 Jun;40(6):609–614. doi: 10.1007/s00276-017-1928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Selvi F., Dodson T.B., Naattestad A., et al. Factors that are associated with injury to inferior alveolar nerve in high risk patients after removal of third molars. Br J Oral Maxillofac Surg. 2013;51:868. doi: 10.1016/j.bjoms.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 4.Baqain Z.H., AlHadidi A. Cone beam computed tomography: rejuvenating dentistry. Fla Dent J. 2016;7:74. [Google Scholar]
- 5.Ghaeminia H., Meijer G.J., Soehardi A., et al. The use of cone beam CT for the removal of wisdom teeth changes the surgical approach compared with panoramic radiography: a pilot study. Int J Oral Maxillofac Surg. 2011;40:834. doi: 10.1016/j.ijom.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 6.Lee, Park Y., Ahn J., et al. Assessment of the proximity between the mandibular third molar and inferioralveolar canal using preoperative 3D-CT to prevent inferior alveolar nerve damage. Maxillofac Plast Reconstr Surg. 2015 Sep 17;37(1):30. doi: 10.1186/s40902-015-0030-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Araujo G.deT. T., Mamani M.P., Silva A., et al. I.R.F.R. Influence of cone beam computed tomography versus panoramic radiography on the surgical technique of third molar removal: a systematic review. Int J Oral Maxillofac Surg. 2019 Oct;48(10):1340–1347. doi: 10.1016/j.ijom.2019.04.003. [DOI] [PubMed] [Google Scholar]
- 8.Xu G.Z., Yang C., Fan X.D., et al. Anatomic relationship between impacted third mandibular molar and the mandibular canal as the risk factor of inferior alveolar nerve injury. Br J Oral Maxillofac Surg. 2013;51:e215–e219. doi: 10.1016/j.bjoms.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 9.Yang J., Cavalcanti M.G., Ruprecht A., et al. 2-D and 3-D reconstructions of spiral computed tomography in localization of the inferior alveolar canal for dental implants. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999 Mar;87(3):369–374. doi: 10.1016/s1079-2104(99)70226-x. [DOI] [PubMed] [Google Scholar]
- 10.Jerjes W., Upile T., Shah P., et al. Risk factors associated with injury to the inferior alveolar and lingual nervesfollowing third molar surgery—revisited. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010 Mar;109(3):335–345. doi: 10.1016/j.tripleo.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 11.Tay A.B.G., Go W.S. Effect of exposed inferior alveolar neurovascular bundle during surgical removal of impacted lower third molars. J Oral Maxillofac Surg. 2004 May;62(5):592–600. doi: 10.1016/j.joms.2003.08.033. [DOI] [PubMed] [Google Scholar]
- 12.Rood J.P., Shehab B.A.A.N. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg. 1990 Feb;28(1):20–25. doi: 10.1016/0266-4356(90)90005-6. [DOI] [PubMed] [Google Scholar]
- 13.Atieh M.A. Diagnostic accuracy of panoramic radiography. J Oral Maxillofac Surg. 2010;68:74–82. doi: 10.1016/j.joms.2009.04.074. [DOI] [PubMed] [Google Scholar]
- 14.Robinson P.P. Observations on the recovery of sensation following inferior alveolar nerve injuries. Br J Oral Maxillofac Surg. 1988;26(3):177–189. doi: 10.1016/0266-4356(88)90161-1. [DOI] [PubMed] [Google Scholar]
- 15.Manor Y., Abir R., Manor A., Kaffe I. Are different imaging methods affecting the treatment decision of extractions of mandibular third molars? Dentomaxillofacial Radiol. 2017 Jan;46(1) doi: 10.1259/dmfr.20160233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glicher D., Gerlach K.L. Sensory impairment of the lingual and inferior alveolar nerves following removal of impacted mandibular third molars. Int J Oral Maxillofac Surg. 2001;30:306–312. doi: 10.1054/ijom.2001.0057. 13. [DOI] [PubMed] [Google Scholar]
- 17.Sedaghatfar M., August M.A., Dodson T.B. Panoramic radiographic findings as predictors of inferior alveolar nerve exposure following third molar extraction. J Oral Maxillofac Surg. 2005;63:3–7. doi: 10.1016/j.joms.2004.05.217. [DOI] [PubMed] [Google Scholar]
- 18.Matzen L.H., Petersen L.B., Schropp L., Wenzel A. Mandibular canal-related parameters interpreted in panoramic images and CBCT of mandibular third molars as risk factors to predict sensory disturbances of the inferior alveolar nerve. Int J Oral Maxillofac Surg. 2019 Aug;48(8):1094–1110. doi: 10.1016/j.ijom.2019.03.898. [DOI] [PubMed] [Google Scholar]